1. Introduction
Osteoporosis is a major risk factor for fractures, reduced quality of life and mortality [
1,
2]. Due to its high prevalence in older societies, it is already a disease of major importance and is expected to increase further in the future [
3]. Therefore, the assessment of risk factors for osteoporosis in terms of prevention and screening is of key importance to reduce the further increase in the disease burden. The main risk factors for osteoporosis are female gender and age [
4], modifiable factors are smoking, BMI, physical activity and diet, especially calcium and vitamin D intake [
5]. Osteoporosis is supposed to be affecting 22 million women and 5.5 million men in the European union [
6] and 800.000 fractures occur in Germany per year [
7].
As we know from the gastroenterologist’s point of view, bone density is linked to liver health [
8]. In patients with liver disease, bone disease is particularly common in the cirrhosis stage, but can also occur at earlier stages [
8]. On the other hand, there is growing evidence that sarcopenia in patients with liver cirrhosis is a major factor for mortality, so that immobility by fractures should be avoided [
9], as these can lead to a vicious circle for patients with osteoporosis [
10].
One of the main causes of liver disease worldwide is viral hepatitis, primarily the hepatitis B virus (HBV) and the hepatitis C virus (HCV)[
11]. Viral hepatitis also remains an important cause of liver disease in Europe, albeit with a decreasing trend [
12]. In Germany 0.2-0.7% of the general population are HBsAg positive (meaning having active hepatitis B infection), 0.2-1.9% are anti-HCV positive and 0.2-0.4% HCV RNA positive [
13]. We know about associations between HBV and HCV and developing osteoporosis and fractures [
14,
15,
16,
17], but with varying results in terms of the strength of association. With regard to HBV and osteoporosis, there is also debate as to whether antiviral treatment, particularly with tenofovir disoproxil fumarate (TDF), promotes the development of osteoporosis compared to other antiviral drugs or patients without treatment [
18,
19,
20].
As HCV treatment has improved dramatically since the introduction of direct antiviral drugs and most of the data we have come across on viral hepatitis and bone disease is from the 2010s, we wanted to re-examine the relationship between viral hepatitis and osteoporosis/fractures in the era of modern antiviral therapy in a high-income country.
2. Materials and Methods
Database
This study was based on the Disease Analyzer database (IQVIA), which contains data on drug prescriptions, diagnoses, and basic medical and demographic data obtained directly in anonymous format from computer systems used in the practices of general practitioners and specialists [
21]. The database covers approximately 2,500 outpatient practices in Germany. It has previously been shown that the panel of practices included in the Disease Analyzer database is representative of general and specialized practices in Germany [
