1. Introduction
Low back pain (LBP) is commonly classified as a lifestyle disease. According to the World Health Organization (WHO), low back pain (LBP) affected more than 619 million people worldwide in 2020, and the number of cases is expected to increase to 843 million cases by 2050, mainly due to population expansion and aging [
1]. LBP lasting more than 12 weeks is a chronic disease and is associated with the risk of sleep problems, depression and/or anxiety, and often disability. LBP is the leading cause of years lived with disability (YLD) and a serious challenge for primary health care worldwide [
2]. The treatment of LBP is very complex and should be comprehensive, including prevention, education, diagnosis and various treatment methods [
3]. The role of physiotherapy in the comprehensive treatment of LBP is very important.
Alves et al compared the clinical care standards for LBP in Australia, Canada and the United Kingdom. These three standards provide consistent recommendations in quality statements regarding imaging and patient education/counseling and self-management. However, the three clinical care standards differ in statements regarding psychological assessment, opioid analgesics, non-opioid analgesics and non-pharmacological therapies [
4].
LBP treatment can be divided into medication-based and non-pharmacological. It is impossible to imagine this treatment without physiotherapists. Jayani et al, based on a systematic review of the literature on physiotherapists’ attitudes and beliefs towards LBP, recently concluded that we still need to develop additional interventions to address attitudes and beliefs that will ultimately support the updating of the biopsychosocial model of care in LBP physiotherapy [
5].
Born in 1940, Dr. Kenzo Kase created in 1973 a tape and therapeutic taping technique that could support muscle and joint function without reducing or limiting range of motion. When developing the kinesio taping method (KT), he also took into account its impact on the lymphatic system. After two years of research on KT, applying Kinesio tapes to muscles, examining their elasticity, adhesion, and breathability, Dr. Kase developed the kinesio taping method (Kinesio® Taping) and taping patches (Kinesio Tex Tape), which are still used today and help in many diseases [
6].
The aim of our study was to evaluate the effectiveness of KT in patients suffering from (LBP). In our first article, we presented the effect of balance training with visual feedback (VFB) on posture and balance in patients suffering from sciatica [
7]. Now, we present the effect of KT on center of pressure (COP) sway, balance, gait, coordination, and pain in patients suffering from LBP.
2. Material and methods
Sixty patients suffering from chronic LBP for 6-24 months (54% women) aged 20 to 83 years (mean 54) met the inclusion and exclusion criteria (
Table 1). The study was initiated after obtaining permission from the local Bioethics Committee (Decision Number 5/16). The study was conducted in a sanatorium-hospital complex for rehabilitation purposes. According to the Quebec Task Force classification, all patients met the QTF 3 criteria, i.e. LBP with irradiation of the limb below the knee, QTF 4 = LBP with irradiation of the limb with neurological symptoms, QTF 6 = spinal cord root compression confirmed by imaging techniques such as CT or MRI, QTF 9 = surgery in the lumbar-sacral spine for more than 6 months [
8,
9]. Of the 60 patients included, 24 had undergone spine surgery. In the first group (KT), in addition to comprehensive stationary rehabilitation (approx. 3 hours per day) for three weeks (six days per week), kinesiotaping was used in the lumbar region (L1-L5). Two thin, cotton, porous, elastic KT tapes, 5 cm wide, were applied to the trunk muscles in a standing position with 75% tension, along the lumbar spine from the level of the L1 to L5 vertebrae, parallel on both sides of the spine, and maintained for four days. This procedure was performed three times during the stay. The break between individual applications was three days, during which the patient did not wear the tapes. In the second group (VBF), in addition to comprehensive rehabilitation, balance control training with visual feedback was used. For this purpose, the "tracking" program on the ALFA platform was used.
