Introduction
Cervical cancer ranks the fourth commonly occurring female malignancy worldwide following breast, colorectal and lung cancers [
1], with more than 570,000 new cases and about 311,000 deaths for the year 2018 [
2]. Highest burden of more than 80% of the cases and deaths is carried by low and middle income countries [
3]. The estimated age- standardized rate of cervical cancer deaths is very high in East Africa compared to other regions in the World [
1,
4]. Cervical cancer is the leading female malignancy in Tanzania with 9772 new cases and 6695 deaths yearly [
4]. Among women with cervical cancer 89.4% are diagnosed with late stage [
5].
Worldwide, cervical cancer rate is 13.1 per 100,000 women [
2]. In developed countries the rate is 4.2 per 100,000 women, South- Eastern Asia 17.2 per 100,000 women, Southern Central Asia 12.2 per 100,000 women, Northern America 6.4 per 100,000 women, Eastern Europe 16 per 100,000 women [
2] In Sub Saharan Africa the rate varies from 8% to 75 %. Western Africa 29.6 per 100,000 women, Southern Africa 43.1 per 100,000 women [
6]. Eswatini was the first country in the World with the highest incidence rate of cervical cancer of 75.3 per 100,000 women [
2,
7] followed by Malawi 72.9 per 100,000 women, Zambia 66.4 per 100,000 women, Zimbabwe 62.3 per 100,000 women [
1]. Tanzania is the fourth country in the world with the highest incidence rate of cervical cancer of 59.1 per 100,000 women [
8,
9,
10]. Distribution of cervical cancer within the country varies from one zone to another. Lake zone appears to have higher rates of cervical cancer followed by southern highlands compared to other zones in the country [
11]
Persistent infection by high- risk oncogenic Human Papilloma virus (HPV), has been firmly established to cause cervical cancer pre malignant and malignant lesions, as well as malignancy of the vulva, vagina, anus, penis and oropharynx. HPV types 16 and 18, cause more than 90% of cervical cancers worldwide [
12,
13]. Cervical cancer in early stage is frequently asymptomatic, and can only be detected by screening methods like Visual Inspection with Acetic acid (VIA) and Cytology based technology Papanicolao Smear [
14]. For symptomatic patients, most common presentations are post coital bleeding, irregular or heavy menses and abnormal vaginal discharge that may be watery or purulent and malodorous [
15]. Cervical cancer can be prevented by using available vaccine and cured if diagnosed early [
13].
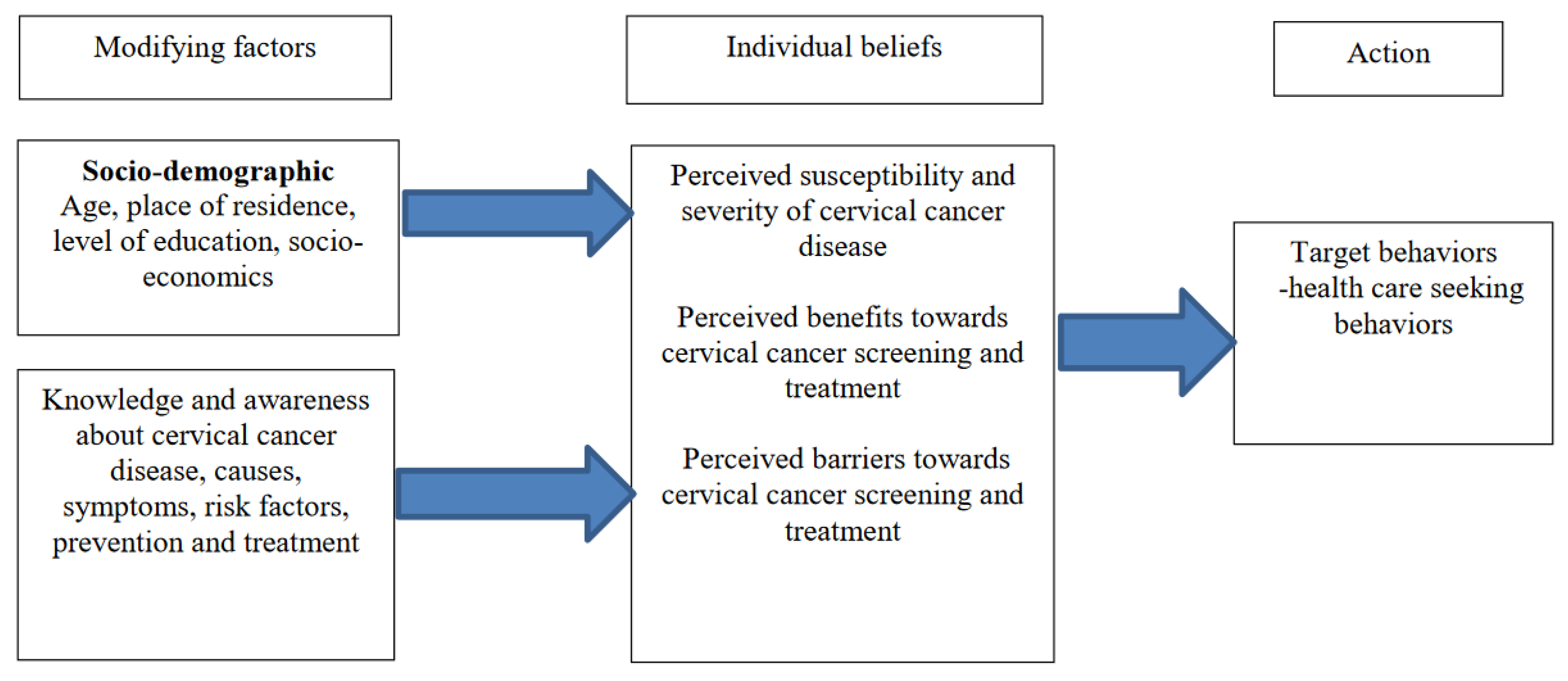
Late stage presentation in seeking care can occur at different levels from individual level, community level and health system level. Knowledge, perceptions and practices have been shown to have an impact on health outcome. Health Belief Model (HBM) has been used in many studies to explain the health behavior. Multiple factors interplay in for cancer patients to present at an advanced stage. This study was mounted on the limited qualitative studies on knowledge, perceptions and behaviors of women with late stage cervical cancer diagnosis in Tanzania. The Health Belief Model was used as a theoretical framework to explore the knowledge, perception and behaviors of women with cervical cancer to gain a detailed understanding and depths.
