1. Introduction
Autism Spectrum Disorder (ASD) is increasingly recognized as a significant public health issue, impacting over 1% of the global population [
1]. It is characterized by neurodevelopmental disorders such as difficulties in social communication and repetitive behaviors [
2]. According to the Centers for Disease Control and Prevention, approximately 1 in 59 young adults are affected by ASD [
3].
Individuals with ASD face numerous challenges, one of the most pressing being adherence to essential dietary guidelines [
4]. Nearly 70% of people with autism struggle to meet these guidelines, especially during adolescence, resulting in dietary issues such as food selectivity and aversion [
4]. These issues manifest as a preference for certain foods and an aversion to others, commonly labeled as "picky eating," particularly prominent during the teenage years [
5]. This selective eating pattern often leads to inadequate intake of essential nutrients, with a noticeable preference for starches and snack foods over fruits, vegetables, and proteins [
6]. Despite the recommendation from the Dietary Guidelines for Americans that fruits and vegetables should constitute half of our plate for a balanced diet [
7], many individuals with ASD tend to avoid these foods [
8]. Fruits and vegetables offer a wide variety of vitamins (vitamin A, thiamin, vitamin B12, vitamin C, and vitamin D) which are beneficial in reducing autism symptoms [
9]. Additionally, they provide dietary fiber that supports shaping the gut microbiota composition, leading to improved cognitive function [
10,
11]. Fruits and vegetables are also a valuable source of minerals, phytochemicals, and antioxidants, all of which have been linked to promoting better neurological outcomes for people with autism [
12].
Beyond dietary concerns, individuals with ASD often experience concurrent comorbidities, with over 70% grappling with conditions such as attention-deficit hyperactivity disorder, anxiety, and depression [
13,
14]. Managing these comorbidities typically involves a combination of pharmacotherapy and nutritional interventions [
14]. Although adolescence typically marks a period of increasing independence and behavioral autonomy, individuals with autism often encounter a plateau and subsequent decline in functional independence, particularly in managing regular medication regimens for co-occurring conditions [
15]. Recognizing this issue, the American Academy of Pediatrics in 2011 emphasized the importance of assessing adolescents' ability to manage their health conditions and access healthcare [
16]. This highlights the value of exploring how well adolescents with ASD can independently manage their health and nutrition to mitigate their symptoms. Using established assessments to evaluate transition skills can help families assess their teens' capabilities, set realistic goals, and implement effective interventions for a smoother transition into adulthood. While pharmacological treatments play a vital role in managing ASD symptoms and related conditions, it is essential to note that these treatments are not aimed at reversing ASD's inherent disabilities [
8,
9].
By the age of 18, most young people have developed the skills needed for a successful transition into adulthood [
17]. However, each year, over 50,000 adolescents with ASD in the U.S. make the transition into adulthood [
2]. While considerable research has been dedicated to understanding autism in children, the same cannot be said for the subsequent journey into adulthood after departing from child-oriented care systems [
17]. Recent findings confirm that fewer than 20% of adolescents with autism experience positive outcomes when assuming adult responsibilities [
18]. During this transitional period, it is imperative to assess their capability to manage their healthcare and nutrition independently. This transitional phase represents a critical opportunity to evaluate and improve the outcomes for these adolescents. A vital aspect of this assessment involves determining their readiness and confidence in handling healthcare-related tasks, such as scheduling medical appointments, managing medications, and effectively communicating with healthcare providers. Equally important is the analysis of their dietary habits, including fruits and vegetables versus empty-calorie foods. Such evaluations provide valuable insights into their diet status and self-efficacy in managing their dietary needs autonomously. This information is essential for devising customized plans and interventions that effectively support their health management during this significant life stage [
19].
This study aims to conduct a preliminary cross-sectional analysis of dietary habits and transition readiness among adolescents with autism. To our knowledge, this is the first retrospective cross-sectional study to examine the correlation between dietary habits and transition readiness in this population. We will collect relevant data using the Starting the Conversation on Diet Questionnaire [
21] and the Transition Readiness Assessment Questionnaire [
5] to understand better how dietary choices affect transition readiness. The alternative hypothesis suggests a correlation between dietary quality and transition readiness in adolescents with autism aged 19 to 22, while the null hypothesis posits no correlation between the variables.
