1. Introduction Referencias Entre Corchetes, Sin Superíndice y Antes del Punto
Balance control is a complex motor skill that depends on interactions between multiple sensorimotor processes, as well as environmental and functional contexts. This motor skill can be affected in patients with certain conditions [
1,
2,
3]. Balance impairment and the fear of falling are the most common reasons for falls among vulnerable populations [
2]. Falls are a major public health problem and have a substantial financial impact on both individuals and communities [
4]. Approximately 28–35% of individuals aged ≥ 65 years experience falls every year [
5]. Furthermore, the global prevalence of Fear of Falling (FOF) is high (close to 50%), especially among patients in developing countries. Demographic characteristics, physical function, chronic diseases and mental health disorders are all significantly associated with FOF [
6].
Balance disturbance is common in patients with Fibromyalgia Syndrome (FMS); loss of balance is classified as one of the top ten most disabling symptoms of this syndrome with a reported prevalence of 45% [
7]. Recent studies have highlighted that FMS patients have an increased risk of losing their balance and falling compared to healthy individuals, demonstrating a Fall Risk Index (FRI) of 45%[
8]. Several studies have found an increased prevalence of falls in this population[
9,
10], while others have pointed to an alteration in sensory integration of visuo-vestibular information as a possible cause of balance disorder in FMS patients [
11,
12,
13]. Symptoms such as pain and chronic fatigue seem to have significant repercussions on proprioception in these patients, causing greater deterioration of their somatosensory system [
14] Although some studies have found a medium effect of exercise on improving balance in subjects with FMS [
15] only vestibular rehabilitation has shown signs of being effective in preventing falls [
16] Nevertheless, knowledge of the effectiveness of this therapy is still scarce.
Postural balance in subjects with FMS is evaluated with the same procedures used in other adult patients; these include posturography, subjective measurements and functional scales focused on objective evaluations. Recently, the ‘Joint Assessment of Equilibrium and Neuromotor Status’ (JAEN Scale) instrument was created to analyze postural balance in patients with FMS both quantitatively and qualitatively[
17] This scale is made up of 20 tests that rate performance using scores from “0” (normal functioning) to “4” (total limitation). The scale provides a total score ranging from 0-80 points and the higher the score, the greater the dysfunction. It should be noted that four subscale scores can also be extracted. The scale showed good psychometric properties, although the Cronbach’s alpha value could indicate redundancy in the items. Furthermore, the scale has excellent sensitivity to change after treatment with vestibular rehabilitation16 and is accepted as a good, functional evaluation instrument for FMS[
18].
Although the validation article of the JAEN Scale indicated that it takes 12- 13 minutes to complete, it could nonetheless induce fatigue in both patients and evaluators. Moreover, some of the test items could be redundant. In light of these factors, reducing the number of items on the scale would make the tool more user-friendly and efficient when measuring balance disorder and the risk of falls in subjects with FMS.
Therefore, the aim of this study was to develop and validate a short form of the JAEN scale that makes the process of measuring balance disorder more efficient, while maintaining its effectiveness. Additionally, the study intends to analyze the psychometric properties of the new instrument, including factorial validity, internal consistency, concurrent validity and diagnostic validity, for the discrimination of subjects with and without FMS, as well as fallers and non-fallers.
2. Materials and Methods
2.1. Study and Sample
To fulfil the objectives of this research, a cross-sectional validation study was designed. The study was carried out in compliance with all legal regulations and the principles of the Declaration of Helsinki. In addition, the protocol was approved by the Research Ethics Committee of the University of Jaen (protocol number JUL.23/6 PRY).
Patients with FMS were recruited from the Fibromyalgia Association of the city of Jaén (AFIXA) and had to meet the following inclusion criteria: (1) to be a woman (2) to be > 18 years old and (3) to fulfil all the diagnostic criteria for FMS, as described in the 2016 American College of Rheumatology (ACR) study. Healthy controls were recruited through advertisements on different social networks and had to fulfil the following inclusion criteria: (1) to be a woman, (2) to be > 18 years old and (3) to not fulfil the diagnostic criteria for FMS. The final sample included 100 women, of whom 56 had FMS and 44 were controls who did not have FMS.
The sample size calculation was performed using a criterion of recruitment of at least 10 subjects per item of the scale, with a minimum of 80 subjects for validity studies[
19].
2.2. Measurements
Anthropometric variables including age, weight and height were collected, from which the body mass index (BMI) was calculated.
