Submitted:
03 September 2024
Posted:
03 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. IL-33 and Its Receptor Biology
2.1. IL-33
2.2. IL-33 Receptor
2.3. IL-33 and ST2 Distribution
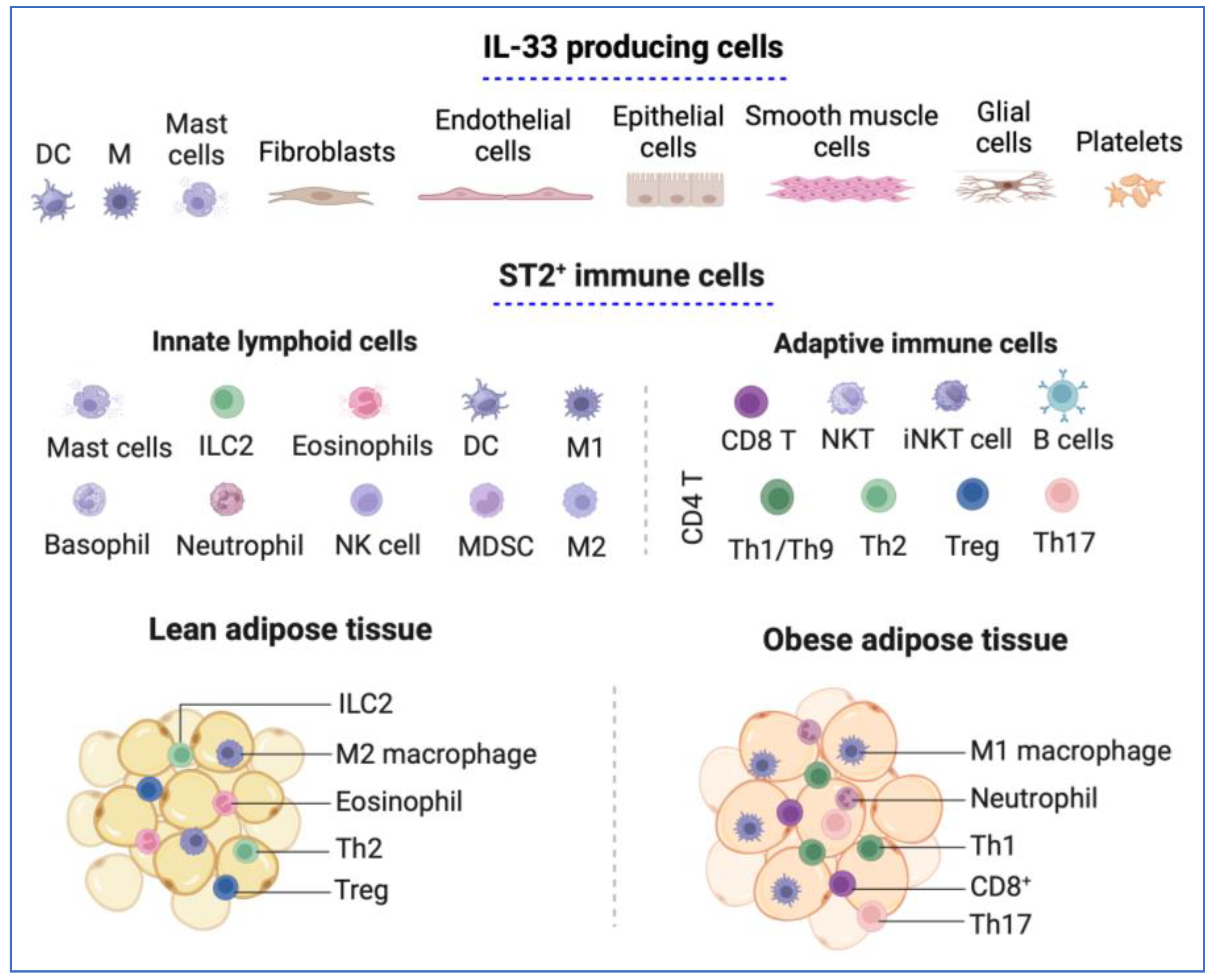
2.3.1. IL-33 and ST2 Expression in Immune Cells
2.3.2. IL-33 and ST2 Immune Cell Distribution in Adipose Tissue
2.3.3. IL-33 and ST2 Immune Cell Distribution in the Tumor Microenvironment
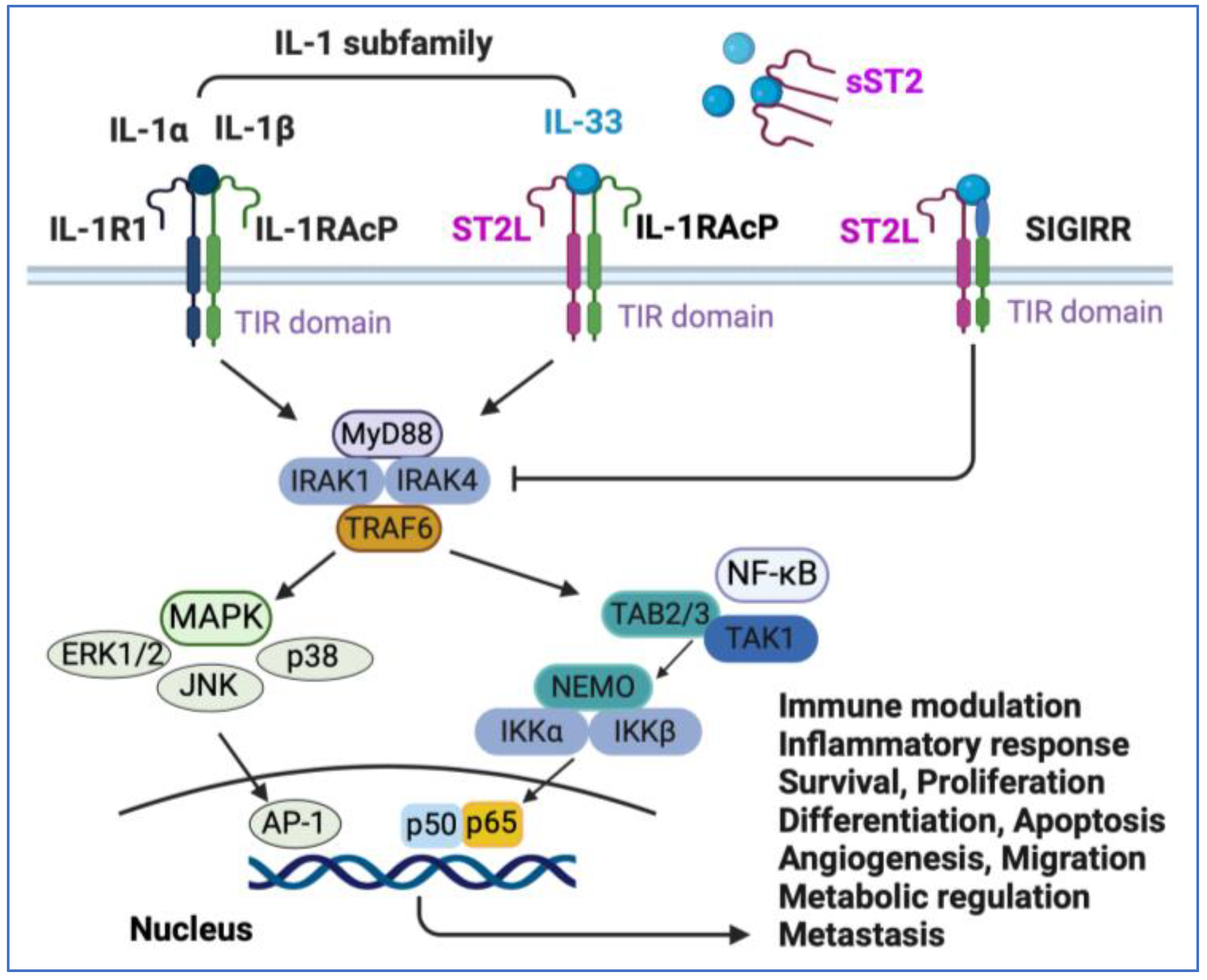
3. IL-33/ST2 Signaling Pathway
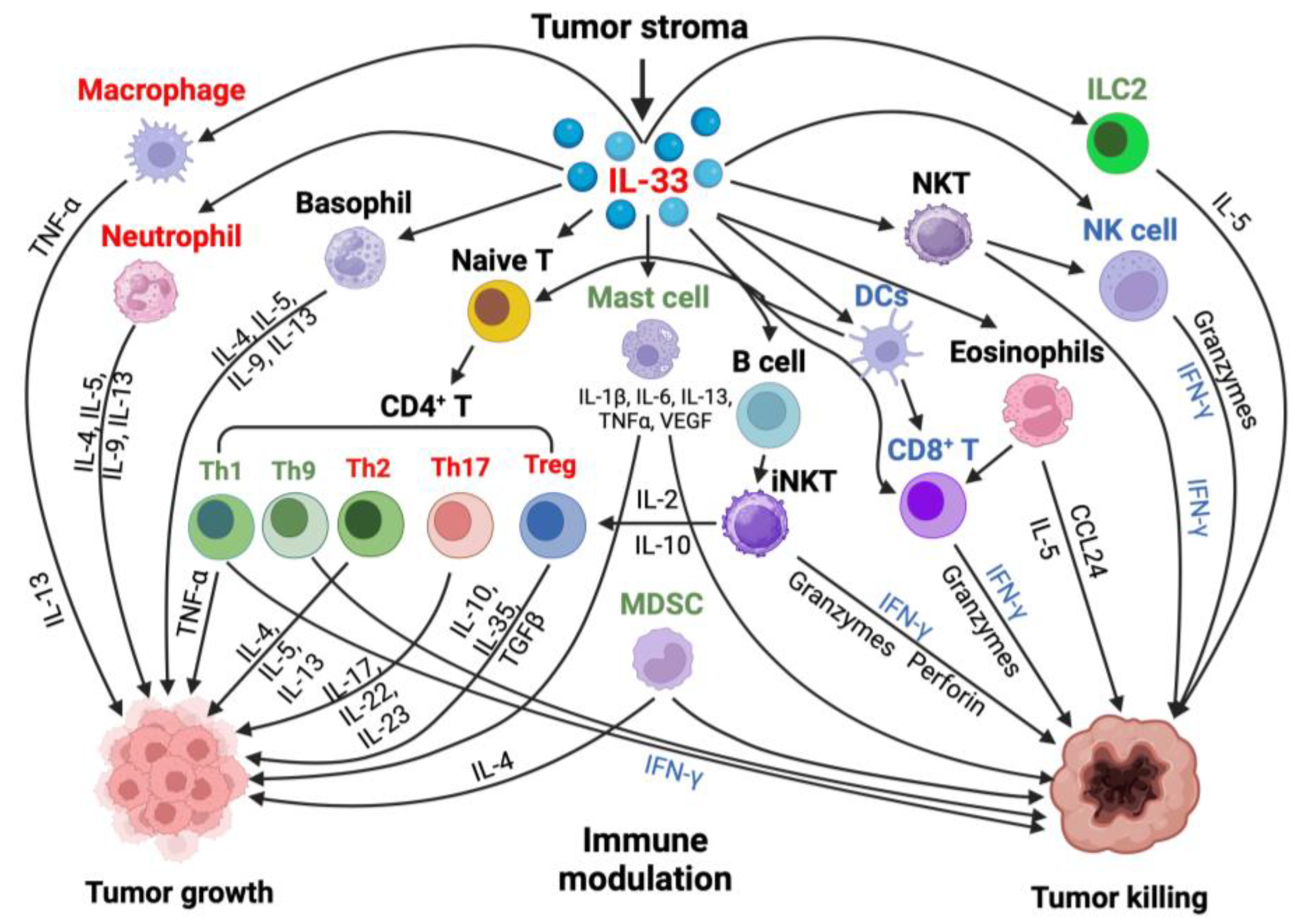
4. Effect of Il-33 in the Tumor Microenvironment
4.1. Effect of Il-33 on Neutrophils, Eosinophils, Mast Cells, and Basophils
4.2. Effect of Il-33 on Macrophages and Dendritic Cells
4.3. Effect of Il-33 on CD8+ T, NK and NKT Cells
4.4. Effect of Il-33 on Myeloid-Derived Suppressor Cells
4.5. Effect of Il-33 on T helper Cells
4.6. Effect of Il-33 on CD4+ Treg Cells and in Tumor Immunity
4.7. IL-33-Expressing Cells and the Effects of IL-33 on Non-Immune Cells in the Tumor Microenvironment
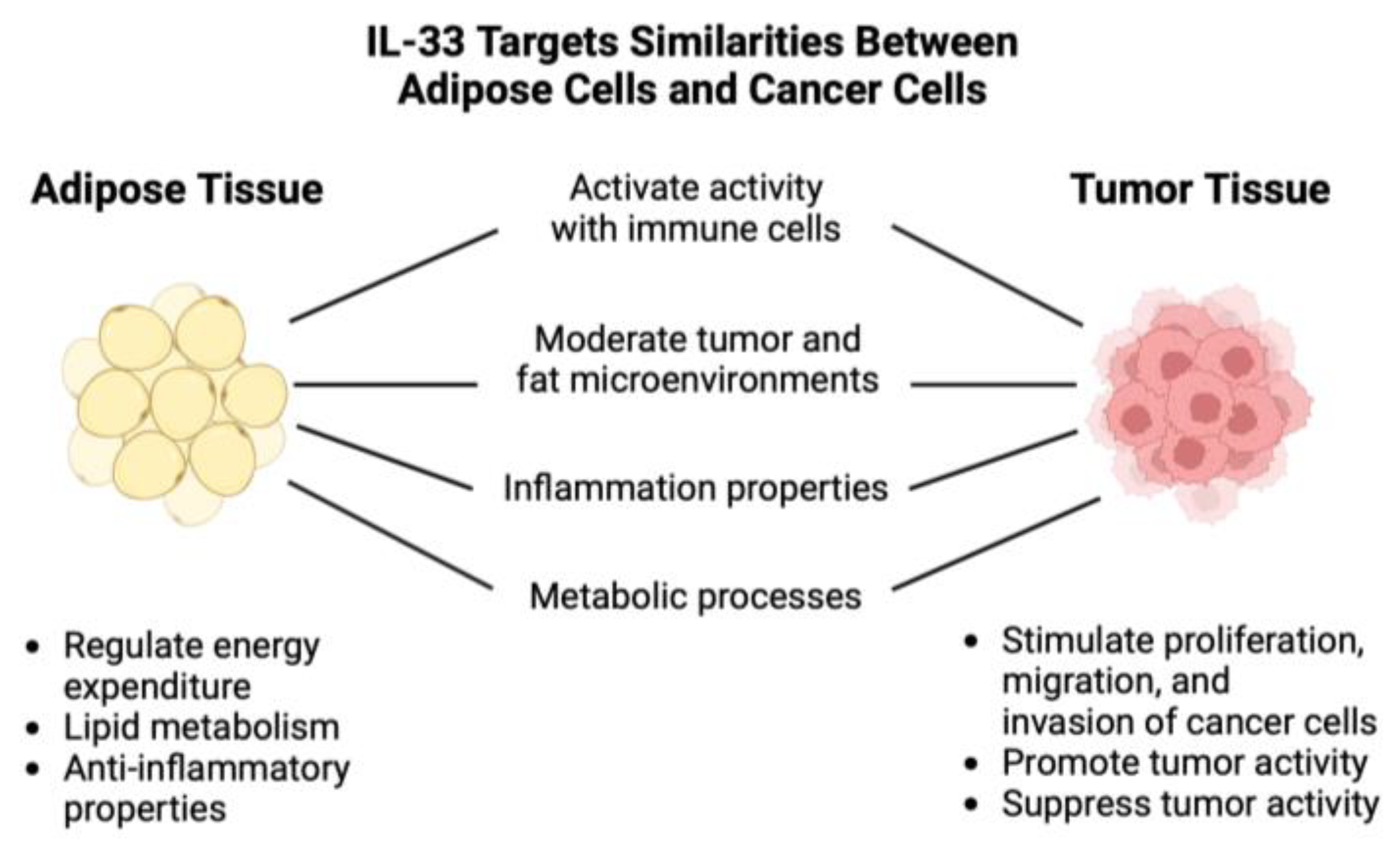
