Submitted:
21 August 2024
Posted:
22 August 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and Methods
Eligibility Criteria
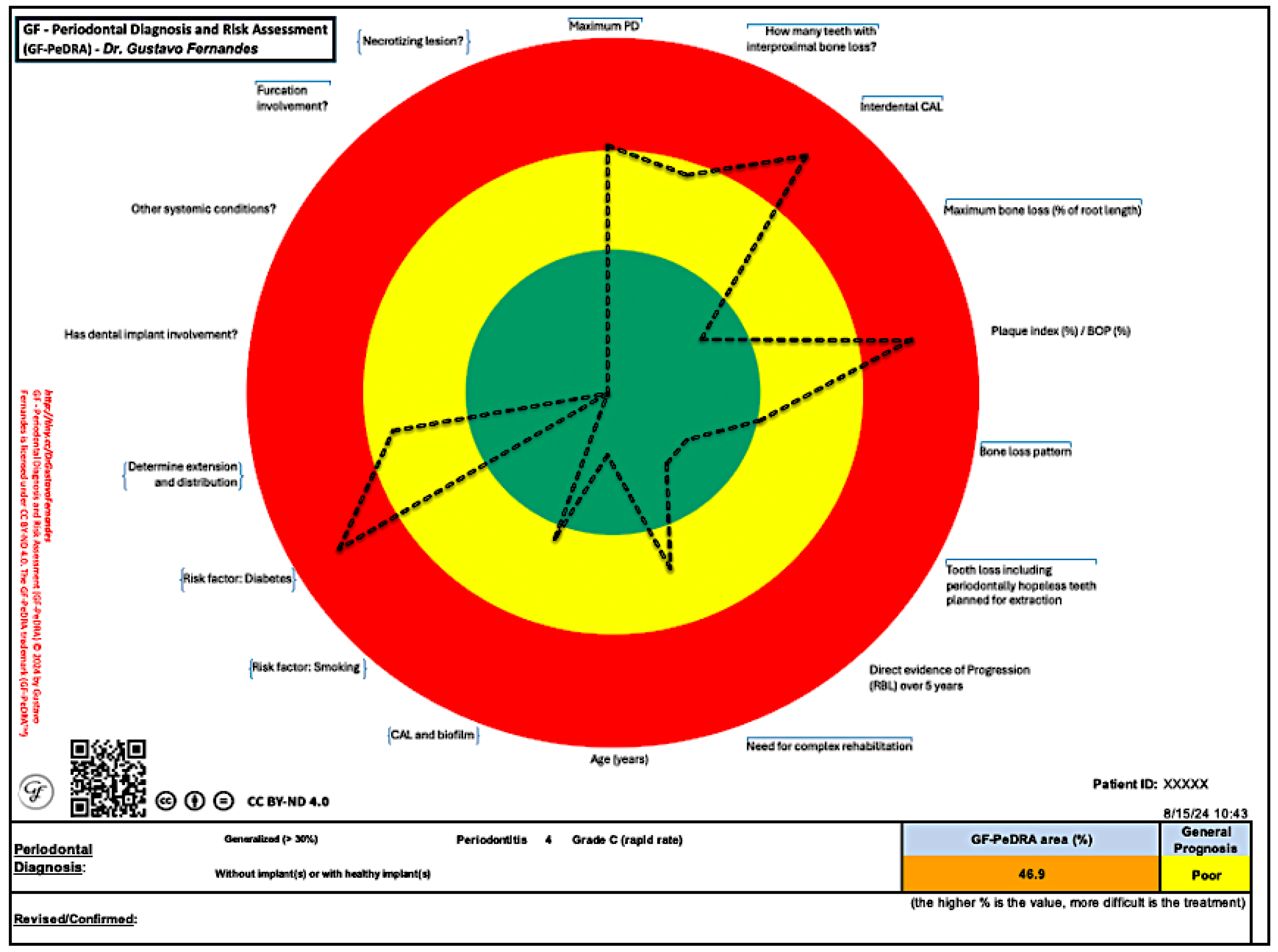
GF-PeDRA© Presentation
Statistical Analysis
RESULTS
Demographic Data
Clinical Data
| Patient | Age | Maximum PD (mm) | How many non-adjacent surfaces with interproximal bone loss? | Interdental CAL (mm) | Maximum RBL (% of root length) (bite-wing) | Bone loss pattern | Tooth loss including periodontally hopeless teeth planned for extraction | Need for complex rehabilitation due to any of the following: | BOP (%) | Has peri-implant disease? | Direct evidence of Progression (RBL) over 5 years | CAL and biofilm | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 44 | 6 | 9 | 5 | 33 | horizontal | None due to Periodontitis | No need | 40 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 2 | 66 | 5 | 12 | 5 | 40 | horizontal | None due to Periodontitis | < 20 remaining teeth; bite colapse | 50 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 3 | 79 | 5 | 5 | 7 | 50 | horizontal | None due to Periodontitis | < 20 remaining teeth | 0 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 4 | 30 | 5 | 0 | 0 | 0 | - | - | no need | 40 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 5 | 20 | 5 | 0 | 0 | 0 | - | - | no need | 100 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 6 | 23 | 4 | 0 | 0 | 0 | - | - | no need | 13 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 7 | 36 | 5 | 0 | 0 | 0 | - | - | no need | 85 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 8 | 37 | 6 | 7 | 7 | 60 | horizontal | Loss up to 4 teeth - periodontitis | bite colapse | 60 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 9 | 75 | 5 | 0 | 2 | 10 | horizontal | - | no need | 15 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 10 | 61 | 4 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 10 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 11 | 58 | 6 | 7 | 8 | 90 | horizontal | Loss of 5 or more teeth - periodontitis | Masticatory disfunction | 23 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 12 | 36 | 6 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 70 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 13 | 44 | 5 | 13 | 2 | 20 | horizontal | None due to Periodontitis | no need | 85 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 14 | 25 | 4 | 0 | 0 | 0 | - | - | no need | 85 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 15 | 43 | 8 | 3 | 6 | 50 | horizontal | No | no need | 15 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 16 | 57 | 5 | 6 | 5 | 30 | horizontal | None due to Periodontitis | no need | 8 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 17 | 20 | 4 | 0 | 0 | 0 | - | no one | no need | 15 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 18 | 18 | 4 | 0 | 0 | 0 | - | no one | no need | 10 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 19 | 47 | 3 | 0 | 0 | 0 | - | no one | no need | 0 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 20 | 70 | 7 | 3 | 6 | 40 | horizontal | None due to Periodontitis | < 20 remaining teeth; masticatory disfunction | 90 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 21 | 78 | 6 | 8 | 8 | 40 | horizontal | None due to Periodontitis | drifting | 40 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 22 | 58 | 5 | 0 | 0 | 0 | - | no one | no need | 20 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 23 | 51 | 6 | 20 | 6 | 40 | horizontal | no one | no need | 20 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 24 | 30 | 6 | 0 | 0 | 0 | - | no one | no need | 90 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 25 | 60 | 7 | 7 | 7 | 50 | horizontal | None due to Periodontitis | < 20 remaining teeth | 15 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 26 | 53 | 14 | 13 | 13 | 70 | horizontal | Loss of 5 or more teeth - periodontitis | bite colapse | 33 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 27 | 31 | 4 | 0 | 0 | 0 | - | no one | no need | 15 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 28 | 69 | 4 | 4 | 1 | 14 | horizontal | None due to Periodontitis | no need | 0 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 29 | 52 | 5 | 0 | 0 | 0 | - | no one | no need | 15 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 30 | 63 | 6 | 5 | 3 | 26 | horizontal | None due to Periodontitis | no need | 92 | no | < 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 31 | 36 | 5 | 3 | 1.5 | 25 | horizontal | no one | no need | 14 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 32 | 58 | 6 | 5 | 3 | 40 | horizontal | no one | no need | 6 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 33 | 37 | 4 | 0 | 0 | 0 | - | None due to Periodontitis | < 20 remaining teeth | 5 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 34 | 37 | 5 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 10 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 35 | 56 | 5 | 10 | 7 | 47 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth | 25 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 36 | 31 | 4 | 0 | 0 | 0 | - | no | no need | 40 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 37 | 42 | 4 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 45 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 38 | 37 | 5 | 17 | 2 | 14 | horizontal | None due to Periodontitis | no need | 20 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 39 | 18 | 4 | 0 | 0 | 0 | - | no | no need | 3 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 40 | 60 | 11 | 11 | 12 | 70 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth; bite colapse | 100 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 41 | 62 | 4 | 0 | 0 | 0 | - | no one | no need | 6 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 42 | 52 | 5 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 5 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 43 | 34 | 5 | 0 | 0 | 0 | - | no | no need | 40 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 44 | 32 | 4 | 0 | 0 | 0 | - | no | no need | 8 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 45 | 28 | 4 | 0 | 0 | 0 | - | no | no need | 33 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 46 | 24 | 3 | 0 | 0 | 0 | - | no | no need | 5 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 47 | 53 | 4 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 33 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 48 | 18 | 2 | 0 | 0 | 0 | - | no | no need | 25 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 49 | 23 | 5 | 0 | 0 | 0 | - | no | no need | 11 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 50 | 67 | 5 | 2 | 8 | 43.5 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth; masticatory disfunction | 0 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 51 | 30 | 4 | 0 | 0 | 0 | - | no | no need | 75 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 52 | 47 | 5 | 4 | 4.5 | 45 | horizontal | None due to Periodontitis | no need | 70 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 53 | 71 | 5 | 13 | 5 | 45 | horizontal | None due to Periodontitis | < 20 remaining teeth | 50 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 54 | 20 | 5 | 0 | 0 | 0 | - | no | no need | 15 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 55 | 46 | 4 | 0 | 0 | 0 | - | no | no need | 0 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 56 | 41 | 6 | 15 | 6 | 65 | vertical | None due to Periodontitis | no need | 14 | no | > 2 mm | Higher disproportionate attachment loss to biofilm levels | ||||||||||