Previous studies which have been done in Tanzania revealed that more than 70% of women with cervical cancer had late stage of the disease during diagnosis [
5,
16]. It is quite undisputed that, progressive efforts have been in place in Tanzania to ensure cervical cancer is diagnosed early. These include advocacy of “screen and treat with VIA and Cryotherapy” implementation in 2012 [
17,
18]. Despite the facts that, cervical cancer can be prevented and detected while in early stages, most women in Tanzania and Sub Saharan Africa are diagnosed in late advanced stage whereby cure is not available [
5,
6,
19]. This study is mounted to explore the experiences of cervical cancer in women attending Bugando Medical Centre
Theoretical Framework
Figure 1 below shows the conceptualization of Health Belief Model (HBM) which was developed in 1950, then modified in 1968 by Rosenstock and has been used worldwide as a behavioural change framework. The Health Belief Model is incorporated into strategies in order to increase knowledge of health challenges, enhance perceptions and encourage actions to reduce the risk or burden and in its later iteration to build a sense of self efficacy to undertake the needed change. While it focuses on the individual, the model recognizes the addresses the social/community context in which health behaviors take place. The theory includes 4 entities, perceived susceptibility, perceived severity, perceived benefits and barriers and perceived cues of action. The Health Belief Model attempts to explain the widespread failure of people to participate in programs to prevent or to detect asymptomatic disease, people’s responses to experienced symptoms and their behavior in response to professionally diagnosed illness and compliance with medical regimes [
20]. The Heath Belief Model constructs has been used for data collection and analysis.
Methods
Study Design
This study was hospital based explorative qualitative study conducted from November to December 2021, involving 11 participants who were diagnosed to have cervical cancer stage IIB and above. The aim was to explore knowledge, perceptions and behaviors among women with late stage cervical cancer to understand the depths and subjective reality. Qualitative studies provide meaningful insights and views of the participants when conducted by using theoretical models and can help to intervene and reduce cervical cancer burden [
21]
.
Study Duration
The study was conducted in a period of 1(one) month, from November 2021 to December 2021.
