Submitted:
19 August 2024
Posted:
20 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
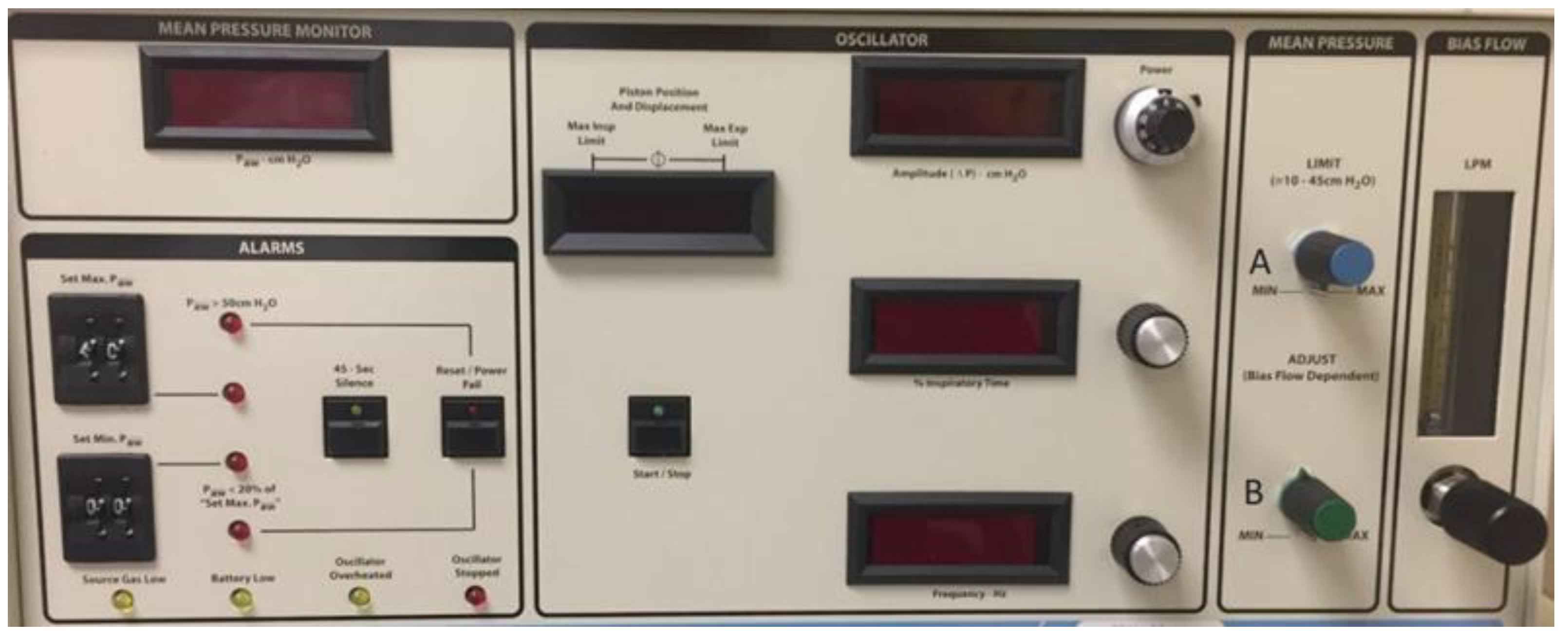
2. HFOV: How It Works
3. Indications and Contraindications
4. Ventilator Settings
5. HFOV in Newborns and Children with Heart Disease
6. Conclusions
7. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Facchin, F.; Fan, E. Airway Pressure Release Ventilation and High-Frequency Oscillatory Ventilation: Potential Strategies to Treat Severe Hypoxemia and Prevent Ventilator-Induced Lung Injury. Respir Care 2015, 60, 1509-1521. [CrossRef]
- Sessler, C.N. Sedation, analgesia, and neuromuscular blockade for high-frequency oscillatory ventilation. Crit Care Med 2005, 33, S209-216. [CrossRef]
- Fessler, H.E.; Hess, D.R. Respiratory controversies in the critical care setting. Does high-frequency ventilation offer benefits over conventional ventilation in adult patients with acute respiratory distress syndrome? Respir Care 2007, 52, 595-605; discussion 606-598.
