Submitted:
15 August 2024
Posted:
16 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Measures
2.2.1. Anxiety
2.2.2. Risk/Protective Factors
2.2.3. Demographics, Home Environment, and Personal Finance
2.2.4. Family Configuration, Social Network, and Care-Related Transfers
2.2.5. Health and Functional Limitations
2.2.6. Cognition and Mental Health
2.3. Data Analysis
2.3.1. Random Forest Machine Learning (RFML)
2.3.2. Generalized Linear Regression (GLR)
3. Results
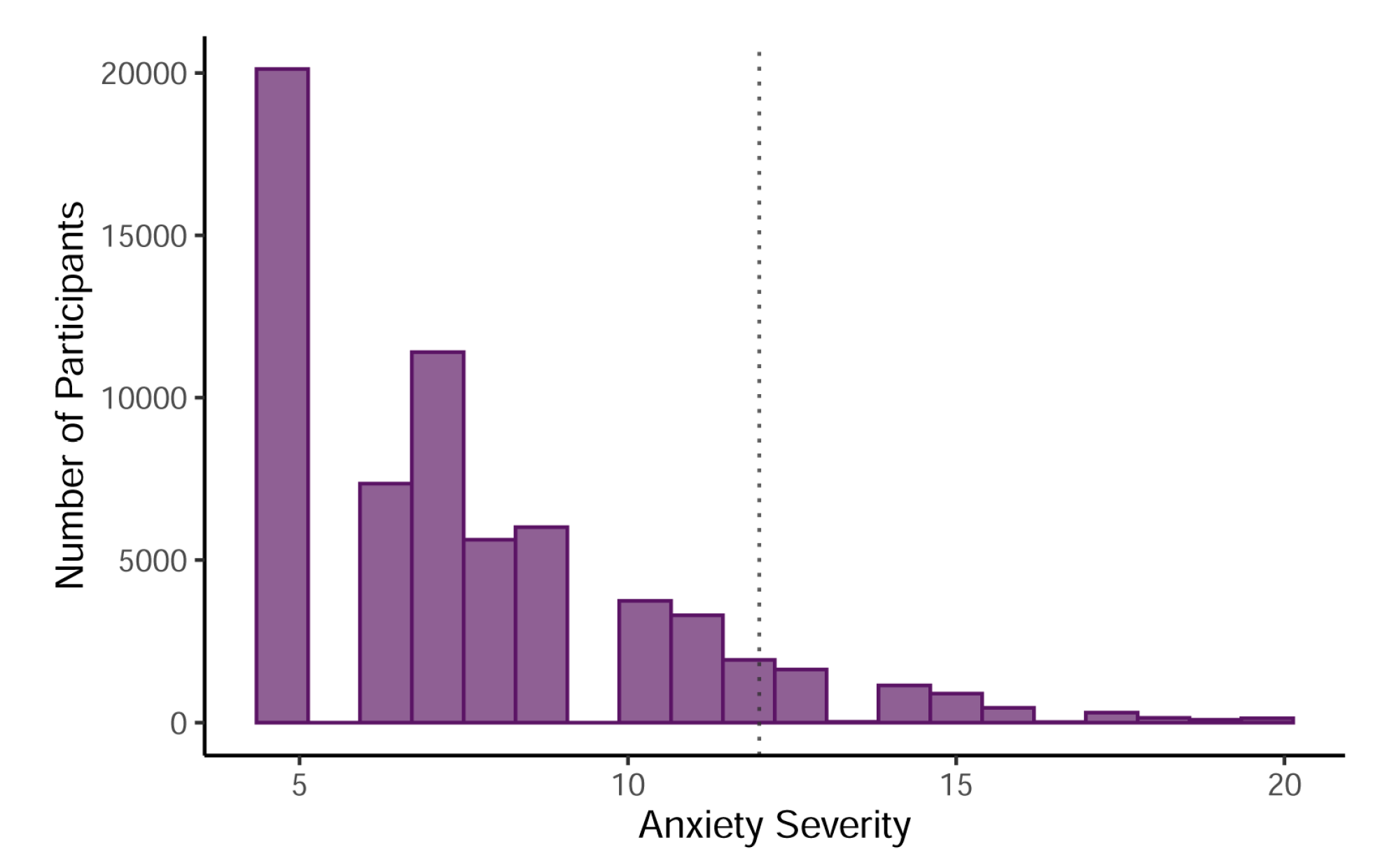
