Submitted:
11 September 2024
Posted:
12 September 2024
You are already at the latest version
Abstract
Keywords:
Introduction
Methods
Results
Discussion
Author Credits
References
- Janus J, Moerschel SK. Evaluation of anemia in children. American Family Physician [Internet]. 2010 Jun 15;81(12):1462–71. Available from: https://pubmed.ncbi.nlm.nih.gov/20540485/.
- The Lancet: New study reveals global anemia cases remain persistently high among women and children. Anemia rates decline for men. | Institute for Health Metrics and Evaluation [Internet]. Institute for Health Metrics and Evaluation. 2023 [cited 2024 Aug 13]. Available from: https://www.healthdata.org/news-events/newsroom/news-releases/lancet-new-study-reveals-global-anemia-cases-remain-persistently#:~:text=Topics&text=One%2Dfourth%20of%20the%20global.
- World Health Organization. Anaemia [Internet]. www.who.int. 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/anaemia.
- Nissenson, Allen R., et al. “Economic Burden of Anemia in an Insured Population.” Journal of Managed Care Pharmacy, vol. 11, no. 7, Sept. 2005, pp. 565–74. [CrossRef]
- Yang F, Liu X, Zha P. Trends in Socioeconomic Inequalities and Prevalence of Anemia Among Children and Nonpregnant Women in Low- and Middle-Income Countries. JAMA Network Open. 2018 Sep 28;1(5):e182899.
- Khan JR, Awan N, Misu F. Determinants of anemia among 6–59 months aged children in Bangladesh: evidence from nationally representative data. BMC Pediatrics. 2016 Jan 11;16(1):6-10.
- Martinez-Torres V, Torres N, Davis JA, Corrales-Medina FF. Anemia and Associated Risk Factors in Pediatric Patients. Pediatric Health Med Ther. 2023;14:267-280. Published 2023 Sep 4. [CrossRef]
- Amegbor, PM. Amegbor PM. Early-life environmental exposures and anaemia among children under age five in Sub-Saharan Africa: An insight from the Demographic & Health Surveys. Science of The Total Environment. 2022 Aug 1;832:154957.
- Zhu Y, He C, Gasparrini A, Vicedo-Cabrera AM, Liu C, Jovine Bachwenkizi, et al. Global warming may significantly increase childhood anemia burden in sub-Saharan Africa. One Earth. 2023 Oct 1;6(10):5-7.
- Moyo E, Nhari LG, Moyo P, Murewanhema G, Dzinamarira T. Health effects of climate change in Africa: A call for an improved implementation of prevention measures. Eco-Environment & Health. 2023 May 8;2(2):75.
- Lakhoo DP, Blake HA, Chersich MF, Nakstad B, Kovats S. The Effect of High and Low Ambient Temperature on Infant Health: A Systematic Review. International Journal of Environmental Research and Public Health. 2022 Jul 26;19(15):9109.
- Brimicombe C, Wieser K, Monthaler T, Jackson D, Jeroen De Bont, Chersich MF, et al. Effects of ambient heat exposure on risk of all-cause mortality in children younger than 5 years in Africa: a pooled time-series analysis. The Lancet Planetary Health. 2024 Aug 1;
- Short EE, Caminade C, Thomas BN. Climate Change Contribution to the Emergence or Re-Emergence of Parasitic Diseases. Infect Dis (Auckl). 2017;10:1178633617732296. Published 2017 Sep 25. [CrossRef]
- ter Kuile FO, Terlouw DJ, Kariuki SK, Phillips-Howard PA, Mirel LB, Hawley WA, Friedman JF, Shi YP, Kolczak MS, Lal AA, et al. Impact of permethrin-treated bed nets on malaria, anemia, and growth in infants in an area of intense perennial malaria transmission in western Kenya. Am J Trop Med Hyg. 2003;68:68–77.
