Atrial fibrillation (AF) is the most common arrhythmia, representing approximately 42% to 70% of all arrhythmias [
1]. Globally, AF is positively associated with increasing mortality and disability rates. The latest data shows that 6 million people worldwide were disabled due to AF in 2017, accounting for 0. 24% of the new disabled population this year[
2]. In China, it is estimated that by 2050, approximately 5.2 million men and 3.1 million women over the age of 60 will be affected by AF, a figure approximately 2.3 times higher than the projected prevalence in the United States [
3]. The lifetime risk of developing AF for individuals over the age of 40 is 23% for women and 26% for men. AF is associated with a two-fold increase in all-cause mortality among women and a 1.5-fold increase among men[
4,
5]. The primary causes of death include progressive heart failure, cardiac arrest, and stroke [
6]. AF can also lead to various other serious complications. For instance, the risk of ischemic stroke in patients with AF is four to five times higher than in patients without AF. The mortality rate among patients with ischemic stroke attributable to AF is approximately 20%, whereas the disability rate is as high as 60% [
7].
1. Clinical Data
1.1. Study Population
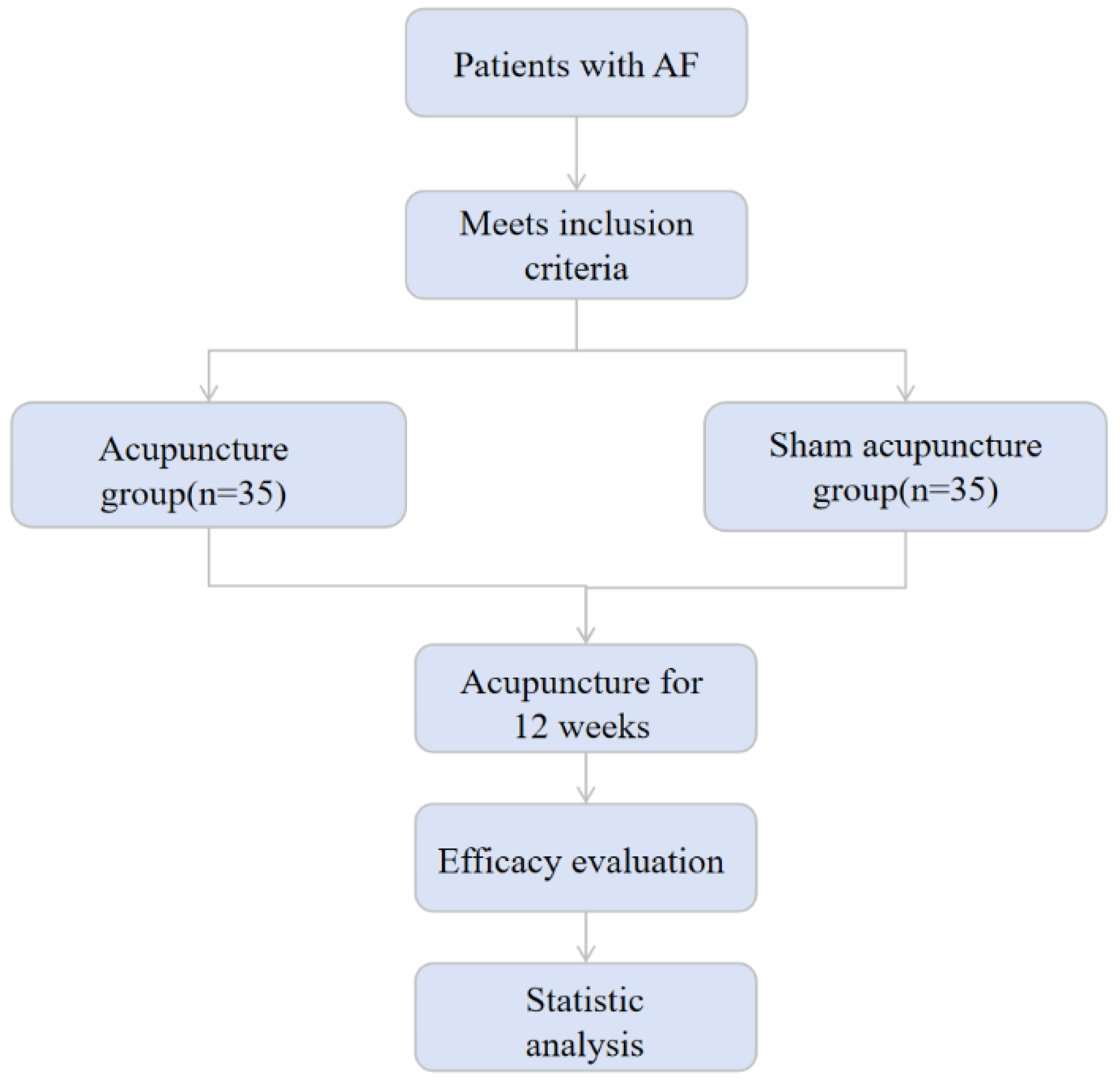
This study was designed as a multicenter prospective cohort study in accordance with the Declaration of Helsinki and received approval from the Ethics Committees of both the Second Affiliated Hospital of Shandong University of Traditional Chinese Medicine and Shanghai Chest Hospital. The study has been registered as a controlled trial in the Cochrane Clinical Trials Register under registration number NCT05125042. All patients included in the study were recruited from the Cardiovascular Department of either the Second Affiliated Hospital of Shandong University of Traditional Chinese Medicine or Shanghai Chest Hospital. A total of 70 patients who visited between September 2021 and September 2023 were included and were randomly assigned to an acupuncture group (n=35) and a sham acupuncture group (n=35) (see
Figure 1). Informed consent was obtained from all participants, who signed informed consent forms.
