1.Introduction
Although complete dentures (CDs) have several limitations, they are still used in the treatment of completely edentulous patients because they are non-invasive and cost-effective [
1,
2]. CD fabrication methods have remained largely unchanged for nearly 90 years [
3]. In the conventional compression molding technique, which is still widely used for CD fabrication, residual stresses generated during the packing stage are released when the material is removed from the flask. This release of stress causes resin shrinkage, leading to a poor fit for the denture base and displacement of artificial teeth [
3]. Fabricating a denture base with high accuracy by reducing fabricating errors is crucial for successful CD treatment [
2].
Recently, the development of dental technology and computer-aided design/computer-aided manufacturing (CAD-CAM) methods has simplified the fabrication process, improved the adaptation of dentures, and enabled the fabrication of identical sets of dentures [
1,
2,
4]. Prosthesis fabrication using CAD-CAM can be divided into subtractive and additive manufacturing techniques [
2,
5,
6]. Using CAD-CAM, CD can be fabricated by processing polymerized resin blocks using CNC-milling or three-dimensional (3D) printing, which involves the incremental filling of resins through light-polymerization [
1,
2,
5]. Moreover, 3D printing has multiple benefits, including its ability to fabricate objects with relatively complex shapes to high precision while reducing noise during fabrication and material waste [
5,
7]. Nevertheless, 3D printing is limited to the use of photo-curable resin materials. The post-processing stage often requires the removal of support structures, which can be labor-intensive. Additionally, the resins used in these processes are difficult to handle, can potentially cause skin irritation, and have a risk of inducing inflammatory responses following direct contact or inhalation. Moreover, these resins have a finite shelf and vat life, and they cannot undergo heat sterilization [
8,
9].
In dentistry, 3D printing is widely used to produce guides for implant surgery, prosthetic prostheses, and casts [
2,
10]. The primary 3D printing techniques employed for fabricating denture bases are stereolithography apparatus (SLA) and digital light processing (DLP), both adhering to the incremental method [
2,
11,
12]. These two additive manufacturing techniques involve stacking thin layers of resin in lines and planes, respectively [
13]. While several studies have compared the accuracy of these two printing methods for dental applications, no consensus has been reached regarding their superiority. Furthermore, most errors fall within the clinically acceptable range [
14,
15]. Meanwhile, Rouzé l'Alzit et al. suggested that the 3D printing method did not significantly impact the accuracy, rather they found that the size of the 3D-printed object could affect its accuracy. Hence, a large implant surgical guide was less accurate than a small one [
16].
In CDs, accurate denture base adaptation and stable occlusion are essential factors that determine the success or failure of treatment and can be achieved by minimizing the deformation of the denture base during the fabrication process [
7,
17,
18,
19]. In previous studies, the clinically acceptable range for adaptation of denture bases was <0.3 mm, whereas that for the vertical dimension increase due to resin tooth displacement of CD was <1 mm [
20,
21,
22,
23]. In addition, the linear deformation observed during the fabrication of the denture base using conventional methods reportedly ranges from approximately 0.45% to 0.9% [
2,
24]. Moreover, 3D-printed CDs showed higher patient satisfaction than those fabricated using conventional methods [
17] but showed lower tissue adaptation than CDs fabricated using the CNC milling method [
7,
20]. Yoon et al. compared the tissue adaptation of CD base fabricated using the DLP, milling, and pack-and-press methods and reported that there were no significant differences among the three methods [
25]. Davda et al. investigated the trueness and precision of copy dentures fabricated using the SLA and conventional methods and suggested that the polishing surface of copy dentures fabricated with the SLA method exhibited greater precision than those fabricated with either of the conventional methods [
26]. However, no clear consensus has been reached [
20]. The tissue and polished surfaces of 3D printing denture bases must have high accuracy for successful fabrication of CD; however, the evidence regarding the accuracy of the current 3D printing methods is limited [
2,
27].
Factors that can affect the accuracy of 3D-printed objects include the printable material, resolution of the printer, light intensity, direction and angle of printing, number of layers, software program, shrinkage between layers, amount of supporting structure, and post-processing procedures [
18,
27]. In addition, the resin output may sag as the build platform of the 3D printer moves upwards [
28]. Several studies have investigated the effects of build angle on 3D printing accuracy. Unkovskiy et al. compared the accuracy of 3D printed denture bases created using the SLA and DLP methods at build angles of 0°, 45°, and 90°. They reported a significant difference in accuracy based on the build angle when using the SLA method, while no such difference was observed with the DLP method [
12]. Rubayo et al. compared the effects of build angles on the accuracy of surgical templates when using the SLA method and reported that 0° and 45° build angles produced more accurate surgical templates than a 90° build angle [
29]. Tsai et al. compared the effects of 45° and 90° build angles on the accuracy of 3D-printed denture models and examined the effects of incorporating a reference model during the postpolymerization step. The 90° build angle showed a higher accuracy of 3D printing than the 45° build angle, and the use of a reference model in the postpolymerization step improved the 3D printing accuracy [
18]. Ko et al. evaluated the effects of build angle and layer height on the accuracy of 3D-printed orthodontic models and stated that there was a significant difference in accuracy. However, despite these differences, the errors remained within clinically acceptable limits [
30]. In an
in vitro study by Jin et al., which compared the tissue adaptation of denture bases printed at build angles of 90°, 100°, 135°, and 150°, there were no significant differences in the adaptation of the build angle [
28]. Charoenphol et al. reported that a 90° build angle for 3D printing the upper CD base resulted in the most accurate tissue surface in the peripheral/posterior palatal seal area. Moreover, 45° and 90° build angles produced better adaptation in the primary supporting area than a 0° build angle. However, no significant differences were observed in the total tissue surface [
9]. Yoshidome et al. reported that dentures fabricated using the SLA method exhibited better fitting accuracy compared to those fabricated using the DLP method. They also recommended using build angles of 45° and 225° to enhance the fitting accuracy of maxillary 3D-printed dentures [
31].
