Submitted:
28 August 2024
Posted:
30 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Subjects
4.2. Characteristics of the Mothers and Their Offspring
4.3. Maternal Plasma Collection
4.4. Umbilical Cord Plasma Collection
4.5. Placental Sample Collection
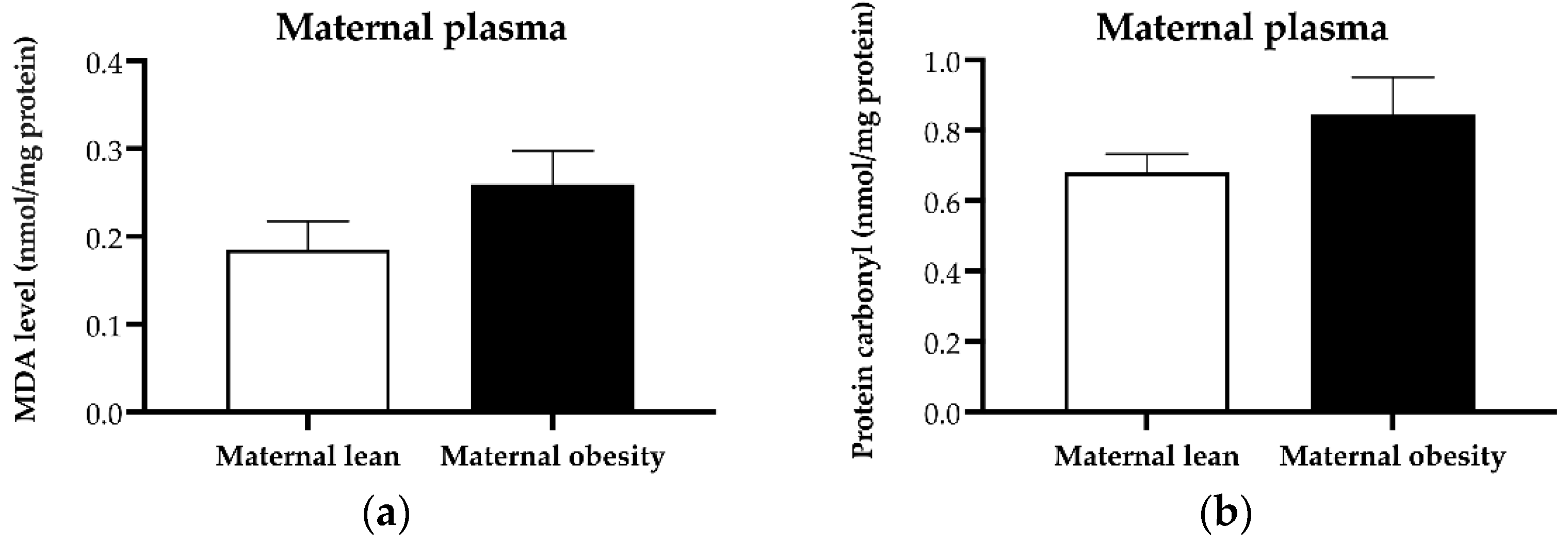
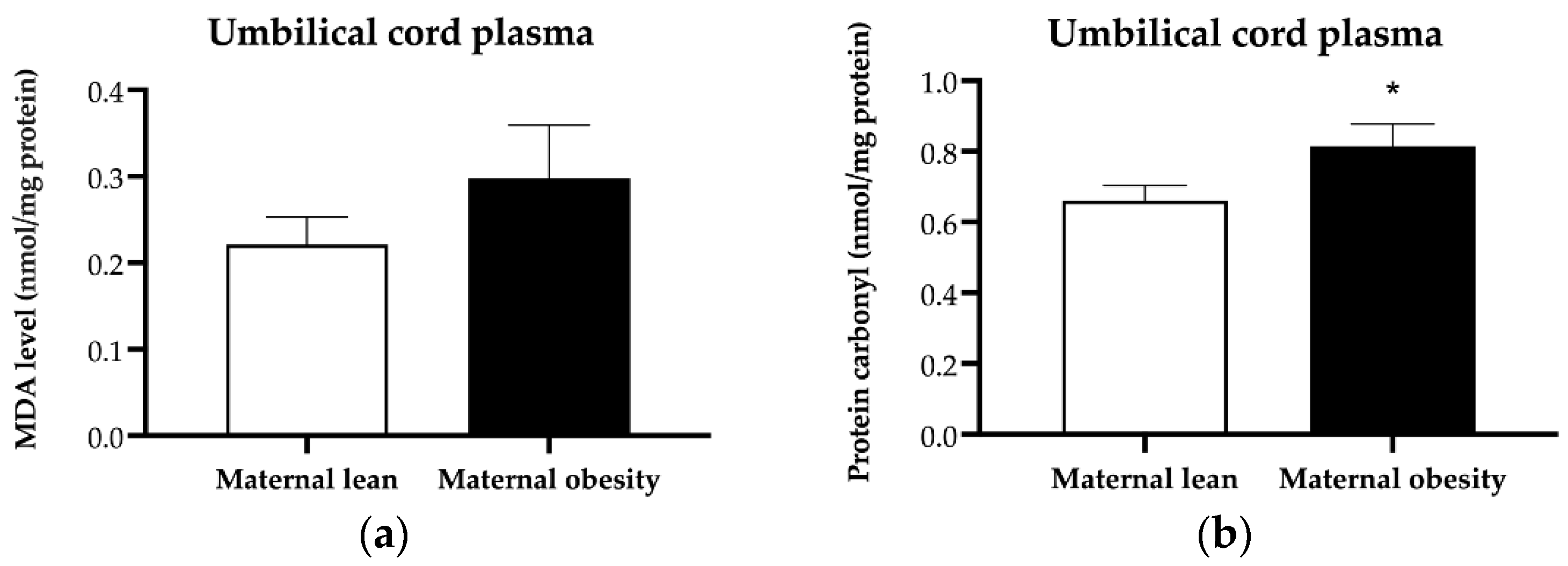
4.6. Assessment of Plasma and Placental MDA
4.7. Assessment of Plasma and Placental Protein Carbonyl
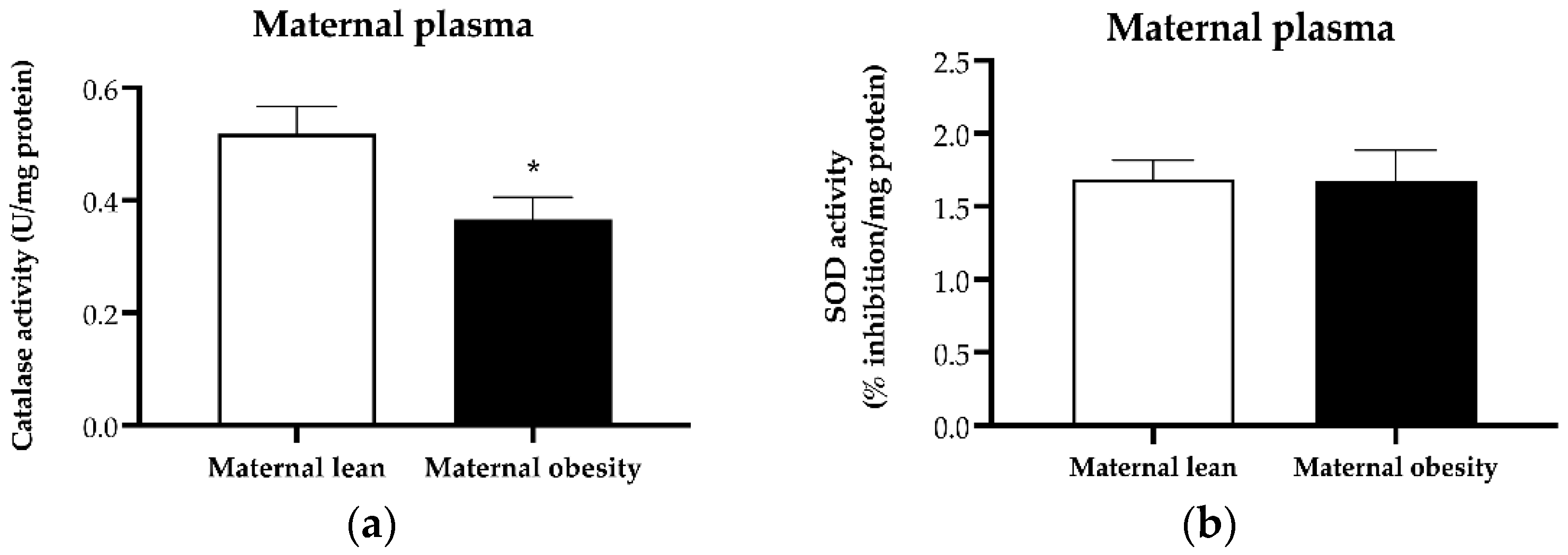
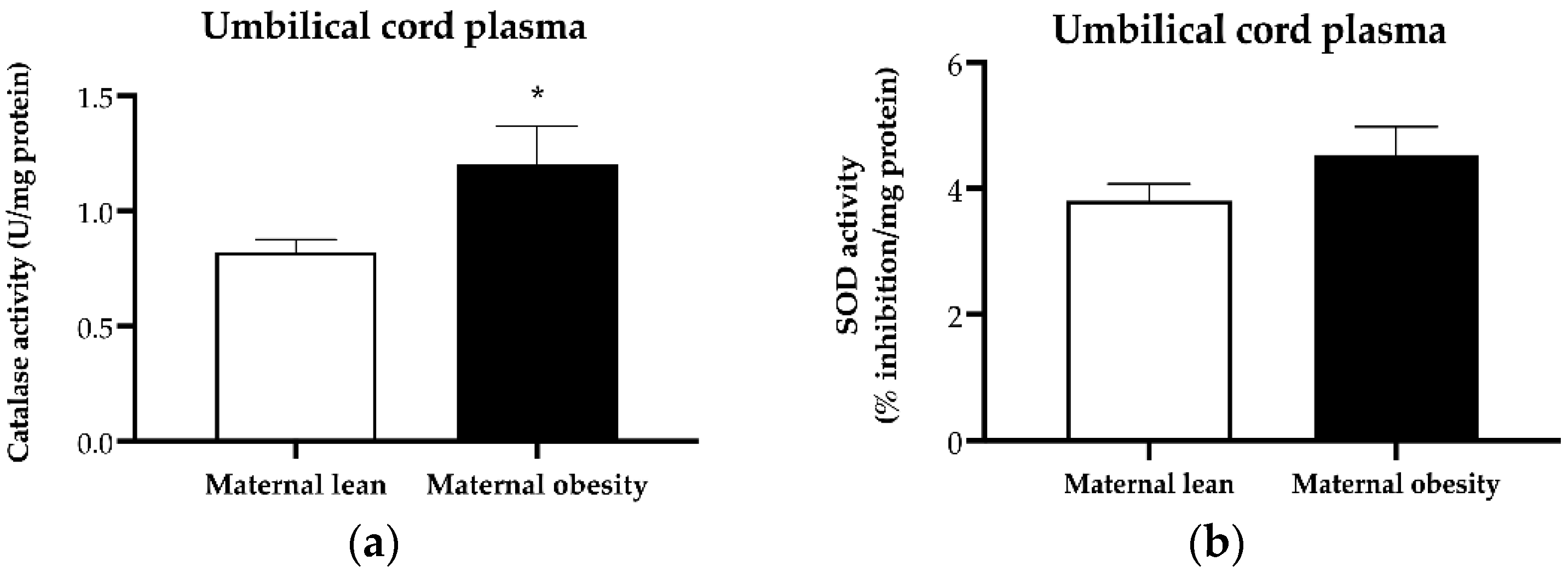
4.8. Assessment of Plasma Catalase Activity
4.9. Assessment of Plasma SOD Activity
4.10. Assessment of Plasma Protein Content and Lipids
4.11. Placental Protein Extraction and Expression Analysis
4.12. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tauqeer, Z.; Gomez, G.; Stanford, F.C. Obesity in Women: Insights for the Clinician. J Womens Health (Larchmt) 2018, 27, 444–457. [Google Scholar] [CrossRef]
- Poston, L.; Caleyachetty, R.; Cnattingius, S.; Corvalan, C.; Uauy, R.; Herring, S.; Gillman, M.W. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol 2016, 4, 1025–1036. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.C.; Powell, T.L.; Jansson, T. Placental function in maternal obesity. Clin Sci (Lond) 2020, 134, 961–984. [Google Scholar] [CrossRef] [PubMed]
- Lamothe, J.; Khurana, S.; Tharmalingam, S.; Williamson, C.; Byrne, C.J.; Lees, S.J.; Khaper, N.; Kumar, A.; Tai, T.C. Oxidative Stress Mediates the Fetal Programming of Hypertension by Glucocorticoids. Antioxidants (Basel) 2021, 10, 531. [Google Scholar] [CrossRef]
- Palaska, E.; Antoniou, E.; Tzitiridou-Chatzopoulou, M.; Eskitzis, P.; Orovou, E. Correlation between Breastfeeding, Maternal Body Mass Index, and Childhood Obesity. Epidemiologia (Basel) 2024, 5, 411–420. [Google Scholar] [CrossRef]
- Jovandaric, M.Z.; Babic, S.; Raus, M.; Medjo, B. The Importance of Metabolic and Environmental Factors in the Occurrence of Oxidative Stress during Pregnancy. Int J Mol Sci 2023, 24, 11964. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chen, Y.; Mao, X.; Du, M. Maternal obesity impairs fetal mitochondriogenesis and brown adipose tissue development partially via upregulation of miR-204-5p. Biochim Biophys Acta Mol Basis Dis 2019, 1865, 2706–2715. [Google Scholar] [CrossRef]
