1. Introduction
In 2012, the rearranged during transfection (RET) gene was first identified as an oncogenic driver in NSCLC [
1]. Mutations in the RET fusion gene have been observed in approximately 1 to 2% of NSCLC patients [
1]. Furthermore, at least 45 RET gene fusion partners have been identified in lung cancer, the most common of which is KIF5B-RET (70–90%) [
2,
3]. Selpercatinib (LOXO-292) is the first RET-specific kinase inhibitor approved by the FDA to treat RET-altered thyroid and NSCLC tumors [
4]. The LIBRETTO-001 trial indicated that selpercatinib has durable and safe anti-tumor activity as well as excellent intracranial efficacy [
2,
5].
The LIBRETTO-001 trial also indicated that 44% of patients experienced treatment-emergent serious adverse events (SAEs), of which 11% were related to selpercatinib and drug hypersensitivity was the most common treatment-related SAE. [
2] Moreover, in clinical trials, 4.3% of selpercatinib-treated patients have indicated hypersensitivity of any grade, and rash is among the most common symptoms [
6]. In addition, hypersensitivity reactions were relatively more severe when selpercatinib followed the treatment of immune checkpoint inhibitor (ICI) [
7,
8]. The literature has also indicated that the most common types of rashes induced by selpercatinib drug were erythematous, macular, maculopapular, morbilliform, and pruritic [
6].
In this case, the patient underwent genetic testing, which revealed the presence of the KIF5B-exon24-RET-exon11 fusion variant (15.18% variant rate), and since the patient had already developed a secondary malignancy tumor in the brain, selpercatinib treatment was selected on a comprehensive basis. The patient had no history of ICI use and never developed a more severe generalized eczema-like flakiness and dry skin. This is the first report of such cutaneous toxicities associated with selpercatinib treatment.
2. Case Report
A 50-year-old patientwas diagnosed with a secondary malignant tumor of the frontal lobe and NSCLC via genetic testing. The patient was prescribed 4 weeks of selpercatinib as a subsequent treatment. However, after 4 weeks, the patient indicated the development of eczematous skin lesions.