3.1. Summary Statistics
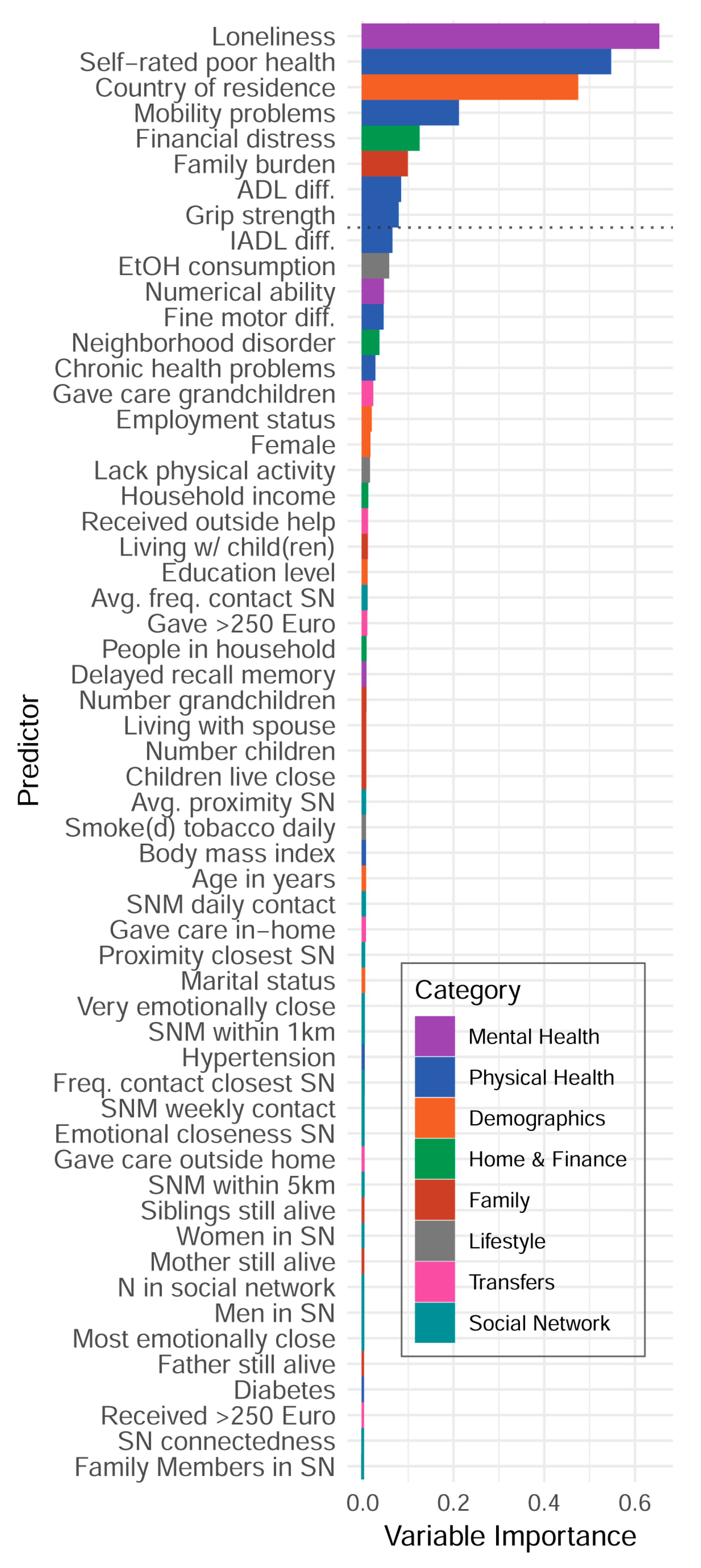
3.2. Random Forest Machine Learning
3.3. Generalized Linear Regression
3.4. Follow-Up Analyses: Predictors of Loneliness
4. Discussion
5. Conclusions
References
- Kessler, R.C.; Angermeyer, M.; Anthony, J. C.; De Graaf, R. O. N.; Demyttenaere, K.; Gasquet, I.; Üstün, T. B.; et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168. [Google Scholar]
- Mental Health of Older Adults. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults (accessed on 24 March 2021).
