Submitted:
23 September 2024
Posted:
24 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
Research Questions
Study Period and Data Source
Patient Identification and Obesity Definition
Statistical Analyses
Comorbidity and Outcome Identification
Ethical Considerations
3. Results
Comparison of Key Demographic and Hospital Characteristics
Comparison of Comorbidities Between Severely Obese and Non-Obese Patients
Comparison of Hospitalization Outcomes Between Severely Obese and Non-Obese Patients
Postoperative Complications in Severely Obese vs. Non-Obese Patients
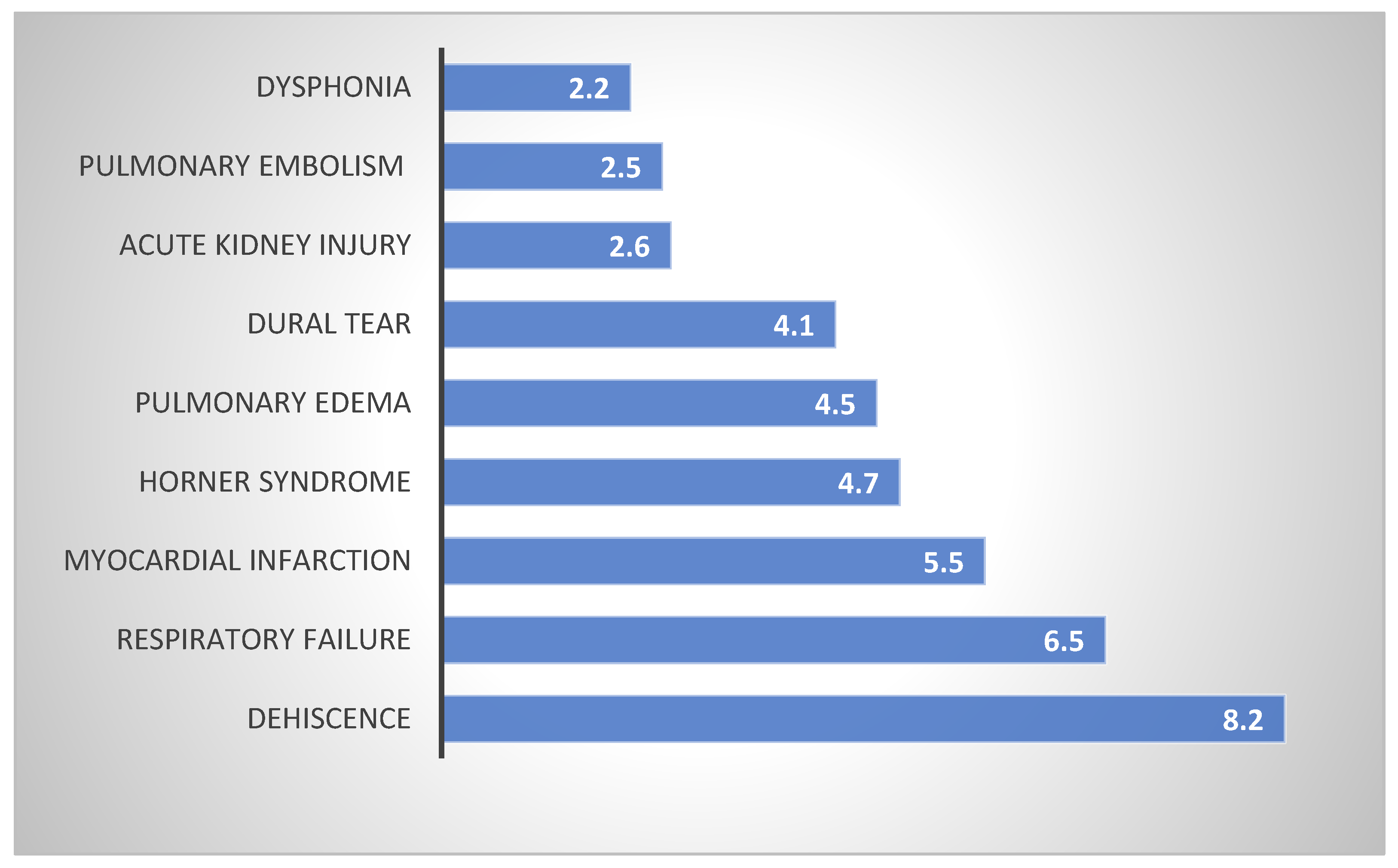
Postoperative Complications with Significantly Higher Odds in Severely Obese Patients
- Dehiscence had the highest OR at 8.2 (95% CI: 2.8–23.9, p<0.001.
