1. Introduction
Biliary tract cancers (BTCs) are a group of malignancies associated with high morbidity and mortality rates. Although these cancers are rare, making up approximately 3% of all gastrointestinal neoplasms, global data highlights a consistently rising incidence over the past 30 years [
1]. BTCs encompass a diverse and challenging group of malignancies, including cholangiocarcinoma (CCA), gallbladder cancer (GBC), and ampullary cancer. CCAs can be further categorised based on their anatomical location into intrahepatic (iCCA) and extrahepatic (eCCA) types. Extrahepatic cholangiocarcinoma (eCCA) itself includes perihilar (pCCA) and distal (dCCA) cholangiocarcinoma [
2]. BTCs are known for their rarity and aggressiveness, resulting in poor prognostic outcomes, making them notoriously difficult to treat. The global incidence of BTC varies across geographical areas, with lower rates observed in Western Europe (2.00-3.59 cases per 100,000 annually) and North America (2.33-2.35 cases per 100,000 annually)[
3] . In contrast, the Asia-Pacific region and South America exhibit higher incidence rates, likely due to a higher prevalence of specific risk factors such as chronic liver disease, liver fluke infections, obesity, and excessive use of alcohol and tobacco [
3]. BTC outcomes remain poor, as demonstrated by a retrospective analysis of 13,827 patients with metastatic BTC over 17 years, revealing a median overall survival (OS) of just 4.5 months [
4]. In another large cohort of Korean patients with localised BTCs, the 5-year survival rate was 48.5% for ampullary cancer, 28.5% for GBC, 19.9% for eCCA and 10.8% for iCCA [
5].
Surgical resection remains the mainstay of curative treatment for patients with BTCs, however only 20% of patients have disease amenable to surgery [
6] . Moreover, surgery is a high-risk procedure, contraindicated in some patients due to co-morbidities or increasing age. Adjuvant chemotherapy with capecitabine is now an approved standard of care option in patients with radically resected CCA or GBC, following the results of the phase III randomised BILCAP study [
6]. However, relapse rates remain high; 60% at 5 years [
7]. The vast majority of patients with BTCs present with a locally advanced or metastatic stage disease, and for these patients, palliative chemotherapy or best supportive care are often the only feasible treatment options. More recently, molecularly targeted therapies including, but not limited to, inhibitors of the isocitrate dehydrogenase 1 (IDH1) and fibroblast growth factor receptor (FGFR) have proven effective in a molecularly selected subgroup of patients with iCCA after at least one previous line of systemic treatment and have received approval by international regulatory agencies for use in this setting [
8,
9,
10,
11]. However, only a minority of patients with BTCs (approximately 15% of those with iCCA) exhibit relevant molecular alterations (i.e.
IDH1 mutation,
FGFR2 fusion or rearrangement) making them eligible for these treatments [
12,
13,
14]. Other molecular alterations have also been identified such as v-raf murine sarcoma viral oncogene homolog B (
BRAF) and human epidermal growth factor 2 (
HER2), with research on-going[
2].
Increasingly ageing populations remain an issue, particularly in developed nations[
15]. Chronic diseases associated with ageing, such as cancer, cardiovascular and cerebrovascular diseases, neurodegenerative disorders, and metabolic conditions, have become major health concerns in these regions[
15,
16]. The medical costs for treating these conditions are taking up a growing share of government and insurance budgets. As a result, drug discovery and development in the coming decades are expected to focus primarily on addressing these chronic diseases [
17,
18]. Novel anticancer targeted therapies, such as antibody drug conjugates (ADCs), are increasingly being researched and utilised, aiming to offer effective alternatives, especially in patients where treatment options are often limited to chemotherapy or immunotherapy.
This review will outline the structure and mechanism of ADCs and highlight their application in various cancer types, including lung, breast, and urothelial cancers, to showcase their current uses and efficacy. Furthermore, the review will explore how these insights could be extrapolated for the treatment of BTCs. The data on the efficacy and safety of ADCs in BTC is currently limited, primarily due to the rarity and complexity of the disease. BTC is a diverse group of cancers, including cholangiocarcinoma, gallbladder cancer, and ampullary cancer, with distinct molecular characteristics. As a result, effective targeted therapies, including ADCs, are still in the early stages of exploration for this disease group. In this review, ongoing ADC trials in BTCs will be discussed, with a focus on their potential role in the future management of patients with BTC.
2. Methods
In relation to ADCs, studies regarding use of antibody drug conjugates in cancer, particularly in BTCs, were searched in Embase (1974 to 2024) and Ovid MEDLINE(R) (1946 to 2024). Search terms included “BTC”, “antibody drug conjugate”, “immunoconjugate”, “biliary tract neoplasms”, “tumour”, “cholangiocarcinoma”, “pancreatic cancer”, “hepatocellular cancer” and “Trastuzumab Deruxtecan” with relevant results displayed. Meta-analyses, conference abstracts, prospective studies and retrospective series were included. ADC use in haematological malignancies and non-English language articles were excluded. The references of eligible studies and relevant review articles (identified from the database search) were examined to detect other studies of interest. Clinical trial data was extracted from the ClinicalTrials.gov trial registry (data last accessed 5th June 2024). The summary findings are discussed in this review.
3. Current Standard of Care Treatments in BTC
For patients with locally advanced or metastatic BTC, Cisplatin and Gemcitabine (CisGem) became the standard of care following the publication of the ABC-02 trial, which demonstrated a median OS of 11.7 months for the combination[
17] . This was statistically significantly superior to gemcitabine alone, which yielded a median OS of 8.1 months (hazard ratio, 0.64; 95% confidence interval, 0.52 to 0.80; P<0.001). More recently, the Keynote 966 and TOPAZ-1 clinical trials supported the addition of an immune checkpoint inhibitor (ICI) to CisGem in the first line advanced setting [
19,
20,
21] . In the Keynote 966 trial, patients with previously untreated, unresectable, locally advanced or metastatic biliary tract cancer were randomly assigned to treatment with pembrolizumab plus gemcitabine and cisplatin, or placebo plus gemcitabine and cisplatin. OS was 12.7 months (hazard ratio, 0.83; 95% confidence interval, 11.5 to 13.6) in the pembrolizumab group versus 10.9 months (hazard ratio, 0.75; 95% confidence interval, 6.70 to 7.40) in the placebo group. Therefore, this study highlighted a meaningful improvement in OS outcomes with use of the ICI, pembrolizumab, in combination with cisplatin and gemcitabine, versus treatment with cisplatin and gemcitabine alone. In the TOPAZ-1 trial, patients with a locally advanced or metastatic BTC receiving first-line CisGem combined with the programmed cell death 1 ligand 1 (PD-L1) inhibitor durvalumab achieved a progression-free survival (PFS) of 7.2 months (hazard ratio, 0.75; 95% confidence interval, 6.70 to 7.40; P=0.001) and an OS of 12.8 months (hazard ratio, 0.80; 95% confidence interval, 11.1 to 14.0; P=0.021). In comparison, the arm with CisGem and placebo achieved a PFS of 5.7 months (hazard ratio, 0.75; 95% confidence interval, 5.6 to 6.7; P=0.001) and an OS of 11.5 months (hazard ratio, 0.80; 95% confidence interval, 10.1 to 12.5; P=0.021).
Following progression on first-line treatment with CisGem and durvalumab or pembrolizumab (or CisGem or Gem alone if immunotherapy is contraindicated), second-line treatment options remain limited. Current standard of care options include chemotherapy with 5-Fluorouracil (5-FU) and Oxaliplatin (FOLFOX) as in the ABC-06 trial, or 5-FU and Irinotecan (FOLFIRI) or 5-FU/liposomal irinotecan [
19,
20,
21]. The ABC-06 trial was a randomised phase III, multicentre, controlled, open-label trial comparing FOLFOX and active symptom control (ASC) to ASC alone in patients with advanced BTC who had progressed on prior CisGem chemotherapy [
22]. This trial met its primary endpoint, showing a median OS of 6.2 months in the FOLFOX and ASC arm (hazard ratio, 0.69; 95% confidence interval, 5.4-7.6; P=0.031) compared to 5.3 months in the ASC alone arm (hazard ratio, 0.80; 95% confidence interval, 0.50-0.97; P=0.021). In the FOLFOX and ASC arms, 69% of patient reported adverse events versus 52% in the ASC group alone. However, FOLFOX and ASC did not show a significant decline in quality-of-life parameters (quality of life and value of health questionnaires) [
23]. Overall, this trial highlighted the potential benefit of FOLFOX chemotherapy in OS rates at 6 and 12 months, establishing this chemotherapy regimen as a potential standard of care option in the second-line setting, in patients not eligible for targeted therapies.
Only a small proportion of patients with BTCs are eligible for second-line treatment, with one retrospective study indicating this figure to be as low as 25% [
24]. This cohort typically comprises younger patients or those with a longer PFS following first-line treatment [
24].
4. Tumour Profiling and Application in BTCs
There is a pressing need for more effective and better tolerated second-line treatment options for patients with BTCs. Targeted molecular therapies are being increasingly studied and utilised for the treatment of various cancers, including BTCs, due to advances in tumour genomic profiling. Next-generation sequencing (NGS) has paved the way for identifying targetable tumour genomic alterations and molecular pathways involved in carcinogenesis [
12,
25].
The MOSCATO 01 trial utilised NGS on tumour biopsies from patients with incurable, relapsed, or resistant solid malignancies, revealing that 411 of the 843 patients had actionable molecular alterations [
12]. Among these, 43 patients had advanced BTC, and 23 of them received targeted therapy. The overall response rate in this cohort was 33%, with a disease control rate as high as 88%. Notably, one patient with HER2-positive BTC, treated with a combination of trastuzumab and chemotherapy, achieved a complete response. These findings underscore the importance of molecular profiling of BTC samples following diagnosis. This approach can potentially help identify further genomic alterations that can inform additional treatment options for patients with BTCs.
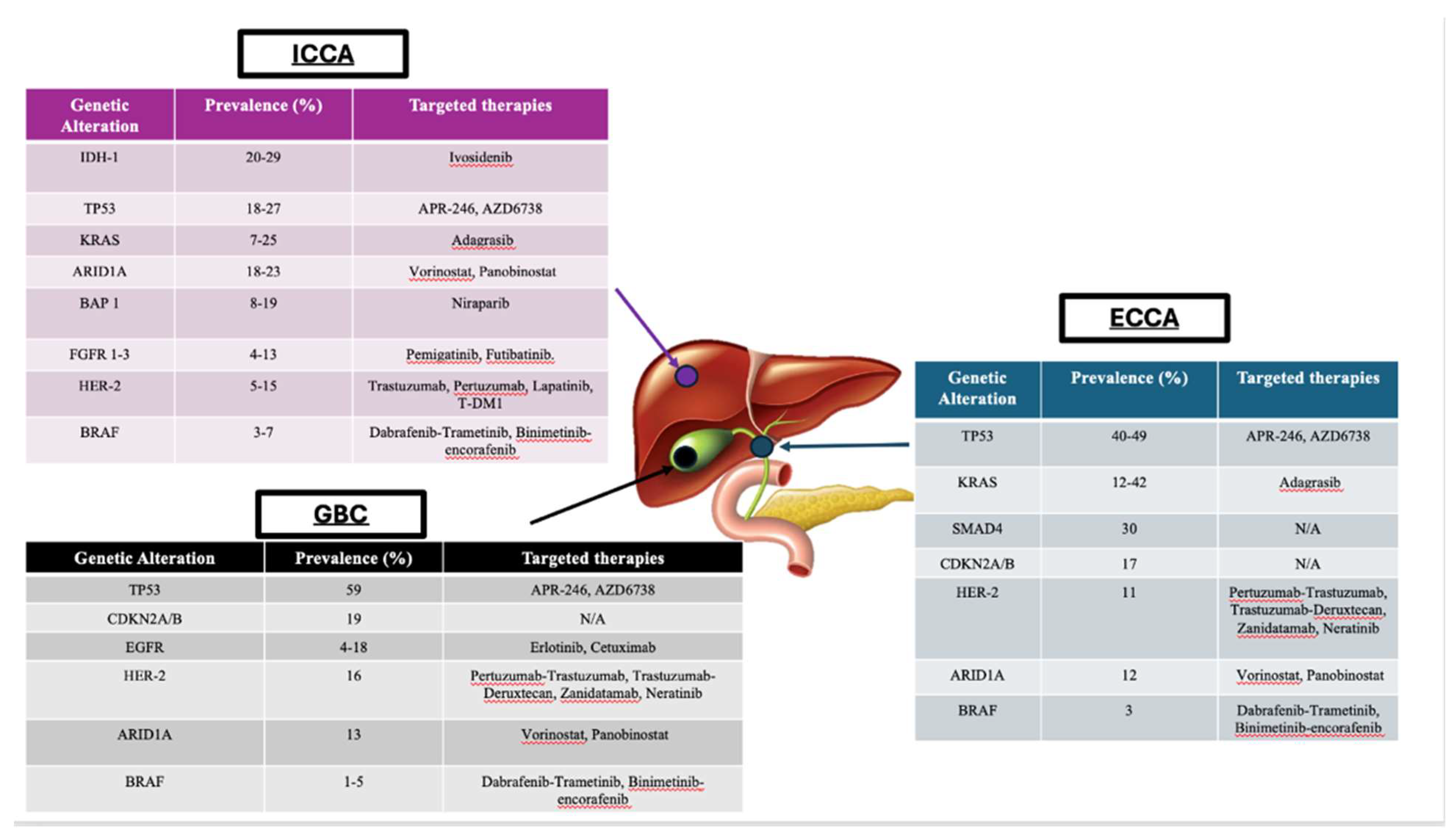
The prevalence of these genomic mutations vary, based on the anatomical location of the tumour, highlighted by
figure 1 [
13]. Thus, integrating molecular profiling into the clinical management of BTC can potentially improve outcomes for patients by allowing for more personalised approaches. Alterations found in iCCA include fibroblast growth factor receptor (
FGFR) 1-3 and isocitrate dehydrogenase (
IDH) mutations.
