1. Introduction
Despite research advances, cancer treatment remains challenging, and cancer incidence and mortality rates continue to increase worldwide [
1]. The complexity of cancer treatment is compounded by several factors, including the presence of metastasis, drug resistance, and treatment discontinuation due to adverse drug events [
2]. Photodynamic therapy (PDT) has been developed to address these complex factors that make cancer treatment difficult. PDT is a highly tumor tissue-specific therapeutic modality that targets cancer cells with internalized photosensitizers [
3]. The lack of adverse events associated with the photosensitizers utilized makes PDT an exceptionally noninvasive modality, as it is unlikely to affect normal tissues [
3]. Photosensitizers, such as sodium talaporfin or sodium porphyrin, excite the surrounding oxygen from its ground state to the singlet state when irradiated with a laser at the sensitizer’s specific excitation wavelength [
4]. This oxidant targets lipid membranes and induces ferroptosis in cancer cells as a result of the depletion of reduced glutathione, a substrate of glutathione peroxidase that reduces lipid peroxides in biological membranes to alcohol [
5,
6,
7]. Damage-associated molecular patterns, such as high-mobility group box 1 and adenosine triphosphate, are released from cell membranes disrupted by ferroptosis and are then recognized by the Toll-like receptor family of dendritic cells. The cells subsequently elicit antigen-presenting responses through dendritic cell activation, leading to the activation of cytotoxic T cells [
8,
9]. It is therefore anticipated that the induction of ferroptosis by PDT will have an antitumor effect not only on light-irradiated tumor tissue, but also on cancers that have metastasized throughout the body and that this effect will be enhanced in combination with immune checkpoints [
10].
Cytotoxic chemotherapeutic agents, including alkylating agents, platinum drugs, microtubule inhibitors, antimetabolite drugs, and topoisomerase inhibitors, function by impeding cell division and are thus not efficacious against slow-growing cancers such as cancer stem cells [
11,
12,
13]. The efficacy of molecularly targeted drug therapy also depends on the expression of the target enzymes. The enzymes targeted by existing molecularly targeted drugs are not consistently expressed in cancer cells. Meanwhile, PDT has the potential to be an effective treatment for drug-resistant cancer cells because it can disrupt cancer cells with singlet oxygen [
4,
5], which in turn induces immunogenic cell death (H-I). In addition, photosensitizers that absorb near-infrared (NIR) light are expected to be effective against cancer cells that are resistant to reactive oxygen species owing to the combined effect of photothermal therapy (PTT) via thermal radiation and the generation of singlet oxygen via photoexcitation [
14]. Accordingly, we focused on heptamethine cyanine (HMC) dyes that serve as photosensitizers when excited by NIR light for PDT because longer-wavelength light has the advantage of a relatively high tissue penetration [
15].
We previously used indocyanine green (ICG) as the HMC for PDT [
16], but IR-783 as the HMC has also been shown to have specific cytotoxic activity against breast cancer cells without being influenced by light [
17,
18]. Low-molecular-weight compounds, such as HMC, facilitate accumulation in solid cancerous tissue when encapsulated in liposomes or micelles [
14,
19]. This phenomenon, designated as the enhanced permeability and retention (EPR) effect, is characterized by the tendency of macromolecules to leak out of blood vessels and into the tumor stroma owing to the markedly higher vascular permeability of tumor tissue than that of normal tissue [
20,
21,
22].
Despite evidence indicating the clinical efficacy and safety of PDT with IR-783, the precise mechanism by which IR-783 exerts its antiproliferative effects remains to be elucidated. Therefore, this study aimed to determine the efficacy of PDT using IR-783 liposomes in the clinical setting and to investigate the cytotoxicity of liposomized HMC in an environment devoid of laser irradiation.
2. Materials and Methods
2.1. Ethics
This study was approved by the Ethics Review Committee of the IGT Clinic on February 24, 2023 (approval number: 30) and was conducted in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical Research Involving Human Subjects established by the Japanese Ministry of Health, Labor, and Welfare. Informed consent was obtained from all patients prior to the clinical trial.
2.2. Study Design and Patients
This x study reported the PDT outcomes in two patients with breast and with tongue cancer. Patients with porphyria and with a history of photosensitivity to previous PDT with photosensitizers such as sodium talaporfin or 5-aminolevulinic acid were not eligible. The study endpoint was the patient ability to receive PDT without photosensitivity reactions or compromising their quality of life.
