1. Introduction
Pacemakers have evolved over the last 70 years [1]. Programing in early single lead pacemakers
consisted of three parameters: amplitude, pulse width, and rate. Pacemakers 40
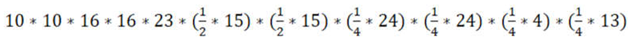
years later have multiple leads and over 233 programmable elements Table 1. Utilizing 170 elements of the 7 main
programmable features; selects 3,875,040,000 programing options to optimize
cardiac function at rest. Additional options are available to improve exercise
capacity. Early device therapy was designed to treat failure of electrical
conduction. Current devices augment heart failure therapy by restoring
synchrony of atrial to ventricular (AV) conduction and ventricular septal
depolarization. Early programming was designed to extend the life of the
pacemaker, whereas current programming may extend the life of the patient at
the expense of battery life. The combination of different pacing settings is an
extremely large number; therefore, programing is often set to “out of the box”
parameters. Many patients benefit from those parameters, but many others have
continued symptoms. Optimization is for this group.
Table 1.
Programmable Choices.
Table 1.
Programmable Choices.
Pacing
Parameter |
Parameter Options |
Programmable
Choices |
Left Lead
single |
4 Positions |
10
|
Left lead
Multi-site |
4 Positions |
10
|
RV LV
sequence |
4 Possibilities
RV before LV
LV before RV
LV only
RV only |
16 Timing Delays |
| Pulse width |
|
16
|
| Amplitude |
|
23 |
| Heart rate |
Base Rate
30-109
Rest Rate
30-95 |
15
15 |
| AV delay |
Paced AV Delay
Sensed AV Delay
Rate Responsive
Shortest AVD |
24
24
4
13 |
| Rate adaptive |
Threshold
Slope
Max sensor rate
Reaction time
Recovery time |
19
21
15
4
4 |
Based on the table, one selection from each row, with multiple choices per row the formula would be
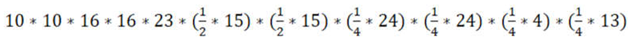
= 3,875,040,000 |
Implantation of the device is limited to the anatomical constraints of the patient which can sometimes be improved by programming. The left ventricular lead evolved from unipolar to bi-polar to 4 different longitudinal leads in part to diminish diaphragmatic stimulation. Multi-lead pacing, His Bundle or Bundle pacing adds additional permutations adding additional complexity. Early randomized pacemaker trials limited the programing; resulting in a small defined group deemed improved. Many other individuals can benefit. The methodology in this paper is not designed around clinical trials. Optimization of echo parameters and physiology of cardiac disease are used to improve cardiac function by selecting pacemaker programming functions.
The spectrum of cardiac disease adds intricacy requiring different optimization goals. Early pacemakers and more modern pacemakers have not accounted for two hearts, a right and a left heart. The failure of either heart will result in morbidity and mortality in the patient. Failure of the left heart eventually causes failure of the right heart. This means the pacing strategy must change as heart function evolves. The function of current devices is to improve right heart function by improving left heart function. The left sided strategy leaves some patients with advanced disease and primary right heart failure no options for improvement.
The purpose of this discussion is to provide an efficient rationale to optimize pacemakers for the spectrum of cardiac disease. The goal is to recognize anatomical and functional abnormalities of the heart, correcting these malfunctions with electrical stimulation. The method uses echocardiography and Doppler principles to identify and modify abnormal cardiac structure and function.
Spectrum of Cardiac Disease
Left Bundle Branch block (LBBB) dyssynchrony, Right Ventricular (RV) pacing dyssynchrony
