Submitted:
12 September 2024
Posted:
12 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Source of Data
2.2. Participants
2.3. Study Variables
2.3.1. Outcomes
2.3.2. Covariates
2.4. Statistical Methods
3. Results
3.1. Prevalence of Telehealth Use Due to the COVID-19 Pandemic by States
3.2. Univariate Logistic Regression Analyses
3.2.1. Telehealth usage due to COVID-19
3.2.2. Telehealth usage NOT due to COVID-19
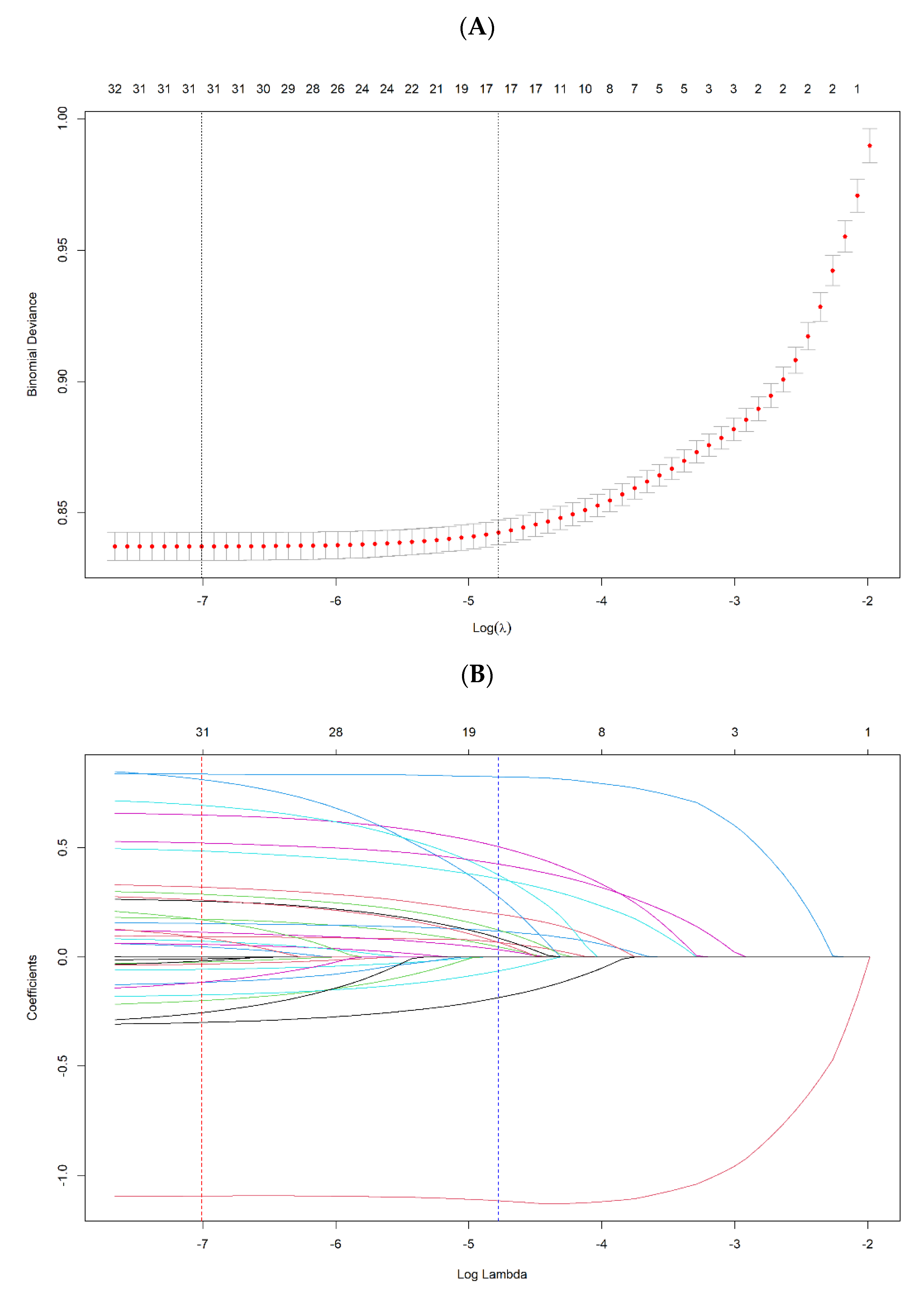
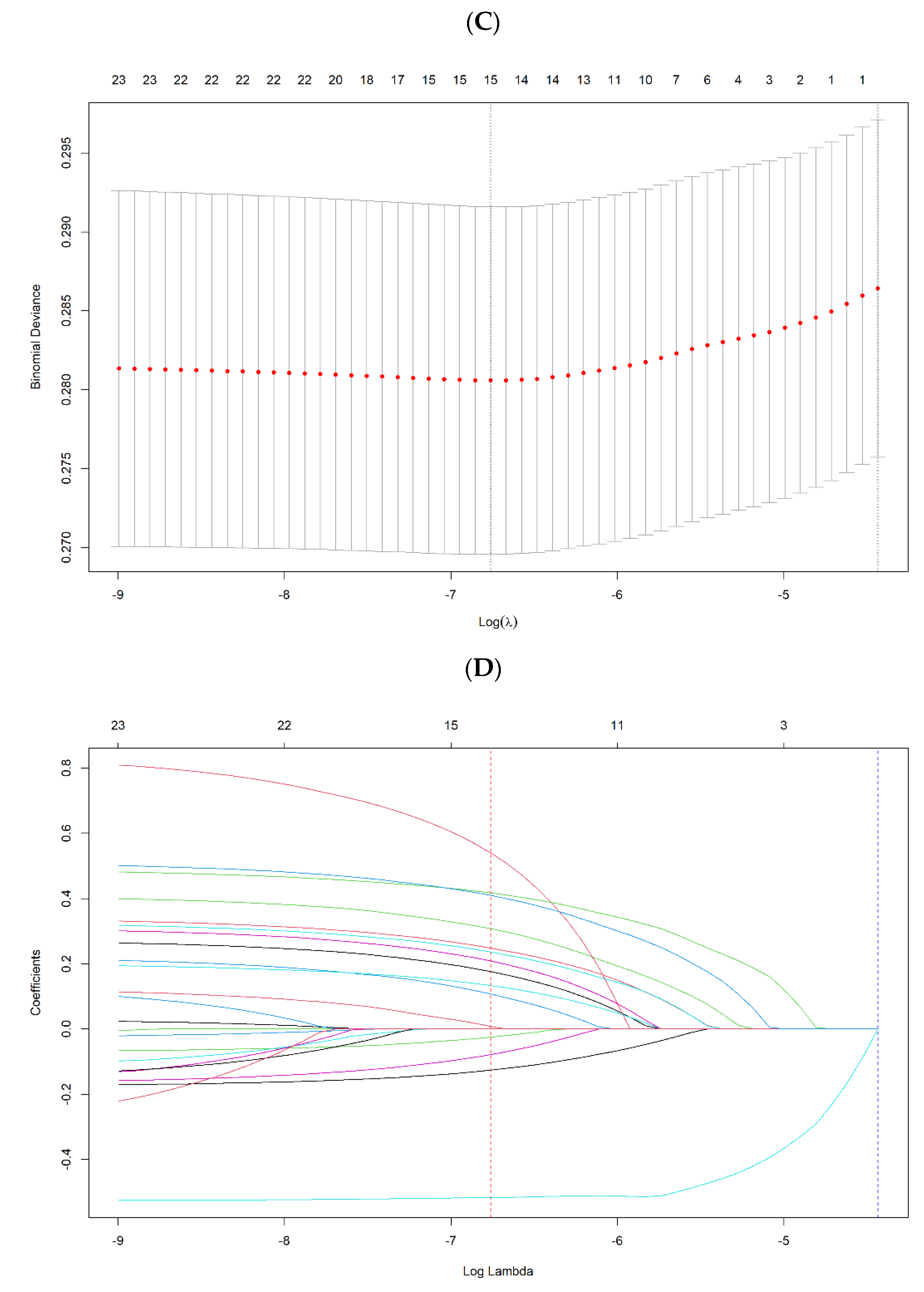
3.3. Multivariable Logistic Regression Modeling by LASSO Method
3.3.1. Telehealth usage due to COVID-19
3.3.2. Telehealth usage NOT due to COVID-19
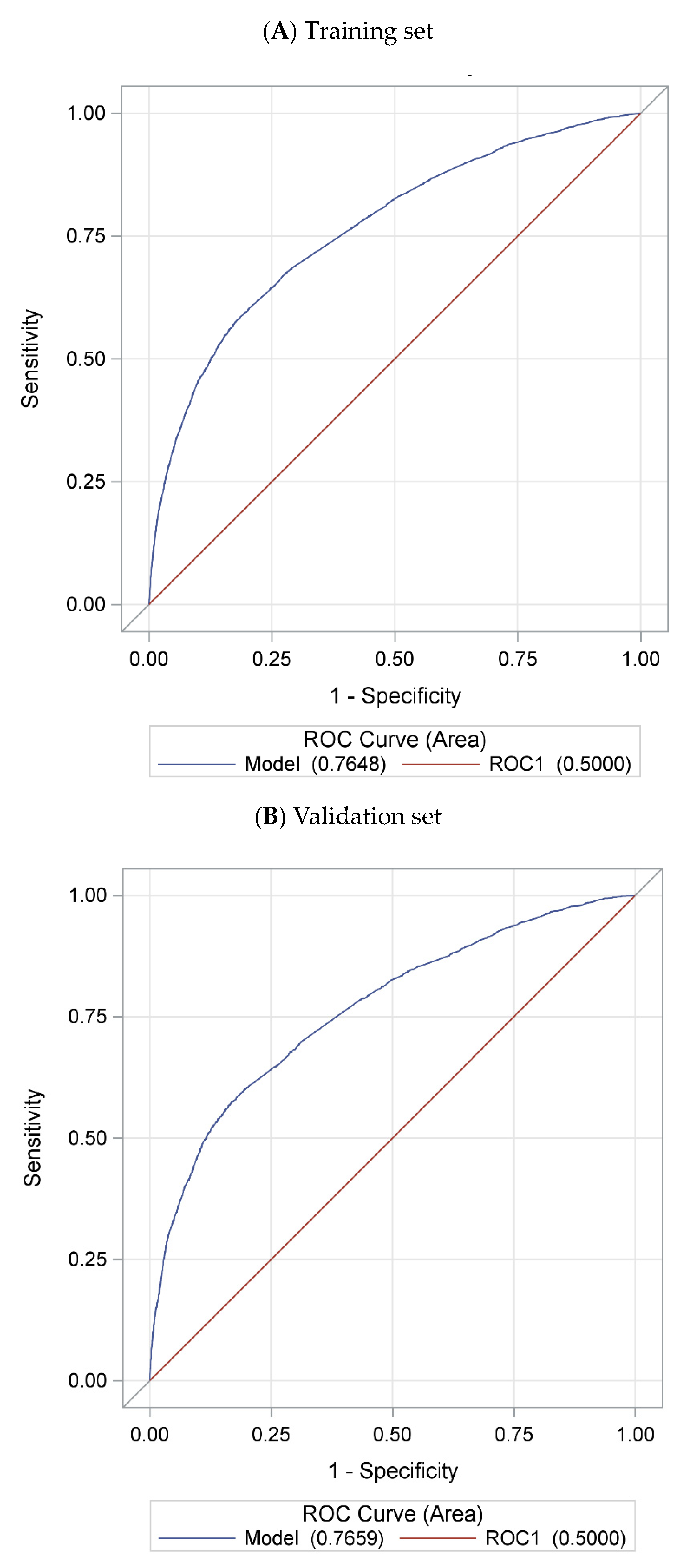
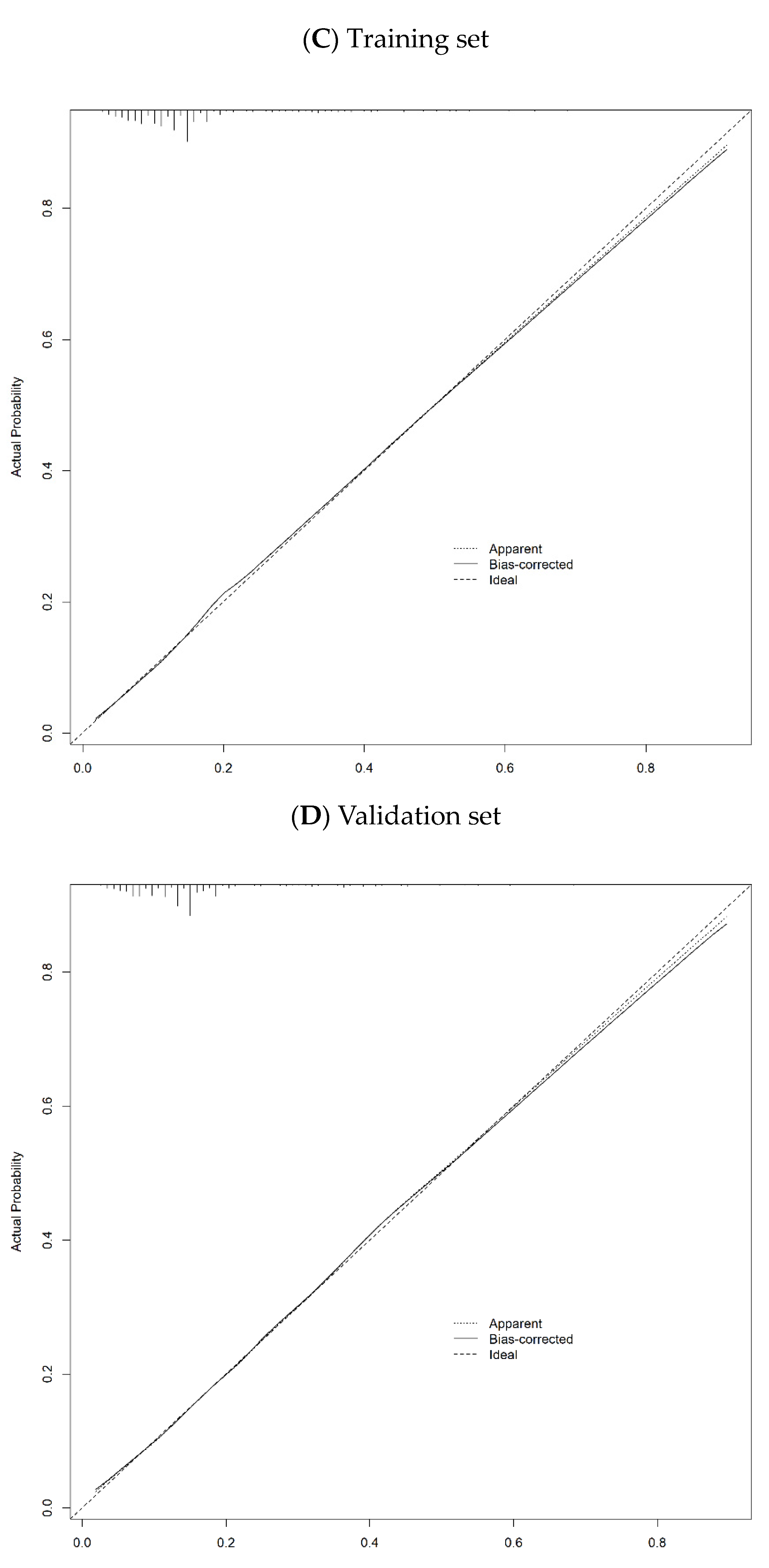
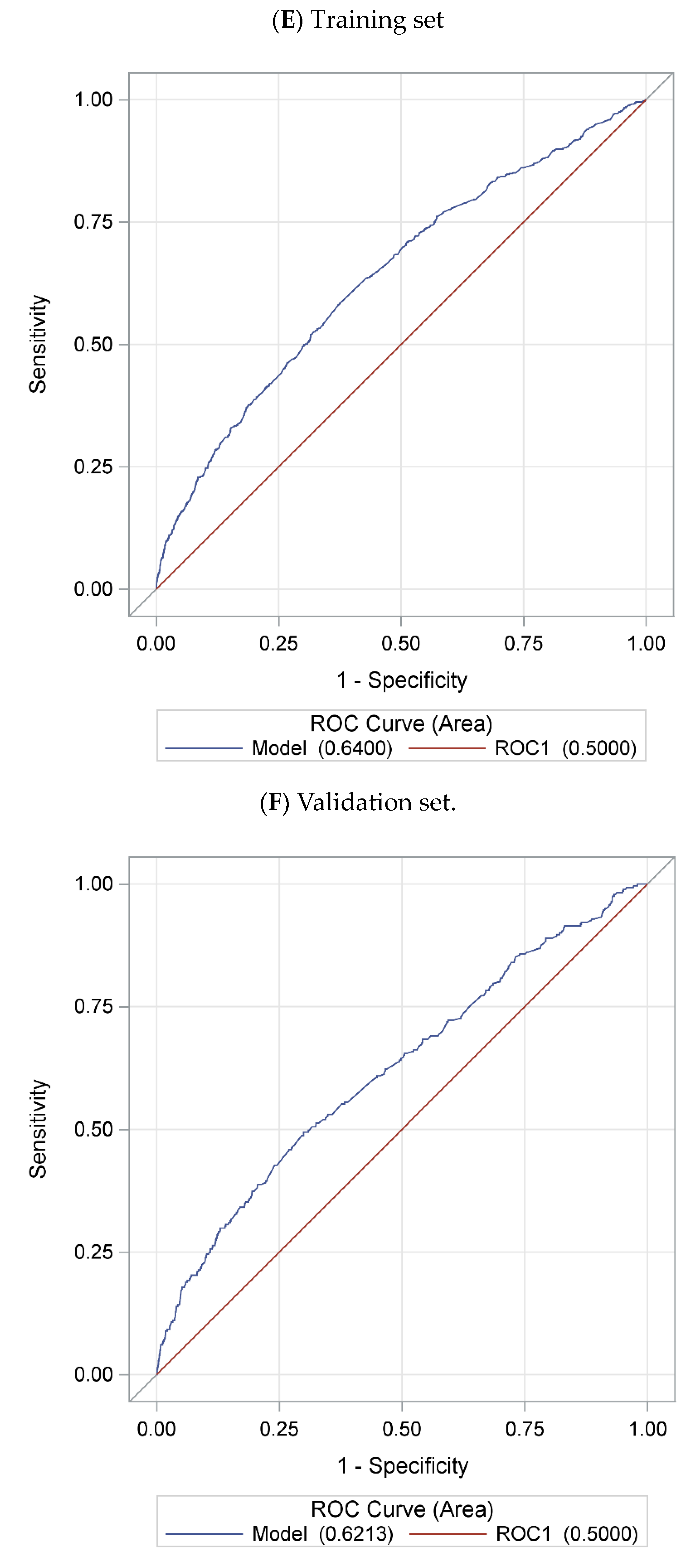
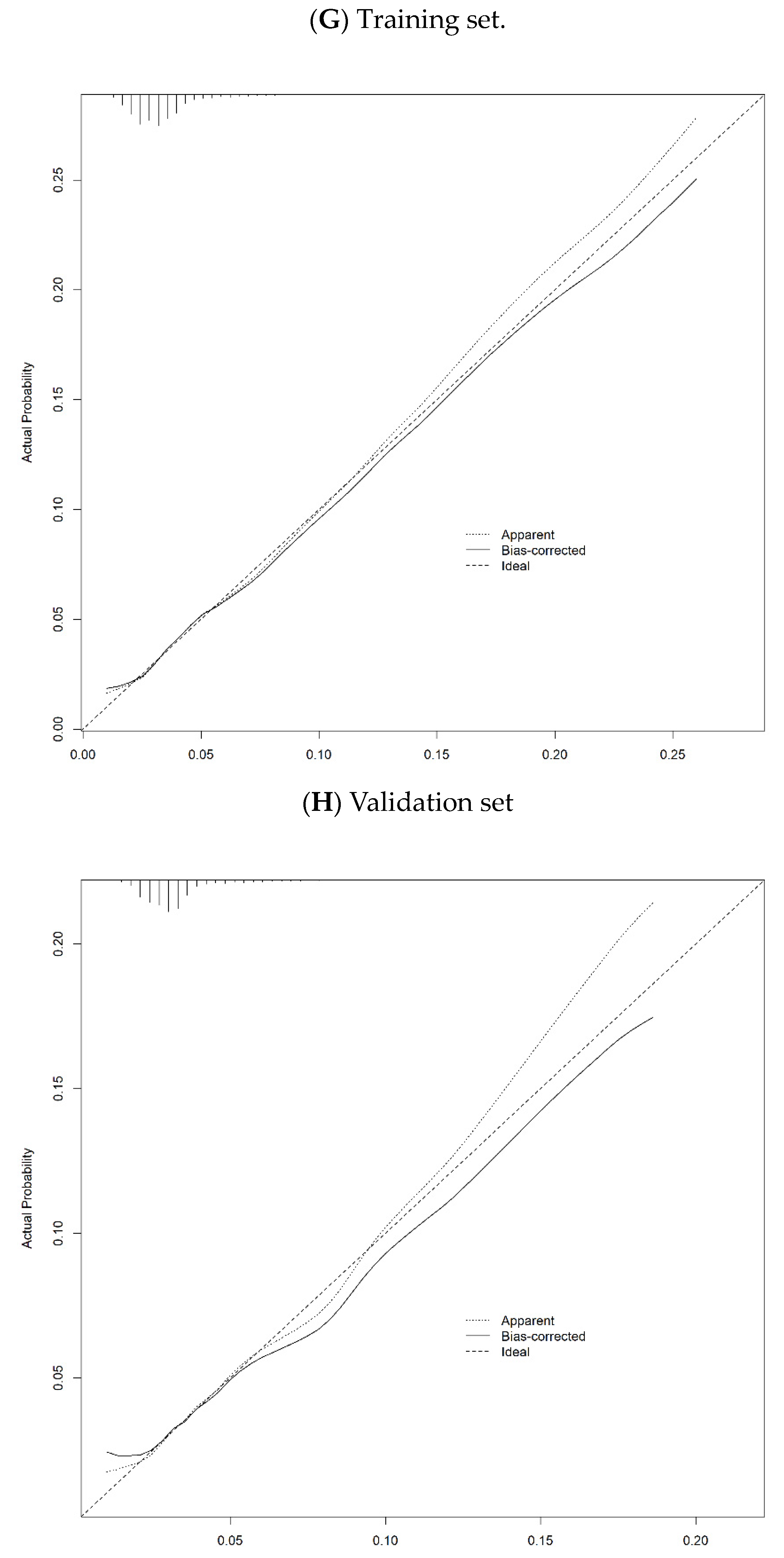
3.4. Prediction Performance of Selected Model by LASSO method
3.4.1. Telehealth usage due to COVID-19
3.4.2. Telehealth usage NOT due to COVID-19
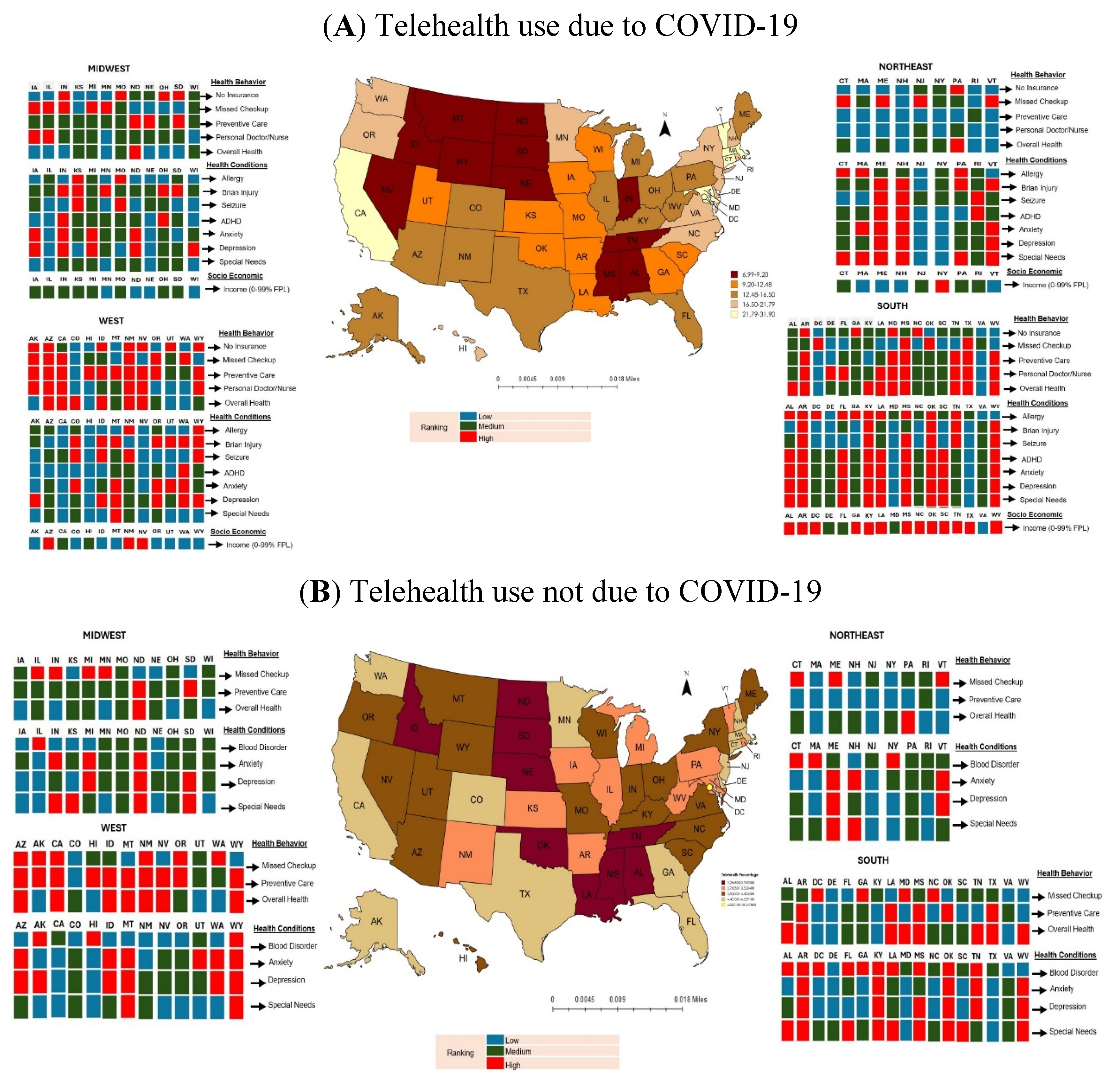
3.5. Prevalence Map and Predictors for Telehealth Use
4. Discussion
4.1. Study Limitations
4.2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.-C.; Wang, C.-B.; Bernardini, S. The COVID-19 pandemic. Critical reviews in clinical laboratory sciences 2020, 57, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.; Khasag, A.; Jia, W.; Jenkins, A.; Huang, C.