- Curran, E.; Rosato, M.; Ferry, F.; Leavey, G. Prevalence and factors associated with anxiety and depression in older adults: Gender differences in psychosocial indicators. J. Affect. Disord. 2020, 267, 114–122. [Google Scholar] [CrossRef]
- Volkert, J.; Schulz, H.; Härter, M.; Wlodarczyk, O.; Andreas, S. The prevalence of mental disorders in older people in Western countries—A meta-analysis. Ageing Res. Rev. 2013, 12, 339–353. [Google Scholar] [CrossRef]
- Witlox, M.; Garnefski, N.; Kraaij, V.; Simou, M.; Dusseldorp, E.; Bohlmeijer, E.; Spinhoven, P. Prevalence of Anxiety Disorders and Subthreshold Anxiety Throughout Later Life: Systematic Review and Meta-Analysis. Psychol. Aging 2021, 36, 268–287. [Google Scholar] [CrossRef]
- Lancet Global Health. Mental health matters. The Lancet. Global Health 2020, 8, e1352. [Google Scholar]
- de Beurs, E.; Beekman, A.T.F.; van Balkom, A.J.L.M.; Deeg, D.J.H.; van Dyck, R.; van Tilburg, W. Consequences of anxiety in older persons: its effect on disability, well-being and use of health services. Psychol. Med. 1999, 29, 583–593. [Google Scholar] [CrossRef]
- de Lijster, J.M.; Dierckx, B.; Utens, E.M.; Verhulst, F.C.; Zieldorff, C.; Dieleman, G.C.; Legerstee, J.S. The Age of Onset of Anxiety Disorders. Can. J. Psychiatry 2017, 62, 237–246. [Google Scholar] [CrossRef]
- Santabárbara, J.; Lipnicki, D.M.; Olaya, B.; Villagrasa, B.; Bueno-Notivol, J.; Nuez, L.; López-Antón, R.; Gracia-García, P. Does Anxiety Increase the Risk of all-Cause Dementia? An Updated Meta-Analysis of Prospective Cohort Studies. J. Clin. Med. 2020, 9, 1791. [Google Scholar] [CrossRef]
- Weisberg, R.B. Overview of generalized anxiety disorder: epidemiology, presentation, and course. J Clin Psychiatry 2009, 70, 4–9. [Google Scholar]
- Weisberg, R.B.; Beard, C.; Moitra, E.; Dyck, I.; Keller, M.B. ADEQUACY OF TREATMENT RECEIVED BY PRIMARY CARE PATIENTS WITH ANXIETY DISORDERS. Depression Anxiety 2014, 31, 443–450. [Google Scholar] [CrossRef]
- Vink, D.; Aartsen, M.J.; Schoevers, R.A. Risk factors for anxiety and depression in the elderly: A review. J. Affect. Disord. 2008, 106, 29–44. [Google Scholar] [CrossRef]
- Wolitzky-Taylor, K.B.; Castriotta, N.; Lenze, E.J.; Stanley, M.A.; Craske, M.G. Anxiety disorders in older adults: a comprehensive review. Depression Anxiety 2010, 27, 190–211. [Google Scholar] [CrossRef]
- Cole, M.G.; Dendukuri, N. Risk Factors for Depression Among Elderly Community Subjects: A Systematic Review and Meta-Analysis. Am. J. Psychiatry 2003, 160, 1147–1156. [Google Scholar] [CrossRef]
- Grenier, S.; Payette, M.; Gunther, B.; Askari, S.; Desjardins, F.F.; Raymond, B.; Berbiche, D. Association of age and gender with anxiety disorders in older adults: A systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 2019, 34, 397–407. [Google Scholar] [CrossRef]
- Aichele, S.; Rabbitt, P.; Ghisletta, P. Think Fast, Feel Fine, Live Long. Psychol. Sci. 2016, 27, 518–529. [Google Scholar] [CrossRef]
- Aichele, S.; Rabbitt, P.; Ghisletta, P. Illness and intelligence are comparatively strong predictors of individual differences in depressive symptoms following middle age. Aging Ment. Heal. 2017, 23, 122–131. [Google Scholar] [CrossRef]