To our knowledge, studies examining the differences in denture base accuracy using detailed 3D printing methods are limited. Most existing studies have explored build angles at 45° intervals, specifically at 0°, 45°, and 90°. Conversely, in this study, we aimed to analyze the effects of finer angle differences by examining build angles at 30° intervals, specifically at 0°, 30°, 60°, and 90°. Particularly, no study has simultaneously assessed the accuracy of the tissue and polished surfaces of the denture base according to different build angles. Therefore, we aimed to investigate differences in the adaptation of tissue surfaces among 3D-printed denture bases produced at various build angles, as well as differences in the distances between the reference points on the polished surfaces. The null hypothesis was that there would be no differences in the adaptation of the tissue surfaces based on the build angle, nor any differences in the distances between reference points on the polished surfaces.
2.Materials and Methods
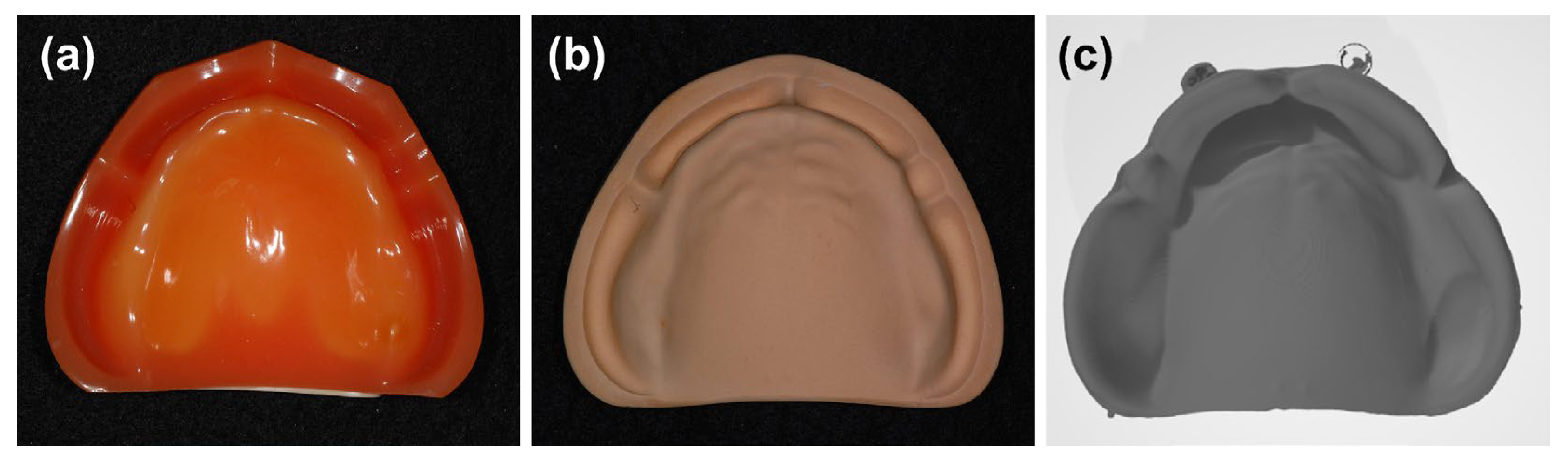
The impression of a Nissin dental model (EDE1001, Nissin, Kyoto, Japan), an edentulous maxilla model, was taken using a rubber impression material (Exadenture, GC, Tokyo, Japan). A plaster model was fabricated with type IV plaster (Fujirock EP, GC, Tokyo, Japan) using the mixing ratio and vacuum mixer provided by the manufacturer. Subsequently, the plaster model was scanned using a Freedom UHD 3D scanner (DOF Inc, Seoul, Republic of Korea) to obtain the standard tessellation language files representing the digital model of the edentulous maxilla. Exocad (Exocad GmbH, Darmstadt, Germany) was used for one-time CAD of the denture base according to the digital model. This ensured that the tissue surface of the CAD of the denture base was identical to that of the digital model. Then, the denture base was built using a 3D printer. The build angles were 0°, 30°, 60°, and 90°, and 15 denture bases were built for each build angle (
Figure 1).
CAD, computer-aided manufacturing
2.1. Fabrication of Denture Bases and Evaluation of Tissue Surface Adaptation
A Dentca denture base II (Dentca Inc., Torrance, CA, USA), a denture base resin, and an SLA 3D printer (Zenith U, Dentis, Daegu, Korea), which uses a blue laser and is operated by a proprietary slicing software, were used for 3D printing.
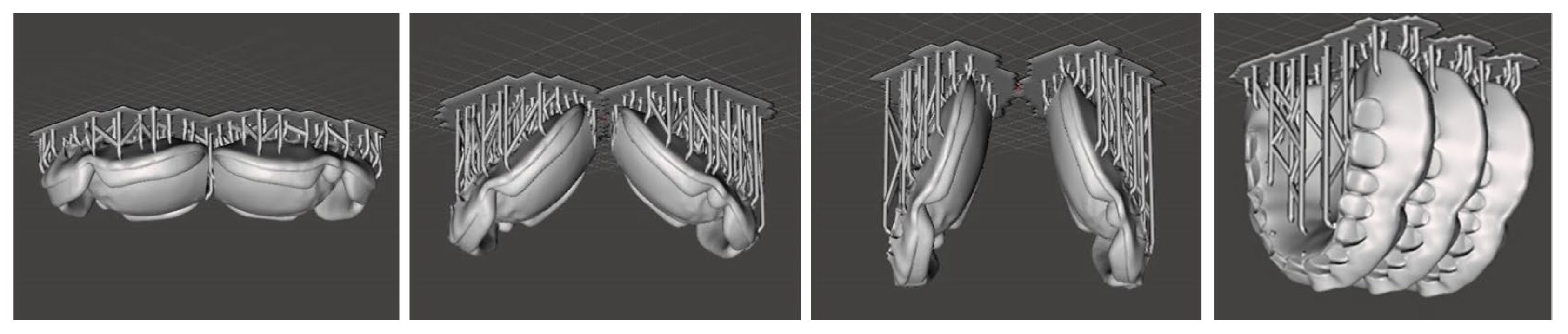
In SLA or DLP 3D printing, the build angle refers to the direction in which the object is thinly sliced during the printing process [
32]. In the present study, the build angles were 0°, 30°, 60°, and 90°, with 15 denture bases printed for each angle. The sliced layers were 100-µm thick. To minimize the effects of build platform position on the printed denture base, two denture bases were printed at the build platform center for 0°, 30°, and 60° each, while three were printed for 90° (
Figure 2).
