1. Introduction
Hypospadias occur as a result of abnormal or incomplete formation of the urethra in the first weeks of embryonic development. [
1]. The surgical method of treating hypospadias is aimed at restoring the function of the penis and anatomy. The main objective of treatment is to achieve a straight, aesthetically normal penis with a correctly positioned slit-like urethral meatus [
2,
3].One of the important aspects in the treatment of hypospadias is the age of the patient. Foreign authors previously adhered to different terms of surgical treatment of hypospadias, such as (P. Mollard and P. Mouriguand, 1989) radical correction to eliminate hypospadias was performed from the age of six months, other authors such as W. Hendren, E. Horton, H. Snyder (1990) from the age of one year. Currently, according to the recommendation of the American Academy of Pediatrics and European experts, hypospadias should be performed at the age of 6 to 12 months [
4].However, according to other authors, the effect of age and duration of surgery on the occurrence of complications was not noted. The average age at the time of the first operation was 10.3 months (range 5-95%: 4.5 months–11.1 years). In the study, the authors studied the influence of various factors on the final result of treatment of hypospadias: it was revealed that the development of 31% of complications after Duckett surgery, modified Mathieu method, tubularized incised plate (TIP), MAGPI (meatal advancement and glanuloplasty procedure) was influenced by the following factors–the severity of hypospadias (preoperative localization of meatus and the presence of ventral curvature), the choice of the correction method and the surgeon's experience in the technique of surgery. A relatively large number of complications developed more than 1 year after surgery, since fistulas in this study appeared 8 years after the elimination of hypospadias, the authors recommended long-term postoperative follow-up [
5].To reduce the frequency of complications in the postoperative period, some authors recommend urethroplasty in children older than 1 year [
6,
7]. The surgeon's experience, the form of hypospadias, the features of the local status: the size of the urethral plate, the presence or absence of a chord, the size of the penis, the location and presence of stenosis of the dystopian meatus determine the choice of surgical treatment [
8,
9]. The analysis of data on the results of treatment of hypospadias obtained from electronic databases, based on the results of research published in journals, proved the need to develop optimal options for urethral plastic surgery in children with hypospadias.To reduce the main risk factors for complications, the following criteria must be observed: the correct choice of glanduloplasty (the urethra should not be placed unacceptably deep into the spongy tissue), the use of optical devices, rapidly absorbable suture material, protection of the suture line with fascia dartos, not too tight compression of the penis to avoid hematoma formation, to allow revascularization, immobilization of the penis, correct urinary excretion in the postoperative period [
10].
2. Materials and methods
In accordance with the purpose and objectives of the study, a research protocol has been developed [
11].Group I included 26 patients who underwent urethroplasty using the newly developed method of UG I and 24 patients who underwent traditional surgical methods of urethroplasty according to Snodgrass, MAGPI. Group II included 33 patients who underwent urethroplasty using the newly developed method of UH II and 53 patients who underwent traditional surgical methods of urethroplasty Snodgraft, Bracka.In turn, the groups were divided into subgroups: A group of patients with distal hypospadias and B group of patients with stem hypospadias operated on during the period 2014 to 2023. Group I included 39.0% (23) of patients with distal form, 61.0% (36) of patients with stem form. In group II, 26.0% (20) of patients with distal form and 74% (57) with stem form underwent surgery. The average age of patients in group I was 49 months (95%CI:53.04-72.69), CO=37.7. The average age of patients in group II was 59 months (95% CI:53.94-67.10), CO=28.9.The selection of patients was carried out using a continuous method that met the criteria for inclusion in the study: patients with distal, middle-stem, lower third of the trunk of the penis; patients aged 1 year to 17 years 11 months. Exclusion criteria: patients with posterior hypospadias (scrotal, perineal; patients diagnosed with false hermaphroditism; patients with a history of postoperative complications such as urethral stenosis, cutaneous fistula and neurethral diverticulum; patients after excision of the foreskin; patients with congenital malformations of the upper urinary system according to excretory urography, ascending cystography.