- Aschwanden, D.; Aichele, S.; Ghisletta, P.; Terracciano, A.; Kliegel, M.; Sutin, A.R.; Brown, J.; Allemand, M. Predicting Cognitive Impairment and Dementia: A Machine Learning Approach. J. Alzheimer's Dis. 2020, 75, 717–728. [Google Scholar] [CrossRef]
- Choi, K.W.; Stein, M.B.; Nishimi, K.M.; Ge, T.; Coleman, J.R.; Chen, C.-Y.; Ratanatharathorn, A.; Zheutlin, A.B.; Dunn, E.C.; 23andMe Research Team; et al. An Exposure-Wide and Mendelian Randomization Approach to Identifying Modifiable Factors for the Prevention of Depression. Am. J. Psychiatry 2020, 177, 944–954. [Google Scholar] [CrossRef]
- Puterman, E.; Weiss, J.; Hives, B. A.; Gemmill, A.; Karasek, D.; Mendes, W. B.; Rehkopf, D. H. Predicting mortality from 57 economic, behavioral, social, and psychological factors. Proceedings of the National Academy of Sciences 2020, 117(28), 16273–16282. [Google Scholar]
- Handing, E.P.; Strobl, C.; Jiao, Y.; Feliciano, L.; Aichele, S. Predictors of depression among middle-aged and older men and women in Europe: A machine learning approach. Lancet Reg. Heal. - Eur. 2022, 18, 100391. [Google Scholar] [CrossRef]
- Li, Y.; Song, Y.; Sui, J.; Greiner, R.; Li, X.-M.; Greenshaw, A.J.; Liu, Y.S.; Cao, B. Prospective prediction of anxiety onset in the Canadian longitudinal study on aging (CLSA): A machine learning study. J. Affect. Disord. 2024, 357, 148–155. [Google Scholar] [CrossRef]
- Byeon, H. Exploring Factors for Predicting Anxiety Disorders of the Elderly Living Alone in South Korea Using Interpretable Machine Learning: A Population-Based Study. Int. J. Environ. Res. Public Heal. 2021, 18, 7625. [Google Scholar] [CrossRef]
- Beck, A. T., Epstein. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1988, 56, 893. [Google Scholar]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Leuk. Res. 2013, 42, 992–1001. [Google Scholar] [CrossRef]
- SHARE-ERIC. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 5. Release version: 9.0.0. SHARE-ERIC. Data set. 2024. [Google Scholar] [CrossRef]
- Bergmann, M., Kneip. Survey participation in the survey of health, ageing and retirement in Europe (SHARE), Wave 1-6. Munich: Munich Center for the Economics of Aging. 2017. [Google Scholar]
- Bardhoshi, G.; Duncan, K.; Erford, B.T. Psychometric Meta-Analysis of the English Version of the Beck Anxiety Inventory. J. Couns. Dev. 2016, 94, 356–373. [Google Scholar] [CrossRef]
- Chlapecka, A.; Wolfová, K.; Fryčová, B.; Cermakova, P. Educational attainment and anxiety in middle-aged and older Europeans. Sci. Rep. 2023, 13, 1–11. [Google Scholar] [CrossRef]
- Schneider, S.L. The international standard classification of education 2011. In Class and stratification analysis; Emerald Group Publishing Limited, 2013; Volume 30, pp. 365–379. [Google Scholar]
- Litwin, H.; Stoeckel, K.J. Social network, activity participation, and cognition: A complex relationship. Research on Aging 2015, 38, 76–97. [Google Scholar]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.R-project.org/ (accessed on 14 January 2024).