1.2. Diagnostic Criteria
According to the 2020 European Society of Cardiology Guidelines for the Management of Atrial Fibrillation (see Appendix 2), an atrial fibrillation (AF) episode that terminates spontaneously or following intervention within 7 days is classified as paroxysmal AF. AF that persists beyond 7 days is classified as persistent AF.
1.3. Inclusion Criteria
(1) Patients diagnosed with paroxysmal or persistent AF following catheter ablation (CA) surgery; (2) Age ≥ 18 years; (3) No restrictions based on gender; (4) Ability to undergo treatment and follow-up for 12 weeks.
1.4. Exclusion Criteria
(1) Severe heart failure (NYHA cardiac function class III or IV) , severe cardiovascular disease, or other significant comorbidities, including severe liver and kidney dysfunction, electrolyte imbalances, and severe bleeding tendencies. (2) Echocardiographic findings: left ventricular ejection fraction < 35% and left atrial diameter > 5.5 cm; (3) Severe pulmonary, hepatic, or renal diseases, or other significant primary conditions; (4) Severe allergic reactions to electrocardiogram monitoring electrodes; (5) Patients who have undergone acupuncture treatment within 6 months prior to CA. (6) Pregnant or lactating women.
1.5. Exclusion and Dropout Criteria Exclusion Criteria
(1) Patients experiencing serious adverse events that prevent continued participation in clinical treatment; (2) Patients who meet the inclusion criteria but are unable to cooperate with treatment in a timely manner; (3) Patients with an atrial fibrillation burden of 100% after the initial long-term ECG monitoring.
Dropout criteria: (1) During the research process, subjects were unable to complete the entire trial due to various reasons; (2) During the research process, subjects received treatment as required but failed to undergo timely follow-up for various reasons; (3) Patients for whom the researcher is unable to obtain final observation results due to prolonged follow-up times, changes in the subjects' living addresses, or other reasons.
2. Research Methods
2.1. Treatment Methods
Both patient groups commenced treatment within one week following coronary artery (CA) surgery, receiving acupuncture twice weekly for a total duration of 12 weeks, amounting to 24 sessions. All acupuncture treatments are performed by professional acupuncturists who have obtained the Traditional Chinese Medicine Practicing Qualification Certificate of the People's Republic of China and have more than 3 years of clinical experience. The acupuncture equipment utilized consisted of disposable, sterile acupuncture needles measuring either 0.25 mm × 40 mm or 0.25 mm × 25 mm, manufactured by Suzhou Medical Products Co., Ltd.
In the acupuncture group, treatment was administered at the acupoints Xinju (BL15), Neiguan (PC6), and Shenmen (HT07).
For heart acupuncture (BL15), the patient was positioned prone. Following routine disinfection of the acupoints, a needle measuring 0.5 to 1.0 inches was inserted. The angle between the needle body and the skin surface was maintained at 15 degrees. The acupuncturist performed techniques such as lifting, inserting, and twisting to facilitate the release of qi from the acupuncture points. During this process, the patient may experience sensations of soreness, numbness, and swelling in the acupuncture area. Subsequently, the acupuncturist employed tonifying and releasing techniques for 30 seconds prior to needle removal. For Neiguan (PC6) and Shenmen (HT07), the patient was positioned supine. Following routine disinfection of the acupoints, needles measuring 0.5 to 1.0 inches were inserted. The subsequent procedures were consistent with those described above.