- Burry, L.D.; Seto, K.; Rose, L.; Lapinsky, S.C.; Mehta, S. Use of sedation and neuromuscular blockers in critically ill adults receiving high-frequency oscillatory ventilation. Ann Pharmacother 2013, 47, 1122-1129. [CrossRef]
- Gupta, P.; Green, J.W.; Tang, X.; Gall, C.M.; Gossett, J.M.; Rice, T.B.; Kacmarek, R.M.; Wetzel, R.C. Comparison of high-frequency oscillatory ventilation and conventional mechanical ventilation in pediatric respiratory failure. JAMA Pediatr 2014, 168, 243-249. [CrossRef]
- Squires, K.A.; De Paoli, A.G.; Williams, C.; Dargaville, P.A. High-frequency oscillatory ventilation with low oscillatory frequency in pulmonary interstitial emphysema. Neonatology 2013, 104, 243-249. [CrossRef]
- Bollen, C.W.; van Well, G.T.; Sherry, T.; Beale, R.J.; Shah, S.; Findlay, G.; Monchi, M.; Chiche, J.D.; Weiler, N.; Uiterwaal, C.S.; et al. High frequency oscillatory ventilation compared with conventional mechanical ventilation in adult respiratory distress syndrome: a randomized controlled trial [ISRCTN24242669]. Crit Care 2005, 9, R430-439. [CrossRef]
- Briggs, S.; Goettler, C.E.; Schenarts, P.J.; Newell, M.A.; Sagraves, S.G.; Bard, M.R.; Toschlog, E.A.; Rotondo, M.F. High-frequency oscillatory ventilation as a rescue therapy for adult trauma patients. Am J Crit Care 2009, 18, 144-148. [CrossRef]
- Mehta, S.; Lapinsky, S.E.; Hallett, D.C.; Merker, D.; Groll, R.J.; Cooper, A.B.; MacDonald, R.J.; Stewart, T.E. Prospective trial of high-frequency oscillation in adults with acute respiratory distress syndrome. Crit Care Med 2001, 29, 1360-1369. [CrossRef]
- Meliones, J.N.; Bove, E.L.; Dekeon, M.K.; Custer, J.R.; Moler, F.W.; Callow, L.R.; Wilton, N.C.; Rosen, D.B. High-frequency jet ventilation improves cardiac function after the Fontan procedure. Circulation 1991, 84, Iii364-368.
- Bojan, M.; Gioanni, S.; Mauriat, P.; Pouard, P. High-frequency oscillatory ventilation and short-term outcome in neonates and infants undergoing cardiac surgery: a propensity score analysis. Crit Care 2011, 15, R259. [CrossRef]
- de Jager, P.; Curley, M.A.Q.; Cheifetz, I.M.; Kneyber, M.C.J. Hemodynamic Effects of a High-Frequency Oscillatory Ventilation Open-Lung Strategy in Critically Ill Children With Acquired or Congenital Cardiac Disease. Pediatr Crit Care Med 2023, 24, e272-e281. [CrossRef]
- Zheng, Y.R.; Xie, W.P.; Liu, J.F.; Wu, H.L.; Xu, N.; Huang, S.T.; Cao, H.; Chen, Q. Application of high-frequency oscillation ventilation combined with volume guarantee in infants with acute hypoxic respiratory failure after congenital heart surgery. Pediatr Pulmonol 2021, 56, 2621-2626. [CrossRef]
- Fan, E.; Brodie, D.; Slutsky, A.S. Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment. Jama 2018, 319, 698-710. [CrossRef]
- Pillow, J.J. High-frequency oscillatory ventilation: mechanisms of gas exchange and lung mechanics. Crit Care Med 2005, 33, S135-141. [CrossRef]
- John, J.; Harcourt, E.R.; Davis, P.G.; Tingay, D.G. Dräger VN500's oscillatory performance has a frequency-dependent threshold. J Paediatr Child Health 2014, 50, 27-31. [CrossRef]
- Keszler, M., Pillow, J. J., and Courtney, S. E. Pediatric and Neonatal Mechanical Ventilation.; Springer: New York, 2015.