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations inR. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Strobl, C.; Boulesteix, A.-L.; Zeileis, A.; Hothorn, T. Bias in random forest variable importance measures: Illustrations, sources and a solution. BMC Bioinform. 2007, 8, 25–25. [Google Scholar] [CrossRef]
- Strobl, C.; Malley, J.; Tutz, G. An introduction to recursive partitioning: Rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychol. Methods 2009, 14, 323–348. [Google Scholar] [CrossRef]
- Nagelkerke, N. J. A note on a general definition of the coefficient of determination. Biometrika 1991, 78, 691–692. [Google Scholar]
- Domènech-Abella, J.; Mundó, J.; Haro, J.M.; Rubio-Valera, M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2019, 246, 82–88. [Google Scholar] [CrossRef]
- Steen, O.D.; Ori, A.P.S.; Wardenaar, K.J.; van Loo, H.M. Loneliness associates strongly with anxiety and depression during the COVID pandemic, especially in men and younger adults. Sci. Rep. 2022, 12, 1–11. [Google Scholar] [CrossRef]
- Infurna, F.J.; Dey, N.E.Y.; Avilés, T.G.; Grimm, K.J.; Lachman, M.E.; Gerstorf, D. Loneliness in midlife: Historical increases and elevated levels in the United States compared with Europe. Am. Psychol. 2024. [Google Scholar] [CrossRef]
- National Academies of Sciences, Division of Behavioral, Medicine Division, Board on Behavioral, Sensory Sciences, Board on Health Sciences Policy,... & Loneliness in Older Adults. (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. National Academies Press.
- Novak, S. Americans are lonelier than Europeans in middle age. Scientific American. 2024. Available online: https://www.scientificamerican.com/article/americans-are-lonelier-than-europeans-in-middle-age/.
- Eres, R.; Lim, M.H.; Lanham, S.; Jillard, C.; Bates, G. Loneliness and emotion regulation: implications of having social anxiety disorder. Aust. J. Psychol. 2021, 73, 46–56. [Google Scholar] [CrossRef]
- Lim, M.H.; Rodebaugh, T.L.; Zyphur, M.J.; Gleeson, J.F.M. Loneliness over time: The crucial role of social anxiety. J. Abnorm. Psychol. 2016, 125, 620–630. [Google Scholar] [CrossRef]
- Gaeta, L.; Brydges, C.R. Coronavirus-related anxiety, social isolation, and loneliness in older adults in Northern California during the stay-at-home order. In The COVID-19 Pandemic and Older Adults; Routledge, 2022; pp. 21–32. [Google Scholar]
- Ridley, M.; Rao, G.; Schilbach, F.; Patel, V. Poverty, depression, and anxiety: Causal evidence and mechanisms. Science 2020, 370, 1289. [Google Scholar] [CrossRef]
- Beaudreau, S.A.; O'Hara, R. The association of anxiety and depressive symptoms with cognitive performance in community-dwelling older adults. Psychol. Aging 2009, 24, 507–512. [Google Scholar] [CrossRef]
