1. Introduction
Univentricular heart defects form a complex group of congenital heart diseases (CHD) that, if untreated, pose a significant mortality risk. The staged Fontan procedure, a crucial palliative intervention, has improved the 30-year survival rate to approximately 85%. However, Fontan circulation leads to long-term complications owing to its passive nature. Venous blood is rerouted directly into the pulmonary arteries, bypassing the right ventricle, so there is no subpulmonary pumping mechanism to increase cardiac output during exertion. This results in exercise intolerance and requires higher central venous pressure to maintain blood flow.
These physiological constraints predispose Fontan patients to complications such as muscle wasting (sarcopenia) and bone demineralisation (osteoporosis) owing to reduced physical activity and lack of weight-bearing exercises [
7,
8,
9]. High venous pressure can also impair cerebral circulation, leading to neurological complications [
10]. Moreover, thromboembolic risks from altered blood flow dynamics can threaten neurological integrity [
11].
Elevated central venous pressure also makes Fontan patients prone to life-threatening conditions, such as protein-losing enteropathy and plastic bronchitis. It can cause liver congestion and progression to fibrosis or cirrhosis, affecting the overall metabolism [
5,
12,
13]. Physical limitations and chronic illnesses often lead to psychological issues such as low self-esteem, social isolation, and depression [
8,
9].
Recent studies suggest personalised cardiac rehabilitation (CR) programs can alleviate these complications [
8]. Aerobic and resistance training significantly improves exercise capacity in Fontan patients, boosting cardiorespiratory fitness [
14,
15] and countering muscle wasting and bone demineralisation [
16,
17]. Resistance training of the lower limb muscles may also improve non-pulsatile venous flow, increasing venous return and systemic preload [
18,
19].
CR programs also improve mental health by fostering community support, which mitigates social isolation. Their structured nature provides a safe environment for exercise, alleviating fear of sudden cardiac events [
9,
20].
This study evaluated the impact of a comprehensive CR program on Fontan patients. It hypothesises that a holistic approach will improve physical and psychosocial aspects, contributing to better rehabilitation strategies and long-term care.
2. Materials and Methods
Study design and participants
This prospective study was conducted at the Pediatric Cardiology Department of the Hospital de Santa Marta, ULS S José, Lisbon, Portugal, with ethical approval from the Medical Ethics Committee (CES 1445/2023). The study recruited children and young adults aged 8 to 30 years who had undergone Fontan total cavopulmonary connection (TCPC) palliation for single-ventricle physiology. Participants were enrolled during routine clinic visits at the Congenital Heart Disease clinics and through referrals, ensuring a diverse and representative sample.
Inclusion Criteria:
Ages 8 to 30 years.
Completion of the Fontan TCPC palliation.
Ability to provide informed consent (or consent from guardians of minors).
Ability and willingness to participate in a CR program and undergo repeated cardiopulmonary exercise testing (CPET).
Impaired aerobic capacity (peak VO2 <80% predicted).
Baseline resting oxygen saturation (SpO2) >85%.
Exclusion Criteria:
Recent (within six months) or planned (within 12 months) cardiac interventions, including catheterisation or surgery.
Formal CR program participation in the past 24 months.
Current or recent pregnancy (<90 days) or planned pregnancy within the next 12 months.
Active heart failure, hospitalisation, or significant clinical changes in the past 30 days.
Recent or planned events are likely to affect exercise capacity significantly.
Haemodynamically significant lesions (e.g. aortic stenosis), uncontrolled arrhythmias, or other contraindications.
NYHA Class IV Heart Failure.
Acute illness in the past three months.
Active protein-losing enteropathy (albumin <2.5 mg/dL).
Pacemaker dependency.
Cognitive delay affecting participation.
Patients who met any of the exclusion criteria were ineligible for the study.
The CR program
The CR program involved three one-hour weekly training sessions over at least three months. If patients continued to show improvement after this period, they were kept in the program. The sessions were group-based and supervised by a physiotherapist, rehabilitation nurse, and paediatric cardiologist.
