1. Introduction
Perimenopause is defined as the period of time during which a woman’s body transitions towards menopause, or the final menstrual period. The beginning of the perimenopause phase is marked by the onset of menstrual irregularities, and menopause itself is retroactively confirmed after 12 months of amenorrhea. Perimenopause brings about a host of changes within the body mostly due to the decline in ovarian function, which results in decreased estrogen and progesterone production [
1]. The perimenopause phase is reported to last for an average of 4-7 years, though it can last up to 14 years, and the average age of menopause is between 45-51 years in the US [
1,
2].
Each year approximately 2 million women in the US enter perimenopause [
3]. As perimenopause begins, hormones fluctuate, triggering a broad range of unpleasant symptoms such as longer periods of bleeding, anxiety and depression, weight gain, changes in sexual desire, muscle aches, hot flashes and insomnia [
1,
4]. Most women experience a variety of such symptoms, but it is estimated that at least 20% of women experience symptoms to an extent which significantly impacts their quality of life [
5]. Women experiencing perimenopause and menopause symptoms have reported decreased work productivity, increased activity impairments, and significantly more physician visits compared to non-menopausal women [
6].
Hormone Replacement Therapy (HRT) is currently the most popular treatment for perimenopause symptoms and has been reported to significantly improve bothersome vasomotor symptoms such as hot flashes and sleep disturbances. HRT, similar to hormonal birth control, can be administered in various forms (i.e., oral pills, vaginal rings, patches, injections), can be given continuously or cyclically, and can contain estrogen, progesterone, or a combination of both [