Annular dilation and mitral regurgitation
Left versus right heart failure
Optimizing right heart function in the setting of an Left Ventricular Assist Device (LVAD)
Annular dilation and tricuspid regurgitation
Restrictive cardiac disease
Valvular disease restricting stroke volume
Peripheral vascular disease with fixed systemic vascular resistance restricting stroke volume
Hypertrophic cardiomyopathy with obstruction
Wide QRS duration dilated cardiomyopathy
Longitudinal versus circumferential dyssynchrony
Narrow QRS duration dilated cardiomyopathy
Ectopy induced dyssynchrony
Variable RR intervals
Desired Outcomes of Pacing
Increase forward flow
Decrease backward flow (regurgitation)
Restore circumferential and longitudinal synchrony
Decrease the size of the heart
Support the failing ventricle with control of the interventricular septum
Narrow the QRS duration to increase the power of the heart
Increase the heart rate in individuals with fixed stroke volume
Reduce ventricular dyssynchrony from ectopic beats
Restore Regularity
Spectrum of Symptoms
Dyspnea, Shortness of breath – decrease filling pressures
Fatigability, Exercise Intolerance – increase cardiac output
Edema, Swelling, Fluid Retention – Improve right heart function
Arrhythmias – Improve function and decrease wall stress
Important Equations
Cardiac Output = Heart Rate X Stroke Volume
Cardiac Output = (Mean Blood Pressure – Right Atrial Pressure) X 80
Systemic Vascular Resistance
QRS duration = longest of (Circumference/2) X Circumferential Conduction Velocity
or (Longitudinal Circumference/2) X Longitudinal Conduction Velocity
Important Echocardiogram Measurements
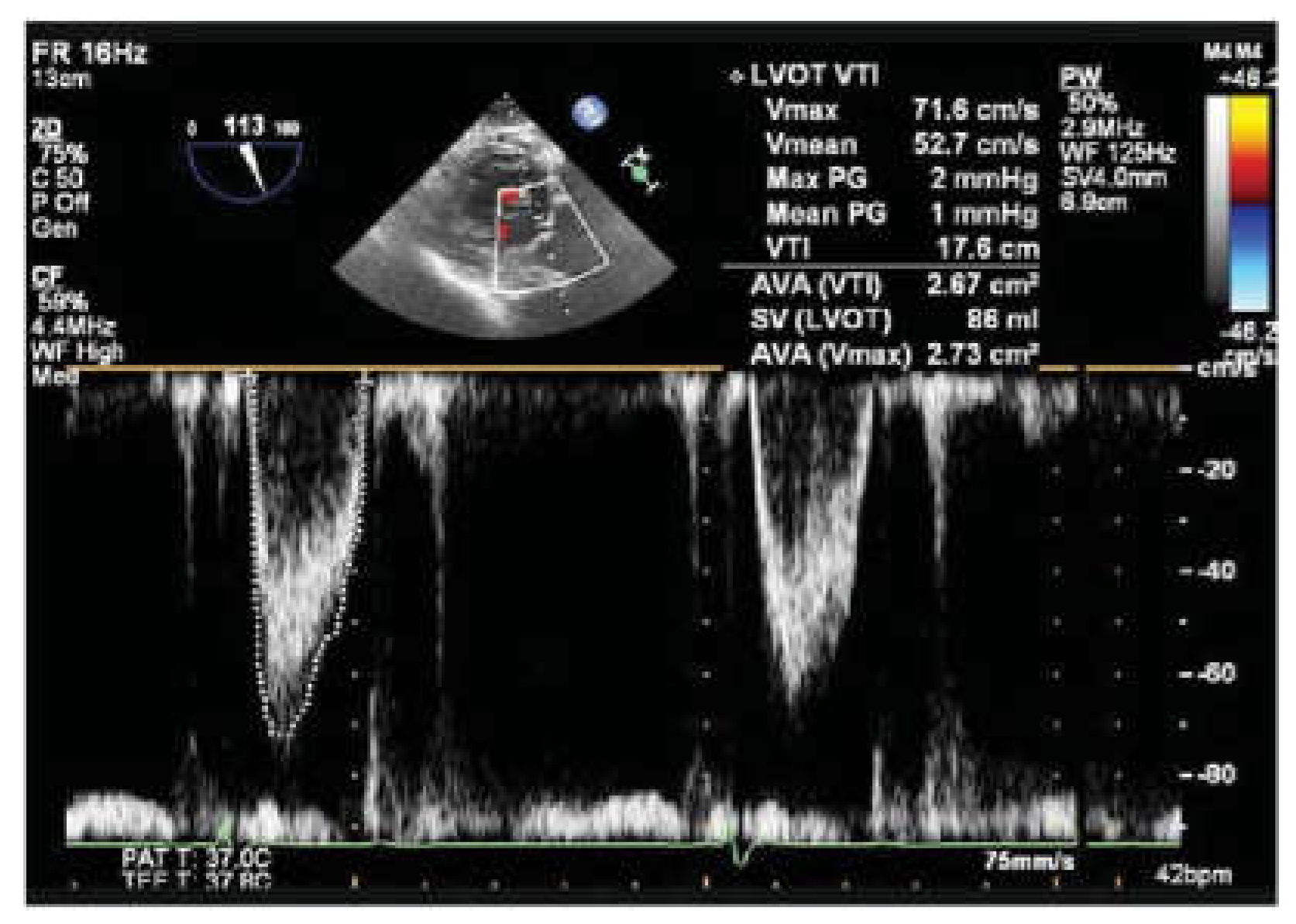
Left Ventricular Outflow Tract Velocity Time Integral (LVOT VTI)
Pulse wave velocity measurement must be taken at the same location for each measurement. Error will be introduced if measurement is taken too close to the aortic valve or too deep into the ventricle. If measurements are not consistent due to failure of consistent positioning of the sample volume (i.e., same location at each programing change) consider continuous wave Doppler as a more reliable measure. Ectopy and variable R-R intervals will also add to measurement error. Choose measurement beats based on similar RR intervals. This parameter reflects stroke volume with the goal of increasing this value. Heart rate has an influence on this value. In normal hearts at rest the cardiac output meets the demands of the body. Heart rate and stroke volume are inversely related. Raising the heart rate will reduce the stroke volume in hearts with normal filling. Stoke volume may not change in hearts with restrictive filling. Therefore, the first parameter in pacemaker optimization should be selection of an appropriate heart rate dependent on the ventricular filling [
2].
Mitral Valve Inflow Velocity
E A Wave Separation
Restrictive inflow pattern occurs if the ventricle is already volume loaded or the ventricle is stiff and fails to fill after initial mitral valve opening. In either condition stroke volume will not increase with greater diastolic filling times. The heart rate needs to increase to increase cardiac output. The selection of heart rate for restrictive disease must be an empirical estimate based on desired cardiac output. A tedious methodology includes titration of the heart rate until stroke volume begins to drop. This technique adds complexity, which is nearly impossible to perform, secondary to variation in respiration and sonographer attention span. For restrictive disease a good place to start is 80 bpm. The heart rate is the most important parameter and has to be selected first. Unfortunately, little is known about the optimum heart rate for restrictive disease [
2].