The printed denture bases were carefully removed from the printing platform. After removal of the support, the denture bases were immersed in isopropyl alcohol for 5 min. They were washed under running water and dried; then, they underwent additional photopolymerization in a curing machine (ProCure, SprintRay, Los Angeles, CA, USA).
Subsequently, 3D scanning spray (Easy Scan, Alphadent, Goyang, Korea) was applied to the tissue surface of the denture bases, and a Freedom UHD 3D scanner was used to obtain the standard tessellation language file of the denture base tissue surface shape. Using Geomagic Control® (3D Systems, Rock Hill, SC, USA) software, a 3D best-fit alignment was conducted between the denture base tissue surface and the digital model of the edentulous maxilla model to calculate the root mean square error (RMSE).
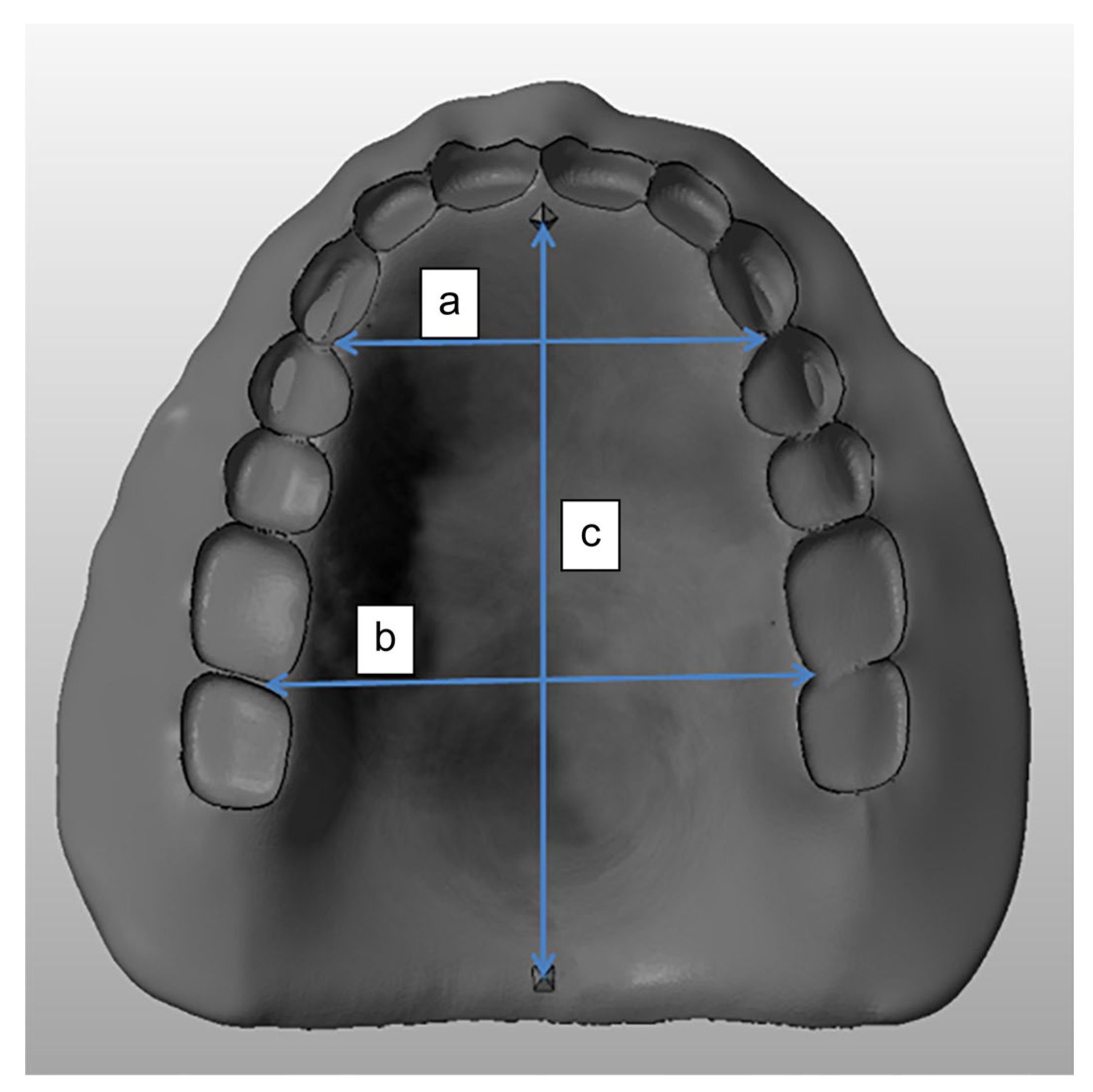
2.2. Setting Polished Surface Reference Points and Distance Measurements
The distances between the disto-palatal gingival papillae of the bilateral canines and those between the disto-palatal gingival papillae of the bilateral first molars were measured. The former was defined as the inter-canine width, and the latter as the inter-molar width. Additionally, two square pyramidal shapes were positioned on the mesio-palatal gingival area of the bilateral central incisors and on the midline of the denture base near the posterior border. The distance between these two pyramidal shapes was defined as the inter-anteroposterior (inter-AP) length (
Figure 3).