In the sham acupuncture group, acupuncture was performed on the skin at non-meridian acupoints, with the number of acupuncture sessions matching the total number of acupuncture points in the treatment group.
The acupuncturist performed superficial acupuncture at the three designated non-acupoints, with a needle insertion depth of 2-3 mm. No manipulation was required at any of the acupoints. Non-meridian acupoint 1: Choose the patient's prone position, perform superficial acupuncture and then remove the needle. For non-meridian acupoints 2 and 3, the patient was positioned supine, and the acupuncture technique was consistent with that described above, with the needle retained for 30 minutes.
According to the "European Society of Cardiology Guidelines for the Management of Atrial Fibrillation" (see Appendix 2), all patients undergo routine pharmacological treatment following catheter ablation (CA), which includes: (1) postoperative anticoagulation, where patients are prescribed anticoagulants such as warfarin or rivaroxaban for a minimum of 8 weeks; (2) postoperative antiarrhythmic medications, which are administered routinely for 3 months; and (3) postoperative acid suppression therapy, in which patients with significant esophageal damage resulting from ablation receive proton pump inhibitors for 4 weeks. Researchers will select appropriate medications based on the patient's clinical condition, as well as drug indications and contraindications. Patients are advised to meticulously document their medication usage, including the drug name and administration times.
2.2. Observation Indicators
(1) Quality of life assessment: before acupuncture and after 3 months of acupuncture treatment, the AF-specific quality of life scale (Atrial fibrillation effect and quality of life, AFEQT) was used to evaluate. The AFEQT scale comprises four dimensions and twenty items, which include symptoms (four items), daily activities (eight items), treatment anxiety (six items), and treatment satisfaction (two items related to AF control and symptom improvement). The average score of the first three dimensions constitutes the total score of the AFEQT. Higher total scores on the scale and in each dimension (ranging from 0 to 100) indicate better quality of life for patients with atrial fibrillation.
(2) Atrial Fibrillation Burden After Three Months of Catheter Ablation Treatment: Atrial fibrillation burden is defined as the ratio of total attack time to monitoring time during the observation period. Following three months of acupuncture-assisted catheter ablation treatment, patients were monitored for seven days using the NS-SP-A-01 adhesive ultra-long dynamic electrocardiogram recorder (Shanghai Enshi Technology) to calculate the atrial fibrillation burden.
(3) Early Recurrence of Atrial Fibrillation After Catheter Ablation: Atrial fibrillation recurrence is defined as an episode of atrial fibrillation, atrial flutter, or atrial tachycardia confirmed by electrocardiogram or 24-hour dynamic electrocardiogram three months after catheter ablation treatment, with a duration of at least 30 seconds. The electrocardiogram returned to sinus rhythm following the resolution of symptoms. (4) Number of Hospitalizations Due to Arrhythmia: The number of hospitalizations related to arrhythmia within three months following catheter ablation was recorded. (5) Incidence Rate of Adverse Events: Adverse events, treatments, and patient relief throughout the trial were recorded using the adverse event evaluation form. Adverse events primarily include acupuncture-related events (such as hematoma, needle fainting, and acupuncture sequelae) and non-acupuncture-related events (including skin allergies caused by electrode pads, as well as drug-related and catheter ablation-related adverse events).
2.3. Statistical Analysis
SPSS 25.0 was used for statistical analysis. All measurement data were expressed as mean±standard deviation (±s);. If the data conformed to the normal distribution and homogeneity of variances, the independent sample t test was used for comparison between groups. Within the group Paired sample t test was used for comparison before and after treatment; non-parametric test was used for results that did not conform to the normal distribution or had uneven variances. Categorical variables of count data were analyzed using χ2 test. P<0.05 was considered as a statistically significant difference.
Results
3.1. Patient Completion Status
During the study period, two patients in the experimental group were excluded due to a 100% atrial fibrillation (AF) burden observed after long-term electrocardiogram (ECG) monitoring, and three patients were lost to follow-up. In the control group, three patients were excluded due to ineffective catheter ablation (CA), and three patients were lost to follow-up. Ultimately, a total of fifty-nine subjects—thirty from the experimental group and twenty-nine from the control group—successfully completed the intervention and assessment.
3.2. Baseline Characteristics
No statistically significant differences were observed in baseline characteristics and general information between the two groups (P > 0.05). All patients underwent successful treatment with pulmonary vein isolation (PVI). The additional ablation strategies included: ablation of the tricuspid valve isthmus for typical atrial flutter (3 cases in the experimental group and 3 cases in the control group), ablation of the left atrial roof to induce roof-dependent atrial flutter (2 cases in the experimental group and 3 cases in the control group), and mitral isthmus ablation (2 cases in the experimental group and 3 cases in the control group). No differences were found between the two groups regarding tricuspid isthmus ablation, left atrial linear ablation, mitral isthmus ablation, and electrical cardioversion (see
Table 1).