- Rettig, J.S.; Smallwood, C.D.; Walsh, B.K.; Rimensberger, P.C.; Bachman, T.E.; Bollen, C.W.; Duval, E.L.; Gebistorf, F.; Markhorst, D.G.; Tinnevelt, M.; et al. High-Frequency Oscillatory Ventilation in Pediatric Acute Lung Injury: A Multicenter International Experience. Crit Care Med 2015, 43, 2660-2667. [CrossRef]
- Miller, A.G.; Bartle, R.M.; Feldman, A.; Mallory, P.; Reyes, E.; Scott, B.; Rotta, A.T. A narrative review of advanced ventilator modes in the pediatric intensive care unit. Transl Pediatr 2021, 10, 2700-2719. [CrossRef]
- Miller, A.G.; Bartle, R.M.; Rehder, K.J. High-Frequency Jet Ventilation in Neonatal and Pediatric Subjects: A Narrative Review. Respir Care 2021, 66, 845-856. [CrossRef]
- Slutsky, A.S.; Drazen, F.M.; Ingram, R.H., Jr.; Kamm, R.D.; Shapiro, A.H.; Fredberg, J.J.; Loring, S.H.; Lehr, J. Effective pulmonary ventilation with small-volume oscillations at high frequency. Science 1980, 209, 609-671. [CrossRef]
- Ng, J.; Ferguson, N.D. High-frequency oscillatory ventilation: still a role? Curr Opin Crit Care 2017, 23, 175-179. [CrossRef]
- Aurilia, C.; Ricci, C.; Tana, M.; Tirone, C.; Lio, A.; Gambacorta, A.; Paladini, A.; Vento, G. Management of pneumothorax in hemodynamically stable preterm infants using high frequency oscillatory ventilation: report of five cases. Ital J Pediatr 2017, 43, 114. [CrossRef]
- Jarvis S, B.M., English W. High frequency oscillatory ventilation. Anaesthesia Tutorial of the Week. 2012, 261: 261–211.
- Clark, R.H.; Gerstmann, D.R.; Null, D.M., Jr.; deLemos, R.A. Prospective randomized comparison of high-frequency oscillatory and conventional ventilation in respiratory distress syndrome. Pediatrics 1992, 89, 5-12.
- Derdak, S.; Mehta, S.; Stewart, T.E.; Smith, T.; Rogers, M.; Buchman, T.G.; Carlin, B.; Lowson, S.; Granton, J. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med 2002, 166, 801-808. [CrossRef]
- Vincent, J.L. High-Frequency Oscillation in Acute Respiratory Distress Syndrome. The End of the Story? Am J Respir Crit Care Med 2017, 196, 670-671. [CrossRef]
- Imai, Y.; Nakagawa, S.; Ito, Y.; Kawano, T.; Slutsky, A.S.; Miyasaka, K. Comparison of lung protection strategies using conventional and high-frequency oscillatory ventilation. J Appl Physiol (1985) 2001, 91, 1836-1844. [CrossRef]
- Johnson, A.H.; Peacock, J.L.; Greenough, A.; Marlow, N.; Limb, E.S.; Marston, L.; Calvert, S.A. High-frequency oscillatory ventilation for the prevention of chronic lung disease of prematurity. N Engl J Med 2002, 347, 633-642. [CrossRef]
- AARC Clinical Practice Guidelines. Endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. Respir Care 2010, 55, 758-764.
- Ferguson, N.D.; Chiche, J.D.; Kacmarek, R.M.; Hallett, D.C.; Mehta, S.; Findlay, G.P.; Granton, J.T.; Slutsky, A.S.; Stewart, T.E. Combining high-frequency oscillatory ventilation and recruitment maneuvers in adults with early acute respiratory distress syndrome: the Treatment with Oscillation and an Open Lung Strategy (TOOLS) Trial pilot study. Crit Care Med 2005, 33, 479-486. [CrossRef]
- Stawicki, S.P.; Goyal, M.; Sarani, B. High-frequency oscillatory ventilation (HFOV) and airway pressure release ventilation (APRV): a practical guide. J Intensive Care Med 2009, 24, 215-229. [CrossRef]
- de Jager, P.; Kamp, T.; Dijkstra, S.K.; Burgerhof, J.G.M.; Markhorst, D.G.; Curley, M.A.Q.; Cheifetz, I.M.; Kneyber, M.C.J. Feasibility of an alternative, physiologic, individualized open-lung approach to high-frequency oscillatory ventilation in children. Ann Intensive Care 2019, 9, 9. [CrossRef]
- Sahin, O.; Colak, D.; Tasar, S.; Yavanoglu Atay, F.; Guran, O.; Mungan Akin, I. Point-of-Care Ultrasound versus Chest X-Ray for Determining Lung Expansion Based on Rib Count in High-Frequency Oscillatory Ventilation. Neonatology 2023, 120, 736-740. [CrossRef]
- Mehta, S.; Granton, J.; MacDonald, R.J.; Bowman, D.; Matte-Martyn, A.; Bachman, T.; Smith, T.; Stewart, T.E. High-frequency oscillatory ventilation in adults: the Toronto experience. Chest 2004, 126, 518-527. [CrossRef]