FGFR alterations are present in up to 13% of iCCA cases [
13]. Pemigatinib, an oral pan-FGFR inhibitor, is approved by the European Medicines Agency (EMA) and United States Food and Drug Administration (FDA) for patients with advanced CCA harbouring
FGFR2 fusions or rearrangement [
8,
26]. The FIGHT-202 trial was a multicentre, open-label, single-arm, multicohort phase II study that recruited patients with inoperable, locally advanced, or metastatic CCA who had already progressed on at least one previous treatment. Patients with and without
FGFR alterations received pemigatinib [
27]. In the cohort with
FGFR2 rearrangements or fusions, the overall response rate (ORR) was 36.6% (95% confidence interval, 26.8-47.2), and the median PFS was 7.0 months (95% confidence interval, 6.1-10.5). Furthermore, the median OS was 17.5 months (95% confidence interval, 14.4-22.9). The FIGHT-202 study showed that pemigatinib is effective in this select cohort of patients and is associated with manageable adverse events. However, it is important to note that acquired resistance remains a significant barrier to the efficacy of adenosine triphosphate-competitive FGFR inhibitors, such as pemigatinib, ultimately limiting their long-term efficacy. Integrating molecular profiling into the clinical management of BTCs is crucial for identifying patients who may benefit from targeted treatments.
Isocitrate Dehydrogenase-1 (
IDH1) mutations have been identified in an estimated 13% of iCCAs [
14]. Following the positive results of the phase III ClarIDHy, the IDH1 inhibitor ivosidenib has been approved by both the EMA and FDA for patients with
IDH1 mutant locally advanced or metastatic iCCA who have been treated with at least one prior line of systemic therapy [
9,
10,
11]. The trial met its primary endpoint of improved median PFS from 1.4 months with placebo to 2.7 months with ivosidenib (hazard ratio 0.37, 95% confidence interval 0.25-0.54;
P = 0.001). Updated survival data from the ClarIDHy trial shows a median OS of 10.3 months with ivosidenib (95% confidence interval, 7.8-12.4 months) versus 7.5 months with placebo (95% CI, 4.8-11.1 months) [
28].
In conclusion, molecular profiling has the potential to inform more personalised therapies that can improve the outcomes of patients with BTCs. However, ongoing research focuses on overcoming the challenges of acquired resistance and expanding the arsenal of targeted therapies available for patients with BTC.
Figure 1.
Diagram highlighting prevalence of common molecular alterations following genomic sequencing in BTC, based on anatomical location and potential targeted therapies. Abbreviations iCCA, intrahepatic cholangiocarcinoma; GBC, gallbladder cancer; eCCA; extrahepatic cholangiocarcinoma [
12,
29,
30,
31,
32,
33].
Figure 1.
Diagram highlighting prevalence of common molecular alterations following genomic sequencing in BTC, based on anatomical location and potential targeted therapies. Abbreviations iCCA, intrahepatic cholangiocarcinoma; GBC, gallbladder cancer; eCCA; extrahepatic cholangiocarcinoma [
12,
29,
30,
31,
32,
33].
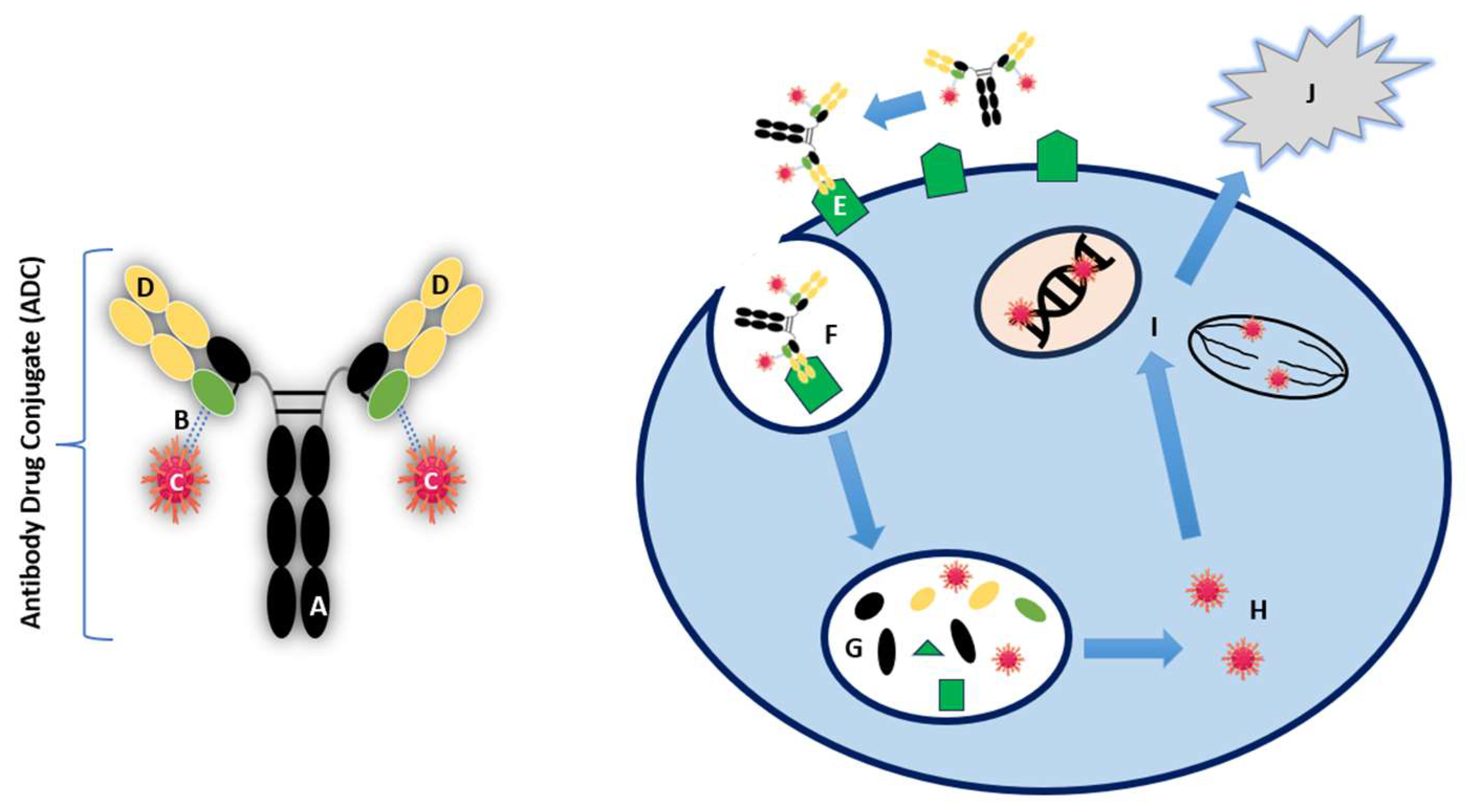
5. Key Components and Mechanism of Action of ADCs
Monoclonal antibodies (mAbs) have been a revolutionary part of anti-cancer therapy in recent times, by directly targeting antigens overexpressed or selectively expressed on tumour cells [
34]. More specifically, antibody-dependent cellular cytotoxicity, complement-dependent cellular cytotoxicity and anti-angiogenic effects on tumour cells are the mechanisms that drive their efficacy. However, despite the number of mechanisms, they lack sufficient cytotoxicity. ADCs consist of three essential components; an antibody, linker and payload, each with a vital role in ultimately causing cell death in cancer cells. The antibody controls immunogenicity and target specificity by expressing selective affinity on the target cell receptor. The linker is the structure that binds the antibody to the payload. The payload is the cytotoxic component that internalises within its target cancer cell, inducing apoptosis[
35,
36]. The structure and mechanism of action of ADCs is summarised in
figure 2.
The selectivity of ADCs is dictated by the antibody that recognises and targets tumour cells over-expressing a specific antigen, thereby sparing normal human tissue. For example, the ADC Trastuzumab emtansine (T-DM1) consists of trastuzumab, an antibody targeting tumour cells over-expressing the human epidermal growth factor 2 (HER2), linked with the antimitotic agent emtansine (DM1). HER2 is overexpressed in about 20% of breast cancers, where T-DM1 allows delivery of the payload specifically to these cancer cells alone, resulting in minimal toxicity to non-malignant tissue and improving the therapeutic index [
37,
38]. T-DM1 has been approved by National Institute for Health and Care Excellence (NICE) since 2017 for treating HER2-positive, unresectable, locally advanced or metastatic breast cancer in adults who previously received trastuzumab or taxane [
39]. Targeting HER2 in BTC will be discussed later in this review.
The linker is pivotal in ensuring that the antibody and payload are bound whilst in the bloodstream, subsequently releasing the cytotoxic payload into the target cancer cells. Therefore, it is the component that determines the stability of an ADC, its pharmacokinetics and pharmacodynamics. Linkers can either be cleavable or non-cleavable. Cleavable linkers can be degraded in certain environments, for example based on pH levels, enzymatic activity (proteolysis) or glutathione levels [
40]. This can be via endosomes or lysosomes. In contrast, non-cleavable linkers require complete lysosomal degradation for the payload to be released. They have shown superior safety profile than ADCs with cleavable linkers, owing to their increased stability in the circulation and a longer half-life [
40,
41].
The payload represents the final key component of the ADC, by delivering the chemotherapeutic agent to the tumour cell following internalisation. These payloads include tubulin inhibitors, immunomodulators and deoxyribonucleic acid (DNA) damaging agents [
36,
40,
41]. ADCs primarily target positive or neutral charges on the tumour cells, for selective cytotoxicity. Specific charges on the payload and linker are carefully engineered to influence targeting, delivery and solubility [
42] Positively charged payloads tend to interact more effectively with the negatively charged phospholipid membranes of cancer cells, aiding in cellular uptake and internalisation. One example is the use of monomethyl auristatin E (MMAE), a commonly used payload that is positively charged at physiological pH and has demonstrated strong cytotoxic activity in targeted cancer cells[
36,
43]. However, balancing the charge is vital, as highly charged molecules can result in off-target toxicity or rapid systemic clearance. Neutral or hydrophilic payloads are often favoured as they reduce off-target toxicity by limiting nonspecific interactions with other cells or proteins in the bloodstream. They can reduce aggregation of the ADC in the circulation and prevent rapid clearance or immune system activation[
44]. Neutral payloads passively diffuse across the cell membrane, contributing to the so-called "bystander effect," where the drug affects both targeted and neighboring cells, enhancing efficacy in heterogeneous tumors[
45]. The selection of the payload in ADCs is driven by several factors, including potency, mechanism of action, stability, and specificity to cancer cells [
46,
47]
Figure 2.
Structure and mechanism of action of ADC. (A) Humanized monoclonal antibody (mAb), (B) Linker at conjugation site(green), (C) Cytotoxic payload, (D) Antigen binding sites (E) Target binding to cell-surface antigen (F) Internalisation of ADC-antigen complex (G) Lysosomal deconjugation (H) Active cytotoxic payload release (I) DNA/microtubule disruption (J) Cell death [
36,
48,
49].
Figure 2.
Structure and mechanism of action of ADC. (A) Humanized monoclonal antibody (mAb), (B) Linker at conjugation site(green), (C) Cytotoxic payload, (D) Antigen binding sites (E) Target binding to cell-surface antigen (F) Internalisation of ADC-antigen complex (G) Lysosomal deconjugation (H) Active cytotoxic payload release (I) DNA/microtubule disruption (J) Cell death [
36,
48,
49].
