1. Introduction
In today’s rapidly evolving and often volatile organizational environments, resilience has emerged as a critical factor for sustaining performance and achieving long-term success. Organizational resilience, defined as the capacity of an organization to anticipate, prepare for, respond to, and adapt to incremental changes and sudden disruptions to survive and prosper, is increasingly recognized as essential in maintaining competitive advantage and operational stability (Barasa et al., 2018; Kantur & İşeri-Say, 2012). This concept is particularly significant in high-stakes settings such as healthcare, where the ability to maintain operations under stress directly impacts patient care and outcomes.
One of the fundamental components underpinning organizational resilience is the health and safety of its workforce. Occupational health (OH) and occupational safety (OS) are pivotal in creating a supportive work environment that fosters employee engagement, resilience, and overall organizational robustness. Despite the intuitive link between these factors, empirical investigations into their direct and indirect effects on organizational resilience are relatively scarce.
The present research seeks to fill this gap by examining the sophisticated relationships between occupational health and safety, staff engagement, staff resilience, and organizational resilience within hospital settings. Specifically, this research aims to investigate the interrelationships between occupational health and safety (OHS), staff resilience (SR), staff engagement (SE), and hospital organizational resilience (HOR) within the context of Saudi Arabian healthcare settings, to provide actionable insights and recommendations for policymakers and healthcare administrators to foster a safer, more resilient, and high-performing healthcare environment in line with the national objectives of Vision 2030.
Previous literature underscores the significance of employee resilience and engagement in fostering organizational resilience. For instance, Kuntz et al. (2016) highlight that resilient employees contribute to organizational resilience by effectively managing stress and adapting to changes. Similarly, employee engagement, characterized by vigour, dedication, and absorption in work, has been linked to higher organizational resilience (Sull et al., 2015; Wang et al., 2017). However, the direct impacts of occupational health and safety on these mediators and, subsequently, on organizational resilience remain underexplored. This research employs a robust analytical framework to investigate these relationships, providing insights into the pathways through which occupational health and safety influence organizational resilience.
The structure of this research is organized as follows: the next section provides a review of relevant literature, followed by an outline of the research design and methodology. Subsequently, the data analysis and results are presented. The findings are then discussed, emphasizing the practical implications for hospital management and policy. The paper concludes with practical recommendations, a discussion of the study’s limitations, and suggestions for future research.
2. Literature Review
This literature review explores the intricate relationships between occupational health and safety (OHS), staff resilience (SR), staff engagement (SE), and hospital organizational resilience (HOR) within the context of hospitals in Saudi Arabia.
2.1. Theoretical Underpinnings
The theoretical foundation of this research is anchored in resilience theory and the job demands–resources (JD–R) model. This theoretical integration underscores the multifaceted impacts of OHS on both individual and organizational levels, providing a comprehensive lens through which to explore the dynamics within Saudi Arabian hospitals.
2.1.1. Resilience Theory
Resilience theory emphasizes the ability of individuals and organizations to withstand, adapt to, and recover from adverse situations. Carlson et al. (2012) describe resilience as a multifaceted concept encompassing robustness, resourcefulness, and adaptability, essential for maintaining functionality during crises. Kantur and İşeri-Say (2012) further elaborate on this by proposing a conceptual, integrative organizational resilience framework, highlighting the interplay between cognitive, behavioural, and contextual factors. This framework underscores the importance of proactive and reactive capabilities in fostering resilience. Kantabutra and Ketprapakorn (2021) build on this by discussing the dynamic and iterative nature of resilience, where organizations continuously evolve and adapt their structures and processes in response to internal and external challenges. Collectively, these perspectives illustrate that resilience is not merely a reactive mechanism but a proactive strategy that involves continuous learning, adaptation, and improvement. Resilience theory provides a comprehensive understanding of how organizations can sustain performance and thrive despite significant disruptions and uncertainties.
2.1.2. The Job Demands–Resources (JD–R) Model
The job demands–resources (JD–R) model, developed by Demerouti et al. (2001), is a comprehensive framework that examines how job demands, and job resources interact to influence employee well-being and organizational outcomes. According to this model, job demands refer to a job’s physical, psychological, social, or organizational aspects that require sustained physical or mental effort and are therefore associated with specific physiological and psychological costs. Conversely, job resources are those physical, psychological, social, or organizational aspects of the job that help achieve work goals, reduce job demands, and stimulate personal growth and development. The model suggests that high job demands can lead to burnout and other adverse outcomes, especially when job resources are insufficient. Conversely, adequate job resources can buffer the negative impact of job demands and enhance motivation and engagement (Demerouti & Bakker, 2011). Taris and Schaufeli (2015) expand on this by highlighting how job resources mitigate the adverse effects of job demands and play a crucial role in fostering employee engagement, which is critical for organizational success. Lesener et al. (2019) provide a meta-analytic review of longitudinal studies supporting the JD–R model, demonstrating that job resources are significantly associated with positive work outcomes over time, while job demands are linked to burnout and other adverse outcomes. Overall, the JD–R model offers a robust framework for understanding the dynamic interplay between job demands and resources, emphasizing the importance of maintaining a balance to promote employee well-being and organizational resilience.
2.2. Relationship between Occupational Health and Safety (OHS) and Staff Resilience (SR)
Occupational health and safety (OHS) refers to practices, policies, and regulations designed to prevent workplace injuries, illnesses, and accidents. This includes risk assessments, safety training, ergonomic interventions, and mental health support (Ahmad & Osei, 2021; Allende et al., 2017). Staff resilience (SR) is the capacity of individuals to recover from adverse events, cope with stress, and adapt positively to changes and challenges in the workplace (Barasa et al., 2018; Kuntz et al., 2016). Resilient staff can effectively manage work-related pressures, maintain performance, and contribute positively to their work environment (Itzhaki et al., 2015). This resilience is influenced by cultural and national values, which shape how employees perceive and respond to organizational challenges, particularly in times of adversity or crisis (Isidro & Calleja, 2021). Additionally, authentic leadership is critical in fostering employee resilience by providing support and promoting a positive organizational climate, which helps employees navigate workplace challenges more effectively (Mao et al., 2022). In hospitals, resilient staff can effectively manage high workloads, emotional stress, and unexpected situations (Sull et al., 2015).
The relationship between OHS and SR involves physical safety, mental health, and organizational support. Comprehensive OHS programmes protect employees from physical hazards and provide psychological support, contributing to overall well-being and resilience (Brown et al., 2017; Gonçalves et al., 2021). García et al. (2007) find that addressing psychosocial risk factors through OHS interventions significantly improves employees’ mental health and resilience. Similarly, Gopang et al. (2017) demonstrate that small and medium-sized enterprises (SMEs) with robust OHS practices have employees who exhibit higher resilience and better performance. Barasa et al. (2018) emphasize the role of organizational resilience, which can be fostered through robust OHS practices. Their systematic review highlights that organizations with strong safety cultures and proactive health measures tend to have more resilient staff, as these measures provide a stable and supportive environment. Moreover, Itzhaki et al. (2015) find that exposure to workplace violence and stress in mental health nurses was mitigated by effective OHS interventions, which enhanced their resilience and life satisfaction. This study underscores the importance of OHS in managing stressors and promoting psychological resilience in high-risk environments. Based on the literature review, the following hypothesis is proposed:
H1. Higher occupational health and safety levels in hospitals (OHS) are positively associated with greater staff resilience (SR).
2.3. Relationship between Staff Resilience (SR) and Hospital Organizational Resilience (HOR)
Hospital organizational resilience refers to a hospital’s ability to anticipate, prepare for, respond to, and adapt to incremental changes and sudden disruptions to survive and thrive (Kantur & İşeri-Say, 2012). This concept involves robust systems, adaptive capacity, and strategic foresight to withstand crises while providing essential healthcare services (Lee et al., 2013). Resilience is crucial for maintaining operational continuity and quality care during natural disasters, pandemics, or other significant disruptions (Barasa et al., 2018; Brown et al., 2017). The importance of organizational resilience is further highlighted by research demonstrating its positive impact on performance during the COVID-19 pandemic, showing that resilient organizations, including hospitals, can better manage and recover from significant challenges (Gröschke et al., 2022; Mohammad et al., 2022).