In the first three weeks, sessions were conducted in the hospital to familiarise the patients. Subsequently, patients could continue at home with real-time supervision. Each session began with a 10-20 minute warm-up of light activities and stretching, followed by 20-40 minutes of aerobic and resistance training. Aerobic exercises included treadmill walking, cycling, rowing, or dynamic play, while resistance training involved wall pulleys and hand weights. A 10-minute cooldown concluded each session.
The training was personalised based on baseline heart rate (HR) and perceived exertion, primarily targeting 60% of the HR reserve. Intensity and duration were increased weekly, and HR monitors and diaries assessed each participant's response and perceived exertion.
Educational sessions led by a rehabilitation nurse covered cardiovascular disease causes, treatment, and medication use. The patients also received guidance on stress reduction, nutrition, smoking cessation, and maintaining a healthy lifestyle.
Clinical data collection
The patients’ medical examinations and psychological assessments were performed at baseline and post-intervention. Baseline assessments were performed within two months before CR started, while post-intervention measurements were performed within two weeks after completing the CR program.
All examinations were standard clinical procedures performed using standardised clinical protocols. Physical fitness was assessed using a graded exercise test with an oxygen uptake evaluation. Blood biomarkers were also analysed, focusing on N Terminal-pro Brain natriuretic peptide levels.
Selective Data Presentation Strategy
This study aimed to analyse the effects of CR on Fontan patients by focusing on two key objectives:
Assessing the impact of the CR program on exercise capacity using cardiopulmonary exercise testing (CPET).
Assessing the effect of the CR program on health-related quality of life (HRQOL) using the SF-36 questionnaire.
Cardiopulmonary Exercise Testing
The Bruce protocol, a standardised treadmill exercise test, was used for CPET to measure the participants' maximum effort based on the Borg scale. Respiratory gases and heart rate were continuously monitored to assess key parameters, such as VO2 max, ventilatory anaerobic threshold, heart rate response, and respiratory exchange ratio. These data provide insights into participants' aerobic capacity and cardiovascular efficiency.
Health-Related Quality of Life Assessments
The SF-36 questionnaire was used to evaluate the impact of CR on patients' health-related quality of life (HRQOL) across domains like physical functioning, general health, vitality, social functioning, and mental health [
21]. Semi-structured interviews conducted by a rehabilitation nurse offered a comprehensive assessment of the effects of the CR program on HRQOL, emotional functioning, social participation, health-related behaviours, leisure activities, and disease-specific knowledge.
Statistical Data Analysis
Python (version 3.8) was used for the data analysis and visualisation. Key libraries included Pandas (1.1.3) for data management, NumPy (1.19.2) for computations, SciPy (1.5.2) for statistical tests, and Matplotlib (3.3.2) with Seaborn (0.11.0) for plots. All analyses were performed in a Jupyter Notebook hosted on Google Colab for transparency and replicability.
The Shapiro-Wilk test was used to check data normality, guiding the choice of statistical tests. Paired t-tests were used for normally distributed data, and the Wilcoxon signed-rank test was used for non-normally distributed data. A significance level of p < 0.05 was used for all analyses.
Continuous variables are reported as the mean ± standard deviation. Categorical variables were analysed for frequency distributions to describe the study population and adherence rates. Adherence was calculated as the percentage of attended sessions of the total number prescribed.
3. Results
3.1. Patient Demographics and Baseline Clinical Characteristics
The study involved ten patients who had undergone Fontan TCPC palliation, including six females, with an average age of 15.6 ± 1.7 years. The most common anatomy was hypoplastic left heart syndrome, which was seen in four patients. Other conditions included tricuspid atresia and double-outlet right ventricle (two patients each), while one patient each had an unbalanced atrioventricular canal, pulmonary atresia, and complex congenital anatomy. One patient was diagnosed with heterotaxy syndrome; however, no other genetic or systemic syndromes were identified (
Table 1).
The Fontan TCPC palliation was performed on patients with an average age of 4.8 ± 0.8 years and an average weight of 20.7 ± 2.4 kg. Seven patients underwent extracardiac conduit surgery, and three underwent a lateral tunnel procedure, all with fenestration during surgery. None of the patients had phrenic nerve paresis, leading to diaphragmatic paresis.