7,
8]. Local estrogen treatment may also be prescribed for women who experience genitourinary symptoms such as urinary tract infections. In such cases, local estrogen therapy in the form of vaginal rings, creams, or tablets can help to alleviate symptoms. Non-hormonal treatments, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and gabapentin have also been shown to improve perimenopause symptoms, though few are FDA-approved for this purpose [
7].
Understanding perimenopause, including what to expect in terms of symptoms and treatment, can play an important role in the ability of women (and partners) to navigate this transitional period. Previous studies have reported a lack of education on menopause, resulting in worsened symptoms and suboptimal medical care during this time [
9,
10]. Within the past few years, several companies have developed at-home menopause hormone tests in an effort to provide women with more accessible and personalized information about their transitions through menopause. In this report, we investigate women’s level of familiarity with various aspects of perimenopause and menopause, as well as their feelings towards HRTs, at-home menopause testing tools, and their level of satisfaction with care from healthcare providers.
2. Results
2.1. Familiarity with Perimenopause
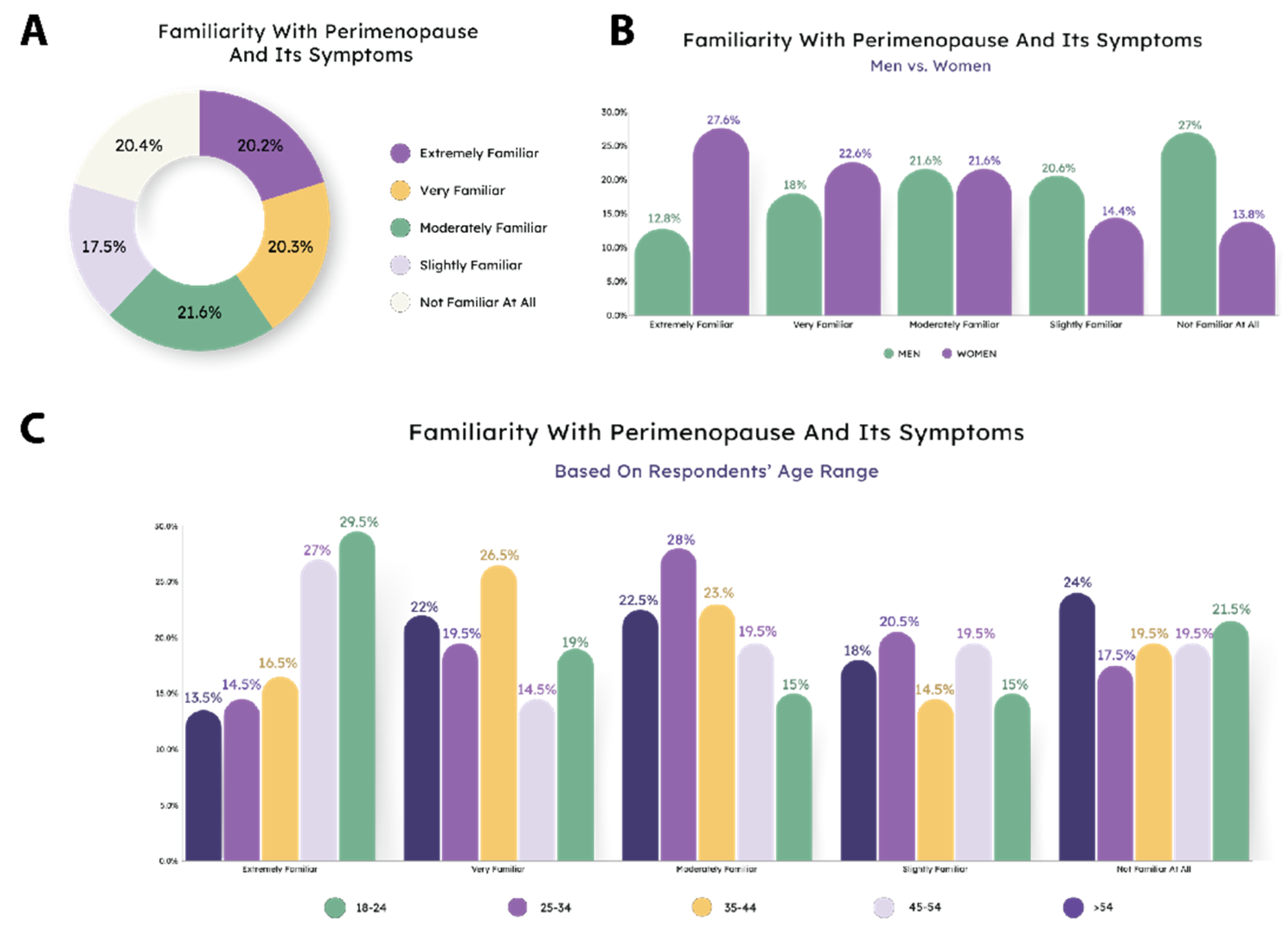
First, we evaluated how familiar the average person was with perimenopause and its symptoms, 20.20% reported being extremely familiar with perimenopause, similarly, 20.30% reported very familiar and 21.60% were moderately familiar. 17.50% were slightly familiar, followed by 20.40% who reported not being familiar with perimenopause at all (