The relationship between staff resilience and hospital organizational resilience is integral, particularly in the high-stakes environment of healthcare. Barasa et al. (2018) underscore that organizational resilience is rooted in the resilience of its members. When staff are resilient, they contribute to a supportive and dynamic organizational culture that enhances overall resilience. Staff resilience equips employees with the skills to handle stress, adapt to changes, and recover from challenges, fostering a resilient organizational framework. Itzhaki et al. (2015) highlight that resilient staff are better prepared to manage job stress and maintain high levels of job satisfaction and mental health, even when exposed to workplace violence or other stressors.
This personal resilience directly influences their ability to contribute positively to the organization’s resilience by ensuring continuous and effective service delivery during crises. In healthcare settings, where unexpected events and high-pressure situations are common, resilient staff are crucial for maintaining operational stability and quality of care (Sull et al., 2015). According to Cooke et al. (2019), high-performance work systems that enhance employee resilience also contribute to increased organizational resilience. In hospitals, such systems include training programmes, supportive leadership, and employee engagement initiatives. These elements enhance individual resilience and create a robust organizational culture that can withstand and adapt to crises (Malik & Garg, 2020). Liang and Cao (2021) demonstrate that resilient employees contribute to organizational resilience through effective coping mechanisms and managerial resilience. This interplay is crucial in hospitals where the well-being of staff directly impacts patient care and organizational effectiveness. Resilient staff are more likely to engage in proactive behaviours, collaborate effectively with colleagues, and support organizational initiatives to enhance resilience (García et al., 2007). Given the relationships and empirical evidence, we hypothesize that:
H2.
Increased staff resilience (SR) is positively associated with enhanced hospital organizational resilience (HOR).
2.4. Relationship between Occupational Health and Safety (OHS) and Hospital Organizational Resilience (HOR)
The relationship between occupational health and safety and hospital organizational resilience is increasingly recognized as critical in ensuring the sustainability and effectiveness of healthcare services, particularly in times of crisis. Occupational health and safety in hospitals refer to the policies, procedures, and practices implemented to protect healthcare workers’ physical and mental well-being. This includes addressing hazards, providing training, ensuring adequate staffing, and promoting a workplace health and safety culture (Ahmad & Osei, 2021). On the other hand, hospital organizational resilience pertains to the hospital’s ability to anticipate, respond to, and recover from adverse events, ensuring continuous service delivery and maintaining its core functions under stress (Barasa et al., 2018). Allende et al. (2017) suggest that effective OHS practices are fundamental in mitigating risks and fostering a resilient organizational structure. They argue that hospitals with robust OHS frameworks are better positioned to withstand and recover from disruptions, enhancing their overall resilience. Additionally, the systematic review by Barasa et al. (2018) highlights the multifaceted nature of resilience, identifying various strategies and interventions that strengthen organizational capacity, such as leadership support, employee training, and comprehensive safety programmes. This aligns with the findings of Gopang et al. (2017), who demonstrate through empirical research that effective OHS measures directly correlate with improved performance metrics and resilience in SMEs, extending the applicability of these principles to healthcare settings. This leads to the formulation of the hypothesis:
H3. Occupational health and safety in hospitals (OHS) has a direct positive impact on hospital organizational resilience (HOR).
2.5. Relationship between Occupational Health and Safety (OHS) and Staff Engagement (SE)
Staff engagement refers to employees’ emotional commitment and involvement with their organization and its goals. Engaged employees display enthusiasm, dedication, and a readiness to surpass their basic job requirements (Hawkes et al., 2017; Saks, 2008). This engagement is influenced by factors such as transformational leadership, job resources, and opportunities for recovery, which collectively enhance employees’ willingness to invest effort and energy in their roles (Hawkes et al., 2017). A safe working environment significantly influences staff engagement. When healthcare workers feel safe and their well-being is prioritized, they are more likely to be motivated and committed to their work. This sense of security enhances their ability to engage fully in their roles, leading to overall job satisfaction (Cooke et al., 2019). Furthermore, job demands and resources are critical in determining engagement levels. High job resources, such as support and feedback, can buffer the adverse effects of job demands, reducing burnout and promoting engagement (Crawford et al., 2010). Healthcare organizations can foster a highly engaged and resilient workforce by ensuring a supportive and safe work environment. For instance, Gopang et al. (2017) emphasize that effective OHS measures directly contribute to employees’ improved performance and well-being, which fosters higher engagement levels. In contrast, poor occupational health and safety can increase stress, burnout, and job dissatisfaction among hospital staff. This affects their mental and physical health and diminishes their capacity to engage positively with their work (Itzhaki et al., 2015). García et al. (2007) find that adverse psychosocial factors and poor occupational health conditions are associated with low levels of staff engagement and increased absenteeism. Based on the reviewed literature, the following hypothesis is proposed:
H4. Occupational health and safety in hospitals (OHS) has a direct positive impact on staff engagement (SE).
2.6. Relationship between Staff Engagement (SE) and Hospital Organizational Resilience (HOR)
Studies have shown that high levels of staff engagement contribute positively to organizational resilience. Allende et al. (2017) emphasize that aligning organizational pathologies with resilience indicators is crucial for sustaining organizational health and productivity. Engaged employees are likelier to exhibit proactive behaviours, adapt to changes, and support their organization through challenges. Similarly, Barasa et al. (2018) highlight that fostering resilience through engaged staff can improve responses to external pressures and shocks. Brown et al. (2017) demonstrate that engaged employees are vital for maintaining operational resilience during disruptions. Their findings suggest that engaged staff are better equipped to handle stress, recover quickly from setbacks, and contribute to organizational continuity. Dwomoh et al. (2020) explore human resource strategies during the COVID-19 pandemic and discover that engaging staff through supportive policies and practices helps maintain business sustainability. This reinforces the idea that employee engagement is a foundational element of organizational resilience. Given the existing literature, it is hypothesized that:
H5. There is a positive relationship between staff engagement (SE) and hospital organizational resilience (HOR).
2.7. Mediator Roles
Staff resilience, the ability of employees to adapt and thrive in the face of adversity, is crucial in mediating the effects of OHS on organizational resilience. Itzhaki et al. (2015) explore the relationship between exposure to violence, job stress, and staff resilience among mental health nurses, highlighting how resilient staff can better cope with occupational hazards and maintain high job satisfaction and performance levels. This resilience, in turn, contributes to overall organizational resilience. García et al. (2007) link adverse psychosocial factors to poor occupational health, demonstrating that addressing these factors through effective OHS measures can enhance staff resilience. Liang and Cao (2021) explore how employee resilience contributes to organizational resilience through coping mechanisms and managerial resilience, suggesting a cascading effect where resilient employees bolster the organization’s overall resilience. Itzhaki et al. (2015) and Kuntz et al. (2016) underscore the importance of psychological resilience among healthcare workers. They suggest that occupational stressors and exposure to violence significantly impact mental health, which, in turn, affects the overall resilience of hospital systems. Creating a supportive work environment through OHS interventions reduces stress and burnout and enhances staff resilience, enabling them to better cope with challenges. This relationship is further supported by the work of Liang and Cao (2021), who illustrate the role of coping mechanisms and managerial resilience in linking employee resilience to organizational resilience, thereby highlighting the interconnectedness of individual and organizational levels of resilience. Given the relationships and empirical evidence, we hypothesize that:
H6. Staff resilience (SR) mediates the relationship between occupational health and safety (OHS) and hospital organizational resilience (HOR).