The distances were measured by three researchers using digital calipers (Absolute Digimatic, Mitutoyo, Japan), and the mean values were used. SPSS Statistics 18 (SPSS Corp., Chicago, IL, USA) software was used for statistical analysis. A Shapiro–Wilk test was used to assess normality and one-way analysis of variance to compare groups. The total sample size required was 40 when G-power 3.1 software (University of Dusseldorf, Dusseldorf, Germany) was used with a previous study`s [
33] effect size (0.65), significance level (0.05), and detection power (0.95). The Shapiro–Wilk test showed that the measured RMSE and distance between the reference points were normally distributed across all groups. A one-way analysis of variance was conducted to compare the mean values among the denture bases with different build angles.
4. Discussion
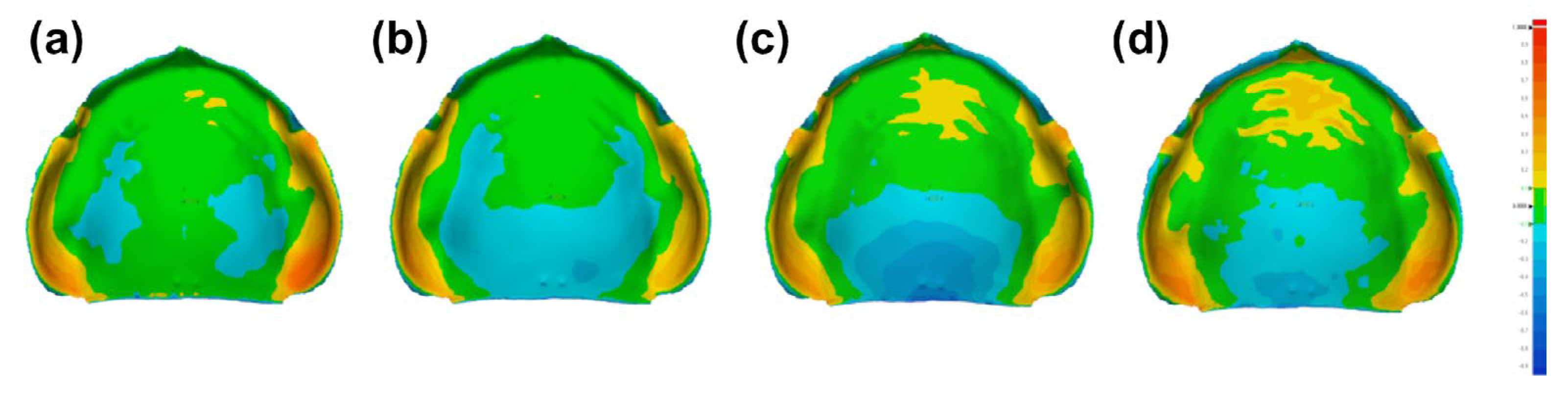
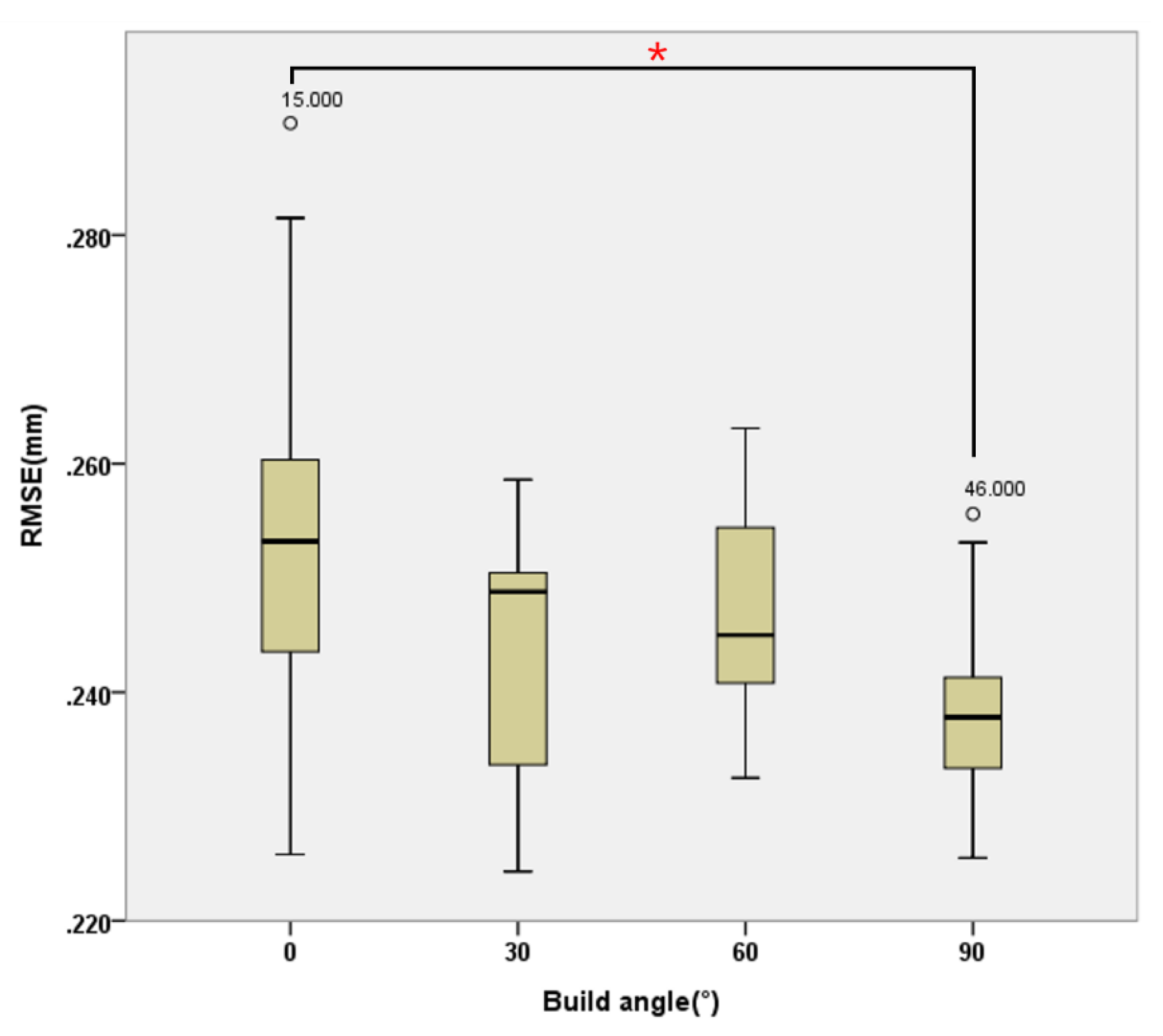
Based on our findings, we rejected the null hypothesis that there would be no differences in the adaptation of tissue surfaces according to build angle and that there would be no differences in the distances between the reference points on the polished surfaces. Our color difference map revealed a greater anterior–posterior variation than left–right variation across different build angles. As the build angle increased, there was a tendency for increased displacement between the digital model and the tissue surface, particularly at the posterior margin and anterior rugae region of the denture base. Significant differences were observed in the inter-AP length based on build angle, whereas no significant differences were found in the inter-canine and inter-molar widths. As described in the Introduction, this may be related to the number of layers required for each build angle and variations in total printing time [
18,
27]. In particular, the SLA 3D printer, which photopolymerizes resin by irradiating light along a straight line, was used in this study. SLA 3D printers require more printing time than DLP 3D printers that polymerize the resin in layers [
34]. In the present study, for the 0° build angle, an output of 237 layers required 2 h and 54 min. At 30°, an output of 431 layers required 3 h and 46 min. At 60°, an output of 600 layers took 4 h and 19 min. At 90°, it took 4 h and 20 min to output 662 layers. This trend suggests that as the build angle increases, both the number of layers and output time for CD base tend to increase correspondingly.
After the polymerization of each layer, the printed product is lifted. In this process, the product inside the resin solution might undergo tensile force due to the adhesive force generated between the product and polyvinyl chloride film or glass plate at the bottom of the resin vat. Lee et al. reported that lower viscosity resins achieve higher trueness in 3D-printed denture bases, which may be attributed to reduced tensile forces during the printing process [
