1. Introduction
The pituitary gland has a transverse diameter of approximately 1 cm and an average weight of 0.6 g, it is divided into an anterior and posterior lobe, where the former comprises 80% of the total mass, and it can undergo dimensional variations in women of childbearing age: despite being one of the smallest organs, pituitary adenomas constitute the second most frequent neoplasm of the central nervous system with 3.47 cases per 100,000 inhabitants each year, but their prevalence in unselected autopsy series reaches up to 25% [
1,
2]. If not recognized, adenomas can grow to considerable size, or continue to modify the patient's endocrine and metabolic profile for a long time; this, together with the risk of visual pathway compression, makes it necessary to reach the diagnosis as early as possible. In fact, despite the often and almost indolent behavior of these tumors, patients affected by pituitary adenomas show higher morbidity and mortality rates than those of the general population [
3]. The prognosis of pituitary adenomas, which has improved in the last two decades, depends on its being functioning or non-functioning. The non-functioning adenomas and prolactinomas have an excellent prognosis if treated promptly with surgery and/or medical therapy [
4]. The treatment of pituitary adenomas includes various options, from medical to surgical and radiotherapy: often the first line of therapy, with the exception of prolactinomas, is represented by surgery, which offers good results in terms of symptomatic and disease control; in particular, the trans-sphenoidal approach has made it possible to intervene on the pituitary gland without affecting the brain structures and show promising results on gross total tumor resection, postoperative pituitary function, visual field changes, length of surgery and hospitalization [
5]. Pituitary adenomas, although considered benign tumors, are associated with reduced quality of life and increased mortality compared to the general population [
6]. Hypopituitarism resulting from pituitary adenomas is due to impaired blood flow or compression to the normal tissue together with interference with the delivery of hypothalamic hormones via the hypothalamus-hypophysial portal system; on the other hand, it is one of the most frequent post operative sequelae, with central adrenal insufficiency being the deficit that requires a timely diagnosis and treatment. Patients with pituitary adenoma should undergo hormonal, clinical, and laboratory evaluation to rule out hyper or hypopituitarism and confounding conditions such as pituitary hyperplasia from primary hypothyroidism [
8].
The aim of this study was to evaluate how the neurosurgical removal of a pituitary adenoma via the trans-sphenoidal approach can modify the patient's hormonal panel and how it influences his overall clinical outcome.
2. Materials and Methods
Consecutive patients undergoing transsphenoidal surgery for functioning radiological diagnosis of pituitary between January 2018 and September 2021 at our Institution were included in this study; among a total of 84 patients, 15 were excluded due to insufficient data at the follow-up resulting in a final series of 69 patients definitively analyzed. Clinical and laboratory data included pre- and post-operative hormonal status, evaluated before surgery and within the following 2 days. Demographics, radiological and histological data as well as post-operative complications, were obtained from the medical records. All patients were operated by pituitary surgeons of the department using neuronavigation-guided endoscopic endonasal technique. The septal mucosa was incised at the level of the sphenoid rostrum, and the mucosa-covered septum was lateralized, thereby sparing the nasoseptal artery. Symptoms were assessed at the beginning of hospitalization and in the immediate post-operative period. Blood chemistry and hormonal assessment were evaluated on the day of hospitalization and within 48 h post-surgery together with the outcome of examinations including imaging and pathology reports; in all cases patients were discharged between 5 and 7 days after surgery. The biochemical and endocrinological parameters were evaluated pre-surgery and within 2 days after the operation. Normal ranges, according to literature, were taken as reference both in the pre- and post-operative evaluation. In addition to glucose and standard electrolytes the following pituitary hormone levels were analyzed: thyroid-stimulating hormone (TSH), luteinizing hormone (LH), follicle-stimulating hormone (FSH), growth hormone (GH) prolactin (PRL), morning cortisol, adrenocorticotropic hormone (ACTH), free thyroxin (T3-T4), testosterone, dehydroepiandrosterone (DHEA) and estradiol. Statistical analysis and data collection were performed using IBM software SPSS statistics version 26. Continuous variables were compared by Student's T test and Chi-square test was conducted for categorical data. P value < 0.05 was considered statistically significant.