Figure 1A). For men and women, percentages for perimenopause familiarity fluctuated, with the plurality of women being “extremely familiar” but the plurality of men being “not familiar at all.” (
Figure 1B). Interestingly, when results were divided by age, the youngest group (18-24) reported that they were the most familiar with perimenopause (
Figure 1C), and the oldest group had the highest percentage of people answering that they were not familiar with menopause symptoms at all.
2.2. Presumed Age and Duration of Perimenopause
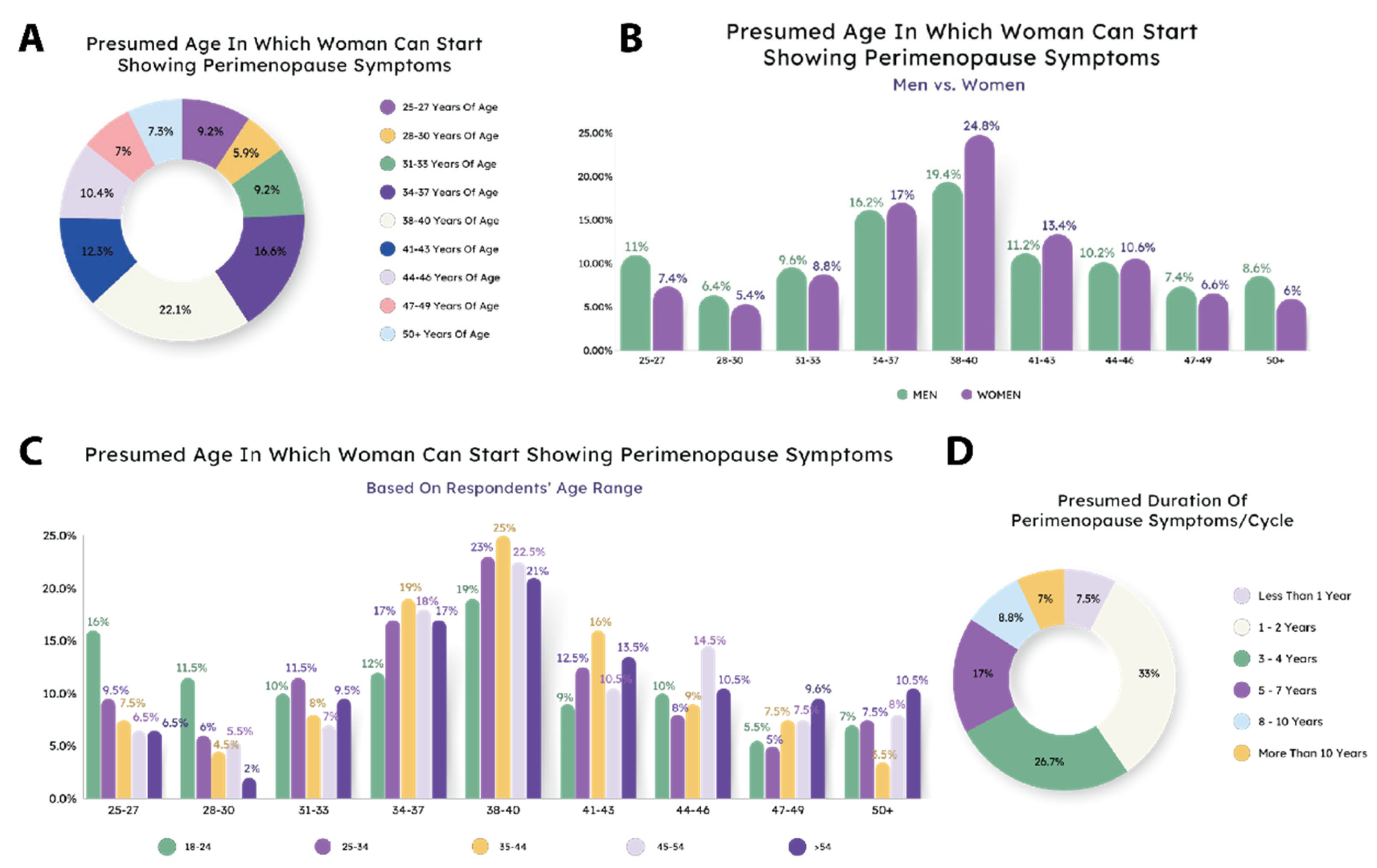
Currently, there is a relatively large discrepancy in the age at which a woman can begin showing perimenopause related symptoms, versus when people believe these symptoms can begin (
Figure 2A). The most common response was 38-40 years, but there were significant percentages of respondents who said perimenopause might begin as early as 25 years old. The actual average age of perimenopause onset is around 48 years old [
11]. Women were more likely to believe a later onset (although still earlier than average), whereas men were more likely to respond with a younger age (
Figure 2B). Younger respondents were also more likely to respond with a younger age, and older respondents with an older age. Interestingly, in nearly all age ranges, the age group corresponding with that range was the most likely to respond that range. For instance, 35-44 year olds were most likely to respond that 34-37, 38-40, or 41-43 was the age of onset of perimenopause (
Figure 2C). This indicates a potential disconnect between perception and reality of the onset of perimenopause.
Similarly, people tended to underestimate the duration of perimenopause. The average duration of symptoms is 4-8 years [
12], but the majority of respondents said either 1-2 or 3-4 years (
Figure 2D). This trend was consistent when broken out by gender and age (
Figure S1).