- Respiratory failure had an OR of 6.5 (95% CI: 3.1–13.6, p<0.001), showing a significantly increased risk for severely obese patients.
- Myocardial infarction had an OR of 5.5 (95% CI: 2.0–15.0, p<0.001), indicating a markedly higher risk in the severely obese group.
- Horner syndrome had an OR of 4.7 (95% CI: 2.3–9.5, p<0.001).
- Pulmonary edema had an OR of 4.5 (95% CI: 2.5–7.9, p<0.001).
- Dural tear had an OR of 4.1 (95% CI: 2.0–8.2, p<0.001).
- Acute kidney injury had an OR of 2.6 (95% CI: 2.0–3.3, p<0.001).
- Pulmonary embolism had an OR of 2.5 (95% CI: 1.3–4.9, p=0.005).
- Dysphonia had an OR of 2.2 (95% CI: 1.6–3.1, p<0.001).
4. Discussion
Impact of BMI on ACDF Outcomes
Study Findings: Demographics
Study Findings: Comorbidities:
Study Findings: Postoperative Complications:
5. Conclusions:
Funding
Informed consent
Acknowledgments
Conflicts of Interest
Ethical approval
References
- Shao Jin Teo, William Yeo, Marcus Zhixing Ling, Poh Ling Fong, Chang Ming Guo, John Li Tat Chen, and Reuben Chee Cheong Soh. The Effect of Body Mass Index on Long-Term Patient-Reported Outcome Scores after Anterior Cervical Discectomy and Fusion in an Asian Population: A 2-Year Study. Asian Spine J. 2020 Sep 22. 15(4): 512–522. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8377209/. [CrossRef] [PubMed]
- Roberto, J. Perez-Roman, David McCarthy, Evan M. Luther, Julian G. Lugo-Pico, Roberto Leon-Correa, Wendy Gaztanaga, Karthik Madhavan, and Steven Vanni1. Effects of Body Mass Index on Perioperative Outcomes in Patients Undergoing Anterior Cervical Discectomy and Fusion Surgery. Neurospine. 2020 Nov 17. 18(1): 79–86. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8021846/. [PubMed]
- Kyung-Jin Song and Byeong-Yeol Choi. Current Concepts of Anterior Cervical Discectomy and Fusion: A Review of Literature. Asian Spine J. 2014 Aug 19. 8(4): 531–539. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4150000/. [CrossRef] [PubMed]
- Elliot, D.K. Cha, Conor P. Lynch, James M. Parrish, Nathaniel W. Jenkins, Shruthi Mohan, Cara E. Geoghegan, Caroline N. Jadczak, and Kern Singh. Recovery of Physical Function Based on Body Mass Index Following Anterior Cervical Discectomy and Fusion. Int J Spine Surg. 2022 Jan 25. 15(6): 1123–1132. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9469024/. [CrossRef] [PubMed]
- Qi, Min MD; Xu, Chen MD; Cao, Peng MD; Tian, Ye MD; Chen, Huajiang MD; Liu, Yang MD; Yuan, Wen MD. Does Obesity Affect Outcomes of Multilevel ACDF as a Treatment for Multilevel Cervical Spondylosis? Clinical Spine Surgery. December 2020. 33(10):p E460-E465. Available online: https://journals.lww.com/jspinaldisorders/abstract/2020/12000/does_obesity_affect_outcomes_of_multilevel_acdf_as.10.aspx. [CrossRef]
- Silky Chotai, J. Alex Sielatycki, Scott L. Parker, Ahilan Sivaganesan, Harrison L. Kay, David P. Stonko, Joseph B. Wick, Matthew J. McGirt, Clinton J. Devin. Effect of obesity on cost per quality-adjusted life years gained following anterior cervical discectomy and fusion in elective degenerative pathology. the spine journal. July 6, 2016. Available online: https://www.thespinejournalonline.com/article/S1529-9430(16)30281-9/abstract. [CrossRef]