| Demographics (N = 65,684) | Summary Statistic |
|---|---|
| 1. Women | n=36,563 (55.7%) |
| 2. Age in years | Mdn=65.9, Range=(45.0, 103.5) |
| 3. Education level None Primary Lower secondary Upper secondary Post-secondary First stage tertiary Second stage tertiary |
n=3,026 ( 4.6%) n=10,683 (16.3%) n=11,889 (18.1%) n=21,163 (32.2%) n=2,945 (4.5%) n=14,231 (21.7%) n=590 (0.9%) |
| 4. Employment status Retired Employed or self-employed Unemployed Permanently sick /disabled Homemaker |
n=36,590 (55.7%) n=18,023 (27.4%) n=1,868 (2.8%) n=2,313 (3.5%) n=5,244 (8.0%) |
| 5. Marital status Married & living w/spouse Registered partnership Separated Never married Divorced Widowed |
n=44,825 (68.2%) n=964 (1.5%) n=769 (1.2%) n=3,615 (5.5%) n=5,673 (8.6%) n=9,403 (14.3%) |
| 6. Country or residence (15 countries; ns not reported to preserve space) | |
| Home and personal finance | |
| 7. # People in household | Mdn=2.0, IQR=(2.0, 2.0) |
| 8. Household income in Euro (*1k) | Mdn=24,877, IQR=(14.5; 42.4) |
| 9. Financial distress1 | Mdn=2.0, IQR=(1.0, 3.0) |
| 10. Neighborhood disorder | Mdn=3.2, IQR=(3.0, 3.8) |
| Family | |
| 11. Living with partner/spouse | n=48,072 (73.2%) |
| 12. # Children | Mdn=2.0, IQR=(1.0, 3.0) |
| 13. # Grandchildren | Mdn=2.0, IQR=(1.0, 4.0) |
| 14. ≥ 1 child in same household | n=15,915 (24.2%) |
| 15. ≥ 1 child lives < 1km away | n=22,184 (33.8%) |
| 16. Mother still alive | n=14,408 (21.9%) |
| 17. Father still alive | n=5,898 (9%) |
| 18. # siblings still alive | Mdn=2.0, IQR=(1.0, 3.0) |
| 19. Burden of family responsibilities1 | M=1.8, SD=1 |
| Table 1. (cont.’d) | |
| Social network | |
| 20. Size social network | Mdn=2.5, IQR=(1.5, 3.5) |
| 21. # SNM in daily contact | Mdn=1.0, IQR=(1.0, 1.5) |
| 22. # SNM in weekly contact | Mdn=2.0, IQR=(1.0, 3.0) |
| 23. # Family members in SNM | Mdn=2.0, IQR=(1.0, 3.0) |
| 24. # Women in SNM | Mdn=1.0, IQR=(1.0, 2.0) |
| 25. # Men in SNM | Mdn=1.0, IQR=(0.0, 1.5) |
| 26. Avg. proximity of SNM | M=3.2, SD=1.5 |
| 27. Proximity, closest SNM | M=1.9, SD=1.4 |
| 28. # SNM within 1km | M=1.2, SD=0.9 |
| 29. # SNM within 5km | M=1.6, SD=1 |
| 30. Avg. freq. of contact from SNM | M=1.9, SD=0.9 |
| 31. Freq. contact, closest SNM | M=1.3, SD=0.7 |
| 32. Avg. emotional closeness in SNM | M=3.3, SD=0.6 |
| 33. Emotional closeness, closest SNM | M=3.6, SD=0.6 |
| 34. # Very emotionally close SNM | Mdn=2.0, IQR=(1.0, 3.0) |
| 35. Social connectedness | M=2, SD=0.9 |
| Care-related transfers (past year) | |
| 36. Received support >250 Euro | n=3,558 (5.4%) |
| 37. Received outside help | n=12,314 (18.7%) |
| 38. Gave support >250 Euro | n=13,104 (20%) |
| 39. Gave regular care in-home | n=4,425 (6.7%) |