To assess the impact of FMS on daily life, the Spanish version of the Fibromyalgia Impact Questionnaire (FIQ) was used. This FIQ assesses pain, rigidity, fatigue, depression and anxiety, disability, and general well- being related to FMS. It scores from 0 to 100, with 100 representing the maximum negative impact of the disease on the patient[
20].
To measure health-related quality of life in the entire patient sample, the Spanish version of the 12-Item Abbreviated Health Survey (SF-12) was used [
21] This tool is a self-administered questionnaire that was extracted from the SF-36 using multiple regression. The SF-12 consists of 12 items; its physical and mental component summaries (PCS-12 and MCS-12, respectively) each yield a single score.
Disability due to dizziness was measured with the Spanish version of the Dizziness Handicap Inventory (DHI)[
22]. This is a self-administered questionnaire comprising 25 questions that provide a total score from 0 to 100 points. The higher the score, the greater the disability due to dizziness. In addition to the total score, the emotional, functional and physical subscales can be extracted. The DHI is a very useful multidimensional tool to quantify disability in patients with vertigo, dizziness or instability, as well as the impact of these conditions on activities of daily living. The Spanish version of the DHI presents good psychometric properties (α = 0.87).
In this study, balance confidence was measured with the Spanish version of the Activity-specific Balance Confidence scale (ABC-16) [
23] This is a 16- item questionnaire in which each item can be scored from 0% (zero confidence) to 100% (total confidence). The total score is between 0% and 100%, with higher values associated with greater confidence in balance. The Spanish version of the ABC was validated with vestibular patients. It demonstrated excellent internal consistency and a possible three- dimensional structure.
Fear of falling during daily activities was assessed with the Spanish version of the Falls Efficacy Scale-International (FES-I) [
24]. The FES-I is a questionnaire containing 16 items that measure fear of falling during social and physical activities inside and outside of the home. A higher score on the FES-I is associated with a greater fear of falling. The Spanish version of the FES-I presents acceptable psychometric properties with high internal consistency and a unifactorial structure with two underlying dimensions related to physical activities of different demands.
The number of falls in the last 12 months was recorded by asking participants to answer the following question: “How many falls have you had in the last year?” Based on this variable, the subjects were classified as fallers or non-fallers.
The JAEN scale [
17] is composed of 20 items derived from classic balance evaluation tests. However, it scores on a scale from 0 to 4, where "0" indicates no problem and "4" indicates a complete problem that prevents the patient from performing the actions detailed in the items. The total score ranges from 0-80 points, with a higher score indicating a more serious balance disturbance. The tool has shown a good ability to discriminate subjects both at risk of suffering falls and those with the balance impairment associated with FMS. However, the analysis of the items showed a high internal consistency with an alpha value that could indicate item redundancy.
2.3. Items Reduction Procedure
The study focused on reducing the number of items in the original version to shorten the time required to complete it. This was done by eliminating redundant items detected in the original validation study, while maintaining the effectiveness of the tool. The extraction of items from all subscales of the original tool followed the following steps:
An analysis of differences in means was performed to explore the ability of each item to differentiate between subjects with and without FMS. The criterion of obtaining a p value <0.05 in the non-parametric Mann-Whitney U test was adopted.
In the second step, the same analysis was conducted to prove that the items could differentiate between fallers and non-fallers. To be pre- selected, an item had to fulfil both criteria.
In the analysis conducted for each subscale, items that contributed to maintaining the scale’s Cronbach’s alpha close to the optimal value of 0.90 were kept.
Finally, factor analysis was conducted to select items that loaded clearly on any of the resulting factors.
2.4. Statistical Analysis
The data were described by means and standard deviations for continuous variables and by frequencies and percentages for categorical variables. The exploration of differences in item scores between subjects and healthy controls and between fallers and non-fallers was carried out with the non- parametric Mann-Whitney U test.
For the analysis of internal consistency, Cronbach’s α coefficient was used, which evaluates the degree to which the items of an instrument correlate with each other[
25]. A Cronbach’s alpha coefficient of less than 0.70 indicates low internal consistency; a coefficient between 0.70 and 0.90 indicates good internal consistency; and a coefficient greater than 0.90 indicates redundancy[
26].
Construct validity was evaluated using a principal component analysis with Varimax rotation. To check whether the sample was suitable for factor analysis, the Kaiser-Meyer-Olkin (KMO) test was used.