- Anam, A.K.; Cooke, K.M.; Dratver, M.B.; O'Bryan, J.V.; Perley, L.E.; Guller, S.M.; Hwang, J.J.; Taylor, H.S.; Goedeke, L.; Kliman, H.J.; et al. Insulin increases placental triglyceride as a potential mechanism for fetal adiposity in maternal obesity. Mol Metab 2022, 64, 101574. [Google Scholar] [CrossRef]
- Johns, E.C.; Denison, F.C.; Reynolds, R.M. The impact of maternal obesity in pregnancy on placental glucocorticoid and macronutrient transport and metabolism. Biochim Biophys Acta Mol Basis Dis 2020, 1866, 165374. [Google Scholar] [CrossRef]
- Santos-Rosendo, C.; Bugatto, F.; Gonzalez-Dominguez, A.; Lechuga-Sancho, A.M.; M, M.R.; Visiedo, F. Placental Adaptive Changes to Protect Function and Decrease Oxidative Damage in Metabolically Healthy Maternal Obesity. Antioxidants (Basel) 2020, 9, 794. [Google Scholar] [CrossRef]
- Martino, J.; Sebert, S.; Segura, M.T.; Garcia-Valdes, L.; Florido, J.; Padilla, M.C.; Marcos, A.; Rueda, R.; McArdle, H.J.; Budge, H.; et al. Maternal Body Weight and Gestational Diabetes Differentially Influence Placental and Pregnancy Outcomes. J Clin Endocrinol Metab 2016, 101, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Yanez Blanco, A.; Diaz-Lopez, K.M.; Vilchis-Gil, J.; Diaz-Garcia, H.; Gomez-Lopez, J.; Medina-Bravo, P.; Granados-Riveron, J.T.; Gallardo, J.M.; Klunder-Klunder, M.; Sanchez-Urbina, R. Diet and Maternal Obesity Are Associated with Increased Oxidative Stress in Newborns: A Cross-Sectional Study. Nutrients 2022, 14, 746. [Google Scholar] [CrossRef]
- Phuthong, S.; Reyes-Hernandez, C.G.; Rodriguez-Rodriguez, P.; Ramiro-Cortijo, D.; Gil-Ortega, M.; Gonzalez-Blazquez, R.; Gonzalez, M.C.; Lopez de Pablo, A.L.; Arribas, S.M. Sex Differences in Placental Protein Expression and Efficiency in a Rat Model of Fetal Programming Induced by Maternal Undernutrition. Int J Mol Sci 2020, 22, 237. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.L.; Mark, P.J.; Lewis, J.L.; Mori, T.A.; Keelan, J.A.; Waddell, B.J. Antioxidant defenses in the rat placenta in late gestation: increased labyrinthine expression of superoxide dismutases, glutathione peroxidase 3, and uncoupling protein 2. Biol Reprod 2010, 83, 254–260. [Google Scholar] [CrossRef]
- Stark, M.J.; Hodyl, N.A.; Butler, M.; Clifton, V.L. Localisation and characterisation of uncoupling protein-2 (UCP2) in the human preterm placenta. Placenta 2012, 33, 1020–1025. [Google Scholar] [CrossRef] [PubMed]
- Gnanalingham, M.G.; Williams, P.; Wilson, V.; Bispham, J.; Hyatt, M.A.; Pellicano, A.; Budge, H.; Stephenson, T.; Symonds, M.E. Nutritional manipulation between early to mid-gestation: effects on uncoupling protein-2, glucocorticoid sensitivity, IGF-I receptor and cell proliferation but not apoptosis in the ovine placenta. Reproduction 2007, 134, 615–623. [Google Scholar] [CrossRef]
- Malti, N.; Merzouk, H.; Merzouk, S.A.; Loukidi, B.; Karaouzene, N.; Malti, A.; Narce, M. Oxidative stress and maternal obesity: feto-placental unit interaction. Placenta 2014, 35, 411–416. [Google Scholar] [CrossRef]
- Evans, L.; Myatt, L. Sexual dimorphism in the effect of maternal obesity on antioxidant defense mechanisms in the human placenta. Placenta 2017, 51, 64–69. [Google Scholar] [CrossRef]
- Vanderlelie, J.; Venardos, K.; Clifton, V.L.; Gude, N.M.; Clarke, F.M.; Perkins, A.V. Increased biological oxidation and reduced anti-oxidant enzyme activity in pre-eclamptic placentae. Placenta 2005, 26, 53–58. [Google Scholar] [CrossRef]
- Wan, Y.; Chen, Y.; Wu, X.; Yin, A.; Tian, F.; Zhang, H.; Huang, X.; Wu, L.; Niu, J. Mediation effect of maternal triglyceride and fasting glucose level on the relationship between maternal overweight/ obesity and fetal growth: a prospective cohort study. BMC Pregnancy Childbirth 2023, 23, 449. [Google Scholar] [CrossRef]
- Mannino, A.; Sarapis, K.; Moschonis, G. The Effect of Maternal Overweight and Obesity Pre-Pregnancy and During Childhood in the Development of Obesity in Children and Adolescents: A Systematic Literature Review. Nutrients 2022, 14, 5125. [Google Scholar] [CrossRef] [PubMed]