21]. Finally, this database has already been used in previous studies focusing on hepatitis [
22] and osteoporosis [
23,
24].
Study Population
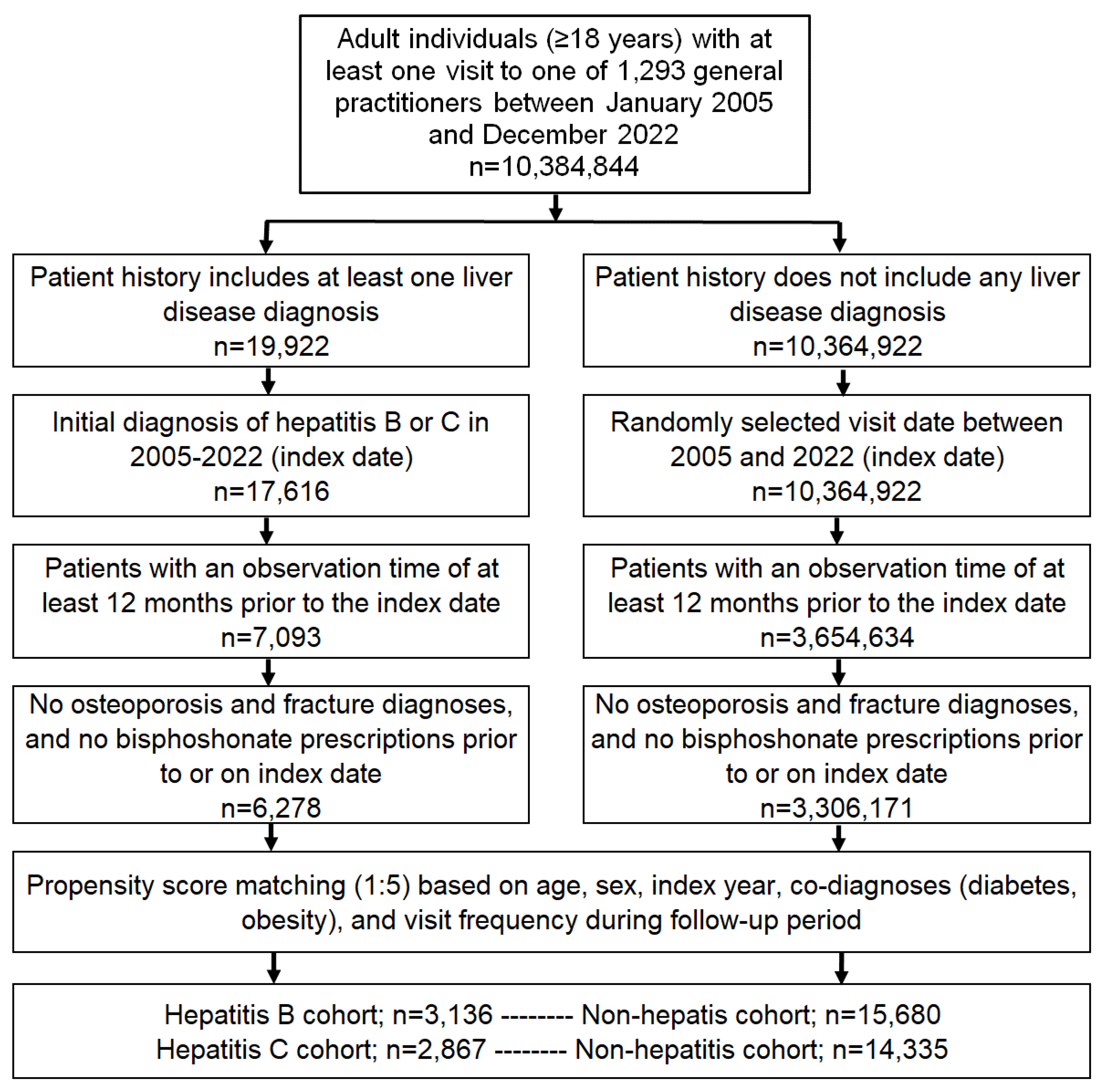
This retrospective cohort study included adult patients (≥18 years) with an initial diagnosis of chronic hepatitis including chronic hepatitis B (CHB, ICD-10: B18.0, B18.1) and chronic hepatitis C (CHC, ICD-10: B18.2) from 1,293 general practices in Germany between January 2005 and December 2022 (index date;
Figure 1). Patients were only included when they had at least 12 months of pre-observation time prior to the index date. Patients with a diagnosis of osteoporosis (ICD-10: M80, M81), or a documented bone fracture (ICD-10: S02, S12, S22, S32, S42, S52, S62, S72, S82, S92, T02, T08, T10, T12) prior to or at index date were excluded. Hepatitis patients were matched to individuals without hepatitis by nearest neighbor propensity scores based on sex, age, index year, obesity, diabetes, and yearly consultation frequency. Diabetes and obesity were used as they are associated with osteoporosis and fractures. As hepatitis patients have a much higher GP consultation frequency, and higher consultation frequency can increase the probability of other diagnoses, we also included the consultation frequency per year in the propensity matching. For the non-hepatitis cohort, the index date was that of a randomly selected visit between January 2005 and December 2022 (
Figure 1). Each kind of hepatis was compared with accordingly matched non-hepatitis individuals. Cohorts were considered to be adequately balanced if the absolute value of the standardized mean difference for each covariate was 0.25 or less.
Study Outcomes and Covariates
The main outcome of the study was the 5-year cumulative incidence of osteoporosis and bone fractures as a function of either chronic hepatitis B or C. As we were unable to differentiate between osteoporotic and non-osteoporotic fractures, we only consider fractures in patients who also were diagnosed with osteoporosis.
Statistical Analyses
Differences in the sample characteristics between patients with and without chronic hepatitis were tested using the Wilcoxon signed-rank test for continuous variables, the McNemar test for categorical variables with two categories, and the Stuart-Maxwell test for categorical variables with more than two categories. The cumulative incidence of osteoporosis and fractures was evaluated using Kaplan-Meier curves. Cox-regression models were conducted to study the association between CHB or CHC and the incidence of osteoporosis and/or bone fractures. Regression analyses were performed separately for women and men. No age-stratified analyses were conducted as the proportion of osteoporosis diagnosis in the age group < 50 years was too small for subgroup analysis. To counteract the problem of multiple comparisons (8 regression models), a p-value <0.005 was considered statistically significant. Analyses were carried out using SAS version 9.4 (SAS institute, Cary, USA).