Six patients had a right systemic ventricle, and four had a left systemic ventricle. Recent echocardiograms showed nine patients with normal to mildly reduced ventricular function and one with moderately reduced function. Eight patients had no to mild atrioventricular valve regurgitation, while two had moderate regurgitation. None of the patients had mild aortic or neo-aortic regurgitation. Resting saturation averaged 90 ± 3%, dropping to 86 ± 2% at peak exercise.
The mean TCPC pressure at the latest catheterisation was 15.9 ± 1.8 mmHg, although some tests were conducted 2-3 years before starting the CR program. At the start of CR, bosentan was prescribed to three patients, sildenafil to one, and enalapril to four. All patients received anticoagulants and diuretics according to the protocol. Two patients with significant Fontan dysfunction were listed for heart transplantation before CR.
The patients attended an average of 69 exercise sessions (range 25-105). Pre- and post-intervention assessments were spaced by 32.1 ± 7.7 weeks, with an average interval of 11.7 ± 3.4 years between TCPC palliation and the start of CR.
3.2. The Effect of CR in Fontan Patients
3.2.1. Enhancement of Cardiorespiratory Fitness
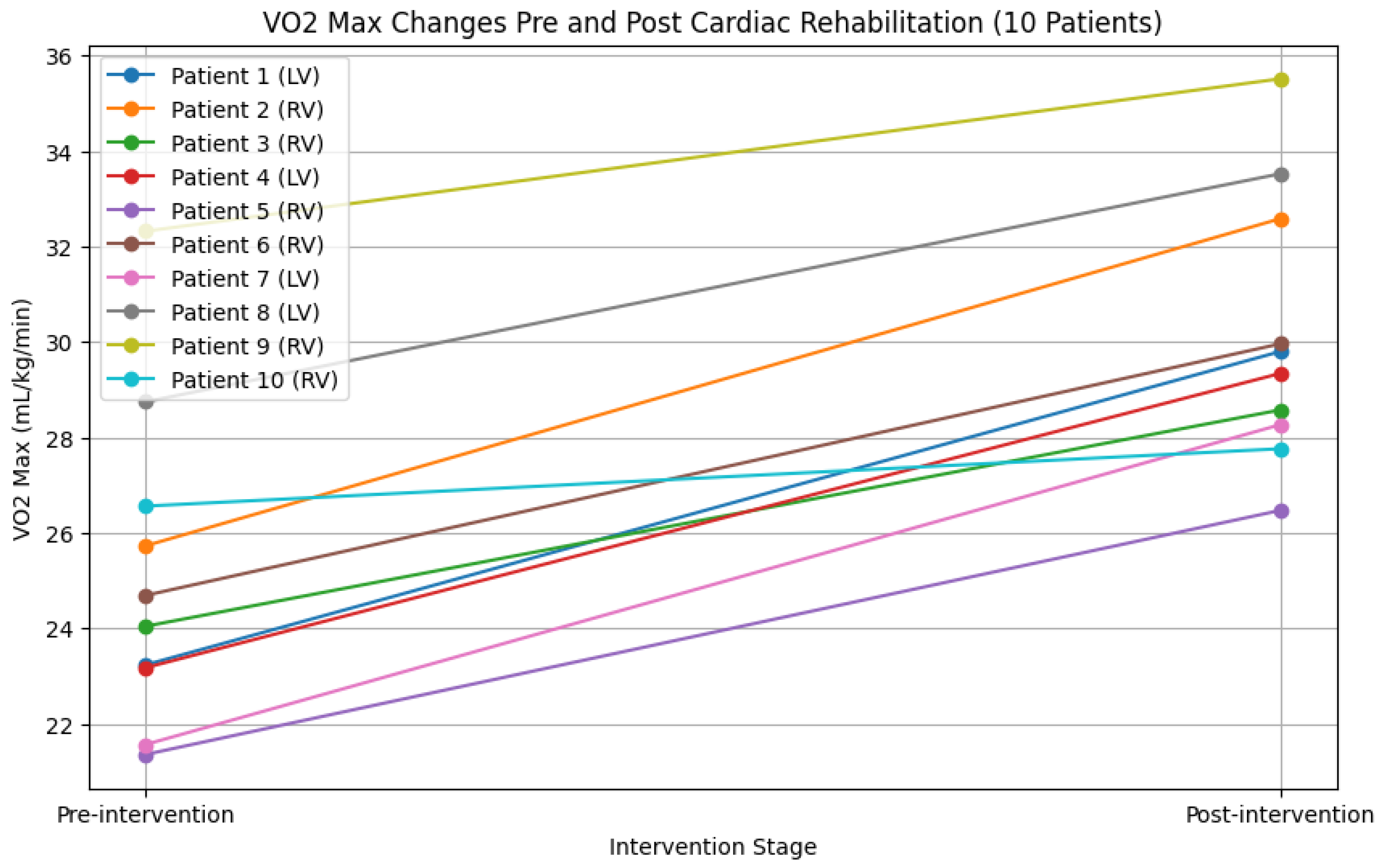
The VO2 max was used to evaluate aerobic capacity, with an initial average of 27.92 ± 5.15 mL/kg/min, which increased to 34.69 ± 1.14 mL/kg/min post-intervention—a significant rise of 6.77 ± 6.35 mL/kg/min (p = 0.0089). Predicted VO2 also showed significant improvement, increasing from 0.67 ± 0.18 to 0.90 ± 0.02 (mean change: 0.23 ± 0.17, p = 0.005). Metabolic efficiency, measured via VCO2, rose from 31.65 ± 6.68 mL/kg/min to 40.33 ± 1.42 mL/kg/min post-CR, but this change of 8.68 ± 8.59 mL/kg/min was not statistically significant (p = 0.05). The results are shown in
Figure 1 and
Table 2.
3.2.2 Haemodynamic Parameters
Peak oxygen saturation levels improved significantly after cardiac rehabilitation, increasing from 86% ± 2 pre-CR to 92% ± 6 post-CR (mean change: 6% ± 7, p = 0.035). Resting oxygen saturation remained unchanged. No significant changes occurred in resting or peak heart rates post-CR. The resting systolic blood pressure increased from 107 ± 5 mmHg to 117 ± 12 mmHg (mean change: 10 ± 13 mmHg, p = 0.102), and the peak systolic pressure increased from 139 ± 6 mmHg to 148 ± 9 mmHg (mean change: 9 ± 11 mmHg, p = 0.067), but the difference was not statistically significant. The results are presented in