2. Materials and Methods
2.1. Study Design and Participants
Our study targeted individuals aged 19-22 diagnosed with autism who also required regular medication for concurrent conditions, including mood disorders, attention-deficit/hyperactivity disorder (ADHD), depression, anxiety, irritability, and disruptive behaviors. We conducted this retrospective cross-sectional pilot study across multiple research sites.
To capture diverse populations, we collaborated with three autism initiative programs in Virginia—specifically, the Mason Autism Support Initiative (MASI) and Mason Life, both at George Mason University in Fairfax, VA, as well as the Autism Society Tidewater in Virginia Beach. These institutions, with verified autism diagnoses among their student populations, ensured the inclusion of individuals with confirmed autism diagnoses. Interested participants answered an eligibility screening question to ensure they met the study criteria, including being aged between 19 and 22, having a diagnosis of autism, and currently taking at least one medication for a co-occurring condition. If they answered YES to the eligibility question, they were routed to the informed consent form. Following this, eligible participants who could autonomously comprehend the study's purpose, procedures, and potential risks and benefits and subsequently provide their consent were included in the study. Participants requiring parental consent were excluded to expedite data collection and streamline the inclusion process.
Our data collection process was meticulous and comprehensive. Two questionnaires, the Transition Readiness Assessment Questionnaire (TRAQ) and Starting the Conversation: Diet (STC), were completed by a nonprobability sample of eligible students enrolled in the autism initiative programs. Prior to disseminating the research study flyers to students, program managers meticulously reviewed survey tools, ensuring both the content and comprehension levels aligned with the research subjects. Data collection, which took place between October 2023 and February 2024, was facilitated by program managers who distributed the study flyer containing a QR code and a hyperlink to the survey via newsletters. To foster inclusivity, the Assistive Technology Initiative at George Mason University ensured that the flyer and research instruments were accessible to screen readers. Digital informed consent was obtained from all participants, and data were securely stored using the Redcap platform.
This research project underwent a rigorous review and received approval from the Institutional Review Board. Forty-seven participants (n= 47) took part in the study. In recognition of their contribution, participants received a $10 gift card as an incentive.
2.2. Instruments
Demographic data, including age and gender, was collected as part of the survey questions.
Starting The Conversation: Diet Scale: The Starting the Conversation (STC) on diet assessment, developed by the Center for Health Promotion and Disease Prevention at the University of North Carolina at Chapel Hill, is a simplified food frequency questionnaire for evaluating dietary patterns [
6]. Derived from a validated 54-item instrument, it focuses on assessing and advising individuals on their dietary quality [
6]. The STC questionnaire consists of eight items, with response options categorized into three columns: the left column represents the healthiest practices (scored 0), the center column represents less healthy practices (scored 1), and the right column represents the least healthy practices (scored 2). A summary score ranging from 0 to 16 is obtained by totaling the item scores. Lower summary scores indicate a healthier diet, while higher scores indicate greater room for improvement [
6]. The eight items in the STC survey assess food choices by examining the variety of foods consumed, including fruits and vegetables, fast food, and soda, and the frequency of consumption over the past few months.
In a recent investigation validating the utilization of the STC instrument, 463 diabetes patients were involved in a study focused on self-management intervention [
22]. The study's outcome revealed that the eight items comprising the STC instrument, and the overall summary score displayed good performance, establishing its reliability and effectiveness as a nutritional assessment tool [
21,
22]. This discovery suggests that the questionnaire will effectively measure eating patterns among adolescents with autism in this research study.
Transition Readiness Scale (TRAQ): The self-management and transition assessment measures the level of preparedness for transition. Recent studies evaluating the preparedness of young individuals with autism [
22] and special healthcare needs utilized the Transition Readiness Assessment Questionnaire, which exhibited satisfactory content validity, construct validity, and internal consistency [
23,
24]. Consequently, it was deemed the most reliable and well-validated tool for assessing adolescent transition readiness [
24]. The TRAQ consists of 20 validated items divided into five subscales, assessing health-related knowledge and self-management skills [
5]. Each subscale focuses on a specific area and contains between two and seven questions. The subscales cover medication management, appointment keeping, tracking health issues, talking with healthcare providers, and managing daily activities [
5].