5. Effect of IL-33 on Adipose Tissue
6. Discussion of Obesity and Cancer Correlation
7. Conclusions and Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schmitz J, Owyang A, Oldham E, Song Y, Murphy E, McClanahan TK, et al. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity 2005; 23(5):479-490.
- Garlanda C, Dinarello CA, Mantovani A. The interleukin-1 family: back to the future. Immunity 2013; 39(6):1003-1018.
- Carriere V RL, Ortega N, Lacorre DA, Americh L, Aguilar L, Bouche G, Girard JP. IL-1-like cytokine ligand for ST2 receptor, is a chromatin-associated nuclear factor in vivo. Proc Natl Acad Sci U S A 2007; 104(287-2).
- Cayrol C, & Girard, J. P.. Interleukin-33 (IL-33): A nuclear cytokine from the IL-1 family. Immunological reviews 2018; 281(1):154–168.
- Gaurav R, Poole JA. Interleukin (IL)-33 immunobiology in asthma and airway inflammatory diseases. J Asthma 2022; 59(12):2530-2538.
- Di Carmine S, Scott MM, McLean MH, McSorley HJ. The role of interleukin-33 in organ fibrosis. Discov Immunol 2022; 1(1):kyac006.
- Chen WY, Li LC, Wu YH, Yang JL, Tzeng HT. Emerging Roles of Interleukin-33-responsive Kidney Group 2 Innate Lymphoid Cells in Acute Kidney Injury. Int J Mol Sci 2020; 21(4).
- Brunetti G, Barile B, Nicchia GP, Onorati F, Luciani GB, Galeone A. The ST2/IL-33 Pathway in Adult and Paediatric Heart Disease and Transplantation. Biomedicines 2023; 11(6).
- De la Fuente M, MacDonald TT, Hermoso MA. The IL-33/ST2 axis: Role in health and disease. Cytokine Growth Factor Rev 2015; 26(6):615-623.
- Yi XM, Lian H, Li S. Signaling and functions of interleukin-33 in immune regulation and diseases. Cell Insight 2022; 1(4):100042.
- Jia Z, Guo M, Ge X, Chen F, Lei P. IL-33/ST2 Axis: A Potential Therapeutic Target in Neurodegenerative Diseases. Biomolecules 2023; 13(10).
- Hasan A, Kochumon, S., Al-Ozairi, E., Tuomilehto, J., & Ahmad, R. Association between Adipose Tissue Interleukin-33 and Immunometabolic Markers in Individuals with Varying Degrees of Glycemia. Disease markers, 2019.
- de Oliveira MFA, Talvani A, Rocha-Vieira E. IL-33 in obesity: where do we go from here?Inflamm Res 2019; 68(3):185-194.