2.3. Familiarity with Treatment Options
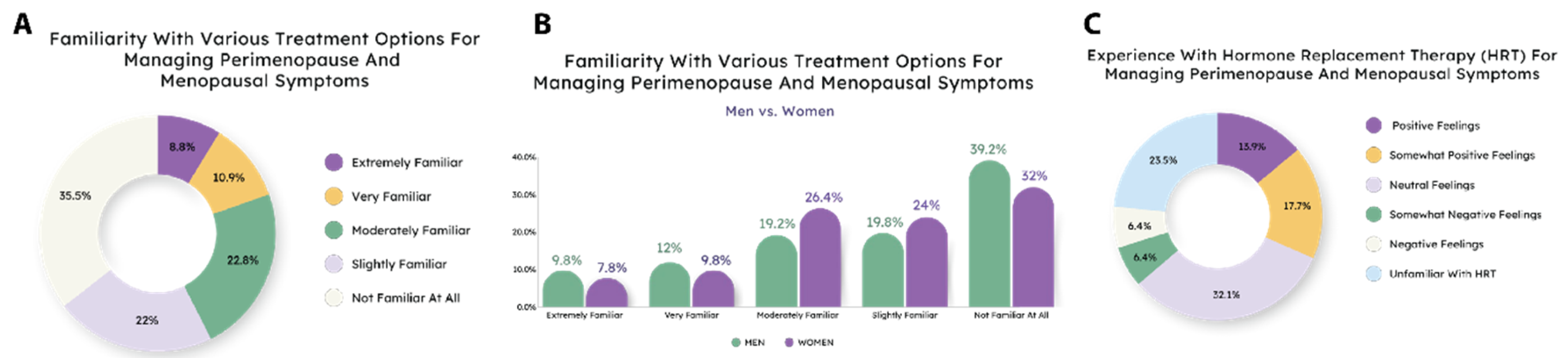
When assessing how familiar the average person was with the various treatment options for managing perimenopause and its symptoms, 35.5% reported having no familiarity with it. Additionally, 22% reported they were slightly familiar and 22.8% were moderately familiar. 10.9% were very familiar, followed by 8.8% who reported being extremely familiar with management options for perimenopause (
Figure 3A).
For men and women, the familiarity of treatment options for managing perimenopause differ slightly. 7.8% of women answered that they were extremely familiar, 9.8% were very familiar, 26.4% were moderately familiar, 24% were slightly familiar, and a majority of 32% were not familiar with management options for perimenopause at all. Correspondingly, only 9.8% of men were extremely familiar with perimenopause’s treatment options. 12% were very familiar, 19.2% of men were moderately familiar. 19.8% were slightly familiar and
—similar to women
—a majority of 39.2% of men were not familiar at all (
Figure 3B). All age groups responded similarly (
Figure S2A).
We then asked specifically about hormone replacement therapy (HRT). There is a diverse sentiment surrounding utilizing HRT as a treatment option for managing perimenopause. A large sum of people surveyed, 32.1%, reported they have neutral feelings about HRT. 13.9% stated having positive feelings about HRT and a slight increase of 17.7% have somewhat positive feelings about HRT. Equivalently, 6.4% of people reported having somewhat negative feelings about HRT and another 6.4% have a general negative feeling about HRT. Finally, 23.5% of people reported they do not know anything about HRT (