6. Application of Biomarkers during ADC Treatment
A biomarker, in the context of cancer, represents a biological molecule that can be found in blood, other bodily fluids or tissue associated with a specific biological process such as tumour development or response to therapy. These alterations may be due to germline or somatic mutations, transcriptional changes, epigenetic signatures etc [
50]. Various types of biomarkers include proteins (enzyme or receptor), nucleic acids, antibodies and peptides [
51]. Diagnostic biomarkers can help detect the presence of cancerous cells, such as prostate specific antigen (PSA) in prostate cancer. [
52,
53] Prognostic biomarkers can help outline the likely course or outcome of the disease and guide how aggressive the cancer may behave e.g.
BRCA 1/2 mutations in assessing breast and ovarian cancer risk[
54,
55,
56]. Predictive biomarkers can help indicate how likely a patient will respond to a particular treatment, helping to guide personalised therapy. For example HER-2 overexpression in breast cancer predicts response to HER-2 targeted therapies (e.g. Trastuzumab) [
57,
58].
A good biomarker for ADCs should possess certain characteristics that allow the ADC to effectively target and kill the cancer cells. These biomarkers help guide the selection of patients who are most likely to benefit from ADC therapy and improve the precision and efficacy of treatment. These characteristics include 1) High and stable expression in tumour cells; ensuring that the ADC can reliably bind to the target, as low or variable expression may result in suboptimal delivery of the cytotoxic payload [
40,
59] . Furthermore, tumour specific antigens that are minimally expressed to reduce to effects of off-target toxicities. 2) Ability to internalise upon ADC binding; a good biomarker must trigger internalisation after the ADC binds to it, to ensure the ADC-antigen complex enters the cancer cell and releases the cytotoxic drug [
36]. 3) Functionally relevant to cancer biology; biomarkers play a key role in tumour growth, survival and progression therefore are targeted to deliver the cytotoxic payload. It can also contribute to disrupting cancer pathways. For example, the HER-2 propagated, PI3K/Akt/mTOR signalling pathway, enhances cancer survival and migration in the metastatic microenvironment, initiating secondary tumours[
60]. Therefore, the ADC, T-Dxd, aims at inhibiting HER-2 signalling and slowing the growth of the cancer cells. This has proven to be an effective targeted treatment, such as in breast cancer, which will be highlighted later in this review. 4) Accessibility to testing; the biomarker must be measurable through clinical testing (e.g. immunohistochemistry (IHC) or genetic profiling) which can help identify patients who are suitable to receive ADC therapy and are most likely to benefit from treatment[
61,
62]. For example, in breast cancer T-DM1 relies on high expression of HER-2 (
HER2 gene amplification or IHC +3 on staining) for efficacy as it relies HER2 signalling for optimal binding and internalisation. In contrast, T-Dxd is less reliant on HER-2 expression as it has shown efficacy in HER-2 low cancers as well (
HER2 gene non-amplified or IHC +1 or +2 on staining)[
63,
64]. This can be attributed to its more potent payload (drug-antibody-ratio 8:1) and ‘bystander effect’, which will be outlined later in this review[
65].
Biomarkers are crucial for early detection, personalised treatment and monitoring of cancer progression or treatment response.
7. Advancements in ADC Research and Development
Paul Ehrlich, a German scientist, laid the foundation for the concept of antibody-drug conjugates (ADCs) through his "magic bullet" theory [
66]. He proposed that antibodies could be used to selectively target disease-causing pathogens without harming the host, an idea that later became crucial for ADC development. The use of monoclonal mAbs to target tumor antigens advanced after the development of hybridoma technology in 1975, enabling the production of mAbs in the lab[
67].
In the 1990s, preclinical studies highlighted the potential of ADCs by improving the therapeutic index of cytotoxic drugs and enhancing their selectivity for tumor cells[
68,
69] . This led to the approval of gemtuzumab ozogamicin in 2000, the first FDA-approved ADC for treating acute myeloid leukemia (AML), which paved the way for further ADC research[
70] .
Modern advancements in ADCs focus on identifying new antigen targets or antibodies, improving linker stability and design, optimising pharmacokinetics, expanding the use of different cytotoxic payloads and overcoming resistance mechanisms[
36,
71].
The FDA approval of trastuzumab deruxtecan (T-DXd) marked a milestone for ADCs in biliary tract cancer (BTC)[
72]. T-DXd uses an anti-HER2 monoclonal antibody linked to a topoisomerase I inhibitor, deruxtecan (Dxd), via a cleavable peptide linker[
73,
74]. Dxd is a highly potent payload, reported to have 10-fold higher potency than SN-38, the active metabolite of irinotecan[
75,
76] . Its high drug-antibody ratio (DAR) of 8 enhances its effectiveness in targeting HER2-positive BTC, and its stable linker reduces systemic toxicity[
73] .
While T-DXd is the only ADC approved for BTC so far, ongoing preclinical studies are exploring other antigens and ADCs in the hopes of expanding targeted treatment options in this cancer type[
77] .
8. ADCs in Breast Cancer
ADCs are an emerging targeted therapeutic strategy that show promising efficacy and safety and may offer a solution to tumour resistance in many solid tumour types, including BTCs. Some examples of their use in various solid tumours will now be presented.
In August 2022, the United States Food and Drug Administration (FDA) approved T-Dxd for the treatment of patients with unresectable or advanced HER2-positive breast cancer who have previously been treated with an anti-HER2-based regimen and have developed disease recurrence during or within 6 months of completing therapy [
78,
79]. This approval followed the results of the DESTINY-Breast 03 trial, an open-label, randomised, multicentre, phase III trial that compared T-Dxd to T-DM1 [
78]. T-Dxd demonstrated a statistically significant improvement in ORR [79% (95% confidence interval, 73.1-83.4) versus 35% (95% confidence interval, 29.2-41.1)]. T-Dxd also led to a superior median PFS [29 months (95% confidence interval, 23.7-40.0) versus 7.2 months (95% confidence interval, 6.8-8.3)] and median OS [52.6 months (95% confidence interval, 48.7-non estimable) versus 42.7 months (95% confidence interval, 35.4-non estimable)]. Moreover, it had a manageable safety profile, reflected in superior treatment duration compared to T-DM1.
In contrast to T-DM1, T-Dxd has proven effective even in HER-2 low (IHC +1 or IHC +2/in-situ hybridisation negative) expressing metastatic breast cancer. It has been approved by the FDA, following outcomes of the DESTINY-Breast 04 trial, where T-Dxd highlighted improved PFS [9.9 months (95% confidence interval, 9.0-11.3) versus 5.1 months (95% confidence interval, 4.2-6.8)] and OS [23.4 months (95% confidence interval, 20.0-24.8) versus 16.8 months (95% confidence interval, 14.5-20.0)] in patients with HER-2 low expressing metastatic breast cancer, compared to treatment of physician’s choice (capecitabine, eribulin, gemcitabine, paclitaxel, or nab-paclitaxel) [
80]. This cohort of patients were traditionally not considered eligible for HER2-targeted therapies, but T-DXd's ability to kill cancer cells through its potent cytotoxic payload and bystander effect (where the drug affects neighboring cancer cells regardless of HER2 status) has led to significant clinical responses. This is particularly important in tumors with heterogeneous HER2 expression, expanding the range of cancers that can potentially be treated with this ADC.
9. ADCs in Lung Cancer
Additionally, T-Dxd was the first ADC approved for use in patients with HER2-mutant non-small cell lung cancer (NSCLC) following the results of the DESTINY-Lung01 and DESTINY-Lung02 trials, reporting an ORR of 56% (95% confidence interval, 41.73-70.0) and a duration of response (DOR) of 16.8 months (95% confidence interval, 6.4-not estimable) [
81,
82]. The estimated median PFS was 8.2 months, and the median OS was 18.6 months. While the study concluded that T-Dxd had an overall acceptable safety profile at a dosage of 5.4 mg/kg (as opposed to 6.4 mg/kg), it is worth noting that rates of treatment-related interstitial lung disease (ILD) were up to 12.9% in the 5.4 mg/kg cohort and 28% in the 6.4 mg/kg cohort. In the aforementioned DESTINY-Breast03 trial, the most common treatment-related adverse events (TRAEs) that led to discontinuation were pneumonitis (15 out of 51 patients) and ILD (13 out of 51 patients). Among patients with metastatic breast cancer and HER2-mutant NSCLC treated with T-Dxd, fatal outcomes due to ILD or pneumonitis were reported in 1% of the cohort [
83]. Therefore, close monitoring and early recognition of potential respiratory symptoms are essential, particularly in anti-HER2-based ADCs. A pooled analysis of phase I and II T-Dxd monotherapy studies by Powell et al., which included 1,150 patients of multiple tumour types (including breast, gastric, colorectal and lung cancer), concluded that adjudicated drug-related ILD/pneumonitis occurred in 15.4% of patients, most commonly within the first year of treatment [
84]. Practical strategies to tackle ADC treatment-related ILD, as evidenced by Rugo et al., include pre-treatment patient screening, recognising appropriate diagnostic imaging (high-resolution CT), multidisciplinary input, patient education, knowing when to suspend treatment, and appropriate steroid dosing based on the toxicity grade [
85].
These findings highlight the need for vigilant monitoring and management strategies to mitigate the risk of ILD in patients undergoing treatment with ADCs. T-Dxd, in particular, has been highlighted as an agent associated with higher prevalence of treatment-related ILD in comparison to other ADCs [
86]. Therefore, implementing these strategies may help improve patient outcomes and ensure the safe use of these promising targeted therapies.
10. ADCs in Urothelial Cancer
In recent times, ADCs have also emerged as a promising therapeutic approach for urinary tumors. Their role in prostate and renal cancers remains in the early stages of investigation, but they are currently explored in larger studies. In urinary tumours, ADCs can potentially provide a safer alternative to current standard of care systemic chemotherapy regimens, for patients with compromised renal function, due to their ability to minimise off-target effects [
87]. The targets of ADCs for urothelial carcinoma are mainly the three membrane proteins: HER-2, TROP2, and Nectin-4 [
88].
Practice changing enfortumab vedotin (EV) plus pembrolizumab was investigated in the phase III EV-302 trial, which randomised 886 patients with previously untreated locally advanced or metastatic urothelial carcinoma to either EV plus pembrolizumab or gemcitabine in combination with either cisplatin or carboplatin [
89]. After a median follow-up of 17.2 months, the median PFS was significantly longer with EV plus pembrolizumab compared to chemotherapy (12.5 months vs. 6.3 months; HR, 0.45; 95% CI, 0.38–0.54; P < .001). The median OS was also significantly longer with EV plus pembrolizumab (31.5 months vs. 16.1 months; HR, 0.47; 95% CI, 0.38– 0.58; < .001). Confirmed ORR was 67.7% and 44.4% for EV plus pembrolizumab and chemotherapy, respectively (P < .001), with complete responses (CRs) observed in 29.1% of patients in the EV plus pembrolizumab group.
Sacituzumab govitecan is another antibody–drug conjugate composed of an anti-Trop-2 humanised monoclonal antibody coupled to SN-38, the active metabolite of the topoisomerase 1 inhibitor irinotecan [
90]. At a median follow-up of 9.1 months, ORR was 27% (95% CI, 19.5%–36.6%) and 77% of participants showed a decrease in measurable disease (in patients with locally advanced unresectable or metastatic urothelial cancer). The median DOR was 7.2 months (95% CI, 4.7–8.6 months), median PFS was 5.4 months (95% CI, 3.5– 7.2 months), and median OS was 10.9 months (95% CI, 9.0–13.8 months) [
90]. T-Dxd data was also reviewed for patients with bladder cancer as part of DESTINY-Pan-tumour02 trial [
91].
11. Use of T-Dxd in a Pan-Tumour Trial
As evidenced in
Figure 1,
HER2 mutations can be found in up to 15% of patients with iCCA, 16% of those with GBC, and 11% of those with eCCA. Given the promising outcomes following the use of ADCs in breast and lung cancer, these therapies are now being investigated in other tumour types harbouring
HER2 alterations.
It is worth noting the differences between HER2 overexpression (or amplification) and
HER2 mutations, particularly in the context of treatment with ADCs. HER2 overexpression refers to excess production of the HER2 protein on the cell surface due to gene amplification, thereby resulting in an abnormally high number of HER2 receptors on the surface of the cancer cells [
92,
93]. Therefore, ADCs such as T-Dxd utilise their antibody component to specifically target these cells with high HER2 expression allowing internalisation and delivery of the cytotoxic payload. HER2 overexpression can be identified through methods such IHC which measures the protein overexpression or fluorescence in-situ hybridisation (FISH) which measures the number of HER2 gene copies in the cancer cells [
93,
94].