- Allegra A, Innao V, Tartarisco G, Pioggia G, Casciaro M, Musolino C, et al. The ST2/Interleukin-33 Axis in Hematologic Malignancies: The IL-33 Paradox. Int J Mol Sci 2019; 20(20).
- Song M, Yang J, Di M, Hong Y, Pan Q, Du Y, et al. Alarmin IL-33 orchestrates antitumoral T cell responses to enhance sensitivity to 5-fluorouracil in colorectal cancer. Theranostics 2023; 13(5):1649-1668.
- Chatrabnous N, Jafarzadeh A, Ghaderi A, Ariafar A, Aminizadeh N, Ghassabi F, et al. Association of elevated interleukin-33 serum levels with tumorstages in patients with prostate cancer. Eur Cytokine Netw 2019; 30(4):144-150.
- Stojanovic B, Gajovic N, Jurisevic M, Stojanovic MD, Jovanovic M, Jovanovic I, et al. Decoding the IL-33/ST2 Axis: Its Impact on the Immune Landscape of Breast Cancer. Int J Mol Sci 2023; 24(18).
- Liu N, Chen J, Zhao Y, Zhang M, Piao L, Wang S, et al. Role of the IL-33/ST2 receptor axis in ovarian cancer progression. Oncol Lett 2021; 22(1):504.
- Borovcanin MM, Vesic K. Breast cancer in schizophrenia could be interleukin-33-mediated. World J Psychiatry 2021; 11(11):1065-1074.
- Pahwa, R. Chronic Inflammation. In. Edited by Goyal A. StatPearls: Treasure Island (FL); 2022.
- Hildebrandt X, Ibrahim M, Peltzer N. Cell death and inflammation during obesity: "Know my methods, WAT(son)". Cell Death Differ 2023; 30(2):279-292.
- Arnold M, Pandeya N, Byrnes G, Renehan PAG, Stevens GA, Ezzati PM, et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol 2015; 16(1):36-46.
- Pati S, Irfan W, Jameel A, Ahmed S, Shahid RK. Obesity and Cancer: A Current Overview of Epidemiology, Pathogenesis, Outcomes, and Management. Cancers (Basel) 2023; 15(2).
- Liew FY, Girard JP, Turnquist HR. Interleukin-33 in health and disease. Nat Rev Immunol 2016; 16(11):676-689.
- Luzina IG, Clerman A, Fishelevich R, Todd NW, Lockatell V, Atamas SP. Identification of the IL-33 protein segment that controls subcellular localization, extracellular secretion, and functional maturation. Cytokine 2019; 119:1-6.
- Cayrol C, Girard JP. The IL-1-like cytokine IL-33 is inactivated after maturation by caspase-1. Proc Natl Acad Sci U S A 2009; 106(22):9021-9026.
- Liu X, Hammel M, He Y, Tainer JA, Jeng US, Zhang L, et al. Structural insights into the interaction of IL-33 with its receptors. Proc Natl Acad Sci U S A 2013; 110(37):14918-14923.
- Lingel A, Weiss TM, Niebuhr M, Pan B, Appleton BA, Wiesmann C, et al. Structure of IL-33 and its interaction with the ST2 and IL-1RAcP receptors--insight into heterotrimeric IL-1 signaling complexes. Structure 2009; 17(10):1398-1410.
- Klemenz R, Hoffmann S, Werenskiold AK. Serum- and oncoprotein-mediated induction of a gene with sequence similarity to the gene encoding carcinoembryonic antigen. Proc Natl Acad Sci U S A 1989; 86(15):5708-5712.
- Tominaga, S. A putative protein of a growth specific cDNA from BALB/c-3T3 cells is highly similar to the extracellular portion of mouse interleukin 1 receptor. FEBS Lett 1989; 258(2):301-304.
- Kakkar R, Lee RT. The IL-33/ST2 pathway: therapeutic target and novel biomarker. Nat Rev Drug Discov 2008; 7(10):827-840.
- Gächter T, Werenskiold AK, Klemenz R. Transcription of the interleukin-1 receptor-related T1 gene is initiated at different promoters in mast cells and fibroblasts. J Biol Chem 1996; 271(1):124-129.
- Mariotti FR, Supino D, Landolina N, Garlanda C, Mantovani A, Moretta L, et al. IL-1R8: A molecular brake of anti-tumor and anti-viral activity of NK cells and ILC. Semin Immunol 2023; 66:101712.
- Bulek K, Swaidani S, Qin J, Lu Y, Gulen MF, Herjan T, et al. The essential role of single Ig IL-1 receptor-related molecule/Toll IL-1R8 in regulation of Th2 immune response. J Immunol 2009; 182(5):2601-2609.
- Cayrol C, Girard JP. Interleukin-33 (IL-33): A critical review of its biology and the mechanisms involved in its release as a potent extracellular cytokine. Cytokine 2022; 156:155891.
- Göpfert C, Andreas N, Weber F, Häfner N, Yakovleva T, Gaestel M, et al. The p38-MK2/3 Module Is Critical for IL-33-Induced Signaling and Cytokine Production in Dendritic Cells. J Immunol 2018; 200(3):1198-1206.
- Ishiguro N, Moriyama M, Furusho K, Furukawa S, Shibata T, Murakami Y, et al. Activated M2 Macrophages Contribute to the Pathogenesis of IgG4-Related Disease via Toll-like Receptor 7/Interleukin-33 Signaling. Arthritis Rheumatol 2020; 72(1):166-178.
- He PY, Wu MY, Zheng LY, Duan Y, Fan Q, Zhu XM, et al. Interleukin-33/serum stimulation-2 pathway: Regulatory mechanisms and emerging implications in immune and inflammatory diseases. Cytokine Growth Factor Rev 2024; 76:112-126.
- Cayrol C, Girard JP. IL-33: an alarmin cytokine with crucial roles in innate immunity, inflammation and allergy. Curr Opin Immunol 2014; 31:31-37.
- Lohning M SA, Coyle AJ, Grogan JL, Lin S, Gutierrez-Ramos JC, et al. T1/ST2 is preferentially expressed on murine Th2 cells, independent of interleukin 4, interleukin 5, and interleukin 10, and important for Th2 effector function. Proc Natl Acad Sci USA 1998.
- Xu D, Chan WL, Leung BP, Huang F, Wheeler R, Piedrafita D, et al. Selective expression of a stable cell surface molecule on type 2 but not type 1 helper T cells. J Exp Med 1998; 187(5):787-794.