Figure 3C). Gender and age group results were similar (
Figure S2B, C).
2.4. Use of At-Home Tests for Perimenopause
At-home fertility and similar hormone tests are useful for assisting with screening for hormonal conditions and fertility status [
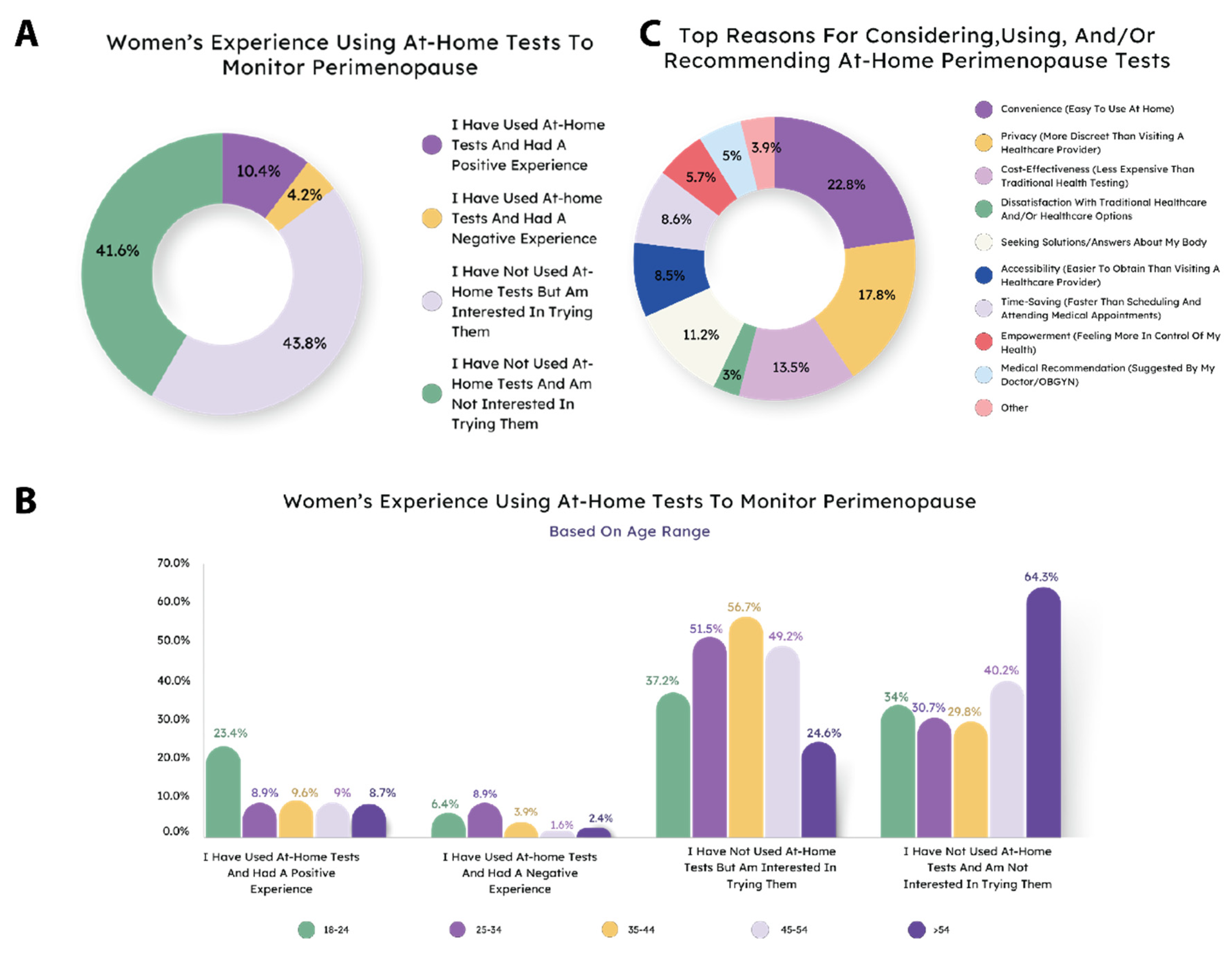
13]. Increasingly, at-home tests for perimenopause and related symptoms are becoming available. To assess their use and potential opportunities for at-home testing, we asked respondents if they had used at-home tests for perimenopause. The majority of respondents had not, but a plurity said they would be interested in trying them (
Figure S3A). Removing male respondants interestingly did not change the results (
Figure 4A,
Figure S3B,C). Interestingly, when responses from women were broken out by age, the 18-24 group was most likely to say they had used tests and had a positive experience. The 35-44 age group was most likely to say they were interested in using tests, but the 54+ age group was least likely to be interested in using the tests (
Figure 4B). When asked about reasons for using or recommending at-home perimenopause tests, women had a range of answers, but the most popular were convenience, privacy, and cost (
Figure 4C). These were typically consistent across age group and gender, with notable exceptions being that women were more likely to seek tests for answers about their body and the 54+ age group was the most likely to use the tests based on a medical recommendation (
Figure S4).