Concurrent validity was analysed by comparing the JAEN Scale with the Spanish versions of the ABC, FES-I, SF-12 and DHI scales, as well as by examining the number of falls during the last 12 months. To analyse the total score obtained on the screening tool with the rest of the measures, the Pearson correlation coefficient was used. A correlation coefficient between 0.3 and 0.5 was considered moderate correlation, while values greater than 0.5 were considered strong correlation[
27].
To analyse the diagnostic validity of the JAEN Scale to discriminate between patients with FMS and controls, and between fallers and non- fallers, a receiver operating characteristic (ROC) curve analysis was performed[
28] The area under the ROC curve (AUC) was used to analyse the ability of the JAEN Scale to discriminate between subjects and controls. A test is considered capable of discriminating between two groups of subjects when the AUC value is > 0.50; an AUC value between 0.50 and 0.70 indicates that the test has “low precision”; when the value is between 0.70 and 0.90 the test has “good precision”; and when the value exceeds 0.90, the test has “high precision”[
29] Through the analysis of ROC curves, the optimal cut-off points of the JAEN Scale score were obtained, which determined the threshold from which the predictive values could be calculated. Sensitivity was defined as the proportion of subjects with FMS (or fallers) who tested positive on the JAEN Scale. Following this line of reasoning, specificity was calculated as the proportion of controls (or non-fallers) who had negative results on the JAEN Scale. Positive predictive value (PPV) was defined as the proportion of subjects with a positive JAEN score who had FMS (or had fallen). Negative predictive value (NPV) was defined as the proportion of patients with a low JAEN score who were healthy controls (or non-fallers).
Data management and analysis were performed using the Statistical Package for Social Sciences (SPSS) version 27 (SPSS Inc., Chicago, IL, USA) and MedCalc® Statistical Software version 22.023 (MedCalc Software Ltd, Ostend, Belgium; https://
www.medcalc.org; 2024). A confidence level of 95% was used (p < 0.05). The data associated with the paper are not publicly available but are available from the corresponding author on reasonable request.
3. Results
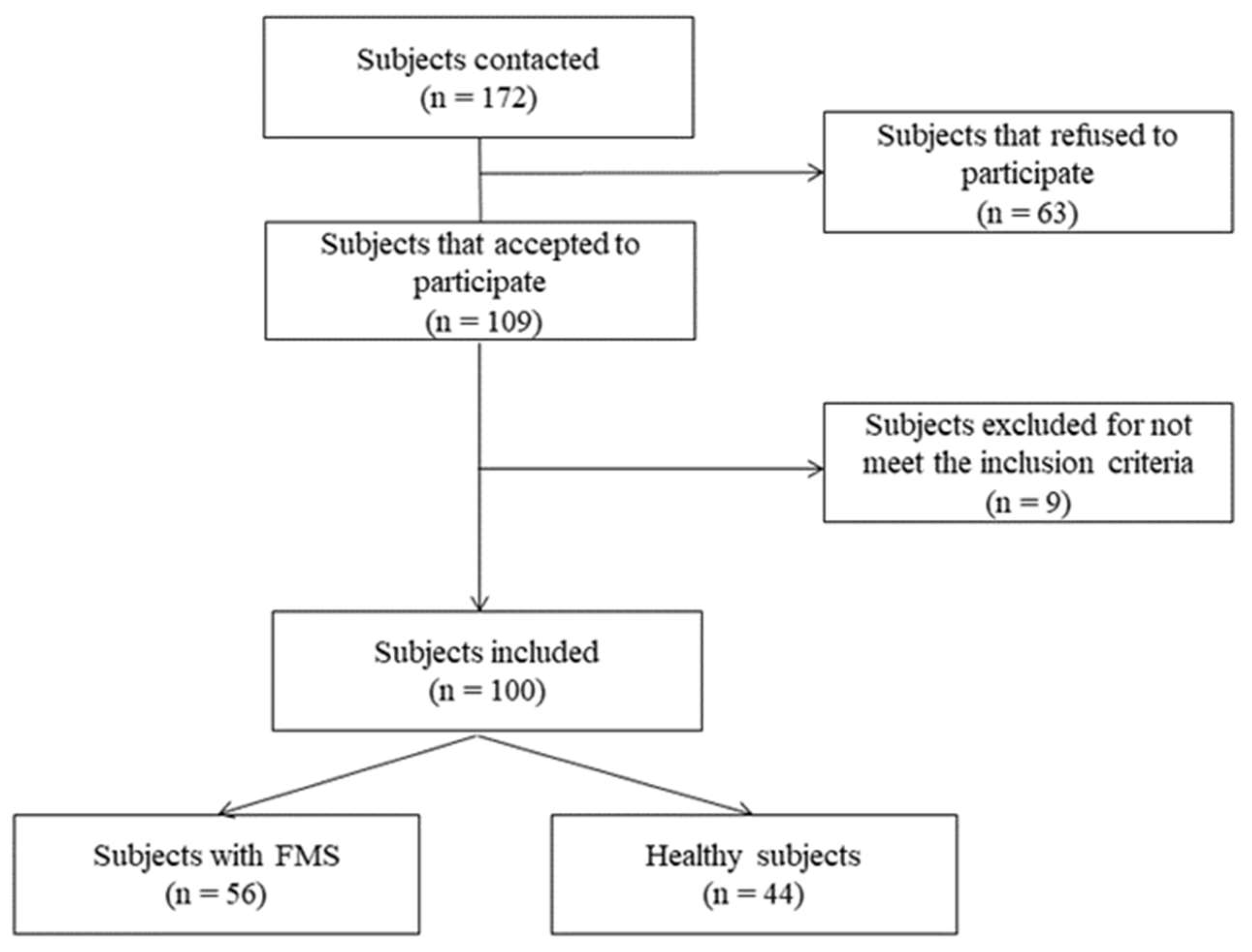