- Francis, E.C.; Kechris, K.; Johnson, R.K.; Rawal, S.; Pathmasiri, W.; Rushing, B.R.; Du, X.; Jansson, T.; Dabelea, D.; Sumner, S.J.; et al. Maternal Serum Metabolomics in Mid-Pregnancy Identifies Lipid Pathways as a Key Link to Offspring Obesity in Early Childhood. Int J Mol Sci 2024, 25, 7620. [Google Scholar] [CrossRef] [PubMed]
- Grilo, L.F.; Tocantins, C.; Diniz, M.S.; Gomes, R.M.; Oliveira, P.J.; Matafome, P.; Pereira, S.P. Metabolic Disease Programming: From Mitochondria to Epigenetics, Glucocorticoid Signalling and Beyond. Eur J Clin Invest 2021, 51, e13625. [Google Scholar] [CrossRef] [PubMed]
- Castilla-Peon, M.F.; Medina Bravo, P.G.; Sanchez-Urbina, R.; Gallardo-Montoya, J.M.; Soriano-Lopez, L.C.; Coronel Cruz, F.M. Diabetes and obesity during pregnancy are associated with oxidative stress genotoxicity in newborns. J Perinat Med 2019, 47, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Shook, L.L.; James, K.E.; Roberts, D.J.; Powe, C.E.; Perlis, R.H.; Thornburg, K.L.; O'Tierney-Ginn, P.F.; Edlow, A.G. Sex-specific impact of maternal obesity on fetal placental macrophages and cord blood triglycerides. Placenta 2023, 140, 100–108. [Google Scholar] [CrossRef]
- Zhou, J.; Bai, J.; Guo, Y.; Fu, L.; Xing, J. Higher Levels of Triglyceride, Fatty Acid Translocase, and Toll-Like Receptor 4 and Lower Level of HDL-C in Pregnant Women with GDM and Their Close Correlation with Neonatal Weight. Gynecol Obstet Invest 2021, 86, 48–54. [Google Scholar] [CrossRef]
- Keleher, M.R.; Erickson, K.; Kechris, K.; Yang, I.V.; Dabelea, D.; Friedman, J.E.; Boyle, K.E.; Jansson, T. Associations between the activity of placental nutrient-sensing pathways and neonatal and postnatal metabolic health: the ECHO Healthy Start cohort. Int J Obes (Lond) 2020, 44, 2203–2212. [Google Scholar] [CrossRef]
- Leonard, S.A.; Rasmussen, K.M.; King, J.C.; Abrams, B. Trajectories of maternal weight from before pregnancy through postpartum and associations with childhood obesity. Am J Clin Nutr 2017, 106, 1295–1301. [Google Scholar] [CrossRef]