Table 3.
3.2.3 Ventilatory Parameters
The tidal volume increased significantly from 1.4±0.7 L to 2.5±0.7 L (p=0.014) post-CR. No significant changes were observed in other ventilatory measures (
Table 4). The maximum respiratory rate increased from 55.3 breaths/min to 63.2 breaths/min without reaching statistical significance (p=0.264). Likewise, the maximum minute ventilation and ventilatory efficiency ratios VE/VO2, VE/VCO2, and respiratory exchange ratio showed no significant changes.
3.2.4 Enhancement of HRQOL
The SF-36 questionnaire showed significant improvements across key areas (p < 0.001) (
Table 5). Physical and social functioning scores increased, similar to the general health perceptions. Vitality scores, which reflect energy and fatigue, also improved substantially. Mental health gains were noted through reduced distress and enhanced well-being.
Semi-structured interviews supported these results, with several patients starting or returning to work. Notably, the two patients awaiting heart transplantation experienced marked improvement, leading to a re-evaluation of their transplant status.
3.3 Adherence and Safety of the CR Program
Patients attended 85-93% of the CR training sessions. No adverse events occurred, and no patients withdrew from the study. Mean NT pro-BNP levels decreased by 14.2 pg/mL after CR (from 192.4 ± 63.6 pg/mL pre-CR to 178.2 ± 5.5 pg/mL post-CR).
4. Discussion
Few studies have examined the effects of CR in patients with Fontan circulation. This study investigated a three-month CR program combining aerobic exercise (AET) and resistance training. Participants included various anatomical subtypes, reflecting the usual heterogeneity in the Fontan population. Sixty per cent of the cohort had a right systemic ventricle (RV).
After CR, significant improvements were observed in aerobic capacity and cardiorespiratory fitness. However, most haemodynamic and ventilatory parameters did not improve significantly, suggesting that CR may help maintain haemodynamic stability.