For systolic dysfunction a formula is available
Ideal heart rate (bpm) = 93 – 0.13 × deceleration time (msec). [
3]
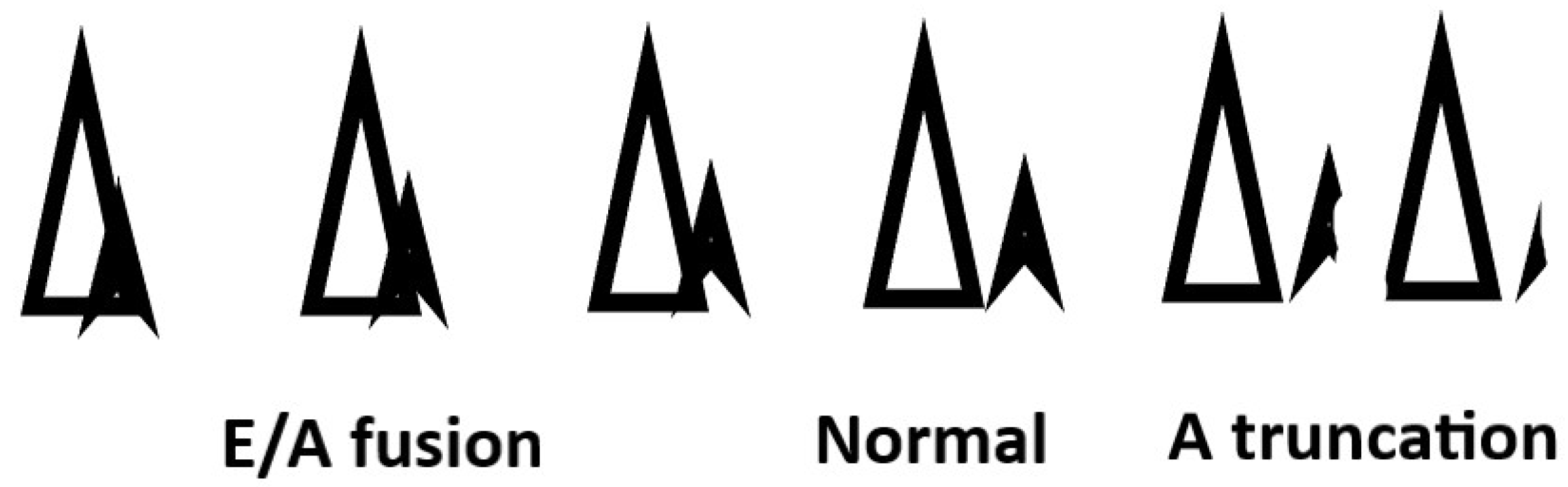
After the heart rate is selected attention to atrial ventricular transport is performed by optimizing E and A wave separation. In systolic heart failure guideline directed medications with beta blockers usually make patients dependent on atrial pacing. When beta blockers are not used as in restrictive disease or right ventricular failure sinus mechanism may be intact. In these cases, atrial pacing versus atrial sensing can make a big difference in AV transport. Thus, the AV delay will depend on atrial pacing or sensing. An intact AV node will allow intrinsic conduction to the ventricle. This is desired if there is no LBBB. These patients can maintain normal QRS configuration and avoid ventricular pacing dyssynchrony by programing a longer AV delay. The downside of this strategy is E and A wave fusion with greater filling pressure over a shorter time period. Long AV delays may harm some patients.
A Short AV delay is desired if mandatory ventricular pacing is the goal. Ventricular pacing is desired if you have a bi-ventricular device and have pre-existing dyssynchrony from left bundle branch block. Right ventricular pacing is desired in obstructive cardiomyopathy to induce paradoxical septal motion to relieve outflow obstruction. Right ventricular pacing is also desired in Cor Pulmonale. The short AV interval truncates the A wave with loss of atrial kick and reduced filling of the ventricle. The only way to manage individuals who are dependent on the atrial kick is to ablate the AV node to assure ventricular pacing and optimize atrial ventricular transport.
Effective Mitral valve Orifice – The iso-velocity curve orifice size is a visual assessment of the severity of mitral regurgitation. Optimization is achieved by reducing this area. An additional check on eccentric regurgitation or suspected occult regurgitation is to examine the height of the E wave of the mitral valve inflow. The reduction of the E wave is a signal of reduced mitral regurgitation
2-Dimensional Assessment of Dyssynchrony, Chamber Dimensions (Left Ventricular End Diastolic Volume), and Ejection Fraction –These standard echocardiographic measures should be performed initially and at the end of the optimizations to give further evidence of success.
Walk test – After the procedure the patient should go for a walk to be sure the adjustments were beneficial clinically.
Pacing Goals for the Spectrum of Cardiac Disease
LBBB dyssynchrony right ventricular pacing dyssynchrony – Clinical trials support bi-ventricular pacing for these two disease processes. The abnormality is circumferential dyssynchrony which causes a delay in septal activation, dyssynchrony, and widened QRS duration. The ejection fraction falls and mitral regurgitation increases. Late depolarization of the papillary muscle causes delayed repolarization with failure to relax the papillary muscle. The mitral valve remains slightly tethered open with the onset of systolic ejection. Early regurgitation begets more regurgitation. Restoring synchrony with left ventricular pacing requires selection of the lead configuration and timing of the right and left ventricular leads.
Annular dilation and mitral regurgitation – A common final pathway in systolic dysfunction is chamber enlargement. As the annulus stretches from ventricular dilation or atrial dilation the mitral valve can no longer co-apt. This results in mitral regurgitation and further atrial and ventricular dilation. Emptying the ventricle more frequently by increasing the heart rate can shrink chamber dimensions. Programing the left lead with the earliest activation (LV before RV set to the largest interval) will assure the mitral valve co-apt properly when systole begins. No clinical trial has addressed this solution.
Left versus right heart failure – There are two hearts; the left and right heart. Between these two hearts is the interventricular septum which can be programmed to help the right heart by right ventricular pacing. The phenotypic patient is an edematous, patient who is lying flat with renal insufficiency, hypotensive, with jugular venous distention and positive Kussmaul’s sign.