3. Results
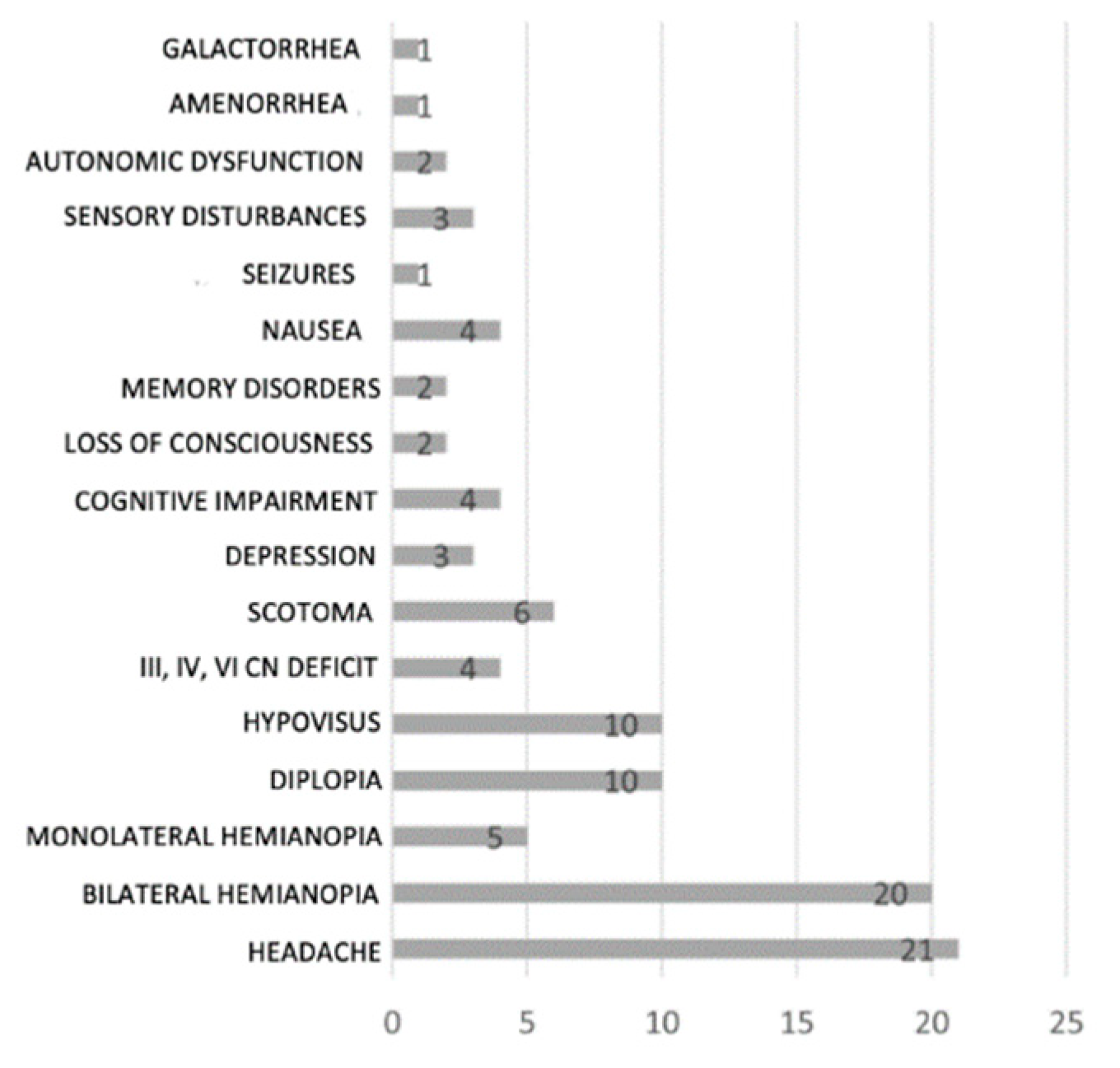
After excluding the 15 patients whose documentation was not available, the analyzed sample of 69 patients is made up of 38 men (55%) and 31 women (45%), with an age at the time of surgery between 15 and 86 years with an average of 55.5 years. 25 patients (36%) were under 50 years old at the time of the operation. At onset, 21 patients (30%) complained of headache and 39 (56%) visual symptoms: bitemporal hemianopia is the most frequently encountered visual deficit (20 patients, 29%), followed by hypovisus and diplopia (complained by 10 patients each, 14%); 6 patients had scotomas on visual field analysis (8%) and 5 had unilateral temporal hemianopia (7%). Cognitive deficits included ideo-motor slowing and behavioral alterations (such as, for example, a case of frontal syndrome). The autonomic disorders complained by 2 patients were erectile dysfunction and incontinence. Sensory disturbances included facial paresthesia, hyposmia, and preauricular pain. Regarding hormonal abnormalities, 2 patients out of 69 had panhypopituitarism at diagnosis, just as 2 patients showed hormonal values compatible with acromegaly; in 23 pts (33%) the onset was with hyperprolactinemia, while only 5 (7%) with hypoprolactinemia. Secondary hypothyroidism was detected in 20 patients (29%), central Addison's disease in 9 (13%), and Cushing's syndrome in 4 (6%). Hypogonadotropic hypogonadism was the most common hormone deficiency, observed in 28 patients (40%) [Tab. 1]. The most frequent histotype is the gonadotroph adenoma, reported in 30 patients (44%), followed by the lactotroph with 16 cases (23%) and the densely granulated somatotroph with 7 cases (10%). Furthermore, 9 corticotroph adenomas (13%) and 7 multihormonal adenomas (10%) were diagnosed. Post-operative complications were documented in 14 patients (20%) who experienced: CSF fistula and Diabetes insipidus 9 patients (13%), 4 patients (5%) developed an infection and hematoma, hypopituitarism occurred in 6 patients (8%). The improvement of hormonal parameters was documented