3.3. AFEQT Scale Score
Before treatment, no statistically significant differences were observed in the total AFEQT score or in any of the individual dimension scores between the two groups (P>0.05). Following treatment, the total AFEQT scores, as well as scores for symptoms, daily activities, treatment anxiety, AF control, and symptom improvement, increased in both groups compared to pre-treatment levels. Post-treatment, statistically significant differences were found in daily activity scores, treatment anxiety scores, and symptom scores between the two groups (P<0.05), suggesting that acupuncture treatment may enhance post-catheter ablation (CA) symptoms in patients with atrial fibrillation (AF) (see
Table 2).
3.4. AF Recurrence 3 Months after CA
Three months post-CA, atrial fibrillation (AF) recurred three times in the experimental group and five times in the control group. There was no statistical difference in the AF recurrence rate between the two groups of patients 3 months after CA. scientific significance (P>0.05). The AF burden was zero in both patient groups, and this difference was not statistically significant (P > 0.05). Patients in the experimental group were hospitalized for arrhythmia three times, while those in the control group were hospitalized four times, with no statistically significant difference observed (P > 0.05). These findings suggest that acupuncture has minimal impact on reducing the recurrence of AF following catheter ablation (CA) (see
Table 3).
3.5. Adverse Events
In this study, one adverse event was reported in the experimental group, while two cases were reported in the control group; all incidents involved bleeding or hematoma following acupuncture. All adverse events resolved following symptomatic treatment. In this study, no complications were observed following CA, and no serious adverse events were reported. There was no statistically significant difference in the incidence of adverse events between the two groups (P > 0.05; see
Table 4).
4. Discussion
In traditional Chinese medicine, AF falls into the categories of "chest numbness" and "heart palpitations". This condition is primarily associated with the heart and is believed to result from blood stasis, Qi deficiency, Yin deficiency, and phlegm accumulation. Acupuncture is a hallmark therapy in traditional Chinese medicine. Acupuncture is grounded in the meridian theory of traditional Chinese medicine and addresses AF by unblocking meridians and balancing Qi, blood, Yin, and Yang. With the increasing promotion of traditional Chinese medicine, acupuncture and other modalities have gradually been employed for the prevention, treatment, and adjunctive management of AF, demonstrating significant clinical efficacy. For instance, acupuncture at the Neiguan point is utilized for the treatment of paroxysmal AF [
13]; acupuncture at the Yingxiang point is employed for AF, supraventricular tachycardia, and other tachyarrhythmias [
14]; additionally, a combination of acupuncture and pharmacological interventions is used to enhance therapeutic outcomes. Some practitioners have also employed techniques such as filiform acupuncture [
15], external applications [
16], acupotomy [
17], and minimally invasive suture embedding [
18], achieving notable therapeutic effects. Animal studies have demonstrated the impact of varying acupuncture depths on the duration of AF in rats with paroxysmal AF. These findings indicate that deep stimulation can significantly reduce the duration of AF, thereby supporting the efficacy of acupuncture in its treatment [58]. Additionally, acupuncture may enhance atrial remodeling by modulating autonomic nerve activity and inflammatory responses [
19].
In recent years, quality of life has emerged as a crucial component in the clinical evaluation of disease severity and treatment efficacy. For the purposes of this study, a significant reduction in AF-related symptoms may be considered a success from the patient’s perspective, even if arrhythmia recurrence is documented. The AFEQT scale is a validated multidimensional AF-specific quality of life assessment scale that assesses not only symptom severity but also patients' daily activities, anxiety, and satisfaction with AF treatment. Some studies have pointed out that the AFEQT scale is more suitable for assessing patients' quality of life than other quality of life assessment scales [
20]. A large-scale study revealed that patients deemed asymptomatic by physicians reported specific atrial fibrillation (AF) symptoms, suggesting that physicians may underestimate the impact of AF on patients, particularly when symptoms are mild. Consequently, this study primarily focused on the changes in the quality of life of atrial fibrillation (AF) patients following catheter ablation (CA) and acupuncture, aiming to explore the impact of acupuncture on enhancing quality of life [
21].
References
- Hindricks G, Potpara T, Dagres N,et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC[J]. European Heart Journal, 2021, 42(5): 373–498.
- Baman J R, Passman R S. Atrial fibrillation[J]. Nat Rev Dis Primers, 2022, 8(1): 20.