Optimizing right heart function with LVAD – Left ventricular assist devices is dependent on preload of the left ventricle. If preload of the left ventricle is reduced due to the right heart inability to pump across the pulmonary bed; the LVAD will have suction events. The cause may be volume depletion or right heart failure. Pacing the right ventricle causes septal dyssynchrony which favors the right ventricular function improving the filling of the left heart.
Annular dilation and tricuspid regurgitation – Further consequence of right heart failure is chamber enlargement with annular dilation. Tricuspid regurgitation secondary to pulmonary hypertension and annular dilation will cause more dilation and more regurgitation. Increasing heart rate may shrink the volume of the right heart providing better coaptation of the tricuspid valve.
Restrictive cardiac disease – Small hearts in amyloidosis or other infiltrative disease have small stroke volumes so these hearts are dependent on heart rate to increase cardiac output. Severe diastolic dysfunction also exists in large hearts with fixed stroke volumes. These large restrictive hearts require a higher heart rates.
Valvular disease restricting stroke volume - Aortic stenosis restricts stroke volume just as Peripheral vascular disease with fixed systemic vascular resistance – These conditions depend on heart rate to increase cardiac output.
Hypertrophic cardiomyopathy with obstruction – Paradoxical motion of the interventricular septum will reduce outflow track obstruction. This can be accomplished with right ventricular pacing. These ventricles are also restrictive and dependent on atrial ventricular transport. Ideally the best way to manage this condition is ablation of the AV node so the optimum AV delay can be chosen. In these patients atrial sensing versus atrial pacing must be assessed. The tradeoff is heart rate, AV delay, and atrial ventricular transport which depend on atrial mechanics. Complete right ventricular pacing without fusion is mandatory to maintain paradoxical sepat motion.
Wide QRS duration dilated cardiomyopathy – Heart enlargement increases the distance the electrical signal has to travel. This is reflected in the electrocardiogram as a wide QRS duration. The QRS may or may not have bundle branch morphology. Multiple leads and position of the leads can increase axial conduction velocity narrowing the QRS, potentially remodeling the heart into smaller chambers (see Mathematical Model below). Longitudinal conduction velocity is the major determinant of dilation and sphericity of the heart. Wider QRS reduces the power of the heart.
Narrow QRS duration dilated cardiomyopathy- Trials investigating cardiac dyssynchrony found no benefit in biventricular pacing for the dilated ventricle with narrow complex < 130 msec QRS duration [
4,
5]. For this reason, the therapy is not offered. The reason for this failure has not been elucidated; however, programming was limited. Proposed pathophysiology of narrow complex dilated cardiomyopathy is presented in the following article [
6]. Houck PD, Jones B, Patel R, et al. Pathophysiology of narrow complex dilated cardiomyopathy insight derived from the velocity equation: velocity = distance/time BMJ Case Rep 2019. The article suggests increasing the amplitude and pulse width can improve electromechanical coupling. Cardiac contractility modulation [
7,
8]is another proposed therapy.
Longitudinal versus circumferential dyssynchrony – With appropriately placed RV and LV lead the optimum timing delay is simultaneous. Circumferential dyssynchrony may require a delay.
Ectopy induced dyssynchrony –A high PVC burden with or without LBBB will cause dyssynchrony. In these case medications have to be added to reduce the burden of ectopy. Some of the PVC’s may be suppressed by increasing the base rate preventing premature beats from capturing the ventricle. Some pacing devices have an option to biventricular pace when an ectopic is sensed in attempt to fuse ectopic beats with normal pacing.
Variable RR intervals- Resynchronization therapy depends on the patient being paced. Atrial fibrillation with rapid response must be controlled to assure pacing therapy is delivered. Increasing the base rate, drugs to slow the rate of atrial fibrillation, or AV nodal ablation are method to restore irregularity of variable intervals.
Remodeling the Dilated Heart by Increasing Axial Propagation Velocity
Mathematical model
The following provides the mathematical relationships of lead placement and timing in relationship to QRS duration. Adding a third lead will increase circumferential propagation velocity by earlier initiation of impulses at the RV apex and lateral wall. Axial propagation velocity may be increased if the lead is placed between the base and apex. By placing multiple electrodes along the axis and timing them from base to apex the axial velocity can be increased and should restore ventricular geometry. The optimal number of leads depends on the conduction velocity, size of the heart (axial length = A defined as 1/2 the axial circumferential length = C and the QRS duration. The new QRS duration can be calculated from the following formula for pacemaker leads placed equidistant from the apex and fired in sequential fashion from apex to base.
QRSnew = (N+1)*QRSold /(2N)
QRS (sec) .196
N = Number of Leads 3
A =Axial Length (cm) 19
VA = Axial Conduction Velocity (cm/sec) 196
QRSnew = .667*.196 = .130 sec
Effective Conduction Velocity = 146 cm/sec
If the 3 leads were fired simultaneously the following formula can be used.
QRSnew = QRSold /(2N-1) QRSnew = .196/5 = .039
Effective Conduction Velocity = 487 cm/sec
(Likely not practical)
For a 2 - lead system firing simultaneously with one lead at the apex and a second lead located X cm from the apex along the axial perimeter with conduction velocity VA, the new QRS duration can be calculated from two formulas one for X≤2A/3 and one for X≥2A/3
There are two equations since for any condition other than 2A/3 there will be overlap of conduction either at the apex or base of the heart.