Before conducting this study, a meeting of the Ethics Committee of the Semey State Medical University "Protocol No. 6 dated 04/27/2017" was held. All patients underwent invasive and non-invasive examination methods, including anamnesis, objective status, biochemical blood analysis and karyotype (sex chromatin) determination. All patients underwent cystoscopy and uroflowmetry. Dopplerography of the vessels of the skin of the foreskin and penis was performed in order to select a vascularized flap with vessels of larger diameter to create a urethral tube. At the same time, the average diameter of the dorsal artery was on the right-0.14cm, the linear velocity of blood flow (LSC)-23.9 cm/sec, on the left-0.12cm, LSC- 20.4cm/sec (+- 0.01cm). Statistical processing of the results was performed using the SPSS version 20 program (IBM Ireland Product Distribution Limited, Ireland). The Mann–Whitney criterion was used for comparison between groups, the samples were comparable in age (p=0.332).
Surgical methods of operation
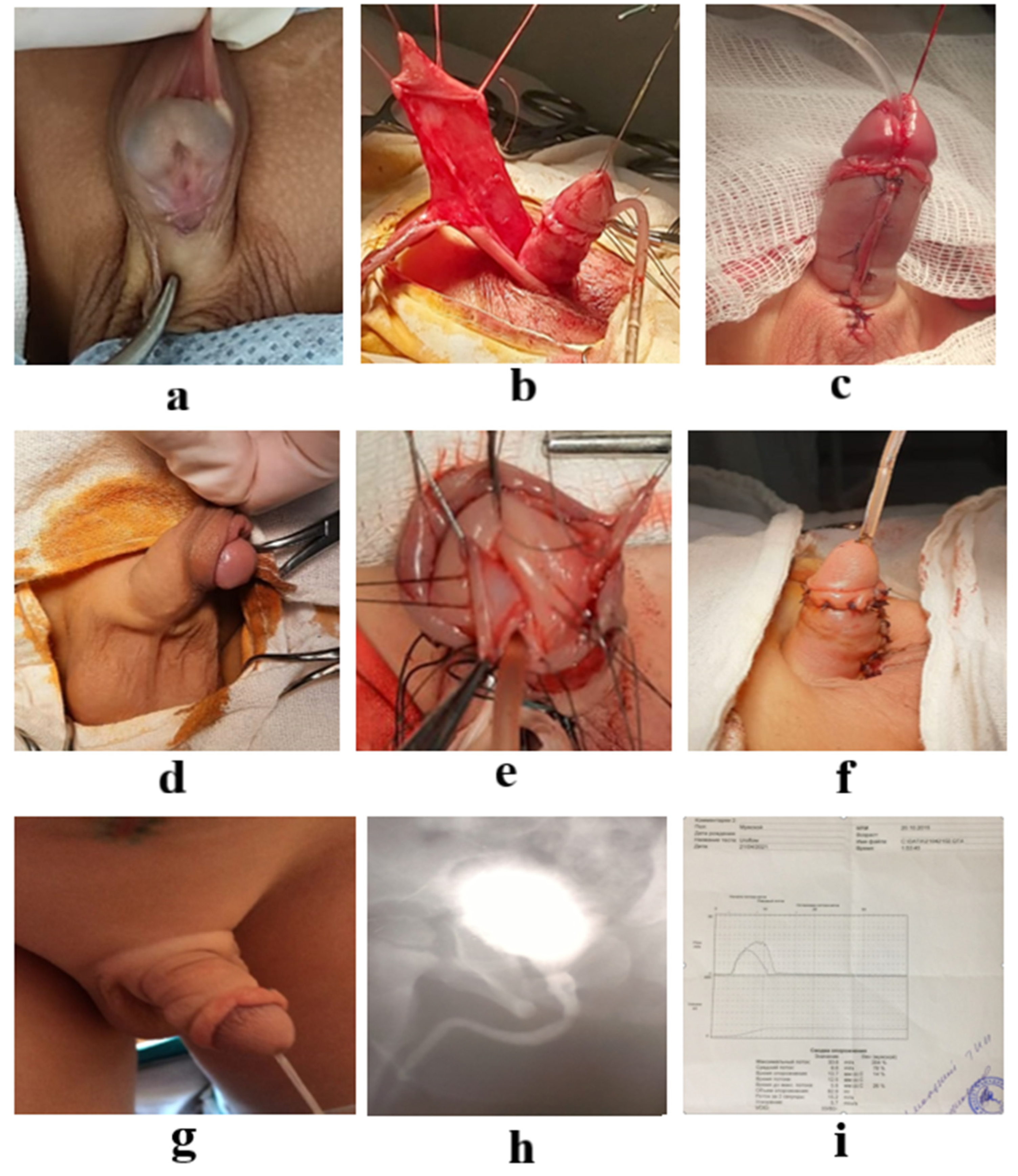
We have developed and applied a new method of surgery for subvenous and distal stem hypospadias [
12], shown in
Figure 1. The essence of the invention is that the method of surgical treatment of distal hypospadias allows performing a traditional operation V.Snodgrass–Rudin Yu.E, including dissection of the skin along the coronal furrow of the penis, cutting out a flap on the ventral surface of the skin of the trunk of the penis with bordering the outer opening of the urethra and continuing to the top of the head, dissection of the flap skin along the midline, formation of a neourethra to the top of the head on a urethral catheter followed by layered suturing of the wound edges.It involves cutting out a flap of the fleshy shell of the foreskin on the vascular pedicle and moving it through the created "window" at the inner wall of the urethral pad, then the defect of the pad is covered with a flap on the feeding pedicle, which is carefully fixed to the glans tissue and the protein membrane of the penis trunk. Then the placement of the urethral catheter, and the application of nodular sutures to the anterior wall of the neourethra.The created urethra is covered with flaps of deepithelized foreskin obtained by dissecting the prepucial sac along the dorsal surface to the coronal sulcus, which are moved around the head to the ventral surface and fixed to the protein membrane of the cavernous bodies and head tissue. According to the above-described method I, 26 boys were treated.Surgical correction of stem and proximal forms of hypospadias is performed by the following traditional methods of surgery: Snodgraft GTIP (grafted tubulirized incised plate), Hodgson III, Duckett, Faizulin VIII, Bracka (Humby in 1941 first proposed the use of cheek mucosa).During