- Baman J R, Passman R S. Atrial fibrillation[J]. JAMA, 2021, 325(21): 2218.
- Chugh S S, Havmoeller R, Narayanan K,et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study[J]. Circulation, 2014, 129(8): 837-847.
- Schnabel R B, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study[J]. Lancet, 2015, 386(9989): 154–162.
- Greccia D, Manicardi M, Malavasi V L, et al. Comparing outcomes in asymptomatic and symptomatic atrial fibrillation: a systematic review and meta-analysis of 81,462 patients[J]. J Clin Med, 2021, 10(17): 3979. [CrossRef]
- Chugh S S, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study[J]. Circulation, 2014, 129(8): 837-847.
- Chinese Association of Rehabilitation Medicine Cardiovascular Disease Prevention and Rehabilitation Professional Committee. Chinese expert consensus on cardiac rehabilitation for patients with atrial fibrillation [J]. Chinese Journal of Internal Medicine, 2021, 60(2): 106-116.
- Zhang Rui, Wei Ling Bo. Clinical research progress of traditional Chinese medicine in the treatment of AF[J]. Journal of Integrated Traditional Chinese and Western Medicine for Cardiovascular and Cerebrovascular Diseases, 2019, 17(19): 2962-2964.
- Huang Xinmiao, Qu Xiufen. Atrial fibrillation and autonomic nervous system Research progress on the correlation of [J]. Chinese Journal of Circulation, 2015, 30(10): 1027-1029.
- Liu Cunzhi. Evidence-based medical evidence and future design ideas for acupuncture treatment of cardiovascular diseases [J]. Chinese Traditional and Western Medicine Integrated Journal, 2019, 39(11): 1306-1308.
- Zhang Rui, Wei Lingbo. Clinical research progress of traditional Chinese medicine in the treatment of atrial fibrillation [J]. Journal of Integrated Traditional Chinese and Western Medicine for Cardio-Cerebral Vascular Disease, 2019, 17( 19): 2962-2964.
- Zhang Yonghuan, Zhou Shenghong. Research progress on acupuncture combined with drugs in the treatment of atrial fibrillation [J]. Clinical Research in Traditional Chinese Medicine, 2017, 9(10): 131-133.
- Zhao Weidong, Tan Wei , Yi Guangqiang et al. Clinical study on the treatment of sinus bradycardia with heart and spleen deficiency syndrome after modified maze surgery by Wenyang Tongmai acupuncture [J]. Clinical Journal of Acupuncture and Moxibustion, 2015, 31(4): 31-33.
- Analysis of the use of placebo acupuncture in domestic randomized controlled trials in the past five years by Wang Shouyan, Wang Hui, Cai Fei and others [J]. Shanghai Journal of Acupuncture, 2017, 36(10): 1269-1276.
- Wang Yuhai. Micro-needle knife treatment of the elderly Clinical observation of 27 cases of human idiopathic atrial fibrillation [J]. Huaihai Medicine, 2007, 25(2): 142.
- Chen Li, Chen Zhifang, Yang Xiaoxue, etc. Effectiveness of Neiguan acupoint catgut embedding in the treatment of atrial fibrillation and safety [J]. New Traditional Chinese Medicine, 2012, 44(8): 148-150.
- Ren Jie. Comparing the effects of different acupuncture depths of Neiguan points on atrial fibrillation electrocardiogram and atrial structure in rats with atrial fibrillation [D ]. Beijing: Beijing University of Chinese Medicine, 2019.
- Wang Huan, Cheng Kai, Ren Jie, et al. Effects of acupuncture pretreatment at "Jiquan" and "Neiguan" points on atrial fibrillation duration and Cx40 protein in rats with atrial fibrillation and the influence of mRNA expression[J]. Clinical Journal of Acupuncture and Moxibustion, 2019, 25(6): 74-78.
- Mark D. Assessing quality-of-life outcomes in cardiovascular clinical research [J]. Nat Rev Cardiol, 2016, 13(5): 286-308.
- Freeman J, Simon D, Go A, et al. Association Between Atrial Fibrillation Symptoms, Quality of Life, and Patient Outcomes: Results From the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) [J]. Circ Cardiovasc Qual, 2015, 8(4): 393-402.
- Li Yingyi, Wang Qunshan. Quality of life assessment and latest symptom classification method for patients with atrial fibrillation [J]. Chinese Journal of Circulation, 2015, 30(7): 3.
- Zhou He, Xu Yawei. Evaluation of intelligent electrocardiogram detectors Accuracy of diagnosing arrhythmias[J]. Beijing Biomedical Engineering, 2022, 41(1): 73-78.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).