1. Introduction
The exact cause of autoimmune responses in neuroinflammatory disorders like multiple sclerosis (MS) remains unclear. While certain genetic variations increase the risk, they do not guarantee disease onset. Environmental factors, including infections, significantly contribute to the development of central nervous system (CNS) inflammatory disorders such as MS [
1]. However, direct evidence of a specific pathogenic agent causing MS is still lacking.
Epstein-Barr virus (EBV), a member of herpes virus family which establishes latent infection with periodic reactivation, is considered a potential environmental trigger in MS development, possibly by infecting B cells [
2]. Research shows a correlation between prior EBV infection and an increased risk of MS onset [
3]. This suggests that molecular mimicry, where EBV antigens resemble self-antigens, may induce autoimmunity in genetically susceptible individuals [
4]. Given that over 90% of the global population is seropositive for EBV [
5], other factors such as interactions with additional pathogens, vaccination profiles, and specific genetic variations likely contribute to the difference in MS prevalence between high- and low-risk areas. These factors can also influence the highly heterogeneous disease course.
Mitochondrial dysfunctions play an important role in the progression of neurological disorders, including MS, contributing to energy deficiency, oxidative stress, inflammation, and neurodegeneration [
6]. Reduced ATP production due to mitochondrial dysfunctions can weaken the immune system, causing metabolic dysfunction in peripheral immune cells [
7]. In MS, demyelinated axons require more energy to propagate action potentials, and mitochondrial dysfunction exacerbates the energy deficit, further compromising neuronal function.
Infections can impact mitochondrial function, and conversely, mitochondrial dysfunction can influence the body’s ability to respond to infections [
8]. Infections can lead to increased production of reactive oxygen species and the release of cytokines, disrupting mitochondrial dynamics [
9]. This bidirectional relationship between mitochondrial dysfunction and infections highlights the complex interplay contributing to the pathogenesis of MS and other neuroinflammatory disorders.
Mitophagy, a selective form of autophagy that target damaged or dysfunctional mitochondria for degradation and recycling, plays a crucial role in the host’s defense against infections by maintaining mitochondrial quality, regulating immune responses, and preventing excessive inflammation [
10]. One of the most well-characterized pathways for mitophagy is the PTEN-induced putative kinase 1 (PINK1)-Parkin Pathway [
11]. In this pathway, PINK1 accumulation on damaged mitochondria recruits and activates Parkin (encoded by the
PARK2 gene), leading to the ubiquitination of mitochondrial proteins and the recruitment of autophagy receptors [
11]. Notably, mutations in PINK1, Parkin, and other mitophagy-related proteins are linked to early-onset Parkinson’s disease [
11].
Recent research has demonstrated that PINK1 and Parkin are also associated with mechanisms related to innate and adaptive immunity in the context of neuroinflammation and neurodegeneration. For instance, intestinal infection with Gram-negative bacteria in
PINK1 knockout mice triggers mitochondrial antigen presentation and autoimmune mechanisms, leading to the establishment of cytotoxic mitochondria-specific CD8 T cells in both the periphery and the brain [
12]. Furthermore, the absence of PINK1 and Parkin proteins exacerbates acute inflammation in active experimental autoimmune encephalomyelitis (EAE) with myelin oligodendrocyte glycoprotein (MOG) in C57BL/6J mice [
13,
14]. Both proteins have an age-related influence on various subsets of innate and adaptive immune cells in the periphery and CNS at different stages of active EAE progression [
13,
14]. This age-related impact suggests that the functional roles of PINK1 and Parkin in immune modulation and neuroprotection may vary over the lifespan, affecting the severity and progression of neuroinflammatory conditions such as MS and other neurodegenerative diseases.
To investigate the relationship between altered mitophagy, EBV, and neuroinflammation, we analyzed the impact of immunization with a recently discovered peptide from the EBV nuclear antigen EBNA1 that cross-reacts with glial cell adhesion protein (GlialCAM) in the CNS [
15]. This study was conducted in both
PARK2 knockout (
PARK2-/-) and wild-type mice, and the results were compared with those from immunization using the MOG-EAE model in the same mice. Our study demonstrated that alterations in mitochondria-mediated immune responses lead to increased inflammation due to the EBV antigenic component. This suggests that EBV peptides might exacerbate neuroinflammation through molecular mimicry and mitochondrial dysfunction, highlighting the potential for targeted therapeutic strategies that address these specific immune and mitochondrial pathways in neuroinflammatory diseases like MS.