Research indicates that staff engagement can mediate the relationship between OHS and organizational resilience. For instance, effective OHS measures can lead to higher employee satisfaction and lower stress levels, enhancing engagement (Egbuta, 2019; García et al., 2007). Engaged employees are more resilient and better able to adapt to changes and challenges, contributing to overall organizational resilience (Kuntz et al., 2016; Malik & Garg, 2020). Based on the literature, the following hypothesis is proposed:
H7. Staff engagement (SE) mediates the relationship between occupational health and safety (OHS) and organizational resilience in hospitals (OR).
Staff engagement and resilience can mediate the relationship between OH and OR. Meintjes and Hofmeyr (2018) find that perceived organizational support enhances employee engagement and resilience, which are crucial for organizational resilience. Similarly, Tonkin et al. (2018) highlight the importance of employee well-being in building organizational resilience through enhanced engagement and resilience. Given these findings we hypothesize that.
H8. Staff engagement (SE) and staff resilience (SR) serially mediate the relationship between occupational health (OHS) and organizational resilience (OR) in hospitals in Saudi Arabia.
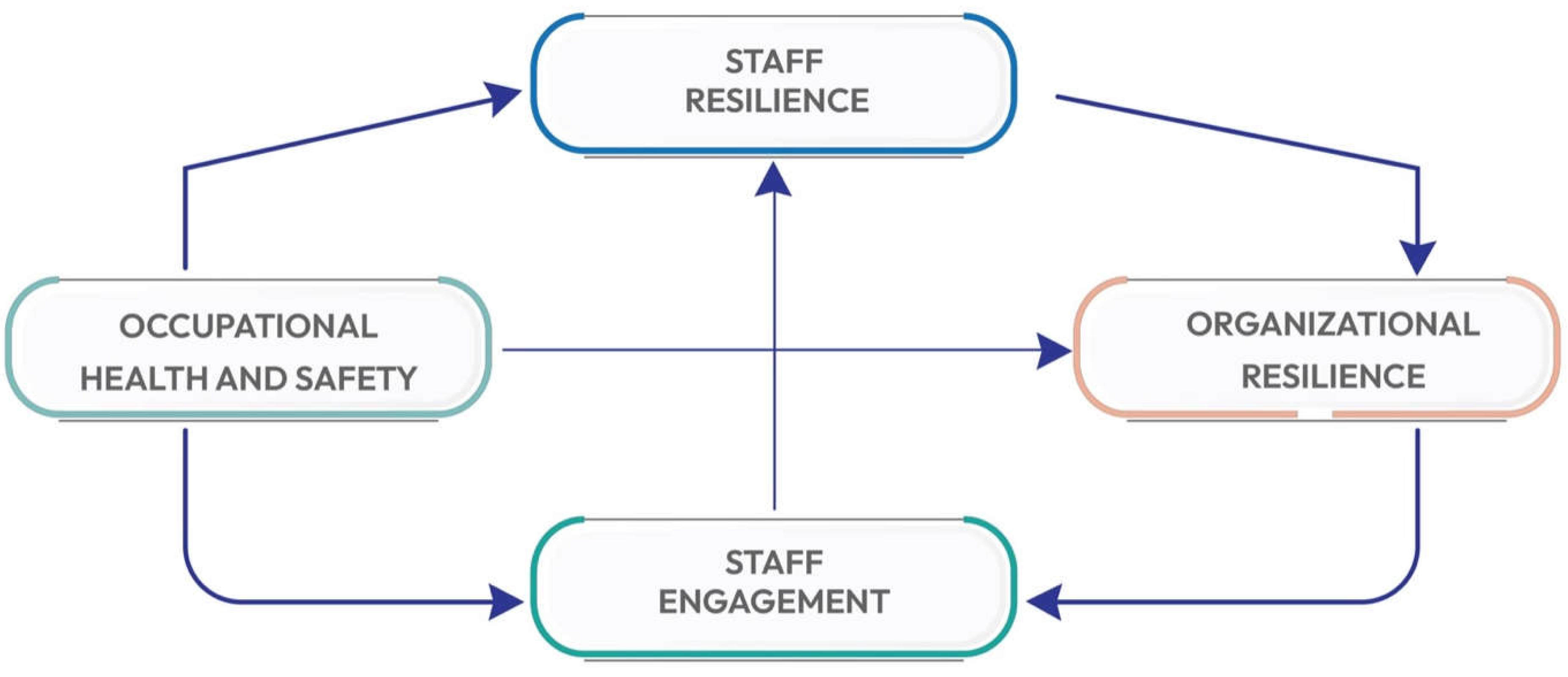
Figure 1.
Research conceptual model.
Figure 1.
Research conceptual model.
3. Method
3.1. Research Design, Sample, and Population
This research investigates the relationships among occupational health and safety (OHS), staff resilience (SR), staff engagement (SE), and hospital organizational resilience (HOR) within hospitals in Saudi Arabia. A robust quantitative research design was utilized, adopting a quantitative approach with PLS-SEM, a sophisticated statistical tool for analysing complex cause-and-effect relationship models that involve multiple predictors and outcomes. Data analysis was conducted using Smart PLS version 4, developed by Ringle et al. in 2024.The population for this research consists of administrative staff working in public and private hospitals across Saudi Arabia. A stratified random sampling method was employed to ensure a representative sample, resulting in 127 respondents. The demographic variables describing the sample are presented in
Table 1.
The demographic analysis highlights key patterns in qualifications and experience among male and female administrative staff in Saudi Arabian hospitals. Most male respondents with secondary education are aged 41–50 (26%), while graduates are mostly in the 31–40 age group (71%), and postgraduates are primarily 41–50 (42%). Female respondents with secondary education are mainly aged 20–30 (15%), with graduates in the 20–30 age range (79%), and postgraduates mostly 31–40 (32%). In terms of experience, a significant number of males have over 15 years of experience (43%), while females predominantly have less than five years (46%). Both genders show a balanced distribution in the 5–10 years’ experience category.
3.2. Data Collection
Data were collected using a structured questionnaire, including validated scales and measures for each variable, as shown in
Table 2.
3.3. Data Analysis and Results
The collected data was analysed using partial least squares (PLS) path modelling. SmartPLS version 4, developed by Ringle et al. in 2024, was used to perform the data analysis, as it enables the analysis of ordinal variables (Hair et al., 2021). In addition, it employs a component-based approach to structural equation modelling, making it highly suitable for exploratory research and applicable for confirmatory research (Sarstedt et al., 2014a). The model has two types of variables: exogenous latent variables, which explain other constructs, and endogenous latent variables, which are the constructs being investigated (Hair et al., 2017c).
3.4. Measurement Model
The analysis of the measurement model, as presented in
Table 3, demonstrates robust reliability and validity across all constructs: occupational health and safety, organizational resilience, staff engagement, and staff resilience.
The Cronbach’s alpha values for all constructs are above the threshold of 0.7, indicating high internal consistency reliability. Specifically, occupational health and safety has a Cronbach’s alpha of 0.928, organizational resilience is 0.950, staff engagement is 0.949, and staff resilience is 0.953, signifying excellent reliability for each construct. Furthermore, the composite reliability (rho_ a and rho_c) values for all constructs exceed 0.7, underscoring the constructs’ high reliability. Occupational health and safety exhibit a rho_a of 0.959 and rho_c of 0.941 organizational resilience shows a rho_a of 0.953 and rho_c of 0.959, staff engagement presents a rho_a of 0.952 and rho_c of 0.958, and staff resilience demonstrates a rho_a of 0.954 and rho_c of 0.959. These high values indicate that the measurement items consistently reflect their respective constructs.
The average variance extracted (AVE) values, which measure convergent validity, are also above the acceptable threshold of 0.5 for all constructs. Occupational health and safety has an AVE of 0.606, organizational resilience has an AVE of 0.744, staff engagement has an AVE of 0.767, and staff resilience has an AVE of 0.659. These AVE values confirm that the latent constructs capture a substantial amount of variance in the observed variables, indicating good convergent validity. According to
Table 3, construct reliability and validity are demonstrated.