| 57 | 25 | 4 | 0 | 0 | 0 | - | no | no need | 29 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 58 | 57 | 5 | 17 | 6 | 65 | horizontal | None due to Periodontitis | no need | 6 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 59 | 18 | 5 | 0 | 0 | 0 | - | no | no need | 35 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 60 | 21 | 3 | 0 | 0 | 0 | - | no | no need | 43 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 61 | 37 | 7 | 23 | 4 | 43 | horizontal | None due to Periodontitis | no need | 40 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 62 | 50 | 6 | 8 | 6 | 41 | horizontal | None due to Periodontitis | no need | 17 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 63 | 24 | 9 | 27 | 6 | 50 | horizontal | no | no need | 100 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 64 | 18 | 5 | 0 | 0 | 0 | - | no | no need | 24 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 65 | 21 | 4 | 0 | 0 | 0 | - | no | no need | 90 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 66 | 45 | 6 | 2 | 2 | 14 | horizontal | None due to Periodontitis | no need | 80 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 67 | 25 | 7 | 26 | 2 | 30 | horizontal | no | no need | 100 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 68 | 24 | 3 | 0 | 0 | 0 | - | None due to Periodontitis | < 20 remaining teeth | 30 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 69 | 34 | 5 | 7 | 1 | 1 | horizontal | None due to Periodontitis | no need | 35 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 70 | 45 | 8 | 19 | 5 | 49 | horizontal | no | no need | 40 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 71 | 40 | 7 | 25 | 4 | 40 | horizontal | no | no need | 100 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 72 | 52 | 11 | 8 | 8 | 80 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth | 0 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 73 | 45 | 8 | 19 | 5 | 49 | horizontal | no | no need | 40 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 74 | 33 | 4 | 0 | 0 | 0 | - | None due to Periodontitis | no need | 17.6 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 75 | 57 | 5 | 5 | 2 | 20 | horizontal | None due to Periodontitis | < 20 remaining teeth | 50 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 76 | 47 | 5 | 5 | 4 | 20 | horizontal | None due to Periodontitis | no need | 30 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 77 | 63 | 5 | 13 | 2 | 25 | horizontal | no | no need | 22 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 78 | 65 | 5 | 12 | 6 | 50 | horizontal | Loss of 5 or more teeth - periodontitis | Masticatory disfunction | 3 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 79 | 18 | 4 | 0 | 0 | 0 | - | no | no need | 7 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 80 | 36 | 4 | 0 | 0 | 0 | - | None due to Periodontitis | < 20 remaining teeth | 9.7 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 81 | 40 | 4 | 9 | 5 | 25 | horizontal | none due to Periodontitis | bite colapse | 60 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 82 | 33 | 6 | 18 | 6 | 40 | horizontal | none due to Periodontitis | no need | 37 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 83 | 44 | 8 | 6 | 12 | 80 | vertical | Loss up to 4 teeth - periodontitis | < 20 remaining teeth | 21 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 84 | 65 | 5 | 7 | 6 | 30 | horizontal | none due to Periodontitis | < 20 remaining teeth | 8 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 85 | 63 | 6 | 13 | 4 | 8 | horizontal | none due to Periodontitis | no need | 40 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 86 | 23 | 5 | 19 | 2 | 6 | horizontal | no | no need | 31 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 87 | 70 | 6 | 13 | 3 | 10 | horizontal | none due to Periodontitis | no need | 15 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 88 | 30 | 7 | 4 | 4 | 10 | horizontal | none due to Periodontitis | no need | 16 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 89 | 42 | 7 | 14 | 7 | 15 | horizontal | none due to Periodontitis | no need | 39 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 90 | 42 | 11 | 12 | 14 | 52 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse | 100 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 91 | 53 | 6 | 7 | 4 | 40 | horizontal | none due to Periodontitis | drifting | 60 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 92 | 18 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 32 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 93 | 18 | 6 | 0 | 0 | 0 | - | no | no need | 90 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 94 | 42 | 4 | 8 | 0.5 | 5 | vertical | no | no need | 15 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 95 | 75 | 4 | 5 | 5 | 20 | horizontal | none due to Periodontitis | no need | 14 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 96 | 34 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 5 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 97 | 36 | 5 | 7 | 1 | 10 | horizontal | none due to Periodontitis | no need | 15 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 98 | 29 | 4 | 0 | 0 | 0 | - | no | no need | 19 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 99 | 30 | 5 | 2 | 1 | 10 | horizontal | none due to Periodontitis | no need | 26 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 100 | 21 | 4 | 0 | 0 | 0 | - | no | no need | 16 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 101 | 58 | 7 | 5 | 6 | 50 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse | 90 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 102 | 58 | 8 | 13 | 5 | 56 | horizontal | none due to Periodontitis | no need | 60 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 103 | 72 | 4 | 5 | 1 | 10 | horizontal | none due to Periodontitis | < 20 remaining teeth, Bite collapse | 15 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 104 | 40 | 8 | 18 | 9 | 43 | horizontal | none due to Periodontitis | no need | 20 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 105 | 61 | 4 | 6 | 7 | 40 | horizontal | none due to Periodontitis | < 20 remaining teeth, Bite collapse | 23 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 106 | 65 | 4 | 0 | 0 | 0 | - | no | no need | 2 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 107 | 32 | 5 | 19 | 5 | 23 | horizontal | none due to Periodontitis | no need | 19 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 108 | 88 | 4 | 0 | 6 | 30 | horizontal | none due to Periodontitis | < 20 remaining teeth, Bite collapse | 25 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 109 | 78 | 7 | 7 | 6 | 60 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse | 19 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 110 | 62 | 7 | 21 | 5 | 43 | horizontal | none due to Periodontitis | no need | 40 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 111 | 56 | 6 | 12 | 6 | 65 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 17 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 112 | 38 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | drifting | 7.1 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 113 | 61 | 4 | 9 | 6 | 48 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, masticatory disfunction | 0 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 114 | 48 | 6 | 18 | 3 | 20 | horizontal | none due to Periodontitis | no need | 39 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 115 | 35 | 5 | 7 | 2 | 10 | horizontal | none due to Periodontitis | no need | 9 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 116 | 28 | 6 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 80 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 117 | 39 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 27 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 118 | 66 | 5 | 2 | 6 | 50 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, masticatory disfunction | 30 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 119 | 18 | 3 | 0 | 0 | 0 | - | no | no need | 29 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 120 | 68 | 7 | 2 | 5 | 60 | horizontal | Loss of 5 or more teeth - periodontitis | Secondary occlusal trauma (mobility II) | 25 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 121 | 65 | 7 | 18 | 5 | 45 | horizontal | Loss of 5 or more teeth - periodontitis | masticatory disfunction | 1 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 122 | 59 | 4 | 16 | 8 | 75 | horizontal | none due to Periodontitis | no need | 25 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 123 | 73 | 6 | 14 | 5 | 76 | horizontal | none due to Periodontitis | Bite colapse, Drifiting, Flaring | 3 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 