in 31 patients (45%) while in 6 cases (8%) the hormonal values worsened. Visual disturbances showed improvement or total regression in 32 patients (46%); In 5 cases (7%), however, remained stable in 2 patients; after surgery new alterations were detected in 2 patients: the first showed exophoria, diplopia, and visual disturbances in the right eye (all transient conditions), the second developed scotoma bilaterally. Pre-operative headache was resolved in 17 cases out of 19 pts (27.5 %). Only one patient reported new onset of headache after surgery, improved with medical therapy. The results of the statistical analysis describing normalization of the pre-operative hormonal and laboratory parameters are summarized below [Tab. 2]. The correlation between the histotype of the neoplasm and the development of post-surgical hormonal complications was almost significant (p=0.0843, significance p<0.05). Finally, the relationship between patient's age, histological diagnosis and onset symptoms was analyzed [Tab 3.]. The age of the patient was significantly associated with the the histological variant of the tumor: an increased prevalence of lactotroph adenomas in young patients was observed; presence of onset headache and visual disorders were not age-related.
3.2. Tables
Table 1.
Hormonal abnormalities
Table 1.
Hormonal abnormalities
Table 2.
The results of the statistical analysis describing normalization of the pre-operative hormonal and laboratory parameters are summarized below.
Table 2.
The results of the statistical analysis describing normalization of the pre-operative hormonal and laboratory parameters are summarized below.
| PARAMETER |
P |
| GLYCEMIA |
0,001 |
| CREATINEMIA |
0,000 |
| SODIUM |
0,000 |
| POTASSIUM |
0,000 |
| ACTH |
0,014 |
| CORTISOL |
0,150 |
| DHEAS |
0,489 |
| TSH |
0,000 |
| fT3 |
0,000 |
| fT4 |
0,000 |
| GH |
0,331 |
| IGF-1 |
0,078 |
| FSH |
0,000 |
| LH |
0,001 |
| ESTRADIOL |
0,284 |
| TESTOSTERONE |
0,001 |
| PRL |
0,000 |
Table 3.
The relationship between patient's age, histological diagnosis and onset symptoms.
Table 3.