In the KT group, the average age was 56.5 years, and in the VBF group 55.2 years. In both groups, on the first and last day of their stay in the ward, a static and dynamic stabilometric test was performed using the ALFA platform. The static test consisted of assessing the so-called load distribution on the left and right limbs within 30 seconds. The patient stood on a special square plate with built-in pressure sensors. The device cooperated with a computer and was equipped with an LCD monitor. The result was given in percentages and helped assess the progress of the patients' rehabilitation based on the above assumptions (the patient loads less on the side where the pain occurs). The dynamic test, which lasted 30 seconds, consisted of using training, which in both groups also assessed the progress of rehabilitation. The dynamic test was performed using a program called "tracking". It was performed on the first and last day of their stay in the ward. In the second group - VFB - the "tracking" program was used for training. The subject stood on a stabilometric platform and observed a point on the monitor, the position of which reflected the projection of the center of gravity of his body on the base plane, scaled according to the way of loading the lower limbs applied during the exercise. The rehabilitated subject performed body movements, as a result of which the point reflecting the scaled projection of the center of gravity of his body followed the stimulus drawn by the software. The distance covered by the center of gravity of the body on the screen in following the escaping virtual point was recorded graphically and digitally (in centimeters). If both points coincided during the test, this was recorded as the "time of target residence". The result was presented as a percentage of the 30-second time. Static and dynamic (follow-up) stabilometry tests were conducted in the same room and at the same time. The conditions in the room were the same on both the first and last day of the study (temperature, light intensity, equipment setup). Each patient was tested in the same environment on both the first and last day. The VBF training lasted 10 minutes, was performed five times a week and lasted three weeks.
The outcome was measured using the Bohannon one-leg stance test, the Functional Ambulatory Category (FAC) scale, the Podsiadło and Richardson Timed Up and Go (TUG) scale [
10,
11,
12], the Schober lumbar spine mobility assessment, the Lasegue sign, the examination of neurological deficit symptoms and self-assessment of pain using the Visual Analogue Scale (VAS) [
13].
4. Discussion
Despite the initial skepticism, the use of KT has continued to grow and is now widely used, especially in musculoskeletal disorders and injuries. In 2013, Kalron and Bar-Sela, based on a systematic review of the effect on musculoskeletal disorders, found moderate evidence for an immediate reduction in pain when wearing KT. However, there was no support for any long-term effect. Further research is clearly needed [
14].
Here are some reports on the effects of KT on LBP. The first systematic review of KT for chronic LBP was published in 2016 by Nelson. She found five studies with 306 participants that met the inclusion criteria; the methodological quality of the included RCTs was good. Moderate evidence suggests that KT, either as a stand-alone treatment or in combination with another treatment, is not more effective than conventional physiotherapy and exercise in improving pain and disability outcomes. Limited evidence suggests that KT is more effective than sham taping in improving range of motion (ROM) and global perceived effect (GPE) in the short term. The author concluded that KT does not replace traditional physiotherapy or exercise, but may be most effective when used as an adjunct therapy, perhaps by improving ROM, muscle endurance, and motor control [
15].
Sheng et al. published a systematic review and meta-analysis of KT for the treatment of chronic nonspecific LBP in 2019. The quality of eight studies (totaling 530 participants aged 18–80 years, including 257 men and 273 women) that met the inclusion and exclusion criteria was moderate. Patients with chronic nonspecific LBP in the KT group achieved better pain relief and improved daily activities than those in the control group. The authors concluded that KT, alone or in combination with other general physical therapies, is superior to other general therapies or placebo patches in the treatment of chronic nonspecific LBP, providing greater pain relief and improved daily activities [
16].
Another systematic review and meta-analysis were presented in the same year by Li et al. They found a total of 10 articles with 627 participants: 317 in the KT group and 310 in the control group. While KT was not superior to placebo patching in reducing pain, neither alone nor in combination with physiotherapy, it was able to significantly improve disability compared with placebo patching. Authors’ conclusion: because KT seems to be convenient to use, it may be used in people with chronic LBP in some cases, especially when patients could not obtain other physiotherapy [
17]. Another systematic review and meta-analysis on the same topic presented also in 2019 by Luz Júnior et al. identified 11 RCTs (pooled n = 743). Very low to moderate quality evidence showed that KT was not superior to any other intervention for most outcomes assessed in patients with chronic non-specific LBP. The authors found no evidence to support the use of KT in clinical practice in patients with chronic nonspecific low back pain. Level of evidence: 1 [
18].