2.3. Preparation of Heptamethine Cyanine Liposomes
ICG and IR-783, as photosensitizers that reacted with the NIR light used in PDT, were used as HMC dyes. We purchased 1,2-Dimyristoyl-sn-glycero-3-phosphocholine (DMPC) from Yu-ka-Sangyo Co., Ltd. (Tokyo, Japan) and IR-783 from Tokyo Chemical Industry Co., Ltd. (Tokyo, Japan). Diagnogreen (ICG) was purchased from Daiichi Sankyo Co., Ltd. (Tokyo, Japan). Liposomes were prepared as previously reported [
16]. Briefly, DMPC was dissolved in a 5% glucose solution at a concentration of 8.85 mM using a Bransonic
® CPX8800H-J Ultrasonic Cleaner (Branson Ultrasonic Co., Ltd., Danbury, CT, USA) and then sonicated at 40 kHz for 60 min under 45 °C. Subsequently, the liposomes were purified using sterile filtration through a 0.20-μm pore size filter (Sartorius, Goettingen, Germany). The particle size of the liposomes was determined using ELSZ-2000 (Otsuka Electronics Co., Ltd., Osaka, Japan). HMC liposomes were prepared by mixing 5 mg IR-783 or ICG with 8.85 mM/10 ml liposomes using a stirrer until the reagent was completely dissolved, followed by sterile filtration through a 0.20-μm filter. HMC liposomalization was determined through gel filtration chromatography using a PD-10 Sephadex G-25 gel filtration column (Cytiva, MA, USA).
2.4. Cell Culture
The human lung adenocarcinoma cell line HCC827 was purchased from the American Type Culture Collection (Manassas, VA, USA). Cells were cultured in Roswell Park Memorial Institute 1640 (RPMI 1640) medium (Merck & Co., Inc., Rahway, N.J., USA) supplemented with 2 mM L-glucose, 10% fetal bovine serum, and 100 U/mL penicillin-streptomycin at 37 °C in 5% CO2.
2.5. Proliferation Measurement
HCC827 cells were seeded in 12-well plates at a density of 1×104 cells per well. After 24 h, ICG, ICG liposomes, IR-783, and IR-783 liposomes were treated with 10 μM of the respective HMC equivalents, and cell growth was monitored using an incubation monitoring system (Olympus CM30).
2.6. MTT Assay
To determine cell viability, 5 mg/mL tetrazolium salt, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was introduced to the culture medium of HCC827 cells and incubated for 3 h at 37 °C. Subsequently, the medium was removed, and the cells were lysed with 500 μL dimethyl sulfoxide. Absorbance was then measured at 570 nm.
2.7. IR-783 Liposome Therapeutic Intervention
IR-783 liposomes were diluted to 50 mL with 5% glucose (Hikari Seiyaku Co., Ltd., Tokyo, Japan) and infused intravenously at a rate of 2 mL/min through a vein in the middle of the patient’s arm. A multilaser delivery system (Weber, Germany) was selected as the laser delivery device for PDT. PDT was performed at a laser power density of 25 mW/cm2 using a fiber with a wavelength of 810 nm approximately 24 h after liposome administration.
2.8. PDT for Tongue Cancer
The outer circumference of the fiber for the MLDS infrared was wrapped with a wrapping film, and the patient was instructed to lightly bite the portion of the fiber that was in contact with the mantle of the syringe. Irradiation with an 810-nm laser for 20 min was subsequently performed. A nasal cannula (MC Medical, Inc., Tokyo, Japan) was attached to a valve with a medical oxygen flow regulator (Air Liquide Japan G.K., Tokyo, Japan), and oxygen was administered intranasally to the patient at approximately 2 L/min during the intervention.
2.9. PDT for Breast Cancer
Five MLDS infrared fibers were passed through the aperture in the masher, wrapped in a wrapping film (Fig. 4A). Irradiation with an 810-nm laser for 40 min at the limit of contact with the lesion was then performed.
2.10. Statistical Analysis
All results are expressed as the mean ± standard deviation. The statistically significant differences were analyzed using the one-way analysis of variance followed by Bonferroni’s post hoc test. All statistical analyses were performed using the add-in software Statcel4 (v4.0; OMS Publishing, Inc., Tokorozawa, Japan). Significance levels were set at P < 0.05 and P <0.01.