The relationship between patient's age, histological diagnosis and onset symptoms.
| AGE |
P |
| HYSTOTYPE |
0,031 |
| HEADACHE AT ONSET |
0,111 |
| VISUAL DISORDERS AT ONSET |
0,440 |
4. Discussion
Endocrinological normalization after neurosurgical treatment with a trans-sphenoidal approach is solid scientific evidence, well documented in literature: Gentili et al since 2008 demonstrated on a large series of patients that a purely endoscopic approach for pituitary adenoma treatment is a safe and effective alternative to the microscopic procedure, with excellent tumor-removal rates, comparable remission rates in functioning tumors, and a very low rate of complications. Specifically, an increasing number of authors have proven over time good clinical results with various hormones: Dehdashti et al with prolactin, Berker et al with ACTH and Yi LS et al with thyroid hormones, gonadotropins and testosterone [
9,
10,
11]; our study confirm the favorable prognostic rule of the surgical treatment of the pituitary adenoma related with the postoperative normalization of the hormonal values. Finally, Bove et al in a multicenter European study identified, among a series of tips and tricks at different phases of an endoscopic endonasal pituitary surgery, the postoperative endocrinological strict monitoring as a crucial step to perform a successful procedure [
12]. Recently, in accordance with the new nomenclature proposed by the International Pituitary Pathology Club (IPPC) which described adenomas as PitNETs (pituitary neuroendocrine tumors), Ferres et al reiterated the effectiveness of the transsphenoidal approach in normalizing GH and IGF-1 values identifying a prognostic-based approach to guide decision making in high risk patients: in this study, the authors determined that younger age, higher preoperative GH and- or IGF-1 levels, group 2b of the clinicopathological classification, Knosp’s grade IV, MRI T2-weighted tumor hyperintensity, and sparsely granulated cytokeratin expression pattern are related to worse postoperative outcomes in long-term follow-up [
13]. Despite the aforementioned correlation has been verified by previous authors [
13,
14,
15], on the contrary, probably due to the small size of our analyzed sample, in our series the surgical approach was not significant in normalizing the values of GH, IGF-1, estradiol and cortisol. According to Thakur et al, our experience suggests that elderly patients carefully selected for endoscopic adenoma removal can have excellent short-term outcomes including high resection rates, low complication rates and short length of hospital stay. Age, however, was significantly associated with the histological variant of the tumor, confirmed by epidemiological studies; presence of onset headache and visual disorders were not age-related as found in literature [
16,
17]. The presence of headache in pituitary tumor is related to a combination of factors, including intrasellar pressure, tumor extension, relationship with the sellar structures, patient predisposition, familial history, and functional disturbance within the hypothalamo-pituitary axis: in our series 19 patients (27.5 %) complained of pre-operative headache, it resolved in 17 cases; only one patient reported new onset headache after surgery, improved with medical therapy [
18]. Hashem et al reported how the trans-sphenoidal approach can potentially produce electrolyte disturbances: in fact, the values of natremia, kaliemia, creatininemia were altered by the surgical intervention, however we noticed a statistically significant resolution during the post-operative period. Although complication rates are low when performed at high-volume centers, disorders of salt and water balance are relatively common postoperatively in large series reviewed [
20]. We maintain that is appropriate, in agreement with Asa et al, that PitNETs including traditionally defined pituitary adenomas should be managed through a multidisciplinary care team in light of advances in the field of clinical and molecular research: Medina et al highlighted the importance of improving knowledge of the molecular profile of these tumors as a critical aspect for understanding their pathogenesis and identifying potential targets for precision medical therapy [
21]; not least, Robbins et al underlined, through the first study examining technique for IOUS (intraoperative ultrasonography)-guided resection of pituitary adenomas, that the development of new promising surgical techniques is equally critical in order to maximize extent of resection and protect vital structures [
22,
23].
5. Conclusions
In this study, the trans-sphenoidal endoscopic approach was confirmed as an effective treatment for pituitary adenomas with an excellent risk-benefit ratio: patients experienced a low rate of post-operative complications, transient in most cases, and an improvement in the post-operative hormonal and clinical outcome. It should be considered, in our opinion and according to recent literature, as the first therapeutic option in the surgical treatment of pituitary adenomas except for prolactinomas.