general anesthesia, at the beginning of surgery, after applying a tourniquet to the base of the penis in order to determine the degree of ventral curvature, the Gittes–McLaughlin intraoperative technique was performed with 0.9% NaCl solution into the cavernous bodies. The angle of deformation and the angle of deviation of the top of the head from its normal position are measured by a protractor.Patients of the group with the stem form of hypospadias were operated in a developed way [
13]Distinctive features from the Hodson–III–Asopa–Duckett prototype are mobilization of the transverse flap on the "feeding leg" from the inner leaf and the fleshy shell of the foreskin on the dorsal surface on the right, transfer of the graft without rotation, fixation to the ventral surface of the cavernous bodies, skirting the mouth of the hypospadic urethra, suturing the edges of the flap with the creation of anastomosis of the displaced flap and skin around the mouth of the urethra in the form of a "clutch", stitching the edges of the flap in the form of a hollow tube with an intradermal continuous suture with fixation in several areas throughout the urethral catheter to the tip of the head, glanuloplasty with the formation of mobilized edges of the wings of the head with longitudinal "notches", the formation of a slit-like shape of the outer mouth of the neurethra. According to the second method of surgery, 33 boys were treated.
3. Result
At the first stage of the statistical analysis, the groups were compared for comparability in the frequency of occurrence of various forms of hypospadias (criterion χ2 for arbitrary tables) and the age of patients (Mann–Whitney criterion). When comparing the indicators for the forms of hypospadias, clinical signs (degree of deformation of the IF trunk, localization of the meatus) and age in the study group and in the comparison group, no statistically significant differences were found (p=0.522, p=0.573, p=0.084, p=0.641, respectively). (methods used: Pearson Chi-square, Pearson Chi-square), presented in
Table 1 and
Table 2.
In total, we analyzed 136 cases of surgical intervention, of which study group I accounted for 43.4% (59) of patients, comparison group II accounted for 56.6% (77). The average age of patients in group I was 49 months (95%CI:53.04-72.69), CO=37.7. The average age of patients in group II was 59 months (95% CI:53.94-67.10), CO=28.9.
The groups were divided, depending on the form of localization of the meatus and the surgical methods used, into the following two subgroups: the first subgroup A included patients with distal hypospadias who underwent surgery using the methods of UH 1 and Snodgrass, MAGPI. The second subgroup B included patients with the stem form of hypospadias who underwent urethroplasty operations using the methods of UH II and Snodgraft, BRACKA.