3. Results
3.1. T Physicochemical Characteristics of HMC Liposomes
IR-783 showed higher NIR absorption than did ICG (Fig. 1A), consistent with previous reports [
23]. Moreover, both liposomalized IR-783 and ICG demonstrated enhanced absorption in the NIR region after processing (Fig. 1A). The absorption wavelength of ICG liposomes undergoes a slight shift towards longer wavelengths because of the dissolution of ICG within the hydrophobic groups of the phospholipid bilayer [
24]. Here, this phenomenon occurred not only with ICG, but also with IR-783 (
Figure 1A). Encapsulation of HMC in liposomes was investigated using gel filtration chromatography. The wavelengths of ICG, ICG liposomes, IR-783, and IR-783 liposomes, as determined by gel filtration chromatography, were identified based on the UV spectrum results. For clarity, only the liposomes are depicted on the right side of
Figure 1B. In gel filtration chromatography, smaller particles were identified in subsequent fractions. ICG was below the limit of detection, whereas IR-783 was detected in an inconsistent manner across the 40–100 mL fractions (
Figure 1B). The same fractions in which liposomes were detected prior to inclusion contained both liposomized ICG and IR-783 (
Figure 1B). For the EPR effect to accumulate macromolecules in tumor tissues, a size of 5–100 nm is considered optimal [
22] because this range is not subject to renal clearance. Recently, a particle size as small as 30 nm was identified as particularly effective as it can easily pass through the cancer stroma [
25]. Accordingly, we modified liposomes to a diameter of approximately 20 nm (
Table 1). Both ICG and IR-783 exhibited a change in charge upon liposomization, with a positive tilt (
Table 1). It has been hypothesized that the incorporation of HMCs into liposomes modifies the surface potential. The results of our UV spectroscopy, gel filtration, and zeta potential analyses demonstrated that the IR-783 liposomes could effectively encapsulate IR-783.
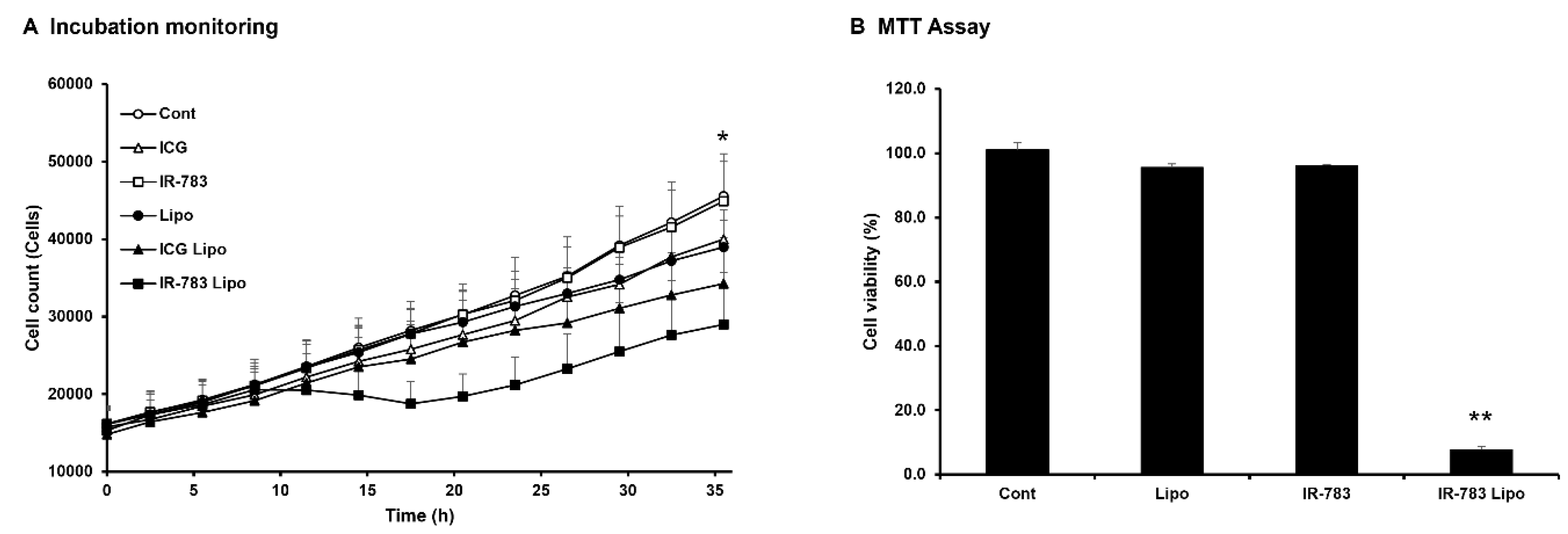
3.2. Inhibitory Effect of IR-783 Liposome Treatment on Cell Proliferation
The inhibitory effects of HMC and HMC liposomes on the proliferation of HCC827 lung cancer-derived cells were observed in real-time using a culture monitoring system (
Figure 2A). The results demonstrated that only IR-783 liposomes significantly inhibited HCC827 cell proliferation at 36 h post culture. Similarly, ICG liposome-treated cells better inhibited cell proliferation than did control, although the difference was not significant. Furthermore, the inhibitory effect of IR-783 liposomes on cell growth was evaluated using the MTT assay (
Figure 2B). The results were comparable to those in the monitoring system, except in cells treated with liposomal IR-783 that exhibited significantly lower in viability than did the control group.