Study Setting
This study was conducted at Bugando Medical Centre (BMC) located in Mwanza, Tanzania, along the shores of Lake Victoria. Mwanza, with an estimated population of 1,182,000 (as of 2022), is the second-largest city in Tanzania and serves as a major medical and referral hub for the Lake Zone regions. BMC is a public, specialized, tertiary, and teaching hospital affiliated with the Catholic University of Health and Allied Sciences (CUHAS). It has a bed capacity of approximately 1,000, providing a wide range of medical services, including specialized oncology care.
BMC is one of the few comprehensive cancer centres in Tanzania, catering to patients from all over the Lake Zone, which includes regions such as Mwanza, Shinyanga, Simiyu, Mara, Kagera, and Geita. Women requiring radiotherapy, chemotherapy, and palliative care for cervical cancer are referred to BMC from these regions and beyond. On average, BMC handles about 100-120 cancer patients daily, with cervical cancer being the most common malignancy treated.
The hospital records indicate that approximately 3-7 new cases of cervical cancer are diagnosed daily, translating to 15-25 new cases per week. In 2020, BMC registered around 1,500 new cervical cancer cases. The study location was selected because BMC is one of the designated centers for comprehensive cancer treatment in the Lake Zone, making it a crucial site for studying cervical cancer care in Tanzania.
At BMC, there are two oncology clinics: one dedicated to public patients and another for private and insured patients. These clinics are situated close to each other and operate from Monday to Friday, staffed by dedicated teams of oncologists, nurses, and support personnel. The choice of BMC as the study setting was driven by its role as a key institution in the national cancer care network and its capacity to handle a large volume of cervical cancer cases.
Study Population
The study population included all women with cervical cancer who received care at Bugando Medical Centre from November to December 2021.
Study Sample
All women with cervical cancer stage IIB and above, diagnosed within 3 months and had not yet received chemo radiation
Inclusion Criteria and Exclusion Criteria
Participants with confirmed histopathological diagnosis of cervical cancer and FIGO clinical stage IIB and above, diagnosed within three months and not yet received treatment who were willing to participate in the study. Patients who were unconscious, very sick, unable to communicate well, and those with severe psychiatric co-morbidities example schizophrenia and severe dementia, or unable to understand informed consent were not included in the study.
Sample Size
The sample size of 11 participants was used. Analytical saturation of data was reached on participant 8, but three more participants were recruited to confirm saturation. Data Saturation was considered when there were no newer themes generated.
Sampling Procedure
Sampling technique was purposive sampling. Women with late stage cervical cancer diagnosed within 3 months who attended clinic but not started chemo-radiation were approached by the principal researcher to participate in the study.
Recruitment of Participants
Participants were recruited at the clinic. The principal researcher stayed at the attending rooms with other clinicians to capture the women. Referral notes and histology result were reviewed to confirm the diagnosis and clinical staging. The participants were left to see the attending clinician first, then followed on their way out. Introduction was done, Participants were told the purpose of the study, benefits and right to withdrawal from the study. Those who consented and agreed to participate in the study were enrolled. Among the approached women, three declined to participate for unclear reasons. Nine participants were recruited from public clinic and two participants recruited from private clinic as there was few number of cervical cancer patients in the private clinic about 0-2 patients per day compared to public clinic with about 2-7 patients per day. Research team recruited participants from rural and urban areas, reproductive and post-menopausal, those with formal and informal education. There was intention to get participants with higher education level, but we didn’t get one during the study period. This was done in order to get variability of participants and to enrich data.
Data Collection
The study used a semi structured and open ended interview guide which was developed by research team after literature search. The interview guide had two sections. First section was basic participant information which included age, residence, level of education, marital status, occupation, Last normal menstrual period, parity, Living children, Date of diagnosis and clinical staging. The second section consisted of knowledge, perceptions, and health care seeking behaviors. It was prepared in English and translated to Kiswahili to ease communication with respondents. The interview guide was first piloted among 3 women with cervical cancer at Bugando medical Center. The responses from the pilot were used to modify the guide. Data gathered from pilot, were not included in the analysis.