Responses to the items in the TRAQ are scored on a Likert-type scale ranging from 1 to 5. The scale includes the following options: 1 = "No, I do not know how," 2 = "No, but I want to learn," 3 = "No, but I am learning to do this," 4 = "Yes, I have started doing this," and 5 = "Yes, I always do this when I need to" [
5].
The overall TRAQ score is determined by calculating the average of the scores from the 20 items, resulting in a score between 1 and 5. Additionally, scores for each domain associated with the five subscales can be calculated by averaging the scores of the questions within each subscale. These domain scores also range from 1 to 5 [
5]. Higher scores on the overall TRAQ and the subscales indicate a greater readiness for transition. While a TRAQ score of below 4.0 indicates that the participant is not yet ready to transition from adolescence to adulthood [
25]
2.3. Statistical Analysis
We utilized mean and standard deviation to describe continuous variables and percentages to describe categorical variables. To test the null hypothesis, we initially conducted t-tests. The hypothesized mean difference was set to 0, while the alpha level was set to 0.05. Subsequently, we performed linear regression analysis to further investigate the relationship, assessing its strength and nature. The regression results are presented through Multiple R (the correlation coefficient between variables), R² (the proportion of variance in the dependent variable explained by the model), standard error (the variability of the dependent variable), and coefficients (used to formulate the regression equation for prediction). To assess the model's suitability, we analyzed the R² value in the regression as a measure of goodness-of-fit. All statistical analyses were conducted using SPSS Statistics (version 27.0; IBM Corp., Armonk, NY, USA), and data visualization was performed using Microsoft Excel 2013.
3. Results
3.1. Description of Sample
Forty-seven subjects (n= 47) were included in this study, with ages ranging from 19 to 22 years and a mean age of 21.0 ± 1.1 years. The majority of the sample (66%) identified as male, while (34%) identified as female. All respondents (100%) had a primary diagnosis of autism, necessitating regular medication for comorbid conditions, including mood disorders, attention-deficit/hyperactivity disorder, depression, anxiety disorders, and irritability. Refer to
Table 1 for a comprehensive overview of the key demographic characteristics.
3.2. T-Test Analysis
Participants exhibited significantly lower scores in the TRAQ survey (3.19 ± 1.10) and higher scores in the STC survey (1.08 ± 0.07). A statistically significant negative correlation (r= -0.51, p<0.001) was observed between diet and the transition readiness of adolescents, as outlined in
Table 2.
3.3. Simple Linear Regression Analysis
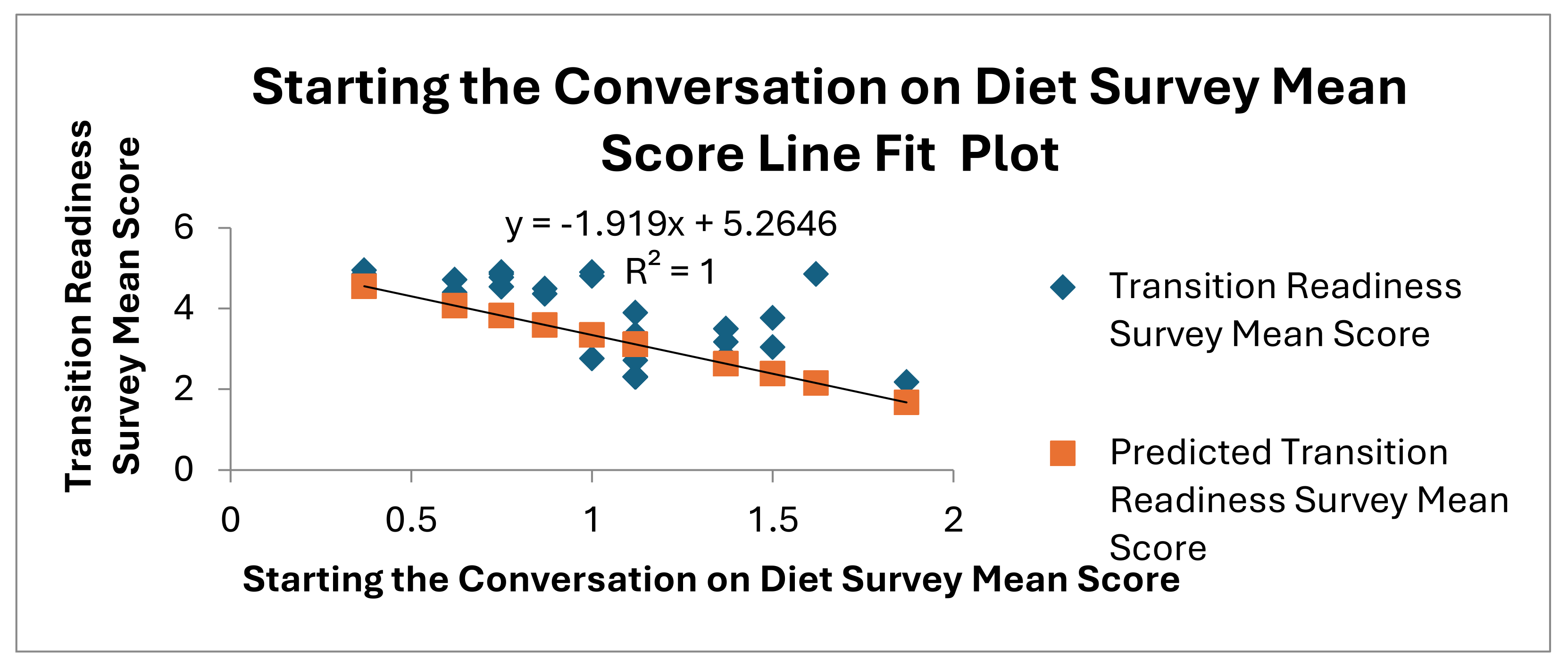
A strong association exists (r = 0.51, P < 0.0002) between dietary habits and transition readiness, with dietary habits accounting for 26.20% of the variation in transition readiness. The predicted values deviate from the actual values by approximately 0.91 units on average. The confidence interval for the coefficient of dietary habits (95% CI: -2.89 to -0.95) shows a statistically significant negative relationship. The results of the linear regression are illustrated in