3. Discussion
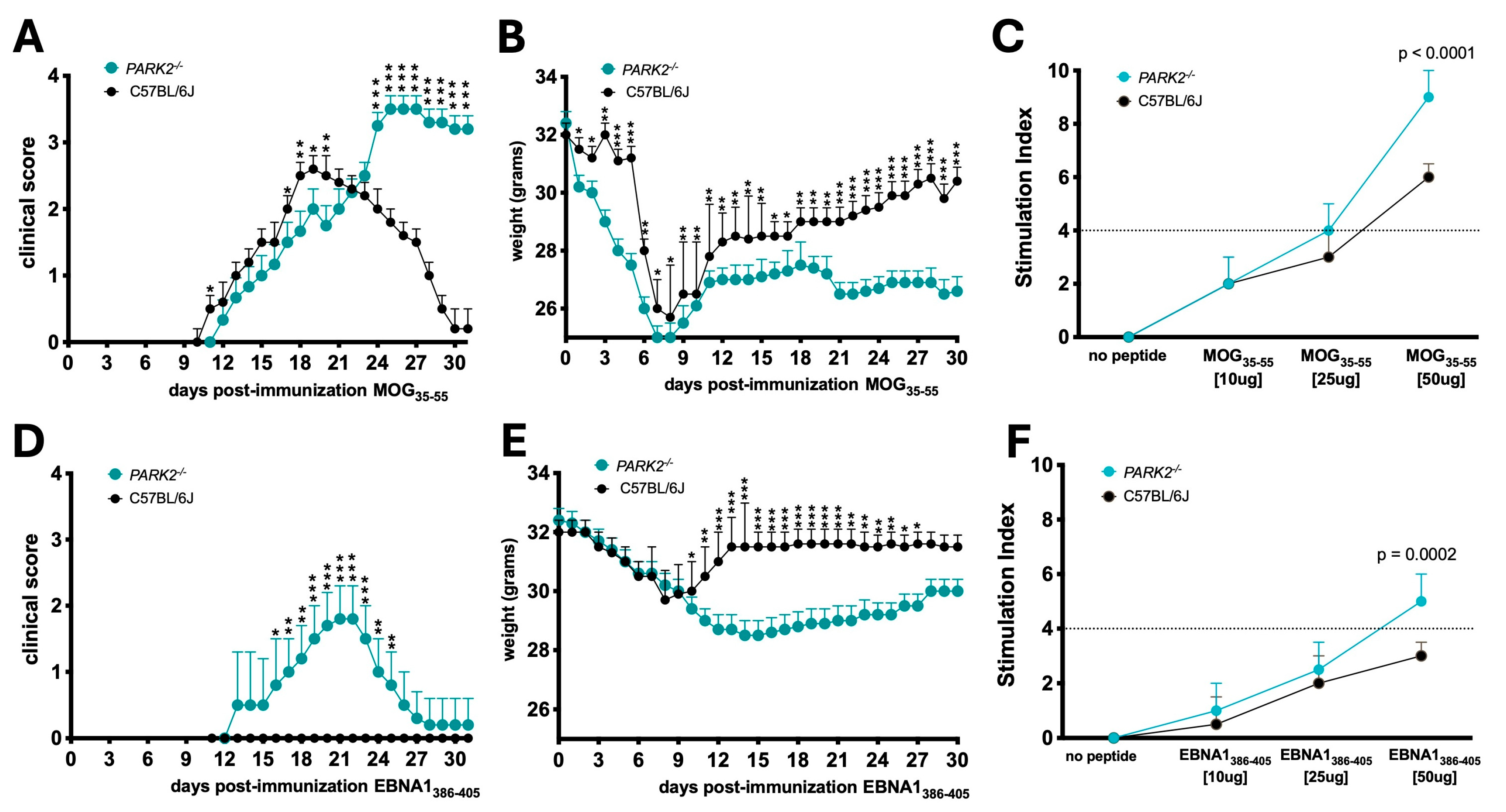
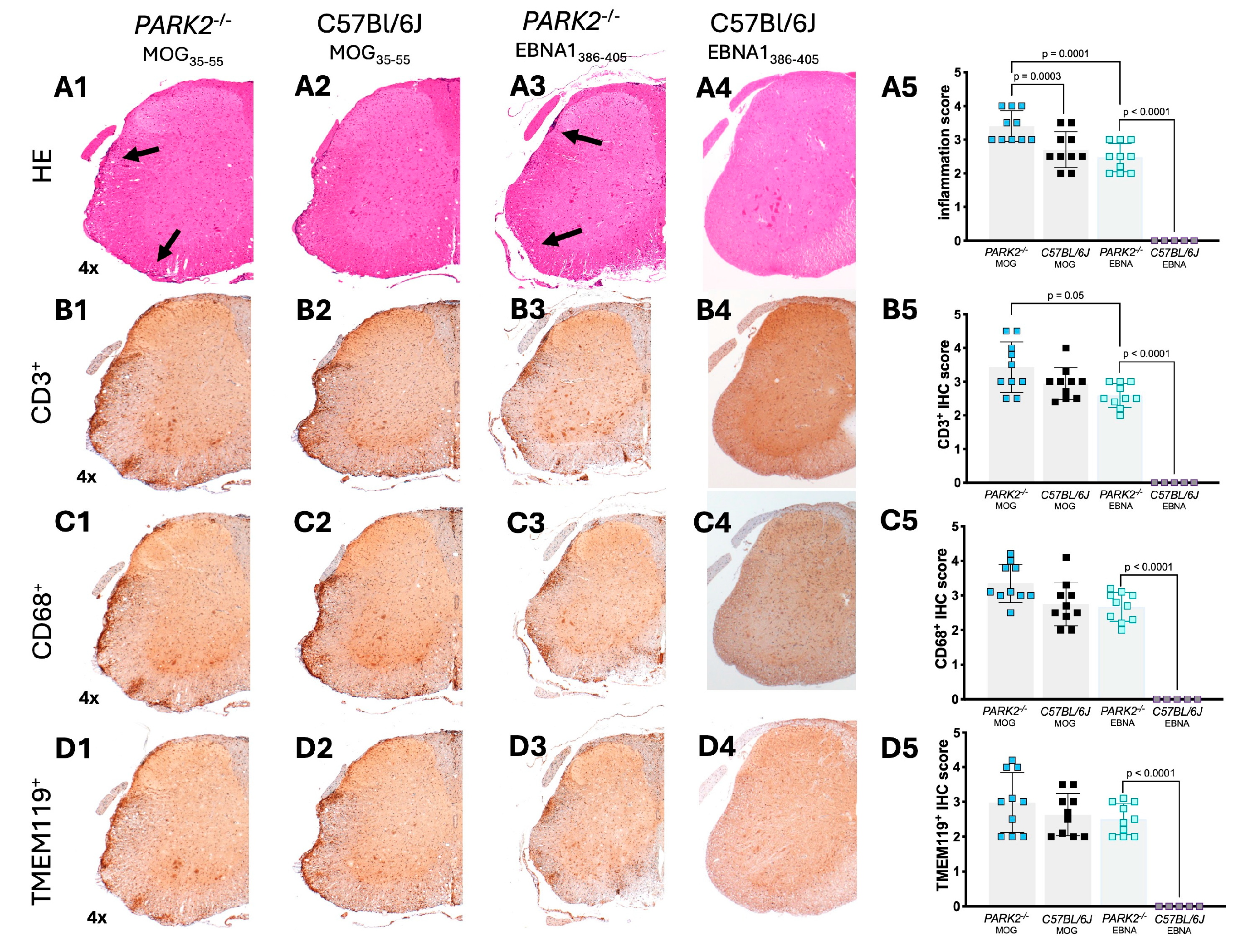
In this study, we confirmed the role of Parkin protein in modulating peripheral immune cells-mediated immunity during EAE, and the role of EBV in neuroinflammation within the context of mitochondrial dysfunctions. Specifically, we demonstrated that subcutaneously immunization with the immunogenic peptide EBNA1385-405 in adjuvant, along with pertussis toxin administration, can induce symptoms consistent with active MOG-EAE in middle-aged female PARK2-/- mice, which exhibit mitochondrial dysfunctions involved in mitophagy.