Interview was conducted in a calm quiet private room within the hospital compounds to get a detailed information of participant own perceptions and accounts in a more relaxed atmosphere and talking openly. The Researcher defined key concepts of the study so as participant was aware of the study and was told to express freely their ideas. Women who were willing to participate signed the informed consents. Tape recorders were used after obtaining permission to do so. The interview involved one participant at a time per day, lasting approximately 30 minutes to 60 minutes. Experienced researcher led the first two interview sessions, other interviews were carried by the principal researcher and a research assistant. Field notes were taken by the trained research assistant on the important issues and events that occurred during the interview. Soon after completion of interview, researcher conducted checks with the participants to verify their information. All participants confirmed their information. A brief meeting was conducted by the research team to discuss issues that occurred during the data collection.
Data Management and Analysis
Data analysis was done manually. A code book was created first, by the research team. Transcription of the audios was done in Swahili verbatim by the principal researcher. Five transcripts which were rich in data were read and re read by three researchers, developed codes independently for each of the transcript, then discussed the codes and agreed on the proper codes to be used. Whenever there were differences in coding, discussion was made, and consensus was reached. The analysis was a deductive process. Translation was done during the coding process during subthemes and themes generation. Six phases of thematic analysis was used which are familiarization with the data , generating initial codes, generating themes, reviewing initial themes, defining and naming themes, Producing the report [
22]
Themes were searched from the general list of code book. Some codes formed main themes or sub-themes, whereas other codes were discarded. Later themes were re-read and reviewed at the level of coded data and theme itself to ensure that all of the data forms a coherent pattern and the relationship between themes to reflect the meaning of data. Themes were then defined and named and later final analysis and report writing was produced.
Trustworthiness
Trustworthiness was applied by using competing paradigm developed by Guba and Lincoln in which four components are used, credibility, transferability, dependability and confirmability [
23]
Credibility: The principal researcher conducted the interviews, transcription and analysis of the data which led to prolonged engagement of the principal researcher with the participants and the data. Member checking was done soon after the interviews to confirm with the participant the information they gave on important issues, in which all participants agreed with the checking. The transcripts were looked by other researcher to verify interpretation of data and coding was in a team.
Transferability the findings applied in the similar context of the phenomenon.
Ethical Considerations
Ethical approval from the CUHAS-BUGANDO Research ethics and Publications Committee (CREC) was obtained for the study. Permission to do research was sought from Bugando Medical Centre The purpose of the study and the right to withdraw from the interview was explained to the participants of the study. Before data collection a written informed consent was sought from the participants. Permission to audio tape the In-depth interview was sought before the start of interviews.
To foster privacy and confidentiality, all interviews were anonymous and kept confidential. Identity of the respondents and study subjects was not disclosed anywhere during data collection and report writing. Only numbers were assigned to participants. Information recorded was not shared to any third party except for research purpose only and without exposing the identity of the respondents. Three participants were emotionally and psychologically affected (crying) during data collection, interviews were stopped and recordings were paused, to provide emotional support and counselling and continued when the participant was okay to do so. The participants were later on linked to psychologists for further management.
Results
Participant Characteristics
Participants had median age of 47 years. (Range 27 -62). Five were pre-menopausal and six were post-menopausal. Five of the participants were from urban areas and six were from rural areas. Nine had primary school education, two had ordinary level secondary education. Ten were unemployed and one was employed as office assistant.
Table 1 below summarizes the themes and subthemes emerged
Lack of Knowledge on Cervical Cancer Disease
Participants said that they never heard about cervical cancer disease, hence could not tell anything on the. causes, preventive measures and treatment options.
“Honestly, I don’t know about it I have never heard of that disease anywhere before, and I am really surprised to find here there are many women with this disease” (participant 05, 42 years, rural)
Myths and Misconception about Cervical Cancer Disease And Symptoms
Poor knowledge about cervical cancer disease symptoms and causes resulted to myths and misconception. Several participants believed witchcraft was the cause of cervical cancer symptoms as a result of family/ social conflicts.
“I am a second wife to my husband, when the symptoms started, I knew it was not normal, the first wife must have witched me, and she doesn’t like me at all. She has tried several times to harm me... She killed one of my son, now she has decided to witch me with this disease” (participant 08, 46, rural)
Inaccurate Perceived Threat of Cervical Cancer Symptoms
Poor Perceived Susceptibility and Severity
Poor knowledge about cervical cancer disease made it difficult to recognize the danger and threat imposed by the symptoms. Participants did not perceive a threat towards the symptoms and they misinterpreted the symptoms to common illness like UTI, fungus and it was not serious.