- Weinberg EO, Shimpo M, De Keulenaer GW, MacGillivray C, Tominaga S, Solomon SD, et al. Expression and regulation of ST2, an interleukin-1 receptor family member, in cardiomyocytes and myocardial infarction. Circulation 2002; 106(23):2961-2966.
- Griesenauer B, Paczesny S. The ST2/IL-33 Axis in Immune Cells during Inflammatory Diseases. Front Immunol 2017; 8:475.
- Neill DR, Wong SH, Bellosi A, Flynn RJ, Daly M, Langford TK, et al. Nuocytes represent a new innate effector leukocyte that mediates type-2 immunity. Nature 2010; 464(7293):1367-1370.
- Schiering C, Krausgruber T, Chomka A, Fröhlich A, Adelmann K, Wohlfert EA, et al. The alarmin IL-33 promotes regulatory T-cell function in the intestine. Nature 2014; 513(7519):564-568.
- Pastille E, Wasmer MH, Adamczyk A, Vu VP, Mager LF, Phuong NNT, et al. The IL-33/ST2 pathway shapes the regulatory T cell phenotype to promote intestinal cancer. Mucosal Immunol 2019; 12(4):990-1003.
- Bourgeois E, Van, L. P., Samson, M., Diem, S., Barra, A., Roga, S., Gombert, M., Schneider, E., Dy, M., Gourdy, P., Girard, P., & Herbelin, A. The pro-Th2 cytokine IL-33 directly interacts with invariant NKT and NK cells to induce IFN-γ production. European Journal of Immunology 2009; 39(4):1046-1055.
- Zou L, Dang W, Tao Y, Zhao H, Yang B, Xu X, et al. THE IL-33/ST2 AXIS PROMOTES ACUTE RESPIRATORY DISTRESS SYNDROME BY NATURAL KILLER T CELLS. Shock 2023; 59(6):902-911.
- Baumann C, Bonilla WV, Fröhlich A, Helmstetter C, Peine M, Hegazy AN, et al. T-bet- and STAT4-dependent IL-33 receptor expression directly promotes antiviral Th1 cell responses. Proc Natl Acad Sci U S A 2015; 112(13):4056-4061.
- Dwyer GK, D'Cruz LM, Turnquist HR. Emerging Functions of IL-33 in Homeostasis and Immunity. Annu Rev Immunol 2022; 40:15-43.
- Brunner TM, Serve S, Marx AF, Fadejeva J, Saikali P, Dzamukova M, et al. A type 1 immunity-restricted promoter of the IL-33 receptor gene directs antiviral T-cell responses. Nat Immunol 2024; 25(2):256-267.
- Gesta S, Tseng YH, Kahn CR. Developmental origin of fat: tracking obesity to its source. Cell 2007; 131(2):242-256.
- Rosen ED, Spiegelman BM. What we talk about when we talk about fat. Cell 2014; 156(1-2):20-44.
- Frontini A, Cinti S. Distribution and development of brown adipocytes in the murine and human adipose organ. Cell Metab 2010; 11(4):253-256.
- Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med 2013; 34(1):1-11.
- Ferrante, AW. The immune cells in adipose tissue. Diabetes Obes Metab 2013; 15 Suppl 3(0 3):34-38.
- Michailidou Z, Gomez-Salazar M, Alexaki VI. Innate Immune Cells in the Adipose Tissue in Health and Metabolic Disease. J Innate Immun 2022; 14(1):4-30.
- Man K, Kallies A, Vasanthakumar A. Resident and migratory adipose immune cells control systemic metabolism and thermogenesis. Cell Mol Immunol 2022; 19(3):421-431.
- Mathis, D. Immunological goings-on in visceral adipose tissue. Cell Metab 2013; 17(6):851-859.
- Deiuliis J, Shah Z, Shah N, Needleman B, Mikami D, Narula V, et al. Visceral adipose inflammation in obesity is associated with critical alterations in tregulatory cell numbers. PLoS One 2011; 6(1):e16376.
- Anderson NM, Simon MC. The tumor microenvironment. Curr Biol 2020; 30(16):R921-R925.
- Truffi M, Sorrentino L, Corsi F. Fibroblasts in the Tumor Microenvironment. Adv Exp Med Biol 2020; 1234:15-29.
- Lu B, Yang M, Wang Q. Interleukin-33 in tumorigenesis, tumor immune evasion, and cancer immunotherapy. J Mol Med (Berl) 2016; 94(5):535-543.
- Ali S, Huber M, Kollewe C, Bischoff SC, Falk W, Martin MU. IL-1 receptor accessory protein is essential for IL-33-induced activation of T lymphocytes and mast cells. Proc Natl Acad Sci U S A 2007; 104(47):18660-18665.
- Chackerian AA, Oldham ER, Murphy EE, Schmitz J, Pflanz S, Kastelein RA. IL-1 receptor accessory protein and ST2 comprise the IL-33 receptor complex. J Immunol 2007; 179(4):2551-2555.
- Seki K, Sanada S, Kudinova AY, Steinhauser ML, Handa V, Gannon J, et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ Heart Fail 2009; 2(6):684-691.
- Zarezadeh Mehrabadi A, Shahba F, Khorramdelazad H, Aghamohammadi N, Karimi M, Bagherzadeh K, et al. Interleukin-1 receptor accessory protein (IL-1RAP): A magic bullet candidate for immunotherapy of human malignancies. Crit Rev Oncol Hematol 2024; 193:104200.
- Choi YS, Choi HJ, Min JK, Pyun BJ, Maeng YS, Park H, et al. Interleukin-33 induces angiogenesis and vascular permeability through ST2/TRAF6-mediated endothelial nitric oxide production. Blood 2009; 114(14):3117-3126.
- Artru F, Bou Saleh M, Maggiotto F, Lassailly G, Ningarhari M, Demaret J, et al. IL-33/ST2 pathway regulates neutrophil migration and predicts outcome in patients with severe alcoholic hepatitis. J Hepatol 2020; 72(6):1052-1061.
- Zeyda M, Wernly B, Demyanets S, Kaun C, Hämmerle M, Hantusch B, et al. Severe obesity increases adipose tissue expression of interleukin-33 and its receptor ST2, both predominantly detectable in endothelial cells of human adipose tissue. Int J Obes (Lond) 2013; 37(5):658-665.
- Kwon JW, Seok SH, Kim S, An HW, Choudhury AD, Woo SH, et al. A synergistic partnership between IL-33/ST2 and Wnt pathway through Bcl-xL drives gastric cancer stemness and metastasis. Oncogene 2023; 42(7):501-515.