3. Results
Baseline Characteristics
The present study included 3,136 patients with CHB and 15,608 matched non-hepatitis individuals. Moreover, in a second cohort, we included 2,867 patients with CHC and 14,335 matched non-hepatitis individuals. The baseline characteristics of the study cohort are shown in
Table 1. The mean age [SD] was 50.2 [14.6] years in the CHB cohort and 50.8 [14.6] in the CHC cohort. 52.7% of patients in the CHB cohort and 60.7% of patients in the CHC cohort were female. Due to the matched pair study design, no significant differences between variables were observed between the two hepatitis cohorts and their matched non-hepatitis cohorts.
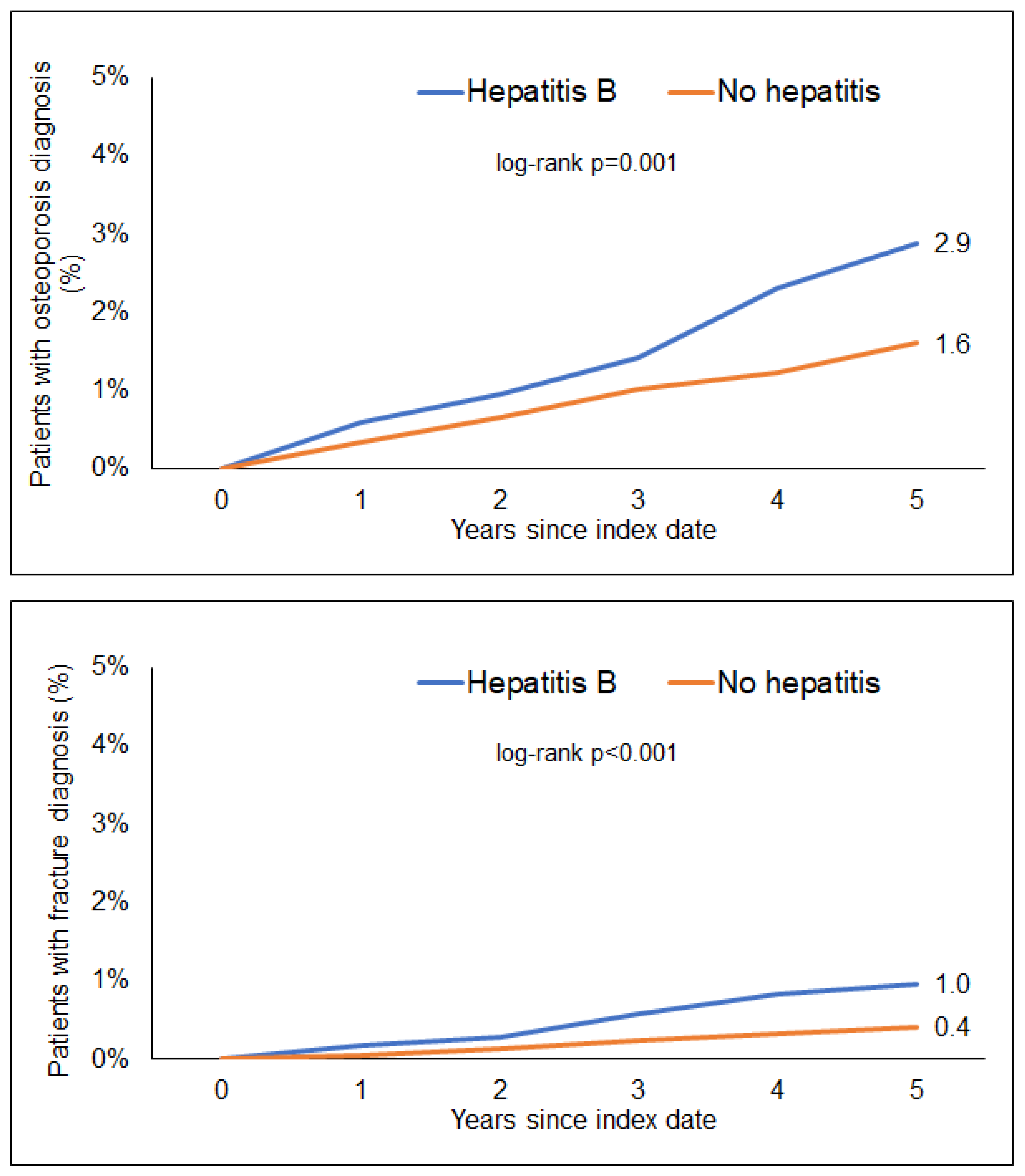
Association of CHB and a Subsequent Diagnosis of Osteoporosis and Bone Fractures
Within 5 years of the index date, 2.9% of CHB patients and 1.6% of individuals without hepatitis were diagnosed with osteoporosis (log-rank, p=0.001). In terms of bone fractures, 1.0% of the CHB patients but only 0.4% of the hon-hepatitis patients were diagnosed with bone fractures (log-rank, p<0.001,
Figure 2). In Cox-regression analyses, CHB was significantly associated with an increased risk of osteoporosis (Hazard Ratio (HR): 1.76; 95% CI: 1.31-2.36) as well as bone fractures (HR: 2.43; 95% CI: 1.42-4.14). The association between CHB and osteoporosis reached the predefined level of statistical significance in women only (HR: 1.92; 95% CI: 1.38-2.69). Contrarily, the association between CHB and bone fractures was only significant in men (HR: 3.42; 95% CI: 1.44-8.12).
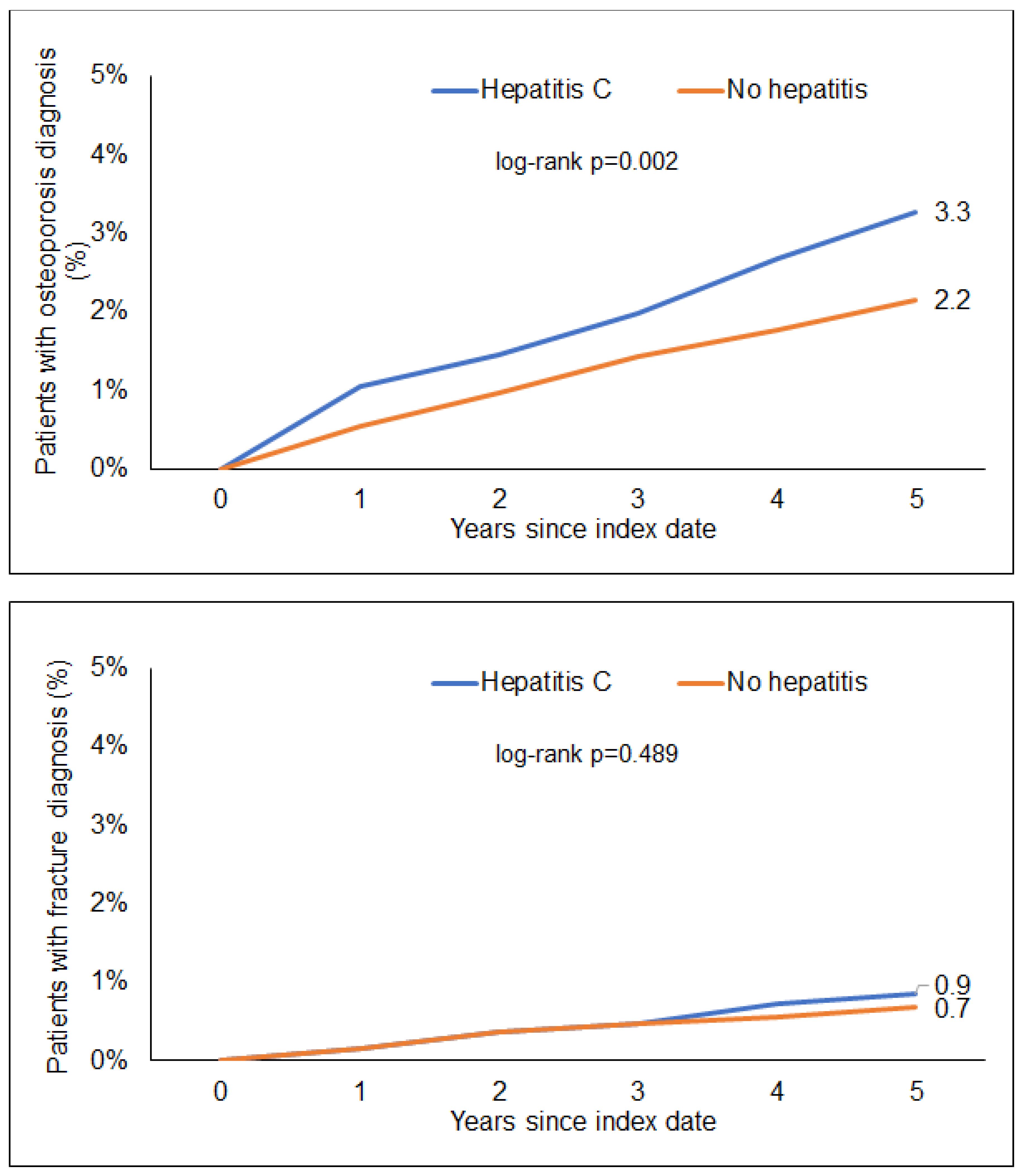
Association of CHC and a Subsequent Diagnosis of Osteoporosis and Bone Fractures
Within 5 years of the index date, 3.3% of CHC patients and 2.2% of individuals without hepatitis were diagnosed with osteoporosis (log-rank, p=0.002). Moreover, 0.9% of CHC patients and 0.7% of the hon-hepatitis patients were diagnosed with a bone fracture (log-rank, p=0.489,