124 | 70 | 5 | 16 | 6 | 32 | horizontal | Loss of 5 or more teeth - periodontitis | Bite colapse, Drifiting, Flaring | 30 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 125 | 76 | 4 | 3 | 2 | 25 | horizontal | none due to Periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 13 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 126 | 29 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 2 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 127 | 31 | 5 | 0 | 0 | 0 | - | no | no need | 15 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 128 | 28 | 7 | 6 | 4 | 40 | horizontal | no | no need | 100 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 129 | 50 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 7 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 130 | 68 | 5 | 3 | 5 | 33 | horizontal | Loss of up to 4 teeth - periodontitis | < 20 remaining teeth | 15 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 131 | 51 | 6 | 19 | 5 | 32.3 | horizontal | none due to Periodontitis | no need | 15 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 132 | 41 | 5 | 5 | 2 | 20 | horizontal | no | no need | 34 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 133 | 24 | 6 | 13 | 3 | 28 | horizontal | none due to Periodontitis | no need | 61 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 134 | 62 | 3 | 0 | 0 | 0 | - | none due to Periodontitis | < 20 remaining teeth | 0 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 135 | 47 | 5 | 22 | 7 | 28 | horizontal | none due to Periodontitis | no need | 24 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 136 | 50 | 3 | 3 | 1 | 10 | horizontal | none due to Periodontitis | < 20 remaining teeth | 7 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 137 | 72 | 6 | 18 | 10 | 37 | horizontal | none due to Periodontitis | < 20 remaining teeth | 1 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 138 | 77 | 6 | 1 | 6 | 35 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction, Secondary occlusal trauma | 2 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 139 | 59 | 6 | 18 | 5 | 37 | horizontal | none due to Periodontitis | no need | 35 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 140 | 18 | 4 | 0 | 0 | 0 | - | no one | no need | 0 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 141 | 54 | 5 | 7 | 3 | 33 | horizontal | none due to Periodontitis | no need | 2 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 142 | 64 | 4 | 12 | 6 | 40 | horizontal | none due to Periodontitis | no need | 21 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 143 | 42 | 5 | 5 | 2 | 4 | horizontal | none due to Periodontitis | < 20 remaining teeth | 67 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 144 | 75 | 6 | 12 | 11 | 46 | horizontal | none due to Periodontitis | no need | 88 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 145 | 64 | 5 | 4 | 1 | 24 | horizontal | none due to Periodontitis | no need | 83 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 146 | 28 | 6 | 0 | 0 | 0 | - | no one | no need | 18 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 147 | 31 | 5 | 0 | 0 | 0 | - | no one | no need | 2 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 148 | 29 | 7 | 16 | 4 | 32 | horizontal | none due to Periodontitis | no need | 7 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 149 | 30 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 28 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 150 | 19 | 3 | 0 | 0 | 0 | - | no one | no need | 11 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 151 | 39 | 6 | 5 | 2 | 14 | horizontal | none due to Periodontitis | no need | 8 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 152 | 76 | 4 | 2 | 1 | 33 | horizontal | none due to Periodontitis | no need | 8 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 153 | 45 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 10 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 154 | 56 | 4 | 7 | 1 | 10 | horizontal | none due to Periodontitis | < 20 remaining teeth | 29 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 155 | 58 | 6 | 5 | 6 | 37 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 45 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 156 | 34 | 4 | 0 | 0 | 0 | - | no one | no need | 13 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 157 | 77 | 6 | 3 | 5 | 40 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse | 21 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 158 | 71 | 4 | 4 | 6 | 43 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth | 21 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 159 | 64 | 7 | 5 | 4 | 38 | horizontal | none due to Periodontitis | no need | 6 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 160 | 67 | 5 | 11 | 6 | 35 | horizontal | none due to Periodontitis | < 20 remaining teeth | 14 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 161 | 71 | 5 | 11 | 7 | 40 | horizontal | none due to Periodontitis | < 20 remaining teeth | 23 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 162 | 48 | 4 | 0 | 0 | 0 | - | no one | no need | 16 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 163 | 29 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 43 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 164 | 26 | 6 | 0 | 0 | 0 | - | no one | no need | 31 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 165 | 69 | 5 | 8 | 2 | 30 | horizontal | none due to Periodontitis | no need | 16 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 166 | 32 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 4 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 167 | 30 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 4 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 168 | 74 | 7 | 8 | 7 | 70 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 17 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 169 | 32 | 5 | - | 6 | - | horizontal | none due to Periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction, Secondary occlusal trauma | 67 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 170 | 74 | 4 | 4 | 5 | 50 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, masticatory disfunction | 5 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 171 | 60 | 7 | 7 | 10 | 63 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth | 100 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 172 | 32 | 4 | 6 | 2 | 23 | horizontal | none due to Periodontitis | < 20 remaining teeth | 52 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 173 | 34 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 41 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 174 | 56 | 5 | 7 | 7 | 35 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth | 19 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 175 | 18 | 6 | 0 | 0 | 0 | - | no one | no need | 67 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 176 | 52 | 5 | 2 | 5 | 20 | horizontal | none due to Periodontitis | < 20 remaining teeth | 8 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 177 | 61 | 5 | 5 | 1 | 10 | horizontal | none due to Periodontitis | no need | 5 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 178 | 54 | 7 | 23 | 7 | 15 | horizontal | none due to Periodontitis | no need | 43 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 179 | 48 | 4 | 16 | 6 | 22 | horizontal | none due to Periodontitis | no need | 20 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 180 | 45 | 6 | 6 | 6 | 33 | horizontal | none due to Periodontitis | Bite colapse, Drifiting, Flaring | 5 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 181 | 46 | 4 | 0 | 0 | 0 | - | no one | no need | 15 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 182 | 27 | 5 | 0 | 0 | 0 | - | no one | no need | 65 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 183 | 48 | 5 | 0 | 0 | 0 | - | no one | no need | 3 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 184 | 78 | 4 | 5 | 4 | 10 | horizontal | none due to Periodontitis | no need | 3 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 185 | 21 | 5 | 0 | 0 | 0 | - | no