- Wang, L.; O'Kane, A.M.; Zhang, Y.; Ren, J. Maternal obesity and offspring health: Adapting metabolic changes through autophagy and mitophagy. Obes Rev 2023, 24, e13567. [Google Scholar] [CrossRef]
- Phengpol, N.; Thongnak, L.; Lungkaphin, A. The programming of kidney injury in offspring affected by maternal overweight and obesity: role of lipid accumulation, inflammation, oxidative stress, and fibrosis in the kidneys of offspring. J Physiol Biochem 2023, 79, 1–17. [Google Scholar] [CrossRef]
- Hernandez-Trejo, M.; Montoya-Estrada, A.; Torres-Ramos, Y.; Espejel-Nunez, A.; Guzman-Grenfell, A.; Morales-Hernandez, R.; Tolentino-Dolores, M.; Laresgoiti-Servitje, E. Oxidative stress biomarkers and their relationship with cytokine concentrations in overweight/obese pregnant women and their neonates. BMC Immunol 2017, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Hussain, T.; Murtaza, G.; Metwally, E.; Kalhoro, D.H.; Kalhoro, M.S.; Rahu, B.A.; Sahito, R.G.A.; Yin, Y.; Yang, H.; Chughtai, M.I.; et al. The Role of Oxidative Stress and Antioxidant Balance in Pregnancy. Mediators Inflamm 2021, 9962860. [Google Scholar] [CrossRef]
- Ballesteros-Guzman, A.K.; Carrasco-Legleu, C.E.; Levario-Carrillo, M.; Chavez-Corral, D.V.; Sanchez-Ramirez, B.; Marinelarena-Carrillo, E.O.; Guerrero-Salgado, F.; Reza-Lopez, S.A. Prepregnancy Obesity, Maternal Dietary Intake, and Oxidative Stress Biomarkers in the Fetomaternal Unit. Biomed Res Int 2019, 5070453. [Google Scholar] [CrossRef] [PubMed]
- Alfonso-Prieto, M.; Biarnes, X.; Vidossich, P.; Rovira, C. The molecular mechanism of the catalase reaction. J Am Chem Soc 2009, 131, 11751–11761. [Google Scholar] [CrossRef] [PubMed]
- Biri, A.; Onan, A.; Devrim, E.; Babacan, F.; Kavutcu, M.; Durak, I. Oxidant status in maternal and cord plasma and placental tissue in gestational diabetes. Placenta 2006, 27, 327–332. [Google Scholar] [CrossRef]
- Psefteli, P.M.; Morris, J.K.; Ehler, E.; Smith, L.; Bowe, J.; Mann, G.E.; Taylor, P.D.; Chapple, S.J. Sulforaphane induced NRF2 activation in obese pregnancy attenuates developmental redox imbalance and improves early-life cardiovascular function in offspring. Redox Biol 2023, 67, 102883. [Google Scholar] [CrossRef]