-N.; Yabe, D.; Kim, D.-M.; Kadowaki, T.; Lee, M.-K. Diabetes and COVID-19: IDF perspective in the Western Pacific region. diabetes research and clinical practice 2020, 166, 108278. [Google Scholar] [CrossRef] [PubMed]
- Padhan, R.; Prabheesh, K. The economics of COVID-19 pandemic: A survey. Economic analysis and policy 2021, 70, 220–237. [Google Scholar] [CrossRef]
- Msemburi, W.; Karlinsky, A.; Knutson, V.; Aleshin-Guendel, S.; Chatterji, S.; Wakefield, J. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 2023, 613, 130–137. [Google Scholar] [CrossRef]
- Boxley, C.; Dixit, R.; Adams, K.; Anderson, R.; Ratwani, R.M.; Booker, E. The impact of COVID-19 on primary care accessibility and the role of telehealth for patients with chronic conditions. Health Policy and Technology 2023, 12, 100772. [Google Scholar] [CrossRef] [PubMed]
- Hangartner, N.; Di Gangi, S.; Elbl, C.; Senn, O.; Bisatz, F.; Fehr, T. Impact of the COVID-19 pandemic on emergency outpatient consultations and admissions of non-COVID-19 patients (ECCO)—A cross-sectional study. PLoS ONE 2022, 17, e0269724. [Google Scholar] [CrossRef]