- Roosens, C.D.; Ama, R.; Leather, H.A.; Segers, P.; Sorbara, C.; Wouters, P.F.; Poelaert, J.I. Hemodynamic effects of different lung-protective ventilation strategies in closed-chest pigs with normal lungs. Crit Care Med 2006, 34, 2990-2996. [CrossRef]
- Li, S.; Wang, X.; Li, S.; Yan, J. High-frequency oscillatory ventilation for cardiac surgery children with severe acute respiratory distress syndrome. Pediatr Cardiol 2013, 34, 1382-1388. [CrossRef]
- Ayoub, D.; Elmashad, A.; Rowisha, M.; Eltomey, M.; El Amrousy, D. Hemodynamic effects of high-frequency oscillatory ventilation in preterm neonates with respiratory distress syndrome. Pediatr Pulmonol 2021, 56, 424-432. [CrossRef]
- Huang, S.T.; Lei, Y.Q.; Xie, W.P.; Zheng, Y.R.; Chen, Q.; Cao, H. Effect of postoperative administration of inhaled nitric oxide combined with high-frequency oscillatory ventilation in infants with acute hypoxemic respiratory failure and pulmonary hypertension after congenital heart surgery: A retrospective cohort study. J Card Surg 2022, 37, 545-551. [CrossRef]
- Zheng, Y.R.; Lin, S.H.; Chen, Y.K.; Cao, H.; Chen, Q. Rescue high-frequency oscillatory ventilation combined with intermittent mandatory ventilation for infants with acute respiratory distress syndrome after congenital heart surgery. Cardiol Young 2023, 33, 1165-1171. [CrossRef]
- Goodman, A.M.; Pollack, M.M. Hemodynamic effects of high-frequency oscillatory ventilation in children. Pediatr Pulmonol 1998, 25, 371-374. [CrossRef]
- Gutiérrez, J.A.; Levin, D.L.; Toro-Figueroa, L.O. Hemodynamic effects of high-frequency oscillatory ventilation in severe pediatric respiratory failure. Intensive Care Med 1995, 21, 505-510. [CrossRef]
- Simma, B.; Fritz, M.; Fink, C.; Hammerer, I. Conventional ventilation versus high-frequency oscillation: hemodynamic effects in newborn babies. Crit Care Med 2000, 28, 227-231. [CrossRef]
- Laubscher, B.; van Melle, G.; Fawer, C.L.; Sekarski, N.; Calame, A. Haemodynamic changes during high frequency oscillation for respiratory distress syndrome. Arch Dis Child Fetal Neonatal Ed 1996, 74, F172-176. [CrossRef]
- Fort, P.; Farmer, C.; Westerman, J.; Johannigman, J.; Beninati, W.; Dolan, S.; Derdak, S. High-frequency oscillatory ventilation for adult respiratory distress syndrome--a pilot study. Crit Care Med 1997, 25, 937-947. [CrossRef]
- Kneyber, M.C. High-frequency oscillatory ventilation and pediatric cardiac surgery: yes, we can! Crit Care 2011, 15, 1011. [CrossRef]
- Tripathi, R.S.; Stein, E.J.; Crestanello, J.A.; Papadimos, T.J. High-frequency oscillatory ventilation after cardiac surgery: a treatment for all ages. Crit Care 2012, 16, 405. [CrossRef]
- Kumar, A.; Joshi, A.; Parikh, B.; Tiwari, N.; Ramamurthy, R.H. High-frequency oscillatory ventilation for respiratory failure after congenital heart surgery: a retrospective analysis. Anaesthesiol Intensive Ther 2023, 55, 60-67. [CrossRef]
- Zheng, Y.R.; Chen, Y.K.; Lin, S.H.; Cao, H.; Chen, Q. Effect of High-Frequency Oscillatory Ventilation, Combined With Prone Positioning, in Infants With Acute Respiratory Distress Syndrome After Congenital Heart Surgery: A Prospective Randomized Controlled Trial. J Cardiothorac Vasc Anesth 2022, 36, 3847-3854. [CrossRef]
- Bizzarro, M.; Gross, I. Inhaled nitric oxide for the postoperative management of pulmonary hypertension in infants and children with congenital heart disease. Cochrane Database Syst Rev 2005, Cd005055. [CrossRef]
- Bizzarro, M.; Gross, I.; Barbosa, F.T. Inhaled nitric oxide for the postoperative management of pulmonary hypertension in infants and children with congenital heart disease. Cochrane Database Syst Rev 2014, Cd005055. [CrossRef]

| INDICATIONS | CONTRAINDICATIONS |
|---|---|
| Pulmonary issues | Pulmonary/thoracic complications |
|
|
| Cardiovascular diseases | Cardiovascular contraindications |
|
|
| Possible indications | Other contraindication |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