For X ≤ 2A/3 QRSnew = QRSold – X/(VA)
For X ≥ 2A/3 QRSnew = X/( 2*VA)
For X = 2A/3 There is no overlap QRSnew = QRSold/3
For X = A There is no overlap QRSnew = QRSold/2
For X = 0 There is 100% overlap QRSnew = QRSold
The QRS in the circumferential directions with one lead at the septal apex and one lead located Y cm away from the septum on the circumference, conduction velocity VC is calculated from two formulas for Y ≥ C/2 and
For Y ≥ C/2 QRSnew = Y/( 2*VC)
For Y ≤ C/2 QRSnew = QRSold – Y/VC
For Y = C/2 There is no overlap QRSnew = QRSold/2
For Y = 0 or Y = C There is 100% overlap QRSnew = QRSold
For a two lead with timing delay T the QRS duration in the axial direction is calculated from the following formula where T is the delay of the lateral lead, X is the apical displacement of the lateral lead from the apical lead and A is ½ the axial perimeter.
For X ≤ 2*A/3 - VAT/3 QRSnew = QRSold – X/VA +T
For X ≥ 2*A/3 - VAT/3 QRSnew = X/( 2*VA) - T
Timing in the circumferential direction can be calculated from the following formula
For the delay of lateral lead of T, Y is the displacement of the lateral lead along the Circumference and the Vc is the propagation velocity in the circumferential direction.
For Y≥ C/2 QRSnew = Y /( 2*VC) –2T
For Y≤ C/2 QRSnew = QRSold – Y /VC + 2T
If the timing is reversed so the lateral lead fires first followed by the apical lead the results will be different.
For (A - VAT) ≤ X ≥ VAT QRSnew = QRSold – X/(2*VA) –T/2
For X < VAT QRSnew = QRSold – X/VA
For X ≥ (A - VAT) QRSnew = X/(2*VA) = T/2
For Y≥ C/2 QRSnew = Y /( 2*VC) + T/2
For Y≤ C/2 QRSnew = QRSold – Y /(2*VC) +T/2
These equations demonstrate
More leads can shorten the QRS than fewer leads
Simultaneous stimulation of multiple leads will shorten the QRS more than sequential pacing.
For a bi-ventricular system, placing a lateral lead 2/3 of the distance from the apex and 180 degrees from the RV septal lead gives the shortest QRS duration for simultaneous pacing.
Lateral first versus apical first gives a wider QRS. A wider QRS duration is the cost for setting the left lead ahead of the RV lead. The lateral first setting favors a reduction in mitral regurgitation. A compromise must be made in these two parameters which are at odds.
2. The Problem
Over 3 billion choices to improve 14 disease states with 9 optimization goals (some of the optimization goals are diametrically opposed) to improve dyspnea, shortness of breath, fatigability, exercise intolerance, edema, swelling, fluid retention, and arrhythmias
3. Method of Optimization of Pacing Devices
Pre-Echo
Step 1 evaluate symptoms
Symptoms – (fatigue, exertional intolerance) determine if right heart or left heart is culprit
Symptoms – (Shortness of breath) Evaluate for AV dyssynchrony, mitral regurgitation, restriction of mitral inflow
Step 2 evaluate available data
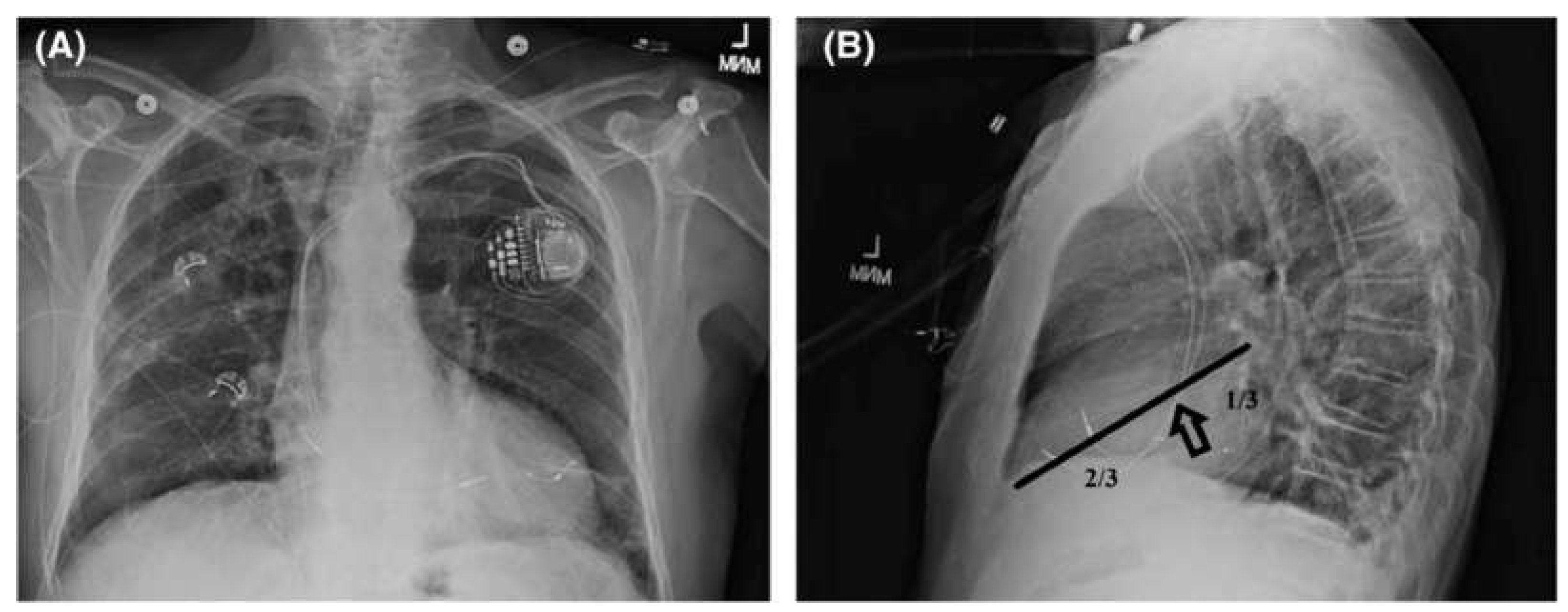
Pick pacing lead from chest X-ray and test for capture or diaphragmatic stimulation
ECG (rate, rhythm, PR interval, QRS duration, ectopy)
Echocardiogram (dyssynchrony, mitral valve inflow, mitral regurgitation, restrictive inflow, chamber dimensions, annular dilation, right heart function)
Chest X-Ray Posterior Anterior and Lateral (determine ideal lead positions)
Examine lateral chest X-ray determining which of the 4 lead positions are optimal (20 possible choices). To optimize longitudinal dyssynchrony choose the best lead configuration - 1/3 distance from the base or 2/3 distance from the apex.