- Sisó-Almirall, A.; Kostov, B.; Sánchez, E.; Benavent-Àreu, J.; González-de Paz, L. Impact of the COVID-19 pandemic on primary health care disease incidence rates: 2017 to 2020. The Annals of Family Medicine 2022, 20, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Haileamlak, A. The impact of COVID-19 on health and health systems. Ethiopian Journal of Health Sciences 2021, 31, 1073. [Google Scholar]
- Brown, C.L.; Montez, K.; Amati, J.B.; Simeonsson, K.; Townsend, J.D.; Orr, C.J.; Palakshappa, D. Impact of COVID-19 on pediatric primary care visits at four academic institutions in the Carolinas. International journal of environmental research and public health 2021, 18, 5734. [Google Scholar] [CrossRef]
- Xu, S.; Glenn, S.; Sy, L.; Qian, L.; Hong, V.; Ryan, D.S.; Jacobsen, S. Impact of the COVID-19 pandemic on health care utilization in a large integrated health care system: Retrospective cohort study. Journal of medical Internet research 2021, 23, e26558. [Google Scholar] [CrossRef]
- Cahan, E.M.; Maturi, J.; Bailey, P.; Fernandes, S.; Addala, A.; Kibrom, S.; Krissberg, J.R.; Smith, S.M.; Shah, S.; Wang, E. The impact of telehealth adoption during COVID-19 pandemic on patterns of pediatric subspecialty care utilization. Academic Pediatrics 2022, 22, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, Y.; Maguire, B.; Zemek, R.; Osmanlliu, E.; Kam, A.J.; Dixon, A.; Desai, N.; Sawyer, S.; Emsley, J.; Lynch, T. Effect