Figure 2). In regression analyses, CHC was significantly associated with an increased risk of osteoporosis (HR: 1.54; 95% CI: 1.17-2.02,
Figure 3). In contrast, CHC was not associated with an increased risk of bone fractures (HR: 1.21; 95% CI: 0.71-2.06,
Figure 3). Interestingly, the association between CHC and osteoporosis was only significant in women (HR: 1.75; 95% CI: 1.29-2.37) but not men (
Table 2).
4. Discussion
In the present study, we evaluate a potential association between CHB and CHC and a subsequent diagnosis of osteoporosis or bone fractures in a large real-world cohort of CHC/CHB patients in Germany. We observe that CHB was significantly associated with an increased risk for osteoporosis and fractures and CHC with osteoporosis. Thereby, we confirm previous findings that CHB is associated with osteoporosis. A Korean study from 2019 compared the odds ratio for diagnosis of CHB or CHC in patients with osteoporosis and a matched control group [
17]. Similar to our data, the association between CHB and osteoporosis was stronger than between CHC and osteoporosis. Furthermore, as in our data, the association was limited to the female subgroup. Tao et al analyzed data from the US NHANES database for association of HBsAg positive and HCV RNA positive patients and lower bone mineral density and found positive relations for both [
15]. A meta-analysis of 15 studies regarding HIV/HCV coinfected patients showed a HR of 1.63 of coinfected patients compared to HIV mono-infected patients for the diagnosis of osteoporosis[
25].
Our data show differing effects of viral hepatitis and sex. The HR for osteoporosis was 1.92 in women with CHB and 1.75 in those with CHC, while in men there was no statistically significant association. This is somewhat counterintuitive, as CHB is known to affect liver health more in men than women. Men are more likely to develop HCC, are less likely to clear HBeAg and less likely to be protected by HBV vaccination[