Figure 1.
Step 3 Echo Examination
Step 3 a Pulse wave mitral valve inflow to choose
heart rate. This is not a trivial task as illustrated by editorial Heart Rate [
2].
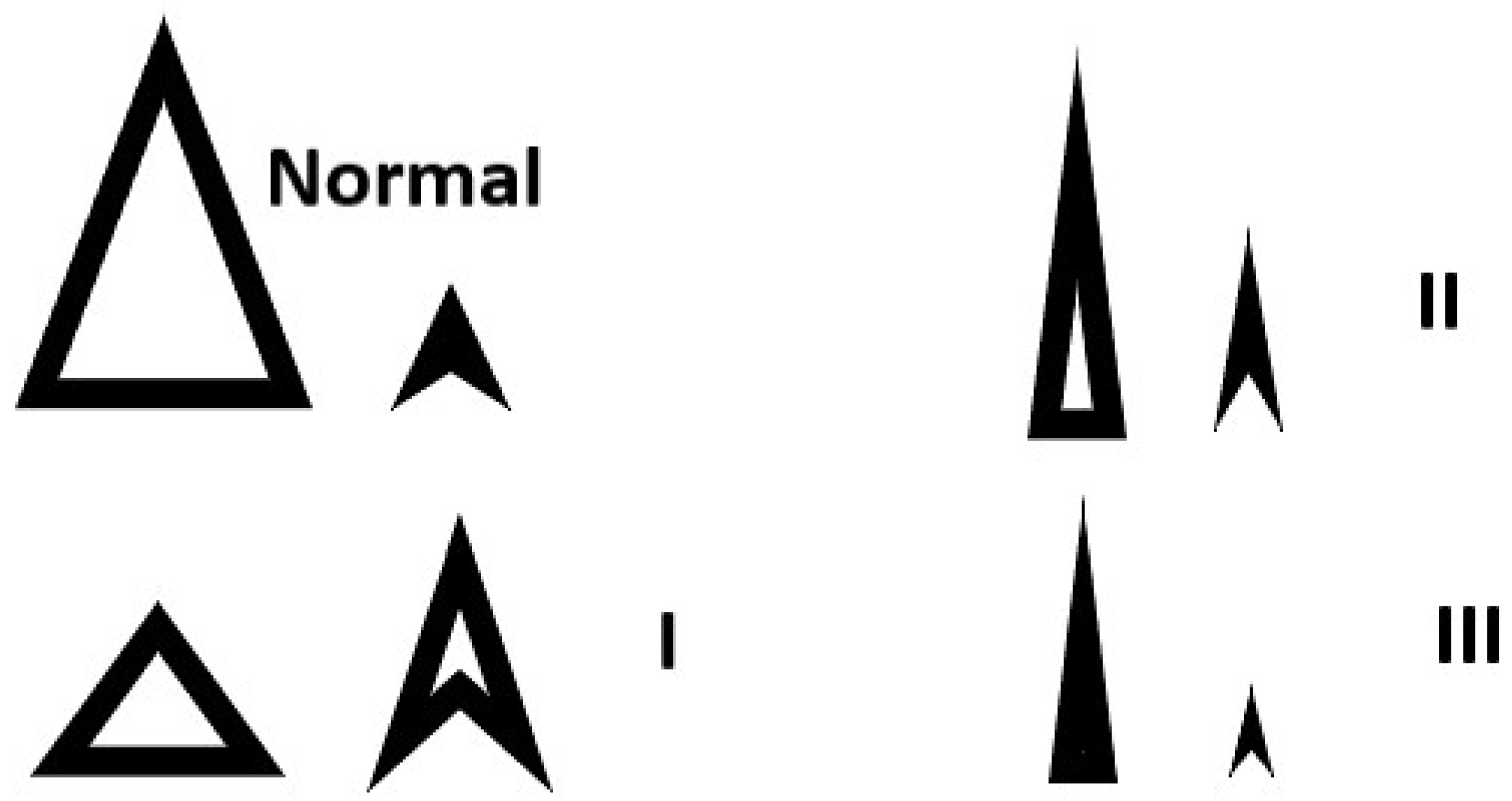
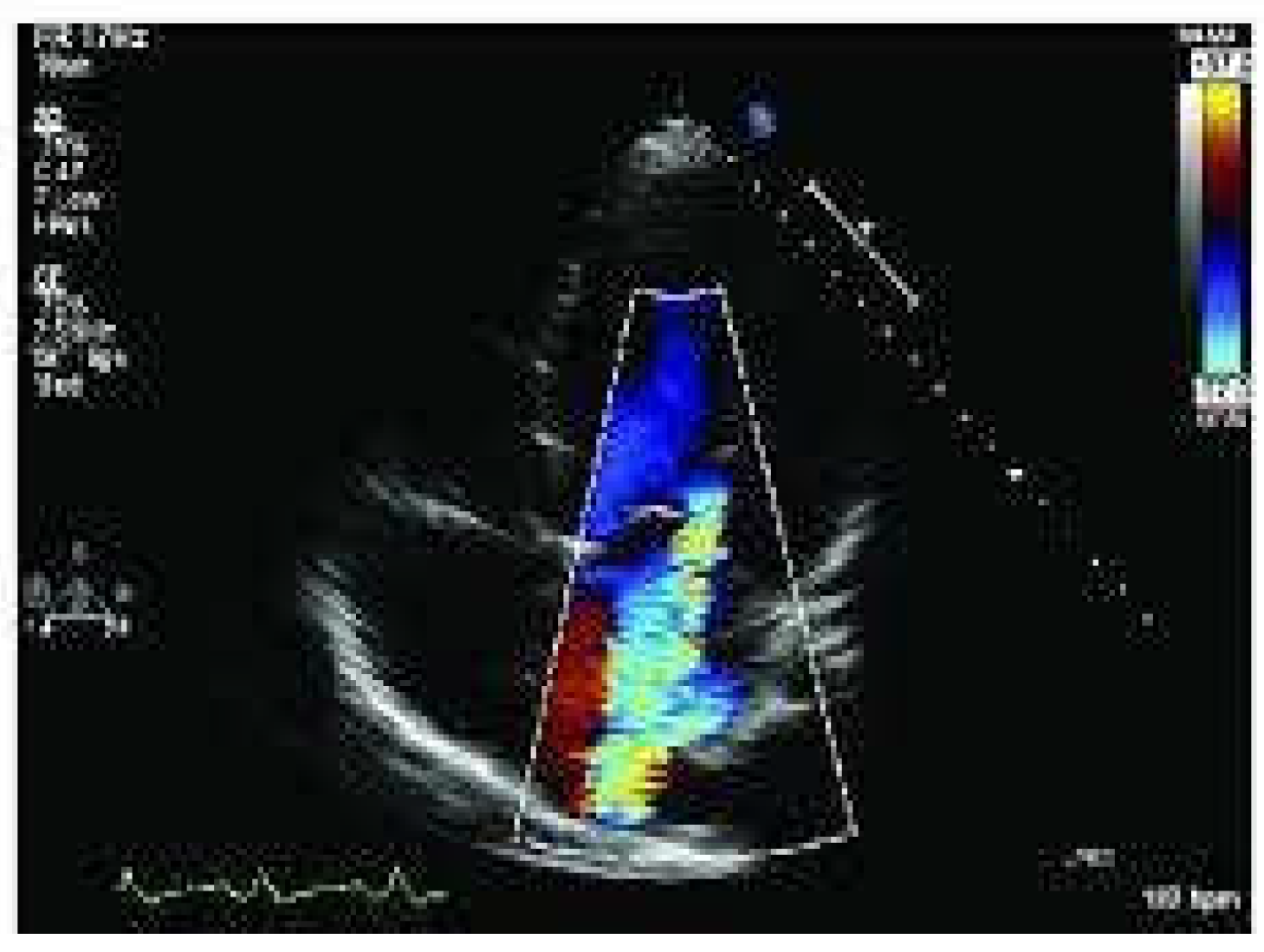
If inflow is restrictive grade 2 or 3 (
Figure 2) the ventricle is already full and needs to be emptied more frequently. Increase heart rate to 80 [
2].
For systolic dysfunction may choose base heart rate with the following formula
Heart rate (bpm) = 93 – 0.13 × deceleration time (msec) [
3]
All others with intact sinus node atrial sense
Figure 2.
Diastolic grades of mitral valve inflow II III have restricted filling.
Figure 2.
Diastolic grades of mitral valve inflow II III have restricted filling.
Step 3b Select AV interval from mitral valve inflow at new heart rate
Set pacing and sensed interval to allow separation of the E and A wave and do not truncate the A wave. Figure 3
Figure 3.
AV interval and mitral valve inflow Normal pattern is desirable.
Figure 3.
AV interval and mitral valve inflow Normal pattern is desirable.
Step 3 c Examine mitral regurgitation. If moderate or severe choose left lead first with longest lead time. The earliest depolarization allows for earlier relaxation and better coaptation of leaflets before systole begins.
Step 3 d Timing of the LV and RV goal is to decrease mitral regurgitation and increase LVOT integral. Evaluate LVOT integral adjust LV/RV timing to maximize LVOT integral and reduce mitral ERO. The RV LV timing delay is chosen by iteration of interval to optimize LVOT VTI. Figure 4
Figure 4.
LVOT Integral and Mitral regurgitation ERO.
Figure 4.
LVOT Integral and Mitral regurgitation ERO.
Step 4 walk patient and assess for symptom improvement. As the heart remodels to the new settings a repeat optimization may be required.
Specific Cardiac Pathology
Annular dilation and mitral regurgitation If step 3c above doses not reduce the ERO due to primary dilated annulus; the pacing heart rate should be increased to make the ventricle smaller. Return to step 3b and re-optimize AV interval for the new higher heart rate.
Left versus right heart failure and Optimizing right heart function in the setting of an LVAD If the right is failing turn off left lead and assure right ventricular pacing reassess for mitral regurgitation and LVOT integral
Annular dilation and tricuspid regurgitation Similar to mitral annular dilation increasing the heart rate to shrink the heart with a return to step 3b AV optimization to optimize for a higher heart rate.