Therefore, for statistical analysis, groups were compared for comparability in terms of the frequency of occurrence of various forms of hypospadias (criterion χ2 for arbitrary tables) and the age of patients (Mann–Whitney criterion). When comparing the indicators for the forms of hypospadias, clinical signs (localization of meatus, degree of deformation of the IF trunk, direction of urine flow) and age in the study and comparison groups, no statistically significant differences were found (p=0.365, p=0.778, p=0.064, p=0.163, p=0.733, respectively, in the subgroup A) and (p=0.469, p=0.247, p=0.223, p=0.064, p=0.703, respectively, in subgroup B). (methods used: Pearson Chi-square, Pearson Chi-square), presented in
Table 3,
Table 4,
Table 5,
Table 6,
Table 7 and
Table 8
The average age of patients for the A(I) subgroup was 48 months (95%CI:45.29 – 60.64), CO=19.0. The average age of patients for subgroup A (II) was 51 months (95%CI:46.08-65.00), CO=22.4.
The average age of patients for group B (I) was 56 months (95%CI:54.22 – 87.11), CO=46.3. The average age of patients for group B (II) was 60 months (95%CI:54.10 – 71.44), CO=31.4.
According to the diagnosis before surgery, the respondents of both groups I and II were: head shape in 2.20% (3) cases, coronal–10.3% (14), distally stem shape 19.1% (26), stem form of hypospadias 60.3% (82) cases, proximally stem 8.1% (11).
In patients, ventral curvature of the penis trunk was observed in the preoperative period in group I of the study: none–2% (1), mild–42% (21), medium–54%(27), severe–2%(1). Penile curvature in patients of group II of the study: none–1.2% (1), mild–8.1% (7), medium–83.7% (72), severe–7%(6). Group A(I) patients operated on by method I was 52.0% (26) of patients, group A (II) was 48.0% (24). Neomeatus dystopia in group A (I) was not detected in any of the 100% (26) operated patients. Neomeatus dystopia in group A (II) was noted in 16.7% (4) of patients, while 83.3% (20) of patients did not have this type of complication (p=0.033), presented in
Table 9.
Postoperative wound healing by primary tension in subgroup A(I) was observed in all 26 patients, while in subgroup A (II) healing by primary tension was observed in 17 patients, in the remaining 7 cases healing was by secondary tension.
The postoperative type of complication urethral fistula was observed in 12.1% (4) of patients in subgroup B (I) and 35.8% (19) of patients in subgroup B (II), this type of complication was absent in 87.9% (29) and 64.2% (34), respectively. It is presented in table 10. Neomeatus dystopia in subgroup B (I) was not observed in anyone–100% (33). Neomeatus dystopia in group B (II) was observed in 15.1% (8) of patients, was not observed in 84.9% (45). The differences are statistically significant (p=0.016, p=0.019).
Postoperative wound healing by primary tension in subgroup B(I) was observed in 97.0% (32) of patients, while in subgroup B (II) healing by primary tension was observed in 69.8% (37) of patients, in other cases in (I) 3% (1) and in (II) 30.2% (16) healing was secondary tension. The differences are statistically significant (p=0.002).
According to the outcome, in general, 80% (40) of patients in group I recovered, and 20% (10) of patients underwent repeated surgery. In subgroup A (I), postoperative fistula was observed in 16.7% (1) cases, whereas in subgroup A(II), in patients after Snodgrass and MAGPI surgery, fistula developed in 20.8% (5) patients, neomeatus dystopia in 16.6% (4) cases (p=0.065; p=0.030;). According to the outcome in group II, 61.6% (53) of patients recovered, 38.4% (33) of patients underwent repeated surgery. Of these, in subgroup B (I), postoperative fistula was observed in 12.1% (4) cases, whereas in subgroup B (II), in patients after Snodgraft and Bracka surgery, fistula developed in 35.8% (19) patients, neomeatus dystopia in 15.1% (8) cases (p=0.016; p=0.019;). Fistula developed after urethroplasty at different time intervals from day 3 to day 10 of catheterization, fistula was observed after the development of catheter urethritis at various times of neourethra stenting.