The first systematic review of the literature on CoP deviation as a measure of balance performance in patients with nonspecific LBP compared with healthy controls was published in 2011 by Ruhe et al. Sixteen articles met the inclusion criteria. The majority of articles (14/16, 88%) found that patients with nonspecific LBP had increased mean CoP velocity and overall deviation compared with healthy controls. This was statistically significant in most studies (11/14, 79%). Increased anteroposterior sway was also observed in patients with LBP. Patients with LBP exhibited greater postural instability than healthy controls, as evidenced by larger CoP deviations and higher mean velocity. While reduced postural stability in LBP patients appears to be additionally related to the presence of pain, it does not seem to be related to the exact location and duration of pain. No correlation could be identified between pain intensity and the magnitude of CoP deviations [
19].
Recently (2024) Sung and Lee reported on postural control and trunk stability in sway parameters in adults with and without chronic low back pain. Twenty-six patients with LBP and 39 control subjects participated in the study. The postural sway ranges, COP/COG (center of gravity) sway, and sway speeds (calculated by dividing the path length by the time in the anteroposterior (AP) and mediolateral (ML) directions within 10 s) were analyzed in three unilateral standing trials. A significant group interaction was observed in the difference in sway range after repeated trials. Regarding COG sway range: significant group interactions were shown in both directions and repeated trials. The authors concluded that the LBP group showed reduced ML sway speeds to increase trunk stability in the first two trials. The COG results highlighted the potential use of trunk strategies in increasing postural stability and optimizing neuromuscular control during unilateral stance [
20].
Jassi et al. reported in 2021 the results of star-shaped KT (four intersecting tapes) compared with sham KT and minimal intervention (MI) on pain intensity and postural control in 120 individuals with chronic LBP aged 18–60 years. The primary outcome measures were pain intensity and mean CoP sway velocity, and disability score (Oswestry Disability Index) was a secondary outcome. Results: Pain intensity was significantly lower in the star-shaped KT group than in the MI group immediately after the intervention and on the seventh day of the intervention. No significant differences were observed between groups in mean CoP sway velocity and disability score at any of the follow-up periods. Author’s conclusions: There was no significant effect of the star-shaped KT intervention on pain intensity and postural control in individuals with LBP compared with MI or sham KT. The results of this study suggest that the benefits of KT are more likely to be attributed to contextual factors than to specific taping parameters [
21]. The authors also wondered about the pain-relieving mechanism of KT – it may lift the skin of the joint or muscle of interest, thus allowing for better circulation and lymphatic drainage. It works by relaxing the tension of sensory receptors. Regarding differences in the mechanism of musculoskeletal disability, they cited the work of Bagheri et al. (2018), according to which KT may work by supporting and increasing the electrical activity of muscles. They included 20 physically inactive healthy male participants aged 22–45 years. Only men were preferred because the excitability of motor neurons could be modulated by regular exercise and could be influenced during the luteal phase. The five experimental sessions included: control without KT or Eutectic Mixture of Local Anesthetics (EMLA); EMLA only; kinesiology tape only; sham tape only; and kinesiology tape and EMLA treatment. H-reflex parameters were facilitated by kinesiology tape with and without EMLA; however, EMLA inhibited H-reflex parameters in both the soleus and lateral gastrocnemius muscles. Sham tape did not change the H-reflex recruitment curve parameters. The statistical model showed a significant difference between KT and sham tape sessions and control sessions, between KT-EMLA and EMLA, and between KT-EMLA and control session. Author's conclusions: KT facilitates muscle activity, and the mechanism underlying the soleus motor neuron pool involves cutaneous receptors [
22].