3.5. Discriminant Validity
Discriminant validity was assessed using the Fornell–Larcker criterion, which evaluates whether each construct shares more variance with its indicators than with other constructs. According to the Fornell–Larcker criterion, the square root of the AVE of each construct should be greater than the highest correlation it has with any other construct. The results are presented in
Table 4 below.
The diagonal elements (bolded) represent the square root of the AVE for each construct, while the off-diagonal elements represent the correlations between constructs. The square roots of the AVEs for OHS (0.778), OR (0.863), SE (0.876), and SR (0.812) are all greater than their respective inter-construct correlations. This indicates that each construct shares more variance with its indicators than other constructs, confirming discriminant validity. These results support the distinctiveness of OHS, OR, SE, and SR within the model, thus providing evidence for the validity of the measurement model according to the Fornell–Larcker criterion.
3.6 Structural Model Measurement
The structural model analysis focuses on assessing the overall explanatory power, path coefficients (β), and significance levels to evaluate the relationships between the constructs. The explanatory power is measured using the R2 value, which indicates the proportion of variance in the dependent variable explained by the independent variables. High R2 values suggest a strong explanatory power of the model. Path coefficients (β) represent the strength and direction of the relationships between constructs, while significance levels determine the statistical significance of these relationships.
Collinearity statistics, represented by the variance inflation factor (VIF), are crucial for assessing multicollinearity among predictor variables. A VIF value below 5 generally indicates that multicollinearity is not a concern. In
Table 5, the VIF values for the paths range from 1.000 to 2.666, all of which are well below the critical threshold of 5, indicating that multicollinearity is not an issue and that the estimates of the path coefficients are reliable.
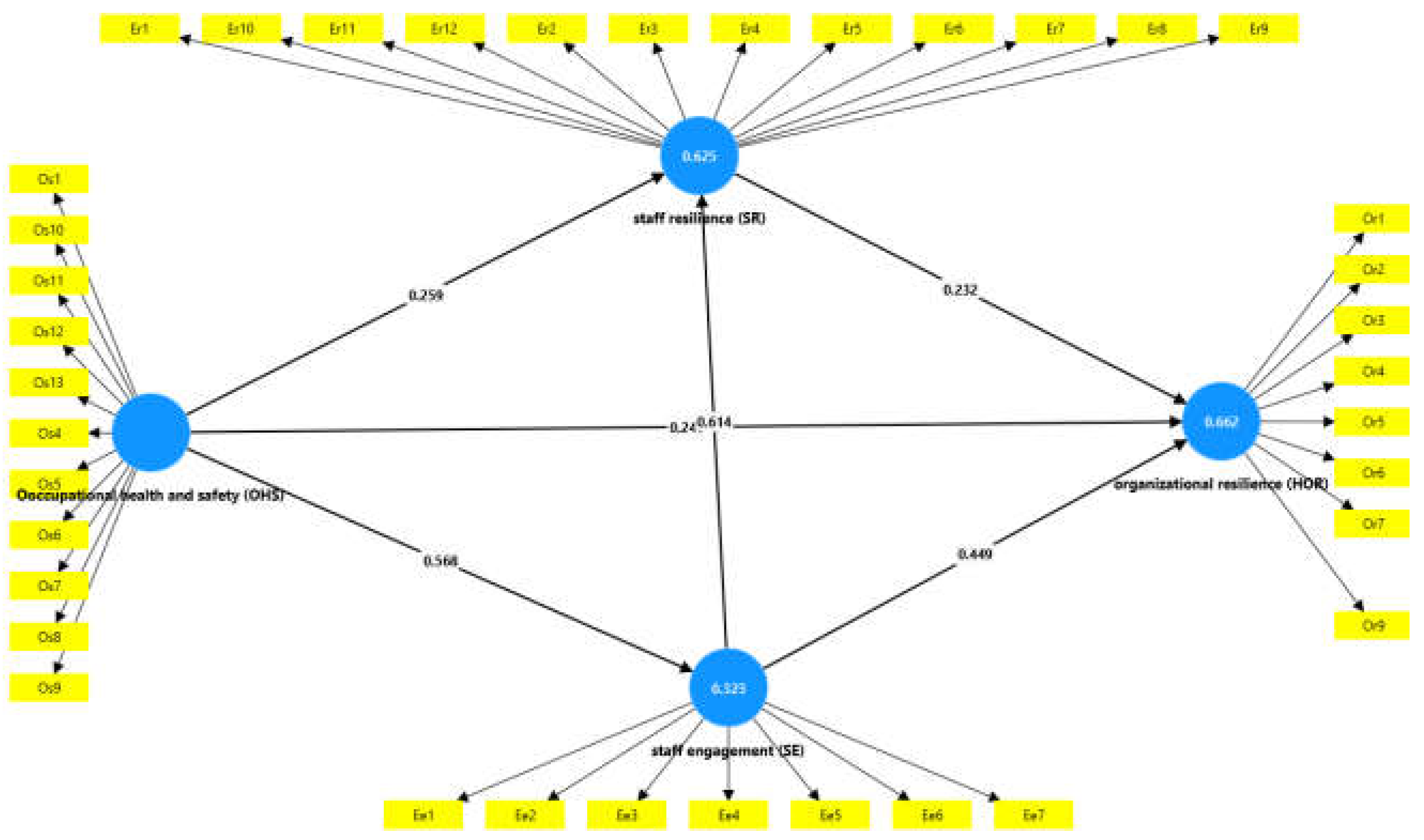
Figure 2.
Structural Model.
Figure 2.
Structural Model.
The values in
Table 5 demonstrate that the predictor variables in the model do not exhibit problematic levels of collinearity, ensuring that the path coefficients derived from the structural model are robust and interpretable. The analysis confirms that occupational health and safety, along with staff engagement and resilience, significantly contribute to explaining organizational resilience, underscoring the importance of these factors in fostering a resilient healthcare environment.
3.7 The Model’s Explanatory Power
The model’s explanatory power is assessed using the coefficient of determination (R-squared) values, which indicates the proportion of variance in the dependent variables that is predictable from the independent variables. As presented in
Table 6, the R-squared value for organizational resilience (OR) is 0.662, with an adjusted R-squared of 0.654, suggesting that the model can explain approximately 66.2% of the variance in organizational resilience. This high value indicates strong explanatory power for this construct. For staff engagement (SE), the R-squared value is 0.323, and the adjusted R-squared is 0.317, indicating that the model accounts for 32.3% of the variance in staff engagement, reflecting moderate explanatory power. Staff resilience (SR) shows an R-squared value of 0.625 and an adjusted R-squared of 0.619, meaning that the model explains 62.5% of the variance, which denotes substantial explanatory power. Overall, these R-squared values demonstrate that the model has good explanatory power, particularly for organizational resilience and staff resilience, highlighting the model’s robustness in explaining the variance in these key constructs within the context of occupational health and safety, staff resilience, and staff engagement. See
Table 6
3.6. Path Coefficients and Hypotheses Testing
This section, based on
Table 7, provides an analysis of the path coefficients and hypotheses testing, which are critical in understanding the relationships between occupational health and safety (OHS), staff resilience (SR), staff engagement (SE), and hospital organizational resilience (HOR) within the studied context.
3.6.1. Hypothesis Testing
Hypothesis H1, which posits that occupational health and safety (OHS) positively affects staff resilience (SR), is strongly supported by the data. The original sample (O) value is 0.608, indicating a positive relationship between OHS and SR. The sample mean (M) is 0.616, with a standard deviation (STDEV) of 0.088, which reflects the variability of this relationship in the sample. The T statistics value of 6.872 (|O/STDEV|) is significantly above the common threshold of 1.645 for significance in a one-tailed test, suggesting strong evidence against the null hypothesis. The p-value of 0.000 further confirms the statistical significance of this relationship. Given these results, hypothesis H1 is accepted, indicating that better occupational health and safety practices significantly enhance staff resilience. This finding underscores the importance of prioritizing OHS in fostering a resilient workforce, which is particularly crucial in the demanding environment of healthcare settings in Saudi Arabia.