one | no need | 19.7 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 186 | 61 | 5 | 13 | 5 | 4 | horizontal | none due to Periodontitis | no need | 13 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 187 | 93 | 7 | 10 | 8 | 17 | horizontal | Loss of up to 4 teeth - periodontitis | no need | 9.5 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 188 | 33 | 5 | 0 | 0 | 0 | - | no one | no need | 3 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 189 | 43 | 5 | 2 | 1 | 3 | horizontal | none due to Periodontitis | no need | 49 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 190 | 62 | 4 | 0 | 0 | 0 | - | none due to Periodontitis | < 20 remaining teeth | 4 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 191 | 43 | 6 | 3 | 6 | 10 | horizontal | none due to Periodontitis | no need | 66 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 192 | 69 | 7 | 20 | 9 | 30 | horizontal | none due to Periodontitis | no need | 33 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 193 | 25 | 4 | 0 | 0 | 0 | - | no one | no need | 8 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 194 | 26 | 5 | 0 | 0 | 0 | - | none due to Periodontitis | no need | 52 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 195 | 71 | 5 | 0 | 1 | 10 | horizontal | none due to Periodontitis | masticatory disfunction | 0 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 196 | 50 | 7 | 13 | 7 | 24 | horizontal | none due to Periodontitis | no need | 13 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 197 | 18 | 4 | 0 | 0 | 0 | - | no one | no need | 0 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 198 | 63 | 7 | 21 | 8 | 33 | horizontal | none due to Periodontitis | no need | 19 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 199 | 46 | 6 | 14 | 8 | 54 | horizontal | none due to Periodontitis | Bite collapse, masticatory disfunction | 2 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 200 | 49 | 6 | 14 | 5 | 10 | horizontal | none due to Periodontitis | no need | 2 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 201 | 76 | 5 | 6 | 2 | 18 | horizontal | none due to Periodontitis | Bite colapse, Drifiting, Flaring | 4 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 202 | 42 | 5 | 0 | 0 | 0 | - | Loss of up to 4 teeth - periodontitis | Bite colapse, Drifiting, Flaring | 1 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 203 | 62 | 5 | 6 | 9 | 15 | horizontal | none due to Periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 93 | no | = 2 mm | Lower attachment loss in spite of heavy biofilm deposits | ||||||||||
| 204 | 63 | 6 | 16 | 8 | 31 | horizontal | none due to Periodontitis | no need | 79.5 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 205 | 53 | 5 | 16 | 5 | 30 | horizontal | no one | no need | 59 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 206 | 80 | 4 | - | 7 | 36 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 28 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 207 | 25 | 5 | 0 | 0 | 0 | - | no one | no need | 27.6 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 208 | 45 | 6 | 3 | 2 | 0 | horizontal | none due to Periodontitis | no need | 6 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 209 | 34 | 6 | 4 | 3 | 27.6 | horizontal | none due to Periodontitis | < 20 remaining teeth | 53 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 210 | 20 | 4 | 0 | 0 | 0 | - | no one | no need | 45 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 211 | 44 | 6 | 0 | 0 | 0 | - | none due to Periodontitis | < 20 remaining teeth | 6 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 212 | 29 | 5 | 0 | 0 | 0 | - | no one | no need | 7 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 213 | 66 | 6 | 4 | 9 | 18 | horizontal | Loss of 5 or more teeth - periodontitis | drifting | 2.5 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 214 | 65 | 8 | 13 | 6 | 23 | horizontal | none due to Periodontitis | Bite collapse, drifting | 9 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 215 | 59 | 6 | 6 | 8 | 10 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction | 13 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 216 | 18 | 5 | 0 | 0 | 0 | - | no one | no need | 26 | no | - | No CAL and no/low level of biofilm | ||||||||||
| 217 | 59 | 9 | 23 | 6 | 22 | horizontal | none due to Periodontitis | no need | 29 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 218 | 66 | 5 | 2 | 1 | 6 | horizontal | no one | no need | 1 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 219 | 58 | 4 | 3 | 1 | 8.4 | horizontal | no one | no need | 4 | no | < 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 220 | 65 | 6 | 9 | 11 | 70 | horizontal | Loss of 5 or more teeth - periodontitis | < 20 remaining teeth, Bite collapse, masticatory disfunction, Secondary occlusal trauma | 6 | no | = 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| 221 | 59 | 6 | 8 | 7 | 20 | horizontal | Loss of up to 4 teeth - periodontitis | drifting | 23 | no | > 2 mm | Attachment loss proportionate with biofilm levels | ||||||||||
| Patients were Classified as B when it was the first appointment as well as = 2 mm for progression in RBL (no evidence of at least 5 years). Green background = Periodontal healthy; Yellow background = gingivitis; No background = Periodontitis. | ||||||||||||||||||||||
| Patient | Risk factor: Smoking | Risk factor: Diabetes | Has any other systemic condition (besides diabetes)? | Determine extension and distribution | Furcation? | Necrotizing lesion |
Number of remnant teeth |
|---|---|---|---|---|---|---|---|
| 1 | non-smoker | HbA1C ≥ 7.0% | no | generalized (> 30%) | no | no | 9 |
| 2 | smoke < 10 | no | 1-2, controlled | generalized (> 30%) | no | no | 23 |
| 3 | non-smoker | no | >2, controlled | localized (< 30%) | no | no | 17 |
| 4 | smoke > 10 | no | no | localized (< 30%) | no | no | 32 |
| 5 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 6 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 7 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 8 | non-smoker | no | no | generalized (> 30%) | no | no | 21 |
| 9 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 25 |
| 10 | non-smoker | no | >2, controlled | localized (< 30%) | no | no | 26 |
| 11 | non-smoker | no | no | generalized (> 30%) | Class I | no | 20 |
| 12 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 32 |
| 13 | smoke < 10 | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 30 |
| 14 | non-smoker | no | no | generalized (> 30%) | no | no | 30 |
| 15 | non-smoker | no | 1-2, non-controlled | generalized (> 30%) | Class I | no | 32 |
| 16 | non-smoker | no | no | localized (< 30%) | no | no | 24 |
| 17 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 18 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 19 | smoke < 10 | no | no | - | no | no | 17 |
| 20 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 11 |
| 21 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 27 |
| 22 | non-smoker | HbA1c > 5.6% and < 7.0% | no | localized (< 30%) | no | no | 23 |
| 23 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 31 |
| 24 | smoke < 10 | no | 1-2, controlled (pregnant) | generalized (> 30%) | no | no | 28 |
| 25 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 17 |
| 26 | smoke < 10 | no | no | generalized (> 30%) | Class II | no | 24 |
| 27 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 30 |
| 28 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 24 |
| 29 | non-smoker | no | no | localized (< 30%) | no | no | 30 |
| 30 | non-smoker | no | >2, controlled | generalized (> 30%) | no | no | 22 |
| 31 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 29 |
| 32 | non-smoker | no | no | localized (< 30%) | no | no | 29 |
| 33 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 21 |
| 34 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 30 |
| 35 | non-smoker | no | no | generalized (> 30%) | no | no | 17 |
| 36 | non-smoker | no | no | generalized (> 30%) | no | no | 31 |
| 37 | non-smoker | no | no | generalized (> 30%) | no | no | 26 |
| 38 | smoke > 10 | no | 1-2, controlled | generalized (> 30%) | no | no | 30 |