Table 3.
The line fit plot shows the relationship between the STC Mean Score and the TRAQ Mean Score. The linear regression equation is (y= −1.919x + 5.2646). The plot (
Figure 2) confirms an adverse relationship between the two variables. The intercept (5.26) shows the TRAQ Mean Score when the STC Mean Score is zero. The R-squared value is 1, demonstrating a perfect fit of the model to the data.
The mean and standard deviation (SD) scores revealed no significant variation in transition preparedness between males and females, as shown in
Table 4. Females had a mean score of 3.13 ± 0.33, while males recorded a mean score of 3.23 ± 0.28.
Table 4 further explores dietary quality and transition preparedness across different genders and age groups, highlighting the consistency in scores among the groups.
4. Discussion
To our knowledge, this study is the first to explore the relationship between dietary quality and transition readiness in adolescents with autism. Our findings confirm the alternative hypothesis, showing a significant correlation between dietary quality and the readiness of young adults with autism to transition into adulthood. Consequently, we reject the null hypothesis, as the p-value (0.001) from the t-test is well below the standard α (0.05). Our analysis indicates that participants with suboptimal dietary habits, reflected by higher scores on the STC, tend to score lower on the TRAQ, implying a lack of preparedness for adult life. The Pearson correlation coefficient of -0.51 highlights an inverse relationship between dietary quality and transition readiness: as dietary practices worsen, readiness for adulthood diminishes.
Conversely, improved dietary patterns correlate with a higher degree of preparedness for adulthood. This negative correlation emphasizes the distinct roles the two measures play in capturing different aspects of the participants’ readiness and health behaviors. Additionally, the perfect R² value in the line fit plot confirms a strong linear relationship between the two variables, indicating that the model's predictions based on the data points are extremely precise.
Our research found that both genders exhibit similar levels of preparedness for the transition, indicating that gender may not be a critical determinant of readiness. This contrasts with another study that found lower preparedness levels among females attributed to dietary patterns [
26]. Nevertheless, our findings highlight the necessity of considering additional factors that could influence transition readiness.
In our analysis, the regression model accounts for only 26.2% of the variability in transition readiness, leaving 73.8% of the variance unexplained. This significant unexplained portion suggests that other influential factors not included in the model may be at play. These factors are crucial in shaping adolescents' behaviors and preparedness for adulthood.