Restrictive cardiac disease, Valvular disease restricting stroke volume, Peripheral vascular disease with fixed systemic vascular resistance restricting stroke volume Increase heart rate to compensate for reduced stroke volume. Returning to step 3b AV optimization is critical since these patients depend on atrioventricular transport.
Hypertrophic cardiomyopathy with obstruction Assure right ventricular pacing ablate the AV node in order to optimize AV transport
Wide QRS duration dilated cardiomyopathy Pacemaker activation of multiple sites can increase the axial and circumferential conduction velocities reducing the size of the heart. The greater the lead number and simultaneous pacing can accomplish this feat. Depending on the lead position circumferential dyssynchrony can be induced.
Optimize exercise parameters
Evaluate Ramp (sensitivity of piezoelectric crystal) increase if orthostatic or exertional intolerance.
Why has this protocol not been studied or recommended?
Designing a study to test 3 billion choices to improve 14 disease states with 9 optimization goals (some of the optimization goals are diametrically opposed) is impossible. Studies designed to prove the clinical benefit of bi-ventricular pacing allowed only minimal programing options as noted in the following
Table 2. The presented method requires knowledge of physiology and hemodynamics. Pacemaker companies have used algorithms to minimize programing; however one size does not fit all. An easy and common device algorithm is for the device to automatically minimize the QRS duration. If mitral regurgitation is present symptoms may worsen. If symptoms persist individualization is required and those algorithms should be turned off.
4. Conclusion
The goal is to increase LVOT integral, reduce mitral regurgitation, increase longitudinal conduction velocities and restore synchrony of the septum to the ventricle that needs it the most. The protocol will help select the most optimum pacing parameters out of the 3,875,040,000 choices. Caveat – As the heart remodels with the new pacing parameters repeat optimization may be required. Do not trust device algorithms in symptomatic patients.
Funding
This research received no external funding
Conflicts of Interest
The author declares no conflicts of interest.
References
- Callaghan J, Bigelow W. An electrical artificial pacemaker for standstill of the heart. Ann Surg 1951;1:8-17.
- Houck, PD. Houck PD. Heart Rate. Am J Cardiol. 2024 Apr 15;217:161-163. Epub 2024 Mar 8. PMID: 38460830. [CrossRef]
- Izumida, T. Izumida, T., Imamura, T., Nakamura, M., Fukuda, N., and Kinugawa, K. (2020) How to consider target heart rate in patients with systolic heart failure. ESC Heart Failure, 7: 3231– 3234. [CrossRef]
- van Bommel RJ, Gorcsan J, Chung ES, et al.. Effects of cardiac resynchronisation therapy in patients with heart failure having a narrow QRS complex enrolled in PROSPECT. Heart 2010;96:1107–13. [CrossRef]
- Ruschitzka F, Abraham WT, Singh JP, et al.. Cardiac-resynchronization therapy in heart failure with a narrow QRS complex. N Engl J Med 2013;369:1395–405. [CrossRef]
- Houck PD, Jones B, Patel R, et al. Pathophysiology of narrow complex dilated cardiomyopathy insight derived from the velocity equation: velocity = distance/time BMJ Case Reports CP 2019;12:e229339.
- Daubert, JC. Daubert JC. Modulation of cardiac contractility. A potential treatment of heart failure? Eur Heart J 2008;29:961–3. [CrossRef]
- Borggrefe MM, Lawo T, Butter C, et al.. Randomized, double blind study of non-excitatory, cardiac contractility modulation electrical impulses for symptomatic heart failure. Eur Heart J 2008;29:1019–28. [CrossRef]
- Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, Kocovic DZ, Packer M, Clavell AL, Hayes DL, Ellestad M, Trupp RJ, Underwood J, Pickering F, Truex C, McAtee P, Messenger J; MIRACLE Study Group. Multicenter InSync Randomized Clinical Evaluation. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002 Jun 13;346(24):1845-53. PMID: 12063368. [CrossRef]
- Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–1549. [CrossRef]
- Linde C, Abraham WT, Gold MR, St John Sutton M, Ghio S, Daubert C; REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction) Study Group. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J Am Coll Cardiol. 2008;52:1834–1843. [CrossRef]
- Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, Estes NA, Foster E, Greenberg H, Higgins SL, et al.; MADIT-CRT Trial Investigators. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361:1329–1338. [CrossRef]
- Brugada J, Delnoy PP, Brachmann J, Reynolds D, Padeletti L, Noelker G, Kantipudi C, Rubin Lopez JM, Dichtl W, Borri-Brunetto A, et al.; RESPOND CRT Investigators. Contractility sensor-guided optimization of cardiac resynchronization therapy: results from the RESPOND-CRT trial. Eur Heart J. 2017;38:730–738. [CrossRef]
- Gold MR, Ellenbogen KA, Leclercq C, Lowy J, Rials SJ, Shoda M, Tomassoni G, Issa Z, Sarrazin JF, Jennings JM, Nair DG. Effects of atrioventricular optimization on left ventricular reverse remodeling with cardiac resynchronization therapy: results of the SMART-CRT trial. Circulation: Arrhythmia and Electrophysiology. 2023 Jun;16(6):e011714.
- Brown CD, Burns KV, Harbin MM, Espinosa EA, Olson MD, Bank AJ. Cardiac resynchronization therapy optimization in nonresponders and incomplete responders using electrical dyssynchrony mapping. Heart Rhythm. 2022 Dec;19(12):1965-1973. Epub 2022 Aug 5. PMID: 35940458. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).