of the COVID-19 pandemic on patient volumes, acuity, and outcomes in pediatric emergency departments: A nationwide study. Pediatric emergency care 2021, 37, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Chuang, M.Y. , Lee Y-S. Exploring Technology Domains for Diabetes Care and Management under Pandemic: A preliminary scoping review. Asia Pacific Journal of Health Management 2023, 18, 281–309. [Google Scholar]
- Doraiswamy, S.; Abraham, A.; Mamtani, R.; Cheema, S. Use of telehealth during the COVID-19 pandemic: Scoping review. Journal of medical Internet research 2020, 22, e24087. [Google Scholar] [CrossRef]
- Williams, S.; Hill, K.; Xie, L.; Mathew, M.S.; Ofori, A.; Perry, T.; Wesley, D.; Messiah, S.E. Pediatric telehealth expansion in response to COVID-19. Frontiers in pediatrics 2021, 9, 642089. [Google Scholar] [CrossRef]
- Strehle, E.; Shabde, N. One hundred years of telemedicine: Does this new technology have a place in paediatrics? Archives of disease in childhood 2006, 91, 956–959. [Google Scholar] [CrossRef]
- Organization, W.H. Telemedicine: Opportunities and developments in member states - Report on the second global survey on eHealth (Global Observatory for eHealth Series, 2); Geneva, Switzerland, (2010).