All five areas of the SF-36 questionnaire showed significant improvement, indicating that CR enhanced the HRQoL of Fontan patients. The CR program proved safe, with no adverse events or dropouts.
The effect of CR on exercise capacity
This study aimed to evaluate the impact of a cardiac rehabilitation (CR) program on the exercise capacity of Fontan patients. Exercise tolerance depends on pulmonary gas exchange, skeletal muscle metabolism, and cardiovascular function; therefore, assessing VO2 max, VCO2, and minute ventilation are crucial to gauge exercise capacity [
22].
VO2 max, the gold standard for evaluating aerobic fitness [
23,
24], showed a significant increase of +6.77 ± 6.35 mL/kg/min, reflecting improved endurance and exertion capacity. Per cent predicted VO2 also rose by 0.23 ± 0.17 (34.3%), reaching a post-CR mean of 0.90 ± 0.02. This 34.3% improvement in oxygen absorption brought participants close to normative levels, as values under 85% were considered abnormal [
25].
VCO2 also increased by +8.68 ± 8.59 mL/kg/min post-CR, though it narrowly missed statistical significance (p = 0.050). This enhanced metabolic response points to improved handling of higher exercise intensities. Apart from tidal volume, ventilatory efficiency also improved, although most measures remained unchanged.
Overall, the remarkable increase in per cent predicted VO2 signifies a substantial improvement in exercise capacity, enabling patients to engage in more varied activities and leading to a healthier lifestyle.
These results are consistent with those in the existing literature. A systematic review involving 264 Fontan patients showed a modest 1.7 mL/kg/min (6%) increase in VO2 max [
8]. However, this study's greater improvement is likely due to a lower baseline VO2 max of 27.92 ± 5.15 mL/kg/min. Similarly, Ali et al. found a significant increase post-CR with a low baseline value [
27]. In contrast, Duppen et al. found no significant improvement with a high baseline VO2 max of 33 mL/kg/min [
28]. Thus, patients with a lower initial VO2 max gain the most from a CR.
While patients with a right systemic ventricle often face worse exercise capacity than those with a left systemic ventricle [
29,
30,
31], 60% of the cohort in this study had a right systemic ventricle. Despite this challenge, the results prove that patients with right systemic ventricles can increase their exercise capacity through rehabilitation and benefit from CR.
The effect of CR on HRQOL
The SF-36 questionnaire and semi-structured interviews revealed a significant improvement in Fontan patients' health-related quality of life (HRQoL) post-CR. The results showed physical, emotional, and psychological health improvements, including better management of chronic fatigue, increased social engagement, and greater self-confidence and independence. Overall, this results in a more positive health outlook. These results align with previous studies that reported improvements in HRQoL post-CR [
15,
28,
32].
However, these studies found that enhanced exercise capacity does not always correlate with an improved HRQoL. Dirks et al. noted better exercise capacity via VO2 max measurements, yet HRQoL remained unchanged [
16]. In contrast, Duppen et al. and Hedlund et al. reported improved HRQoL without significant gains in VO2 max post-CR [
28,
32]. This suggests that, while exercise capacity is important, other aspects of CR also significantly impact the HRQoL of Fontan patients.
Optimisation of CR for Fontan patients
This study's CR program combined AET with resistance training, resulting in improved exercise capacity in Fontan patients. The enhancement came from gains in cardiac and muscular parameters, whereas most ventilatory parameters showed no significant improvement. Pulmonary function is crucial for Fontan patients because pulmonary blood flow is not actively propelled [
5]. Research shows that inspiratory muscle training (IMT) can improve pulmonary function by enhancing the thoracic pump and increasing blood flow, preload, cardiac output, and exercise capacity [
16].
Abdulkarim et al. suggested that combining AET with IMT could improve exercise capacity and pulmonary function in Fontan patients [
13]. However, resistance training also appears promising, as Scheffers et al. found that leg-focused high-weight resistance training significantly improved exercise capacity after 12 weeks [
33]. The optimal combination of training remains debated; however, AET is fundamental, and pairing it with resistance training seems promising. Adding IMT may be valuable for enhancing ventilatory parameters.