- Yang Q, Li G, Zhu Y, Liu L, Chen E, Turnquist H, et al. IL-33 synergizes with TCR and IL-12 signaling to promote the effector function of CD8+ T cells. Eur J Immunol 2011; 41(11):3351-3360.
- Smithgall MD, Comeau MR, Yoon BR, Kaufman D, Armitage R, Smith DE. IL-33 amplifies both Th1- and Th2-type responses through its activity on human basophils, allergen-reactive Th2 cells, iNKT and NK cells. Int Immunol 2008; 20(8):1019-1030.
- Arrizabalaga L, Risson A, Ezcurra-Hualde M, Aranda F, Berraondo P. Unveiling the multifaceted antitumor effects of interleukin 33. Front Immunol 2024; 15:1425282.
- Peng L, Sun W, Wei F, Chen L, Wen W. Interleukin-33 modulates immune responses in cutaneous melanoma in a context-specific way. Aging (Albany NY) 2021; 13(5):6740-6751.
- Schuijs MJ, Png S, Richard AC, Tsyben A, Hamm G, Stockis J, et al. ILC2-driven innate immune checkpoint mechanism antagonizes NK cell antimetastatic function in the lung. Nat Immunol 2020; 21(9):998-1009.
- Gao K, Li X, Zhang L, Bai L, Dong W, Shi G, et al. Transgenic expression of IL-33 activates CD8(+) T cells and NK cells and inhibits tumor growth and metastasis in mice. Cancer Lett 2013; 335(2):463-471.
- Gao X, Wang X, Yang Q, Zhao X, Wen W, Li G, et al. Tumoral expression of IL-33 inhibits tumor growth and modifies the tumor microenvironment through CD8+ T and NK cells. J Immunol 2015; 194(1):438-445.
- Lucarini V, Ziccheddu G, Macchia I, La Sorsa V, Peschiaroli F, Buccione C, et al. IL-33 restricts tumor growth and inhibits pulmonary metastasis in melanoma-bearing mice through eosinophils. Oncoimmunology 2017; 6(6):e1317420.
- Dominguez D, Ye C, Geng Z, Chen S, Fan J, Qin L, et al. Exogenous IL-33 Restores Dendritic Cell Activation and Maturation in Established Cancer. J Immunol 2017; 198(3):1365-1375.
- Briukhovetska D, Dörr J, Endres S, Libby P, Dinarello CA, Kobold S. Interleukins in cancer: from biology to therapy. Nat Rev Cancer 2021; 21(8):481-499.
- Hatzioannou A, Banos A, Sakelaropoulos T, Fedonidis C, Vidali MS, Köhne M, et al. An intrinsic role of IL-33 in T. Nat Immunol 2020; 21(1):75-85.
- Yeoh WJ, Vu VP, Krebs P. IL-33 biology in cancer: An update and future perspectives. Cytokine 2022; 157:155961.
- Miller, AM. Role of IL-33 in inflammation and disease. Journal of Inflammation (London, England) 2011; 8(22).
- Milovanovic M, Volarevic V, Radosavljevic G, Jovanovic I, Pejnovic N, Arsenijevic N, et al. IL-33/ST2 axis in inflammation and immunopathology. Immunol Res 2012; 52(1-2):89-99.
- O'Donnell C, Mahmoud A, Keane J, Murphy C, White D, Carey S, et al. An antitumorigenic role for the IL-33 receptor, ST2L, in colon cancer. Br J Cancer 2016; 114(1):37-43.
- Kurowska-Stolarska M KP, Murphy G, Russo RC, Stolarski B, Garcia CC, Komai-Koma M, Pitman N, Li Y, Niedbala W. et al. IL-33 induces antigen-specific IL-5+ T cells and promotes allergic-induced airway inflammation independent of IL-4. J Immunol 2008:4780–4790.
- Kokubo K, Onodera, A., Kiuchi, M., Tsuji, K., Hirahara, K., & Nakayama, T. Conventional and pathogenic Th2 cells in inflammation, tissue repair, and fibrosis Frontiers in immunology 2022; 13.
- Stark JM, Tibbitt CA, Coquet JM. The Metabolic Requirements of Th2 Cell Differentiation. Frontiers in Immunology 2019; 10.
- Pelaia C, Paoletti, G., Puggioni, F., Racca, F., Pelaia, G., Canonica, G. W., & Heffler, E. Interleukin-5 in the Pathophysiology of Severe Asthma. Frontiers in Physiology 2019; 10.
- Setrerrahmane S, Xu H. Tumor-related interleukins: old validated targets for new anti-cancer drug development. Mol Cancer 2017; 16(1):153.
- Joshi BH, Leland P, Lababidi S, Varrichio F, Puri RK. Interleukin-4 receptor alpha overexpression in human bladder cancer correlates with the pathological grade and stage of the disease. Cancer Med 2014; 3(6):1615-1628.
- Prokopchuk O, Liu Y, Henne-Bruns D, Kornmann M. Interleukin-4 enhances proliferation of human pancreatic cancer cells: evidence for autocrine and paracrine actions. Br J Cancer 2005; 92(5):921-928.
- Todaro M, Lombardo Y, Francipane MG, Alea MP, Cammareri P, Iovino F, et al. Apoptosis resistance in epithelial tumors is mediated by tumor-cell-derived interleukin-4. Cell Death Differ 2008; 15(4):762-772.
- Pavord CEBaDDaID. Cytokine-Specific Therapy in Asthma. Middleton's Allergy (Eighth Edition) 2014:1491-1502.
- Gour N, & Wills-Karp, M. IL-4 and IL-13 signaling in allergic airway disease. Cytokine 2015; 75(1):68-78.
- A. SM. Interleukin-13 Stimulation Reveals the Cellular and Functional Plasticity of the Airway Epithelium. Annals of the American Thoracic Society 2018; 15(Suppl 2):S98–S102.
- Doran E, Cai, F., Holweg, C. T. J., Wong, K., Brumm, J., & Arron, J. R. Interleukin-13 in Asthma and Other Eosinophilic Disorders. Frontiers in medicine 2017; 4:139.
- Knudson KM, Hwang S, McCann MS, Joshi BH, Husain SR, Puri RK. Recent Advances in IL-13Rα2-Directed Cancer Immunotherapy. Front Immunol 2022; 13:878365.