The analysis validates hypothesis H2, which proposes that staff resilience (SR) positively influences organizational resilience (OR). The original sample (O) value of 0.232 indicates a positive association between SR and OR. The sample mean (M) is 0.221, with a standard deviation (STDEV) of 0.096, highlighting the variability within the data. The T statistic of 2.416 (|O/STDEV|) exceeds the threshold of 1.645 for a one-tailed test, providing robust evidence against the null hypothesis. Additionally, the p-value of 0.008 signifies statistical significance. Therefore, hypothesis H2 is accepted, demonstrating that enhanced staff resilience significantly contributes to greater organizational resilience. This result emphasizes the critical role of fostering staff resilience to strengthen the overall resilience of healthcare organizations, aligning with broader efforts to enhance healthcare quality and stability in Saudi Arabia.
The analysis strongly supports hypothesis H3, which posits that occupational health and safety (OHS) positively influences organizational resilience (OR). The original sample (O) value is 0.636, indicating a robust positive relationship between OHS and OR. The sample mean (M) is 0.646, with a standard deviation (STDEV) of 0.072, suggesting consistent findings. The T statistic 8.845 (|O/STDEV|) significantly exceeds the critical value 1.645 for a one-tailed test, providing substantial evidence against the null hypothesis. The p-value of 0.000 confirms the statistical significance of this relationship. Therefore, hypothesis H3 is accepted, demonstrating that effective occupational health and safety measures significantly enhance organizational resilience. This underscores the importance of OHS practices in building a resilient healthcare system, which is crucial for improving the quality and stability of healthcare services in Saudi Arabia. The findings align with the broader goals of national health policies, emphasizing the need for robust OHS frameworks to support organizational resilience in the healthcare sector.
Hypothesis H4, which asserts that occupational health and safety (OHS) positively impacts staff engagement (SE), is confirmed by the data analysis. The original sample (O) value of 0.568 signifies a substantial positive effect of OHS on SE. The sample mean (M) is 0.577, with a standard deviation (STDEV) of 0.087, indicating a reliable and consistent relationship. The T statistic 6.553 (|O/STDEV|) greatly exceeds the critical value 1.645 for a one-tailed test, providing robust evidence against the null hypothesis. The p-value of 0.000 further reinforces the statistical significance of this finding. Consequently, hypothesis H4 is accepted, demonstrating that effective occupational health and safety measures significantly enhance staff engagement. This result highlights the critical role of OHS in fostering a motivated and engaged workforce, which is essential for the overall performance and resilience of healthcare organizations in Saudi Arabia. The findings suggest that improving OHS practices can lead to higher levels of staff engagement, contributing to a more committed and productive workforce, thereby aligning with the objectives of national health initiatives and policies.
Hypothesis H5, which posits that staff engagement (SE) positively influences organizational resilience (OR), is supported by the data analysis. The original sample (O) value is 0.591, indicating a strong positive effect of SE on OR. The sample mean (M) is 0.580, with a standard deviation (STDEV) of 0.090, reflecting a consistent and reliable relationship between these constructs. The T statistic 6.593 (|O/STDEV|) significantly exceeds the critical value 1.645 for a one-tailed test, providing compelling evidence to reject the null hypothesis. The p-value of 0.000 further confirms the statistical significance of this result. Therefore, hypothesis H5 is accepted, demonstrating that higher levels of staff engagement contribute significantly to organizational resilience. This finding underscores the importance of fostering engagement among staff to enhance the resilience of healthcare organizations in Saudi Arabia. Engaged employees are likely to be more proactive, adaptive, and supportive. These are key attributes for building resilient healthcare institutions capable of surviving various operational challenges and improving healthcare delivery.
Table 7.
Path Coefficients and Hypotheses Testing.
Table 7.
Path Coefficients and Hypotheses Testing.
| |
Original sample (O) |
Sample mean (M) |
Standard deviation (STDEV) |
T statistic (|O/STDEV|) |
p-value |
Status |
| H1: Occupational health and safety (OHS) -> Staff resilience (SR) |
0.608 |
0.616 |
0.088 |
6.872 |
0.000 |
Accepted |
| H2: Staff resilience (SR) -> Organizational resilience (OR) |
0.232 |
0.221 |
0.096 |
2.416 |
0.008 |
Accepted |
| H3: Occupational health and safety (OHS) -> Organizational resilience (OR) |
0.636 |
0.646 |
0.072 |
8.845 |
0.000 |
Accepted |
| H4: Occupational health and safety (OHS) -> Staff engagement (SE) |
0.568 |
0.577 |
0.087 |
6.553 |
0.000 |
Accepted |
| H5: Staff engagement (SE) -> Organizational resilience (OR) |
0.591 |
0.580 |
0.090 |
6.593 |
0.000 |
Accepted |
| Assessment of the mediator construct |
|
| H6: Occupational health and safety (OHS) -> Staff resilience (SR) -> Organizational resilience (OR) |
0.060 |
0.057 |
0.030 |
2.012 |
0.022 |
Accepted |
| H7: Occupational health and safety (OHS) -> Staff engagement (SE) -> Staff resilience (SR) |
0.349 |
0.343 |
0.055 |
6.329 |
0.000 |
Accepted |
| Assessment of the serial mediators construct |
|
| H8: Occupational health and safety (OHS) -> Staff engagement (SE) -> Staff resilience (SR) -> Organizational resilience (OR) |
0.081 |
0.077 |
0.038 |
2.148 |
0.016 |
accepted |
3.6.2. Assessment of the Mediator Construct
Hypothesis H6 examines the mediating role of staff resilience (SR) in the relationship between occupational health and safety (OHS) and organizational resilience (OR). The analysis supports this hypothesis, with an original sample (O) value of 0.060, indicating a positive indirect effect of OHS on OR through SR. The sample mean (M) is 0.057, with a standard deviation (STDEV) of 0.030. The T statistic of 2.012 (|O/STDEV|) exceeds the critical value of 1.645 for a one-tailed test, providing significant evidence to reject the null hypothesis. The p-value of 0.022 confirms the statistical significance of this mediating effect. Therefore, hypothesis H6 is accepted, indicating that staff resilience partially mediates the relationship between occupational health and safety and organizational resilience. This finding highlights the critical role of staff resilience in translating the benefits of occupational health and safety measures into enhanced organizational resilience.
Hypothesis H7 posits that staff engagement (SE) mediates the relationship between occupational health and safety (OHS) and staff resilience (SR). The analysis confirms this hypothesis with an original sample (O) value of 0.349, indicating OHS’s strong positive indirect effect on SR through SE. The sample mean (M) is 0.343, with a standard deviation (STDEV) of 0.055. The T statistic of 6.329 (|O/STDEV|) is significantly above the critical value of 1.645 for a one-tailed test, providing substantial evidence to reject the null hypothesis. The p-value of 0.000 further confirms the statistical significance of this mediating effect. Consequently, hypothesis H7 is accepted, demonstrating that staff engagement significantly mediates the relationship between occupational health and safety and staff resilience. This result underscores the importance of fostering an engaging work environment to enhance staff resilience.
3.6.3. Assessment of the Serial Mediators Construct
The research summarized in
Table 8 assessed the serial mediation effect of staff engagement and staff resilience in the relationship between occupational health and safety (OHS) and organizational resilience (OR). The total effect of OHS on OR was significant (β = 0.636, p < 0.005), indicating a strong direct relationship. The direct effect of OHS on HOR remained significant (β = 0.240, p < 0.005), suggesting that OHS directly influences OR even in the presence of mediators. The indirect effect of OHS on OR through staff engagement and staff resilience was found to be 0.081 with a T statistic of 2.148 and a p-value of 0.016, indicating significance. However, this mediation effect was deemed partial, as the direct effect still held considerable influence. The confidence interval for the indirect effect ranged from 0.019 to 0.143, supporting the presence of mediation. Despite the partial mediation, these findings emphasize that while staff engagement and resilience mediate the impact of OHS on OR, there remains a significant direct effect of OHS on OR. This underscores the importance of OHS in fostering organizational resilience, both directly and indirectly, through its influence on staff engagement and resilience.