“I never thought of getting a bad disease like this one because at first the symptoms were on and off and not severe. I thought it was UTI and it will go away. I was very okay continuing with my activities until when it started getting worse” (participant 07, 27 years, rural)
Poor Perceived Benefits of Screening
Participants had not been screened for cervical cancer before. Most of the participants never heard about cervical cancer screening. Others heard about cervical cancer screening, but did not screen as they did not see the importance of screening because they were okay.
“When I went to take my medications for HIV, health care provider told me to go for screening done by people from Dar es Salaam, but I didn’t go for that screening as I was not sick at that time. I didn’t see the need to do so” (participant 01, 46 yrs., rural)
Socially Imposed Stigma
Symptoms of cervical cancer have brought different emotions and changes in the participants’ life, participants had offensive per vagina watery discharge and/ or abnormal per vaginal bleeding which had impacts on their daily life. The symptoms led to poor interaction with spouse, family and community.
“One day I went to plait my hair and I forgot to put sanitary cloths to prevent that offensive discharge from wetting my clothes. While I was sitting, that water came, offensive smell started to be obvious, flies came to me, and people started covering their noses and one by one walked away from me. I was so embarrassed that day, and from that day, I never went out to interact with other people… (Crying)” (participant 04, aged 47years rural)
Perceived Barriers Towards Health Care Seeking Behaviors
Lack of external and internal cues with limited interpersonal and public communication about cervical disease and symptoms
Participants emphasized the need for health education about cervical cancer and they wished someone could have told them about how bad the disease was, and the symptoms of the disease. Several participants thought there could be women in their communities with the disease, but due to the nature of the disease, they find it very difficult to open up.
“I wished I knew someone who had similar disease to tell me what she went through and how bad this disease is, but the symptoms are very embarrassing to discuss with someone. It is not easy to talk about private parts with everyone, maybe there are women with this disease in my village, but they cannot talk about it, they keep it a secret” (Participant 09,54yrs, rural)
Financial Challenges
Participants had financial problems that caused them not to seek health care services as expected.
“I wanted to go to hospital to check what was wrong with me, but we didn’t have the money, we live in the village and doing farming only, we don’t get much. I told my relatives that I needed a help from them. They started contributing but it took too long to get enough money” (participant 10, 36 years, rural)
Preference to Traditional Healers
Some participants preferred traditional healers as they believed in witchcraft but also easily accessible and not expensive
“My mother and other relatives advised me to go the best traditional healer in the village, and this man usually don’t take money until you are cured, he lives very close to our home. I went to him, he checked me and said my problem was not big. He gave me some herbs to drink, and others to insert in my underparts” (participant 06 rural)
Limited Access to Health Facilities
Majority of participants from rural areas, stated that health facilities were far from their home with limited transport services. They only go to health facilities when condition is very bad
“It takes about 5 hours, and fare of 5000 to 10,000 to reach to a small hospital, it is very far, we don’t have any facility nearby, there is small shop selling medicines nearby, we normally go there to get medicines”
Inappropriate Services Care at the Lower Health Facilities
Participants stated that they went to nearby facilities multiple times and there was misdiagnosis of the symptoms. Women mentioned Investigations like ultrasound, urinalysis and blood investigations, and were told to have fungus or dirt in the womb and were given medications without improvement
“I had unstopped bleeding and the doctors said the ultrasound showed there were some dirties in my womb though they tested for pregnancy and it was negative. They said I should be evacuated; I was evacuated three times at different facilities. I lost a lot of blood and I lost consciousness too… (Silence). I could have died” (participant 03, 35 years, urban)
Discussion
This study aimed to explore knowledge about cervical cancer disease and their perceived susceptibility and severity of the symptoms and disease and the health care seeking behaviors which had impact on late stage detection of the disease.
Findings from this study suggests that cervical cancer has not been well mentioned and very unfamiliar to these women before the diagnosis but even after the diagnosis, the details of the disease was lacking. Perceiving the symptoms to commonly occurring conditions known to them and considering them as not a threat to their health, misinterpretation of symptoms, limited interpersonal and public communication about cervical cancer disease, financial challenges reflect the behaviors which made these women not able to seek health care services. Inappropriate services at the primary health facilities could have attributed by lack of knowledge about cervical cancer disease and management by the primary health care providers.