- Alvarez F, Fritz, J. H., & Piccirillo, C. A. Pleiotropic Effects of IL-33 on CD4+ T Cell Differentiation and Effector Functions. rontiers in immunology 2019; 10(522).
- Zhou Z, Yan, F., & Liu, O. Interleukin (IL)-33: An orchestrator of immunity from host defence to tissue homeostasis. Clinical & Translational Immunology 2020; 9(6).
- Kang MH, Bae YS. IL-33 and IL-33-derived DC-based tumor immunotherapy. Exp Mol Med 2024; 56(6):1340-1347.
- Andreone S, Spadaro F, Buccione C, Mancini J, Tinari A, Sestili P, et al. IL-33 Promotes CD11b/CD18-Mediated Adhesion of Eosinophils to Cancer Cells and Synapse-Polarized Degranulation Leading to Tumor Cell Killing. Cancers (Basel) 2019; 11(11).
- Marichal T, Tsai M, Galli SJ. Mast cells: potential positive and negative roles in tumor biology. Cancer Immunol Res 2013; 1(5):269-279.
- Ribatti, D. Mast Cells and Resistance to Immunotherapy in Cancer. Arch Immunol Ther Exp (Warsz) 2023; 71(1):11.
- Lv Y, Tian W, Teng Y, Wang P, Zhao Y, Li Z, et al. Tumor-infiltrating mast cells stimulate ICOS. J Adv Res 2024; 57:149-162.
- Andreone S, Gambardella, A. R., Mancini, J., Loffredo, S., Marcella, S., La Sorsa, V., Varricchi, G., Schiavoni, G., & Mattei, F. Anti-Tumorigenic Activities of IL-33: A Mechanistic Insight. Frontiers in immunology 2020; 11, 571593.
- Afferni C, Buccione C, Andreone S, Galdiero MR, Varricchi G, Marone G, et al. The Pleiotropic Immunomodulatory Functions of IL-33 and Its Implications in Tumor Immunity. Front Immunol 2018; 9:2601.
- Schneider E, Petit-Bertron AF, Bricard R, Levasseur M, Ramadan A, Girard JP, et al. IL-33 activates unprimed murine basophils directly in vitro and induces their in vivo expansion indirectly by promoting hematopoietic growth factor production. J Immunol 2009; 183(6):3591-3597.
- Pecaric-Petkovic T, Didichenko SA, Kaempfer S, Spiegl N, Dahinden CA. Human basophils and eosinophils are the direct target leukocytes of the novel IL-1 family member IL-33. Blood 2009; 113(7):1526-1534.
- Rivellese F, Suurmond J, de Paulis A, Marone G, Huizinga TW, Toes RE. IgE and IL-33-mediated triggering of human basophils inhibits TLR4-induced monocyte activation. Eur J Immunol 2014; 44(10):3045-3055.
- Afferni C BC, Andreone S, Galdiero MR, Varricchi G, Marone G, Mattei F, Schiavoni G. The Pleiotropic Immunomodulatory Functions of IL-33 and Its Implications in Tumor Immunity. Frontiers in immunology 2018; 9(2601).
- Prete AD, Salvi, V., Soriani, A., Laffranchi, M., Sozio, F., Bosisio, D., & Sozzani, S. Dendritic cell subsets in cancer immunity and tumor antigen sensing. Cellular and Molecular Immunology 2023; 20(5):432-447.
- Xu H, Li, D., Ma, J., Zhao, Y., Xu, L., Tian, R., Liu, Y., Sun, L., & Su, J. The IL-33/ST2 axis affects tumor growth by regulating mitophagy in macrophages and reprogramming their polarization. Cancer Biology & Medicine 2021; 18(1):172-183.
- Chen J ZY, Jiang Y, et al. Interleukin-33 Contributes to the Induction of Th9 Cells and Antitumor Efficacy by Dectin-1-Activated Dendritic Cells. Front Immunol 2018.
- Zhang X, Chen, W., Zeng, P., Xu, J., & Diao, H. The Contradictory Role of Interleukin-33 in Immune Cells and Tumor Immunity. Cancer management and research 2020; 12:7527-7537.
- Liu X, Li L, Si F, Huang L, Zhao Y, Zhang C, et al. NK and NKT cells have distinct properties and functions in cancer. Oncogene 2021; 40(27):4521-4537.
- Choi MR, Sosman, J. A., & Zhang, B.. The Janus Face of IL-33 Signaling in Tumor Development and Immune Escape. Cancers 2021; 13(13):3281.
- Zhang X CW, Zeng P, Xu J, Diao H. The Contradictory Role of Interleukin-33 in Immune Cells and Tumor Immunity. 2020.
- Stojanovic B, Gajovic, N., Jurisevic, M., Stojanovic, M. D., Jovanovic, M., Jovanovic, I., Stojanovic, B. S., & Milosevic, B. Decoding the IL-33/ST2 Axis: Its Impact on the Immune Landscape of Breast Cancer. International Journal of Molecular Sciences 2023; 24(18).
- Xiao P, Wan, X., Cui, B., Liu, Y., Qiu, C., Rong, J., Zheng, M., Song, Y., Chen, L., He, J., Tan, Q., Wang, X., Shao, X., Liu, Y., Cao, X., & Wang, Q. Interleukin 33 in tumor microenvironment is crucial for the accumulation and function of myeloid-derived suppressor cells. Oncoimmunology 2016; 5(1).
- Komai-Koma M, Wang, E., Kurowska-Stolarska, M., Li, D., McSharry, C., & Xu, D. Interleukin-33 promoting Th1 lymphocyte differentiation dependents on IL-12. Immunobiology 2016; 221(3):412–417.
- Wu X, Tian J, Wang S. Insight Into Non-Pathogenic Th17 Cells in Autoimmune Diseases. Front Immunol 2018; 9:1112.
- Xing J, Man C, Liu Y, Zhang Z, Peng H. Factors impacting the benefits and pathogenicity of Th17 cells in the tumor microenvironment. Front Immunol 2023; 14:1224269.
- Pascual-Reguant A, Bayat Sarmadi J, Baumann C, Noster R, Cirera-Salinas D, Curato C, et al. T. Mucosal Immunol 2017; 10(6):1431-1442.
- Guo H BE, Ma X, Zhao C, Zhao Y. Dual Immune Regulatory Roles of Interleukin-33 in Pathological Conditions. Cells 2022.