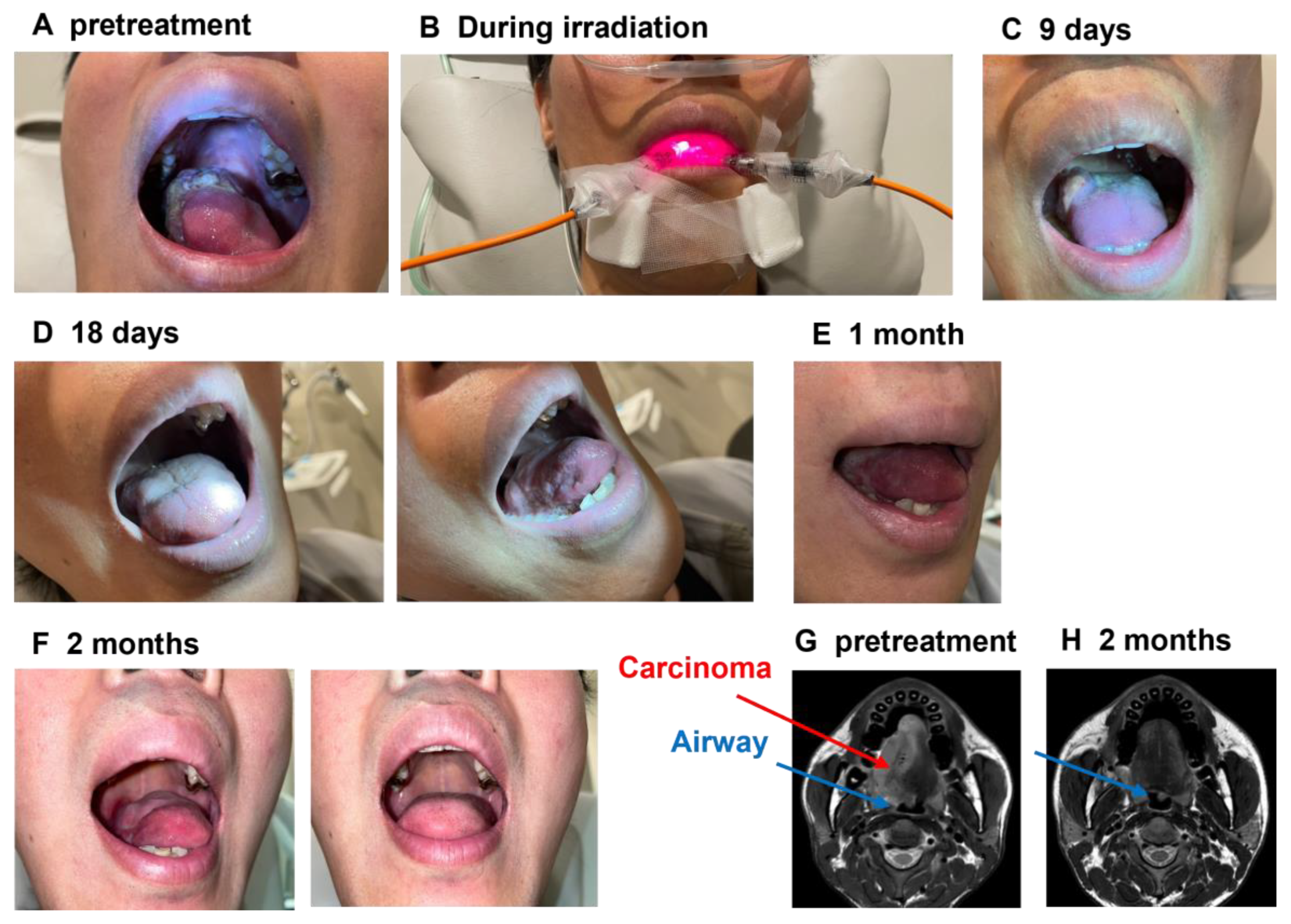
3.3. PDT Using IR-783 Liposome for the Patient with Tongue Cancer
Despite being diagnosed with tongue cancer in 2022, the male patient in his 30s did not pursue professional cancer treatment and thus had disease progression without intervention. In December 2023, the lesion advanced, extending to the upper palate and causing respiratory distress (
Figure 3A, G). Consequently, the patient sought phototherapy in our hospital. In February 2024, 5 mg of IR-783 liposomes was administered intravenously at an IR-783 equivalent dose, and PDT was performed the following day at 60 J/cm² using two 810-nm probes (
Figure 3B). Owing to the improvement in lesions, pain, and normal biochemical test results after PDT, we decided to increase the IR-783 dosage. At 1 week after the initial dose, IR-783 liposomes (10 mg in 783 equivalents) were intravenously administered over 2 days. On days 2 and 3, we performed under conditions identical to those used for the initial dose. After three phototherapy sessions, the tumor in contact with his upper palate started to shed partially (
Figure 3C), and he reported an improvement in his breathing. Eighteen days after the initial intervention, the tumor in the upper portion of the tongue regressed, leaving only an ulcerative lesion on the right lateral aspect of the tongue (
Figure 3D). After 1 month, the ulcerated area had disappeared (
Figure 3F), and magnetic resonance imaging (MRI) T2 scans taken 3 months later showed no lesions. Additionally, an improvement in airway narrowing was observed on the initial scan (
Figure 3G–H).