Recent research indicates that medications prescribed for comorbid conditions in autism, such as venlafaxine, a common antidepressant used to treat anxiety and depression, can impact appetite due to side effects [
27]. This interaction underscores the potential for medication to alter dietary intake, a particularly significant consideration for individuals with comorbidities [
28].
Furthermore, food selectivity, affecting 46% to 89% of children with autism and often persisting into adolescence, has been identified as another significant factor [
29]. Food selectivity can substantially influence the nutritional intake of adolescents with autism, potentially exacerbating the severity of autism symptoms and impacting their overall development and readiness for adult responsibilities.
It is imperative to acknowledge several constraints when interpreting the study's findings. This cross-sectional pilot study includes 47 participants with autism and co-occurring conditions, such as mood disorders, attention-deficit/hyperactivity disorder, depression, anxiety disorders, irritability, and disruptive behavior. Future directions involve large-scale studies with neurotypical individuals over a longitudinal period. Another limitation is the exclusion of participants requiring parental consent, emphasizing the need for a more diverse subject sample over an extended period to establish the generalizability of the findings.
The implications of our research extend to future endeavors, urging a broader research scope that includes a neurotypical control group for comparative analysis. Considering the impact of parental involvement and the role of comorbid conditions is crucial for a comprehensive assessment. Additionally, intervention studies targeting dietary behaviors and assessing their impact on transition readiness could provide a more holistic perspective on the complex interplay between diet and readiness for transition.
Our study underscores the importance of addressing the significant funding disparity in autism research. In 2018, only 3% of the U.S. federal funding dedicated to autism research was allocated towards understanding the pivotal transition into adulthood [
30,
31]. Meanwhile, despite federal mandates under the Individuals With Disabilities Education Act (IDEA) [
32], which guarantees special education services until the age of 21, many adolescents with autism face significant challenges transitioning into adulthood. This stark underfunding highlights the critical need for thorough investigations. Thus, our research is an essential foundation for future studies to effectively support adolescents with autism during this crucial developmental phase.
5. Conclusions
The evidence shows an association between dietary quality and transition readiness, emphasizing challenges in the transitional process. Additional research is essential to explore potential interventions.
Author Contributions
Conceptualization, B.S.; methodology, B.S.; software, B.S.; formal analysis, B.S.; resources, B.S.; data curation, B.S.; writing—original draft preparation, B.S.; writing review, B.S and L.D.J.; visualization, B.S.; supervision, L.D.J.; editing, B.S., and L.D.J.; funding acquisition, B.S.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of George Mason University (2077203-1, September 22, 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated from this study are available from the corresponding author upon reasonable request.
Acknowledgments
We would like to acknowledge the invaluable contributions of the participants and the various program coordinators at the institutions where data was collected. Your cooperation has been instrumental to the success of this research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cekici, H.; Sanlier, N. Current Nutritional Approaches in Managing Autism Spectrum Disorder: A Review. Nutritional Neuroscience 2019, 22, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.-C.; Lombardo, M.V.; Baron-Cohen, S. Autism. Lancet 2014, 383, 896–910. [Google Scholar] [CrossRef] [PubMed]
- White, S.W.; Smith, I.C.; Miyazaki, Y.; Conner, C.M.; Elias, R.; Capriola-Hall, N.N. Improving Transition to Adulthood for Students with Autism: A Randomized Controlled Trial of STEPS. J Clin Child Adolesc Psychol 2021, 50, 187–201. [Google Scholar] [CrossRef]