HER2 mutation refers to specific changes in the DNA sequence of the
HER2 gene that can lead to a permanent activation of the HER2 protein, even without gene amplification. Although these mutations may not cause overexpression of the protein, they are still a driving factor for signalling pathways associated with carcinogenesis [
95]. ADCs may be effective in this context if there is a high enough level of the mutant HER2 protein expressed on the cell surface, that the antibody component can target. Furthermore, some mutations can affect the binding affinity of the ADC which can diminish their efficacy [
96]. Therefore, ADC treatment in cancers with
HER2 mutations are more variable and depend on the specific nature of the mutation.
HER2 mutations can be identified through methods such as next-generation sequencing (NGS), which can detect specific mutations in the sequence of the
HER2 gene (point mutations, deletions etc) [
97,
98]. It can also be identified through use of polymerase chain reaction (PCR) based assays that target known mutations in the
HER2 gene [
97].
The DESTINY-PanTumor02 trial was an open-label, multicentre, phase II study that assessed the efficacy and safety profile of T-Dxd in HER2-overexpressing solid tumours. Patients recruited included those with histologically confirmed locally advanced or metastatic solid HER2-overexpressing (immunohistochemistry +2/+3) tumours across seven different disease groups, including BTCs (n=41), that had progressed or were refractory to alternative systemic treatment options (including prior HER2 therapy). Of the 267 patients included, 99 achieved tumour response, corresponding to an ORR of 37%. In the BTC cohort, the ORR was 22% (95% confidence interval, 10.6-37.6). Notably, those with HER2 IHC +3 expression across all disease groups achieved the longest DOR, PFS and OS, with an ORR of 56.3% and a median OS of 12.4 months in the BTC cohort [
91]. Another phase II trial also analysed the use of T-Dxd in HER2-expressing BTCs, suggesting this may be a promising targeted therapy for the future [
99].
A phase I study presented at the American Society of Clinical Oncology (ASCO) meeting in 2024 showed promising preliminary results for the ADC IBI343 in patients with Claudin 18.2-expressing advanced pancreatic ductal adenocarcinoma (PDAC) and BTCs that were intolerant or refractory to standard treatments [
100]. In this study, 28 patients with PDAC and 7 patients with BTCs were included. Seven patients achieved a partial response (PDAC n=5, BTC n=2), with an ORR of 38.5% (95% confidence interval, 13.9-68.4) and a disease control rate (DCR) of 84.6% (95% confidence interval, 54.6-98.1). Treatment-related adverse events (TRAEs) occurred in 80% of patients, although only 25% experienced grade 3 or higher TRAEs. Overall, this study highlighted promising efficacy and tolerability profiles for IBI343, prompting further larger population studies.
ADCs are associated with several potential side effects, including haematological toxicities, nausea, vomiting, diarrhoea and less commonly ocular toxicities or ILD [
101]. Side effects caused by ADCs can be explained by different mechanisms including the type of payload (hydrophobic versus hydrophilic), type of linker (cleavable versus non-cleavable), and drug-to-antibody ratio (DAR). The "bystander effect" is a vital component of ADCs in bypassing tumour heterogeneity, but it is complicated by releasing systemic effects to non-target cells that carry the target antigen (on-target, off-tumour toxicity) [
101,
102]. Hydrophobic payloads with strong membrane penetration result in a potent bystander effect; however, this also means the drug is easily absorbed by healthy tissue, resulting in systemic side effects [
101]. Further investigation is required to ascertain the correct combination of antibody target, drug-linker, DAR, and dosing regimens to improved safety profiles of ADCs.
12. Current Trials Assessing the Use of ADCs in BTCs
Ongoing phase I and II clinical trials are currently recruiting patients with cancers including BTCs, aiming to assess the efficacy and safety of treatment with ADCs in this cohort and identifying further actionable tumour alterations (
Table 1). For example, MRG003, is an ADC comprised of an anti-epidermal growth factor receptor (EGFR) humanised immunoglobulin G1 monoclonal antibody that is conjugated with monomethyl auristatin E via a valine-citrulline linker. As evidenced in
Table 1, this ADC is being utilised in an open-label, single-arm, multicentre phase II clinical study, in the treatment of
EGFR-positive unresectable, locally advanced or metastatic BTC who have progressed during or relapsed after at least one previous standard therapy (NCT04838964). Projected enrollment for this cohort is 80 patients.
EGFR somatic mutations can be present in 4-18% of GBCs as highlighted in
figure 1, whilst EGFR amplifications are associated with poorer prognosis and occur in 19-31% of iCCA or eCCA [
103]. MRG003 has already shown encouraging outcomes, following results of another phase I trial, when used in the treatment of patients with
EGFR positive refractory advanced squamous cell carcinomas of the head and neck (SCCHN), nasopharyngeal carcinoma (NPC), and colorectal cancer (CRC) [
104]. Confirmed ORR was 40% in the cohort with SCCHN and 44% with NPC. Although a small sample size (n=61), the promising anti-tumour effects highlighted in this study as well as the acceptable safety profile, are promising, and it is hoped that these outcomes can be replicated in the BTC trial (NCT0483894).
AZD8205 is another ADC comprised of human anti-B7-H4 antibody conjugated via a chemical linker to a topoisomerase I inhibitor payload. As evidenced in
Table 1, it is being investigated in an open-label, multicentre phase I/IIa trial as monotherapy or in combination with other anti-cancer agents, in patients with advanced or metastatic solid tumours including breast, endometrial, ovarian and BTCs (NCT051203482). Estimated enrollment for this study is 340 patients. B7-H4 is overexpressed in multiple tumour types and known to negatively regulate T cell mediated anti-tumour immune response [
105,
106]. Analysis of tumour samples using western blotting and quantitative real-time PCR in patients with iCCA, highlighted higher levels of B7-H4 expression compared to peri-tumoural tissues. Furthermore, high B7-H4 expression in these tumour samples were associated with lymph node metastasis, advanced tumour stage and poorer differentiation, with shorter OS and disease-free survival in this cohort of patients [
105]. Therefore, this may be an additional targetable tumour alteration in BTC (NCT051203482).
Datopotamab deruxtecan (Dato-Dxd) is an ADC comprised of a trophoblast cell surface antigen 2 (TROP2)-directed monoclonal antibody linked to the topoisomerase I inhibitor payload deruxtecan via a cleavable linker. As evidenced in
Table 1, it is being investigated in an open-label, multicentre phase II trial as monotherapy or in combination with other anti-cancer agents, in patients with advanced or metastatic solid tumours including BTCs, colorectal, endometrial, gastric, ovarian, prostate and urothelial cancers (NCT05849211). Estimated enrollment for this study is 582 patients. TROP2 over-expression in GBC tumour samples has been associated with promotion of cell proliferation, clone formation, invasion and migration in-vitro through regulation of the phosphoinositide-3-kinase–protein kinase B/Akt (PI3K-PKB/Akt) pathway [
107]. Dato-Dxd has a DAR of 4, allowing for a wider therapeutic window [
108]. It has resulted in encouraging outcomes in the open-label, randomised, phase III TROPION-lung01 trial, in patients with advanced non-small cell lung cancer with an actionable genetic alteration, assigned to treatment with Dato-Dxd or docetaxel (DTX)[
109]. Patients treated with Dato-Dxd achieved superior ORR (26.4% versus 12.8%), and treatment duration [4.2 months (range 0.7-18.3 months) versus 2.8 months (range 0.7-18.9 months)] when compared to DTX.
It is uncertain if other molecular alterations will be investigated as potential targets for ADC development in the future. As highlighted in
figure 1, other alterations such as
TP53,
KRAS and
ARID1A which are more commonly associated with BTC tumours, may be targets of interest in future ADC development.
TP53 and
KRAS are well-known oncogenes, and their mutations are common in aggressive cancers like BTC.
KRAS mutations are found in approximately 90% of patients with metastatic PDAC, specifically
KRAS G12D and
KRAS G12V comprising the majority of these identified mutations[
110]. KRAS G12D directly drives expression of the glycoprotein, intracellular adhesion molecule 1 (ICAM1), which is abnormally overexpressed in a variety of cancers including PDACs[
111,
112]. One particular pre-clinical study has shown promising results in targeting this pathway by utilizing an ADC called ICAM1-DM1. Use of this ADC demonstrated significant regression in tumour growth and metastasis when examined on an orthotopic pancreatic cancer model[
113]. Future trials may explore
ARID1A mutations as a target, which are involved in chromatin remodeling, and are increasingly recognised in BTCs, especially intrahepatic cholangiocarcinoma.
It is hoped that outcome data from the ongoing trials utilising ADCs in the treatment of patients with BTC, may help identify key components that drive the efficacy e.g charge of the payload (discussed in
Section 5 of this review). T-Dxd uses a non-charged topoisomerase I inhibitor as the payload, allowing it to be more effective in HER2-low and heterogeneous cancer cells. Future ADC development could focus on identifying other suitable payload charges. DM1 and DM4, are derivatives of the cytotoxic agent maytansine, used in ADCs like T-DM1. These payloads are neutral, which helps improve their therapeutic index by minimizing off-target binding and immune clearance, while maintaining potent cytotoxic activity via microtubule disruption. Calicheamicin, used in gemtuzumab ozogamicin (Mylotarg) for acute myeloid leukemia (AML), is another example of a neutral payload. It binds to DNA and induces double-strand breaks, leading to apoptosis. Its neutral charge aids in targeted delivery and avoids rapid clearance from circulation [
114].
Notably, these select trials highlighted in
table 1, involve treatment of patients with BTC in the locally advanced or metastatic setting, therefore depending on the outcomes from these advanced trials, future trials may investigate the use of ADCs in the treatment of patients with BTC in the neoadjuvant or adjuvant setting. Most ongoing trials, as noted in
table 1, are primarily evaluating pharmacokinetics, safety, and efficacy as their primary endpoints. Pharmacokinetic studies help in understanding how the drug is absorbed, distributed, metabolised, and excreted, while safety profiles and efficacy data will establish the therapeutic window and benefit-risk ratio of each ADC in BTC patients. Currently, T-DXd is the only ADC approved by the FDA for the treatment of unresectable or metastatic HER2-positive BTC. The paucity of outcome and safety data in BTC emphasizes the need for more studies to expand the clinical application of ADCs in this disease group. The trials under review are expected to provide important data on efficacy, safety and overcoming issues with resistance, potentially broadening the use of ADCs in BTC. Expanding the data on ADCs could lead to their wider adoption in BTC, not only for HER2-positive disease but possibly for other subtypes, depending on the molecular landscape and drug development.
13. Limitations and Ongoing Challenges Associated with ADCs
Despite their emergence as a useful drug class in oncology, the application of ADCs in clinical practice faces several limitations, necessitating the creation of an ideal agent that balances optimum efficacy with minimal toxicity.
Key challenges include: 1) Overcoming off-target effects, by identifying target antigens that are highly specific to cancer cells. Off-target binding can lead to damage of healthy tissues and adverse side effects. Research is ongoing to find biomarkers that are exclusively or predominantly expressed on cancer cells [
42,
115]. 2) Minimising ADC immunogenicity; immunogenic responses can reduce the efficacy of ADCs and cause unwanted immune reactions. Strategies to reduce immunogenicity include using humanised or fully human antibodies and modifying linker and payload components to reduce recognition by the immune system [
42,
115]. 3) Stability of cytotoxic payload; ensuring the cytotoxic payload remains stable during conjugation and circulation is essential. Premature release of the payload can reduce therapeutic efficacy and increase toxicity. Developing stable linker technologies that only release the payload in the target environment (e.g., the tumour microenvironment) is a key focus area [
71,
116]. 4) Optimising pharmacokinetic properties; tailoring the pharmacokinetic properties of ADCs to achieve the necessary systemic clearance and optimal tumour penetration is vital. This involves adjusting the size, charge, and other properties of the ADC to enhance its ability to reach and be retained in the tumour tissue while avoiding rapid clearance from the bloodstream [
36,
44,
96]. 5) Cost-Effectiveness; developing cost-effective ADCs is crucial for their widespread adoption and accessibility. The manufacturing process of ADCs is complex and expensive, involving the production of antibodies, cytotoxic drugs, and linkers, and the conjugation process itself. Streamlining production processes and improving efficiency may help reduce costs [
42,
71]. 6) Acquired resistance; this issue remains an emerging challenge in ADCs, as is the case with many standard chemotherapies, where tumours develop mechanisms to evade their effects over time. This resistance may have arisen from the start of treatment (de novo) or following treatment with the drug (acquired). The causes underlying ADC resistance is not fully characterised as this remains a novel form of treatment with a complex mechanism of action[
40]. Therefore, preclinical studies have hypothesised potential mechanisms of resistance that stem from each component of the ADC[
117]. Antigen downregulation: ADCs rely on the specific expression of antigens on cancer cells therefore if these tumour cells lose expression of target antigens, then ADCs may no longer effectively bind and destroy the cancer cells [
117,
118]. Altered internalisation and trafficking: ADCs must be internalized by the cancer cells for the cytotoxic payload to be released. Changes in receptor-mediated endocytosis or intracellular trafficking can prevent the drug from reaching its intended target inside the cell[
119,
120]. Drug efflux mechanisms: cancer cells can overexpress efflux transporters such as P-glycoprotein, which pump the cytotoxic payload of the ADC out of the cell, reducing its intracellular concentration and diminishing its effectiveness[
60]. Overexpression of multidrug resistance-associated protein 1 (MRP1) was demonstrated in different T-DM1 cell lines[
117]. Alterations in Payload Sensitivity: tumor cells may develop resistance to the cytotoxic drug itself. This can occur via upregulation of DNA repair mechanisms, changes in cell cycle regulation, or mutations that render the cell less susceptible to the drug’s effects[
121]. Tumor Microenvironment: the microenvironment surrounding the tumor can influence ADC efficacy. For instance, factors like hypoxia, low pH, or stromal cell interactions may affect drug release, cellular uptake, or ADC stability, potentially leading to resistance[
122,
123].