A total of 100 women were selected and agreed to participate in the study. Of these, 56 met the criteria for FMS and 44 were healthy controls (
Figure 1). The morphological characteristics and balance impairment levels are shown in
Table 1. In general, there were no significant differences between the groups in the morphological variables, although weight difference and the average number of falls in in the last year were on the limit of statistical significance in favour of women with FMS. Regarding quality of life, disability due to dizziness and all of the secondary variables, the sample of women with FMS had a worse health status with very significant differences.
After applying the item selection criteria, a total of 10 were pre-selected (1, 7, 9, 10-14, 19-20). These items represent the subscales of the original tool and their scores were statistically different between subjects with FMS and controls, as well as between fallers and non-fallers.
The analysis of the items of the new scale provided an alpha value of 0.904, which represents a balance between having the best internal consistency and no redundant items.
Table 2 illustrates the analysis of the items; the new items (2 and 3) result in the scale having an alpha compatible with redundant items.
Regarding the principal component analysis, the Kaiser-Meyer-Olkin (KMO) measure was 0.849, and the Bartlett sphericity test was equal to 836.769 (p<0.001). Therefore, the sample can be considered optimal for principal component analysis. This analysis showed a dimensional structure that explained 72% of the variance from two factors (
Table 3).
Table 4 shows the items included in each of the two factors identified: 1) First Factor = Instability when Support is Reduced with Eyes Closed (SREC): balance related to more demanding sensory conditions (Items 1,2 and 3); 2) Second Factor = Instability when Standing and Walking with Head Movements (SWHM): static and dynamic balance related to head movements (Items 4-10).
The concurrent validity analysis of the 10-item JAEN showed high correlation of all variables measuring balance (DHI, ABC and FES) and other impact measures of quality of life (FIQ and Physical Component Summary of SF-12), except the Mental Component Summary of the SF-12, where the correlation was moderate. Additionally, it can be observed that the different correlations with JAEN-20 and JAEN-10 are practically identical (
Table 5).