The absence of improvement in ventilatory parameters may be due to the short three-month duration of this study. Pulmonary issues such as restrictive lung diseases, plastic bronchitis, and cyanosis are common in 61% of patients with TCPC [
34]; therefore, meaningful improvements may require a longer rehabilitation period.
Safety of CR for Fontan patients
The CR program was evaluated as safe, consistent with the current literature [
8]. However, it should be mentioned that this study did not include patients with a failing Fontan circulation. Therefore, no statements could be made regarding the safety of exercise training for this type of patient.
Study limitations
This study has several limitations. Without a Fontan control group, whether the observed improvements were directly due to the CR program or whether a learning curve influenced assessment performance is unclear. Additionally, the study’s small cohort limited the statistical power, and while the diverse population reflects the heterogeneity of Fontan patients, a larger group is needed for better statistical analysis.
Cardiac function was mainly assessed through echocardiography owing to logistical and clinical constraints, despite cardiac MRI being the gold standard. Although cardiac MRI was used in some cases, differences between the imaging modalities could have led to a conservative estimate of cardiac function.
The CR program lasted at least three months, with participants completing between 25 and 105 sessions. Some patients stayed in the program longer if they showed continued improvement. However, the small cohort size made conducting a sub-analysis of the CR duration difficult. Thus, no conclusion can be drawn regarding the optimal CR duration for Fontan patients.
Future research
Our study was limited by the small sample size and a follow-up period of just three months. Future research should investigate this CR program with a larger cohort and longer follow-up, ideally over at least a year, as the long-term effects of CR in Fontan patients remain unexplored. This study found improved exercise capacity due to improvements in cardiac and muscle parameters. Investigating whether ventilatory parameters improve over a longer period of time would be valuable.
There is no consensus regarding the optimal CR program for Fontan patients. Although some studies suggest that combining AET and IMT is the most effective, this study evaluated AET with resistance training. Further research is needed to identify the most beneficial combination for Fontan patients.
5. Conclusions
This study examined the impact of CR program on exercise capacity and HRQOL in Fontan patients. The results showed improved exercise capacity and HRQOL, even with 60% of the study population having a right systemic ventricle. This underscores the importance of physical conditioning for enhancing the quality of life of patients with Fontan circulation. We recommend that all Fontan patients engage in regular exercise, and further research is needed to optimise CR to reduce morbidity and mortality in this population.
Author Contributions
Conceptualization, Ana Félix and Sérgio Laranjo; Data curation, Luna Ven, Ana Félix and Joana Suarez; Formal analysis, Luna Ven; Methodology, Ana Félix, Jorge Dias and Sérgio Laranjo; Supervision, Fátima Pinto and Sérgio Laranjo; Writing – original draft, Luna Ven and Joana Suarez; Writing – review & editing, Ana Félix, Jorge Dias, Fátima Pinto and Sérgio Laranjo. Luna Van de Ven, Ana Clara Félix and Joana Suarez have contributed equally to this work.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Unidade Local de Saúde São José (Ethics Committee approval number CES 1445/2023)). Ethical approval was obtained prior to the commencement of the study, ensuring that all procedures adhered to the ethical standards set forth in the Declaration.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data supporting the reported results in this study are not publicly available due to privacy and ethical restrictions. The study involved patient medical records, and the data were anonymised to protect patient confidentiality in accordance with institutional guidelines. Access to the data is restricted and may be available from the corresponding author upon reasonable request, subject to approval by the Institutional Review Board and in compliance with applicable data protection regulations.