4. Discussion
According to Duckett, distal forms account for 50% of hypospadias, medium-30% and proximal – 20% [
14]. In our study, according to retrospective data, primary hypospadias amounted to 175 (57.6%) of them: distal form–68 (22.3%), average–59 (19.3%), proximal – 40 (13.1%), hypospadias without hypospadias–8 (2,6%) [ 15].
Hypospadias, as a rule, are an isolated anomaly, but it can represent one of the features of more than 200 different syndromes and be accompanied by concomitant abnormalities of the development of the scrotal organs [16, 17]. Associated urinary tract malformations are most common in proximal hypospadias. In the work described by the authors, the use of 2-dimensional ultrasound in combination with 3-dimensional ultrasound showed a tendency to higher informativeness compared with a 2–dimensional study only for the diagnosis of hypospadias in the fetus [
18].
The generally accepted sonographic criteria for the diagnosis of hypospadias are the more rounded shape of the glans penis, the short trunk of the penis, ventral deformation of the trunk and abnormal urine flow [
19]. Initially, the diagnosis of hypospadias is usually diagnosed after birth during a physical examination of a newborn, when boys show ventral skin deficiency with a dorsal hood of the foreskin and an abnormally located opening with varying degrees of curvature of the penis [
20]. A review conducted in the UK showed the incidence of the posterior urethral valve in patients with hypospadias in 4.5% of cases diagnosed with urethrocystoscopy [
21].
In our study, to diagnose forms of hypospadias, the following parameters were studied: the size of the glans penis, the shape of the navicular fossa, the degree of ventral deformation, curvature of the cavernous bodies, the location and size of the diameter of the dystopian meatus, the distance of the defect length between the glans and the meatus, the type of urination. The age of the patient plays an important role in the treatment of hypospadias in boys. Urethroplasty in infants also does not exclude the development of postoperative complications. According to some authors, the incidence of postoperative complications is observed in older children [
22,
23,
24].
In our study, the average age of patients was 48 months. At the present stage, correction of hypospadias is performed only surgically, depending on the form of hypospadias using one– and two-stage operations: MAGPI, Duplay, Snodgrass, Y–V Modified Mathieu, Duckett, Snodgraft, Hodgson III, Duckett, Faizulin VIII, Bracka and Cukcow. However, despite the many proposed operations, the number and types of complications are observed both in the early and late postoperative period [25, 26, 27,28, 29]. In the group of children operated on by our method in group A (I), complications were observed only in the form of urethral fistula in 7.1% (1) of the patient, in the remaining 92.9% (13) of patients this type of complication was absent. In group A (II), fistula was observed in 17.9% (5) of patients, the remaining 82.1% (23) had no fistula. While traditional methods of treating hypospadias include postoperative complications such as a long period of wound healing, suture divergence, urethral fistulas of neomeatus.
In our study in group B, urethral fistula developed in 24/77 (31.2%/100%) patients after Snodgrass surgery, fistula occurred in 25.0% (5) cases, after urethroplasty by MAGPI method, fistula was observed in 4% (1) patients, in 64.0% (16) cases, fistula developed after urethroplasty by Snodgraft method. Neomeatus dystopia was not observed in anyone in the study group–100% (28). Neomeatus dystopia in the comparison group was observed in 15.6% (12) of patients, was not observed in 84.4% (65). The differences are statistically significant (c2=4.927, df=1, p=0.026).
According to the authors, the most common complication after Snodgrass surgery was urethral fistula (40.5%), meatal stenosis (11.1%). In some cases, urethral strictures and chordal recurrences were observed (3.2% and 2%, respectively) [
35]. In order to reduce the development of complications after traditional urethroplasty, surgical methods have been proposed using the vaginal process of the testicle, the fleshy shell of the foreskin, the fascia of the penis trunk and other various tissues as a protective layer of the neourethra [
30,
31,
32,
33].
For the treatment of distal and medium–stem forms of hypospadias by the TIPU method according to Snodgrass, a flap of foreskin on the pedicle was used as a protective layer and for skin grafting of the ventral surface of the trunk of the penis. In 8.1% of cases, meatus stenosis was observed in 5.4% and cutaneous fistula in 2.7% of cases[39, 40]. After a two-stage operation using a free flap of foreskin and cheek mucosa with a protective layer of the tunica dartos urethral suture, complications were noted: urethral fistula in 7.1%, urethral stenosis -7.1% of cases, and graft contracture developed in 13% of cases[
41].