26]. Considering the better viral control of women, differences in osteoporosis may be due to immunological phenomena. For HCV infection there are also known gender differences: Women are more likely to clear HCV infections and progress slower towards cirrhosis [
27]. However, these effects are only seen in pre-menopausal women and are lost after menopause, showing the influence of estrogen. In conclusion, the differences are also not explained by liver disease but by the immune response. Analysis of immune response and cytokine markers may help to explain the different effect on bone disease. Dessordi et al suggest a higher osteoclastic activity triggers osteoporosis in HBV infected patients regardless of antiviral treatment, meaning that the better immune control in women could be related to osteoclastic activation[
20]. Furthermore, the overall higher prevalence of osteoporosis in female patients could lead to a higher statistical power for that subgroup and explain why differences are only significant for women.
Of note, the association between CHB and fractures was only significant in men with an HR of 3.42 in the reported data of our study. In contrast, we could only find a non-significant association between CHB and osteoporosis in men. Therefore, it seems likely that fractures were not related to osteoporosis and probably more frequent in male CHB patients because of co-founders. A big proportion of HBV infected patients in Germany have history of migration, 4% of the migrant population are HBV positive in contrast to <1% of the general population in western Europe[
28], 5% of the Turkish population in Germany are reported to be HBV positive for example [
29]. There is also an association between socio-economic status of patients and fractures[
30]. In conclusion most of the association between male CHB patients and fractures could be due to the co-founder of migration and socio-economic status. Another confounder leading to more fracture risk could be alcohol consumption, which is also reported to be an important factor for patients with HBV infection in terms of liver disease progression [
31,
32].