- NSCH. National Survey of Children’s Health. Available online: https://www.childhealthdata.org/learn-about-the-nsch/methods (accessed on 5/30).
- Gurney, J.G.; McPheeters, M.L.; Davis, M.M. Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Archives of pediatrics & adolescent medicine 2006, 160, 825–830. [Google Scholar]
- Child; Initiative, A.H.M. National Survey of Children’s Health (2 Years Combined Data Set): SPSS Data Set.[Internet]. Child and Adolescent Health Measurement Initiative, 2021.
- Shaw, T.E.; Currie, G.P.; Koudelka, C.W.; Simpson, E.L. Eczema prevalence in the United States: Data from the 2003 National Survey of Children's Health. Journal of Investigative Dermatology 2011, 131, 67–73. [Google Scholar] [CrossRef]
- Stock, J.H.; Watson, M.W. Introduction to econometrics; Pearson: 2020.
- Breiman, L. Classification and regression trees; Routledge: 2017.
- Chang, E.; Penfold, R.B.; Berkman, N.D. Patient characteristics and telemedicine use in the US, 2022. JAMA network open 2024, 7, e243354–e243354. [Google Scholar] [CrossRef]
- Ing, E.B.; Ing, R. The use of a nomogram to visually interpret a logistic regression prediction model for giant cell arteritis. Neuro-Ophthalmology 2018, 42, 284–286. [Google Scholar] [CrossRef]
- Zlotnik, A.; Abraira, V. A general-purpose nomogram generator for predictive logistic regression models. The Stata Journal 2015, 15, 537–546. [Google Scholar] [CrossRef]
- Chun, F.K.-H.; Graefen, M.; Briganti, A.; Gallina, A.; Hopp, J.; Kattan, M.W.; Huland, H.; Karakiewicz, P.I. Initial biopsy outcome prediction—Head-to-head comparison of a logistic regression-based nomogram versus artificial neural network. European urology 2007, 51, 1236–1243. [Google Scholar] [CrossRef] [PubMed]
- Bertens, L.C.; Moons, K.G.; Rutten, F.H.; van Mourik, Y.; Hoes, A.W.; Reitsma, J.B. A nomogram was developed to enhance the use of multinomial logistic regression modeling in diagnostic research. Journal of clinical epidemiology 2016, 71, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.-S.; Lee, J.-Y. Building a Nomogram for Metabolic Syndrome Using Logistic Regression with a Complex Sample—A Study with 39,991,680 Cases. In Proceedings of the Healthcare; 2022; p. 372. [Google Scholar]
- Doximity. 2020 State of Telemedicine Report: Examining Patient Perspectives and Physician Adoption of Telemedicine Since the COVID-19 Pandemic. Available online: https://c8y.doxcdn.com/image/upload/Press%20Blog/Research%20Reports/2020-state-telemedicine-report.pdf (accessed on.
- Huang, M.; Wen, A.; He, H.; Wang, L.; Liu, S.; Wang, Y.; Zong, N.; Yu, Y.; Prigge, J.E.; Costello, B.A. Midwest rural-urban disparities in use of patient online services for COVID-19. The Journal of Rural Health 2022, 38, 908–915. [Google Scholar] [CrossRef] [PubMed]
- Pullyblank, K.; Krupa, N.; Scribani, M.; Chapman, A.; Kern, M.; Brunner, W. Trends in telehealth use among a cohort of rural patients during the COVID-19 pandemic. Digital Health 2023, 9, 20552076231203803. [Google Scholar] [CrossRef]
- Chu, C.; Cram, P.; Pang, A.; Stamenova, V.; Tadrous, M.; Bhatia, R.S. Rural telemedicine use before and during the COVID-19 pandemic: Repeated cross-sectional study. Journal of medical Internet research 2021, 23, e26960. [Google Scholar] [CrossRef]
- Turcios, Y. Digital access: A super determinant of health. Substance Abuse and Mental Health Services Administration 2023, 1–9. [Google Scholar]
- Philip, L.; Cottrill, C.; Farrington, J.; Williams, F.; Ashmore, F. The digital divide: Patterns, policy and scenarios for connecting the ‘final few’in rural communities across Great Britain. Journal of rural studies 2017, 54, 386–398. [Google Scholar] [CrossRef]
- Commission, F.C. Mapping broadband health in America. Accessed on March 2020, 28. [Google Scholar]
- Stewart, A. Internet Access Measures the Impact of the Digital Divide and COVID-19. Available online: https://www.shadac.org/news/internet-access-measures-impact-digital-divide-and-covid-19 (accessed on.
- U.S. Department of Commerce, C.B. U.S. Department of Commerce, C.B. 2015 American Community Survey (ACS) Public Use Microdata Sample (PUMS) data. Available online: https://www.census.gov/programs-surveys/acs/microdata.html (accessed on.
- Obermier, T.R. Residential internet access cost in Nebraska. Great Plains Research 2018, 28, 149–154. [Google Scholar] [CrossRef]
- Commission, F.C. Eighth Broadband Progress Report. Available online: https://www.fcc.gov/reports-research/reports/broadband-progress-reports/eighth-broadband-progress-report (accessed on.
- ForbesAdvisor. Millions Of Americans Are Still Missing Out On Broadband Access And Leaving Money On The Table—Here’s Why. Available online: https://www.forbes.com/advisor/personal-finance/millions-lack-broadband-access/ (accessed on.
- Kyle, M.A.; Blendon, R.J.; Findling, M.G.; Benson, J.M. Telehealth use and satisfaction among US households: Results of a national survey. Journal of patient experience 2021, 8, 23743735211052737. [Google Scholar] [CrossRef] [PubMed]
- Sisk, B.; Alexander, J.; Bodnar, C.; Curfman, A.; Garber, K.; McSwain, S.D.; Perrin, J.M. Pediatrician attitudes toward and experiences with telehealth use: Results from a national survey. Academic pediatrics 2020, 20, 628–635. [Google Scholar] [CrossRef]
- Administration, N.T.a.I. Office of Internet Connectivity and Growth 2023 Annual Report. Available online: https://www.ntia.gov/report/2024/office-internet-connectivity-and-growth-2023-annual-report (accessed on.
- Services, C.f.M.a.M. Coronavirus waivers & flexibilities. Available online: https://www.cms.gov/coronavirus-waivers (accessed on.