- Blaine, R.E.; Blaine, K.P.; Cheng, K.; Banuelos, C.; Leal, A. Priorities, Barriers, and Facilitators for Nutrition-Related Care for Autistic Children: A Qualitative Study Comparing Interdisciplinary Health Professional and Parent Perspectives. Front Pediatr 2023, 11, 1198177. [Google Scholar] [CrossRef]
- Chan, J.T.; Soni, J.; Sahni, D.; Mantis, S.; Boucher-Berry, C. Measuring the Transition Readiness of Adolescents With Type 1 Diabetes Using the Transition Readiness Assessment Questionnaire. Clin Diabetes 2019, 37, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Paxton, A.E.; Strycker, L.A.; Toobert, D.J.; Ammerman, A.S.; Glasgow, R.E. Starting the Conversation Performance of a Brief Dietary Assessment and Intervention Tool for Health Professionals. Am J Prev Med 2011, 40, 67–71. [Google Scholar] [CrossRef]
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, Vegetables, and Health: A Comprehensive Narrative, Umbrella Review of the Science and Recommendations for Enhanced Public Policy to Improve Intake. Critical Reviews in Food Science and Nutrition 2020, 60, 2174–2211. [Google Scholar] [CrossRef]
- Slavin, J.L.; Lloyd, B. Health Benefits of Fruits and Vegetables. Advances in Nutrition 2012, 3, 506–516. [Google Scholar] [CrossRef]
- Yule, S.; Wanik, J.; Holm, E.M.; Bruder, M.B.; Shanley, E.; Sherman, C.Q.; Fitterman, M.; Lerner, J.; Marcello, M.; Parenchuck, N.; et al. Nutritional Deficiency Disease Secondary to ARFID Symptoms Associated with Autism and the Broad Autism Phenotype: A Qualitative Systematic Review of Case Reports and Case Series. Journal of the Academy of Nutrition and Dietetics 2021, 121, 467–492. [Google Scholar] [CrossRef]
- Cui, J.; Lian, Y.; Zhao, C.; Du, H.; Han, Y.; Gao, W.; Xiao, H.; Zheng, J. Dietary Fibers from Fruits and Vegetables and Their Health Benefits via Modulation of Gut Microbiota. Comprehensive Reviews in Food Science and Food Safety 2019, 18, 1514–1532. [Google Scholar] [CrossRef]
- Mangiola, F.; Ianiro, G.; Franceschi, F.; Fagiuoli, S.; Gasbarrini, G.; Gasbarrini, A. Gut Microbiota in Autism and Mood Disorders. World J Gastroenterol 2016, 22, 361–368. [Google Scholar] [CrossRef]
- Yahia, E.M.; García-Solís, P.; Celis, M.E.M. Chapter 2 - Contribution of Fruits and Vegetables to Human Nutrition and Health. In Postharvest Physiology and Biochemistry of Fruits and Vegetables; Yahia, E.M., Ed.; Woodhead Publishing, 2019; pp. 19–45. ISBN 978-0-12-813278-4.
- Filbert, K.M. Assessment of Strength-Based Functioning, Behavioural Problems, and Adaptive Functioning in Adolescents with Autism Spectrum Disorders and Developmental Disabilities. Thesis, 2005.
- Sharma, S.R.; Gonda, X.; Tarazi, F.I. Autism Spectrum Disorder: Classification, Diagnosis and Therapy. Pharmacol Ther 2018, 190, 91–104. [Google Scholar] [CrossRef]
- Hume, K.; Boyd, B.A.; Hamm, J.V.; Kucharczyk, S. Supporting Independence in Adolescents on the Autism Spectrum. Remedial and Special Education 2014, 35, 102–113. [Google Scholar] [CrossRef]
- Wood, D.L.; Sawicki, G.S.; Miller, M.D.; Smotherman, C.; Lukens-Bull, K.; Livingood, W.C.; Ferris, M.; Kraemer, D.F. The Transition Readiness Assessment Questionnaire (TRAQ): Its Factor Structure, Reliability, and Validity. Academic Pediatrics 2014, 14, 415–422. [Google Scholar] [CrossRef] [PubMed]
- White, P.H.; Cooley, W.C.; TRANSITIONS CLINICAL REPORT AUTHORING GROUP, A.A.O.P., AMERICAN ACADEMY OF FAMILY PHYSICIANS, AMERICAN COLLEGE OF PHYSICIANS Supporting the Health Care Transition From Adolescence to Adulthood in the Medical Home. Pediatrics 2018, 142, e20182587. [CrossRef]
- Ishler, K.J.; Berg, K.A.; Olgac, T.; Obeid, R.; Biegel, D.E. Barriers to Service and Unmet Need among Autistic Adolescents and Young Adults. Autism 2023, 27, 1997–2010. [Google Scholar] [CrossRef] [PubMed]
- Płatos, M.; Pisula, E. Service Use, Unmet Needs, and Barriers to Services among Adolescents and Young Adults with Autism Spectrum Disorder in Poland. BMC Health Serv Res 2019, 19, 587. [Google Scholar] [CrossRef]
- Vohra, R.; Madhavan, S.; Sambamoorthi, U. Comorbidity Prevalence, Healthcare Utilization, and Expenditures of Medicaid Enrolled Adults with Autism Spectrum Disorders. Autism 2017, 21, 995–1009. [Google Scholar] [CrossRef]
- Paxton, A.E.; Strycker, L.A.; Toobert, D.J.; Ammerman, A.S.; Glasgow, R.E. Starting The Conversation: Performance of a Brief Dietary Assessment and Intervention Tool for Health Professionals. American Journal of Preventive Medicine 2011, 40, 67–71. [Google Scholar] [CrossRef]
- Staff Healing Tool Series: Starting the Conversation on Diet - Healing Works Foundation 2018.