A previous study showed that young
PARK2-/- mice experienced more severe EAE disease and an earlier onset compared to wild-type controls, characterized by a high frequency of CD8
+ T cells in the periphery and brain [
13]. This indicates that mitochondrial dysfunctions influence the course of MOG-EAE-induced neuroinflammation in mice with a C57Bl/6J genetic background. Another recent study highlighted that EBNA1
386-405 is involved in high-affinity molecular mimicry with the CNS protein GlialCAM, revealing cross-reactive anti-EBNA1 and anti-GlialCAM antibodies in patients with MS [
15]. Additionally, this study showed that young SJL/J mice immunized with the EBNA1
386-405 peptide a few weeks before inducing active EAE with myelin proteolipid protein (PLP)
139-151 developed more severe EAE in terms of symptoms, CNS immune cell infiltration, and demyelination [
15]. EBNA1
385-405 also stimulated the secretion of B cell stimulatory T helper cytokines and a strong CD4 response [
15].
Our study confirms the encephalitogenic role of EBNA1386-405 but with several key differences. Firstly, only PARK2-/- mice developed symptoms similar to EAE, not wild-type mice. We did not evaluate the effect of EBNA1386-405 before or after MOG-EAE immunization or the effect of a boost. Instead, we assessed the direct immunization effect of EBNA1386-405 and compared it to MOG-EAE.
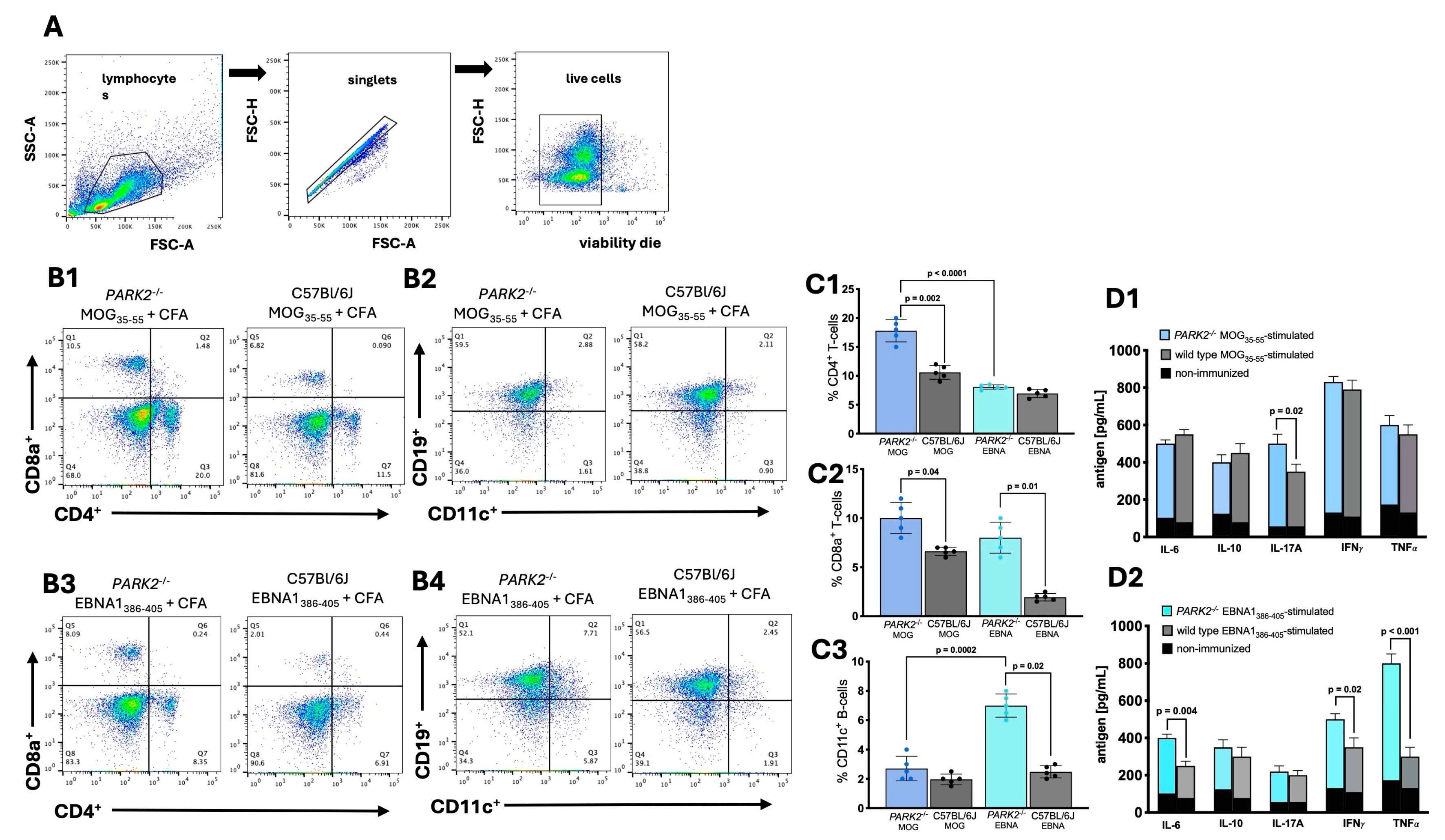
In our model,
PARK2-/- mice immunized with EBNA1
386-405 exhibited a significant percentage of CD8
+ cells in the periphery compared to C57Bl/6J wild-type controls that did not develop any symptoms. The Parkin protein encoded by
PARK2 regulates adaptive immunity by repressing mitochondrial antigen presentation [