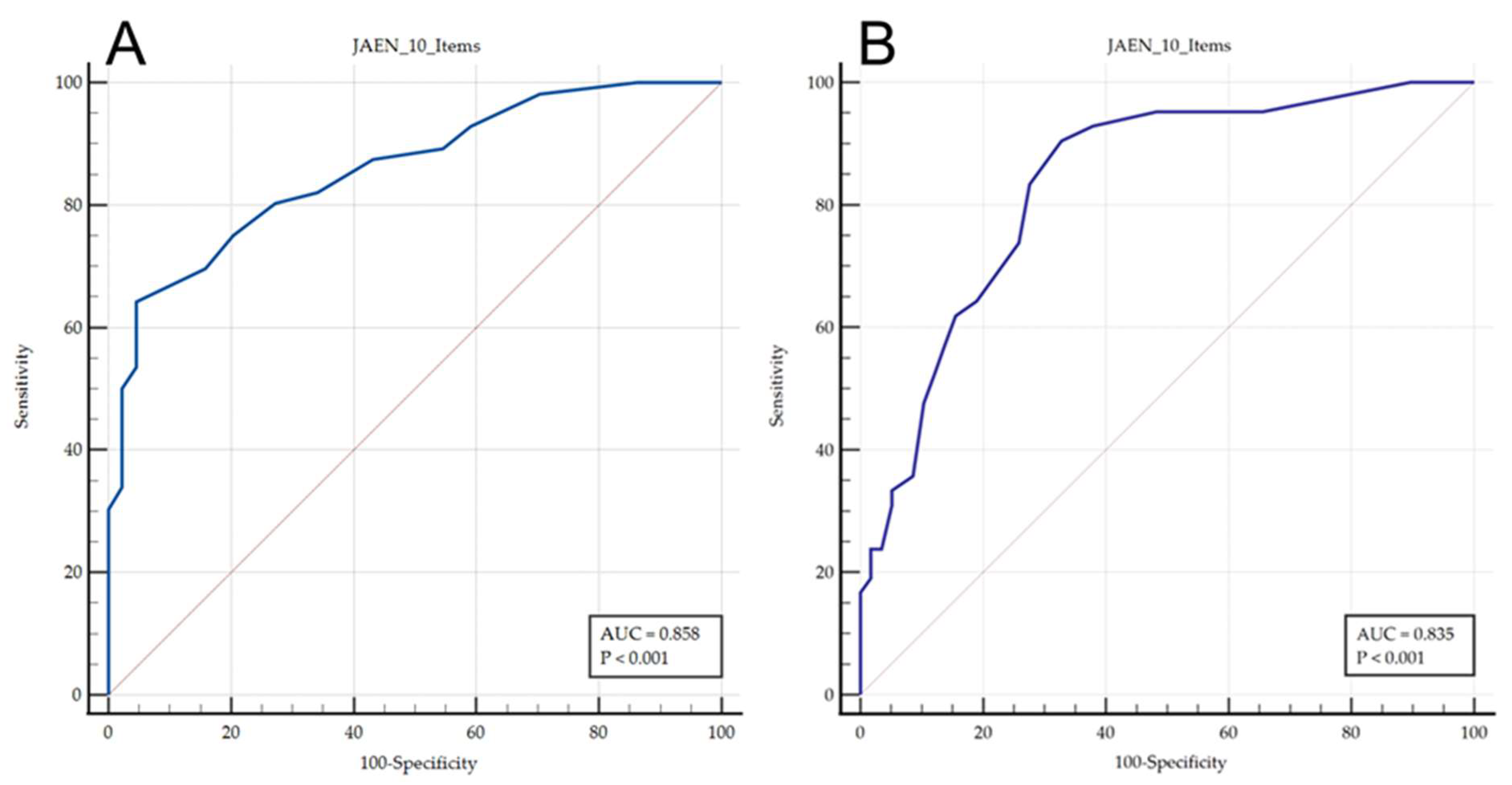
Regarding diagnostic validity (
Table 6), the ROC curve analysis showed that a cut-off point <14 showed a sensitivity of 64% and a specificity of 95% for the discrimination of subjects with or without FMS (in terms of balance disorders). Regarding falls, a cut-off point <11 provided a sensitivity of 90% to detect fallers with a sensitivity of 67%. The area under the ROC curve (
Figure 2) for the discrimination of patients with FMS was 0.858 (0.774 to 0.920, p<0.001), while for fallers it was 0.835 (0.748 to 0.902, p<0.001).
4. Discussion
This study aimed to develop and validate a short form of the instrument ‘Joint Assessment of Equilibrium and Neuromotor Status’ (JAEN Scale), to improve the evaluation of postural balance and the prediction of the risk of falls in subjects with FMS[
17]. The original instrument (JAEN-20 items) already showed good internal consistency, perhaps even excessive for the criteria of some authors[
26] It also shows greater sensitivity to change than other commonly used tools. As a result of this study, a 10-item version (JAEN-10 items) has been obtained that can be completed in about 5 minutes.