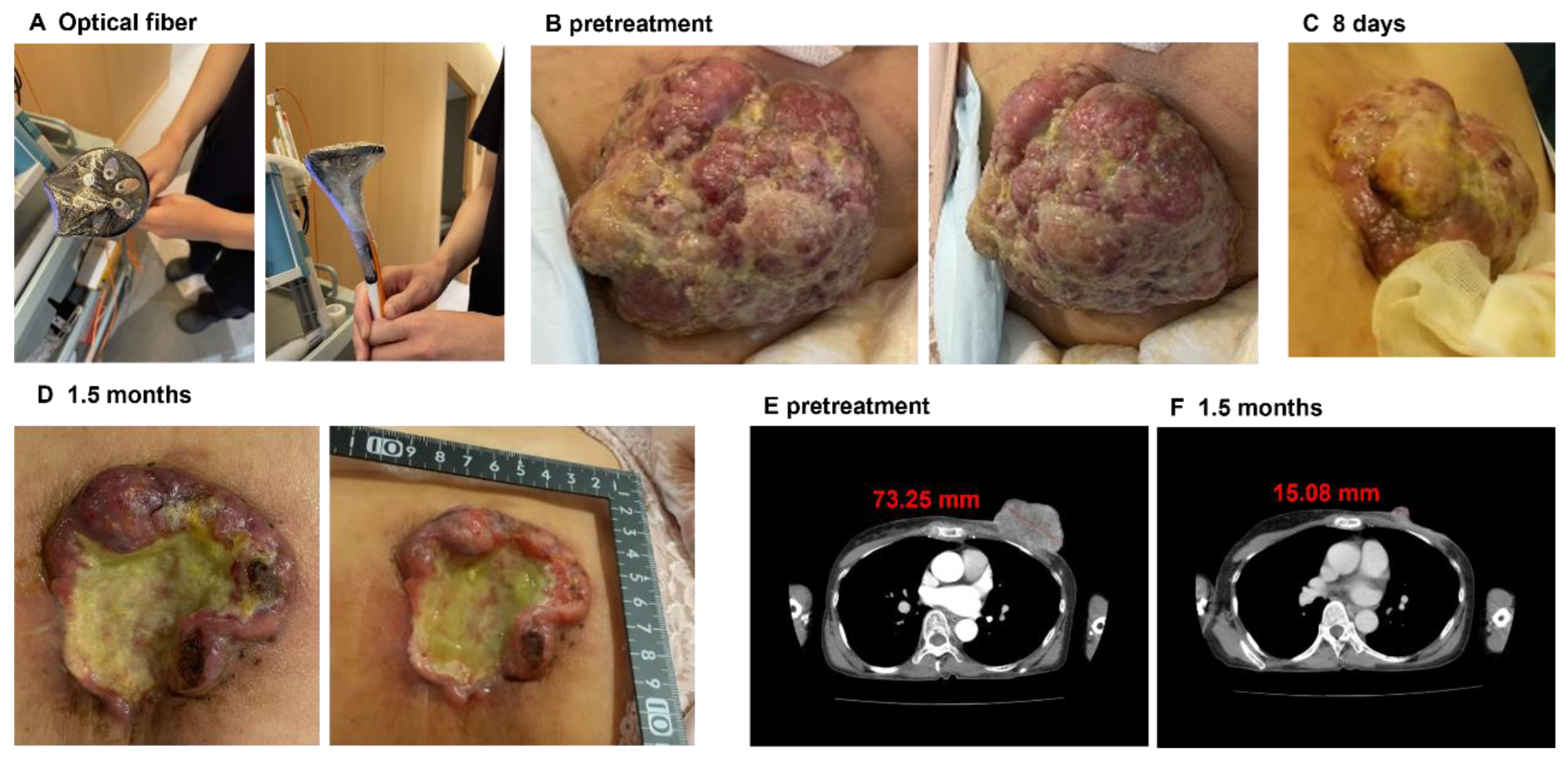
3.4. PDT Using IR-783 Liposome for the Patient with Breast Cancer
A woman in her 60s was diagnosed with breast cancer in 2015 and was initially treated with a combination of taxane and pembrolizumab. In 2022, the patient developed massive breast discharge and pelvic metastasis and required radiation therapy for pain relief. In 2023, her physician determined that the pharmacological intervention was ineffective and thus withdrew treatment. In May 2024, she was admitted to our hospital because of the lack of alternative treatment options for her medical condition following the cessation of medication. When she visited our clinic, computed tomography (CT) confirmed the presence of a mass in her left breast (Fig. B, E). With her informed consent, we decided to perform PDT with IR-783 liposomes because the lesion was visible. On the first 2 days, 12.5 mg of IR-783 liposomes was intravenously administered at an equivalent dose of IR-783, and PDT at 300 mJ/cm
2 was subsequently performed using five 810-nm fibers in the next 2 days. During PDT, the lesion exhibited significant exudate secretion; however, the patient did not report any pain. Exudation immediately ceased after the initial PDT, and over the course of 1 week, the lesion surface slowly turned blackish and dry. As the lesion improved (Fig 4C), we administered IR-783 liposomes on day 8 for 2 more days under the same conditions, followed by two additional PDT sessions. When she returned to our clinic approximately 6 weeks later, CT imaging showed that the raised mass previously observed had been dislodged and had significantly decreased in size than that at the initial visit (
Figure 4D, F).