- Ruano, C.S.M.; Miralles, F.; Mehats, C.; Vaiman, D. The Impact of Oxidative Stress of Environmental Origin on the Onset of Placental Diseases. Antioxidants (Basel) 2022, 11, 106. [Google Scholar] [CrossRef]
- Xia, Y.; Zhai, X.; Qiu, Y.; Lu, X.; Jiao, Y. The Nrf2 in Obesity: A Friend or Foe? Antioxidants (Basel) 2022, 11, 2067. [Google Scholar] [CrossRef]
- Song, Y.R.; Kim, J.K.; Lee, H.S.; Kim, S.G.; Choi, E.K. Serum levels of protein carbonyl, a marker of oxidative stress, are associated with overhydration, sarcopenia and mortality in hemodialysis patients. BMC Nephrol 2020, 21, 281. [Google Scholar] [CrossRef]
- Negro, S.; Boutsikou, T.; Briana, D.D.; Tataranno, M.L.; Longini, M.; Proietti, F.; Bazzini, F.; Dani, C.; Malamitsi-Puchner, A.; Buonocore, G.; et al. Maternal obesity and perinatal oxidative stress: the strength of the association. J Biol Regul Homeost Agents 2017, 31, 221–227. [Google Scholar]
- Rocha, S.; Gomes, D.; Lima, M.; Bronze-da-Rocha, E.; Santos-Silva, A. Peroxiredoxin 2, glutathione peroxidase, and catalase in the cytosol and membrane of erythrocytes under H2O2-induced oxidative stress. Free Radic Res 2015, 49, 990–1003. [Google Scholar] [CrossRef]
- Fukai, T.; Ushio-Fukai, M. Superoxide dismutases: role in redox signaling, vascular function, and diseases. Antioxid Redox Signal 2011, 15, 1583–1606. [Google Scholar] [CrossRef] [PubMed]
- Arogbokun, O.; Rosen, E.; Keil, A.P.; Milne, G.L.; Barrett, E.; Nguyen, R.; Bush, N.R.; Swan, S.H.; Sathyanarayana, S.; Ferguson, K.K. Maternal Oxidative Stress Biomarkers in Pregnancy and Child Growth from Birth to Age 6. J Clin Endocrinol Metab 2021, 106, 1427–1436. [Google Scholar] [CrossRef] [PubMed]
- Redmer, D.A.; Milne, J.S.; Aitken, R.P.; Johnson, M.L.; Borowicz, P.P.; Reynolds, L.P.; Caton, J.S.; Wallace, J.M. Decreasing maternal nutrient intake during the final third of pregnancy in previously overnourished adolescent sheep: effects on maternal nutrient partitioning and feto-placental development. Placenta 2012, 33, 114–121. [Google Scholar] [CrossRef]