33]. Therefore, it is hypothesized that as the number of layers increases, the potential exposure to tensile stress may correspondingly increase. Gravity also has effects on the printed product as the printing time increases [
29]. These two factors are thought to be the causes of discrepancies between the denture bases of different build angles. In our study, as the build angle increased, the number of layers and time for printing subsequently increased, leading to a greater risk of error. In denture bases with 30°, 60°, and 90° build angles, the posterior region, which is printed before other parts of the denture base, was subjected to tensile forces from the increasing number of layers and the effects of gravity during printing. This led to larger negative errors (misfits) compared to denture bases with a 0° build angle [
28,
34].
Interestingly, the 90° build angle exhibited a significantly lower RMSE compared to the 0° print angle. Despite localized large discrepancies at the 90° build angle, the smaller cross-sectional area of the slices may have contributed to a more uniform distribution of overall errors, resulting in a lower RMSE value. Although the color difference map indicates notable deviations in specific regions, the reduced cross-sectional area at the 90° build angle likely led to less cumulative error across the entire surface.
Consistent with previous studies, the mean RMSE was the smallest in 3D-printed prostheses with a build angle of approximately 90° [
12,
18,
35]. However, based on our color difference map, denture bases with a 90° build angle do not have clinically better tissue adaptation on the overall surface than denture bases of other build angles, similar to the results reported by Tsai et al. [
18]. This is primarily because the negative deviation at the posterior palatal seal region decreases the retention of the denture base. In contrast to our study, Jin et al. used a DLP 3D printer and adjusted the build angles by lifting the posterior part of the denture base; they showed clinically better tissue adaption at the posterior region of the denture base [
28]. However, across all build angles, the range of error values between the digital model and the denture base tissue surface was as follows: RMSE ranged from 220 to 290 µm, mean positive deviation (impingement) ranged from 130 to 220 µm, and mean negative deviation (misfit in space) ranged from −227 to −133 µm. All these values were within the clinically acceptable range [
20].