Recently, Tran et al. published a systematic review and meta-analysis of the effectiveness of KT compared with other treatments for musculoskeletal disorders. A total of 36 studies were included in the quantitative analysis. KT improved both pain and disability when applied to any body region. Within the first five days of treatment, KT significantly reduced pain in all body regions and also after four to six weeks of treatment. When applied to disability in patients with LBP, KT significantly reduced disability within five days of treatment. Furthermore, KT showed improvement in disability in all body regions after four to six weeks of treatment. According to the authors, these findings support KT as an adjuvant to other treatments for musculoskeletal disorders [
23].
It is well known that individuals with LBP may have poorer motor control compared to their healthy counterparts. Ge et al. published a systematic review and meta-analysis in 2019 on the impact of LBP on balance in older adults. Thirteen case-control studies comparing balance parameters in individuals with LBP and healthy individuals were included. The experimental group (LBP) was found to be associated with a significantly larger CoP area, faster CoP sway velocity in the anteroposterior and mediolateral directions, longer anteroposterior path, slower walking speed, and longer TUG time than the control group. Conclusions: These results showed that balance was impaired in older adults with LBP [
24].
The biomechanics of the trunk and lower limbs during walking and running are frequently assessed in people with LBP. It can be expected that LBP affects both qualitative and quantitative gait parameters. Smith et al. published a systematic review and meta-analysis of walking in people with LBP in 2022. Ninety-seven studies were included. Compared with people with a normal spine, people with persistent LBP walked more slowly and had a shorter stride. There were no differences in the amplitude of movement of the thoracic or lumbar spine, pelvis, or hips in people with LBP. There were no consistent differences in running biomechanics between groups. Author's conclusion: There is moderate to strong evidence that people with persistent LBP show differences in gait compared with people with a normal spine [
25].
Pain is the primary cause of suffering for the patient. LBP encompasses a spectrum of different types of pain (e.g., nociceptive, neuropathic, and nociplastic or nonspecific pain), which often overlap. Various instruments have been developed to assess two key dimensions of pain experience—pain intensity (how much the person suffers) and pain impact (how much the person suffers). The most popular are: Visual Analogue Scale (VAS) [
13], Numerical Rating Scale (NRS), McGill Pain Questionnaire (1972) modified to a short form (1987), Aberdeen Low Back Pain Scale (1994), and von Korff Graded Chronic Pain Scale (1992) modified in 2000 [
26,
27,
28,
29,
30,
31].
The best measure of outcome in LBP treatment seems to be disability assessment. Recently, Chmielewski and Wilski described the psychometric properties of five of the most popular and well-known measures currently used to assess disability in LBP: Oswestry Disability Index (ODI), Roland-Morris Disability Questionnaire (RMDQ), Quebec Back Pain Disability Scale (QBPDS), Low Back Outcome Score (LBOS), and Low Back Pain Rating Scale (LBPRS) [
32,
33]. Roland-Morris Disability Questionnaire (RMDQ) can also be considered a quality of life questionnaire [
34,
35].
The primary method of comprehensive rehabilitation is exercise. Hayden et al conducted a systematic review of the Cochrane database of exercise therapy for chronic low back pain. They found 249 exercise treatment trials. Sixty-one percent of the studies (151 trials) tested the effectiveness of two or more different types of exercise therapy, and 57% (142 trials) compared exercise therapy with a comparator without exercise. The mean age of the study participants was 43.7 years, and a mean of 59% of the study population was women. Most of the trials were considered at risk of bias, including 79% at risk of performance bias because of difficulties in blinding exercise therapy. Finally, the authors concluded that there was moderate-certainty evidence that exercise is probably effective for treating chronic low back pain compared with no treatment, usual care, or placebo for pain. The effect of exercise treatment compared with no treatment, usual care, or placebo comparisons was small for functional limitations, failing to meet our threshold for a minimally clinically important difference. Exercise also improved pain (low-certainty evidence) and functional limitation scores (moderate-certainty evidence) compared with other conservative treatments; however, these effects were small and not clinically significant when all comparisons were considered together. Subgroup analyses suggested that exercise therapy was probably more effective than advice or education or electrotherapy alone, but no differences were observed for manual therapy treatments [
36].