16]. The absence of Parkin can promote the establishment of peripheral mitochondrial antigen-specific T cell populations, which can access the CNS during infections or neuroinflammation [
16]. Interestingly, studies investigating anti-EBV immunity in the CNS of MS patients suggest that EBV-specific T cells gain access to the brain and that altered intrathecal CD8 T cell responses toward EBV could contribute to CNS inflammation and tissue damage [
17].
We also observed an increased frequency of CD11C
+ CD19
+ B cells in the periphery of
PARK2-/- mice immunized with EBNA1
386-405 compared to wild-type controls [
18]. These cells, primarily memory B cells prone to differentiate into antibody secreting cells [
19], continuously expands with age in healthy individuals but show a premature and pronounced accumulation in autoimmune diseases [
18]. It has been suggested that these age-related cells are functional mediators of viral-enhanced autoimmunity, as they increase during latent viral infections [
18]. The latent form of EBV appears to prime CD11C
+ CD19
+ B cells, contributing pathogenically to autoimmune diseases [
20,
21].
Interestingly,
PARK2-/- mice immunized with MOG
35-55 showed in the periphery elevated concentrations of the key Th17 cytokine IL-17A during the acute phase compared to wild-type control. In contrast,
PARK2-/- mice immunized with EBNA1
386-405 exhibited lower IL-17A levels but higher concentration of IL-6, IFN-γ and TNF-α. Notably, TNF-α was also elevated in
PARK2-/- mice immunized with EBNA1
386-405 compared to those immunized with MOG
35-55. These findings partially align with previously studies, which demonstrated that EBNA1
386–405 stimulated the secretion of IFN-γ, TNF, and IL-12, as well as IL-6 and IL-10, while suppressing IL-17 [