Acknowledgments
We would like to sincerely thank the patients who participated in this study and their families for their support. We also extend our heartfelt thanks to the dedicated staff at Santa Marta Hospital for their expertise and assistance in implementing the cardiac rehabilitation program. Special appreciation goes to the medical colleagues who referred the participants and contributed to a representative cohort.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kverneland LS, Kramer P, Ovroutski S. Five decades of the Fontan operation: a systematic review of international reports on outcomes after univentricular palliation. Congenital heart disease. 2018, 13, 181–193. [Google Scholar] [CrossRef]
- Schilling C, Dalziel K, Nunn R, Du Plessis K, Shi WY, Celermajer D, et al. The Fontan epidemic: population projections from the Australia and New Zealand Fontan registry. International journal of cardiology. 2016, 219, 14–19. [Google Scholar] [CrossRef]
- Rychik J, Atz AM, Celermajer DS, Deal BJ, Gatzoulis MA, Gewillig MH, et al. Evaluation and management of the child and adult with Fontan circulation: a scientific statement from the American Heart Association. Circulation. 2019, 140, e234–e84. [Google Scholar]
- Downing TE, Allen KY, Glatz AC, Rogers LS, Ravishankar C, Rychik J, et al. Long-term survival after the Fontan operation: twenty years of experience at a single center. The Journal of thoracic and cardiovascular surgery. 2017, 154, 243–253. [Google Scholar] [CrossRef]
- Mazza GA, Gribaudo E, Agnoletti G. The pathophysiology and complications of Fontan circulation. Acta bio-medica : Atenei Parmensis. 2021, 92, e2021260. [Google Scholar]
- Gewillig, M. The fontan circulation. Heart. 2005, 91, 839–846. [Google Scholar] [CrossRef]
- Goldberg DJ, Avitabile CM, McBride MG, Paridon SM. Exercise capacity in the Fontan circulation. Cardiology in the Young. 2013, 23, 824–830. [Google Scholar] [CrossRef]
- Scheffers LE, Berg LEv, Ismailova G, Dulfer K, Takkenberg JJ, Helbing WA. Physical exercise training in patients with a Fontan circulation: a systematic review. European journal of preventive cardiology. 2021, 28, 1269–1278. [Google Scholar] [CrossRef]
- McCrindle BW, Williams RV, Mital S, Clark BJ, Russell JL, Klein G, et al. Physical activity levels in children and adolescents are reduced after the Fontan procedure, independent of exercise capacity, and are associated with lower perceived general health. Archives of disease in childhood. 2007, 92, 509–514. [Google Scholar] [CrossRef]
- Saiki H, Kurishima C, Masutani S, Senzaki H. Cerebral circulation in patients with Fontan circulation: assessment by carotid arterial wave intensity and stiffness. The Annals of thoracic surgery. 2014, 97, 1394–1399. [Google Scholar] [CrossRef]
- Monagle P, Karl TR. Thromboembolic problems after the Fontan operation. Seminars in thoracic and cardiovascular surgery Pediatric cardiac surgery annual. 2002, 5, 36–47. [Google Scholar] [CrossRef]
- Lastinger L, Zaidi AN. The adult with a fontan: a panacea without a cure? Review of long-term complications. Circulation journal : official journal of the Japanese Circulation Society. 2013, 77, 2672–2681. [Google Scholar] [CrossRef]
- Abdulkarim A, Shaji S, Elfituri M, Gunsaulus M, Zafar MA, Zaidi AN, et al. Pulmonary Complications in Patients With Fontan Circulation: JACC Review Topic of the Week. Journal of the American College of Cardiology. 2023, 81, 2434–2444. [Google Scholar] [CrossRef]
- Sutherland N, Jones B, Westcamp Aguero S, Melchiori T, du Plessis K, Konstantinov IE, et al. Home- and hospital-based exercise training programme after Fontan surgery. Cardiol Young. 2018, 28, 1299–1305. [Google Scholar] [CrossRef]
- Turquetto ALR, Dos Santos MR, Agostinho DR, Sayegh ALC, de Souza FR, Amato LP, et al. Aerobic exercise and inspiratory muscle training increase functional capacity in patients with univentricular physiology after Fontan operation: A randomized controlled trial. Int J Cardiol. 2021, 330, 50–58. [Google Scholar] [CrossRef]
- Dirks S, Kramer P, Schleiger A, Speck HM, Wolfarth B, Thouet T, et al. Home-Based Long-Term Physical Endurance and Inspiratory Muscle Training for Children and Adults With Fontan Circulation-Initial Results From a Prospective Study. Frontiers in cardiovascular medicine. 2021, 8, 784648. [Google Scholar]
- Avitabile CM, McBride MG, Zhang X, Ampah S, Goldstein BH, Alsaied T, et al. Peak Work Rate Increases With Lower Extremity-Focused Exercise Training in Adolescents With Fontan Circulation. Journal of the American Heart Association. 2022, 11, e027464. [Google Scholar] [CrossRef]
- Cordina RL, O'Meagher S, Karmali A, Rae CL, Liess C, Kemp GJ, et al. Resistance training improves cardiac output, exercise capacity and tolerance to positive airway pressure in Fontan physiology. International journal of cardiology. 2013, 168, 780–788. [Google Scholar] [CrossRef]
- Cordina R, Celermajer DS, d’Udekem Y. Lower limb exercise generates pulsatile flow into the pulmonary vascular bed in the setting of the Fontan circulation. Cardiology in the Young. 2018, 28, 732–733. [Google Scholar] [CrossRef]
- Longmuir, PE. Importance of Physical Activity and Exercise in Paediatric Fontan Patients. CJC Pediatric and Congenital Heart Disease. 2022. [CrossRef]
- McHorney CA, Ware JE, Jr. , Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical care. 1994, 32, 40–66. [Google Scholar] [CrossRef]
- Piña, IL. Exercise capacity and VO2 in heart failure. UpToDate.