Nwodo et al conducted a review of reports of core stability exercises compared with conventional exercises for the treatment of chronic LBP. Core stability exercises (CSE) have gained popularity in recent years, but there is a lack of consensus on the best exercise treatment. A total of 14 RCTs were included in the analysis. The data indicated that core stability exercises were superior to conventional exercises for short-term pain relief. Ten studies included self-reports of specific back functional status, and compared with conventional exercises, core stability exercises resulted in significant improvements in function. The authors concluded that compared with conventional exercises, core stability exercises were more effective in reducing pain and improving physical function in people with CLBP in the short term, although only two studies conducted post-intervention follow-up assessments [
37].
Salavati et al. enrolled 40 patients with chronic LBP in a randomized trial of stabilization exercises (SE) or a control group. Both groups received 12 sessions of routine physiotherapy for four weeks. The SE group also received intensive stabilization exercises. Balance (referring to the overall (OSI), anteroposterior (APSI), and medial-lateral stability (MLSI) indices) and functional disability were assessed using the Biodex Balance System with open and closed eyes. Both groups effectively demonstrated improved stability indices and functional abilities, as well as reduced pain intensity. The SE protocol made patients less dependent on vision, possibly due to improved stability. Since pain reduction did not differ between groups, the greater functional improvement in the SE group cannot be simply interpreted as pain interference and may be related to the patients’ postural control abilities [
38].
Table 1.
General characteristics of the subjects.
Table 1.
General characteristics of the subjects.
| |
Group KT |
Group VBF |
| n |
% |
n |
% |
| Gender |
Females |
16 |
27% |
16 |
27% |
| Men |
14 |
23% |
14 |
23% |
| Age (years) |
20-83 |
36-80 |
| Mean age (mean±SD) |
53,9±14,65 |
55,2±13 |
| Body lenght (mean±SD) cm |
170,10±19,59 |
169,17±7,18 |
| Body mass (mean±SD) |
79,53 |
80,37±15,42 |
| BMI (average) |
27,49 |
28,08 |
Table 2.
COP sway and coincidence with moving point.
Table 2.
COP sway and coincidence with moving point.
| |
Group KT Group VBF |
| Parameter |
Before
intervention |
After
intervention |
P value |
Before
intervention |
After
intervention |
P value |
COP sway (cm)
Eyes open |
175.53 |
216.96 |
0.001 |
216.19 |
229.31 |
0.14 |
| Execution time (%) |
16.37 |
30.50 |
0.00002 |
18,93 |
36.93 |
0.00001 |
Table 3.
Distribution of limb loads and standing time on one leg with eyes open .
Table 3.
Distribution of limb loads and standing time on one leg with eyes open .
| |
Group KT Group VBF |
| Parameter |
Before
intervention |
After
intervention |
P value |
Before
intervention |
After
intervention |
P value |
Limb load distribution
L/R leg (%) |
L:49.93
R:50.07 |
L:50
R:50 |
0.69 |
L:49.97
R:50.03 |
L:49.40
R:50.60 |
0.21 |
| Standing time (s) on left leg |
8.48 |
12.92 |
0.000002 |
6.04 |
9.62 |
0.000002 |
| Standing time (s) on right leg |
8.53 |
13.16 |
0.000003 |
6.49 |
10.75 |
0.000002 |
Table 4.
Changes of lumbar spine mobility (Schober), Laségue`s sign, Functional Ambulatory Category (FAC), Timed Up and Go test (TUG) and VAS after intervention.
Table 4.