4. Discussion
The findings of this study indicate that IR-783 liposomes can impede the proliferation of cancer cells without the need for photoexcitation, and they have antitumor effects against both tongue and breast cancers as photosensitizers for PDT. Although several anti-tumor effects of PDT and PTT using IR-783 have been documented in cell and animal studies [
26,
27,
28], to the best of our knowledge, this is the first clinical report of PDT using IR-783 in humans.
IR-783 can inhibit the growth of cancer cells in the absence of laser irradiation [
17,
18]. This study demonstrated that liposomalized IR-783, but not IR-783 alone, had a notable inhibitory effect on the proliferation of lung cancer cells (
Figure 2). This discrepancy may be because previous studies required treatment of cells with IR-783 at concentrations of 100 μM or higher to achieve cell death comparable to ours [
17,
18], whereas the present study used a significantly lower concentration of 10 μM. The previous findings indicate that although the survival rate in breast cancer cells treated with IR-783 at concentrations below 10 μM was reduced, it was largely unaltered when compared to that in control cells [
17,
18]. The inhibitory effects of both IR-783 and ICG on cancer cell growth through liposomalization (
Figure 2) support that these HMCs have enhanced efficacy owing to increased cellular uptake facilitated by liposomalization. In this clinical trial, PDT was performed with IR-783 liposomes as these liposomes demonstrated a superior anti-tumor effect compared to ICG liposomes.
A patient with tongue cancer presented with various symptoms, including dyspnea, dysphagia, dysgeusia, taste disorders, and speech disorders, all of which were attributed to the tumor. Pre-treatment MRI observations indicated that surgical intervention and radiotherapy were unlikely to be effective in improving cancer-related complications. However, lesion size was markedly reduced with PDT treatment (Fig 3), and this improved his breathing, taste, and speech functions. These findings indicate that PDT may represent a promising modality for the future treatment of tongue cancer. Further, the patient with breast cancer who previously demonstrated no improvement with drug therapy exhibited a notable reduction in tumor size following the PDT intervention (
Figure 4). These findings suggest that PDT using IR-783 liposomes may be an effective treatment tumors resistant to cytotoxic chemotherapeutic agents and immune checkpoint inhibitors. Although not reported in this report, the patient’s lesions are improving and will continue to be monitored and, if necessary, treated in the same manner.
Despite the evidence indicating the clinical efficacy and safety of PDT with IR-783, several challenges remain unresolved. The precise mechanism by which IR-783 exerts its antiproliferative effects remains to be elucidated, and further investigation is required to gain a deeper understanding of this process. With the enhancement of endocytosis through IR-783 liposomalization in this study, further studies will be conducted to investigate the previously reported mitochondrial mitogenic effect of IR-783 [
17,
18]. With the limited number of patients reported in this study (only two), we will expand the scope of our research through collaboration and other means as more patients are accumulated. Ultimately, we intend to conduct further statistical analyses, including 5-year survival rates. Invasive procedures such as laparotomy and thoracotomy are required to treat visceral tumor tissues with PDT, given that this treatment is essentially aimed at tumor tissue confined to the superficial layers of the body. Such a procedure would be challenging to perform in a clinic of our size and would require the resources of a larger hospital. Sonodynamic therapy (SDT), which employs ultrasound waves that penetrate deep into the body to stimulate photosensitizers, has garnered considerable attention in recent years [
29]. The inhibitory effect of SDT with IR-780, a derivative of IR-783, on cancer cells was demonstrated in both cell and animal experiments [29, 30]. Further studies are planned to investigate the potential of SDT using IR-783 as a treatment modality for pancreatic and liver cancers. Subsequent studies will be conducted at our clinic using SDT with IR-783, including in patients with pancreatic and liver cancers.