Patients with chronic HBV and or HCV should be screened for risk of osteoporosis and this risk should be addressed in patient communication. Lifestyle factors like smoking or physical exercise should be optimized, since they do not only affect risk for osteoporosis but also risk of liver disease progression. Patients should also be evaluated for vitamin D supplementation and/or guided for improvement of diet choices.
By study design this study is limited because of its retrospective nature. Furthermore, we cannot differentiate between treated and untreated patients meaning we only can report association between diagnosis of viral hepatitis and osteoporosis or fractures. Since antiviral treatment of HBV is reportedly affecting risk of osteoporosis this is further limiting. We also cannot match lifestyle factors such as physical exercise, BMI, alcohol intake or smoking. Smoking is for example more frequent in HCV patients than in the general population [
33]. Since this study is set in a general practitioner setting, we also did not differentiate between patients with or without liver cirrhosis since we estimated the prevalence too small for matching.
Author’ contribution
SHL, KK, and CR designed the study, KK performed statistical analyses and generated figures and tables, AK, SHL, and KK wrote the manuscript, HB and TL provided intellectual input, all authors agreed to the final version of the manuscript.
Funding
There was no funding associated with this work.
Data availability statement
The underlying data are available upon reasonable request from the corresponding author.
Ethical approval
The "Disease Analyzer" database, used for analysis, contains anonymized electronic patient records. Patient data was analyzed in aggregated form without individual data being available. An individual consent form was not obtained following national and European legislation.
Consent for publication
All authors approved the publication of this manuscript.
Conflict of interest
The authors declare no competing interest. AK did lectures for Gilead, received travel bursary from Gilead and Abbvie and a research grant from Gilead. TL received consulting fees from Gilead, Abbvie, and Ipsen; payment or honoraria for lectures or presentations from Gilead and Abbvie.
References
- Stanghelle B, Bentzen H, et al. Associations between health-related quality of life, physical function and pain in older women with osteoporosis and vertebral fracture. BMC geriatrics 2019;19(1):298. [CrossRef]
- Bliuc D, Nguyen ND, et al. Accelerated bone loss and increased post-fracture mortality in elderly women and men. Osteoporos Int 2015;26(4):1331–9. [CrossRef]
- Cooper C, Cole ZA, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporosis international a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2011;22(5):1277–88. [CrossRef]
- Pietschmann P, Rauner M, et al. Osteoporosis: an age-related and gender-specific disease—a mini-review. Gerontology 2009;55(1):3–12. [CrossRef]
- Dontas IA, Yiannakopoulos CK. Risk factors and prevention of osteoporosis-related fractures. Journal of musculoskeletal & neuronal interactions 2007;7(3):268–72. [PubMed]
- Kanis JA, Norton N, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Archives of osteoporosis 2021;16(1):82. [CrossRef]
- O’Kelly J, Bartsch R, et al. Real-world effectiveness of osteoporosis treatments in Germany. Archives of osteoporosis 2022;17(1):119. [CrossRef]
- Danford CJ, Trivedi HD, Bone Health in Patients With Liver Diseases. Journal of Clinical Densitometry 2020;23(2):212–22. [CrossRef]
- Tantai X, Liu Y, et al. Effect of sarcopenia on survival in patients with cirrhosis: A meta-analysis. Journal of hepatology 2022;76(3):588–99. [CrossRef]
- Kerr C, Bottomley C, et al. The importance of physical function to people with osteoporosis. Osteoporosis international a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 2017;28(5):1597–607. [CrossRef]
- Stanaway JD, Flaxman AD, et al. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet (London, England) 2016;388(10049):1081–8. [CrossRef]
- Hepatitis B and C in Europe: an update from the Global Burden of Disease Study 2019. The Lancet. Public health 2023;8(9):e701-e716. [CrossRef]