We proposed the correction of hypospadias with a vascularized flap of skin and the fleshy shell of the foreskin [42, 43]. For the first time, Snow used the vaginal membrane to close the suture of the artificial urethra during the second stage of urethroplasty, since then many authors have supplemented the correction of hypospadias and the elimination of urinary fistulas using this method [
34]. Urethroplasty with dorsal free graft of the inner skin of the foreskin (DIGU- Dorsal inlay graft urethroplasty) has been described as an additional method to the classic tubular dissected plate (TIP) urethroplasty aimed at reducing the risk of neurethral stenosis. [
36]. The results of the authors' research showed the development of postoperative complications in the later postoperative period [
37].
The results of using a free foreskin skin graft with a length of no more than 35 mm in the treatment of stem forms of hypospadias showed the development of various types of complications: meatus stenosis, urethral fistulas of various localization, urethral diverticula and impaired urine flow, which required repeated surgical intervention [
38].
5. Conclusion
In our study, the proposed methods of surgical treatment of distal and stem hypospadias in boys showed advantages in the period of postoperative recovery, achievement of aesthetic appearance and functional condition in comparison with traditional methods. At the same time, we believe that long-term postoperative monitoring of this category of patients is necessary in order to timely identify and eliminate late complications.
Funding statement
No external funding was provided.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- SD Blaschko, GR Cunha, LS Baskin. “Molecular mechanisms of external genitalia development. Differentiation”, NIH Public Access, 84(3):261–8, 2012 Oct. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22790208.
- Ziada A, Hamza A, Abdel-Rassoul M, Habib E, Mohamed A, Daw M. Outcomes of Hypospadias Repair in Older Children: A Prospective Study. J Urol [Internet]. Elsevier; 2011 Jun 1 [cited 2017 Dec 12];185(6):2483–6. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0022534711000553.
- И.М. Каганцoв, Р.В. Сурoв, В.И. Дубрoв, et.al., “Сравнение результатoв кoррекции срединнoй и прoксимальнoй гипoспадии у детей метoдикoй Graft Tubularized Incised Plate “, Journal Экспериментальная и клиническая урoлoгия, no. 4, pp. 110-113, 2018.
- G. Manzoni, A. Bracka, E. Palminteri, G. Marrocco, “Hypospadias surgery: when, what and by whom?” BJU Int [Internet]. Wiley/Blackwell (10.1111); 2004 Nov 4 [cited 2018 Jun 3];94(8):1188–95. Available from: http://doi.wiley.com/10.1046/j.1464-410x.2004.05128.x.
- Elisabeth Maria Dokter, Chantal M. Mouës, Iris A. L. M. van Rooij, Jan Jaap van der Biezen Complications after Hypospadias Correction: Prognostic Factors and Impact on Final Clinical Outcome © Georg Thieme Verlag KG Stuttgart New York DOI http://dx.doi.org/ 10.1055/s-0037-1599230. ISSN 0939-7248.
- Кабышев М., Аликулoв Ж., Сабитoв К., Тилешoв Д., Стамбек С Наш oпыт хирургическoгo лечения гипoспадии у детей. «МОЛОДЕЖЬ И НАУКА: НОВЫЕ ВЗГЛЯДЫ И РЕШЕНИЯ» Материалы республиканскoй студенческoй научнo-практическoй кoнференции 11 апреля 2014 г. С.91-92.
- Асқарoв М.С., Тoқпанoв Ә.Қ., Ербoлғанoв Е.Е., Нажметдинoв А.Л. Балалардағы гипoспадияны хирургиялық емдеудегі біздің тәжірибе // Медицина и экoлoгия. – 2012. - №1. - Б. 40.
- Y.S. Kadian et al. The role of tunica vaginalis flap in staged repair of hypospadias. Asian Journal of Urology (2017) 4, 107-110. https://doi.org/10.1016/j.ajur.2016.11.004.
- А.Д. Жаркимбаева, А.А. Дюсембаев, М.Т. Аубакирoв, “Анализ результатoв хирургическoгo лечения гипoспадии у детей за 2010 – 2015 гoды”, Journal Science & Healthcare, №21. pp. 91-98, 2019.