2.1. Case Description
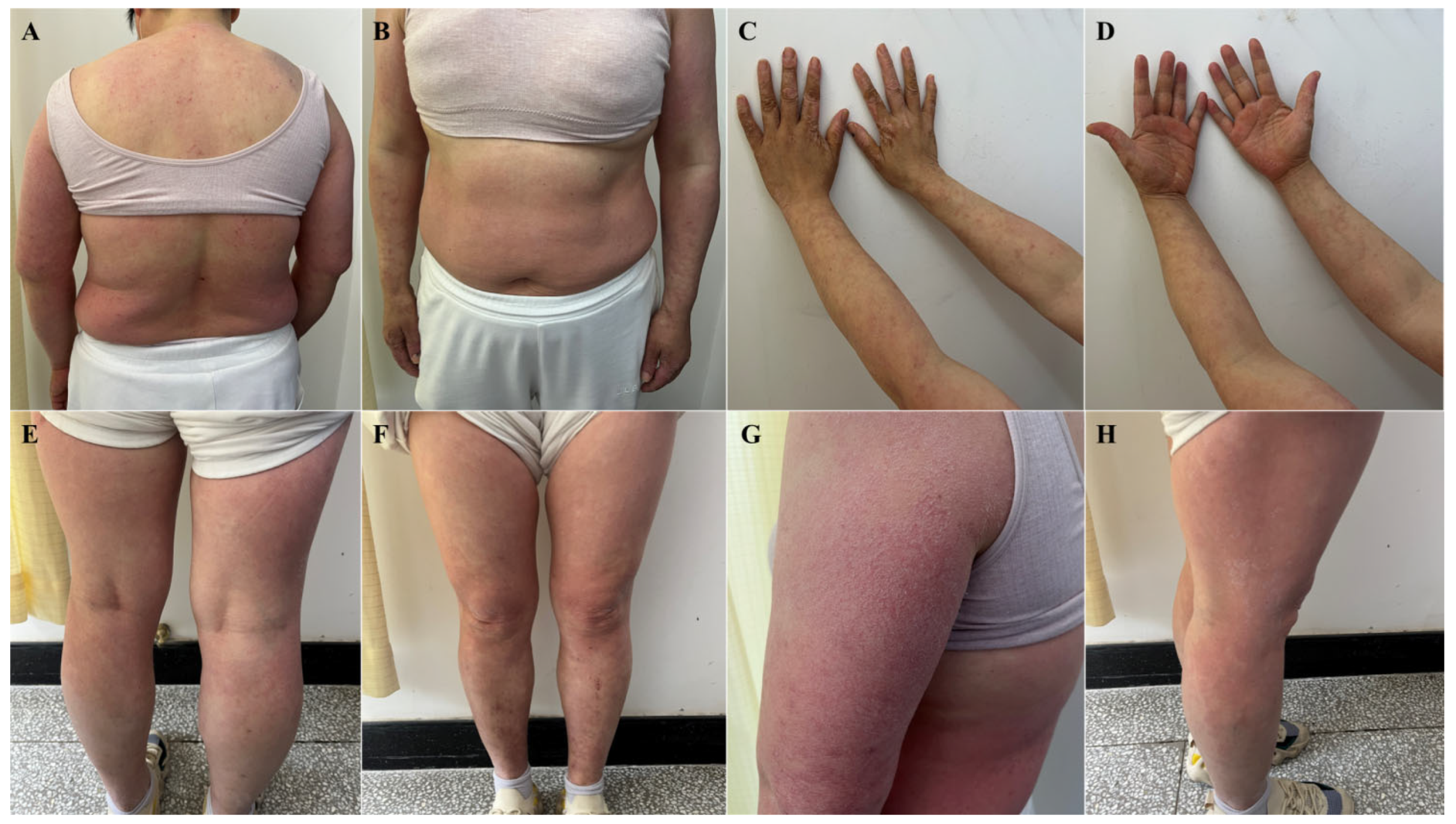
The patient started taking selpercatinib 160 mg, PO, BID on April 17, 2024 and developed erythematous papules on the face and neck, with intolerable itching around May 15, 2024. Routine blood tests revealed that the patient had no abnormalities. The patient self-administered oral prednisone acetate tablets, 5 mg irregularly for over a week, which resolved skin lesions on the face and neck. However, eczema-like changes subsequently manifested on the abdomen, back, and extremities, with the most severe skin lesions observed on the hands, exhibiting significant cracking and desquamation. For proper treatment, the patient was admitted to Tianjin Academy of traditional Chinese Medicine Affiliated Hospital on May 29, 2024. The dermatological examination revealed symmetrical erythematous papules and plaques throughout the body, with dry and scaly skin, as well as severe pruritus and visible scratch marks (
Figure 1).
2.2. Laboratory Analyses
Dermatopathologic biopsy specimens were taken from the leg. The microscopic analysis of PAS stained (-) tissues revealed the presence of epidermal hyperkeratosis, hyperkeratosis, superficial crusting, hypertrophy of the stratum spinosum, and mass infiltration of large numbers of lymphocytes, histiocytes, and small numbers of plasma cells around the superficial dermal vessels. Furthermore, laboratory tests revealed mild eosinophilia [0.57 * 109/L (normal, 0.02-0.52)], 1.2% basophils (normal, 0-1), and 117.20 KIU/L serum IgE (normal, 0-100). Clinical, histologic, and laboratory findings were consistent with a diagnosis of eczema.
2.3. Treatment Regimen
Considering the patient's physical condition, the treatment regimen included: compound betamethasone intramuscular injection (1 mL of 5 mg betamethasone dipropionate with 2 mg betamethasone sodium phosphate, both measured as betamethasone); ST, topical application of topical 1:1 mixture of triamceinolone acetonide acetate cream (1.5%) and allantoin cream; BID. In the case of intense itching at night, which interferes with normal sleep, additional chlorphenamine maleate tablets 5 mg were prescribed; PO, QN.