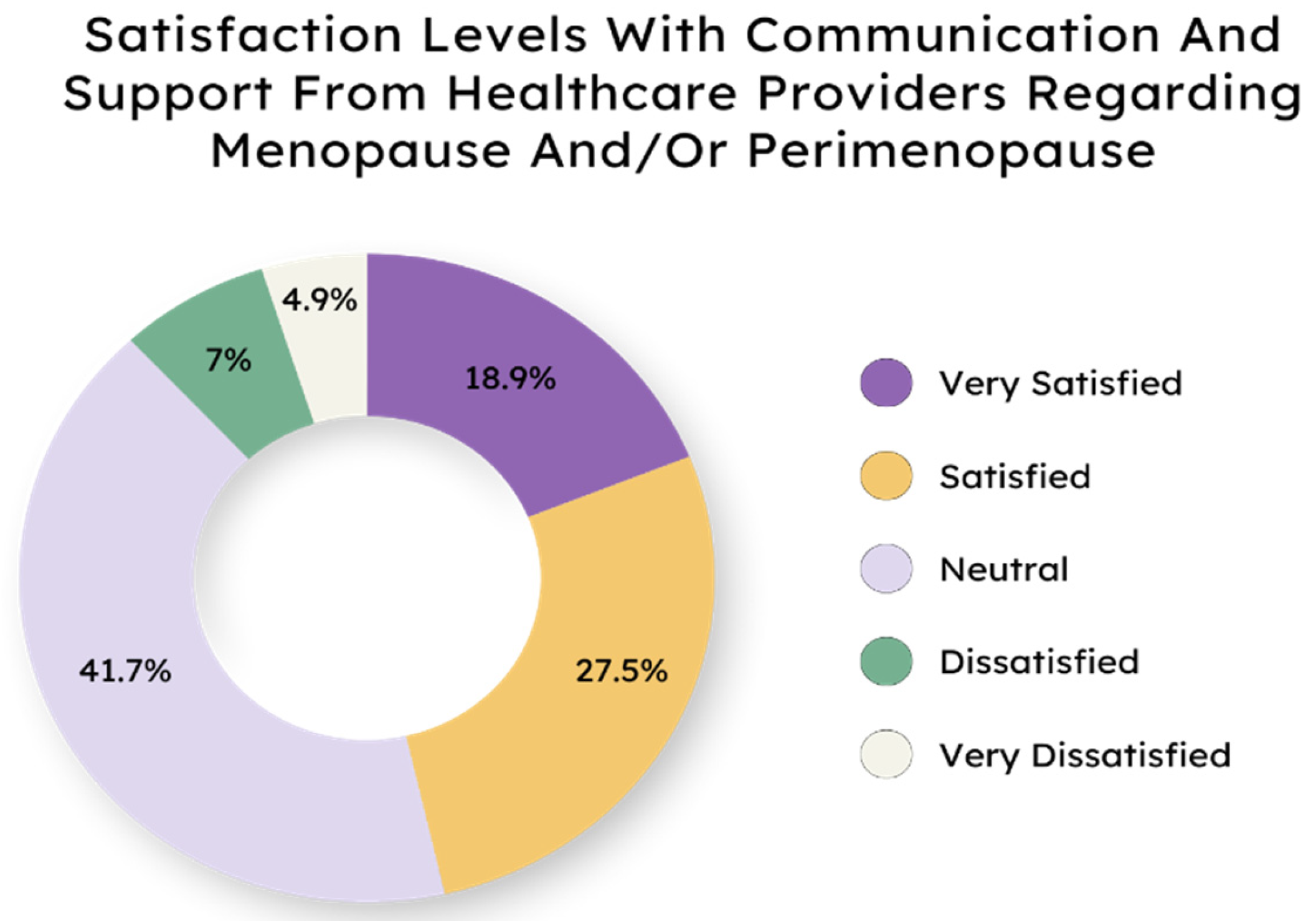
2.5. Satisfaction Regarding Healthcare Communication Surrounding Menopausal States
Finally, we wanted to assess if people were satisfied with the communication received from their health care providers with regard to menopause. Levels of satisfaction in individuals differed with regard to the communication about menopausal states
—such as the transition to menopause, known as perimenopause
—from their healthcare providers (
Figure 5). A majority of 41.7% of people stated they had neutral feelings about their provider’s communication and support around menopausal states. 27.5% reported they were satisfied and 18.9% noted they were very satisfied by the support and communication their provider provided. 7% of people stated they were dissatisfied and 4.9% reported they were very dissatisfied with their provider. Satisfaction levels did not differ greatly between genders, nor were there major discrepancies between age groups (
Figure S5).
3. Discussion
The collective data from this survey illustrate a significant gap in awareness and understanding of perimenopause and its management within the general population. Despite 75 million women in the U.S. currently living in a menopausal state, there is a concerning lack of knowledge about perimenopause, including when it begins, how long it lasts, and the available treatment options. This gap in understanding leaves many women unprepared to effectively manage their symptoms during this critical transition period.
The surveys reveal that nearly half of the women have little to no familiarity with perimenopause and its symptoms, with 59.5% of respondents indicating low to moderate awareness. This lack of knowledge is further reflected in the widespread misconceptions about the onset and duration of perimenopause. While the transition typically begins in a woma
n’s 40s and can last five to 10 years [
12], a significant portion of respondents believe it lasts less than four years, highlighting the need for better education on this topic.