4. Discussion
Hypothesis H1 is accepted, indicating that better occupational health and safety practices significantly enhance staff resilience. This finding underscores the importance of prioritizing OHS in fostering a resilient workforce, which is particularly crucial in the demanding environment of healthcare settings in Saudi Arabia. These results align with earlier studies, which highlight the critical role of OHS in building resilient organizations (Allende et al., 2017; Barasa et al., 2018; Brown et al., 2017). Research by Cooke et al. (2019) and Itzhaki et al. (2015) also supports the notion that focusing on health and safety can enhance staff engagement and resilience, leading to better organizational outcomes. Additionally, studies like those by Gopang et al. (2017) and Sull et al. (2015) emphasize that robust OHS measures protect workers and promote a culture of safety and resilience, essential for high-stress environments such as healthcare. This evidence suggests that Saudi Arabian hospitals can benefit significantly from investing in OHS to improve staff and organizational resilience, contributing to better healthcare delivery and patient outcomes.
The acceptance of hypothesis H2 underscores that enhanced staff resilience significantly contributes to greater organizational resilience. This finding highlights the critical importance of fostering staff resilience to strengthen the overall resilience of healthcare organizations, aligning with broader efforts to enhance healthcare quality and stability in Saudi Arabia. These results are consistent with previous research, emphasizing the role of both individual and organizational resilience in maintaining effective operations within healthcare settings (Allende et al., 2017; Barasa et al., 2018; Brown et al., 2017). Specifically, it underscores that resilient staff members can better cope with workplace stressors and challenges, ultimately contributing to the robustness and adaptability of healthcare organizations (Kantur & İşeri-Say, 2012; Kuntz et al., 2016; Wang & Wang, 2023). Furthermore, the role of creative self-efficacy in enhancing resilience and performance, as highlighted by Prayag and Dassanayake (2023), supports the notion that empowering staff through skills development and supportive leadership can significantly bolster organizational resilience. Additionally, the insights from Prayag et al. (2020) on the interplay between psychological resilience, organizational resilience, and life satisfaction further reinforce the importance of a resilient workforce in maintaining high performance and effective operations, particularly in challenging environments.
Hypothesis H3, which posits that occupational health and safety (OHS) positively influences organizational resilience (OR), is strongly supported by the analysis. This underscores the importance of OHS practices in building a resilient healthcare system, which is crucial for improving the quality and stability of healthcare services in Saudi Arabia. The findings align with existing literature on organizational resilience and health and safety practices. For instance, Allende et al. (2017) emphasize the alignment of organizational resilience indicators with health and safety measures as a strategy to mitigate organizational pathologies. Barasa et al. (2018) highlight the nurturing of resilience through robust health policies, while Brown et al. (2017) illustrate the impact of safety measures on the resilience of critical infrastructure providers.
Additionally, studies by Cooke et al. (2019) and Gopang et al. (2017) support the link between high-performance work systems, including OHS, and enhanced resilience and performance. These findings suggest that by investing in OHS, organizations can create a more resilient workforce capable of withstanding and adapting to various challenges. Moreover, the positive influence of OHS on organizational resilience aligns with the broader goals of national health policies in Saudi Arabia, which emphasize the need for robust OHS frameworks to support organizational resilience in the healthcare sector. Consequently, hypothesis H4 is accepted, indicating that effective occupational health and safety measures significantly enhance staff engagement. This finding aligns with the research conducted by Ghoudarzi et al. (2019), which demonstrates a positive relationship between health and safety management and job satisfaction.
Similarly, Gyensare et al. (2019) provide evidence from the SME sector in Ghana, showing that robust occupational health and safety practices are crucial for fostering high levels of employee engagement. Additionally, Cooke et al. (2019) highlight the relationship between high-performance work systems and employee engagement, supporting that a safe and healthy work environment fosters higher engagement levels. The positive impact of OHS on SE in this study also resonates with the insights from Gopang et al. (2017), who find that occupational health and safety measures improve performance in SMEs, indicating the broader applicability of these findings across different organizational contexts. In the Saudi Arabian healthcare context, enhancing OHS practices can lead to a more engaged and resilient workforce, ultimately contributing to better patient care and organizational performance, as suggested by the overarching principles of the Vision 2030 initiative.
Hypothesis H5, which posits that staff engagement (SE) positively influences organizational resilience (OR), is supported by the data analysis. This finding highlights the crucial role of fostering engagement among staff to bolster the resilience of healthcare organizations in Saudi Arabia. Engaged employees are more likely to be proactive, adaptive, and supportive, key attributes for building resilient healthcare institutions capable of withstanding various operational challenges and improving overall healthcare delivery. This conclusion is consistent with existing literature on organizational resilience and engagement. For instance, Allende et al. (2017) emphasize aligning organizational practices with resilience indicators to enhance overall robustness. Barasa et al. (2018) underscore the critical role of nurturing resilience within healthcare settings, while Brown et al. (2017) highlight the importance of employee engagement in fostering resilience in critical infrastructure.
Additionally, research by Cooke et al. (2019) and Kuntz et al. (2016) supports the notion that engaged employees contribute to stronger organizational resilience, enabling organizations to adapt and thrive amidst adversity. Furthermore, Ning and Tantasanee (2023) illustrate the development of strategic plans to strengthen organizational resilience through employee empowerment and engagement, reinforcing the connection between engaged employees and resilient organizations, while Prasongthan (2022) highlights the role of job security and employee engagement in building resilience during crises such as the COVID-19 pandemic. These studies collectively validate the critical link between staff engagement and organizational resilience, emphasizing the need for strategic initiatives to enhance employee engagement within healthcare organizations.
Hypothesis H6 is accepted, demonstrating that staff resilience partially mediates the relationship between occupational health and safety and organizational resilience. This finding highlights the critical role of staff resilience in translating the benefits of occupational health and safety measures into enhanced organizational resilience. In the context of Saudi Arabian hospitals, this emphasizes the need for policies and interventions that improve occupational health and safety and actively build and support staff resilience to foster a more robust and adaptable healthcare system. This aligns with the studies suggesting the importance of resilience and safety culture in enhancing organizational performance and resilience (Allende et al., 2017; Barasa et al., 2018; Brown et al., 2017). Specifically, integrating occupational health and safety measures with strategies to enhance staff resilience is vital for creating resilient healthcare organizations capable of withstanding and adapting to various challenges, as highlighted by the significant positive impacts reported in these studies.
The analysis confirms that staff engagement (SE) mediates the relationship between occupational health and safety (OHS) and staff resilience (SR). This result underscores the importance of fostering an engaging work environment to enhance staff resilience. Improving occupational health and safety measures in Saudi Arabian hospitals can lead to higher staff engagement, boosting resilience among healthcare workers. This finding is consistent with the literature, such as the studies by Barasa et al. (2018) and Kuntz et al. (2016), which emphasize the role of engagement in building organizational resilience. Furthermore, it aligns with the work of Meintjes and Hofmeyr (2018) on the impact of perceived organizational support on employee engagement, indicating that a supportive and safe work environment can enhance staff resilience. This highlights the need for hospital management to focus on safety protocols and engagement strategies to build a more resilient workforce capable of effectively managing workplace challenges and stressors.
The research assessed the serial mediation effect of staff engagement and staff resilience in the relationship between occupational health and safety (OHS) and organizational resilience (OR). This partial mediation underscores that while staff engagement and resilience significantly mediate the impact of OHS on OR, the direct influence of OHS on OR remains substantial. These findings align with the theoretical perspectives highlighted by Allende et al. (2017) and Kantur and İşeri-Say (2012), emphasizing the importance of organizational resilience indicators and frameworks. Barasa et al. (2018) and Brown et al. (2017) further corroborate the critical role of resilience in enhancing organizational outcomes, suggesting that fostering a resilient workforce through robust OHS measures can lead to improved organizational performance. Additionally, the studies by Cooke et al. (2019), Meintjes and Hofmeyr (2018), Sholikhah et al. (2021), and Ojo et al. (2021) highlight the interconnectedness of employee engagement, resilience, and organizational success, reinforcing the importance of these constructs in achieving resilient healthcare environments.