| 39 | non-smoker | no | no | - | no | no | 28 |
| 40 | non-smoker | no | >2, controlled | generalized (> 30%) | Class III | no | 15 |
| 41 | non-smoker | no | 1-2, controlled | - | no | no | 27 |
| 42 | smoke < 10 | no | no | - | no | no | 24 |
| 43 | non-smoker | no | no | generalized (> 30%) | no | no | 31 |
| 44 | non-smoker | no | no | - | no | no | 28 |
| 45 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 46 | non-smoker | no | no | - | no | no | 28 |
| 47 | non-smoker | no | no | generalized (> 30%) | no | no | 23 |
| 48 | non-smoker | no | no | localized (< 30%) | no | no | 26 |
| 49 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 50 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 4 |
| 51 | non-smoker | no | no | generalized (> 30%) | no | no | 27 |
| 52 | non-smoker | no | no | localized (< 30%) | no | no | 26 |
| 53 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 19 |
| 54 | non-smoker | no | no | localized (< 30%) | no | no | 27 |
| 55 | non-smoker | no | 1-2, controlled | - | no | no | 28 |
| 56 | non-smoker | no | 1-2, controlled | localized molar-incisor pattern | Class I | no | 30 |
| 57 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 58 | non-smoker | no | 1-2, controlled | generalized (> 30%) | Class II | no | 28 |
| 59 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 60 | non-smoker | no | no | generalized (> 30%) | no | no | 28 |
| 61 | non-smoker | no | no | generalized (> 30%) | no | no | 27 |
| 62 | non-smoker | no | no | localized (< 30%) | no | no | 29 |
| 63 | non-smoker | no | no | generalized (> 30%) | no | no | 28 |
| 64 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 65 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 66 | non-smoker | no | >2, controlled | localized (< 30%) | no | no | 29 |
| 67 | non-smoker | no | no | generalized (> 30%) | no | no | 30 |
| 68 | non-smoker | no | no | localized (< 30%) | no | no | 13 |
| 69 | non-smoker | no | no | localized (< 30%) | no | no | 26 |
| 70 | smoke > 10 | no | no | generalized (> 30%) | no | no | 28 |
| 71 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 72 | non-smoker | no | no | generalized (> 30%) | no | no | 12 |
| 73 | smoke > 10 | no | no | generalized (> 30%) | no | no | 28 |
| 74 | non-smoker | no | no | localized (< 30%) | no | no | 17 |
| 75 | smoke < 10 | no | 1-2, controlled | generalized (> 30%) | no | no | 15 |
| 76 | smoke > 10 | no | no | localized (< 30%) | Class II | no | 25 |
| 77 | non-smoker | HbA1C ≥ 7.0% | 1-2, controlled | localized (< 30%) | no | no | 29 |
| 78 | non-smoker | HbA1c > 5.6% and < 7.0% | >2, controlled | generalized (> 30%) | no | no | 23 |
| 79 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 80 | smoke > 10 | no | no | localized (< 30%) | no | no | 22 |
| 81 | non-smoker | no | no | localized (< 30%) | no | no | 24 |
| 82 | smoke < 10 | no | no | generalized (> 30%) | no | no | 25 |
| 83 | non-smoker | HbA1c > 5.6% and < 7.0% | no | localized (< 30%) | Class I | no | 23 |
| 84 | non-smoker | no | no | generalized (> 30%) | no | no | 15 |
| 85 | non-smoker | no | no | generalized (> 30%) | no | no | 25 |
| 86 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 87 | non-smoker | HbA1c > 5.6% and < 7.0% | >2, controlled | generalized (> 30%) | no | no | 20 |
| 88 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 24 |
| 89 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 31 |
| 90 | smoke > 10 | no | 1-2, non-controlled | generalized (> 30%) | Class I | no | 16 |
| 91 | non-smoker | no | no | localized (< 30%) | no | no | 26 |
| 92 | non-smoker | no | no | generalized (> 30%) | no | no | 24 |
| 93 | non-smoker | no | no | generalized (> 30%) | no | no | 32 |
| 94 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 95 | non-smoker | no | no | localized (< 30%) | no | no | 26 |
| 96 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 24 |
| 97 | non-smoker | no | no | localized (< 30%) | no | no | 29 |
| 98 | non-smoker | no | no | localized (< 30%) | no | no | 30 |
| 99 | smoke < 10 | no | 1-2, non-controlled | localized (< 30%) | no | no | 25 |
| 100 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 101 | non-smoker | HbA1c > 5.6% and < 7.0% | no | generalized (> 30%) | no | no | 20 |
| 102 | non-smoker | no | 1-2, non-controlled | generalized (> 30%) | no | no | 24 |
| 103 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 17 |
| 104 | non-smoker | no | no | generalized (> 30%) | no | no | 30 |
| 105 | smoke < 10 | no | 1-2, controlled | generalized (> 30%) | no | no | 9 |
| 106 | non-smoker | no | no | localized (< 30%) | no | no | 24 |
| 107 | smoke < 10 | no | no | generalized (> 30%) | no | no | 23 |
| 108 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 4 |
| 109 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 19 |
| 110 | non-smoker | no | no | generalized (> 30%) | no | no | 27 |
| 111 | smoke > 10 | HbA1c > 5.6% and < 7.0% | >2, controlled | generalized (> 30%) | no | no | 19 |
| 112 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 113 | smoke < 10 | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 10 |
| 114 | smoke < 10 | no | no | generalized (> 30%) | no | no | 26 |
| 115 | non-smoker | no | 1-2, non-controlled | generalized (> 30%) | no | no | 27 |
| 116 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 30 |
| 117 | non-smoker | no | no | localized (< 30%) | no | no | 25 |
| 118 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 5 |
| 119 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 120 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 24 |
| 121 | non-smoker | no | >2, controlled | generalized (> 30%) | no | no | 26 |
| 122 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 22 |
| 123 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 24 |
| 124 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 24 |
| 125 | non-smoker | no | no | generalized (> 30%) | Class I | no | 18 |
| 126 | non-smoker | no | no | localized (< 30%) | no | no | 31 |
| 127 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 128 | smoke > 10 | no | 1-2, controlled | generalized (> 30%) | no | no | 28 |
| 129 | non-smoker | no | 1-2, controlled | - | no | no | 29 |
| 130 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 24 |
| 131 | smoke < 10 | no | no | generalized (> 30%) | no | no | 25 |
| 132 | non-smoker | no | no | localized (< 30%) | no | no | 29 |
| 133 | non-smoker | no | no | generalized (> 30%) | no | no | 27 |
| 134 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | - | no | no | 12 |
| 135 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 27 |
| 136 | non-smoker | no | no | localized (< 30%) | no | no | 16 |
| 137 | non-smoker | no | no | generalized (> 30%) | no | no | 23 |
| 138 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 6 |
| 139 | non-smoker | no | no | generalized (> 30%) | no | no | 25 |
| 140 | non-smoker | no | no | - | no | no | 32 |
| 141 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 24 |
| 142 | non-smoker | no | 1-2, controlled | generalized (> 30%) | Class II | no | 27 |
| 143 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 16 |
| 144 | non-smoker | no | 1-2, controlled | generalized (> 30%) | Class I | no | 24 |
| 145 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 26 |
| 146 | smoke < 10 | no | no | localized (< 30%) | no | no | 28 |
| 147 | non-smoker | no | no | - | no | no | 30 |
| 148 | non-smoker | no | no | generalized (> 30%) | no | no | 27 |
| 149 | non-smoker | no | no | localized (< 30%) | no | no | 22 |
| 150 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 151 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | localized (< 30%) | no | no | 27 |
| 152 | non-smoker | no | no | localized (< 30%) | no | no | 24 |
| 153 | non-smoker | no | no | localized (< 30%) | no | no | 24 |
| 154 | non-smoker | HbA1c > 5.6% and < 7.0% | >2, controlled | generalized (> 30%) | no | no | 22 |
| 155 | smoke < 10 | no | 1-2, controlled | generalized (> 30%) | Class II | no | 7 |
| 156 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 157 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 7 |
| 158 | non-smoker | no | no | generalized (> 30%) | no | no | 16 |