Author Contributions
Conceptualization, M.D. and D.A; methodology, A.I.; software, V.L.; validation, L.D.S., M.G.; formal analysis, A.M.; investigation, D.A.; resources, M.I.; data curation, A.I.; writing—original draft preparation, A.M.; writing—review and editing, M.D.; visualization, D.A.; supervision, M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and ethical review and approval were waived for this study by our local ethics committee in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Informed Consent Statement
All participants provided written informed consent for their participation in the study, and patient consent was obtained for the purpose of the study with due care to maintain their privacy.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, [M.D.]
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Pituitary tumours: pituitary incidentalomas. ME, Molitch. 2009, Best Pract Res Clin Endocrinol Metab.
- Møller MW, Andersen MS, Glintborg D, Pedersen CB, Halle B, Kristensen BW, Poulsen FR. Endoscopic vs. microscopic transsphenoidal pituitary surgery: a single centre study. Sci Rep. 2020 Dec 14;10(1):21942. [CrossRef] [PubMed] [PubMed Central]
- Tampourlou M, Fountas A, Ntali G, Karavitaki N. Mortality in patients with non-functioning pituitary adenoma. Pituitary. 2018 Apr;21(2):203-207. [CrossRef] [PubMed] [PubMed Central]
- Russ S, Anastasopoulou C, Shafiq I. Pituitary Adenoma. [Updated 2023 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554451/#.
- Li, A. et al. Endoscopic versus microscopic transsphenoidal surgery in the treatment of pituitary adenoma: a systematic review and meta-analysis. World Neurosurg. 101, 236–246. 2017. [CrossRef]
- AlMalki MH, Ahmad MM, Brema I, et al. Contemporary Management of Clinically Non-functioning Pituitary Adenomas: A Clinical Review. Clinical Medicine Insights: Endocrinology and Diabetes. 2020;13. [CrossRef]
- Prete A, Corsello SM, Salvatori R. Current best practice in the management of patients after pituitary surgery. Ther Adv Endocrinol Metab. 2017 Mar;8(3):33-48. [CrossRef] [PubMed] [PubMed Central]
- Drummond JB, Ribeiro-Oliveira A Jr, Soares BS. Non-Functioning Pituitary Adenomas. 2022 Oct 12. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, New M, Purnell J, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000–. [PubMed]
- Dehdashti AR, Ganna A, Karabatsou K, Gentili F. Pure endoscopic endonasal approach for pituitary adenomas: early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery. 2008 May;62(5):1006-15; discussion 1015-7. [CrossRef] [PubMed]
- Berker M, Işikay I, Berker D, Bayraktar M, Gürlek A. Early promising results for the endoscopic surgical treatment of Cushing's disease. Neurosurg Rev. 2013 Nov 15. [CrossRef] [PubMed]
- Yi LS, Alias A, Ghani ARI, Bidin MBL. Endocrinological Outcome of Endoscopic Transsphenoidal Surgery for Functioning and Non-Functioning Pituitary Adenoma. Malays J Med Sci. 2019 May;26(3):64-71. [CrossRef] [PubMed] [PubMed Central]
- Bove I, Solari D, Bruneau M, Berhouma M, Jouanneau E, Cornelius JF, Messerer M, Daniel RT, Froelich S, Mazzatenta D, Meling T, Paraskevopoulos D, Roche PH, Schoeder HWS, Zazpe I, Visocchi M, Kasper E, Tatagiba M, Cavallo LM. Endoscopic endonasal pituitary surgery: How we do it. Consensus statement on behalf of the EANS skull base section. Brain Spine. 2023 Oct 8;3:102687. [CrossRef] [PubMed] [PubMed Central]