In comparison to the original version, the JAEN-20 items presented an internal consistency alpha=0.928,17 which may indicate item redundancy. The JAEN-10 items (Supplementary Table 1) has an alpha value=0.904, which implies an optimal value with no redundancy[
26]. Regarding construct validity, while the extended version JAEN-20 items provided 4 subscales, the short version JAEN-10 items only has a two-factor structure: Factor 1: Instability when Support is Reduced with Eyes Closed (SREC), and Factor 2: Instability when Standing and Walking with Head Movements (SWHM). While this may appear to be a limitation, it actually makes the short version more suitable for use in clinical settings as it is easier to interpret. Additionally, although the AUC for the diagnostic prediction of FMS is reduced from 0.928 on the JAEN-20 to 0.858, the tool improves the precision of detecting falling subjects from 0.795 on the JAEN-20 to 0.835 of the JAEN-10 items version. Finally, the concurrent validity of both the standard and short instruments is almost identical to other scales.
One of the main reasons why the authors designed the extended version of the JAEN Scale (JAEN-20) was precisely due to how simple it was to complete for subjects prone to fatigue. This made the JAEN-20 items a more convenient tool than the Berg Balance Scale (BBS), the BEStest or the expensive computerized dynamic posturography. While the BBS has sometimes been used to measure balance in FMS[
30,
31,
32], the BESTest was only used once[
9]. It should be noted that the concurrent validity of the FIQ in the two versions of the JAEN Scale is similar to that of the BBS and the BESTest, showing moderate correlation[
9].
However, although the use of JAEN-10 items may be suitable in clinical settings for assessing and monitoring balance disorder progression, the standard version JAEN-20 items may be more useful in research settings, as the subscales reveal potential balance impairment specifically due to the alteration of visuo-vestibular afferents. This was also proven with Computerized Dynamic Posturography[
11], but at a higher cost given its latest technology. The JAEN-20 items would also be appropriate to measure changes in patient health status as it has shown a certain degree of responsiveness[
16]. However, this property is yet to be evaluated in the short version JAEN-10 items.
This study has numerous limitations. Firstly, the sample only comprised women. However, this is representative of the much higher prevalence of FMS in women than in men. Furthermore, all patients were from the same geographical area, which makes extrapolation of our results to other settings difficult. Furthermore, although several psychometric properties have been measured for this new instrument, others are yet to be evaluated, including interobserver reliability and responsiveness. These factors should be evaluated in further research. It would also be desirable to extend its validation to different populations, beyond solely subjects with FMS.
5. Conclusions
The JAEN-10-item scale is a valid instrument to measure postural balance and risk of falls in women with FMS. This tool can be implemented quickly and interpreted relatively easily given the thresholds that may indicate the possible presence of FMS (14 points) and/or risk of falls (11 points). Further research should be conducted to verify interobserver reliability, sensitivity to change and the ability to predict falls prospectively. It should also aim to validate the use of the instrument in a different population to subjects with FMS.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Table S1: The short form of the Joint Assessment of Equilibrium and Neuromotor Status Scale (JAEN-10).
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, R.L-V, M.C.O.-P., A.B.P.-R., N.Z.-A., D.N.-F and D.R.-A.; methodology, R.L-V, M.C.O.-P., A.B.P.-R. and N.Z.-A.; validation R.L-V, M.C.O.-P., A.B.P.-R. and N.Z.-A., formal analysis, R.L-V, M.C.O.-P., A.B.P.-R. and N.Z.-A; investigation, R.L-V, M.C.O.-P., A.B.P.-R., N.Z.-A., D.N.-F and D.R.-A.; resources, R.L-V, M.C.O.-P., A.B.P.-R., D.N.-F and D.R.-A.; data curation, R.L-V, M.C.O.-P., A.B.P.-R., N.Z.-A., and D.R.-A; writing—original draft preparation, R.L-V, M.C.O.-P., A.B.P.-R., N.Z.-A.; writing—review and editing, R.L.-V., A.B.P.-R., D.N.-F and D.R.-A.; visualization, R.L-V, M.C.O.-P., A.B.P.-R., N.Z.-A., D.N.-F and D.R.-A..; supervision, R.L-V, M.C.O.-P., and N.Z.-A, project administration, R.L.-V.; funding acquisition, R.L.-V. and M.C.O.-P. All authors have read and agreed to the published version of the manuscript.”.
Funding
Please add: This study was supported by the Project FEDER reference 1263880.