| 159 | non-smoker | HbA1C ≥ 7.0% | 1-2, controlled | localized (< 30%) | no | no | 27 |
| 160 | non-smoker | HbA1C ≥ 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 23 |
| 161 | non-smoker | no | no | generalized (> 30%) | no | no | 17 |
| 162 | non-smoker | no | no | localized (< 30%) | no | no | 31 |
| 163 | non-smoker | no | no | generalized (> 30%) | no | no | 28 |
| 164 | non-smoker | no | no | generalized (> 30%) | no | no | 30 |
| 165 | non-smoker | HbA1C ≥ 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 25 |
| 166 | non-smoker | no | no | - | no | no | 24 |
| 167 | non-smoker | no | no | - | no | no | 28 |
| 168 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 18 |
| 169 | smoke > 10 | no | no | generalized (> 30%) | no | no | 5 |
| 170 | smoke < 10 | no | >2, non-controlled | generalized (> 30%) | no | no | 14 |
| 171 | non-smoker | HbA1C ≥ 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 16 |
| 172 | smoke < 10 | no | no | generalized (> 30%) | no | no | 14 |
| 173 | non-smoker | HbA1c > 5.6% and < 7.0% | no | generalized (> 30%) | no | no | 28 |
| 174 | non-smoker | no | no | generalized (> 30%) | Class II | no | 13 |
| 175 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 28 |
| 176 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 15 |
| 177 | non-smoker | no | no | localized (< 30%) | no | no | 25 |
| 178 | non-smoker | no | 1-2, controlled | generalized (> 30%) | Class III | no | 25 |
| 179 | smoke < 10 | no | no | generalized (> 30%) | no | no | 26 |
| 180 | smoke < 10 | no | no | localized (< 30%) | Class II | no | 23 |
| 181 | non-smoker | no | no | localized (< 30%) | Class I | no | 28 |
| 182 | non-smoker | no | no | generalized (> 30%) | no | no | 30 |
| 183 | non-smoker | no | 1-2, controlled | - | no | no | 28 |
| 184 | non-smoker | HbA1c > 5.6% and < 7.0% | >2, controlled | generalized (> 30%) | no | no | 23 |
| 185 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 186 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 25 |
| 187 | non-smoker | no | >2, controlled | generalized (> 30%) | no | no | 23 |
| 188 | non-smoker | no | no | - | no | no | 28 |
| 189 | non-smoker | no | no | localized (< 30%) | no | no | 24 |
| 190 | non-smoker | no | >2, controlled | localized (< 30%) | no | no | 12 |
| 191 | non-smoker | no | no | generalized (> 30%) | no | no | 27 |
| 192 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 26 |
| 193 | non-smoker | no | no | - | no | no | 24 |
| 194 | non-smoker | no | no | generalized (> 30%) | no | no | 28 |
| 195 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 20 |
| 196 | non-smoker | no | no | generalized (> 30%) | Class I | no | 20 |
| 197 | non-smoker | no | no | localized (< 30%) | no | no | 34 |
| 198 | non-smoker | no | no | generalized (> 30%) | Class I | no | 25 |
| 199 | smoke < 10 | no | no | generalized (> 30%) | no | no | 21 |
| 200 | smoke > 10 | no | 1-2, controlled | generalized (> 30%) | Class II | no | 22 |
| 201 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | localized (< 30%) | no | no | 24 |
| 202 | non-smoker | no | no | - | no | no | 27 |
| 203 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 12 |
| 204 | smoke > 10 | no | 1-2, controlled | generalized (> 30%) | Class I | no | 22 |
| 205 | non-smoker | no | no | generalized (> 30%) | no | no | 25 |
| 206 | non-smoker | no | 1-2, controlled | generalized (> 30%) | no | no | 3 |
| 207 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 208 | non-smoker | HbA1c > 5.6% and < 7.0% | >2, controlled | localized (< 30%) | no | no | 23 |
| 209 | non-smoker | no | no | generalized (> 30%) | no | no | 16 |
| 210 | non-smoker | no | no | generalized (> 30%) | no | no | 31 |
| 211 | non-smoker | no | no | - | no | no | 21 |
| 212 | non-smoker | no | 1-2, controlled | - | no | no | 32 |
| 213 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | Class I | no | 20 |
| 214 | non-smoker | no | 1-2, controlled | generalized (> 30%) | Class I | no | 23 |
| 215 | smoke > 10 | no | 1-2, controlled | generalized (> 30%) | no | no | 9 |
| 216 | non-smoker | no | no | localized (< 30%) | no | no | 32 |
| 217 | non-smoker | HbA1C ≥ 7.0% | 1-2, controlled | generalized (> 30%) | Class II | no | 30 |
| 218 | non-smoker | no | 1-2, controlled | localized (< 30%) | no | no | 28 |
| 219 | non-smoker | no | no | localized (< 30%) | no | no | 28 |
| 220 | non-smoker | HbA1c > 5.6% and < 7.0% | 1-2, controlled | generalized (> 30%) | no | no | 15 |
| 221 | non-smoker | HbA1C ≥ 7.0% | >2, controlled | generalized (> 30%) | Class I | no | 25 |
| Patients were Classified as B when it was the first appointment as well as = 2 mm for progression in RBL (no evidence of at least 5 years). Green background = Periodontal healthy; Yellow background = gingivitis; No background = Periodontitis. | |||||||
GF-PeDRA© Score and Inter-Agreement Level
Discussion
Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Papapanou, P.N., Sanz, M., Buduneli, N., Dietrich, T., Feres, M., Fine, D.H., Flemmig, T.F., Garcia, R., Giannobile, W.V., Graziani, F., Greenwell, H., Herrera, D., Kao, R.T., Kebschull, M., Kinane, D.F., Kirkwood, K.L., Kocher, T., Kornman, K.S., Kumar, P.S., Loos, B.G., Machtei, E., Meng, H., Mombelli, A., Needleman, I., Offenbacher, S., Seymour, G.J., Teles, R., Tonetti, M.S. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol, 2018, 89(S1), S173-S182. [CrossRef]
- Armitage, G.C. Development of a classification system for periodontal diseases and conditions. Ann Periodontol, 1999, 4(1), 1-6. [CrossRef]
- Takedachi, M., Shimabukuro, Y., Sawada, K., Koshimizu, M., Shinada, K., Asai, H., Mizoguchi, A., Hayashi, Y., Tsukamoto, A., Miyago, M., Nishihara, F., Nishihata, T., Shimabukuro, M., Kurakami, H., Sato, T., Hamazaki, Y., Iwayama, T., Fujihara, C., Murakami, S. Evaluation of periodontitis-related tooth loss according to the new 2018 classification of periodontitis. Sci Rep, 2022, 12, 11893. [CrossRef]
- Cafiero C, Matarasso S. Predictive, preventive, personalised and participatory periodontology: ‘the 5Ps age’ has already started. EPMA J, 2013, 4, 16.
- Heitz-Mayfield, L.J. (2005). Disease progression: Identification of high-risk groups and individuals for periodontitis. J Clin Periodontol, 2005, 32(Suppl 6), 196–209. [CrossRef]
- Lang, N.P., Suvan, J.E., Tonetti, M.S. Risk factor assessment tools for the prevention of periodontitis progression a systematic review. J Clin Periodontol, 2015, 42(Suppl 16), S59–S70. [CrossRef]
- Lang, N.P., Tonetti, M.S. Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev Dent, 2003, 1(1), 7–16.
- Chandra, R.V. Evaluation of a novel periodontal risk assessment model in patients presenting for dental care. Oral Health Prev Dent, 2007, 5(1), 39-48.
- Kornman, K. S., Crane, A., Wang, H.Y., di Giovine, F.S., Newman, M.G., Pirk, F.W., Wilson, T.G., Higginbottom, F.L., Duff, G.W. The interleukin-1 genotype as a severity factor in adult periodontal disease. J Clin Periodontol, 1997, 24(1), 72-77. [CrossRef]
- Genco, R.J., Borgnakke, W.S. Risk factors for periodontal disease. Periodontol 2000, 2013, 62(1), 59-94.
- Van der Velden, U. Purpose and problems of periodontal disease classification. Periodontol 2000, 2003, 32(1), 13-21.
- Lindskog, S., Blomlöf, J., Persson, I., Niklason, A., Hedin, A., Ericsson, L., Ericsson, M., Järncrantz, B., Palo, U., Tellefsen, G., Zetterström, O., Blomlöf, L. Validation of an algorithm for chronic periodontitis risk assessment and prognostication: risk predictors, explanatory values, measures of quality, and clinical use. J Periodontol, 2010, 81(4), 584-593. [CrossRef]
- Page, R.C., Krall, E.A., Martin, J.A., Mancl, L., Garcia, R.I. Validity and accuracy of a risk calculator in predicting periodontal disease. J Am Dental Assoc, 2002, 133(5), 569-576. [CrossRef]
- Chapple, I.L.C., Van der Weijden, F., Doerfer, C., Herrera, D., Shapira, L., Polak, D., Madianos, P., Louropoulou, A., Machtei, E., Donos, N., Greenwell, H. Primary prevention of periodontitis: managing gingivitis. J Clin Periodontol, 2006, 42(S16), S71-S76. [CrossRef]
- Kinane, D.F., Chestnutt, I.G. (2000). Smoking and periodontal disease. Crit Rev Oral Biol Med, 2000, 11(3), 356-365.