15].
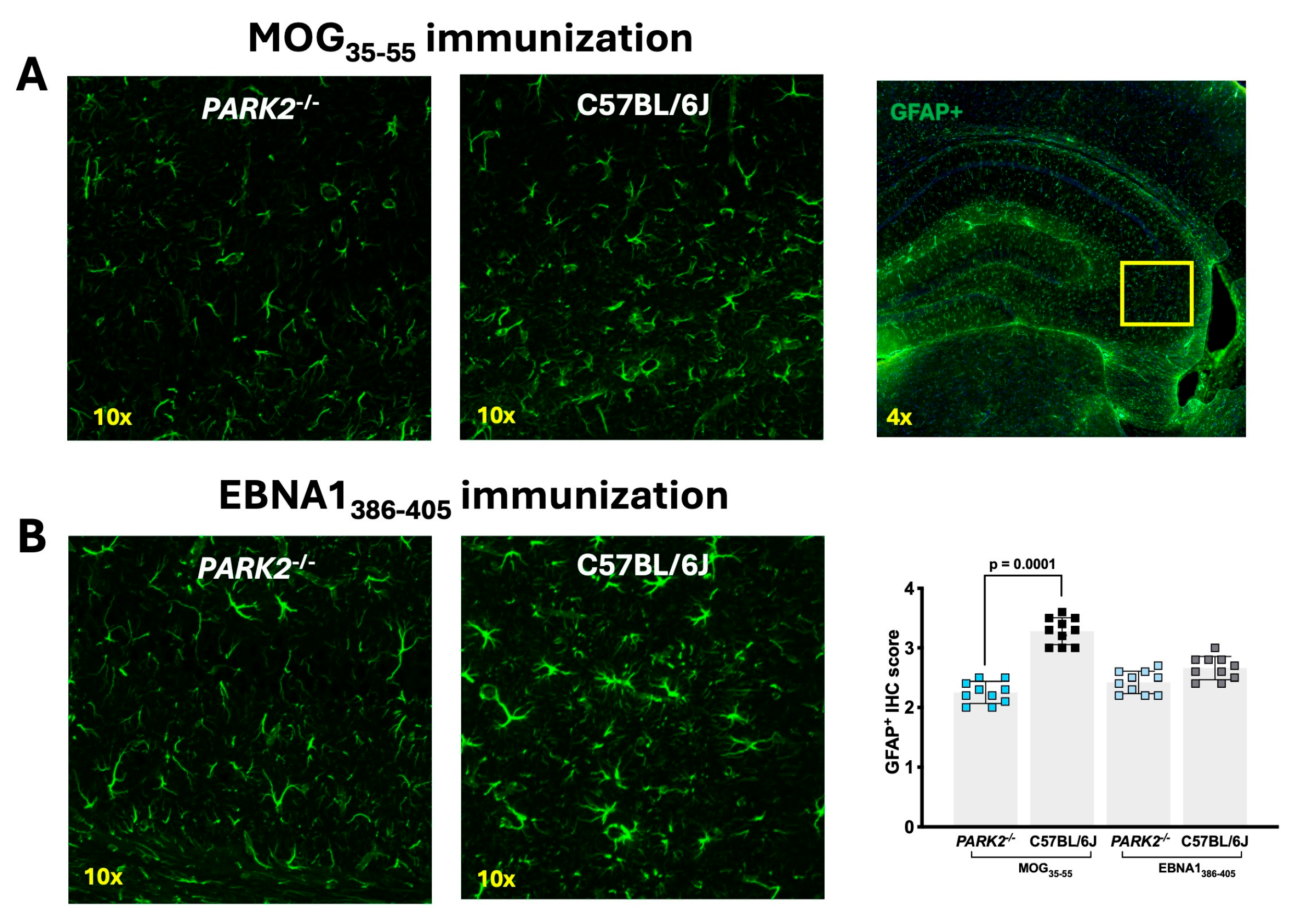
Notably, we observed a reduced number of GFAP
+ cells in the hippocampus of
PARK2-/- compared to wild-type mice, regardless of MOG
35-55 or EBNA1
386-405 immunization. While GFAP
+ cells in the hippocampus are primarily associate with astrocytes, they may also include neuronal precursor cells, as embryonic GFAP
+ cells in young adult mice predominantly differentiate into neurons rather than astrocytes [
22]. This reduction in GFAP
+ cells could potentially compromise the integrity of the blood-brain barrier, increasing the brain’s vulnerability to pathogens, and may also negatively affect neurological recovery.
Another difference is that we selected 9-month-old mice for this study. This age represents a middle-aged mouse, typically extending from 8 to 15 months [
23], corresponding approximately 35 years in humans. MS onset usually occurs in women between 20-40 years, with an average onset at 35 years. Moreover, a significant proportion of people with MS experience progression independent of relapse activity (PIRA) followed by post-inflammatory neurodegenerative processes over the years. The first attack of PIRA MS usually occurs at an average age of 32 years [
24].
We hypothesize that progressing mitochondrial dysfunction, associated with aging [
25], and EBV infection could be pathological drivers in progressive forms of MS, transiently exacerbating pre-existing symptoms. To test this hypothesis, we require a chronic model of EAE, as our current model induces only a monophasic form of EAE. Additionally, we need to investigate the presence of EBV markers by directly analyzing body fluids from patients with PIRA or progressive forms of MS.