This body of research collectively underscores the pivotal role of OHS in promoting individual and organizational resilience, thereby enhancing overall performance and sustainability within the healthcare sector. These comprehensive insights emphasize the need to integrate OHS practices with strategies that enhance staff engagement and resilience to bolster organizational resilience.
5. Conclusion and Recommendations
This research provides significant insights into the intricate relationships between occupational health and safety (OHS), staff engagement, staff resilience, and organizational resilience (OR) within Saudi Arabian hospitals. The findings demonstrate that OHS exerts a strong direct effect on OR, underscoring the critical importance of robust safety measures in enhancing the resilience of healthcare organizations. Specifically, the results show that 67.1% of the variance in HOR can be attributed to factors related to OHS, indicating a substantial impact. Additionally, staff engagement and staff resilience serve as partial mediators in this relationship, highlighting their pivotal role in converting effective OHS practices into improved organizational outcomes. This partial mediation suggests that while OHS directly enhances organizational resilience, its impact is amplified when staff are engaged and resilient, reinforcing the need for a holistic approach to workplace safety and employee well-being.
The implications of these findings are particularly pertinent in the context of Saudi Arabia’s Vision 2030, which aims to transform the nation’s healthcare system to be more efficient, effective, and resilient. By prioritizing OHS initiatives, hospital administrators and policymakers can foster a safer and more supportive work environment, enhancing staff engagement and resilience. This approach improves organizational resilience and ensures high standards of patient care and better health outcomes. By doing so, Saudi Arabian hospitals can achieve the dual objectives of safeguarding employee well-being and improving organizational resilience, ultimately contributing to the broader goals of Vision 2030.
The healthcare sector in Saudi Arabia faces distinct challenges, including rapid population growth, a high prevalence of chronic diseases, and the continuous need to upgrade healthcare infrastructure and services. Implementing robust occupational safety measures is crucial in addressing these challenges by ensuring that healthcare workers are protected, engaged, and resilient. This, in turn, can lead to better patient outcomes and more efficient healthcare delivery.
Furthermore, fostering a culture of safety and resilience within hospitals aligns with the broader national goals of improving public health, enhancing healthcare efficiency, and maintaining high standards of care throughout the Kingdom. By prioritizing occupational safety and recognizing its positive impacts on staff engagement and resilience, Saudi hospitals can develop a more robust and adaptable healthcare system capable of meeting current and future demands. Several practical recommendations can be made to enhance hospital organizational resilience through improved occupational safety, staff engagement, and staff resilience in alignment with the goals of Vision 2030.
First, implementing comprehensive occupational safety programmes tailored to the specific needs of Saudi healthcare settings is crucial. These programmes should address physical, psychological, and environmental hazards to ensure a safe working environment for all healthcare workers. Regular updates and strict enforcement of safety protocols are essential.
Second, fostering a supportive work environment is vital to enhance staff engagement. This can be achieved through regular feedback, recognition programmes, and professional development opportunities. Communication between staff and management ensures that concerns and suggestions are promptly addressed.
Third, building staff resilience should be prioritized by providing training and resources that help staff develop effective coping strategies and resilience skills. Stress management workshops, resilience training programmes, and access to mental health support are recommended.
Promoting work-life balance through flexible working hours and personal support initiatives is also important. Aligning occupational safety initiatives with the broader Vision 2030 objectives ensures a cohesive approach to improving healthcare quality and resilience. Involving staff in planning and implementing OHS initiatives fosters ownership and accountability. Regular assessments of OHS measures’ effectiveness and their impact on staff engagement and resilience, using data-driven adjustments, are essential for continuous improvement.
Lastly, expanding research to include a broader range of healthcare professionals and exploring the role of organizational culture and external factors will provide deeper insights. By implementing these recommendations, Saudi hospitals can build a more resilient, engaged, and safe workforce, ultimately leading to improved healthcare outcomes and a stronger healthcare system capable of meeting future challenges.
This research has several limitations. The focus on administrative staff means that future research may need to pay more attention to the perspectives of other vital healthcare professionals, such as nurses and doctors, whose resilience and engagement are also crucial for overall hospital resilience. Additionally, the relatively small sample size may limit the generalization of findings across diverse healthcare settings.
Author Contributions
Conceptualization, S.A., A.A.Q methodology, S.A., A.A.Q and Software S.A., validation, S.A., formal analysis S.A., investigation, A.A.Q; resources, data curation, S.A., A.A.Q.; writing—original draft preparation, S.A., A.A.Q and.; writing—review S.A., A.A.Q and editing, S.A., A.A.Q.; visualization. S.A., A.A.Q; supervision, S.A., A.A.Q. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no direct funding for this research.
Data Availability Statement
The results of this study are derived from surveys conducted as part of the research. Due to privacy and ethical considerations, the raw data, which contain potentially identifiable information, have not been made publicly available. However, the authors have prepared aggregated data that exclude any personal or sensitive details and can be shared. Researchers interested in accessing this data can contact the corresponding author with a reasonable request, subject to ethical standards and relevant privacy regulations. The survey instrument and methodology used in this study were carefully designed to ensure comprehensive and accurate insights into the research objectives.
References
- Ahmad, I. A., & Osei, E. (2021). Occupational Health and Safety Measures in Healthcare Settings during COVID-19: Strategies for Protecting Staff, Patients and Visitors. Disaster Medicine and Public Health Preparedness, 1–9. [CrossRef]
- Allende, M. M., Ruiz-Martin, C., Lopez-Paredes, A., & Perez Ríos, J. M. (2017). Aligning Organizational Pathologies and Organizational Resilience Indicators. International Journal of Production Management and Engineering, 5(2), 107. [CrossRef]
- Barasa, E., Mbau, R., & Gilson, L. (2018). What Is Resilience and How Can It Be Nurtured? A Systematic Review of Empirical Literature on Organizational Resilience. International Journal of Health Policy and Management, 7(6), 491–503.
- Brown, C., Seville, E., & Vargo, J. (2017). Measuring the organizational resilience of critical infrastructure providers: A New Zealand case study. International Journal of Critical Infrastructure Protection, 18, 37–49. [CrossRef]
- Connor, K. M., & Davidson, J. R. (2003). Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and anxiety, 18(2), 76–82.
- Cooke, F. L., Cooper, B., Bartram, T., Wang, J., & Mei, H. (2019). Mapping the relationships between high-performance work systems, employee resilience and engagement: A study of the banking industry in China. The International Journal of Human Resource Management, 30(8), 1239–1260.
- Crawford, E. R., LePine, J. A., & Rich, B. L. (2010). Linking job demands and resources to employee engagement and burnout: a theoretical extension and meta-analytic test. Journal of Applied Psychology, 95(5), 834.
- Dwomoh, G., Luguterah, A. W., & Duah, S. B. (2020). Hoteliers’ human resource strategies for business sustainability during Covid-19 pandemic in Ghana. Journal of Business & Retail Management Research, 14(03). [CrossRef]
- Egbuta, O. (2019). Occupational Health and Safety Management and Employee Resilience in Private Universities. Journal of Economics and Sustainable Development, 10(12)(2222-1700). [CrossRef]
- García, J. M., Moreno, L., Jaén Díaz, M., Rubio Valdehita, S., Jesús, C., & García, M. (2007). Relación entre factores psicosociales adversos, evaluados a través del cuestionario multidimensional Decore, y salud laboral deficiente. Psicothema, 19(1), 95–101. https://redined.educacion.gob.es/xmlui/bitstream/handle/11162/4707/01720083000176.pdf?sequence=1.