- Ferrés A, Reyes L, Di Somma A, Topczewski T, Mosteiro A, Guizzardi G, De Rosa A, Halperin I, Hanzu F, Mora M, et al. The Prognostic-Based Approach in Growth Hormone-Secreting Pituitary Neuroendocrine Tumors (PitNET): Tertiary Reference Center, Single Senior Surgeon, and Long-Term Follow-Up. Cancers. 2023; 15(1):267. [CrossRef]
- Asa SL, Asioli S, Bozkurt S, Casar-Borota O, Chinezu L, Comunoglu N, Cossu G, Cusimano M, Delgrange E, Earls P, Ezzat S, Gazioglu N, Grossman A, Guaraldi F, Hickman RA, Ikeda H, Jaffrain-Rea ML, Karavitaki N, Kraljević I, La Rosa S, Manojlović-Gačić E, Maartens N, McCutcheon IE, Messerer M, Mete O, Nishioka H, Oz B, Pakbaz S, Pekmezci M, Perry A, Reiniger L, Roncaroli F, Saeger W, Söylemezoğlu F, Tachibana O, Trouillas J, Turchini J, Uccella S, Villa C, Yamada S, Yarman S. Pituitary neuroendocrine tumors (PitNETs): nomenclature evolution, not clinical revolution. Pituitary. 2020 Jun;23(3):322-325. [CrossRef] [PubMed]
- Hazer DB, Işık S, Berker D, Güler S, Gürlek A, Yücel T, Berker M. Treatment of acromegaly by endoscopic transsphenoidal surgery: surgical experience in 214 cases and cure rates according to current consensus criteria. J Neurosurg. 2013 Dec;119(6):1467-77. [CrossRef] [PubMed]
- Thakur JD, Corlin A, Mallari RJ, Huang W, Eisenberg A, Sivakumar W, Krauss H, Griffiths C, Rettinger S, Cohan P, Barkhoudarian G, Araque KA, Kelly D. Pituitary adenomas in older adults (≥ 65 years): 90-day outcomes and readmissions: a 10-year endoscopic endonasal surgical experience. Pituitary. 2021 Feb;24(1):14-26. [CrossRef] [PubMed]
- Yu B, Ji N, Ma Y, Yang B, Kang P, Luo F. Clinical characteristics and risk factors for headache associated with non-functioning pituitary adenomas. Cephalalgia. 2017 Apr;37(4):348-355. [CrossRef] [PubMed]
- Gondim JA, de Almeida JP, de Albuquerque LA, Schops M, Gomes E, Ferraz T. Headache associated with pituitary tumors. J Headache Pain. 2009 Feb;10(1):15-20. [CrossRef] [PubMed] [PubMed Central]
- Hashem R, Weissman C. Renal dysfunction and fluid and electrolyte disturbances. Curr Opin Crit Care. 2011 Aug;17(4):390-5. [CrossRef] [PubMed]
- Brooks EK, Inder WJ. Disorders of Salt and Water Balance After Pituitary Surgery. J Clin Endocrinol Metab. 2022 Dec 17;108(1):198-208. [CrossRef] [PubMed] [PubMed Central]
- Medina EJ, Zohdy YM, Porto E, Revuelta Barbero JM, Bray D, Maldonado J, Rodas A, Mayol M, Morales B, Neill S, Read W, Pradilla G, Ioachimescu A, Garzon-Muvdi T. Therapeutic response to pazopanib: case report and literature review on molecular abnormalities of aggressive prolactinomas. Front Endocrinol (Lausanne). 2023 Jul 17;14:1195792. [CrossRef] [PubMed] [PubMed Central]
- Robbins AC, Winter KA, Smalley ZP, Godil S, Luzardo G, Washington CW, Prevedello DM, Stringer SP, Zachariah M. Side-Firing Intraoperative Ultrasonograhy for Resection of Giant Pituitary Adenomas. World Neurosurg. 2023 May;173:79-87. [CrossRef] [PubMed]
- Iacoangeli M, Nasi D, Colasanti R, Pan B, Re M, Di Rienzo A, di Somma L, Dobran M, Specchia N, Scerrati M. Endoscopic Endonasal Odontoidectomy with Anterior C1 Arch Preservation in Rheumatoid Arthritis: Long-Term Follow-Up and Further Technical Improvement by Anterior Endoscopic C1-C2 Screw Fixation and Fusion. World Neurosurg. 2017 Nov;107:820-829. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).