- Beal, S.J.; Riddle, I.K.; Kichler, J.C.; Duncan, A.; Houchen, A.; Casnellie, L.; Woodward, J.; Corathers, S.D. The Associations of Chronic Condition Type and Individual Characteristics With Transition Readiness. Academic Pediatrics 2016, 16, 660–667. [Google Scholar] [CrossRef]
- Sawicki, G.S.; Lukens-Bull, K.; Yin, X.; Demars, N.; Huang, I.-C.; Livingood, W.; Reiss, J.; Wood, D. Measuring the Transition Readiness of Youth with Special Healthcare Needs: Validation of the TRAQ—Transition Readiness Assessment Questionnaire. Journal of Pediatric Psychology 2011, 36, 160–171. [Google Scholar] [CrossRef]
- Zhang, L.F.; Ho, J.S.; Kennedy, S.E. A Systematic Review of the Psychometric Properties of Transition Readiness Assessment Tools in Adolescents with Chronic Disease. BMC Pediatrics 2014, 14, 4. [Google Scholar] [CrossRef]
- Hooker, E.; Eckenrode, M.; Hopson, B.; Somerville, C.S. Initial Observations of Medically Complex Young Adults Transitioning to Adult Care: Revealing Data Regarding Mental Health, Nutrition, and Transition Preparedness. Health Care Transitions 2023, 1, 100005. [Google Scholar] [CrossRef]
- Wallace, G.L.; Richard, E.; Wolff, A.; Nadeau, M.; Zucker, N. Increased Emotional Eating Behaviors in Children with Autism: Sex Differences and Links with Dietary Variety. Autism 2021, 25, 603–612. [Google Scholar] [CrossRef]
- Dean, L. Venlafaxine Therapy and CYP2D6 Genotype. In Medical Genetics Summaries; Pratt, V.M., Scott, S.A., Pirmohamed, M., Esquivel, B., Kattman, B.L., Malheiro, A.J., Eds.; National Center for Biotechnology Information (US): Bethesda (MD), 2012.
- Basiri, R.; Seidu, B.; Rudich, M. Exploring the Interrelationships between Diabetes, Nutrition, Anxiety, and Depression: Implications for Treatment and Prevention Strategies. Nutrients 2023, 15, 4226. [Google Scholar] [CrossRef] [PubMed]
- Maitin-Shepard, M.; O’Tierney-Ginn, P.; Kraneveld, A.D.; Lyall, K.; Fallin, D.; Arora, M.; Fasano, A.; Mueller, N.T.; Wang, X.; Caulfield, L.E.; et al. Food, Nutrition, and Autism: From Soil to Fork. The American Journal of Clinical Nutrition 2024. [Google Scholar] [CrossRef] [PubMed]
- Autism Research Database - Strategic Plan Questions | IACC. Available online: https://iacc.hhs.gov/funding/data/?fy=2018 (accessed on 11 February 2024).
- | Answering the Questions about Autism in Adulthood Available online:. Available online: http://sparkforautism.org/discover/autism-in-adulthood (accessed on 11 February 2024).
- Lipkin, P.H.; Okamoto, J.; the COUNCIL ON CHILDREN WITH DISABILITIES and COUNCIL ON SCHOOL HEALTH; Norwood, K.W., Jr; Adams, R.C.; Brei, T.J.; Burke, R.T.; Davis, B.E.; Friedman, S.L.; Houtrow, A.J.; et al. The Individuals With Disabilities Education Act (IDEA) for Children With Special Educational Need. Pediatrics 2015, 136, e1650–e1662. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).