- Shaver, J. The state of telehealth before and after the COVID-19 pandemic. Primary Care: Clinics in Office Practice 2022, 49, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Khera, N.; Knoedler, M.; Meier, S.K.; TerKonda, S.; Williams, R.D.; Wittich, C.M.; Coffey, J.D.; Demaerschalk, B.M. Payment and Coverage Parity for Virtual Care and In-Person Care: How Do We Get There? Telemedicine Reports 2023, 4, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Baumann, I.; Jaks, R.; Robin, D.; Juvalta, S.; Dratva, J. Parents’ health information seeking behaviour–does the child’s health status play a role? BMC family practice 2020, 21, 1–9. [Google Scholar] [CrossRef]
- Yardi, S.; Caldwell, P.H.; Barnes, E.H.; Scott, K.M. Determining parents' patterns of behaviour when searching for online information on their child's health. Journal of paediatrics and child health 2018, 54, 1246–1254. [Google Scholar] [CrossRef]
- Nicholas, D.; McNeill, T.; Montgomery, G.; Stapleford, C.; McClure, M. Communication features in an online group for fathers of children with spina bifida: Considerations for group development among men. Social Work with Groups 2004, 26, 65–80. [Google Scholar] [CrossRef]
- Provenzi, L.; Grumi, S.; Borgatti, R. Alone with the kids: Tele-medicine for children with special healthcare needs during COVID-19 emergency. Frontiers in psychology 2020, 11, 2193. [Google Scholar] [CrossRef]
- Aishworiya, R.; Kang, Y.Q. Including children with developmental disabilities in the equation during this COVID-19 pandemic. Journal of autism and developmental disorders 2021, 51, 2155–2158. [Google Scholar] [CrossRef]
- Riley, E.N.; Cordell, K.D.; Shimshock, S.M.; Perez Figueroa, R.E.; Lyons, J.S.; Vsevolozhskaya, O.A. Evaluation of telehealth in child behavioral health services delivery during the COVID-19 pandemic. Psychiatric Services 2023, 74, 237–243. [Google Scholar] [CrossRef]
- Pinkerton, L.M.; Murphy, A.; Bruckner, E.; Risser, H. Therapy service delivery for children with disabilities during COVID-19: Parent perceptions and implementation recommendations. Journal of Community Psychology 2023, 51, 2430–2441. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, N.R.; Ely, S.L.; Garcia, B.N.B.; Bowden, J. Addressing pediatric mental health using telehealth during coronavirus disease-2019 and beyond: A narrative review. Academic pediatrics 2021, 21, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Schweiberger, K.; Hoberman, A.; Iagnemma, J.; Schoemer, P.; Squire, J.; Taormina, J.; Wolfson, D.; Ray, K.N. Practice-level variation in telemedicine use in a pediatric primary care network during the COVID-19 pandemic: Retrospective analysis and survey study. Journal of medical internet research 2020, 22, e24345. [Google Scholar] [CrossRef] [PubMed]
- Saunders, N.R.; Toulany, A.; Deb, B.; Strauss, R.; Vigod, S.N.; Guttmann, A.; Chiu, M.; Huang, A.; Fung, K.; Chen, S. Acute mental health service use following onset of the COVID-19 pandemic in Ontario, Canada: A trend analysis. Canadian Medical Association Open Access Journal 2021, 9, E988–E997. [Google Scholar] [CrossRef]
- Madigan, S.; Racine, N.; Vaillancourt, T.; Korczak, D.J.; Hewitt, J.M.; Pador, P.; Park, J.L.; McArthur, B.A.; Holy, C.; Neville, R.D. Changes in depression and anxiety among children and adolescents from before to during the COVID-19 pandemic: A systematic review and meta-analysis. JAMA pediatrics 2023. [Google Scholar] [CrossRef]
| Telehealth Visits were Due to COVID-19 (n=16,583) |
Telehealth Visits but Not Due to COVID-19 (n=3,797) |
||||||
| State/District | Frequency1 | Percentage2 | 95 % Confidence Interval | State/District | Frequency1 | Percentage2 | 95 % Confidence Interval |
| North Dakota | 100 | 6.99 | (5.26, 8.73) | Oklahoma | 48 | 2.26 | (1.49, 3.04) |
| Wyoming | 133 | 7.40 | (5.79, 9.01) | Idaho | 41 | 2.27 | (1.43, 3.10) |
| Idaho | 133 | 7.43 | (5.68, 9.19) | North Dakota | 45 | 2.31 | (1.49, 3.12) |
| Mississippi | 140 | 7.45 | (5.84, 9.07) | Louisiana | 44 | 2.32 | (1.44, 3.20) |
| Montana | 140 | 7.47 | (5.81, 9.13) | Tennessee | 70 | 2.34 | (1.60, 3.09) |
| South Dakota | 133 | 8.18 | (6.39, 9.97) | Nebraska | 54 | 2.53 | (1.67, 3.39) |
| Alabama | 149 | 8.22 | (6.46, 9.99) | Mississippi | 44 | 2.66 | (1.65, 3.67) |
| Nebraska | 204 | 8.59 | (7.10, 10.08) | South Dakota | 51 | 2.71 | (1.80, 3.61) |
| Tennessee | 239 | 8.67 | (7.11, 10.23) | Alabama | 48 | 2.77 | (1.58, 3.95) |
| Nevada | 156 | 9.20 | (7.25, 11.16) | Arkansas | 56 | 2.91 | (1.93, 3.89) |
| Utah | 189 | 10.21 | (8.37, 12.05) | West Virginia | 49 | 2.99 | (1.94, 4.04) |
| Missouri | 188 | 10.27 | (8.31, 12.23) | New Mexico | 62 | 3.13 | (2.00, 4.27) |
| Indiana | 206 | 11.07 | (9.21, 12.94) | Iowa | 55 | 3.14 | (2.05, 4.24) |
| Georgia | 338 | 11.34 | (9.60, 13.08) | Illinois | 46 | 3.14 | (1.85, 4.44) |
| Arkansas | 193 | 11.55 | (9.37, 13.74) | Kansas | 59 | 3.35 | (2.31, 4.40) |
| Iowa | 218 | 11.86 | (9.94, 13.79) | Vermont | 48 | 3.45 | (2.24, 4.65) |
| Wisconsin | 375 | 11.97 | (10.17, 13.78) | Rhode Island | 40 | 3.53 | (2.09, 4.97) |
| Louisiana | 184 | 11.99 | (9.61, 14.36) | Missouri | 51 | 3.60 | (2.30, 4.90) |
| Oklahoma | 204 | 12.01 | (9.88, 14.14) | Ohio | 101 | 3.64 | (2.74, 4.55) |
| Kansas | 220 | 12.35 | (10.33, 14.37) | Wisconsin | 88 | 3.67 | (2.60, 4.74) |
| South Carolina | 228 | 12.49 | (10.34, 14.63) | New York | 211 | 3.68 | (2.89, 4.47) |
| Ohio | 434 | 13.19 | (11.68, 14.71) | Kentucky | 47 | 3.75 | (2.28, 5.21) |
| Florida | 249 | 13.47 | (11.33, 15.60) | North Carolina | 68 | 3.75 | (2.49, 5.01) |
| Illinois | 271 | 13.95 | (11.77, 16.14) | Hawaii | 67 | 3.77 | (2.46, 5.07) |