5. Conclusions
In conclusion, this study demonstrates that IR-783 liposomes inhibit cell growth and shrink tongue and breast cancer cells. The utilization of IR-783 as a photosensitizer for PDT is anticipated to represent a novel approach to cancer eradication, particularly for patients with refractory advanced cancer, without imposing undue burden.
Author Contributions
Conceptualization, Y. K. and S. K.; methodology, Y. K.; software, S. K., T. K., and F. Y. ; validation, Y. K., S. K., Y. H., T. K., A. T., F. Y., S. Y., and H. M.; formal analysis, Y. K. and S. K.; investigation, Y. K. and S. K.; resources, Y. K. and Y. K.; data curation, S. K.; writing—original draft preparation, S. K.; writing—review and editing, O. I. and K. H.; visualization, H. M.; supervision, O. I. and K. H.; project administration, Y. K.; funding acquisition, none. All the authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the IGT CLINIC (protocol code 30 and date of approval: February 24, 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
All data necessary to evaluate the conclusions of the study are presented in this paper. Additional data are available upon request from the corresponding author [KH].
Acknowledgments
We express our sincere gratitude to the staff of Rinku Medical Clinic and StateArt Inc. for their invaluable assistance in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Klement, R.J. Cancer as a global health crisis with deep evolutionary roots. Glob Transit 2024, 6, 45–65. [Google Scholar] [CrossRef]
- Khan, S.U.; Fatima, K.; Aisha, S.; Malik, F. Unveiling the mechanisms and challenges of cancer drug resistance. Cell Commun Signal 2024, 22, 109. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, N.; Sevilla, A. Current advances in photodynamic therapy (PDT) and the future potential of PDT-combinatorial cancer therapies. Int J Mol Sci 2024, 25, 1023. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, H.; Hayashi, N.; Tanaka, M.; Kubota, E.; Yano, S.; Joh, T. Tumor affinity photosensitizers for photodynamic therapy. JJSLSM 2015, 36, 159–165. [Google Scholar] [CrossRef]
- Zhang, X.; Wu, L.; Zhen, W.; Li, S.; Jiang, X. Generation of singlet oxygen via iron-dependent lipid peroxidation and its role in Ferroptosis. Fundam Res 2022, 2, 66–73. [Google Scholar] [CrossRef]
- Kojima, Y.; Tanaka, M.; Sasaki, M.; Ozeki, K.; Shimura, T.; Kubota, E.; Kataoka, H. Induction of ferroptosis by photodynamic therapy and enhancement of antitumor effect with ferroptosis inducers. J Gastroenterol 2024, 59, 81–94. [Google Scholar] [CrossRef]
- Chang, Q.; Wang, P.; Zeng, Q.; Wang, X. A review on ferroptosis and photodynamic therapy synergism: Enhancing anticancer treatment. Heliyon 2024, 10, e28942. [Google Scholar] [CrossRef]
- Tan, L.; Shen, X.; He, Z.; Lu, Y. The role of photodynamic therapy in triggering cell death and facilitating antitumor immunology. Front Oncol 2022, 12, 863107. [Google Scholar] [CrossRef]
- Chou, W.; Sun, T.; Peng, N.; Wang, Z.; Chen, D.; Qiu, H.; Zhao, H. Photodynamic therapy-induced anti-tumor immunity: Influence factors and synergistic enhancement strategies. Pharmaceutics 2023, 15, 2617. [Google Scholar] [CrossRef]
- Aebisher, D.; Przygórzewska, A.; Bartusik-Aebisher, D. The latest look at PDT and immune checkpoints. Curr Issues Mol Biol 2024, 46, 7239–7257. [Google Scholar] [CrossRef]
- Dean, M.; Fojo, T.; Bates, S. Tumour stem cells and drug resistance. Nat Rev Cancer 2005, 5, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Maugeri-Saccà, M.; Vigneri, P.; De Maria, R. Cancer stem cells and chemosensitivity. Clin Cancer Res 2011, 17, 4942–4947. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, G.J.; Saya, H. Therapeutic strategies targeting cancer stem cells. Cancer Sci. 2016, 107, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Overchuk, M.; Weersink, R.A.; Wilson, B.C.; Zheng, G. Photodynamic and photothermal therapies: Synergy opportunities for nanomedicine. ACS Nano 2023, 17, 7979–8003. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Wu, J.B.; Pan, D. Review on near-infrared heptamethine cyanine dyes as theranostic agents for tumor imaging, targeting, and photodynamic therapy. J Biomed Opt 2016, 21, 50901. [Google Scholar] [CrossRef]