Addressing these challenges involves a multidisciplinary approach, combining advances in molecular biology, chemistry, pharmacology, and bioengineering[
71,
117].
14. Conclusions and Future Directions
Biliary tract cancers remain a challenging group of malignancies to treat, especially in advanced stages, due to their poor prognosis and limited treatment options. Despite the reliance on chemotherapy and immunotherapy as the primary treatment modalities in cases where patients are fit to receive systemic treatment, ADCs have emerged as a promising targeted therapy option. ADCs offer improved cytotoxicity, specifically against cancer cells, while potentially reducing systemic toxicities [
37].
A notable advancement in ADCs is the development of anti-HER2 ADCs, such as T-Dxd. T-Dxd has shown significant survival benefit in patients with HER2-positive solid tumours. In recognition of these benefits, the FDA granted approval in April 2024 for the use of T-Dxd in adult patients with unresectable or metastatic HER2-positive solid tumours, who have previously undergone systemic treatment and lack satisfactory alternative treatment options [
72]. In September 2023, the EMA granted approval for the use of T-Dxd as monotherapy in adult patients with unresectable or metastatic HER2-positive breast cancer who have received one or more prior anti-HER2-based regimens, and also for the treatment of adult patients with unresectable or metastatic HER2-low breast cancer who have received prior chemotherapy in the metastatic setting or developed disease recurrence during or within 6 months of completing adjuvant chemotherapy. It was also approved for the treatment of adult patients with advanced NSCLC whose tumours have an activating
HER2 (
ERBB2) mutation and who require systemic therapy following platinum-based chemotherapy with or without immunotherapy, and for adult patients with advanced HER2-positive gastric or gastro-oesophageal junction adenocarcinoma who have received a prior trastuzumab-based regimen [
124]. These approvals underscore the potential for T-Dxd to improve outcomes for patients with challenging malignancies, including BTCs.
Current trials are ongoing to explore other ADC actionable alterations in BTCs, as has been highlighted in this review. However, despite their emergence as a useful drug class in oncology, there remains certain limitations, with a pressing need to create a cost-effective agent that possesses optimum efficacy with minimal toxicity. Overall, this review has highlighted that ADCs have shown encouraging outcomes in cancer therapy, and this should lead to further research including in BTCs, where treatment options are often limited. The promising results observed with ADCs in various cancers underscore their potential as a transformative approach in oncology, warranting continued exploration and development and the need for education on management of their specific toxicities. By addressing current challenges and optimising ADC design and application, future studies could potentially improve treatment outcomes for patients with BTCs and beyond, potentially in the advanced and earlier stage settings.
Author Contributions
Conceptualisation contributed by Shaun Alexander and Mairéad G. McNamara. Methodology (
section 2) contributed by Timothy Jacobs.
Section 1,
Section 3,
Section 4,
Section 5,
Section 6,
Section 7,
Section 9,
Section 11,
Section 12,
Section 13,
table 1 and
figure 1 contributed by Shaun Alexander.
Section 10 and
figure 2 contributed by Umair Aleem. Writing—review and editing contributed by Shaun Alexander, Umair Aleem, Melissa Frizziero, Victoria Foy, Richard A. Hubner, Mairéad G. McNamara. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
SA. received speaker honoraria from Novartis. MMN. received research grant support from Astra Zeneca, Servier, Ipsen and NuCana. She received travel and accommodation support from Bayer and Ipsen and speaker honoraria from Pfizer, Ipsen, NuCana, Mylan and AAA. She served on advisory boards for Celgene, Ipsen, Sirtex, Baxalta, Incyte and Astra Zeneca; all outside of the scope of this work. R.H. served on advisory boards for Roche, BMS, Eisai, Celgene, Beigene, Ipsen, BTG. He received speaker fees from Eisai, Ipsen, Mylan, PrimeOncology and received travel and educational support from Bayer, BMS and Roche; all outside of the scope of this work. MF. Received honoraria and travel and accommodation support from AAA/Novartis, and travel and accommodation support from Roche; all are outside the scope of this work. VF-has received travel and educational support from Servier, Ipsen and AstraZeneca. U.A and T.J declare no conflict of interest.
References
- Bridgewater, J.A.; Goodman, K.A.; Kalyan, A.; Mulcahy, M.F. Biliary Tract Cancer: Epidemiology, Radiotherapy, and Molecular Profiling. American Society of Clinical Oncology Educational Book 2016, e194–e203. [Google Scholar] [CrossRef]
- Vogel, A.; Bridgewater, J.; Edeline, J.; Kelley, R.K.; Klümpen, H.J.; Malka, D.; Primrose, J.N.; Rimassa, L.; Stenzinger, A.; Valle, J.W.; et al. Biliary Tract Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Annals of Oncology 2023, 34, 127–140. [Google Scholar] [CrossRef]
- Baria, K.; De Toni, E.N.; Yu, B.; Jiang, Z.; Kabadi, S.M.; Malvezzi, M. Worldwide Incidence and Mortality of Biliary Tract Cancer. Gastro Hep Advances 2022, 1, 618–626. [Google Scholar] [CrossRef]
- Nghiem, V.; Wood, S.; Ramachandran, R.; Williams, G.; Outlaw, D.; Paluri, R.; Kim, Y.; Gbolahan, O. Short- and Long-Term Survival of Metastatic Biliary Tract Cancer in the United States From 2000 to 2018. Cancer Control 2023, 30. [Google Scholar] [CrossRef]
- Kang, M.J.; Lim, J.; Han, S.-S.; Park, H.M.; Kim, S.-W.; Won, Y.-J.; Park, S.-J. Distinct Prognosis of Biliary Tract Cancer According to Stage, Treatment and Tumor Location: A Population-Based Study. HPB 2022, 24, S468–S469. [Google Scholar] [CrossRef]
- Primrose, J.N.; Fox, R.P.; Palmer, D.H.; Malik, H.Z.; Prasad, R.; Mirza, D.; Anthony, A.; Corrie, P.; Falk, S.; Finch-Jones, M.; et al. Capecitabine Compared with Observation in Resected Biliary Tract Cancer (BILCAP): A Randomised, Controlled, Multicentre, Phase 3 Study. Lancet Oncol 2019, 20, 663–673. [Google Scholar] [CrossRef]
- Rizzo, A.; Brandi, G. BILCAP Trial and Adjuvant Capecitabine in Resectable Biliary Tract Cancer: Reflections on a Standard of Care. Expert Rev Gastroenterol Hepatol 2021, 15, 483–485. [Google Scholar] [CrossRef] [PubMed]
- Committee for Medicinal Products for Human Use (CHMP). Available online: https://www.ema.europa.eu/en/documents/smop-initial/chmp-summary-positive-opinion-pemazyre_en.pdf (accessed on 8 June 2024).
- Abou-Alfa, G.K.; Macarulla, T.; Javle, M.M.; Kelley, R.K.; Lubner, S.J.; Adeva, J.; Cleary, J.M.; Catenacci, D. V; Borad, M.J.; Bridgewater, J.; et al. Ivosidenib in IDH1-Mutant, Chemotherapy-Refractory Cholangiocarcinoma (ClarIDHy): A Multicentre, Randomised, Double-Blind, Placebo-Controlled, Phase 3 Study. Lancet Oncol 2020, 21, 796–807. [Google Scholar] [CrossRef]
- Tibsovo; European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/tibsovo (accessed on 8 June 2024).
- FDA Approves Ivosidenib for Advanced or Metastatic Cholangiocarcinoma; FDA. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-ivosidenib-advanced-or-metastatic-cholangiocarcinoma (accessed on 8 June 2024).
- Jain, A.; Javle, M. Molecular Profiling of Biliary Tract Cancer: A Target Rich Disease. J Gastrointest Oncol 2016, 7, 797–803. [Google Scholar] [CrossRef]
- Arai, Y.; Totoki, Y.; Hosoda, F.; Shirota, T.; Hama, N.; Nakamura, H.; Ojima, H.; Furuta, K.; Shimada, K.; Okusaka, T.; et al. Fibroblast Growth Factor Receptor 2 Tyrosine Kinase Fusions Define a Unique Molecular Subtype of Cholangiocarcinoma. Hepatology 2014, 59, 1427–1434. [Google Scholar] [CrossRef]
- Boscoe, A.N.; Rolland, C.; Kelley, R.K. Frequency and Prognostic Significance of Isocitrate Dehydrogenase 1 Mutations in Cholangiocarcinoma: A Systematic Literature Review. J Gastrointest Oncol 2019, 10, 751–765. [Google Scholar] [CrossRef]
- Gu, Y.F.; Lin, F.P.; Epstein, R.J. How Aging of the Global Population Is Changing Oncology. Ecancermedicalscience 2021, 15, ed119. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wei, W.; Xu, H. Drug Discovery Is an Eternal Challenge for the Biomedical Sciences. Acta Materia Medica 2022, 1. [Google Scholar] [CrossRef]
- Valle, J.; Wasan, H.; Palmer, D.H.; Cunningham, D.; Anthoney, A.; Maraveyas, A.; Madhusudan, S.; Iveson, T.; Hughes, S.; Pereira, S.P.; et al. Cisplatin plus Gemcitabine versus Gemcitabine for Biliary Tract Cancer. New England Journal of Medicine 2010, 362, 1273–1281. [Google Scholar] [CrossRef]
- Li, J.; Gu, A.; Nong, X.; Zhai, S.; Yue, Z.; Li, M.; Liu, Y. Six-Membered Aromatic Nitrogen Heterocyclic Anti-Tumor Agents: Synthesis and Applications. The Chemical Record 2023, 23. [Google Scholar] [CrossRef] [PubMed]
- Lamarca, A.; Edeline, J.; Goyal, L. How I Treat Biliary Tract Cancer. ESMO Open 2022, 7, 100378. [Google Scholar] [CrossRef]
- Kim, J.W.; Suh, K.J.; Kim, J.-W.; Park, J.H.; Kim, K.H.; Kim, Y.J.; Kim, J.-S.; Kim, J.H.; Choi, I.S. A Randomized Phase II Study of Oxaliplatin/5-FU (MFOLFOX) versus Irinotecan/5-FU (MFOLFIRI) Chemotherapy in Locally Advanced or Metastatic Biliary Tract Cancer Refractory to First-Line Gemcitabine/Cisplatin Chemotherapy. Journal of Clinical Oncology 2020, 38, 4603–4603. [Google Scholar] [CrossRef]
- Yoo, C.; Kim, K.; Jeong, J.H.; Kim, I.; Kang, M.J.; Cheon, J.; Kang, B.W.; Ryu, H.; Lee, J.S.; Kim, K.W.; et al. Liposomal Irinotecan plus Fluorouracil and Leucovorin versus Fluorouracil and Leucovorin for Metastatic Biliary Tract Cancer after Progression on Gemcitabine plus Cisplatin (NIFTY): A Multicentre, Open-Label, Randomised, Phase 2b Study. Lancet Oncol 2021, 22, 1560–1572. [Google Scholar] [CrossRef]
- Lamarca, A.; Palmer, D.H.; Wasan, H.S.; Ross, P.J.; Ma, Y.T.; Arora, A.; Falk, S.; Gillmore, R.; Wadsley, J.; Patel, K.; et al. Second-Line FOLFOX Chemotherapy versus Active Symptom Control for Advanced Biliary Tract Cancer (ABC-06): A Phase 3, Open-Label, Randomised, Controlled Trial. Lancet Oncol 2021, 22, 690–701. [Google Scholar] [CrossRef]
- Lamarca, A.; Palmer, D.; Wasan, H.S.; Ross, P.; Ma, Y.T.; Arora, A.; Falk, S.; Gillmore, R.; Wadsley, J.; Patel, K.; et al. 54MO Quality of Life (QoL) and Value of Health (V-He) in Advanced Biliary Cancers (ABC) Treated with Second-Line Active-Symptom-Control (ASC) Alone or ASC with Oxaliplatin/5-FU Chemotherapy (ASC+FOLFOX) in the Randomised Phase III, Multi-Centre, Open-Label ABC-06 Trial. Annals of Oncology 2022, 33, S564–S565. [Google Scholar] [CrossRef]
- Walter, T.; Horgan, A.M.; McNamara, M.; McKeever, L.; Min, T.; Hedley, D.; Serra, S.; Krzyzanowska, M.K.; Chen, E.; Mackay, H.; et al. Feasibility and Benefits of Second-Line Chemotherapy in Advanced Biliary Tract Cancer: A Large Retrospective Study. Eur J Cancer 2013, 49, 329–335. [Google Scholar] [CrossRef]
- Massard, C.; Michiels, S.; Ferté, C.; Le Deley, M.-C.; Lacroix, L.; Hollebecque, A.; Verlingue, L.; Ileana, E.; Rosellini, S.; Ammari, S.; et al. High-Throughput Genomics and Clinical Outcome in Hard-to-Treat Advanced Cancers: Results of the MOSCATO 01 Trial. Cancer Discov 2017, 7, 586–595. [Google Scholar] [CrossRef]
- Center for Drug Evaluation and Research. FDA Grants Accelerated Approval to Pemigatinib for Cholangiocarcinoma, U.S. Food and Drug Administration, Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-pemigatinib-cholangiocarcinoma-fgfr2-rearrangement-or-fusion (accessed on 8 June 2024).