- Correia-Branco, A.; Keating, E.; Martel, F. Maternal undernutrition and fetal developmental programming of obesity: the glucocorticoid connection. Reprod Sci 2015, 22, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Mando, C.; Calabrese, S.; Mazzocco, M.I.; Novielli, C.; Anelli, G.M.; Antonazzo, P.; Cetin, I. Sex specific adaptations in placental biometry of overweight and obese women. Placenta 2016, 38, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Consultation, W.H.O.E. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar]
- Poasakate, A.; Maneesai, P.; Rattanakanokchai, S.; Bunbupha, S.; Tong-Un, T.; Pakdeechote, P. Genistein Prevents Nitric Oxide Deficiency-Induced Cardiac Dysfunction and Remodeling in Rats. Antioxidants (Basel) 2021, 10, 237. [Google Scholar] [CrossRef]
- Ramiro-Cortijo, D.; Calle, M.; Rodriguez-Rodriguez, P.; Pablo, A.L.L.; Lopez-Gimenez, M.R.; Aguilera, Y.; Martin-Cabrejas, M.A.; Gonzalez, M.D.C.; Arribas, S.M. Maternal Antioxidant Status in Early Pregnancy and Development of Fetal Complications in Twin Pregnancies: A Pilot Study. Antioxidants (Basel) 2020, 9, 269. [Google Scholar] [CrossRef]


| Parameter | Maternal lean | Maternal obesity | p-value |
|---|---|---|---|
| Maternal age at delivery (year) | 27.65 ± 0.85 | 30.30 ± 1.20 | 0.0779 |
| Gestational age at delivery (weeks) | 38.71 ± 0.21 | 38.81 ± 0.28 | 0.7744 |
| Pre-pregnancy weight (kg) | 52.56 ± 1.29 | 75.32 ± 1.79 *** | <0.0001 |
| Pre-pregnancy BMI (kg/m2) | 20.26 ± 0.45 | 29.40 ± 0.58 *** | <0.0001 |
| Weight at delivery (kg) | 66.90 ± 2.10 | 90.64 ± 2.22 *** | <0.0001 |
| Neonatal gender, male n (%) | 10 (50) | 11 (55) | 0.7575 |
| Neonatal birth weight (g) | 3083 ± 101 | 3327 ± 110 | 0.1103 |
| Neonatal length (cm) | 49.20 ± 0.57 | 49.21 ± 0.59 | 0.9898 |
| Placental weight (g) | 581.50 ± 28.02 | 701.50 ± 41.89 * | 0.0224 |
| Feto-placental ratio | 5.43 ± 0.19 | 4.87 ± 0.16 * | 0.0374 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