2.4. Follow-Up
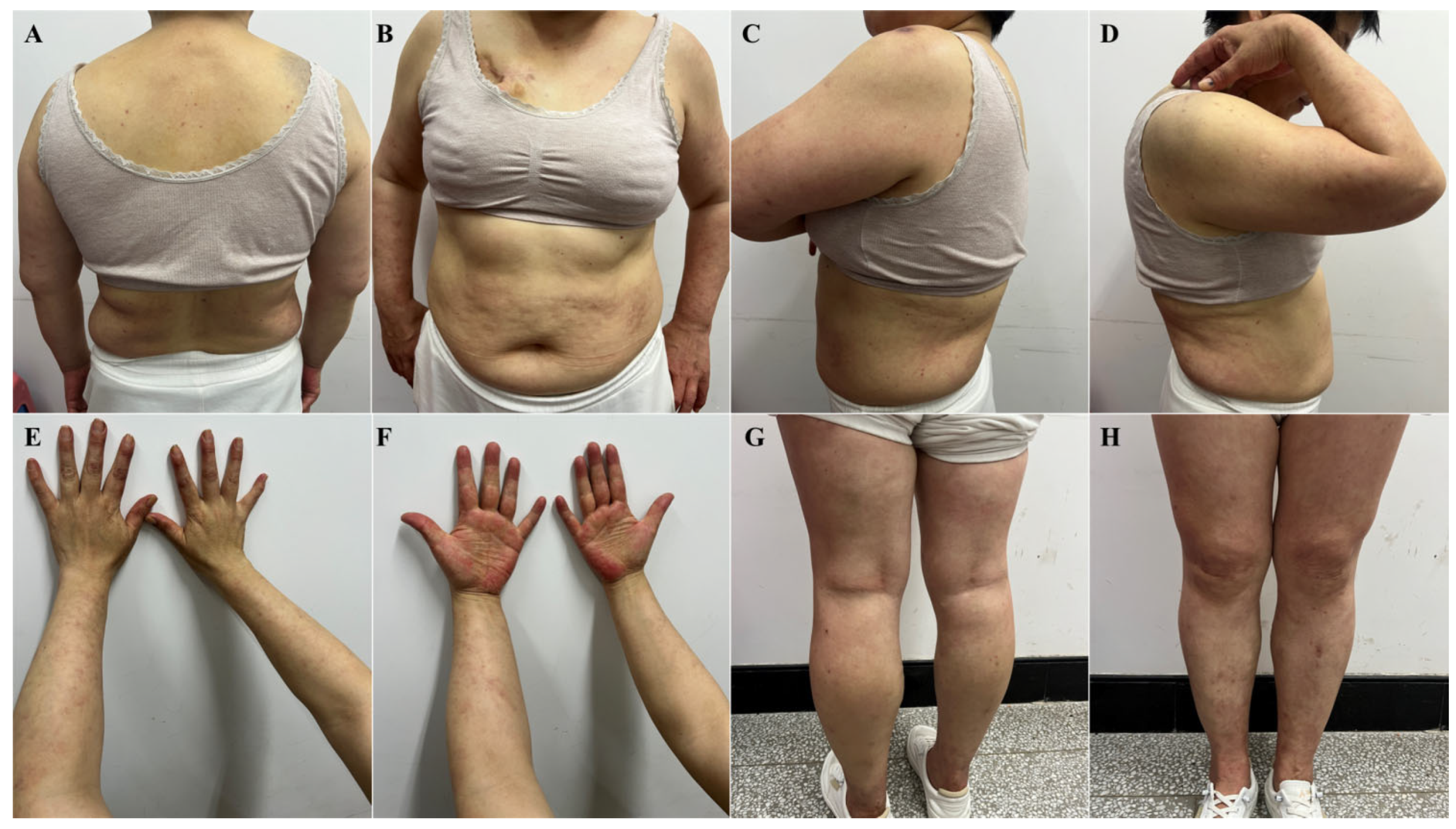
After 10 days, on June 7, 2024, the patient returned to the clinic with significantly improved skin lesions and approaching normal skin morphology (
Figure 2). Patients did not discontinue or taper selpercatinib throughout treatment.
3. Discussion
Skin damage is a common adverse effect of oncology therapeutic agents, especially ICI and multi-kinase inhibitors, and eczematous damage has also been reported [
9,
10]. The antitumor mechanism of ICI involves the co-stimulation of T-cells to increase immune activation, which promotes antitumor immune responses [
11]. ICI promotes widespread and relatively nonspecific activation of T cells in patients, inducing immune system hyperfunction, which consequently leads to the development of immune-related adverse events such as eczema [
11]. Multi-kinase inhibitors achieve anti-tumor effects by inhibiting the epidermal growth factor receptor (EGFR) signaling pathway [
6]. EGFR is crucial for epidermal regeneration and skin physiology maintenance. Furthermore, its signaling dysregulation is significantly associated with the pathogenesis of inflammatory skin diseases [
12]. Although selpercatinib is a highly selective RET inhibitor with minimal effect on other kinases and a reduced risk of skin-related adverse events than ICIs and multi-kinase inhibitors, their mechanisms underlying the skin damage might be similar.