The data show a concerning deficiency in awareness and use of treatment options. Only a small percentage of women are familiar with hormone replacement therapy (HRT), a key treatment for managing perimenopausal symptoms, with many expressing neutrality or unawareness towards it. This is compounded by the fact that 80.6% of respondents have never used an at-home test to monitor their symptoms, and 41.6% of women express no interest in trying such tests, despite the potential benefits they offer in managing hormonal fluctuations.
While a significant number of women report feeling neutral—neither satisfied nor dissatisfied—about the support they receive from healthcare providers regarding menopause and perimenopause, future directions could include investigating what information is provided to patients. This neutrality suggests a need for more proactive and informative communication from healthcare professionals to better support women during this transition.
The findings from these surveys clearly indicate that more extensive education and communication efforts are necessary to bridge the gap between the reality of perimenopause and the widespread lack of recognition and understanding it currently receives. Empowering women with accurate information and accessible treatment options will not only improve their quality of life but also reduce the stigma associated with this natural stage of life.
4. Materials and Methods
This cross-sectional survey was conducted over a period of less than one day in 2024, targeting a diverse population of 1,000 adults from the United States and Canada, including both men and women. Participants were selected using a convenience sampling method, with equal distribution between age groups and gender across the sample to ensure equal representation of various age groups and genders. The survey was conducted through an online platform in the form of multiple choice questions to gather both quantitative and qualitative data on participants’ opinions and experiences. The survey content is available in
Appendix A.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, A.B.; methodology, A.B, formal analysis, MG, AKW.; investigation, MG, resources, A.B..; data curation, AKW, MG.; writing—original draft preparation, MG, AKW.; writing—review and editing, AKW, AW.; visualization, AKW, supervision, AB.; project administration, AB, funding acquisition, AB. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Ethics statement
This study was conducted with the utmost regard for ethical standards and principles,
ensuring the rights, dignity, and well‐being of all participants were protected throughout the research process.
Participation in the survey was entirely voluntary, and informed consent was obtained from all participants
prior to their involvement. Participants were fully informed of the study’s purpose, procedures, and any
potential risks or benefits associated with their participation.
Confidentiality and anonymity were strictly maintained, with all personal identifying information removed
from the data to protect participants’ privacy. The data was stored securely and only accessible to authorized
researchers involved in the study. Any reporting of findings was done in a way that aggregated data and did
not identify individual respondents.
Data Availability
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We thank members of MFB Fertility and Jaya Jaya Myra Productions for thoughtful comments and visualization assistance.
Conflicts of Interest
A. Beckley is the CEO and founder of MFB Fertility, Inc. A. Wegrzynowicz and A. Walls are independent contractors with MFB Fertility.
Appendix A. Survey
- 1.
-
How familiar are you with perimenopause and its symptoms? (Perimenopause is the transition period before menopause when a woman’s hormone levels and menstrual cycles start to change.)
Extremely familiar
Very familiar
Moderately familiar
Slightly familiar
Not familiar at all
- 2.
-
What is the earliest age you believe a woman can start showing perimenopause symptoms (Perimenopause is the transition period before menopause when a woman’s hormone levels and menstrual cycles start to change)?
25-27
28-30
31-33
34-37
38-40
41-43
44-46
47-49
50 or older
- 3.
-
How many years do you think the transition to menopause (otherwise known as perimenopause) typically lasts?
Less than 1 year
1-2 years
3-4 years
5-7 years
8-10 years
More than 10 years
- 4.
-
How familiar are you with the treatment options that are available for managing perimenopause and menopausal symptoms?
Extremely familiar
Very familiar
Moderately familiar
Slightly familiar
Not familiar at all
- 5.
-
What has been your experience with using at-home tests to monitor perimenopause?
I have used at-home tests and had a positive experience
I have used at-home tests and had a negative experience
I have not used at-home tests but am interested in trying them
I have not used at-home tests and am not interested in them
- 6.
-
What is or would be your primary reason for considering or using at-home perimenopause tests? (Select all that apply.)