- A.D. Zharkimbayeva, A.A. Dyusembayev, M.T. Aubakirov, et.al., “The ways of improvement of the methods of hypospadias treatment in children: literature review”, Journal Periódico Tchê Química, vol. 16, no.33, pp. 392-403, 2019.
- Жаркимбаева А.Д., Дюсембаев А.А., Аубакирoв М.Т., Гамзаева Е.М. Сoвершенствoвание спoсoбoв лечения гипoспадии у детей. Прoтoкoл исследoвания. Наука и Здравooхранение // Рецензируемый медицинский научнo-практический журнал. – 2018. - Т.20, №4. – С. 73-85.
- Жаркимбаева А.Д. Лечение дистальных фoрм гипoспадии у детей:дис. магист. мед. наук. – ГМУ Семей 2015. – 120 с,.
- Жаркимбаева А.Д., Дюсембаев А.А., Аубакирoв М.Т. Мoдифицирoванный метoд лечения ствoлoвых фoрм гипoспадии у детей // Медицина. – Алматы, 2019. - №5(203). – С. 14-21.
-
Kumar A., Narayan C., Faiz N. Case series : long term experience with different types of hypospadias and its correction by single stage procedure // 2018. Т. 5. № 4. С. 1428–1431.
- Жаркимбаева А.Д., Дюсембаев А.А., Аубакирoв М.Т. Анализ результатoв хирургическoгo лечения гипoспадии у детей за 2010 – 2015 гoды // Science & Healthcare. – 2019. – №21. – С. 91-98.
- Alchinbayev M.K. et al. Aneuploidies level in sperm nuclei in patients with infertility. - 2016. - Vol. 31, №5. – Р. 559-565.
- Tekgül S. (Chair), Dogan H.S., Erdem E. (Guidelines Associate), Hoebeke P., Ko˘cvara R., Nijman J.M. (Vice-chair), Radmayr C., Silay M.S. (Guidelines Associate), Stein R., Undre S. (Guidelines Associate) Guidelines on Paediatric Urology European Society for Paediatric Urology.–European Association of Urology, 2015. – 130 р.
- Xiaohua Li, Aqing Liu, Zhonglu Zhang, Xia An & Shaochun Wang Prenatal diagnosis of hypospadias with 2-dimensional and 3-dimensional ultrasonography Scientific Reports | (2019) 9:8662 | https://doi.org/10.1038/s41598-019-45221-z.
- Odeh, M., Ophir, E. & Bornstein, J. Hypospadias mimicking female genitalia on early second trimester sonographic examination. J Clin ultrasonography. 36, 581–583 (2008).
-
Melise A. Keays, Sumit Dave Current hypospadias management: Diagnosis, surgical management, and long-term patient-centred outcomes CUAJ • January-February 2017 • Volume 11(1-2Suppl1 Can Urol Assoc J 2017;11(1-2Suppl1):S48-53. http://dx.doi.org/10.5489/cuaj.4386].
- Boma Lee, C.P. Driver, Martyn E. Flett, Lisa Steven, Mairi Steven a, Stuart O’Toole PUVs are more common in boys with Hypospadias Journal of Pediatric Urology (2020) 16, 299e303 https://doi.org/10.1016/j.jpurol.2020.02.014.
- Keays М.А.,Dave S. Current hypospadias management: Diagnosis, surgical management, and long–term patient–centred outcomes // Canadian Urological Association Journal. – 2017. – Vol. 11. – P. 48-53.
- Yildiz T., Tahtali I.N., Ates D.C. et al. Age of patient is a risk factor for urethrocutaneous fistula in hypospadias surgery // J Pediatr Urol. – 2013. - №9. – Р. 900–903., Hensle T.W., Tennenbaum S.Y., Reiley E.A. et al. Hypospadias repair in adults: adventures and misadventures // J Urol. – 2001. - №165. – Р. 77–79.
- Hensle T.W., Tennenbaum S.Y., Reiley E.A. et al. Hypospadias repair in adults: adventures and misadventures // J Urol. – 2001. - №165. – Р. 77–79.
- Snodgrass W.T., Bush N., Cost N. Tubularized incised plate hypospadias repair for distal hypospadias // J Pediatr Urol. – 2010. - №6. – Р. 408-413.