Changes of lumbar spine mobility (Schober), Laségue`s sign, Functional Ambulatory Category (FAC), Timed Up and Go test (TUG) and VAS after intervention.
| |
Group KT Group VBF |
| Parameter |
Before
intervention |
After
intervention |
P value |
Before
intervention |
After
intervention |
P value |
| Schober (cm) |
2.85 |
4.28 |
0.00001 |
3.17 |
4.25 |
0.00003 |
| Laségue L |
53.87° |
69.20° |
0.000003 |
52.03° |
67.50° |
0.000003 |
| Laségue P |
55.17° |
68.60° |
0.000002 |
55.37° |
69.90° |
0.000002 |
| FAC |
4.83 |
4.97 |
0.067 |
4.60 |
4.90 |
0.01 |
| TUG sec. |
13.40 |
10.28 |
0.000004 |
14.24 |
11.35 |
0.00003 |
| mean VAS |
5.40 |
3.10 |
0.00001 |
5.87 |
3.50 |
0.00001 |
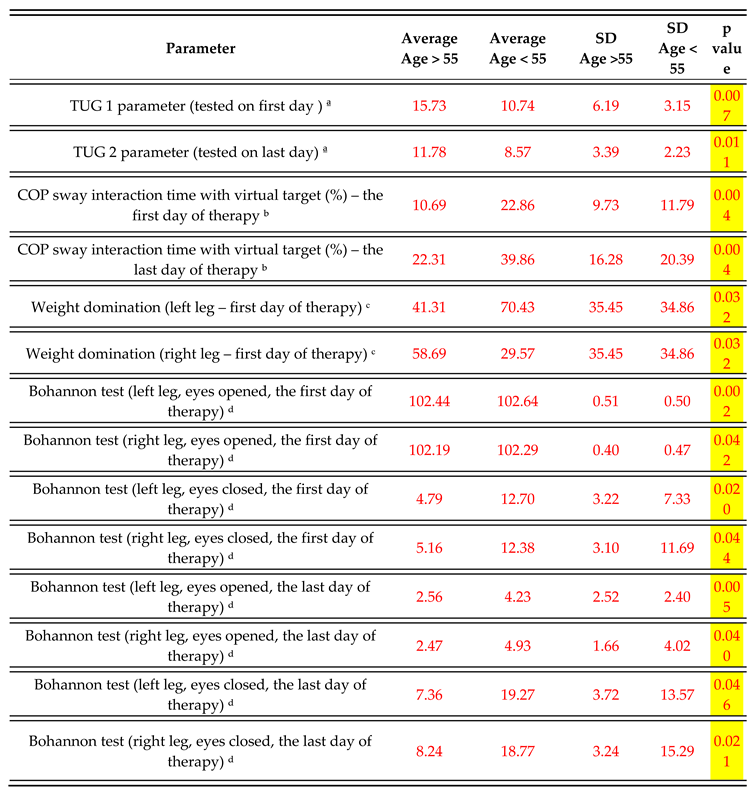
Table 5.
Mann-Whitney U test for the "Age" variable in group KT. Mann-Whitney U test for the "Age" variable in the research group.
Table 5.
Mann-Whitney U test for the "Age" variable in group KT. Mann-Whitney U test for the "Age" variable in the research group.
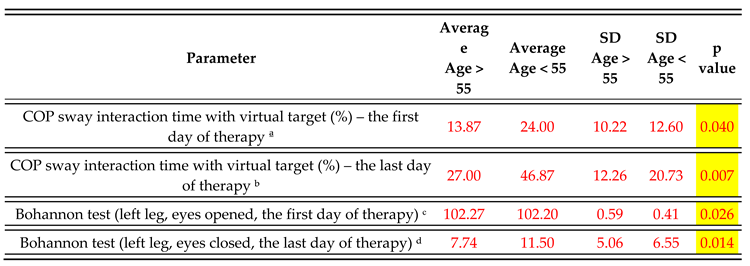
Table 6.
Mann-Whitney U test for the "Age" variable in group VBF.
Table 6.
Mann-Whitney U test for the "Age" variable in group VBF.