| 40. Gave help outside home | n=12,917 (19.7%) |
| 41. Gave care for grandchildren | n=14,322 (21.8%) |
| Health and functional limitations | |
| 42. # Chronic diseases | M=1.2, SD=1.2 |
| 43. Self-rated poor health | M=3.1, SD=1.1 |
| 44. Hypertension diagnosis | n=25,800 (39.3%) |
| 45. Diabetes diagnosis | n=8,400 (12.8%) |
| 46. Body mass index | M=26.8, SD=4.7 |
| 47. Lack of physical activity | M=2.6, SD=1.3 |
| 48. Ever smoked daily | n=29,661 (45.2%) |
| 49. Alcohol consumption frequency | M=3.4, SD=2.2 |
| 50. Maximum grip strength | M=33.7, SD=11.8 |
| 51–54. Difficulties in: | |
| Activities of daily living (ADL) | M=0.2, SD=0.8 |
| Instrumental activities (IADL) | M=0.1, SD=0.5 |
| Fine motor skills | M=0.2, SD=0.5 |
| Mobility | M=0.5, SD=1.0 |
| Table 1. (cont.’d) | |
| Cognition and mental health | |
| 55. Numerical ability | M=4.1, SD=1.5 |
| 56. Delayed recall memory | M=3.9, SD=2.2 |
| 57. Loneliness | M=1.3, SD=0.4 |
| OC. Anxiety symptoms | M=7.6, SD=2.9 |
| Estimates (unstandardized) |
Estimates (standardized) |
R2Nk | |||||
|---|---|---|---|---|---|---|---|
| Predictor | B | S.E. | B.exp | β | β.exp | stepwise | cumulative |
| (Intercept) | 1.560 | 0.028 | 4.761 | 2.019 | 7.530 | ||
| Loneliness | 0.172 | 0.005 | 1.187 | 0.077 | 1.081 | 0.169 | 0.169 |
| Self-rated poor health | 0.069 | 0.002 | 1.071 | 0.075 | 1.078 | 0.103 | 0.272 |
| Country of residencea | 0.044 | 0.316 | |||||
| Austria | -0.004 | 0.010 | 0.996 | -0.001 | 0.999 | ||
| Sweden | -0.105 | 0.010 | 0.901 | -0.027 | 0.973 | ||
| Netherlands | -0.111 | 0.010 | 0.895 | -0.028 | 0.973 | ||
| Spain | 0.048 | 0.010 | 1.050 | 0.014 | 1.015 | ||
| Italy | -0.033 | 0.010 | 0.967 | -0.009 | 0.992 | ||
| France | -0.038 | 0.010 | 0.963 | -0.010 | 0.991 | ||
| Denmark | -0.068 | 0.011 | 0.935 | -0.016 | 0.984 | ||
| Switzerland | -0.023 | 0.012 | 0.977 | -0.005 | 0.995 | ||
| Belgium | 0.018 | 0.010 | 1.018 | 0.005 | 1.005 | ||
| Israel | 0.050 | 0.013 | 1.052 | 0.010 | 1.010 | ||
| Czech Republic | 0.050 | 0.010 | 1.051 | 0.014 | 1.014 | ||
| Luxembourg | 0.092 | 0.014 | 1.096 | 0.014 | 1.015 | ||
| Slovenia | -0.033 | 0.012 | 0.967 | -0.007 | 0.993 | ||
| Estonia | -0.112 | 0.010 | 0.894 | -0.031 | 0.970 | ||
| Mobility problems | 0.049 | 0.003 | 1.050 | 0.048 | 1.049 | 0.019 | 0.335 |
| Financial distress | 0.036 | 0.002 | 1.037 | 0.036 | 1.036 | 0.010 | 0.345 |
| Family burden | 0.038 | 0.002 | 1.039 | 0.036 | 1.037 | 0.011 | 0.356 |
| Grip strength | -0.003 | 0.000 | 0.997 | -0.037 | 0.963 | 0.009 | 0.364 |
| Biological sex (Female) | -0.003 | 0.006 | 0.997 | -0.001 | 0.999 | 0.000 | 0.364 |
| Age in years | 0.000 | 0.000 | 1.000 | -0.004 | 0.996 | 0.000 | 0.364 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