- Iannotti LL, Tielsch JM, Black MM, Black RE. Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr. 2006;84:1261–1276. [CrossRef]
- Awuah RB, Colecraft EK, Wilson ML, et al. Perceptions and beliefs about anaemia: A qualitative study in three agroecological regions of Ghana. Matern Child Nutr. 2021;17(4):e13181. [CrossRef]
- Hung SC, Kuo KL, Peng CH, Wu CH, Wang YC, Tarng DC. Association of fluid retention with anemia and clinical outcomes among patients with chronic kidney disease. J Am Heart Assoc. 2015;4(1):e001480. Published 2015 Jan 5. [CrossRef]
- Azmeraw M, Kassaw A, Habtegiorgis SD, et al. Prevalence of anemia and its associated factors among children aged 6-23 months, in Ethiopia: a systematic review and meta analysis. BMC Public Health. 2023;23(1):2398. Published 2023 Dec 2. [CrossRef]
- Humphrey JH, Jones AD, Manges A, Mangwadu G, Maluccio JA, Mbuya MNN, Moulton LH, Ntozini R, Prendergast AJ, et al. Sanitation Hygiene Infant Nutrition Efficacy SHINE Trial Team. The Sanitation Hygiene Infant Nutrition Efficacy (SHINE) Trial: Rationale, Design, and Methods. Clin Infect Dis. 2015;61:S685–S702. [CrossRef]
- Wilson SE, Rogers LM, Garcia-Casal MN, Barreix M, Bosman A, Cunningham J, Goga A, Montresor A, Tuncalp O. Comprehensive framework for integrated action on the prevention, diagnosis, and management of anemia: An introduction. Ann N Y Acad Sci. 2023;1524:5–9. [CrossRef]
- Dimitrova A, Dimitrova A, Mengel M, et al. Temperature-related neonatal deaths attributable to climate change in 29 low- and middle-income countries. Nat Commun. 2024;15:5504. [CrossRef]
- Scovronick N, Sera F, Acquaotta F, et al. The association between ambient temperature and mortality in South Africa: A time-series analysis. Environ Res. 2018;161:229-235. [CrossRef]
- Tobías, Aurelio; Armstrong, Ben; Gasparrini, Antonio. Brief Report: Investigating Uncertainty in the Minimum Mortality Temperature. Epidemiology 28(1):p 72-76, January 2017. |. [CrossRef]
- Brehm R, South A, George EC. Use of point-of-care haemoglobin tests to diagnose childhood anaemia in low- and middle-income countries: A systematic review. Tropical Medicine & International Health. 2023 Dec 3;
- Firdian Makrufardi, Triasih R, Nurnaningsih Nurnaningsih, Kian Fan Chung, Lin SC, Chuang HC. Extreme temperatures increase the risk of pediatric pneumonia: a systematic review and meta-analysis. Frontiers in pediatrics. 2024 Feb 2;12.
- Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian S. Anaemia in low-income and middle-income countries. The Lancet [Internet]. 2011 Dec;378(9809):2123–35. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)62304-5/fulltext.
- Kang N, Wang R, Lu H, Onyai F, Tang M, Tong M, et al. Burden of Child Anemia Attributable to Fine Particulate Matters Brought by Sand Dusts in Low- and Middle-Income Countries. Environmental Science & Technology. 2024 Jul 12;2024:12954.
- Shimanda PP, Amukugo HJ, Norström F. Socioeconomic factors associated with anemia among children aged 6-59 months in Namibia. Journal of Public Health in Africa. 2020 Apr 29;11(1):29-33.
- Nkulikiyinka R, Binagwaho A, Palmer K. The changing importance of key factors associated with anaemia in 6- to 59-month-old children in a sub-Saharan African setting where malaria is on the decline: analysis of the Rwanda Demographic and Health Survey 2010. Tropical Medicine & International Health. 2015 Oct 14;20(12):1722–32.
- Kothari MT, Coile A, Huestis A, Pullum T, Garrett D, Engmann C. Exploring associations between water, sanitation, and anemia through 47 nationally representative demographic and health surveys. Annals of the New York Academy of Sciences. 2019 Aug 1;1450(1):249–67.
- Ogwang BA, Chen H, Li X, Gao C. The Influence of Topography on East African October to December Climate: Sensitivity Experiments with RegCM4. Advances in Meteorology. 2014 Oct 21;2014:e143917.
- Choi HJ, Lee HJ, Jang HB, Park JY, Kang JH, Park KH, et al. Effects of maternal education on diet, anemia, and iron deficiency in Korean school-aged children. BMC Public Health. 2011 Nov 16;11(1):1-8.