- Lei S, Jin J, Zhao X, Zhou L, Qi G, Yang J. The role of IL-33/ST2 signaling in the tumor microenvironment and Treg immunotherapy. Exp Biol Med (Maywood) 2022; 247(20):1810-1818.
- Chen CC, Kobayashi, T., Iijima, K., Hsu, F. C., & Kita, H. IL-33 dysregulates regulatory T cells and impairs established immunologic tolerance in the lungs. The Journal of allergy and clinical immunology 2017; 140(5):1351–1363.e1357.
- Shani O, Vorobyov T, Monteran L, Lavie D, Cohen N, Raz Y, et al. Fibroblast-Derived IL33 Facilitates Breast Cancer Metastasis by Modifying the Immune Microenvironment and Driving Type 2 Immunity. Cancer Res 2020; 80(23):5317-5329.
- Monteran L, Erez N. The Dark Side of Fibroblasts: Cancer-Associated Fibroblasts as Mediators of Immunosuppression in the Tumor Microenvironment. Front Immunol 2019; 10:1835.
- Chen SF, Nieh S, Jao SW, Wu MZ, Liu CL, Chang YC, et al. The paracrine effect of cancer-associated fibroblast-induced interleukin-33 regulates the invasiveness of head and neck squamous cell carcinoma. J Pathol 2013; 231(2):180-189.
- Peng L, Sun W, Chen L, Wen WP. The Role of Interleukin-33 in Head and Neck Squamous Cell Carcinoma Is Determined by Its Cellular Sources in the Tumor Microenvironment. Front Oncol 2020; 10:588454.
- Andersson P, Yang Y, Hosaka K, Zhang Y, Fischer C, Braun H, et al. Molecular mechanisms of IL-33-mediated stromal interactions in cancer metastasis. JCI Insight 2018; 3(20).
- He Z, Chen L, Souto FO, Canasto-Chibuque C, Bongers G, Deshpande M, et al. Epithelial-derived IL-33 promotes intestinal tumorigenesis in Apc. Sci Rep 2017; 7(1):5520.
- Chen L, Sun R, Xu J, Zhai W, Zhang D, Yang M, et al. Tumor-Derived IL33 Promotes Tissue-Resident CD8. Cancer Immunol Res 2020; 8(11):1381-1392.
- Yang M, Feng Y, Yue C, Xu B, Chen L, Jiang J, et al. Lower expression level of IL-33 is associated with poor prognosis of pulmonary adenocarcinoma. PLoS One 2018; 13(3):e0193428.
- Liu J, Shen JX, Hu JL, Huang WH, Zhang GJ. Significance of interleukin-33 and its related cytokines in patients with breast cancers. Front Immunol 2014; 5:141.
- Kim JY, Kim G, Lim SC, Choi HS. IL-33-Induced Transcriptional Activation of LPIN1 Accelerates Breast Tumorigenesis. Cancers (Basel) 2021; 13(9).
- Kirichenko TV, Markina, Y. V., Bogatyreva, A. I., Tolstik, T. V., Varaeva, Y. R., & Starodubova, A. V. The Role of Adipokines in Inflammatory Mechanisms of Obesity. International journal of molecular sciences 2022; 23(23).
- Schmidt FM, Weschenfelder, J., Sander, C., Minkwitz, J., Thormann, J., Chittka, T., Mergl, R., Kirkby, K. C., Faßhauer, M., Stumvoll, M., Holdt, L. M., Teupser, D., Hegerl, U., & Himmerich, H.. Inflammatory Cytokines in General and Central Obesity and Modulating Effects of Physical Activity. PLoS ONE 2015; 10(3).
- Kim JW, Kim, J. H., & Lee, Y. J. The Role of Adipokines in Tumor Progression and Its Association with Obesity. Biomedicines 2024; 12(1):97.
- Molofsky AB, Van Gool F, Liang HE, Van Dyken SJ, Nussbaum JC, Lee J, et al. Interleukin-33 and Interferon-γ Counter-Regulate Group 2 Innate Lymphoid Cell Activation during Immune Perturbation. Immunity 2015; 43(1):161-174.
- Odegaard JI, Lee MW, Sogawa Y, Bertholet AM, Locksley RM, Weinberg DE, et al. Perinatal Licensing of Thermogenesis by IL-33 and ST2. Cell 2016; 166(4):841-854.
- Li Q, Li D, Zhang X, Wan Q, Zhang W, Zheng M, et al. E3 Ligase VHL Promotes Group 2 Innate Lymphoid Cell Maturation and Function via Glycolysis Inhibition and Induction of Interleukin-33 Receptor. Immunity 2018; 48(2):258-270.e255.
- Brestoff JR, Kim BS, Saenz SA, Stine RR, Monticelli LA, Sonnenberg GF, et al. Group 2 innate lymphoid cells promote beiging of white adipose tissue and limit obesity. Nature 2015; 519(7542):242-246.
- Lee MW, Odegaard JI, Mukundan L, Qiu Y, Molofsky AB, Nussbaum JC, et al. Activated type 2 innate lymphoid cells regulate beige fat biogenesis. Cell 2015; 160(1-2):74-87.
- Miller AM, Asquith DL, Hueber AJ, Anderson LA, Holmes WM, McKenzie AN, et al. Interleukin-33 induces protective effects in adipose tissue inflammation during obesity in mice. Circ Res 2010; 107(5):650-658.
- Wang L, Luo Y, Luo L, Wu D, Ding X, Zheng H, et al. Adiponectin restrains ILC2 activation by AMPK-mediated feedback inhibition of IL-33 signaling. J Exp Med 2021; 218(2).
- Brestoff JR, Kim, B. S., Saenz, S. A., Stine, R. R., Monticelli, L. A., Sonnenberg, G. F., Thome, J. J., Farber, D. L., Lutfy, K., Seale, P., & Artis, D. Group 2 innate lymphoid cells promote beiging of white adipose tissue and limit obesity. Nature 2015; 519(7542):242-246.
- de Oliveira MFA, Talvani, A., & Rocha-Vieira, E. IL-33 in obesity: where do we go from here? Inflammation research : official journal of the European Histamine Research Society [et al] 2019; 68(3):185-194.
- Sanada S HD, Higgins LJ, Schreiter ER, McKenzie AN, Lee RT. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. Clin Investig 2007:1538-1549.
- Miller AM XD, Asquith DL, Denby L, Li Y, Sattar N, Baker AH, McInnes IB, Liew FY. IL-33 reduces the development of atherosclerosis. J Exp Med 2008:339-346.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