- Shephard RJ, Allen C, Benade AJ, Davies CT, Di Prampero PE, Hedman R, et al. The maximum oxygen intake. An international reference standard of cardiorespiratory fitness. Bulletin of the World Health Organization. 1968, 38, 757–764. [Google Scholar]
- ATS/ACCP Statement on cardiopulmonary exercise testing. American journal of respiratory and critical care medicine. 2003, 167, 211–277. [CrossRef]
- Wasserman K, Whipp BJ. Excercise physiology in health and disease. The American review of respiratory disease. 1975, 112, 219–249. [Google Scholar]
- Myers, J. Applications of cardiopulmonary exercise testing in the management of cardiovascular and pulmonary disease. International journal of sports medicine. 2005, 26, S49–55. [Google Scholar] [CrossRef]
- Ait Ali L, Pingitore A, Piaggi P, Brucini F, Passera M, Marotta M, et al. Respiratory Training Late After Fontan Intervention: Impact on Cardiorespiratory Performance. Pediatric cardiology. 2018, 39, 695–704. [Google Scholar] [CrossRef]
- Duppen N, Etnel JR, Spaans L, Takken T, van den Berg-Emons RJ, Boersma E, et al. Does exercise training improve cardiopulmonary fitness and daily physical activity in children and young adults with corrected tetralogy of Fallot or Fontan circulation? A randomized controlled trial. American heart journal. 2015, 170, 606–614. [Google Scholar] [CrossRef]
- Erikssen G, Aboulhosn J, Lin J, Liestøl K, Estensen ME, Gjesdal O, et al. Survival in patients with univentricular hearts: the impact of right versus left ventricular morphology. Open heart. 2018, 5, e000902. [Google Scholar] [CrossRef]
- Anderson PA, Sleeper LA, Mahony L, Colan SD, Atz AM, Breitbart RE, et al. Contemporary outcomes after the Fontan procedure: a Pediatric Heart Network multicenter study. Journal of the American College of Cardiology. 2008, 52, 85–98. [Google Scholar] [CrossRef]
- d'Udekem Y, Iyengar AJ, Galati JC, Forsdick V, Weintraub RG, Wheaton GR, et al. Redefining expectations of long-term survival after the Fontan procedure: twenty-five years of follow-up from the entire population of Australia and New Zealand. Circulation. 2014, 130, S32–8. [Google Scholar]
- Hedlund ER, Lundell B, Söderström L, Sjöberg G. Can endurance training improve physical capacity and quality of life in young Fontan patients? Cardiol Young. 2018, 28, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Scheffers LE, Helbing WA, Pereira T, Utens E, Dulfer K, Hirsch A, et al. Leg-focused high-weight resistance training improves ventricular stroke volume, exercise capacity and strength in young patients with a Fontan circulation. Eur J Prev Cardiol. 2023.
- Liptzin DR, Di Maria MV, Younoszai A, Narkewicz MR, Kelly SL, Wolfe KR, et al. Pulmonary Screening in Subjects after the Fontan Procedure. The Journal of pediatrics. 2018, 199, 140–143. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).