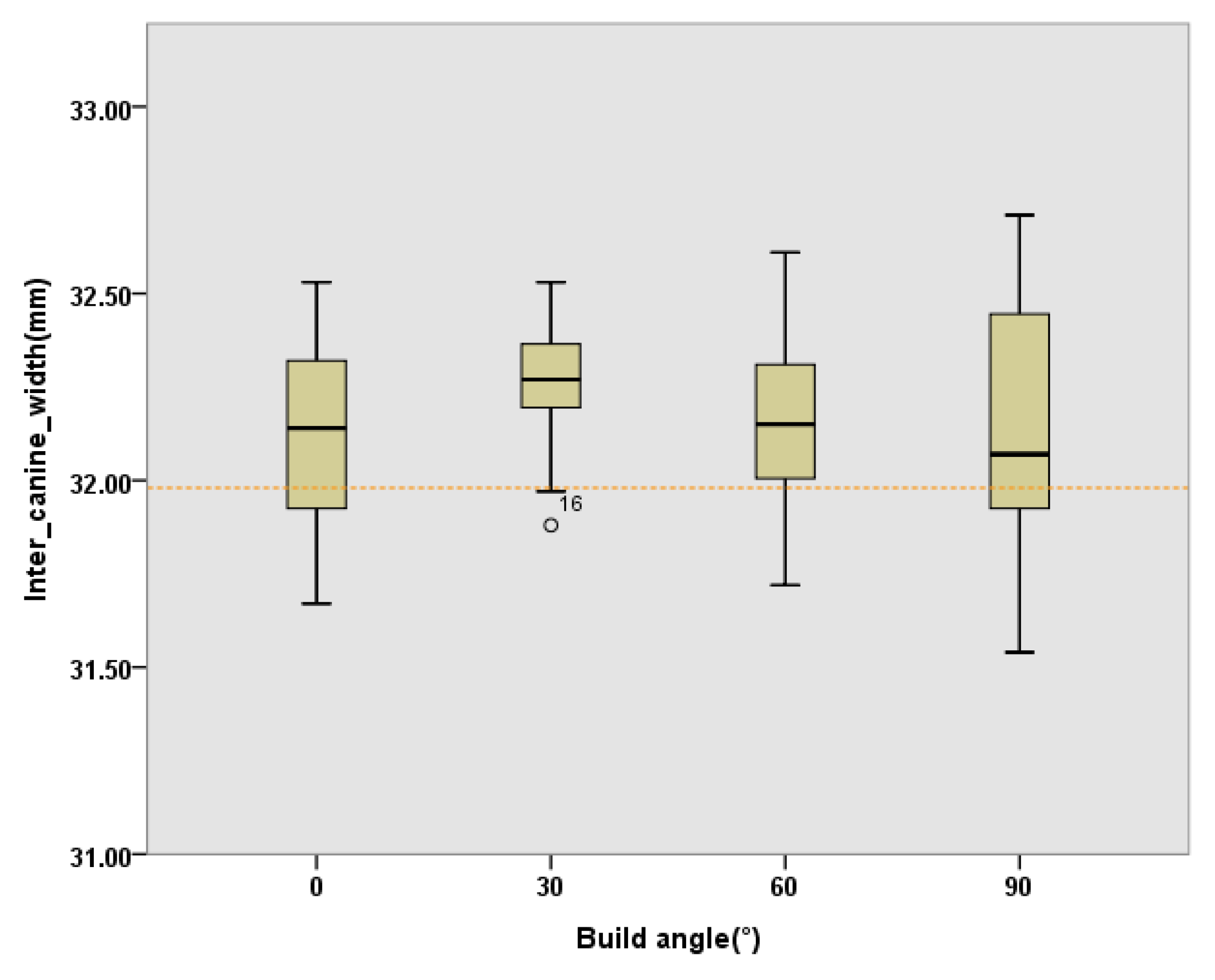
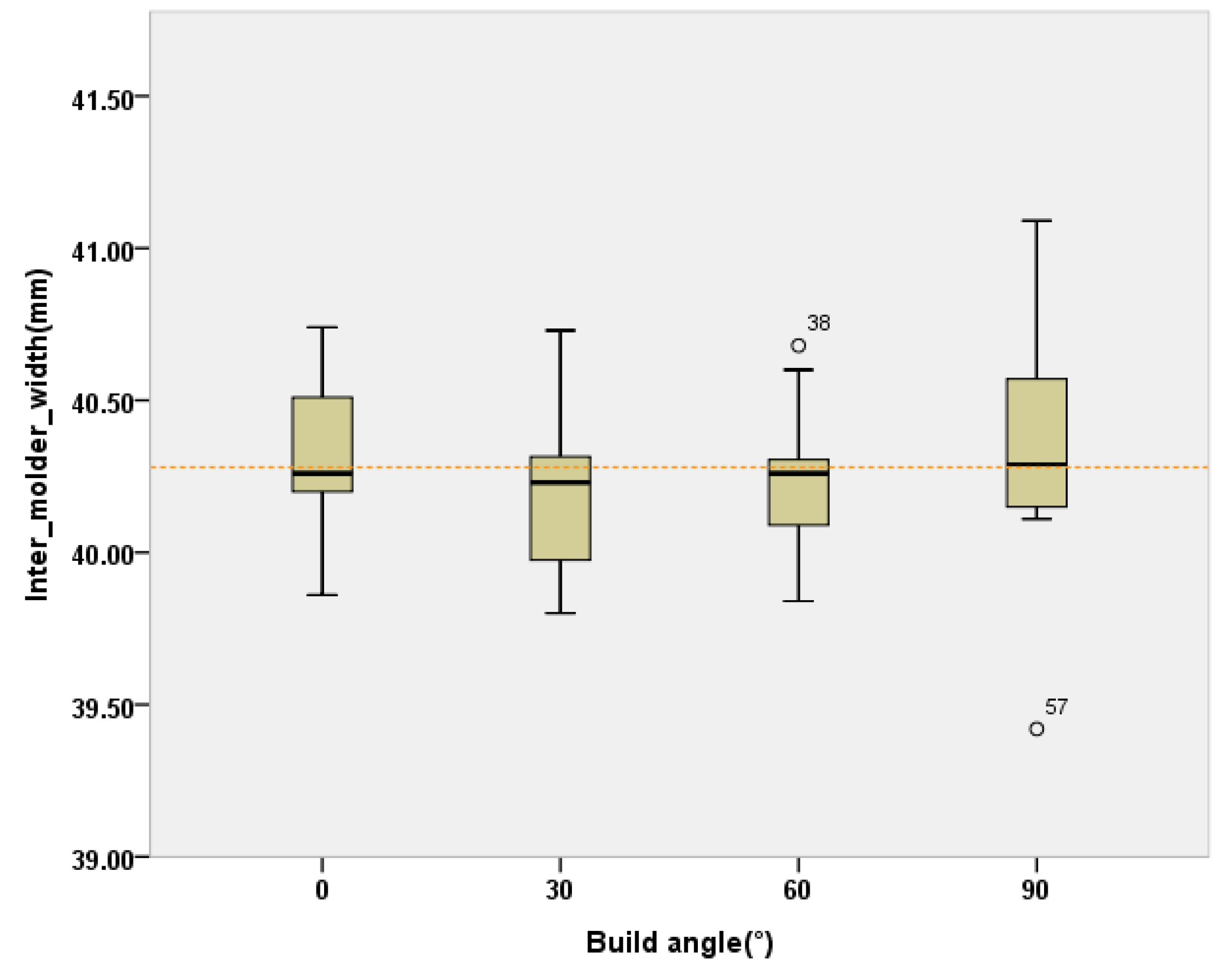
Unlike previous studies that showed significant differences in the distance between bilateral canines and molars in denture bases with different build angles [
18], our results did not show differences in the inter-canine width and inter-molar width.