- Vogel, A.; Sahai, V.; Hollebecque, A.; Vaccaro, G.; Melisi, D.; Al-Rajabi, R.; Paulson, A.S.; Borad, M.J.; Gallinson, D.; Murphy, A.G.; et al. FIGHT-202: A Phase II Study of Pemigatinib in Patients (Pts) with Previously Treated Locally Advanced or Metastatic Cholangiocarcinoma (CCA). Annals of Oncology 2019, 30, v876. [Google Scholar] [CrossRef]
- Zhu, A.X.; Macarulla, T.; Javle, M.M.; Kelley, R.K.; Lubner, S.J.; Adeva, J.; Cleary, J.M.; Catenacci, D.V.T.; Borad, M.J.; Bridgewater, J.A.; et al. Final Results from ClarIDHy, a Global, Phase III, Randomized, Double-Blind Study of Ivosidenib (IVO) versus Placebo (PBO) in Patients (Pts) with Previously Treated Cholangiocarcinoma (CCA) and an Isocitrate Dehydrogenase 1 ( IDH1 ) Mutation. Journal of Clinical Oncology 2021, 39, 266–266. [Google Scholar] [CrossRef]
- Chakrabarti, S.; Kamgar, M.; Mahipal, A. Targeted Therapies in Advanced Biliary Tract Cancer: An Evolving Paradigm. Cancers (Basel) 2020, 12, 2039. [Google Scholar] [CrossRef]
- Valery, M.; Vasseur, D.; Fachinetti, F.; Boilève, A.; Smolenschi, C.; Tarabay, A.; Antoun, L.; Perret, A.; Fuerea, A.; Pudlarz, T.; et al. Targetable Molecular Alterations in the Treatment of Biliary Tract Cancers: An Overview of the Available Treatments. Cancers (Basel) 2023, 15, 4446. [Google Scholar] [CrossRef]
- Farha, N.; Dima, D.; Ullah, F.; Kamath, S. Precision Oncology Targets in Biliary Tract Cancer. Cancers (Basel) 2023, 15, 2105. [Google Scholar] [CrossRef]
- DiPeri, T.P.; Javle, M.M.; Meric-Bernstam, F. Next Generation Sequencing for Biliary Tract Cancers. Expert Rev Gastroenterol Hepatol 2021, 15, 471–474. [Google Scholar] [CrossRef]
- Wu, C.-E.; Pan, Y.-R.; Yeh, C.-N.; Lunec, J. Targeting P53 as a Future Strategy to Overcome Gemcitabine Resistance in Biliary Tract Cancers. Biomolecules 2020, 10, 1474. [Google Scholar] [CrossRef]
- Zahavi, D.; Weiner, L. Monoclonal Antibodies in Cancer Therapy. Antibodies 2020, 9, 34. [Google Scholar] [CrossRef]
- Song, C.H.; Jeong, M.; In, H.; Kim, J.H.; Lin, C.-W.; Han, K.H. Trends in the Development of Antibody-Drug Conjugates for Cancer Therapy. Antibodies 2023, 12, 72. [Google Scholar] [CrossRef]
- Fu, Z.; Li, S.; Han, S.; Shi, C.; Zhang, Y. Antibody Drug Conjugate: The “Biological Missile” for Targeted Cancer Therapy. Signal Transduct Target Ther 2022, 7, 93. [Google Scholar] [CrossRef]
- Wolff, A.C.; Hammond, M.E.H.; Allison, K.H.; Harvey, B.E.; McShane, L.M.; Dowsett, M. HER2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update Summary. J Oncol Pract 2018, 14, 437–441. [Google Scholar] [CrossRef]
- Hunter, F.W.; Barker, H.R.; Lipert, B.; Rothé, F.; Gebhart, G.; Piccart-Gebhart, M.J.; Sotiriou, C.; Jamieson, S.M.F. Mechanisms of Resistance to Trastuzumab Emtansine (T-DM1) in HER2-Positive Breast Cancer. Br J Cancer 2020, 122, 603–612. [Google Scholar] [CrossRef]
- Trastuzumab Emtansine for Treating HER2-Positive Advanced Breast Cancer after Trastuzumab and a Taxane. Available online: https://www.nice.org.uk/guidance/ta458 (accessed on 22 July 2024).
- Khongorzul, P.; Ling, C.J.; Khan, F.U.; Ihsan, A.U.; Zhang, J. Antibody–Drug Conjugates: A Comprehensive Review. Molecular Cancer Research 2020, 18, 3–19. [Google Scholar] [CrossRef]
- Marei, H.E.; Cenciarelli, C.; Hasan, A. Potential of Antibody–Drug Conjugates (ADCs) for Cancer Therapy. Cancer Cell Int 2022, 22, 255. [Google Scholar] [CrossRef]
- Nguyen, T.D.; Bordeau, B.M.; Balthasar, J.P. Mechanisms of ADC Toxicity and Strategies to Increase ADC Tolerability. Cancers (Basel) 2023, 15, 713. [Google Scholar] [CrossRef]
- Lucas, A.; Price, L.; Schorzman, A.; Storrie, M.; Piscitelli, J.; Razo, J.; Zamboni, W. Factors Affecting the Pharmacology of Antibody–Drug Conjugates. Antibodies 2018, 7, 10. [Google Scholar] [CrossRef]
- Wang, Z.; Li, H.; Gou, L.; Li, W.; Wang, Y. Antibody–Drug Conjugates: Recent Advances in Payloads. Acta Pharm Sin B 2023, 13, 4025–4059. [Google Scholar] [CrossRef]
- Dean, A.Q.; Luo, S.; Twomey, J.D.; Zhang, B. Targeting Cancer with Antibody-Drug Conjugates: Promises and Challenges. MAbs 2021, 13. [Google Scholar] [CrossRef]
- Widdison, W.C.; Chari, R.V.J. Factors Involved in the Design of Cytotoxic Payloads for Antibody–Drug Conjugates. In Antibody-Drug Conjugates and Immunotoxins; Springer New York: New York, NY, 2013; pp. 93–115. [Google Scholar]
- Conilh, L.; Sadilkova, L.; Viricel, W.; Dumontet, C. Payload Diversification: A Key Step in the Development of Antibody–Drug Conjugates. J Hematol Oncol 2023, 16, 3. [Google Scholar] [CrossRef] [PubMed]
- Mecklenburg, L. A Brief Introduction to Antibody–Drug Conjugates for Toxicologic Pathologists. Toxicol Pathol 2018, 46, 746–752. [Google Scholar] [CrossRef]
- Tsuchikama, K.; An, Z. Antibody-Drug Conjugates: Recent Advances in Conjugation and Linker Chemistries. Protein Cell 2018, 9, 33–46. [Google Scholar] [CrossRef]
- Henry, N.L.; Hayes, D.F. Cancer Biomarkers. Mol Oncol 2012, 6, 140–146. [Google Scholar] [CrossRef]
- Das, S.; Dey, M.K.; Devireddy, R.; Gartia, M.R. Biomarkers in Cancer Detection, Diagnosis, and Prognosis. Sensors 2023, 24, 37. [Google Scholar] [CrossRef]
- Eberly, H.W.; Sciscent, B.Y.; Lorenz, F.J.; Rettig, E.M.; Goyal, N. Current and Emerging Diagnostic, Prognostic, and Predictive Biomarkers in Head and Neck Cancer. Biomedicines 2024, 12, 415. [Google Scholar] [CrossRef]
- Califf, R.M. Biomarker Definitions and Their Applications. Exp Biol Med 2018, 243, 213–221. [Google Scholar] [CrossRef]
- Jin, T.Y.; Park, K.S.; Nam, S.E.; Yoo, Y.B.; Park, W.S.; Yun, I.J. BRCA1/2 Serves as a Biomarker for Poor Prognosis in Breast Carcinoma. Int J Mol Sci 2022, 23, 3754. [Google Scholar] [CrossRef]
- Jóhannsson, O.T.; Ranstam, J.; Borg, A.; Olsson, H. Survival of BRCA1 Breast and Ovarian Cancer Patients: A Population-Based Study from Southern Sweden. Journal of Clinical Oncology 1998, 16, 397–404. [Google Scholar] [CrossRef]
- Chetrit, A.; Hirsh-Yechezkel, G.; Ben-David, Y.; Lubin, F.; Friedman, E.; Sadetzki, S. Effect of BRCA1/2 Mutations on Long-Term Survival of Patients With Invasive Ovarian Cancer: The National Israeli Study of Ovarian Cancer. Journal of Clinical Oncology 2008, 26, 20–25. [Google Scholar] [CrossRef]
- Patani, N.; Martin, L.-A.; Dowsett, M. Biomarkers for the Clinical Management of Breast Cancer: International Perspective. Int J Cancer 2013, 133, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Blanquisett, A.; Touya, D.; Strasser-Weippl, K.; Ruiz, R.; St. Louis, J.; Goss, P. Current and Emerging Therapies of HER2-Positive Metastatic Breast Cancer. The Breast 2016, 29, 170–177. [Google Scholar] [CrossRef]
- Bussing, D.; Sharma, S.; Li, Z.; Meyer, L.F.; Shah, D.K. Quantitative Evaluation of the Effect of Antigen Expression Level on Antibody–Drug Conjugate Exposure in Solid Tumor. AAPS J 2021, 23, 56. [Google Scholar] [CrossRef]
- Cheng, X. A Comprehensive Review of HER2 in Cancer Biology and Therapeutics. Genes (Basel) 2024, 15, 903. [Google Scholar] [CrossRef]
- De Matos, L.L.; Trufelli, D.C.; De Matos, M.G.L.; Da Silva Pinhal, M.A. Immunohistochemistry as an Important Tool in Biomarkers Detection and Clinical Practice. Biomark Insights 2010, 5, BMI–S2185. [Google Scholar] [CrossRef]
- Colomer, R.; Mondejar, R.; Romero-Laorden, N.; Alfranca, A.; Sanchez-Madrid, F.; Quintela-Fandino, M. When Should We Order a next Generation Sequencing Test in a Patient with Cancer? EClinicalMedicine 2020, 25, 100487. [Google Scholar] [CrossRef]
- Bosi, C.; Bartha, Á.; Galbardi, B.; Notini, G.; Naldini, M.M.; Licata, L.; Viale, G.; Mariani, M.; Pistilli, B.; Ali, H.R.; et al. Pan-Cancer Analysis of Antibody-Drug Conjugate Targets and Putative Predictors of Treatment Response. Eur J Cancer 2023, 195, 113379. [Google Scholar] [CrossRef]
- FDA Approves Fam-Trastuzumab Deruxtecan-Nxki for HER2-Low Breast Cancer Available online: FDA approves fam-trastuzumab deruxtecan-nxki for HER2-low breast cancer (accessed on 20 July 2024).