Institutional Review Board Statement
The study was approved by the Ethics Committee of the University of Jaén (protocol number JUL.23/6 PRY).) in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Statement: Data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
The authors would like to thank AFIXA (Asociación de Fibromialgia de Jaén) association and especially all the participants of this study for their insightful contribution.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Xu, T.; Clemson, L.; O’Loughlin, K.; Lannin, N.A.; Dean, C.; Koh, G. Risk Factors for Falls in Community Stroke Survivors: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 563–573.e5. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Delbaere, K.; Zijlstra, G.A.R.; Carpenter, H.; Iliffe, S.; Masud, T.; Skelton, D.; Morris, R.; Kendrick, D. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing 2016, 45, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Peinado-Rubia, A.; Osuna-Pérez, M.C.; Rodríguez-Almagro, D.; Zagalaz-Anula, N.; López-Ruiz, M.C.; Lomas-Vega, R. Impaired Balance in Patients with Fibromyalgia Syndrome: Predictors of the Impact of This Disorder and Balance Confidence. Int. J. Environ. Res. Public Health 2020, 17. [Google Scholar] [CrossRef] [PubMed]
- Simpkins, C.; Soysa, I.B.; Christey, G. Falls at home: hospital admissions in a health region of Aotearoa New Zealand. N. Z. Med. J. 2024, 137, 47–56. [Google Scholar] [CrossRef] [PubMed]
-
WHO TEAM WHO global report on falls prevention in older age; WHO Library Cataloguing-in-Publication Data: France, 2007; ISBN 9789241563536.
- Xiong, W.; Wang, D.; Ren, W.; Liu, X.; Wen, R.; Luo, Y. The global prevalence of and risk factors for fear of falling among older adults: a systematic review and meta-analysis. BMC Geriatr. 2024, 24. [Google Scholar] [CrossRef]
- Bennett, R.M. Emerging concepts in the neurobiology of chronic pain: evidence of abnormal sensory processing in fibromyalgia. Mayo Clin. Proc. 1999, 74, 385–398. [Google Scholar] [CrossRef]
- Sarihan, K.; Uzkeser, H.; Erdal, A. Evaluation of balance, fall risk, and related factors in patients with fibromyalgia syndrome. Turkish J. Phys. Med. Rehabil. 2021, 67, 409–415. [Google Scholar] [CrossRef]
- Jones, K.D.; Horak, F.B.; Winters-Stone, K.; Irvine, J.M.; Bennett, R.M. Fibromyalgia is associated with impaired balance and falls. J. Clin. Rheumatol. Pract. reports Rheum. Musculoskelet. Dis. 2009, 15, 16–21. [Google Scholar] [CrossRef]
- Meireles, S.A.; Antero, D.C.; Kulczycki, M.M.; Skare, T.L. Prevalence of falls in fibromyalgia patients. Acta Ortop. Bras. 2014, 22, 163–166. [Google Scholar] [CrossRef]
- Núñez-Fuentes, D.; Obrero-Gaitán, E.; Zagalaz-Anula, N.; Ibáñez-Vera, A.J.; Achalandabaso-Ochoa, A.; López-Ruiz, M.D.C.; Rodríguez-Almagro, D.; Lomas-Vega, R. Alteration of Postural Balance in Patients with Fibromyalgia Syndrome-A Systematic Review and Meta-Analysis. Diagnostics (Basel, Switzerland) 2021, 11. [Google Scholar] [CrossRef]
- Mucci, V.; Demori, I.; Rapallo, F.; Molinari, E.; Losacco, S.; Marinelli, L.; Browne, C.J.; Burlando, B. Vestibular Disability/Handicap in Fibromyalgia: A Questionnaire Study. J. Clin. Med. 2022, 11. [Google Scholar] [CrossRef] [PubMed]
- Lomas-Vega, R.; Ogáyar-Anguita, C.J.; Segura-Sánchez, R.J.; Rueda-Ruiz, A.J.; Osuna-Pérez, M.C.; Peinado-Rubia, A.B. Misperception of Visual Verticality Measured with a Virtual Reality Device in Patients with Fibromyalgia Syndrome: A Cross-Sectional Study. Appl. Sci. 2023, Vol. 13, Page 10579 2023, 13, 10579. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Raizah, A.; Al-Otaibi, M.L.; Gular, K.; Ahmad, I.; Sirajudeen, M.S. Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life (Basel, Switzerland) 2022, 12. [Google Scholar] [CrossRef] [PubMed]