| Arizona | 217 | 14.00 | (11.45, 16.55) | South Carolina | 48 | 3.79 | (2.32, 5.25) |
| Michigan | 247 | 14.22 | (12.02, 16.41) | Montana | 43 | 3.81 | (2.26, 5.36) |
| Kentucky | 234 | 14.22 | (11.89, 16.54) | Nevada | 60 | 3.88 | (2.51, 5.25) |
| Texas | 250 | 14.66 | (12.15, 17.18) | Maine | 55 | 3.92 | (2.54, 5.30) |
| Alaska | 279 | 14.68 | (12.41, 16.96) | Michigan | 64 | 3.92 | (2.64, 5.20) |
| West Virginia | 252 | 14.86 | (12.47, 17.24) | Wyoming | 92 | 4.02 | (3.01, 5.03) |
| Colorado | 542 | 16.01 | (14.17, 17.86) | Indiana | 59 | 4.15 | (2.75, 5.55) |
| Pennsylvania | 407 | 16.24 | (14.21, 18.26) | Utah | 76 | 4.16 | (2.98, 5.35) |
| New Mexico | 294 | 16.44 | (13.90, 18.97) | Arizona | 61 | 4.27 | (2.77, 5.78) |
| Maine | 312 | 16.51 | (14.28, 18.73) | Pennsylvania | 97 | 4.28 | (3.05, 5.51) |
| New York | 866 | 16.85 | (14.77, 18.93) | Oregon | 202 | 4.37 | (3.48, 5.26) |
| Minnesota | 279 | 16.95 | (14.49, 19.40) | Virginia | 63 | 4.40 | (3.03, 5.77) |
| North Carolina | 279 | 17.45 | (14.74, 20.16) | Massachusetts | 53 | 4.60 | (2.86, 6.33) |
| Virginia | 318 | 17.56 | (15.00, 20.11) | Texas | 70 | 4.68 | (3.23, 6.13) |
| Washington | 322 | 17.78 | (15.25, 20.31) | Georgia | 107 | 4.69 | (3.51, 5.87) |
| Delaware | 323 | 18.08 | (15.56, 20.59) | Maryland | 62 | 4.82 | (3.10, 6.54) |
| Hawaii | 411 | 18.84 | (16.49, 21.19) | New Jersey | 66 | 4.88 | (3.34, 6.42) |
| Rhode Island | 341 | 19.48 | (16.69, 22.27) | Delaware | 71 | 4.90 | (3.30, 6.50) |
| New Jersey | 337 | 20.40 | (17.60, 23.21) | New Hampshire | 48 | 4.92 | (3.16, 6.69) |
| New Hampshire | 343 | 20.53 | (18.02, 23.05) | Alaska | 62 | 5.04 | (3.24, 6.84) |
| Oregon | 1290 | 21.80 | (20.22, 23.37) | Colorado | 150 | 5.07 | (3.95, 6.18) |
| Connecticut | 388 | 23.29 | (20.38, 26.20) | Connecticut | 67 | 5.23 | (3.59, 6.86) |
| California | 1154 | 23.65 | (21.24, 26.07) | Minnesota | 73 | 5.27 | (3.58, 6.97) |
| Vermont | 414 | 24.61 | (21.82, 27.39) | Washington | 71 | 5.34 | (3.56, 7.12) |
| Maryland | 405 | 25.66 | (22.54, 28.79) | California | 307 | 5.70 | (4.25, 7.16) |
| Massachusetts | 438 | 27.18 | (24.25, 30.12) | Florida | 88 | 6.53 | (4.74, 8.32) |
| District of Columbia | 617 | 31.91 | (28.03, 35.79) | District of Columbia | 89 | 10.35 | (7.16, 13.54) |
| Telehealth Visits were Due to COVID-19 | Telehealth Visits but Not Due to COVID-19 | |||||
| Variables | OR1 | 95% C.I.2 | p-value3 | OR1 | 95% C.I.2 | p-value3 |
| Age | ||||||
| <4 | 1 | 1 | ||||
| 4-8 | 0.89 | 0.84-0.95 | 0.0001* | 0.74 | 0.66-0.82 | <.0001* |
| 9-12 | 1.14 | 1.07-1.21 | <.0001* | 0.76 | 0.67-0.85 | <.0001* |
| 13-17 | 1.42 | 1.34-1.50 | <.0001* | 0.91 | 0.82-1.01 | 0.1110 |
| Sex | ||||||
| Female | 1 | 1 | ||||
| Male | 0.99 | 0.95-1.03 | 0.4574 | 0.95 | 0.88-1.03 | 0.2925 |
| Race/Ethnicity | ||||||
| Black, non-Hispanic | 1 | 1 | ||||
| Hispanic | 1.25 | 1.13-1.38 | <.0001* | 1.07 | 0.89-1.29 | 0.4674 |
| White, non-Hispanic | 1.17 | 1.07-1.27 | 0.0008* | 0.94 | 0.80-1.10 | 0.4427 |
| Other/Multi-racial, non-Hispanic | 1.20 | 1.08-1.32 | 0.0005* | 1.02 | 0.84-1.22 | 0.8931 |
| Child born in the United States | ||||||
| No | 1 | 1 | ||||
| Yes | 1.09 | 0.96-1.23 | 0.1792 | 0.90 | 0.73-1.12 | 0.3880 |
| Parent’s highest education level | ||||||
| Less than high school | 1 | 1 | ||||
| High school/GED | 1.34 | 1.13-1.59 | 0.0009* | 1.20 | 0.89-1.63 | 0.2925 |
| Greater than high school | 2.08 | 1.77-2.44 | <.0001* | 1.51 | 1.14-2.00 | 0.0097* |
| Family structure of child’s household | ||||||
| Two parents, currently married | 1 | 1 | ||||
| Two parents, not currently married | 0.92 | 0.84-1.00 | 0.0651 | 0.92 | 0.77-1.09 | 0.3777 |
| Single parent | 1.00 | 0.95-1.06 | 0.9081 | 0.93 | 0.84-1.03 | 0.2552 |
| Grandparent household | 0.86 | 0.75-0.98 | 0.0212* | 0.79 | 0.61-1.03 | 0.1266 |
| Other | 1.48 | 1.22-1.78 | <.0001* | 1.41 | 0.98-2.03 | 0.1107 |
| Number of family members | ||||||
| 1 or 2 | 1 | 1 | ||||
| 3 | 0.94 | 0.87-1.02 | 0.1677 | 1.09 | 0.92-1.28 | 0.3777 |
| 4 | 0.83 | 0.76-0.90 | <.0001* | 0.91 | 0.78-1.08 | 0.3444 |
| 5+ | 0.69 | 0.63-0.75 | <.0001* | 0.79 | 0.66-0.94 | 0.0149* |
| Difficulty covering basics | ||||||
| Never or rarely | 1 | 1 | ||||
| Somewhat or very often | 1.26 | 1.18-1.34 | <.0001* | 1.05 | 0.93-1.19 | 0.4497 |
| Residence in metropolitan area | ||||||
| No | 1 | 1 | ||||
| Yes | 1.69 | 1.59-1.80 | <.0001* | 1.36 | 1.21-1.52 | <.0001* |
| English is the primary language spoken at home | ||||||
| No | 1 | 1 | ||||
| Yes | 1.35 | 1.24-1.46 | <.0001* | 0.92 | 0.80-1.05 | 0.2925 |
| Type of Insurance | ||||||
| Uninsured | 1 | 1 | ||||
| Public | 2.38 | 2.06-2.74 | <.0001* | 1.33 | 1.06-1.67 | 0.0259* |
| Private | 2.48 | 2.15-2.84 | <.0001* | 1.34 | 1.08-1.66 | 0.0172* |
| Public + Private | 3.80 | 3.24-4.47 | <.0001* | 1.78 | 1.36-2.34 | <.0001* |
| Consistent health insurance coverage during the past 12 months | ||||||
| No | 1 | 1 | ||||
| Yes | 1.97 | 1.75-2.21 | <.0001* | 1.31 | 1.08-1.59 | 0.0138* |
| Household income | ||||||
| 400% FPL4 | 1 | 1 | ||||
| 200-399% FPL | 0.69 | 0.66-0.73 | <.0001* | 0.81 | 0.74-0.89 | 0.0319* |
| 100-199% FPL | 0.72 | 0.68-0.76 | <.0001* | 0.80 | 0.71-0.90 | 0.0003* |
| 0-99% FPL | 0.68 | 0.64-0.73 | <.0001* | 0.86 | 0.76-0.97 | <.0001* |
| Missed preventive care in past 12 months due to the COVID-19 pandemic | ||||||
| No | 1 | 1 | ||||
| Yes | 1.49 | 1.40-1.58 | <.0001* | 0.73 | 0.63-0.86 | 0.0003* |
| Usual source of pediatric preventive care | ||||||
| Yes | 1 | 1 | ||||
| No | 0.40 | 0.38-0.43 | <.0001* | 0.57 | 0.51-0.64 | <.0001* |
| Personal doctor or nurse for child | 1 | |||||