- Mealey, B.L., Oates, T.W. (2006). Diabetes mellitus and periodontal diseases. J Periodontol, 2006, 77(8), 1289-1303. [CrossRef]
- Tonetti, M.S., Pini-Prato, G., Cortellini, P. Periodontal regeneration of human intrabony defects. IV. Determinants of healing response. J Periodontol, 2005, 66(6), 544-550. [CrossRef]
- Trombelli, L., Tatakis, D.N., Scapoli, C., Bottega, S., Orlandini, E., Tosi, M. Modulation of clinical expression of plaque-induced gingivitis. II. Identification of "high-responder" and "low-responder" subjects. J Clin Periodontol, 2004, 31(4), 239-252. [CrossRef]
| Patient number |
Diagnosis (GVOF) |
Diagnosis (JCHF) |
Final Diagnosis (after discussion) |
Diagnosis (GF-PeDRA©) |
GF-PeDRA score (0-100%) |
Prognosis |
|---|---|---|---|---|---|---|
| 1 | Periodontitis III-C | Periodontitis IV-C | Periodontitis III-C | Periodontitis III-C | 41.4 | Questionable |
| 2 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 47.9 | Questionable |
| 3 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 41 | Questionable |
| 4 | gingivitis | gingivitis | gingivitis | gingivitis | 16.8 | Fair |
| 5 | gingivitis | gingivitis | gingivitis | gingivitis | 15.4 | Fair |
| 6 | gingivitis | Healthy periodontium | gingivitis | gingivitis | 9.4 | Good |
| 7 | gingivitis | gingivitis | gingivitis | gingivitis | 15.4 | Fair |
| 8 | Periodontitis III-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 48.8 | Questionable |
| 9 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 25.4 | Poor |
| 10 | gingivitis | gingivitis | gingivitis | gingivitis | 12.7 | Fair |
| 11 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 51.5 | Hopeless |
| 12 | gingivitis | gingivitis | gingivitis | gingivitis | 17.4 | Fair |
| 13 | Periodontitis I-B | Periodontitis II-B | Periodontitis I-B | Periodontitis I-B | 36.7 | Poor |
| 14 | gingivitis | gingivitis | gingivitis | gingivitis | 11.2 | Fair |
| 15 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 39.8 | Questionable |
| 16 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 32.4 | Poor |
| 17 | gingivitis | gingivitis | gingivitis | gingivitis | 7.4 | Good |
| 18 | gingivitis | gingivitis | gingivitis | gingivitis | 7.4 | Good |
| 19 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 1.7 | Good |
| 20 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 46.6 | Questionable |
| 21 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 48.2 | Questionable |
| 22 | gingivitis | gingivitis | gingivitis | gingivitis | 11.4 | Fair |
| 23 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 40.2 | Questionable |
| 24 | gingivitis | gingivitis | gingivitis | gingivitis | 17.1 | Fair |
| 25 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 44.8 | Questionable |
| 26 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 59.8 | Hopeless |
| 27 | gingivitis | gingivitis | gingivitis | gingivitis | 7.4 | Good |
| 28 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 24.4 | Fair |
| 29 | gingivitis | gingivitis | gingivitis | gingivitis | 9.7 | Good |
| 30 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 39.1 | Questionable |
| 31 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 27.1 | Poor |
| 32 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 26.8 | Poor |
| 33 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 7.4 | Good |
| 34 | gingivitis | gingivitis | gingivitis | gingivitis | 11.7 | Fair |
| 35 | Periodontitis III-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 45.7 | Questionable |
| 36 | gingivitis | gingivitis | gingivitis | gingivitis | 11.2 | Fair |
| 37 | gingivitis | gingivitis | gingivitis | gingivitis | 13.2 | Fair |
| 38 | Periodontitis I-C | Periodontitis I-C | Periodontitis I-C | Periodontitis I-C | 37.7 | Poor |
| 39 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 2.9 | Good |
| 40 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 64.1 | Hopeless |
| 41 | Healthy periodontium | gingivitis | Healthy periodontium | Healthy periodontium | 1.5 | Good |
| 42 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 7.4 | Good |
| 43 | gingivitis | gingivitis | gingivitis | gingivitis | 13.5 | Fair |
| 44 | Healthy periodontium | gingivitis | Healthy periodontium | Healthy periodontium | 3.2 | Good |
| 45 | gingivitis | gingivitis | gingivitis | gingivitis | 11.2 | Fair |
| 46 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 0.6 | Good |
| 47 | gingivitis | gingivitis | gingivitis | gingivitis | 13.2 | Fair |
| 48 | gingivitis | gingivitis | gingivitis | gingivitis | 6.4 | Good |
| 49 | gingivitis | gingivitis | gingivitis | gingivitis | 9.7 | Good |
| 50 | Periodontitis IV-B | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 43.4 | Questionable |
| 51 | gingivitis | gingivitis | gingivitis | gingivitis | 11.2 | Fair |
| 52 | Periodontitis II-B | Periodontitis III-B | Periodontitis II-B | Periodontitis II-B | 32.1 | Poor |
| 53 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 45.6 | Questionable |
| 54 | gingivitis | Healthy periodontium | gingivitis | gingivitis | 9.7 | Good |
| 55 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 1.0 | Good |
| 56 | molar/incisor Periodontitis III-C | molar/incisor Periodontitis III-C | molar/incisor Periodontitis III-C | molar/incisor Periodontitis III-C | 52.6 | Hopeless |
| 57 | gingivitis | gingivitis | gingivitis | gingivitis | 7.4 | Good |
| 58 | Periodontitis III-C | Periodontitis IV-C | Periodontitis III-C | Periodontitis III-C | 40.2 | Questionable |
| 59 | gingivitis | gingivitis | gingivitis | gingivitis | 13.5 | Fair |
| 60 | gingivitis | gingivitis | gingivitis | gingivitis | 10.2 | Fair |
| 61 | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | 41.3 | Questionable |
| 62 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 36.2 | Poor |
| 63 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 41.6 | Questionable |
| 64 | gingivitis | gingivitis | gingivitis | gingivitis | 9.7 | Good |
| 65 | gingivitis | gingivitis | gingivitis | gingivitis | 11.2 | Fair |
| 66 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 31.2 | Poor |
| 67 | Periodontitis I-C | Periodontitis I-B | Periodontitis I-C | Periodontitis I-C | 36.1 | Poor |
| 68 | gingivitis | gingivitis | gingivitis | gingivitis | 12.3 | Fair |
| 69 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 31.5 | Poor |
| 70 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 45 | Questionable |
| 71 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 39 | Questionable |
| 72 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 46.8 | Questionable |
| 73 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 45 | Questionable |
| 74 | gingivitis | gingivitis | gingivitis | gingivitis | 9.4 | Good |
| 75 | Periodontitis I-B | Periodontitis IV-B | Periodontitis I-B | Periodontitis I-B | 38.5 | Questionable |
| 76 | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | 35.2 | Poor |
| 77 | Periodontitis I-C | Periodontitis I-C | Periodontitis I-C | Periodontitis I-C | 34.1 | Poor |
| 78 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 49.6 | Questionable |
| 79 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 3.5 | Good |
| 80 | Healthy periodontium | gingivitis | Healthy periodontium | Healthy periodontium | 12.4 | Fair |
| 81 | Periodontitis IV-C | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 39 | Questionable |
| 82 | Periodontitis III-B | Periodontitis IV-B | Periodontitis III-B | Periodontitis III-B | 43.3 | Questionable |
| 83 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 55.5 | Hopeless |
| 84 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 41 | Questionable |
| 85 | Periodontitis II-A | Periodontitis II-A | Periodontitis II-A | Periodontitis II-A | 42.3 | Questionable |
| 86 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 35.9 | Poor |
| 87 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 41.5 | Questionable |
| 88 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 33.5 | Poor |
| 89 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 40.6 | Questionable |
| 90 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 63.3 | Hopeless |
| 91 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 40.3 | Questionable |
| 92 | gingivitis | gingivitis | gingivitis | gingivitis | 17.4 | Fair |
| 93 | gingivitis | gingivitis | gingivitis | gingivitis | 15.4 | Fair |
| 94 | Periodontitis I-A | Periodontitis II-A | Periodontitis I-A | Periodontitis I-A | 26.8 | Poor |
| 95 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 29.4 | Poor |
| 96 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 3.5 | Good |
| 97 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 26.3 | Poor |
| 98 | gingivitis | gingivitis | gingivitis | gingivitis | 7.4 | Good |
| 99 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 27.7 | Poor |
| 100 | gingivitis | Healthy periodontium | gingivitis | gingivitis | 7.4 | Good |
| 101 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 53.1 | Hopeless |
| 102 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 48.4 | Questionable |
| 103 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 32.2 | Poor |
| 104 | Periodontitis III-C | Periodontitis IV-C | Periodontitis III-C | Periodontitis III-C | 42.2 | Questionable |
| 105 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 42.9 | Questionable |
| 106 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 2.9 | Good |
| 107 | Periodontitis III-B | Periodontitis IV-B | Periodontitis III-B | Periodontitis III-B | 39.3 | Questionable |