In this study, Knowledge of cervical cancer is lacking in all participants. Understanding of cervical cancer symptoms, causes, risk factors, prevention and treatment options can have positive impact on the behaviors and can help these women to seek necessary services. Poor knowledge on cervical cancer causes, risk factors, prevention and treatment options has been found in other studies done in South Africa by Harries J
et al [
24],Nigeria by Ndikom C
et al [
25], in Ghana by Binka C
et al [
26] and in Uganda by Mwaka AD
et al [
27]. Tanzania [
28,
29,
30].
Results from this study suggest perceptions that had low impact on the individual level but also at the community level. The participants did not perceive themselves at risk of getting the disease, and when the symptoms started they did think it could serious or a threat to their health. The symptoms were compared to common diseases which are known to them which might have been caused by poor knowledge about the disease and the complications thus making decision to seek health care not of urgency, leading to disease advancing and poor treatment outcome. The community seemed to lack support or involvement in these women probably due to low knowledge of the disease leading to stigma and embarrassment towards these women. Similar findings were found in other studies. [
16,
21,
31,
32,
33].
Participants went to seek health care services when the symptoms worsened. Health seeking practices was influenced by poor knowledge of the disease, lack of individual decision making, financial challenges, stigma from the community, limited access to health facilities showed to impact health seeking behaviors. These findings are similar from previous studies [
16,
21,
31,
32,
33],which found poor health care seeking behaviors
The findings showed majority of the participants attended lower facility levels for health services in which they had multiple consultations, inadequate assessment and management. This could have been contributed to inadequate knowledge about cervical cancer disease and its management among primary health care providers. The findings are similar from other studies done in Nepal, Bangladesh, South Africa, Eswatini, Zimbabwe, Malawi, Ghana, Rwanda, and Uganda.
Conclusions
Cervical cancer is preventable and can be cured if detected in early stages. Knowledge and awareness about cervical cancer symptoms, causes, and risk factors, preventive measures like screening and treatment options and complications of the disease should be clearly and well explained to the community and health care providers through health education promotion and awareness. Controlling cervical cancer needs an active involvement of health care providers, leaders in different aspects, the community, policy makers and different stake holders.
Recommendations
Health education should be provided through mass media and meetings to promote screening for early detection and primary prevention. Secondly, Outreach activities and to educate primary health providers about cervical cancer disease, the proper management and early referral. Lastly, advocacy of cervical cancer victims to their respective communities
Limitations of the Study
The study included limited number of participants to explore the participant’s own detailed perceptions and in depths of, the finding cannot be used for generalization. Only one group of participants was involved and the study didn’t involve family members.
Conflicts of Interest
Author’s declare there is no conflict of interest.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2018;68(6):394–424. [CrossRef]
- Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. The Lancet Global Health. 2020;8(2):e191–203. [CrossRef]
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2015;65(2):87–108. [CrossRef]
- Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. Human Papillomavirus and Related Diseases in the World- Summary report. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). 2019;(June):307.
- T Kabalimu GKM, Muindi R. Social and Cultural factors affecting treatment seeking behaviour of Patients with Cancer of Cervix at Ocean Road Cancer Institute in Dar es Salaam, Tanzania. Huria Journal. 2018;25(2):54–63.
- Jedy-Agba E, Joko WY, Liu B, Buziba NG, Borok M, Korir A, et al. Trends in cervical cancer incidence in sub-Saharan Africa. British Journal of Cancer. 2020;123(1):148–54. [CrossRef]
- GLOBOCAN. Cervix uteri Source: Globocan 2020. international Agent for Research on Cervic Uteri. 2020;419:1–10.
- The United Republic of Tanzania Ministry of Health and Social Welfare. National Cancer Control Strategy (NCCS) 2013 - 2022. 2013. 2013;72.
- WHO. WHO Cancer Report 2020 Global Profile. 2020. 2020;(2019):2019–20.
- Republic U. United Republic of Tanzania. Population policy compendium. 1980;1–6.