- Modi, S.; Jacot, W.; Yamashita, T.; Sohn, J.; Vidal, M.; Tokunaga, E.; Tsurutani, J.; Ueno, N.T.; Prat, A.; Chae, Y.S.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. New England Journal of Medicine 2022, 387, 9–20. [Google Scholar] [CrossRef]
- Strebhardt, K.; Ullrich, A. Paul Ehrlich’s Magic Bullet Concept: 100 Years of Progress. Nat Rev Cancer 2008, 8, 473–480. [Google Scholar] [CrossRef]
- Köhler, G.; Milstein, C. Continuous Cultures of Fused Cells Secreting Antibody of Predefined Specificity. Nature 1975, 256, 495–497. [Google Scholar] [CrossRef]
- Trail, P.A.; Willner, D.; Lasch, S.J.; Henderson, A.J.; Hofstead, S.; Casazza, A.M.; Firestone, R.A.; Hellström, I.; Hellström, K.E. Cure of Xenografted Human Carcinomas by BR96-Doxorubicin Immunoconjugates. Science (1979) 1993, 261, 212–215. [Google Scholar] [CrossRef]
- Petersen, B.H.; DeHerdt, S. V; Schneck, D.W.; Bumol, T.F. The Human Immune Response to KS1/4-Desacetylvinblastine (LY256787) and KS1/4-Desacetylvinblastine Hydrazide (LY203728) in Single and Multiple Dose Clinical Studies. Cancer Res 1991, 51, 2286–2290. [Google Scholar]
- Norsworthy, K.J.; Ko, C.-W.; Lee, J.E.; Liu, J.; John, C.S.; Przepiorka, D.; Farrell, A.T.; Pazdur, R. FDA Approval Summary: Mylotarg for Treatment of Patients with Relapsed or Refractory CD33-Positive Acute Myeloid Leukemia. Oncologist 2018, 23, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Sasso, J.M.; Tenchov, R.; Bird, R.; Iyer, K.A.; Ralhan, K.; Rodriguez, Y.; Zhou, Q.A. The Evolving Landscape of Antibody–Drug Conjugates: In Depth Analysis of Recent Research Progress. Bioconjug Chem 2023, 34, 1951–2000. [Google Scholar] [CrossRef]
- Center for Drug Evaluation and Research. FDA Grants Accelerated Approval to Fam-Trastuzumab Deruxtecan-Nxki for, U.S. Food and Drug Administration, n.d. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-fam-trastuzumab-deruxtecan-nxki-unresectable-or-metastatic-her2 (accessed on 20 July 2024).
- Nakada, T. Discovery Research and Translation Science of Trastuzumab Deruxtecan, from Non-Clinical Study to Clinical Trial. Translational and Regulatory Sciences 2021, 3, 2021–010. [Google Scholar] [CrossRef]
- Martín, M.; Pandiella, A.; Vargas-Castrillón, E.; Díaz-Rodríguez, E.; Iglesias-Hernangómez, T.; Martínez Cano, C.; Fernández-Cuesta, I.; Winkow, E.; Perelló, M.F. Trastuzumab Deruxtecan in Breast Cancer. Crit Rev Oncol Hematol 2024, 198, 104355. [Google Scholar] [CrossRef]
- Ogitani, Y.; Aida, T.; Hagihara, K.; Yamaguchi, J.; Ishii, C.; Harada, N.; Soma, M.; Okamoto, H.; Oitate, M.; Arakawa, S.; et al. DS-8201a, A Novel HER2-Targeting ADC with a Novel DNA Topoisomerase I Inhibitor, Demonstrates a Promising Antitumor Efficacy with Differentiation from T-DM1. Clinical Cancer Research 2016, 22, 5097–5108. [Google Scholar] [CrossRef]
- Bailly, C. Irinotecan: 25 Years of Cancer Treatment. Pharmacol Res 2019, 148, 104398. [Google Scholar] [CrossRef]
- Wittwer, N.L.; Brown, M.P.; Liapis, V.; Staudacher, A.H. Antibody Drug Conjugates: Hitting the Mark in Pancreatic Cancer? Journal of Experimental & Clinical Cancer Research 2023, 42, 280. [Google Scholar] [CrossRef]
- Hamilton, E.P.; Bragaia, V.P.H.; Yeo, W.; Kim, S.-B.; Bianchini, G.; Yamashita, T.; Yonemori, K.; Inoue, K.; Curigliano, G.; Hurvitz, S.A.; et al. Trastuzumab Deruxtecan (T-DXd) versus Trastuzumab Emtansine (T-DM1) in Patients (Pts) with HER2-Positive (HER2+) Unresectable and/or Metastatic Breast Cancer (MBC): Safety Follow-up of the Randomized, Phase 3 Study DESTINY-Breast03. Journal of Clinical Oncology 2022, 40, 1000–1000. [Google Scholar] [CrossRef]
- FDA Grants Regular Approval to Fam-Trastuzumab Deruxtecan-Nxki for Breast Cancer. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-regular-approval-fam-trastuzumab-deruxtecan-nxki-breast-cancer (accessed on 20 July 2024).
- Modi, S.; Jacot, W.; Yamashita, T.; Sohn, J.; Vidal, M.; Tokunaga, E.; Tsurutani, J.; Ueno, N.T.; Prat, A.; Chae, Y.S.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Low Advanced Breast Cancer. New England Journal of Medicine 2022, 387, 9–20. [Google Scholar] [CrossRef]
- Smit, E.F.; Felip, E.; Uprety, D.; Nakagawa, K.; Paz-Ares, L.; Pacheco, J.; Li, B.T.; Planchard, D.; Baik, C.; Goto, Y.; et al. 975P Trastuzumab Deruxtecan in Patients (Pts) with HER2-Overexpressing (HER2-OE) Metastatic Non-Small Cell Lung Cancer (NSCLC): Results from the DESTINY-Lung01 Trial. Annals of Oncology 2022, 33, S994–S995. [Google Scholar] [CrossRef]
- Goto, K.; Goto, Y.; Kubo, T.; Ninomiya, K.; Kim, S.-W.; Planchard, D.; Ahn, M.-J.; Smit, E.F.; de Langen, A.J.; Pérol, M.; et al. Trastuzumab Deruxtecan in Patients With HER2 -Mutant Metastatic Non–Small-Cell Lung Cancer: Primary Results From the Randomized, Phase II DESTINY-Lung02 Trial. Journal of Clinical Oncology 2023, 41, 4852–4863. [Google Scholar] [CrossRef]
- Interstitial Lung Disease/Pneumonitis: ENHERTU® (FAM-Trastuzumab Deruxtecan-Nxki), n.d. ENHERTU®. Available online: https://www.enhertuhcp.com/en/managing-adverse-reactions/interstitial-lung-disease-pneumonitis (accessed on 20 July 2024).
- Powell, C.A.; Modi, S.; Iwata, H.; Takahashi, S.; Smit, E.F.; Siena, S.; Chang, D.-Y.; Macpherson, E.; Qin, A.; Singh, J.; et al. Pooled Analysis of Drug-Related Interstitial Lung Disease and/or Pneumonitis in Nine Trastuzumab Deruxtecan Monotherapy Studies. ESMO Open 2022, 7, 100554. [Google Scholar] [CrossRef]
- Rugo, H.S.; Crossno, C.L.; Gesthalter, Y.B.; Kelley, K.; Moore, H.N.; Rimawi, M.F.; Westbrook, K.E.; Buys, S.S. Real-World Perspectives and Practices for Pneumonitis/Interstitial Lung Disease Associated With Trastuzumab Deruxtecan Use in Human Epidermal Growth Factor Receptor 2–Expressing Metastatic Breast Cancer. JCO Oncol Pract 2023, 19, 539–546. [Google Scholar] [CrossRef]
- Zhu, Z.; Shen, G.; Li, J.; Qiu, T.; Fang, Q.; Zheng, Y.; Xin, Y.; Liu, Z.; Zhao, F.; Ren, D.; et al. Incidence of Antibody–Drug Conjugates-Related Pneumonitis in Patients with Solid Tumors: A Systematic Review and Meta-Analysis. Crit Rev Oncol Hematol 2023, 184, 103960. [Google Scholar] [CrossRef]
- Li, K.; Xie, G.; Deng, X.; Zhang, Y.; Jia, Z.; Huang, Z. Antibody-Drug Conjugates in Urinary Tumors: Clinical Application, Challenge, and Perspectives. Front Oncol 2023, 13. [Google Scholar] [CrossRef]
- Ungaro, A.; Tucci, M.; Audisio, A.; Di Prima, L.; Pisano, C.; Turco, F.; Delcuratolo, M.D.; Di Maio, M.; Scagliotti, G.V.; Buttigliero, C. Antibody-Drug Conjugates in Urothelial Carcinoma: A New Therapeutic Opportunity Moves from Bench to Bedside. Cells 2022, 11, 803. [Google Scholar] [CrossRef]
- Powles, T.; Valderrama, B.P.; Gupta, S.; Bedke, J.; Kikuchi, E.; Hoffman-Censits, J.; Iyer, G.; Vulsteke, C.; Park, S.H.; Shin, S.J.; et al. Enfortumab Vedotin and Pembrolizumab in Untreated Advanced Urothelial Cancer. New England Journal of Medicine 2024, 390, 875–888. [Google Scholar] [CrossRef]
- Tagawa, S.T.; Balar, A. V.; Petrylak, D.P.; Kalebasty, A.R.; Loriot, Y.; Fléchon, A.; Jain, R.K.; Agarwal, N.; Bupathi, M.; Barthelemy, P.; et al. TROPHY-U-01: A Phase II Open-Label Study of Sacituzumab Govitecan in Patients With Metastatic Urothelial Carcinoma Progressing After Platinum-Based Chemotherapy and Checkpoint Inhibitors. Journal of Clinical Oncology 2021, 39, 2474–2485. [Google Scholar] [CrossRef]
- Meric-Bernstam, F.; Makker, V.; Oaknin, A.; Oh, D.-Y.; Banerjee, S.; González-Martín, A.; Jung, K.H.; Ługowska, I.; Manso, L.; Manzano, A.; et al. Efficacy and Safety of Trastuzumab Deruxtecan in Patients With HER2-Expressing Solid Tumors: Primary Results From the DESTINY-PanTumor02 Phase II Trial. Journal of Clinical Oncology 2024, 42, 47–58. [Google Scholar] [CrossRef]
- Gutierrez, C.; Schiff, R. HER2: Biology, Detection, and Clinical Implications. Arch Pathol Lab Med 2011, 135, 55–62. [Google Scholar] [CrossRef]
- Rubin, E.; Shan, K.; Dalal, S.; Vu, D.; Milillo-Naraine, A.; Guaqueta, D.; Ergle, A. Molecular Targeting of the Human Epidermal Growth Factor Receptor-2 (HER2) Genes across Various Cancers. Int J Mol Sci 2024, 25, 1064. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Noske, A.; Ramach, C.; Padberg, B.; Moch, H. Assessment of HER2 Status in Breast Cancer: Overall Positivity Rate and Accuracy by Fluorescence in Situ Hybridization and Immunohistochemistry in a Single Institution over 12 Years: A Quality Control Study. BMC Cancer 2013, 13, 615. [Google Scholar] [CrossRef]
- Ayasun, R.; Ozer, M.; Sahin, I. The Role of HER2 Status in the Biliary Tract Cancers. Cancers (Basel) 2023, 15, 2628. [Google Scholar] [CrossRef]
- Lucas, A.; Price, L.; Schorzman, A.; Storrie, M.; Piscitelli, J.; Razo, J.; Zamboni, W. Factors Affecting the Pharmacology of Antibody–Drug Conjugates. Antibodies 2018, 7, 10. [Google Scholar] [CrossRef]
- Gagan, J.; Van Allen, E.M. Next-Generation Sequencing to Guide Cancer Therapy. Genome Med 2015, 7, 80. [Google Scholar] [CrossRef]
- ten Haaft, B.H.E.A.; Pedregal, M.; Prato, J.; Klümpen, H.-J.; Moreno, V.; Lamarca, A. Revolutionizing Anti-HER2 Therapies for Extrahepatic Cholangiocarcinoma and Gallbladder Cancer: Current Advancements and Future Perspectives. Eur J Cancer 2024, 199, 113564. [Google Scholar] [CrossRef]
- Ohba, A.; Morizane, C.; Kawamoto, Y.; Komatsu, Y.; Ueno, M.; Kobayashi, S.; Ikeda, M.; Sasaki, M.; Furuse, J.; Okano, N.; et al. Trastuzumab Deruxtecan (T-DXd; DS-8201) in Patients (Pts) with HER2-Expressing Unresectable or Recurrent Biliary Tract Cancer (BTC): An Investigator-Initiated Multicenter Phase 2 Study (HERB Trial). Journal of Clinical Oncology 2022, 40, 4006–4006. [Google Scholar] [CrossRef]
- Yu, X.; Zhang, J.; Tazbirkova, A.; Yang, J.; Yue, J.; Sun, Y.; Pan, Y.; Sun, M.; Qin, Y.; Shen, L.; et al. Safety and Efficacy of IBI343 (Anti-Claudin18.2 Antibody-Drug Conjugate) in Patients with Advanced Pancreatic Ductal Adenocarcinoma or Biliary Tract Cancer: Preliminary Results from a Phase 1 Study. Journal of Clinical Oncology 2024, 42, 3037–3037. [Google Scholar] [CrossRef]