- Ghoudarzi, H., Vameghi, R., Hosseini Fouladi, S., Khammar, A., Poursadeqiyan, M., & Kavari, S. H. (2019). Relationship between health and safety management status and job.
- Gonçalves, L., Sala, R., & Navarro, J. B. (2022). Resilience and occupational health of health care workers: a moderator analysis of organizational resilience and sociodemographic attributes. International archives of occupational and environmental health, 95(1), 223-232.
- Gonçalves, L., Sala, R., & Navarro, J.-B. (2021). Resilience and occupational health of health care workers: a moderator analysis of organizational resilience and sociodemographic attributes. International Archives of Occupational and Environmental Health. [CrossRef]
- Gopang, M. A., Nebhwani, M., Khatri, A., & Marri, H. B. (2017). An assessment of occupational health and safety measures and performance of SMEs: An empirical investigation. Safety Science, 93, 127–133. [CrossRef]
- Gröschke, D., Hofmann, E., Müller, N. D., & Wolf, J. (2022). Individual and organizational resilience—Insights from healthcare providers in Germany during the COVID-19 pandemic. Frontiers in Psychology, 13, 965380.
- Gyensare, M. A., Anku-Tsede, O., Boakye, K. O., & Twumasi, E. (2019). Occupational health and safety and employee engagement: Evidence from the SMEs sector in Ghana. In Advances in Safety Management and Human Factors: Proceedings of the AHFE 2018 International Conference on Safety Management and Human Factors, July 21-25, 2018, Loews Sapphire Falls Resort at Universal Studios, Orlando, Florida, USA 9 (pp. 202-216). Springer International Publishing.
- Hair, J.F., Hult, G.T.M., Ringle, C.M. and Sarstedt, M. (2017c) A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed., SAGE, Thousand Oaks, CA. [CrossRef]
- Hawkes, A. J., Biggs, A., & Hegerty, E. (2017). Work engagement: Investigating the role of transformational leadership, job resources, and recovery. The Journal of Psychology, 151(6), 509–531.
- Isidro, M. Q. Y., & Calleja, M. T. (2021). How do national values contribute to perceived organizational and employee resilience during disaster? An example from the Philippines. Asian Journal of Social Psychology, 24(4), 511-523.
- Itzhaki, M., Peles-Bortz, A., Kostistky, H., Barnoy, D., Filshtinsky, V., & Bluvstein, I. (2015). Exposure of mental health nurses to violence associated with job stress, life satisfaction, staff resilience, and post-traumatic growth. International Journal of Mental Health Nursing, 24(5), 403–412. [CrossRef]
- Kantur, D., & İşeri-Say, A. (2012). Organizational resilience: A conceptual integrative framework. Journal of Management & Organization, 18(6), 762–773. [CrossRef]
- Kantur, D., & Say, A. I. (2015). Measuring organizational resilience: A scale development. Journal of Business Economics and Finance, 4(3).
- Kuntz, J. R. C., Näswall, K., & Malinen, S. (2016). Resilient Employees in Resilient Organizations: Flourishing Beyond Adversity. Industrial and Organizational Psychology, 9(2), 456–462. doi:10.1017/iop.2016.39.
- Lee, A. V., Vargo, J., & Seville, E. (2013). Developing a Tool to Measure and Compare Organizations’ Resilience. Natural Hazards Review, 14(1), 29–41. [CrossRef]
- Liang, F., & Cao, L. (2021). Linking employee resilience with organizational resilience: The roles of coping mechanism and managerial resilience. Psychology Research and Behavior Management, 1063-1075.
- Makori, E. M., Thuo, J. K., & Wanyama, K. W. (2012). Influence of occupational health and safety programmers on performance of manufacturing firms in Western Province, Kenya.
- Malik, P., & Garg, P. (2020). Learning organization and work engagement: The mediating role of employee resilience. The International Journal of Human Resource Management, 31(8), 1071-1094.
- Mao, Y., Lai, Y., Zhai, Y., Xie, M., Yu, J., Wang, Q., Lu, S., Ma, J., & Bonaiuto, M. (2022). Authentic Leadership and Employee Resilience: A Moderated Mediation Analysis. Frontiers in Psychology, 13, 901085. [CrossRef]
- Meintjes, A., & Hofmeyr, K. (2018). The impact of resilience and perceived organizational support on employee engagement in a competitive sales environment. SA Journal of Human Resource Management, 16(1),1.11. [CrossRef]
- Mohammad, H., Abdinagoro, S. B., Zulkarnain, A., Leonandri, D. G., & Ichsan, M. (2022). The Impact of Organizational Resilience on Hotel Performance during Pandemic Covid-19. Global Business Finance Review, 27(1), 1–15. [CrossRef]
- Ning, K. S., & Tantasanee, S. (2023). Developing A Strategic Plan for Strengthening Organizational Resilience Through Employee Empowerment and Engagement in KMSS-Mandalay. ProQuest, 128–148. [CrossRef]
- Ojo, A. O., Fawehinmi, O., & Yusliza, M. Y. (2021). Examining the predictors of resilience and work engagement during the COVID-19 pandemic. Sustainability, 13(5), 2902.
- Prasongthan, S. (2022). Organizational Resilience and Job Security on Building Employee Engagement During Covid-19 Pandemic of Thai Hotel Industry. ABAC Journal, 42(2), 107–127. [CrossRef]
- Prayag, G., & Dassanayake, D. C. (2023). Tourism employee resilience, organizational resilience and financial performance: the role of creative self-efficacy. Journal of Sustainable Tourism, 31(10), 2312-2336.
- Prayag, G., Muskat, B., & Dassanayake, C. (2024). Leading for resilience: Fostering employee and organizational resilience in tourism firms. Journal of Travel Research, 63(3), 659-680.
- Prayag, G., Spector, S., Orchiston, C., & Chowdhury, M. (2020). Psychological resilience, organizational resilience and life satisfaction in tourism firms: Insights from the Canterbury earthquakes. Current Issues in Tourism, 23(10), 1216–1233.
- Saks, A. M. (2008). The meaning and bleeding of employee engagement: How muddy is the water? Industrial and Organizational Psychology, 1(1), 40–43.
- Sarstedt, M., Ringle, C.M., Henseler, J. and Hair, J.F. (2014a). 'On the emancipation of PLS-SEM: a commentary on Rigdon 2012', Long Range Planning, Vol. 47, No. 3, pp.154–160. [CrossRef]
- satisfaction among employees of rehabilitation centers with crisis management approach in kohgiluyeh and boyer-ahmad province. Health in Emergencies and Disasters Quarterly, 4(4), 193-200.
- Sholikhah, S., Marbun, R. N., & Parimita, W. (2021). The Influence of Learning Organization and Employee Resilience on Work Engagement at Bumn Bank Branch Office in Bogor. IJHCM (International Journal of Human Capital Management), 5(2), 11-25.
- Shrotryia, V. K., & Dhanda, U. (2020). Development of employee engagement measure: experiences from best companies to work for in India. Measuring Business Excellence, 24(3), 319–343.Shuck, B., & Reio, T. G. (2013). Employee Engagement and Well-Being. Journal of Leadership & Organizational Studies, 21(1), 43–58. [CrossRef]
- Sull, A., Harland, N., & Moore, A. (2015). Resilience of healthcare workers in the UK; a cross-sectional survey. Journal of Occupational Medicine and Toxicology, 10(1). [CrossRef]
- Tonkin, K., Malinen, S., Näswall, K., & Kuntz, J. C. (2018). Building employee resilience thrTough well-being in organizations. Human resource development quarterly, 29(2), 107-124.
- Wang, D., & Wang, P. (2023). Effect of employee resilience on organizational resilience in construction projects: considering the role of project tasks. Engineering, Construction and Architectural Management.
- Wang, Z., Li, C., & Li, X. (2017). Resilience, leadership and work engagement: The mediating role of positive affect. Social Indicators Research, 132, 699-708.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).