| Yes | 0.56 | 0.53-0.59 | <.0001* | 0.83 | 0.76-0.91 | 0.0003* |
| No | ||||||
| Perceived child health | ||||||
| Excellent or very good | 1 | 1 | ||||
| Good | 2.59 | 2.42-2.76 | <.0001* | 2.05 | 1.80-2.33 | <.0001* |
| Fair or poor | 4.91 | 4.25-5.67 | <.0001* | 3.55 | 2.71-4.65 | <.0001* |
| Mother’s physical health | ||||||
| Excellent or very good | 1 | 1 | ||||
| Good | 1.21 | 1.15-1.27 | <.0001* | 1.07 | 0.98-1.18 | 0.2116 |
| Fair or poor | 1.47 | 1.34-1.60 | <.0001* | 1.20 | 1.01-1.43 | 0.0696 |
| Father’s physical health | ||||||
| Excellent or very good | 1 | 1 | ||||
| Good | 1.16 | 1.10-1.22 | <.0001* | 1.05 | 0.95-1.17 | 0.3712 |
| Fair or poor | 1.34 | 1.21-1.48 | <.0001* | 0.99 | 0.80-1.22 | 0.9105 |
| Mother’s mental health | ||||||
| Excellent or very good | 1 | 1 | ||||
| Good | 1.34 | 1.28-1.40 | <.0001* | 1.05 | 0.96-1.16 | 0.3542 |
| Fair or poor | 1.61 | 1.49-1.73 | <.0001* | 1.21 | 1.04-1.41 | 0.0261* |
| Father’s mental health | ||||||
| Excellent or very good | 1 | 1 | ||||
| Good | 1.29 | 1.22-1.36 | <.0001* | 1.07 | 0.96-1.19 | 0.2925 |
| Fair or poor | 1.75 | 1.59-1.92 | <.0001* | 1.13 | 0.93-1.39 | 0.2925 |
| Child had the health conditions (Yes vs. No) | ||||||
| Allergy to food, drug, or insect | 1.86 | 1.78-1.95 | <.0001* | 1.41 | 1.29-1.54 | <.0001* |
| Asthma | 2.23 | 2.08-2.39 | <.0001* | 1.69 | 1.47-1.95 | <.0001* |
| Blood disorders | 1.95 | 1.52-2.50 | <.0001* | 2.31 | 1.50-3.56 | 0.0004* |
| Brain injury | 2.09 | 1.91-2.29 | <.0001* | 1.77 | 1.48-2.12 | <.0001* |
| Cerebral palsy | 6.54 | 4.88-8.78 | <.0001* | 2.02 | 0.98-4.17 | 0.0965 |
| Seizure | 6.32 | 5.15-7.75 | <.0001* | 4.01 | 2.73-5.90 | <.0001* |
| Attention-deficit/hyperactivity disorder (ADHD) | 4.22 | 3.98-4.46 | <.0001* | 2.56 | 2.27-2.88 | <.0001* |
| Autism Spectrum Disorder (ASD) | 3.83 | 3.50-4.20 | <.0001* | 2.24 | 1.84-2.73 | <.0001* |
| Headache | 3.03 | 2.73-3.37 | <.0001* | 2.21 | 1.78-2.74 | <.0001* |
| Tourette Syndrome | 5.79 | 4.28-7.85 | <.0001* | 3.13 | 1.66-5.89 | 0.0010* |
| Anxiety | 5.81 | 5.50-6.14 | <.0001* | 3.40 | 3.05-3.80 | <.0001* |
| Depression | 6.78 | 6.28-7.33 | <.0001* | 4.78 | 4.13-5.53 | <.0001* |
| Deafness or problems with hearing | 1.99 | 1.69-2.34 | <.0001* | 1.43 | 1.01-2.02 | 0.0807 |
| Blindness or problems with seeing | 1.81 | 1.56-2.10 | <.0001* | 1.21 | 0.87-1.68 | 0.3260 |
| Special health care needs | ||||||
| No | 1 | 1 | ||||
| Yes | 5.11 | 4.90-5.34 | <.0001* | 2.83 | 2.60-3.07 | <.0001* |
| Telehealth Visits were Due to COVID-19 | Telehealth Visits but Not Due to COVID-19 | |||||
| OR1 | 95% C.I.2 | p-value3 | OR1 | 95% C.I.2 | p-value3 | |
| Age | ||||||
| <4 | -- | -- | -- | 1 | ||
| 4-8 | -- | -- | -- | 0.81 | 0.65-1.01 | 0.1157 |
| 9-12 | -- | -- | -- | 0.68 | 0.53-0.87 | 0.0080* |
| 13-17 | -- | -- | -- | 0.68 | 0.54-0.86 | 0.0056* |
| Parent’s highest education level | ||||||
| Less than high school | 1 | 1 | ||||
| High school/GED | 0.89 | 0.70-1.14 | 0.3590 | 0.78 | 0.50-1.22 | 0.3964 |
| Greater than high school | 1.23 | 0.98-1.55 | 0.0935 | 0.93 | 0.61-1.41 | 0.7635 |
| Number of family members | ||||||
| 1 or 2 | -- | -- | -- | 1 | ||
| 3 | -- | -- | -- | 1.03 | 0.77-1.38 | 0.8258 |
| 4 | -- | -- | -- | 0.87 | 0.65-1.16 | 0.4735 |
| 5+ | -- | -- | -- | 0.83 | 0.62-1.12 | 0.3601 |
| Type of Insurance | ||||||
| Uninsured | 1 | -- | -- | -- | ||
| Public | 1.45 | 1.19-1.76 | 0.0003* | -- | -- | -- |
| Private | 1.55 | 1.29-1.88 | <.0001* | -- | -- | -- |
| Public + Private | 2.06 | 1.65-2.57 | <.0001* | -- | -- | -- |
| Household income | ||||||
| 400% FPL4 | 1 | -- | -- | -- | ||
| 200-399% FPL | 0.68 | 0.63-0.72 | <.0001* | -- | -- | -- |
| 100-199% FPL | 0.69 | 0.63-0.76 | <.0001* | -- | -- | -- |
| 0-99% FPL | 0.64 | 0.57-0.72 | <.0001* | -- | -- | -- |
| Missed preventive care in past 12 months due to the COVID-19 pandemic | ||||||
| No | 1 | 1 | ||||
| Yes | 1.25 | 1.18-1.33 | <.0001* | 0.70 | 0.60-0.81 | <.0001* |
| Usual source of pediatric preventive care | ||||||
| Yes | 1 | 1 | ||||
| No | 0.50 | 0.46-0.55 | <.0001* | 0.73 | 0.61-0.87 | 0.0031* |
| Personal doctor or nurse for child | ||||||
| Yes | 1 | 1 | ||||
| No | 0.75 | 0.70-0.81 | <.0001* | 1.06 | 0.91-1.24 | 0.5304 |
| Perceived child health | ||||||
| Excellent or very good | 1 | 1 | ||||
| Good | 1.26 | 1.14-1.40 | <.0001* | 1.35 | 1.06-1.73 | 0.0360* |
| Fair or poor | 1.98 | 1.58-2.47 | <.0001* | 1.98 | 1.20-3.26 | 0.0213* |
| Mother’s mental health | ||||||
| Excellent or very good | -- | -- | -- | 1 | ||
| Good | -- | -- | -- | 0.97 | 0.83-1.14 | 0.7635 |
| Fair or poor | -- | -- | -- | 0.92 | 0.69-1.22 | 0.6235 |
| Child had the health conditions (Yes vs. No) | ||||||
| Allergy to food, drug, or insect | 1.13 | 1.06-1.21 | 0.0003* | -- | -- | -- |
| Asthma | -- | -- | -- | 1.26 | 0.99-1.60 | 0.1031 |
| Blood disorders | -- | -- | -- | 2.30 | 1.18-4.49 | 0.0360* |
| Brain injury | 1.35 | 1.19-1.54 | <.0001* | -- | -- | -- |
| Cerebral palsy | 1.43 | 0.94-2.17 | 0.1121 | -- | -- | -- |
| Seizure | 1.80 | 1.32-2.46 | 0.0003* | -- | -- | -- |
| Attention-deficit/hyperactivity disorder (ADHD) | 1.67 | 1.53-1.82 | <.0001* | 1.12 | 0.88-1.41 | 0.4753 |
| Autism Spectrum Disorder (ASD) | 1.12 | 0.98-1.28 | 0.1166 | 1.33 | 0.96-1.85 | 0.1386 |
| Headache | 1.08 | 0.92-1.25 | 0.3590 | -- | -- | -- |
| Anxiety | 2.17 | 1.99-2.37 | <.0001* | 1.41 | 1.11-1.80 | 0.0171* |
| Depression | 1.78 | 1.57-2.01 | <.0001* | 1.83 | 1.33-2.52 | 0.0015* |
| Special health care needs | ||||||
| No | 1 | 1 | ||||
| Yes | 3.04 | 2.83-3.26 | <.0001* | 1.72 | 1.44-2.06 | <.0001* |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