- D’Arienzo, A.; Verrazzo, A.; Pagliuca, M.; Napolitano, F.; Parola, S.; Viggiani, M.; Caputo, R.; Puglisi, F.; Giuliano, M.; Del Mastro, L.; et al. Toxicity Profile of Antibody-Drug Conjugates in Breast Cancer: Practical Considerations. EClinicalMedicine 2023, 62, 102113. [Google Scholar] [CrossRef]
- Colombo, R.; Rich, J.R. The Therapeutic Window of Antibody Drug Conjugates: A Dogma in Need of Revision. Cancer Cell 2022, 40, 1255–1263. [Google Scholar] [CrossRef]
- Bogenberger, J.M.; DeLeon, T.T.; Arora, M.; Ahn, D.H.; Borad, M.J. Emerging Role of Precision Medicine in Biliary Tract Cancers. NPJ Precis Oncol 2018, 2, 21. [Google Scholar] [CrossRef] [PubMed]
- Qiu, M.-Z.; Zhang, Y.; Guo, Y.; Guo, W.; Nian, W.; Liao, W.; Xu, Z.; Zhang, W.; Zhao, H.-Y.; Wei, X.; et al. Evaluation of Safety of Treatment With Anti–Epidermal Growth Factor Receptor Antibody Drug Conjugate MRG003 in Patients With Advanced Solid Tumors. JAMA Oncol 2022, 8, 1042. [Google Scholar] [CrossRef]
- Xie, N.; Cai, J.-B.; Zhang, L.; Zhang, P.-F.; Shen, Y.-H.; Yang, X.; Lu, J.-C.; Gao, D.-M.; Kang, Q.; Liu, L.-X.; et al. Upregulation of B7-H4 Promotes Tumor Progression of Intrahepatic Cholangiocarcinoma. Cell Death Dis 2017, 8, 3205. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Guo, F.; Li, Z.; Jiang, P.; Deng, X.; Tian, F.; Li, X.; Wang, S. Aberrant Expression of B7-H4 Correlates with Poor Prognosis and Suppresses Tumor-Infiltration of CD8+ T Lymphocytes in Human Cholangiocarcinoma. Oncol Rep 2016, 36, 419–427. [Google Scholar] [CrossRef]
- Li, X.; Teng, S.; Zhang, Y.; Zhang, W.; Zhang, X.; Xu, K.; Yao, H.; Yao, J.; Wang, H.; Liang, X.; et al. TROP2 Promotes Proliferation, Migration and Metastasis of Gallbladder Cancer Cells by Regulating PI3K/AKT Pathway and Inducing EMT. Oncotarget 2017, 8, 47052–47063. [Google Scholar] [CrossRef]
- Lombardi, P.; Filetti, M.; Falcone, R.; Altamura, V.; Paroni Sterbini, F.; Bria, E.; Fabi, A.; Giannarelli, D.; Scambia, G.; Daniele, G. Overview of Trop-2 in Cancer: From Pre-Clinical Studies to Future Directions in Clinical Settings. Cancers (Basel) 2023, 15. [Google Scholar] [CrossRef]
- Ahn, M.-J.; Lisberg, A.; Paz-Ares, L.; Cornelissen, R.; Girard, N.; Pons-Tostivint, E.; Vicente Baz, D.; Sugawara, S.; Cobo Dols, M.; Pérol, M.; et al. LBA12 Datopotamab Deruxtecan (Dato-DXd) vs Docetaxel in Previously Treated Advanced/Metastatic (Adv/Met) Non-Small Cell Lung Cancer (NSCLC): Results of the Randomized Phase III Study TROPION-Lung01. Annals of Oncology 2023, 34, S1305–S1306. [Google Scholar] [CrossRef]
- Lee, J.K.; Sivakumar, S.; Schrock, A.B.; Madison, R.; Fabrizio, D.; Gjoerup, O.; Ross, J.S.; Frampton, G.M.; Napalkov, P.; Montesion, M.; et al. Comprehensive Pan-Cancer Genomic Landscape of KRAS Altered Cancers and Real-World Outcomes in Solid Tumors. NPJ Precis Oncol 2022, 6, 91. [Google Scholar] [CrossRef]
- Liou, G.-Y.; Döppler, H.; Necela, B.; Edenfield, B.; Zhang, L.; Dawson, D.W.; Storz, P. Mutant KRAS–Induced Expression of ICAM-1 in Pancreatic Acinar Cells Causes Attraction of Macrophages to Expedite the Formation of Precancerous Lesions. Cancer Discov 2015, 5, 52–63. [Google Scholar] [CrossRef]
- Benedicto, A.; Romayor, I.; Arteta, B. Role of Liver ICAM-1 in Metastasis. Oncol Lett 2017, 14, 3883–3892. [Google Scholar] [CrossRef]
- Huang, J.; Agoston, A.T.; Guo, P.; Moses, M.A. A Rationally Designed ICAM1 Antibody Drug Conjugate for Pancreatic Cancer. Advanced Science 2020, 7. [Google Scholar] [CrossRef]
- Vollmar, B.S.; Frantz, C.; Schutten, M.M.; Zhong, F.; del Rosario, G.; Go, M.A.T.; Yu, S.-F.; Leipold, D.D.; Kamath, A. V.; Ng, C.; et al. Calicheamicin Antibody–Drug Conjugates with Improved Properties. Mol Cancer Ther 2021, 20, 1112–1120. [Google Scholar] [CrossRef]
- Kondrashov, A.; Sapkota, S.; Sharma, A.; Riano, I.; Kurzrock, R.; Adashek, J.J. Antibody-Drug Conjugates in Solid Tumor Oncology: An Effectiveness Payday with a Targeted Payload. Pharmaceutics 2023, 15. [Google Scholar] [CrossRef]
- Bosi, C.; Bartha, Á.; Galbardi, B.; Notini, G.; Naldini, M.M.; Licata, L.; Viale, G.; Mariani, M.; Pistilli, B.; Ali, H.R.; et al. Pan-Cancer Analysis of Antibody-Drug Conjugate Targets and Putative Predictors of Treatment Response. Eur J Cancer 2023, 195, 113379. [Google Scholar] [CrossRef]
- Loganzo, F.; Sung, M.; Gerber, H.-P. Mechanisms of Resistance to Antibody-Drug Conjugates. Mol Cancer Ther 2016, 15, 2825–2834. [Google Scholar] [CrossRef]
- Loganzo, F.; Tan, X.; Sung, M.; Jin, G.; Myers, J.S.; Melamud, E.; Wang, F.; Diesl, V.; Follettie, M.T.; Musto, S.; et al. Tumor Cells Chronically Treated with a Trastuzumab–Maytansinoid Antibody–Drug Conjugate Develop Varied Resistance Mechanisms but Respond to Alternate Treatments. Mol Cancer Ther 2015, 14, 952–963. [Google Scholar] [CrossRef]
- Owen, S.C.; Patel, N.; Logie, J.; Pan, G.; Persson, H.; Moffat, J.; Sidhu, S.S.; Shoichet, M.S. Targeting HER2 + Breast Cancer Cells: Lysosomal Accumulation of Anti-HER2 Antibodies Is Influenced by Antibody Binding Site and Conjugation to Polymeric Nanoparticles. Journal of Controlled Release 2013, 172, 395–404. [Google Scholar] [CrossRef]
- Sung, M.; Tan, X.; Lu, B.; Golas, J.; Hosselet, C.; Wang, F.; Tylaska, L.; King, L.; Zhou, D.; Dushin, R.; et al. Caveolae-Mediated Endocytosis as a Novel Mechanism of Resistance to Trastuzumab Emtansine (T-DM1). Mol Cancer Ther 2018, 17, 243–253. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, Y.; Shao, Z.; Yu, K. Resistance to Antibody-drug Conjugates in Breast Cancer: Mechanisms and Solutions. Cancer Commun 2023, 43, 297–337. [Google Scholar] [CrossRef]
- Chen, G.; Wu, K.; Li, H.; Xia, D.; He, T. Role of Hypoxia in the Tumor Microenvironment and Targeted Therapy. Front Oncol 2022, 12. [Google Scholar] [CrossRef]
- Hanker, A.B.; Garrett, J.T.; Estrada, M.V.; Moore, P.D.; Ericsson, P.G.; Koch, J.P.; Langley, E.; Singh, S.; Kim, P.S.; Frampton, G.M.; et al. HER2-Overexpressing Breast Cancers Amplify FGFR Signaling upon Acquisition of Resistance to Dual Therapeutic Blockade of HER2. Clinical Cancer Research 2017, 23, 4323–4334. [Google Scholar] [CrossRef]
- Enhertu, 2020; European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/enhertu (accessed on 22 July 2024).
Table 1.
Some select current phase I and II trials assessing the efficacy and safety of ADCs in BTC, which aim to analyse survival outcomes, identify further actionable biomarkers, and highlight which patient populations would most likely gain clinical benefit. .
Table 1.
Some select current phase I and II trials assessing the efficacy and safety of ADCs in BTC, which aim to analyse survival outcomes, identify further actionable biomarkers, and highlight which patient populations would most likely gain clinical benefit. .
| ID |
Title of Study |
Antibody drug conjugate |
Primary site |
Primary outcome |
Target recruitment number |
| NCT04482309 |
A Phase 2, Multicentre, Open-label Study to Evaluate the Efficacy and Safety of Trastuzumab Deruxtecan (T-DXd, DS-8201a) for the Treatment of Selected HER2 Expressing Tumours (DESTINY-PanTumor02)
|
Trastuzumab Deruxtecan |
Biliary tract, bladder, cervical, colorectal, endometrial, epithelial, gastric, non-small cell lung, ovarian, pancreatic. |
Evaluate the efficacy and safety of Trastuzumab Deruxtecan (T-DXd) for the treatment of selected HER2-expressing tumours |
468 |
| NCT04644068 |
A Modular Phase I/IIa, Open-label, Multicentre Study to Assess the Safety, Tolerability, Pharmacokinetics, Pharmacodynamics and Preliminary Efficacy of Ascending Doses of AZD5305 as Monotherapy and in Combination With Anti-cancer Agents in Patients With Advanced Solid Malignancies
|
Trastuzumab Deruxtecan |
Biliary tract, ovarian, breast, pancreatic, prostate, small cell and non-small cell lung, colorectal, bladder, gastric, cervical, endometrial |
Determine if experimental treatment with PARP inhibitor, AZD5305, alone, or in combination with anti-cancer agents is safe, tolerable, and has anti-cancer activity in patients with advanced solid tumors. |
804 |
NCT04838964
|
An Open-label, Single-arm, Multi-center, Phase II Clinical Study of MRG003 in the Treatment of Patients With EGFR-positive Unresectable, Locally Advanced or Metastatic Biliary Tract Cancer
|
MRG003 |
Advanced or metastatic biliary cancer |
Assess the safety, efficacy, pharmacokinetics, and immunogenicity of MRG003 as single agent in EGFR-positive unresectable locally advanced or metastatic biliary tract cancer patients who have progressed during or relapsed after at least one prior standard therapy. |
80 |
| NCT05123482 |
A Phase I/IIa Multi-center, Open-label Master Protocol Dose Escalation and Expansion Study of AZD8205 as Monotherapy and in Combination With Anticancer Agents in Participants With Advanced Solid Tumours (BLUESTAR)
|
AZD8205 |
Biliary tract, breast, endometrial, ovarian |
Study as a possible treatment for advanced or metastatic solid tumours alone or in combination with anti-cancer agents |
340 |
| NCT05489211 |
A Phase II, Multicentre, Open-label, Master Protocol to Evaluate the Efficacy and Safety of Datopotamab Deruxtecan (Dato-DXd) as Monotherapy and in Combination With Anticancer Agents in Patients With Advanced/Metastatic Solid Tumours
|
Datopotamab Deruxtecan |
Biliary tract, urothelial, colorectal, ovarian, endometrial, gastric, prostate |
Investigate the safety, tolerability, and anti-tumour activity of Datopotamab Deruxtecan (Dato-DXd) as Monotherapy and in Combination with Anticancer Agents in Patients with Advanced/Metastatic Solid Tumours. |
582 |
| NCT04329429 |
An Open-label, Single-arm, Multi-center, Phase II Study of RC48-ADC in Subjects With HER2 Overexpressed Locally Advanced or Metastatic Biliary Tract Cancer (BTC) Who Have Failed First-line Chemotherapy |
RC48-ADC |
Biliary tract |
Evaluate the efficacy and safety of intravenous RC48-ADC in patients with locally advanced or metastatic HER2 overexpressed biliary tract cancer who have failed first-line chemotherapy. |
57
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).