- Evan, G. Gross, Nicholas M.B. Laskay, James Mooney, M. Chandler McLeod, Travis J. Atchley, Dagoberto Estevez-Ordonez, Jakub Godzik. Morbid Obesity Increases Length of Surgery in Elective Anterior Cervical Discectomy and Fusion Procedures but Not Readmission or Reoperation Rates: A Cohort Study. Orld neurosurgery. 2023 Mar 11 173:e830-e837. Available online: https://pubmed.ncbi.nlm.nih.gov/36914028/. [CrossRef] [PubMed]
- George THOMAS, Puneet GUPTA, Taimur CHAUDHRY, Neil D ALMEIDA, William WOODALL, John THOMAS, Bennett R. LEVY, Nyle C. ALMEIDA, Jonathan H SHERMAN. Impact of Obesity on Anterior Cervical Discectomy and Fusion (ACDF): Postoperative Morbidity and Mortality. Turk Neurosurg. 25.09.2023. Available online: https://pubmed.ncbi.nlm.nih.gov/37846533/. [CrossRef] [PubMed]
- Andrew, B. Andrew B. Koo , Aladine A. Elsamadicy , Margot Sarkozy , Wyatt B. David , Benjamin C. Reeves , Christopher S. Hong , Arianne Boylan , Maxwell Laurans , Luis Kolb. Independent Association of Obesity and Nonroutine Discharge Disposition After Elective Anterior Cervical Discectomy and Fusion for Cervical Spondylotic Myelopathy. World neurosurgery. 2021 May 18. 151:e950-e960. Available online: https://pubmed.ncbi.nlm.nih.gov/34020060/. [CrossRef] [PubMed]
- Eric Tecce, Advith Sarikonda, Adam Leibold, Daniyal Mansoor Ali, Sara Thalheimer, Ashmal Sami, Joshua Heller, Srinivas Prasad, Ashwini Sharan, James Harrop, Alexander Vaccaro, Ahilan Sivaganesan. Does Body Mass Index Influence Intraoperative Costs and Operative Times for Anterior Cervical Discectomy and Fusion? A Time-Driven Activity-Based Costing Analysis. World Neurosurg. 2024 Feb 19. 185:e563-e571. Available online: https://pubmed.ncbi.nlm.nih.gov/38382758/. [CrossRef] [PubMed]
- Taylor, D. Ottesen, Rohil Malpani, Anoop R. Galivanche, Cheryl K. Zogg, Arya G. Varthi, and Jonathan N. Grauer. Underweight patients are at just as much risk as super morbidly obese patients when undergoing anterior cervical spine surgery. Spine J. 2020 Mar 16. 20(7): 1085–1095. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7380546/. [CrossRef] [PubMed]
- Bryce A Basques, Jannat M Khan, Philip K Louie, Jeremy Mormol, Steven Heidt, Arya Varthi, Justin C Paul, Edward J Goldberg, Howard S An. Obesity does not impact clinical outcome but affects cervical sagittal alignment and adjacent segment degeneration in short term follow-up after an anterior cervical decompression and fusion. Spine J. 2019 Mar 23. 19(7):1146-1153. Available online: https://pubmed.ncbi.nlm.nih.gov/30914278/. [CrossRef] [PubMed]
- Shyam J Kurian, Waseem Wahood, Yagiz Ugur Yolcu, Elena Blaginykh, Anshit Goyal, Arjun S Sebastian, Mohamad Bydon. Risk Factors for Unplanned Readmissions Following Anterior Cervical Discectomy and Fusion and Posterior Lumbar Fusion Procedures: Comparison of Two National Databases. World Neurosurg. 2020 Aug 8. 143:e613-e630. Available online: https://pubmed.ncbi.nlm.nih.gov/32781151/. [CrossRef] [PubMed]
- Alba Scerrati, Antonino Germano', Nicola Montano, Jacopo Visani, Fabio Cacciola, Giovanni Raffa,Ilaria Ghetti,Fabrizio Pignotti, Michele Alessandro Cavallo, Alessandro Olivi, and Pasquale de Bonis. Factors affecting functional outcome after anterior cervical discectomy and fusion: A multicenter study. J Craniovertebr Junction Spine. 2021 Jun 10. 12(2): 144–148. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8214232/. [CrossRef] [PubMed]