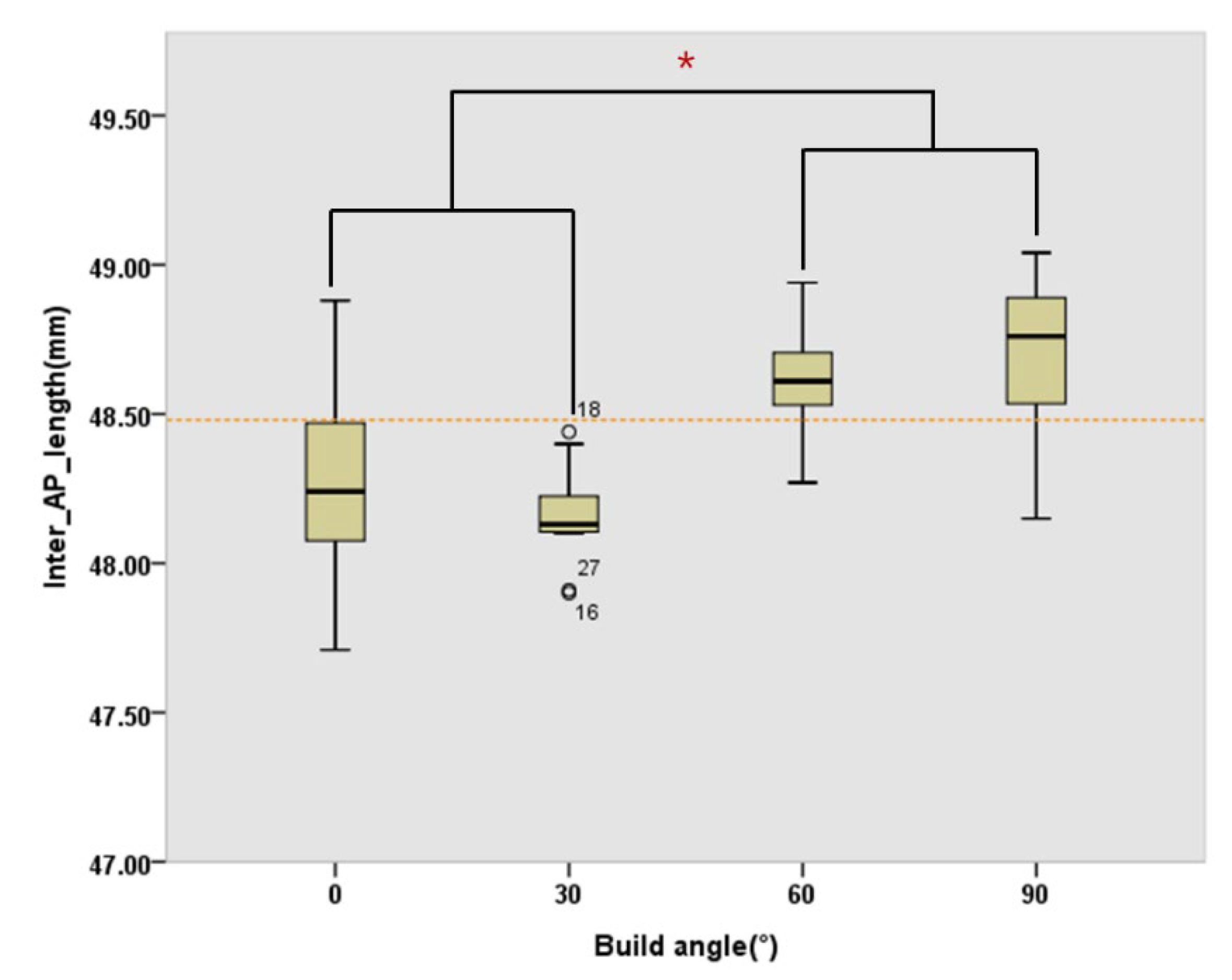
The inter-AP lengths were not significantly different between denture bases with 0° and 30° build angles or between those with 60° and 90° build angles. However, compared to the denture bases with 0° and 30° build angles, those with 60° and 90° build angles exhibited a significantly greater inter-AP length. This observation aligns with the differences in adaptation between the digital model and the denture base tissue surface in the anterior and posterior regions, as illustrated by the color difference map.
As the build angle increases, notable changes in adaptation are observed in both the anterior palatal rugae area and the posterior border seal area of the denture base. The primary reason for this is that the posterior border seal area, printed first, is more susceptible to tensile forces and gravity, which increases as the build angle rises. Consequently, this area is more prone to deformation with higher build angles. Additionally, at higher build angles (60° and 90°), tissue adaptation in the anterior palatal rugae region tends to show a positive deviation. This effect may result from the best-fit algorithm used in Geomagic Control®, which aims to minimize overall deviation when significant deformation occurs in the posterior border seal area of the denture.