- Sperle I, Steffen G, et al. Prevalence of Hepatitis B, C, and D in Germany: Results From a Scoping Review. Frontiers in public health 2020;8:424. [CrossRef]
- Wijarnpreecha K, Thongprayoon C, et al. Hepatitis C virus infection and risk of osteoporosis: A meta-analysis. Saudi Journal of Gastroenterology Official Journal of the Saudi Gastroenterology Association 2017;23(4):216–21. [CrossRef]
- Tao J, Yan Z, et al. Seropositive for hepatitis B and C viruses is associated with the risk of decreased bone mineral density in adults: An analysis of studies from the NHANES database. Frontiers in medicine 2023;10:1120083. [CrossRef]
- Pelazas-González R, González-Reimers E, et al. Bone alterations in hepatitis C virus infected patients. European journal of internal medicine 2013;24(1):92–6. [CrossRef]
- Min C, Bang WJ, et al. The association between hepatitis and osteoporosis: a nested case-control study using a national sample cohort. Archives of osteoporosis 2019;14(1):34. [CrossRef]
- Yip TC-F, Lai JC-T, et al. Long-term use of tenofovir disoproxil fumarate increases fracture risk in elderly patients with chronic hepatitis B. Journal of hepatology 2024;80(4):553–63. [CrossRef]
- Kim E, Lee HW, et al. Tenofovir disoproxil fumarate versus tenofovir alafenamide on risk of osteoporotic fracture in patients with chronic hepatitis B: A nationwide claims study in South Korea. Alimentary pharmacology & therapeutics 2023;58(11-12):1185–93. [CrossRef]
- Dessordi R, Watanabe LM, et al. Bone loss in hepatitis B virus-infected patients can be associated with greater osteoclastic activity independently of the retroviral use. Scientific reports 2021;11(1):10162. [CrossRef]
- Rathmann W, Bongaerts B, et al. Basic characteristics and representativeness of the German Disease Analyzer database. International journal of clinical pharmacology and therapeutics 2018;56(10):459–66. [CrossRef]
- Loosen SH, Schöler D, et al. Differential role of chronic liver diseases on the incidence of cancer: a longitudinal analysis among 248,224 outpatients in Germany. Journal of cancer research and clinical oncology 2023;149(7):3081–7. [CrossRef]
- Kostev K, Hadji P, Impact of Osteoporosis on the Risk of Dementia in Almost 60,000 Patients Followed in General Practices in Germany. Journal of Alzheimer’s disease JAD 2018;65(2):401–7. [CrossRef]
- Stumpf U, Hadji P, et al. Incidence of fractures in patients with type 1 diabetes mellitus-a retrospective study with 4420 patients. Osteoporos Int 2020;31(7):1315–22. [CrossRef]
- Dong HV, Cortés YI, et al. Osteoporosis and fractures in HIV/hepatitis C virus coinfection: a systematic review and meta-analysis. AIDS (London, England) 2014;28(14):2119–31. [CrossRef]
- Wang S-H, Chen P-J, Gender disparity in chronic hepatitis B: Mechanisms of sex hormones. Journal of gastroenterology and hepatology 2015;30(8):1237–45. [CrossRef]
- Baden R, Rockstroh JK, Natural history and management of hepatitis C: does sex play a role? The Journal of infectious diseases 2014;209 Suppl 3:S81-5. [CrossRef]
- Gnyawali B, Pusateri A, et al. Epidemiologic and socioeconomic factors impacting hepatitis B virus and related hepatocellular carcinoma. World Journal of Gastroenterology 2022;28(29):3793–802. [CrossRef]
- Burgazli KM, Mericliler M, et al. The prevalence of hepatitis B virus (HBV) among Turkish immigrants in Germany. European review for medical and pharmacological sciences 2014;18(6):869–74. [PubMed]
- Hansen L, Judge A, et al. Social inequality and fractures-secular trends in the Danish population: a case-control study. Osteoporos Int 2018;29(10):2243–50. [CrossRef]
- Ganesan M, Eikenberry A, et al. Role of alcohol in pathogenesis of hepatitis B virus infection. World Journal of Gastroenterology 2020;26(9):883–903. [CrossRef]
- Mota A, Guedes F, et al. Alcohol consumption among patients with hepatitis B infection in northern Portugal considering gender and hepatitis B virus genotype differences. Alcohol 2010;44(2):149–56. [CrossRef]
- Chew KW, Bhattacharya D, et al. Short Communication: Coronary Heart Disease Risk by Framingham Risk Score in Hepatitis C and HIV/Hepatitis C-Coinfected Persons. AIDS research and human retroviruses 2015;31(7):718–22. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).