Unbalanced mitochondrial activity is involved in inflammation in several neurological diseases [
26]. It is important to note that our studies used
PARK2-/- mice, which have mutations related to Parkinson’s disease [
11]. Despite exhibiting different clinical profiles, common mechanisms related to neurodegeneration, such as mitochondrial dysfunctions, are observed in patients with Parkinson ‘disease and MS, suggesting converging pathogenic pathways of neurodegeneration. Several cases of co-occurrence of PD after diagnosis of MS have been reported [
27], including a patient with early-onset Parkinson’s disease and a heterozygous PARK2 mutation who after 8 years developed primary progressive MS [
28]. Moreover, the detection of significantly increased levels of Parkin protein in the peripheral blood and cerebrospinal fluids of patients with MS [
29,
30] indicates a potential role for Parkin in the pathogenesis of MS.
Abnormalities in mitochondria are related to dysfunctional response to infection [
31]. Conversely, EBV-encoded proteins during both the latency and lytic infection reduce autophagy, decrease intracellular reactive oxygen species, and modulate mitochondrial function, altering bioenergetics [
32]. Clinical and in-vitro evidences associates EBV to Parkinson’s disease and the occurrence of parkinsonism [
33], with virus-mediated cell-cycle dysregulation potentially initiating neurodegenerative processes [
34]. However, further studies are needed to clarify the precise role of EBV. For instance, one limitation of our study is that our data were obtained from experiments conducted on female mice. Although previously published data indicate no differences in the development of EAE between male and female
PARK2-/- mice [
13,
14], our findings are restricted to the monophasic EAE model during the effector phase of the disease. Given that in MS, sex differences influence disease pathogenesis, such as men accumulating disability more rapidly than women [
35], future research should focus on the recovery phase, utilizing progressive EAE models. In this context, there may be significant differences between male and female mice. Another area for investigation is the impact of mycobacterial components, such as CFA, on the development of EAE in
PARK2-/- mice. Literature indicates that CFA administration can induce mild neuroinflammation [
36] and that immunization with mycobacterial components can modulate EAE development [
37]. Therefore, it would be interesting to evaluate the effects of CFA alone and other mycobacterial components in our model, particularly in the context of mitochondrial dysfunctions.
Despite areas requiring further clarification, our study demonstrated that alterations in mitochondria-mediated immune responses lead to increased inflammation triggered by the EBV antigenic component. This suggests that EBV peptides may exacerbate neuroinflammation through mechanism of molecular mimicry and mitochondrial dysfunction. These findings highlight the potential for developing targeted therapeutic strategies that significantly address these immune and mitochondrial pathways in neuroinflammatory diseases like MS.
4. Materials and Methods
4.1. Generation and Maintenance of PARK2-/- Mice
PARK2-/- middle-aged (9 months old) female mice (N=20 / group) were generated at Juntendo University [
38]. A targeting vector was constructed with 1.5- and 7-kb DNA fragments serving as the 5′ and 3′ homologous sequences, respectively. A negative selection cassette, DTA, encoding diphtheria toxin, was also included. The linearized targeting vector was transfected into TT2 ES cells, and clones were selected in G418. Screening for homologous recombination was done by Southern blotting, using a 5′ external probe and a neo-specific probe, confirming the desired recombination in the clones. ES cells from these clones were injected into C57BL/6J embryos, and chimeric offspring were crossed with C57BL/6J mice to achieve germline transmission, verified by Southern analysis with the 5′ probe. Heterozygous mice were interbred to produce homozygous knockout mice and wild-type littermate, which were sex-and aged-matched as controls. We chose female mice because previous experiments demonstrated that both knockout and wild-type young (8-12 weeks old) female mice have high susceptibility to EAE induction [
13]. Animals were housed in a pathogen-free facility, maintained under a 12-12-hour light/dark cycle. Procedures were approved by the Animal Experimental Committee of the Juntendo University Graduate School of Medicine (approved protocol no. 290238) and conducted in accordance with NIH and Juntendo University guidelines.
4.2. Immunization and Monitoring of PARK2-/- and Wild-Type Mice
Peptides EBNA1386-405 (sequence CSQSSSSGSPPRRPPPGRRPF), derived from the EBNA1 protein (UniProt accession number P03211), and MOG35-55 (sequence MEVGWYRSPFSRVVHLYRNGK) were chemically synthesized to a purity exceeding 95% by Synpeptide Co, Shanghai, China.