The average of the error values for all building angles was within the clinical limits. However, the error values for the distances between the polished surfaces of the denture bases ranged from −2.14 mm to +2.28 mm, which exceeds the error range typically observed in dentures produced using the conventional heat-curing process [
2]. This is thought to be a result of additional errors incurred while modifying the positions of the automatically generated supporters around the reference points of the denture base`s polished surface in a 3D printer slicing program, which may have had an impact on the precision in that area [
36]. Additionally, manually identifying and measuring the length between the reference points, which were set in the CAD model for the 3D-printed dentures, may have caused this result. Thus, a method for assessing the accuracy of the polished surface that incorporates a supporter for 3D printing is needed.
In SLA or DLP 3D printing, the build angle refers to the orientation in which the object is sliced during the printing process [
32]. However, the exact definition of build angle can vary, as the orientation of the object relative to the build platform is not standardized across studies. This variation highlights the need for a more precise definition of build angle. In this study, a 0° build angle was defined as the orientation where the plane formed by the major axis and the second major axis of the 3D-printed product is parallel to the build platform. Then, the build angle is defined as the acute angle between the build platform and the major axis-second major axis plane when the anterior part of the printed product is elevated. Conversely, if the posterior part of the printed product is elevated, the build angle can be considered as the obtuse angle. For products with both upper and lower surfaces, defining the 0° build angle as when the lower surface is parallel to the build platform could serve as a universal standard for determining build angles in future studies.
This study had some limitations. The number and position of supports to be removed, which were automatically generated on the reference points on the polished surface, were different for each sample. Moreover, in this study, only four different build angles were evaluated, and the tissue surface of the denture base could be divided into several parts for RMSE calculation.
The evolution of materials and printing technologies may play a crucial role in overcoming the observed discrepancies related to build angles in 3D printing of dentures. As noted, the SLA 3D printer was associated with certain issues, and future research should explore the use of advanced printing technologies or alternative resin materials that may mitigate these issues. This study emphasizes the importance of a standardized definition of build angles, advocating for the development of an international standard that ensures consistency across various studies. Such standardization would significantly contribute to the more reliable translation of research findings into clinical practice. Moreover, as the results of this study are clinically significant, it is essential to consider how these findings can be implemented in a real-world clinical setting. This necessitates further studies to evaluate additional factors that may influence the clinical application of these findings, such as patient comfort, durability of the dentures, and ease of the fabrication process.
Figure 1.
(a) Edentulous maxilla model, (b) plaster model, and (c) tissue surface of CAD of the denture base (replication of the negative form of the digital model).
Figure 1.
(a) Edentulous maxilla model, (b) plaster model, and (c) tissue surface of CAD of the denture base (replication of the negative form of the digital model).
Figure 2.
Denture bases with build angles of 0°, 30°, 60°, and 90° (from left to right).
Figure 2.
Denture bases with build angles of 0°, 30°, 60°, and 90° (from left to right).
Figure 3.
Setting polished surface reference points and distance measurements. (a) inter-canine width, (b) inter-molar width, and (c) inter-AP length. inter-AP, inter-anteroposterior
Figure 3.
Setting polished surface reference points and distance measurements. (a) inter-canine width, (b) inter-molar width, and (c) inter-AP length. inter-AP, inter-anteroposterior
Figure 4.
Overlapped color difference map between the digital model and denture base tissue surface. (a) 0°, (b) 30°, (c) 60°, and (d) 90° build angles.
Figure 4.
Overlapped color difference map between the digital model and denture base tissue surface. (a) 0°, (b) 30°, (c) 60°, and (d) 90° build angles.
Figure 5.
Interquartile boxplot of the RMSE between the digital model and tissue surfaces of denture bases with 0°, 30°, 60°, and 90° build angles. Outliers are denoted by "○" and significant differences are marked with "*". RMSE, root mean square error
Figure 5.
Interquartile boxplot of the RMSE between the digital model and tissue surfaces of denture bases with 0°, 30°, 60°, and 90° build angles. Outliers are denoted by "○" and significant differences are marked with "*". RMSE, root mean square error
Figure 6.
Boxplot of the inter-canine width in denture bases with 0°, 30°, 60°, and 90° build angles. The true distance, as specified in the CAD model, is 31.98 mm (indicated by the orange dashed line). Outliers are marked with "o.". CAD, computer-aided manufacturing
Figure 6.
Boxplot of the inter-canine width in denture bases with 0°, 30°, 60°, and 90° build angles. The true distance, as specified in the CAD model, is 31.98 mm (indicated by the orange dashed line). Outliers are marked with "o.". CAD, computer-aided manufacturing
Figure 7.
Boxplot of the inter-molar width in denture bases with 0°, 30°, 60°, and 90° build angles. The true distance, as defined in the CAD model, is 40.28 mm (indicated by the orange dashed line). Outliers are marked with "o." CAD, computer-aided manufacturing
Figure 7.
Boxplot of the inter-molar width in denture bases with 0°, 30°, 60°, and 90° build angles. The true distance, as defined in the CAD model, is 40.28 mm (indicated by the orange dashed line). Outliers are marked with "o." CAD, computer-aided manufacturing
Figure 8.
Boxplot of the inter-AP length with 0°, 30°, 60°, and 90° build angles. The true distance, according to the CAD model, is 48.48 mm (indicated by the orange dashed line). Outliers are marked with "o" and significant differences are indicated by "*." CAD, computer-aided manufacturing
Figure 8.
Boxplot of the inter-AP length with 0°, 30°, 60°, and 90° build angles. The true distance, according to the CAD model, is 48.48 mm (indicated by the orange dashed line). Outliers are marked with "o" and significant differences are indicated by "*." CAD, computer-aided manufacturing