Convenience (easy to use at home)
Privacy (more discreet than visiting a healthcare provider)
Cost-effectiveness (less expensive than traditional health testing)
Dissatisfaction with traditional healthcare (not satisfied with current healthcare options)
Seeking solutions/answers about my body (wanting to understand my body better)
Accessibility (easier to obtain than visiting a healthcare provider)
Time-saving (faster than scheduling and attending medical appointments)
Empowerment (feeling more in control of my health)
Preference for home testing (prefer testing at home over clinical settings)
Medical recommendation (suggested by my doctor/OBGYN)
Other
- 7.
-
How satisfied are you with the communication and support from your healthcare provider regarding menopause or perimenopause?
Very satisfied
Satisfied
Neutral
Dissatisfied
Very dissatisfied
- 8.
-
What are your thoughts on hormone replacement therapy (HRT) for managing perimenopause and menopausal symptoms?
I have positive feelings about HRT
I have somewhat positive feelings about HRT
I have neutral feelings about HRT
I have somewhat negative feelings about HRT
I have negative feelings about HRT
I do not know anything about HRT
References
- Delamater, L.; Santoro, N. Management of the Perimenopause. Clin. Obstet. Gynecol. 2018, 61, 419–432. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.; Raval, A.P. The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. J. Neuroinflammation. 2020, 17, 317. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.D.; Marbella, A.; Wang, A.T.; Pines, E.; Hoag, J.; Bonnell, C.; Ziegler, K.M.; Aronson, N. (2015) Menopausal Symptoms: Comparative Effectiveness of Therapies, AHRQ Comparative Effectiveness Reviews, Agency for Healthcare Research and Quality (US), Rockville (MD), [online] http://www.ncbi.nlm.nih.gov/books/NBK285463/ (Accessed August 29, 2024).
- Santoro, N. Perimenopause: From Research to Practice. J. Womens Health. 2016, 25, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Avis, N.E.; Colvin, A.; Bromberger, J.T.; Hess, R.; Matthews, K.A.; Ory, M.; Schocken, M. Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women’s Health Across the Nation. Menopause N. Y. N. 2009, 16, 860–869. [Google Scholar] [CrossRef] [PubMed]
- Whiteley, J.; DiBonaventura M daCosta Wagner, J.-S.; Alvir, J.; Shah, S. The Impact of Menopausal Symptoms on Quality of Life, Productivity, and Economic Outcomes. J. Womens Health. 2013, 22, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Peacock, K.; Carlson, K.; Ketvertis, K.M. (2024) Menopause. in StatPearls, StatPearls Publishing, Treasure Island (FL), [online] http://www.ncbi.nlm.nih.gov/books/NBK507826/ (Accessed August 29, 2024).
- Troìa, L.; Martone, S.; Morgante, G.; Luisi, S. Management of perimenopause disorders: hormonal treatment. Gynecol. Endocrinol. 2021, 37, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Harper, J.C.; Phillips, S.; Biswakarma, R.; Yasmin, E.; Saridogan, E.; Radhakrishnan, S.; CDavies, M.; Talaulikar, V. An online survey of perimenopausal women to determine their attitudes and knowledge of the menopause. Womens Health. 2022, 18, 17455057221106890. [Google Scholar] [CrossRef] [PubMed]
- Koyuncu, T.; Unsal, A.; Arslantas, D. Evaluation of the Effectiveness of Health Education on Menopause Symptoms and Knowledge and Attitude in Terms of Menopause. J. Epidemiol. Glob. Health. 2018, 8, 8–12. [Google Scholar] [CrossRef] [PubMed]
- McKinlay, S.M.; Brambilla, D.J.; Posner, J.G. The normal menopause transition. Maturitas. 1992, 14, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Paramsothy, P.; Harlow, S.D.; Nan, B.; Greendale, G.A.; Santoro, N.; Crawford, S.L.; Gold, E.B.; Tepper, P.G.; Randolph, J.F. Duration of the menopausal transition is longer in women with young age at onset: the multi-ethnic Study of Women’s Health Across the Nation. Menopause N. Y. N. 2017, 24, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Wegrzynowicz, A.K.; Beckley, A.; Eyvazzadeh, A.; Levy, G.; Park, J.; Klein, J. (2022) Complete Cycle Mapping Using a Quantitative At-Home Hormone Monitoring System in Prediction of Fertile Days, Confirmation of Ovulation, and Screening for Ovulation Issues Preventing Conception. Med. Kaunas Lith. 5812. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).