- Del-Moral-garcía, M.; Obrero-Gaitán, E.; Rodríguez-Almagro, D.; Rodríguez-Huguet, M.; Osuna-Pérez, M.C.; Lomas-Vega, R. Effectiveness of Active Therapy-Based Training to Improve the Balance in Patients with Fibromyalgia: A Systematic Review with Meta-Analysis. J. Clin. Med. 2020, 9, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Peinado-Rubia, A.B.; Osuna-Pérez, M.C.; Cortés-Pérez, I.; Rojas-Navarrete, A.; Ibancos-Losada, M. del R.; Lomas-Vega, R. Effectiveness of Vestibular Rehabilitation in Improving Health Status and Balance in Patients with Fibromyalgia Syndrome: A Single-Blind Randomized Controlled Trial. Biomedicines 2023, 11. [Google Scholar] [CrossRef]
- Lomas-Vega, R.; Rodríguez-Almagro, D.; Peinado-Rubia, A.B.; Zagalaz-Anula, N.; Molina, F.; Obrero-Gaitán, E.; Ibáñez-Vera, A.J.; Osuna-Pérez, M.C. Joint Assessment of Equilibrium and Neuromotor Function: A Validation Study in Patients with Fibromyalgia. Diagnostics (Basel, Switzerland) 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Vega, E.; Martínez-Moya, M.; Barni, L.; Guiducci, S.; Nacci, F.; Gonzalez-Sanchez, M. Questionnaires for the subjective evaluation of patients with fibromyalgia: a systematic review. Eur. J. Phys. Rehabil. Med. 2023, 59, 353–363. [Google Scholar] [CrossRef]
- Hobart JC, Cano SJ, Warner T T, T. A. What sample sizes for reliability and validity studies in neurology? J. Neurol. 2012, 259, 2681–2694. [Google Scholar] [CrossRef] [PubMed]
- Salgueiro, M.; García-Leiva, J.M.; Ballesteros, J.; Hidalgo, J.; Molina, R.; Calandre, E.P. Validation of a Spanish version of the Revised Fibromyalgia Impact Questionnaire (FIQR). Health Qual. Life Outcomes 2013, 11. [Google Scholar] [CrossRef]
- Vilagut, G.; Valderas, J.M.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. [Interpretation of SF-36 and SF-12 questionnaires in Spain: physical and mental components]. Med. Clin. (Barc). 2008, 130, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Pérez N, Garmendia I, Martín E, G. -T.R. Cultural adaptation of 2 questionnaires for health measurement in patients with vertigo. Acta Otorrinolaringol. Esp. 2000, 51, 572–80. [Google Scholar]
- Montilla-Ibáñez, A.; Martínez-Amat, A.; Lomas-Vega, R.; Cruz-Díaz, D.; Torre-Cruz, M.J.D. la; Casuso-Pérez, R.; Hita-Contreras, F. The Activities-specific Balance Confidence scale: reliability and validity in Spanish patients with vestibular disorders. Disabil. Rehabil. 2017, 39, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Lomas-Vega, R.; Hita-Contreras, F.; Mendoza, N.; Martínez-Amat, A. Cross-cultural adaptation and validation of the Falls Efficacy Scale International in Spanish postmenopausal women. Menopause 2012, 19, 904–908. [Google Scholar] [CrossRef] [PubMed]
- Cortina, J.M. What Is Coefficient Alpha? An Examination of Theory and Applications. J. Appl. Psychol. 1993, 78, 98–104. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53. [Google Scholar] [CrossRef]
-
Cohen J Statistical Power Analysis for the Behavioral Sciences; Academic Press: New York, New York, 1977.
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef]
- Kasapoğlu Aksoy, M.; Altan, L.; Ökmen Metin, B. The relationship between balance and vitamin 25(OH)D in fibromyalgia patients. Mod. Rheumatol. 2017, 27, 868–874. [Google Scholar] [CrossRef]
- Ulus, Y.; Akyol, Y.; Tander, B.; Durmuş, D.; Bilgici, A.; Kuru, Ö. Is There a Balance Problem in Hypermobile Patients with Fibromyalgia? Arch. Rheumatol. 2013, 28, 010–015. [Google Scholar] [CrossRef]
- Ulus, Y.; Akyol, Y.; Tander, B.; Bilgici, A.; Kuru, O. Knee Proprioception and Balance in Turkish Women With and Without Fibromyalgia Syndrome. Turk J Phys Med Rehab 2013, 59, 128–132. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).