A cohort of PARK2-/- and wild-type mice were subcutaneously immunized with either 200 μg of EBNA1386-405 peptide or with 200 μg of the MOG35−55 peptide, both emulsified in incomplete Freund’s adjuvant (BD Diagnosis) supplemented with Mycobacterium tuberculosis H37Ra (Difco, Detroit, MI, USA) at a final concentration of 4mg/mL. Pertussis toxin (200 ng) (Difco) was administrated intraperitoneally to all mice at the time of immunization and 48 h post-immunization. All mice were monitored daily, and disease severity was assessed using the following criteria: 0, no clinical signs; 1, flaccid tail; 2, mild hind limb weakness; 3, severe hind limb weakness; 4, hind limb paralysis; 5, moribund state or death.
4.3. Assessment of T Cell Proliferation Using 3H-Thymidine Incorporation in MOG35-55 and EBNA1386-405 Immunized Mice
For the T cell proliferation assay, CD3+ T cells were isolated and purified by immunomagnetic positive selection from the spleens of mice immunized with either MOG35–55 or EBNA1386-405 using the MojoSort Mouse CD3 Cell Isolation Kit (BioLegend). T cells (4 x 105 cells/well) were cultured for 2 days with 50 μg/mL of the specific peptide. This was done in the presence of gamma-irradiated (3000 rad) accessory spleen cells, which were syngeneic to the responding T cells, at a concentration of 1 x 106 cells/ml. Cell proliferation during the last 18 hours was measured by determining the radioactivity of incorporated-3H-thymidine (PerkinElmer, Waltham, MA, USA) using a microplate scintillation counter (MicroBeta TriLux, PerkinElmer). The proliferative response was expressed as a stimulation index (counts per minute [cpm] of cells with test peptides/cpm of cells without stimulation) from triplicate determinations.
4.4. Cytofluorimetric Analysis of Spleen Cells
For cytofluorimetric analysis, spleen cell single-cell suspensions (1x106 cells) were labeled with live/dead markers (Zombie NIR Fixable Viability Kit, Biolegend, USA) for 15 min at room temperature, followed by a 10-minutes preincubation with FcBlock (FcγRII-RIII) on ice. Afterward, the cells were stained on ice for 20 min with fluorochrome-labeled monoclonal antibodies targeting CD4 (GK1.5), CD8a (53-6.7], CD19 (1D3), CD11c (N418), CD5 (53.7.3), Ly6G (1A8), CD11b (M1/70), CD115 (AFS98), I-A/I-E (M5/114.15.2), all purchased from Biolegend, or performed with appropriate isotype-matched controls. Sample acquisition (20000 events/sample) was performed on a BD FACSCelesta™ (BD Biosciences, USA), and data was analysis conducted using FlowJo software version 10.10.0 (FlowJo Company).
4.5. Cytokine Profiling Following Antigen-Specific T-Cell Stimulation
Spleen cells were isolated from all mice 20 days post immunization and incubated with either MOG
35-55 or EBNA1
386-405 for 48 hours, following previously established protocols [
13,
14]. Cytokine concentrations in the culture supernatants were then measured using a multi-analyte ELISArray kit (Qiagen, Hilden, Germany), according to the manufacturer’s instructions.
4.6. Histology and Immunohistochemical Analysis of Mice Tissues
Mice were transcardially perfused with PBS followed by 4% paraformaldehyde (PFA) in PBS. The brains and spinal cords were then post-fixed in 4% PFA and embedded for sectioning. Paraffin-embedded tissue sections were stained with Hematoxylin/Eosin to evaluate inflammation, quantified as the percentage of infiltrated area over the total spinal cord sections.
Immunohistochemistry and immunofluorescence were performed as previously described [
14], utilizing primary antibodies against CD3 (1:100), CD68 (1:500), glial fibrillary acidic protein (GFAP) (1:1000), and transmembrane protein 119 (TMEM119) (1:300), all obtained from Abcam, Tokyo, Japan. These were followed by incubation with appropriate biotinylated or fluorescent secondary antibodies. All samples were processed simultaneously to ensure comparability, and results were quantified using a previously established semi-quantitative scoring system [
14].
4.7. Statistical Analysis
Statistical analysis was conducted using GraphPad Prism version 10.2.3 (GraphPad Software, La Jolla, CA, USA). Clinical scores, body weights, and T cell proliferation data were analyzed using two-way analysis of variance (ANOVA). Flow cytometry, cytokine assays, and histological data were assessed with the Kruskal-Wallis non-parametric test followed by Dunn’s post hoc analysis. A p-value of less than 0.05 was considered statistically significant.