- Scott C Robertson, Mason R Ashley. Complications of Anterior Cervical Discectomy and Fusion. Acta Neurochir Suppl. 2023:130:169-178. Available online: https://pubmed.ncbi.nlm.nih.gov/37548736/. [CrossRef] [PubMed]
- Kimia Khalatbari Kani, Felix S Chew. Anterior cervical discectomy and fusion: review and update for radiologists. Skeletal Radiol. 2017 Oct 23. 47(1):7-17. Available online: https://pubmed.ncbi.nlm.nih.gov/29058045/. [CrossRef] [PubMed]
- John A Sielatycki, Silky Chotai, Harrison Kay, David Stonko, Matthew McGirt, Clinton J Devin. Does Obesity Correlate With Worse Patient-Reported Outcomes Following Elective Anterior Cervical Discectomy and Fusion? Neurosurgery. 2016 Jul;79(1):69-74. Available online: https://pubmed.ncbi.nlm.nih.gov/27166659/. [CrossRef] [PubMed]
- Peter Y Joo, Justin R Zhu, Christopher Wilhelm, Kevin Tang, Wesley Day, Jay Moran, Jonathan N Grauer. Anterior Cervical Discectomy and Fusion Outcomes in Patients With and Without Bariatric Surgery-Weight Loss Does Make a Difference. Spine (Phila Pa 1976). 2023 Jan 24.2023 Mar 15;48(6):400-406. Available online: https://pubmed.ncbi.nlm.nih.gov/36735637/. [CrossRef] [PubMed]
- Tangyiheng Chen, Yujie Wang, Hong Zhou, Cheng Lin, Xuefeng Li, Huilin Yang, Yijie Liu, Weimin Jiang. Comparison of anterior cervical discectomy and fusion versus anterior cervical corpectomy and fusion in the treatment of localized ossification of the posterior longitudinal ligament. J Orthop Surg (Hong Kong). 2023 Jan-Apr;31(1):10225536231167704. Available online: https://pubmed.ncbi.nlm.nih.gov/36972216/. [CrossRef] [PubMed]
- Ankur S Narain, Fady Y Hijji, Brittany E Haws, Krishna T Kudaravalli, Kelly H Yom, Jothan Markowitz, Kern Singh. Impact of body mass index on surgical outcomes, narcotics consumption, and hospital costs following anterior cervical discectomy and fusion. J Neurosurg Spine. 2017 Dec 1. 28(2):160-166. Available online: https://pubmed.ncbi.nlm.nih.gov/29192877/. [CrossRef] [PubMed]
- Vladimir Katuch, Jan Banoci, Veronika Magocova, Martin Cmorej, Jana Katuchova, Kleanthia Efthymiou, Veronika Roskovicova. Postoperative complications associated with anterior cervical discectomy and three years follow-up. Bratisl Lek Listy. 2024;125(3):183-188. Available online: https://pubmed.ncbi.nlm.nih.gov/38385545/. [CrossRef] [PubMed]
- Maman, D.; Mahamid, A.; Finkel, B.; Gan-Or, H.; Fournier, L.; Berkovich, Y.; Behrbalk, E. Comparative evaluation of postoperative outcomes and expenditure between robotic and conventional single-level lumbar fusion surgery: A comprehensive analysis of nationwide inpatient sample data. Eur. Spine J. 2024, 33, 2637–2645. [Google Scholar] [CrossRef] [PubMed]
- Maman, D.; Laver, L.; Becker, R.; Mahamid, A.; Berkovich, Y. Robotic-assisted total knee arthroplasty reduces postoperative complications and length of stay without increased cost compared to navigation-guided techniques: A national analysis. Knee Surg. Sports Traumatol. Arthrosc.
- Maman, D.; Laver, L.; Becker, R.; Takrori, L.A.; Mahamid, A.; Finkel, B.; Gan-Or, H.; Yonai, Y.; Berkovich, Y. Trends and Epidemiology in Robotic-Assisted Total Knee Arthroplasty: Reduced Complications and Shorter Hospital Stays. Knee Surg. Sports Traumatol. Arthrosc.