- Gesink MP, Chamberlain RM, Mwaiselage J, Kahesa C, Jackson K, Mueller W, et al. Quantifying the under-estimation of cervical Cancer in remote regions of Tanzania. BMC Cancer. 2020;20(1):1–8. [CrossRef]
- Castellsagué X. Natural history and epidemiology of HPV infection and cervical cancer. Gynecologic Oncology. 2008;110(3 SUPPL.2):4–7. [CrossRef]
- Strategy G, Accelerate TO, Elimination THE, Cervical OF, As C, Health AP. Global strategy to accelerate the elimination of cervical cancer as a public health problem.
- Test T, Follow-up T. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention.
- Ali F, Kuelker R, Wassie B. Understanding cervical cancer in the context of developing countries. 2012;5(1). [CrossRef]
- Mlange R, Matovelo D, Rambau P, Kidenya B. Patient and disease characteristics associated with late tumour stage at presentation of cervical cancer in northwestern Tanzania. BMC Women’s Health. 2016;16(1):1–6. [CrossRef]
- Welfare S. National Cervical Cancer Prevention and Control Strategic Plan. 2015;
- Moran T. Prevention of cervical cancer through screening using visual inspection with acetic acid ( VIA ) and treatment with cryotherapy.
- Dunyo P, Effah K, Udofia EA. Estimates in delays in ccervical cancer diagnosis Nepal. 2018;1–10.
- Karen Glanz, Barbara K. Rimer KV. Health Behavior adn Health Education. Jossey Bass. 2008. 465–485 p.
- Mwaka AD, Okello ES, Wabinga H, Walter FM. Symptomatic presentation with cervical cancer in Uganda: A qualitative study assessing the pathways to diagnosis in a low-income country. BMC Women’s Health. 2015;15(1):1–13. [CrossRef]
- Clarke V, Braun V. Using thematic analysis in counselling and psychotherapy research: A critical reflection. Counselling and Psychotherapy Research. 2018;18(2):107–10. [CrossRef]
- 10-guba_lincoln_94.pdf.
- Harries J, Scott SE, Walter FM, Mwaka AD, Moodley J. Women’s appraisal, interpretation and help-seeking for possible symptoms of breast and cervical cancer in South Africa: a qualitative study. BMC women’s health. 2020;20(1):251. [CrossRef]
- Ndikom CM, Ofi BA. Awareness , perception and factors affecting utilization of cervical cancer screening services among women in Ibadan , Nigeria : a qualitative study. 2012;1–8. [CrossRef]
- Binka C, Doku DT, Awusabo-asare K. Experiences of cervical cancer patients in rural Ghana : An exploratory study. 2017;1–12. [CrossRef]
- Mwaka AD, Okello ES, Kiguli J, Rutebemberwa E. Understanding cervical cancer : an exploration of lay perceptions , beliefs and knowledge about cervical cancer among the Acholi in northern Uganda. 2014;1–9. [CrossRef]
- Mabelele MM, Materu J, Ng FD, Mahande MJ. Knowledge towards cervical cancer prevention and screening practices among women who attended reproductive and child health clinic at Magu district hospital , Lake Zone Tanzania : a cross-sectional study. 2018;1–8. [CrossRef]
- Mburu A, Itsura P, Mabeya H, Kaaria A, Brown DR. Knowledge of Cervical Cancer and Acceptability of Prevention Strategies Among Human Papillomavirus-Vaccinated and Human Papillomavirus-Unvaccinated Adolescent Women in Eldoret , Kenya. 2019;8:139–45. [CrossRef]
- Moshi F V., Vandervort EB, Kibusi SM. Cervical Cancer Awareness among Women in Tanzania: An Analysis of Data from the 2011-12 Tanzania HIV and Malaria Indicators Survey. International Journal of Chronic Diseases. 2018;2018:1–7. [CrossRef]
- Birhanu Z, Abdissa A, Belachew T, Deribew A, Segni H, Tsu V, et al. Health seeking behavior for cervical cancer in Ethiopia : a qualitative study. 2012;1–8. [CrossRef]
- Williams P, Murchie P, Bond C. Patient and primary care delays in the diagnostic pathway of gynaecological cancers : 2019;(February):106–11.
- Scott SE, Walter FM, Webster A, Sutton S, Emery J. The model of pathways to treatment: Conceptualization and integration with existing theory. British Journal of Health Psychology. 2013;18(1):45–65. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).