- Yorozu, K.; Kaibori, M.; Kimura, S.; Ichikawa, M.; Matsui, K.; Kaneshige, S.; Kobayashi, M.; Jimbo, D.; Torikai, Y.; Fukuzawa, Y.; et al. Experience with photodynamic therapy using indocyanine green liposomes for refractory cancer. J Pers Med 2022, 12, 1039. [Google Scholar] [CrossRef]
- Tang, Q.; Liu, W.; Zhang, Q.; Huang, J.; Hu, C.; Liu, Y.; Wang, Q.; Zhou, M.; Lai, W.; Sheng, F.; et al. Dynamin-related protein 1-mediated mitochondrial fission contributes to IR-783-induced apoptosis in human breast cancer cells. J Cell Mol Med 2018, 22, 4474–4485. [Google Scholar] [CrossRef]
- Li, P.; Liu, Y.; Liu, W.; Li, G.; Tang, Q.; Zhang, Q.; Leng, F.; Sheng, F.; Hu, C.; Lai, W.; et al. IR-783 inhibits breast cancer cell proliferation and migration by inducing mitochondrial fission. Int J Oncol 2019, 55, 415–424. [Google Scholar] [CrossRef]
- Okumura, M.; Ichihara, H.; Matsumoto, Y. Hybrid liposomes showing enhanced accumulation in tumors as theranostic agents in the orthotopic graft model mouse of colorectal cancer. Drug Deliv. 2018, 25, 1192–1199. [Google Scholar] [CrossRef]
- Matsumura, Y.; Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: Mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986, 46, 6387–6392. [Google Scholar]
- Islam, W.; Kimura, S.; Islam, R.; Harada, A.; Ono, K.; Fang, J.; Niidome, T.; Sawa, T.; Maeda, H. EPR-effect enhancers strongly potentiate tumor-targeted delivery of nanomedicines to advanced cancers: Further extension to enhancement of the therapeutic effect. J Pers Med 2021, 11, 487. [Google Scholar] [CrossRef] [PubMed]
- Maeda, H. The 35th anniversary of the discovery of EPR effect: A new wave of nanomedicines for tumor-targeted drug delivery-Personal remarks and future prospects. J Pers Med 2021, 11, 229. [Google Scholar] [CrossRef] [PubMed]
- James, N.S.; Chen, Y.; Joshi, P.; Ohulchanskyy, T.Y.; Ethirajan, M.; Henary, M.; Strekowsk, L.; Pandey, R.K. Evaluation of polymethine dyes as potential probes for near infrared fluorescence imaging of tumors: Part – 1. Theranostics 2013, 3, 692–702. [Google Scholar] [CrossRef] [PubMed]
- Shinoda, K.; Suganami, A.; Moriya, Y.; Yamashita, M.; Tanaka, T.; Suzuki, A.S.; Suito, H.; Akutsu, Y.; Saito, K.; Shinozaki, Y.; et al. Indocyanine green conjugated phototheranostic nanoparticle for photodiagnosis and photodynamic therapy. Photodiagn Photodyn Ther 2022, 39, 103041. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Zhou, L.; Lu, J.; Wang, Y.; Liu, C.; You, L.; Guo, J. Stroma-targeting therapy in pancreatic cancer: One coin with two sides? Front Oncol 2020, 10, 576399. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Li, H.; Yang, M.; Li, X.; Gao, J.; Yuan, Z. IR783 Encapsulated in TR-conjugated liposomes for enhancing NIR imaging-guided photothermal and photodynamic therapy. ChemistrySelect 2022, 7, e202202560. [Google Scholar] [CrossRef]
- Zhu, M.; Wang, P.; Chen, B.; Shi, L.; Long, R.; Wang, S.; Liu, Y. Active-oxygenating hollow Prussian Blue nanosystems loaded with biomacromolecules for photodynamic/photothermal therapy of cancer and alleviating hypoxic tumors. Mater Des 2024, 237, 112618. [Google Scholar] [CrossRef]
- Park, Y.; Park, M.H.; Hyun, H. Structure-inherent tumor-targeted IR-783 for near-infrared fluorescence-guided photothermal therapy. Int J Mol Sci 2024, 25, 5309. [Google Scholar] [CrossRef]
- Zhang, L.; Yi, H.; Song, J.; Huang, J.; Yang, K.; Tan, B.; Wang, D.; Yang, N.; Wang, Z.; Li, X. Mitochondria-targeted and ultrasound-activated nanodroplets for enhanced deep-penetration sonodynamic cancer therapy. ACS Appl Mater Interfaces 2019, 11, 9355–9366. [Google Scholar] [CrossRef]
- Li, Y.; Zhou, Q.; Deng, Z.; Pan, M.; Liu, X.; Wu, J.; Yan, F.; Zheng, H. IR-780 dye as a sonosensitizer for sonodynamic therapy of breast tumor. Sci Rep 2016, 6, 25968. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).