- Maman, D.; Mahamid, A.; Yonai, Y.; Berkovich, Y. Comparing Complication Rates, Costs, and Length of Stay between Unicompartmental and Total Knee Arthroplasty: Insights from a Big Data Analysis Using the National Inpatient Sample Dataset. J. Clin. Med. 2024, 13, 3888. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Without Severe Obesity (%) | Severe Obesity (%) | Significance |
|---|---|---|---|
| Total Surgeries | 80650 | 4935 | - |
| Average Age (y) | 55.7 | 54 | P<0.001 |
| Female (%) | 51.3 | 57.1 | P<0.001 |
| Primary expected payer - Medicare (%) | 33.8 | 35 | P<0.001 |
| Primary expected payer - Medicaid (%) | 10.6 | 12.2 | |
| Primary expected payer - private including HMO (%) | 44.5 | 44.8 | |
| Primary expected payer - self-pay (%) | 1.2 | 1.1 | |
| Primary expected payer - no charge (%) | 0.1 | 0.1 | |
| Primary expected payer - other (%) | 9.8 | 6.9 | |
| Status of hospital (STRATA) - Rural (%) | 72.9 | 75.6 | P<0.001 |
| Status of hospital (STRATA) - Urban nonteaching (%) | 23.3 | 20.7 | |
| Status of hospital (STRATA) - Urban teaching (%) | 3.8 | 3.7 |
| Prameter | Without Severe Obesity (%) | Severe Obesity (%) | Significance |
|---|---|---|---|
| Type 2 Diabetes Mellitus | 17.8 | 38 | P<0.001 |
| Diabetes Mellitus | 19.5 | 38.5 | P<0.001 |
| Mental Disorders | 40.4 | 45.7 | P<0.001 |
| Hypertension | 56.3 | 43.7 | P<0.001 |
| Dyslipidemia | 70 | 30 | P<0.001 |
| Obstructive Sleep Apnea | 9.5 | 31.1 | P<0.001 |
| Chronic Kidney Disease | 3.6 | 6.4 | P<0.001 |
| Chronic Lung Disease | 7.8 | 11.4 | P<0.001 |
| Thyroid Disorder | 11.7 | 15.4 | P<0.001 |
| Chronic Anemia | 2.3 | 3.5 | P<0.001 |
| Heart Failure | 0.1 | 0.3 | P<0.001 |
| Connective Tissue Disorder | 0.1 | 0.1 | P=0.621 |
| History of Myocardial Infarction | 2.9 | 3.1 | P=0.372 |
| Peripheral Vascular Disease | 1.3 | 1.4 | P=0.559 |
| Dementia | 0.2 | 0.2 | P=0.002 |
| Peptic Ulcer Disease | 0.3 | 0.3 | P=0.623 |
| IBD (Inflammatory Bowel Disease) | 0.5 | 0.3 | P=0.038 |
| Hemiplegia | 0.2 | 0.1 | P=0.085 |
| Neoplasms | 0.8 | 0.9 | P=0.576 |
| Neoplasms of Lymphoid/Hematopoietic | 0.3 | 0.3 | P=0.664 |
| Fibromyalgia | 3.8 | 4.4 | P=0.041 |
| Smoking | 1.2 | 0.7 | P=0.001 |
| Alcohol Abuse | 1.2 | 1 | P=0.279 |
| Osteoporosis | 2.3 | 2 | P=0.137 |
| Parkinson Disease | 0.5 | 0.3 | P=0.103 |
| Alzheimer Disease | 0.1 | 0.1 | P=0.097 |
| Parameter | Without Severe Obesity (%) | Severe Obesity (%) | Significance |
|---|---|---|---|
| Died During Hospitalization (%) | 0.1 | 0.1 | P=0.506 |
| Length of stay (Days) | 1.65 | 1.92 | P<0.001 |
| Total charges ($) | 66913 | 66655 | P=0.702 |
| Parameter | Without Severe Obesity (%) | Severe Obesity (%) | Significance |
|---|---|---|---|
| Venous Thromboembolism | 0.1 | 0.1 | P=0.452 |
| Cardiac Arrhythmias | 2 | 2.3 | P=0.092 |
| Pneumonia | 0.2 | 0.3 | P=0.446 |
| Urinary Tract Infection (UTI) | 0.6 | 0.8 | P=0.059 |
| Blood Transfusion | 0.2 | 0.1 | P=0.347 |
| Blood Loss Anemia | 1.6 | 1.6 | P=0.907 |
| Dysphagia | 5.1 | 4.9 | P=0.383 |
| Brachial Plexus Injury | 0 | 0 | P=0.338 |
| Cerebrospinal Fluid Leak | 0.3 | 0.2 | P=0.483 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