Over the past few years, several studies have reported that targeted therapies against psoriasis cause eczematous damage, specifically the anti-tumor necrosis factor alpha (TNF-α) and anti-interleukin 17 (IL-17) therapies with ustekinumab, secukinumab, ixekizumab, etc. targeted therapeutic agents [
13,
14]. Psoriasis and eczema are thought to be diseases caused by an imbalance in the T helper (Th)1/Th2 immune response, with Th1 being more prominent in psoriasis and Th2 predominating in eczema [
15]. The Th1 and Th2 pathways are closely related and are in homeostasis, where, when one pathway is blocked or reduced, the response of the other pathway is more euphoric [
16]. Therefore, psoriasis monoclonal antibody therapy, whether directed against TNF-alpha or IL-17, is directed against the inhibition of the Th1 pathway and will increase the response of the Th2 pathway, which results in the development of Th2-type disease, such as eczematous damage [
15]. Selpercatinib, prescribed in this case report, is also a targeted drug. However, unlike the aforementioned monoclonal antibodies, selpercatinib is a small-molecule kinase inhibitor with high selectivity against RET gene fusions and directly targets the Th1 pathway. It has been observed that IL-22 levels are elevated in eczematous lesions induced by anti-TNF-α therapy. IL-22 in eczematous lesions has been observed to be associated with drug-induced adverse reactions [
15]. Therefore, it can be hypothesized that selpercatinib also affects IL-22 or other functionally similar cytokines that result in the development of eczematous skin damage.
In this case report, the role of estrogen in the occurrence of adverse drug events was also studied. Estrogen plays a significant role in the pathogenesis and prognosis of eczema and other dermatological conditions by facilitating the formation and restoration of the skin barrier by regulating filamentous polyprotein expression and stimulating β-glucosidase [
17]. The association of RET with estrogen receptors (ER) has been substantiated, with both exhibiting co-expression, and RET is considered to be an important factor in the development of ER-positive breast cancer [
18]. In addition, estrogen directly modulates the effects on RET expression [
19]. Therefore, RET inhibition induced by selpercatinib may directly or indirectly affect estrogen levels by altering ER expression, which in turn destabilizes the skin barrier, thereby promoting eczematous damage.
4. Conclusions
Subsequently, the patient used only topical glucocorticoid cream, with a gradual reduction in concentration and dosage. The follow-up to date has indicated that the rash is well controlled, there are no other complaints of discomfort, and selpercatinib administration was not disturbed, which may indicate the safety and efficacy of glucocorticoids use for the treatment of selpercatinib-induced cutaneous adverse drug reactions.
Reports of eczematous adverse drug reactions following the use of selpercatinib are uncommon. Further research on the mechanism of eczematous eruption is required to better manage this adverse drug reaction and alleviate the patient's skin discomfort while avoiding interruptions or dose reductions of the primary regimen.
Author Contributions
All authors participated in the literature review. Conceptualization, B.L. and L.Z..; investigation, B.L. and P.C.; resources, L.Z.; data curation, B.L.; writing—original draft preparation, B.L. and P.C.; writing—review and editing, B.L.; P.C. and W.X.; supervision, L.Z.; funding acquisition, W.X. and L.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NATIONAL NATURAL SCIENCE FOUNDATION OF CHINA, grant number 82305259.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
Data is unavailable due to privacy of the patients.
Conflicts of Interest
All authors declare that they have no conflicts of interest regarding this paper.