| Region | Country | Number of Children with Anemia |
|---|---|---|
| East (n=613,660,310) | Burundi | 17,626,800 |
| Comoros | 1,187,090 | |
| Eritrea | 4,714,000 | |
| Ethiopia | 158,345,000 | |
| Kenya | 57,797,000 | |
| Madagascar | 36,580,000 | |
| Malawi | 32,383,000 | |
| Mauritius | 459,320 | |
| Mozambique | 56,049,000 | |
| Rwanda | 13,688,100 | |
| South Sudan | 18,374,200 | |
| Uganda | 74,517,000 | |
| United Republic of Tanzania | 96,414,000 | |
| Zambia | 27,740,000 | |
| Zimbabwe | 17,785,800 | |
| Central (n=323,793,130) | Angola | 55,729,000 |
| Cameroon | 43,674,000 | |
| Central African Republic | 10,984,700 | |
| Chad | 33,943,000 | |
| Congo | 8,928,000 | |
| Democratic Republic of the Congo | 167,170,000 | |
| Gabon | 3,003,400 | |
| Sao Tome and Principe | 361,030 | |
| South (n=50,795,450) | Botswana | 2,020,990 |
| Eswatini | 1,298,760 | |
| Lesotho | 2,545,000 | |
| Namibia | 2,724,700 | |
| South Africa | 42,206,000 | |
| West (n=787,156,600) | Benin | 22,949,200 |
| Burkina Faso | 47,534,000 | |
| Cote d’Ivoire | 50,802,000 | |
| Gambia | 4,291,700 | |
| Ghana | 49,904,000 | |
| Guinea | 27,065,000 | |
| Guinea-Bissau | 3,718,300 | |
| Liberia | 9,127,400 | |
| Mali | 46,473,000 | |
| Mauritania | 7,693,400 | |
| Niger | 53,040,000 | |
| Nigeria | 401,095,000 | |
| Senegal | 32,168,000 | |
| Sierra Leone | 15,842,100 | |
| Togo | 15,453,500 | |
| Total | 1,775,405,490 |
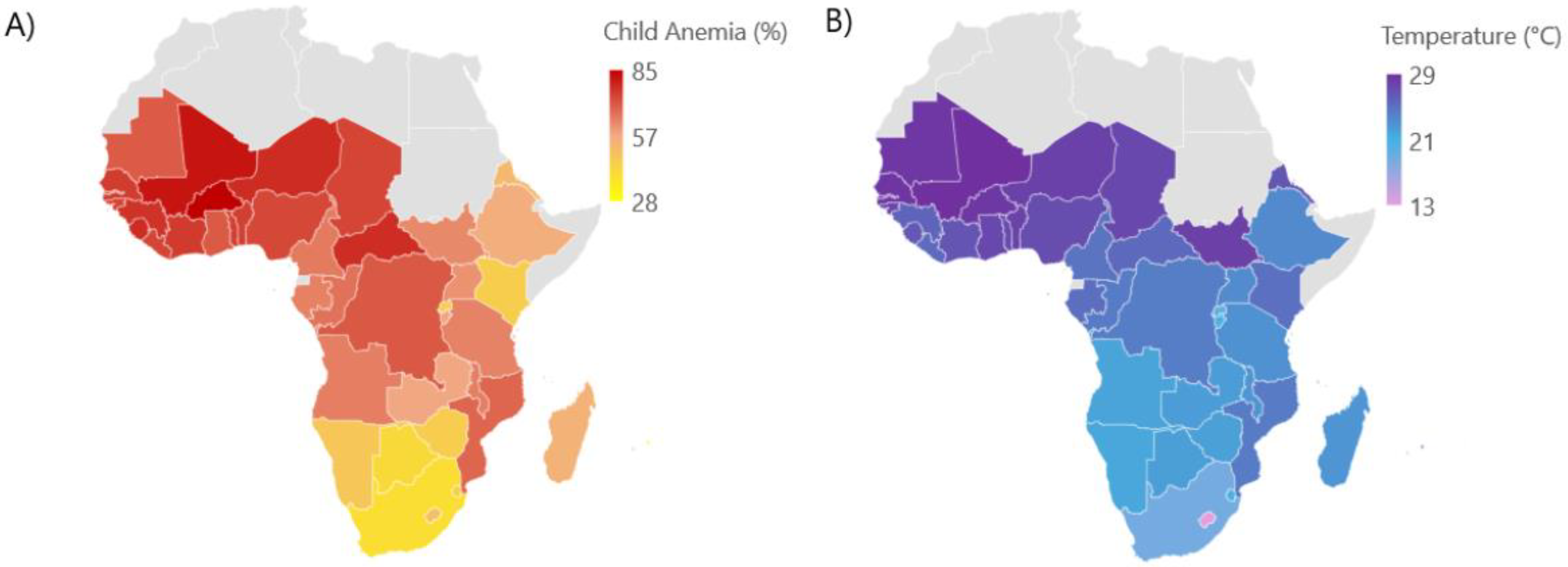
| Region | Number of Child with Anemia | Adjusted RR (P-value)* |
|---|---|---|
| West | 787,156,600 | 0.989 (P=0.0013) |
| East | 613,660,310 | 0.993 (P=0.001) |
| Central | 323,793,130 | 1.023 (P<0.0001) |
| South | 50,795,450 | 1.005 (P=0.006) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