| 108 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 37.3 | Poor |
| 109 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 52.6 | Hopeless |
| 110 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 43.3 | Questionable |
| 111 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 58.2 | Hopeless |
| 112 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 5.8 | Good |
| 113 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 46.3 | Questionable |
| 114 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 37.6 | Poor |
| 115 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 30 | Poor |
| 116 | gingivitis | gingivitis | gingivitis | gingivitis | 17.4 | Fair |
| 117 | gingivitis | gingivitis | gingivitis | gingivitis | 9.4 | Good |
| 118 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 47.1 | Questionable |
| 119 | gingivitis | gingivitis | gingivitis | gingivitis | 8.4 | Good |
| 120 | Periodontitis IV-B | Periodontitis III-B | Periodontitis IV-B | Periodontitis IV-B | 50 | Hopeless |
| 121 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 50.8 | Hopeless |
| 122 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 40.2 | Questionable |
| 123 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 46.6 | Questionable |
| 124 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 52.7 | Hopeless |
| 125 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 30.2 | Poor |
| 126 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 5.2 | Good |
| 127 | gingivitis | Healthy periodontium | gingivitis | gingivitis | 9.7 | Good |
| 128 | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | 40.8 | Questionable |
| 129 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 5.8 | Good |
| 130 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 43.2 | Questionable |
| 131 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 41.9 | Questionable |
| 132 | Periodontitis II-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 26.6 | Poor |
| 133 | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | 39 | Questionable |
| 134 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 7.5 | Good |
| 135 | Periodontitis III-B | Periodontitis IV-B | Periodontitis III-B | Periodontitis III-B | 39.6 | Questionable |
| 136 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 23.1 | Fair |
| 137 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 40 | Questionable |
| 138 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 37.3 | Poor |
| 139 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 41.6 | Questionable |
| 140 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 1 | Good |
| 141 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 24.9 | Fair |
| 142 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 34.8 | Poor |
| 143 | Periodontitis I-A | Periodontitis II-A | Periodontitis I-A | Periodontitis I-A | 30.1 | Poor |
| 144 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 39.2 | Questionable |
| 145 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 24.9 | Fair |
| 146 | gingivitis | gingivitis | gingivitis | gingivitis | 13.3 | Fair |
| 147 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 3.3 | Good |
| 148 | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | 35.7 | Poor |
| 149 | gingivitis | gingivitis | gingivitis | gingivitis | 9.4 | Good |
| 150 | gingivitis | gingivitis | gingivitis | gingivitis | 6.4 | Good |
| 151 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 29.8 | Poor |
| 152 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 21.6 | Fair |
| 153 | gingivitis | gingivitis | gingivitis | gingivitis | 9.7 | Good |
| 154 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 35.6 | Poor |
| 155 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 55 | Hopeless |
| 156 | gingivitis | Healthy periodontium | gingivitis | gingivitis | 7.4 | Good |
| 157 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 51.7 | Hopeless |
| 158 | Periodontitis IV-B | Periodontitis III-B | Periodontitis IV-B | Periodontitis IV-B | 41.8 | Questionable |
| 159 | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | Periodontitis II-C | 35.1 | Poor |
| 160 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 45.5 | Questionable |
| 161 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 40.9 | Questionable |
| 162 | gingivitis | gingivitis | gingivitis | gingivitis | 7.4 | Good |
| 163 | gingivitis | gingivitis | gingivitis | gingivitis | 13.2 | Fair |
| 164 | gingivitis | gingivitis | gingivitis | gingivitis | 14.3 | Fair |
| 165 | Periodontitis I-C | Periodontitis I-C | Periodontitis I-C | Periodontitis I-C | 37.1 | Poor |
| 166 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 3.5 | Good |
| 167 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 5.2 | Good |
| 168 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 54.9 | Hopeless |
| 169 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 40.4 | Questionable |
| 170 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 44.6 | Questionable |
| 171 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 54.5 | Hopeless |
| 172 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 34.5 | Poor |
| 173 | gingivitis | gingivitis | gingivitis | gingivitis | 17.1 | Fair |
| 174 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 47.3 | Questionable |
| 175 | gingivitis | gingivitis | gingivitis | gingivitis | 17.1 | Fair |
| 176 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 35.7 | Poor |
| 177 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 22.4 | Fair |
| 178 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 47 | Questionable |
| 179 | Periodontitis III-B | Periodontitis IV-B | Periodontitis III-B | Periodontitis III-B | 37 | Poor |
| 180 | Periodontitis IV-C | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 44.1 | Questionable |
| 181 | gingivitis | Healthy periodontium | gingivitis | gingivitis | 10 | Fair |
| 182 | gingivitis | gingivitis | gingivitis | gingivitis | 15.1 | Fair |
| 183 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 4.9 | Good |
| 184 | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | Periodontitis II-B | 29.5 | Poor |
| 185 | gingivitis | gingivitis | 9.7 | Good | ||
| 186 | Periodontitis III-A | Periodontitis III-A | Periodontitis III-A | Periodontitis III-A | 38 | Questionable |
| 187 | Periodontitis III-A | Periodontitis III-A | Periodontitis III-A | Periodontitis III-A | 42.6 | Questionable |
| 188 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 3.3 | Good |
| 189 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 31.8 | Poor |
| 190 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 10.7 | Fair |
| 191 | Periodontitis III-B | Periodontitis III-A | Periodontitis III-A | Periodontitis III-A | 36.3 | Poor |
| 192 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 44 | Questionable |
| 193 | Healthy periodontium | gingivitis | Healthy periodontium | Healthy periodontium | 3.5 | Good |
| 194 | gingivitis | gingivitis | gingivitis | gingivitis | 22 | Fair |
| 195 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 25.5 | Poor |
| 196 | Periodontitis III-B | Periodontitis IV-B | Periodontitis III-B | Periodontitis III-B | 41.7 | Questionable |
| 197 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 7.5 | Good |
| 198 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 42.4 | Questionable |
| 199 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 45.3 | Questionable |
| 200 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 41.2 | Questionable |
| 201 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 33.4 | Poor |
| 202 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 14.3 | Fair |
| 203 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 43.3 | Questionable |
| 204 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 47.2 | Questionable |
| 205 | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | Periodontitis III-B | 37.1 | Poor |
| 206 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 42.2 | Questionable |
| 207 | gingivitis | gingivitis | gingivitis | gingivitis | 9.7 | Good |
| 208 | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | Periodontitis I-B | 28.9 | Poor |
| 209 | Periodontitis II-B | Periodontitis IV-B | Periodontitis II-B | Periodontitis II-B | 39.7 | Questionable |
| 210 | gingivitis | gingivitis | gingivitis | gingivitis | 11.2 | Fair |
| 211 | Healthy periodontium | Healthy periodontium | Healthy periodontium | Healthy periodontium | 11.6 | Fair |
| 212 | Healthy periodontium | gingivitis | Healthy periodontium | Healthy periodontium | 5.5 | Good |
| 213 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 47.1 | Questionable |
| 214 | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | Periodontitis IV-B | 47.7 | Questionable |
| 215 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 51.3 | Hopeless |
| 216 | gingivitis | gingivitis | gingivitis | gingivitis | 9.7 | Good |
| 217 | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | Periodontitis III-C | 48 | Questionable |
| 218 | Periodontitis I-A | Periodontitis II-A | Periodontitis I-A | Periodontitis I-A | 19.4 | Fair |
| 219 | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | Periodontitis I-A | 18.2 | Fair |
| 220 | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | Periodontitis IV-C | 51.4 | Hopeless |
| 221 | Periodontitis IV-C | Periodontitis III-C | Periodontitis IV-C | Periodontitis IV-C | 50.7 | Hopeless |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