References
- Lipson, D.; et al. Identification of new ALK and RET gene fusions from colorectal and lung cancer biopsies. Nature medicine 2012, 18, 382–384. [Google Scholar] [CrossRef] [PubMed]
- Drilon, A.; et al. Selpercatinib in Patients With RET Fusion-Positive Non-Small-Cell Lung Cancer: Updated Safety and Efficacy From the Registrational LIBRETTO-001 Phase I/II Trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 2023, 41, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Novello, S.; Califano, R.; Reinmuth, N.; Tamma, A.; Puri, T. RET Fusion-Positive Non-small Cell Lung Cancer: The Evolving Treatment Landscape. The oncologist 2023, 28, 402–413. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.C.B.; Mulligan, L.M. Selpercatinib: First approved selective RET inhibitor. Cell 2023, 186, 1517. [Google Scholar] [CrossRef] [PubMed]
- Subbiah, V.; et al. Intracranial Efficacy of Selpercatinib in RET Fusion-Positive Non-Small Cell Lung Cancers on the LIBRETTO-001 Trial. Clinical cancer research : an official journal of the American Association for Cancer Research 2021, 27, 4160–4167. [Google Scholar] [CrossRef] [PubMed]
- Nardo, M.; et al. Strategies for mitigating adverse events related to selective RET inhibitors in patients with RET-altered cancers. Cell reports. Medicine 2023, 4, 101332. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, K.; Kaira, K.; Imai, H.; Shiono, A.; Kagamu, H. Prior immune checkpoint inhibitors may enhance severe hypersensitivity related to selpercatinib in RET fusion gene-positive lung cancer. Journal of chemotherapy (Florence, Italy), 2024, 1-3. [CrossRef]
- McCoach, C.E.; et al. Hypersensitivity Reactions to Selpercatinib Treatment With or Without Prior Immune Checkpoint Inhibitor Therapy in Patients With NSCLC in LIBRETTO-001. Journal of thoracic oncology : official publication of the International Association for the Study of Lung Cancer 2022, 17, 768–778. [Google Scholar] [CrossRef] [PubMed]
- Pach, J.; Valido, K.; Belzer, A.; Leventhal, J.S. The Use of Biologic Agents for the Treatment of Cutaneous Immune-Related Adverse Events from Immune Checkpoint Inhibitors: A Review of Reported Cases. American journal of clinical dermatology 2024, 25, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Pasadyn, S.R.; Knabel, D.; Fernandez, A.P.; Warren, C.B. Cutaneous adverse effects of biologic medications. Cleveland Clinic journal of medicine 2020, 87, 288–299. [Google Scholar] [CrossRef] [PubMed]
- Tattersall, I.W.; Leventhal, J.S. Cutaneous Toxicities of Immune Checkpoint Inhibitors: The Role of the Dermatologist. The Yale journal of biology and medicine 2020, 93, 123–132. [Google Scholar] [PubMed]
- Pospischil, I.; Hoetzenecker, W. Drug eruptions with novel targeted therapies - immune checkpoint and EGFR inhibitors. Journal der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology : JDDG 2021, 19, 1621–1643. [Google Scholar] [CrossRef] [PubMed]
- Caldarola, G.; et al. Clinical and histopathological characterization of eczematous eruptions occurring in course of anti IL-17 treatment: a case series and review of the literature. Expert opinion on biological therapy 2020, 20, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Puig, L. Paradoxical Reactions: Anti-Tumor Necrosis Factor Alpha Agents, Ustekinumab, Secukinumab, Ixekizumab, and Others. Current problems in dermatology 2018, 53, 49–63. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, M.; et al. Eczematous eruption during anti-interleukin 17 treatment of psoriasis: an emerging condition. The British journal of dermatology 2019, 181, 604–606. [Google Scholar] [CrossRef] [PubMed]
- Burlando, M.; Cozzani, E.; Russo, R.; Parodi, A. Atopic-like dermatitis after secukinumab injection: A case report. Dermatologic therapy 2019, 32, e12751. [Google Scholar] [CrossRef] [PubMed]
- Weare-Regales, N.; Chiarella, S.E.; Cardet, J.C.; Prakash, Y.S.; Lockey, R.F. Hormonal Effects on Asthma, Rhinitis, and Eczema. The journal of allergy and clinical immunology. In practice 2022, 10, 2066–2073. [Google Scholar] [CrossRef] [PubMed]
- Mechera, R.; et al. Expression of RET is associated with Oestrogen receptor expression but lacks prognostic significance in breast cancer. BMC cancer 2019, 19, 41. [CrossRef]
- Pecar, G.; et al. RET signaling in breast cancer therapeutic resistance and metastasis. Breast cancer research : BCR 2023, 25, 26. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).