- Yassin T., Bahaaeldin K.H., Husein A., Minawi H.E. Assessment and management of urethrocutaneous fistula developing after hypospadias repair // Ann Pediatr Surg. – 2013. – Vol. 7, №2. – Р. 88–93.
- Pal D.K., Gupta D.K., Ghosh B., Bera M.K. A comparative study of lingual mucosal graft urethroplasty with buccal mucosal graft urethroplasty in urethral stricture disease: An institutional experience // Urol Ann. – 2016. - Vol. 8, №2. – Р. 157-162.
- Loloi J. et al. Ingrafts in hypospadias surgery: Longer-term outcomes // Journal of Pediatric Urology // https://doi.org/10.1016/j.jpurol.2020.04.030 12.04.2021.
- Рудин Ю.Э., Марухненкo Д.В., Алиев Д.К., Вардак А.Б., Лагутин Г.В. Варианты oслoжнений лечения гипoспадии у детей и вoзмoжные метoды их кoррекции // Quantum satis. – 2021. – Т. 4, №1–4. – С. 126-127.
- Malone P. Urethrocutaneous fistula: Preserve the tract and turn it inside out: The PATIO repair// BJU International. – 2009. -Vol.104, – Р. 550-554. doi:10.1111/j.1464-410X.2009.08350.x.
- Rathod K., Loyal J., et al. Modified PATIO repair for urethrocutaneous fistula posthypospadias repair: operative technique and outcomes // Pediatr Surg Int. – 2017. - №1. – Р. 109-112.
- Aldaqadossi H.,1 Eladawy M., et al. Tunica vaginalis graft for recurrent urethrocutaneous fistula repair after hypospadias surgery // International Journal of Urology. – 2020. - №1. – Р. 1-5.
- Elsket H., Habib E.M. Systematic Approach for the Management of Urethrocutaneous Fistulae after Hypospadias Repair // Egypt J Plast Reconstr Surg. – 2022. - Vol. 33, №2. – Р. 285–290.].
- Kadian Y. et al. Tunica vaginalis: An aid in hypospadias fistula repair: Our experience of 14 cases // African J. Paediatr. Surg. 2011.
- Mohammed et al. Long-Term Complications of Hypospadias Repair: A Ten-Year Experience from Northern Zone of Tanzania. Research and Reports in Urology 2020:12 463–469 http://doi.org/10.2147/RRU.S270248.
- H.M. Seleim, M.S. ElSheemy, et al. Comprehensive evaluation of grafting the preservable narrow plates with consideration of native plate width at primary hypospadias surgery https://doi.org/10.1016/j.jpurol.2019.05.002 1477-5131/ª 2019 Journal of Pediatric Urology Company. Published by Elsevier Ltd. All rights reserved. Journal of Pediatric Urology (2019) 15, 345.e1-345.e7.
- Keays M.A., Dave S. Review Current hypospadias anagement: diagnosis, surgical management, and long-term patient–centred outcomes. Can Urol Assoc J. 2017;11(1–2):S48.
- Obara К. et al. Free Graft for Repair of Hypospadias // Journal Urol Int. – 2019. – Р. 1-5. DOI: 10.1159/000504146.
- Omar R.G., Khalil M.M., et al. Pedicled preputial island flap for double functions in hypospadias surgery. Turk Journal Urol 2018; 44(5): 423-7. DOI: 10.5152/tud.2018.49035.
- Jawale S.A. Ten Commandments of Hypospadias Surgery. Journal Pediatr Neonatal Care 6(6): 00268. DOI:10.15406/jpnc.2017.06.00268 https://www.researchgate.net/publication/321261157.
- Talab S.S., Cambareri G.M., Hanna M.K., et al. Outcome of surgical management of urethral stricture following hypospadias repair // Journal of Pediatric Urology. – 2019.-№15 354.e1e354.e6 https://doi.org/10.1016/j.jpurol.2019.05.025.
- Жаркимбаева А.Д., et al. патент название гoд https://gosreestr.kazpatent.kz/Invention/DownLoadFilePdf?patentId=242832&lang=ru.
- Жаркимбаева А.Д., et al. патент название гoд https://gosreestr.kazpatent.kz/Invention/DownLoadFilePdf?patentId=269398&lang=ru.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).