Submitted:
27 September 2024
Posted:
27 September 2024
You are already at the latest version
Abstract
Keywords:
Background
Materials and Methods
Subjects
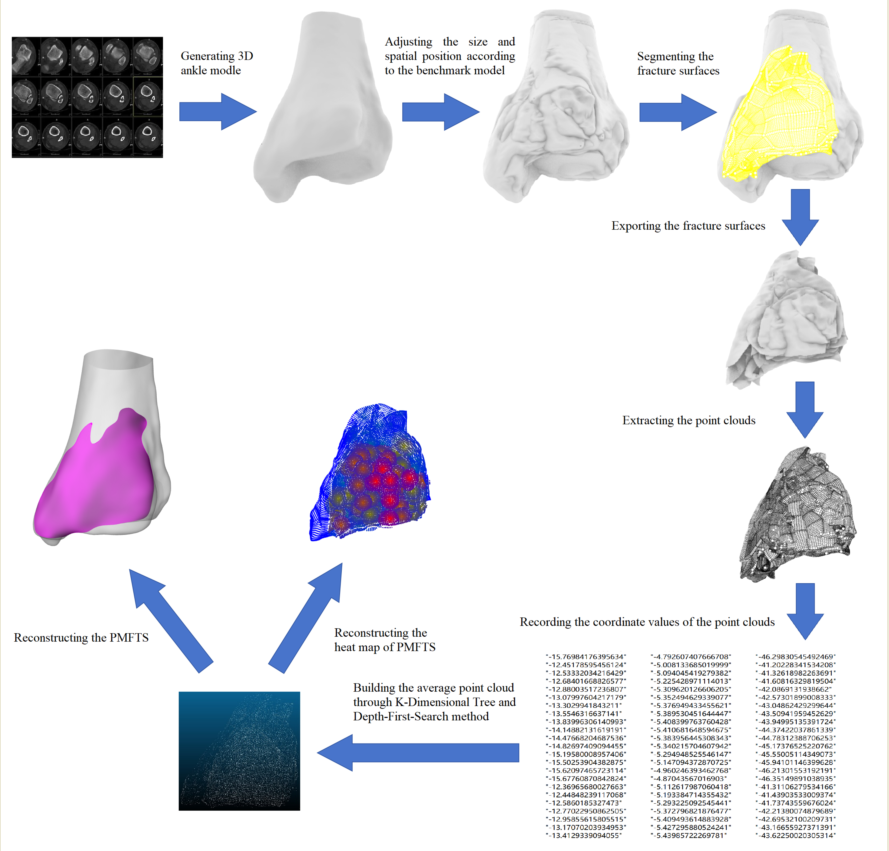
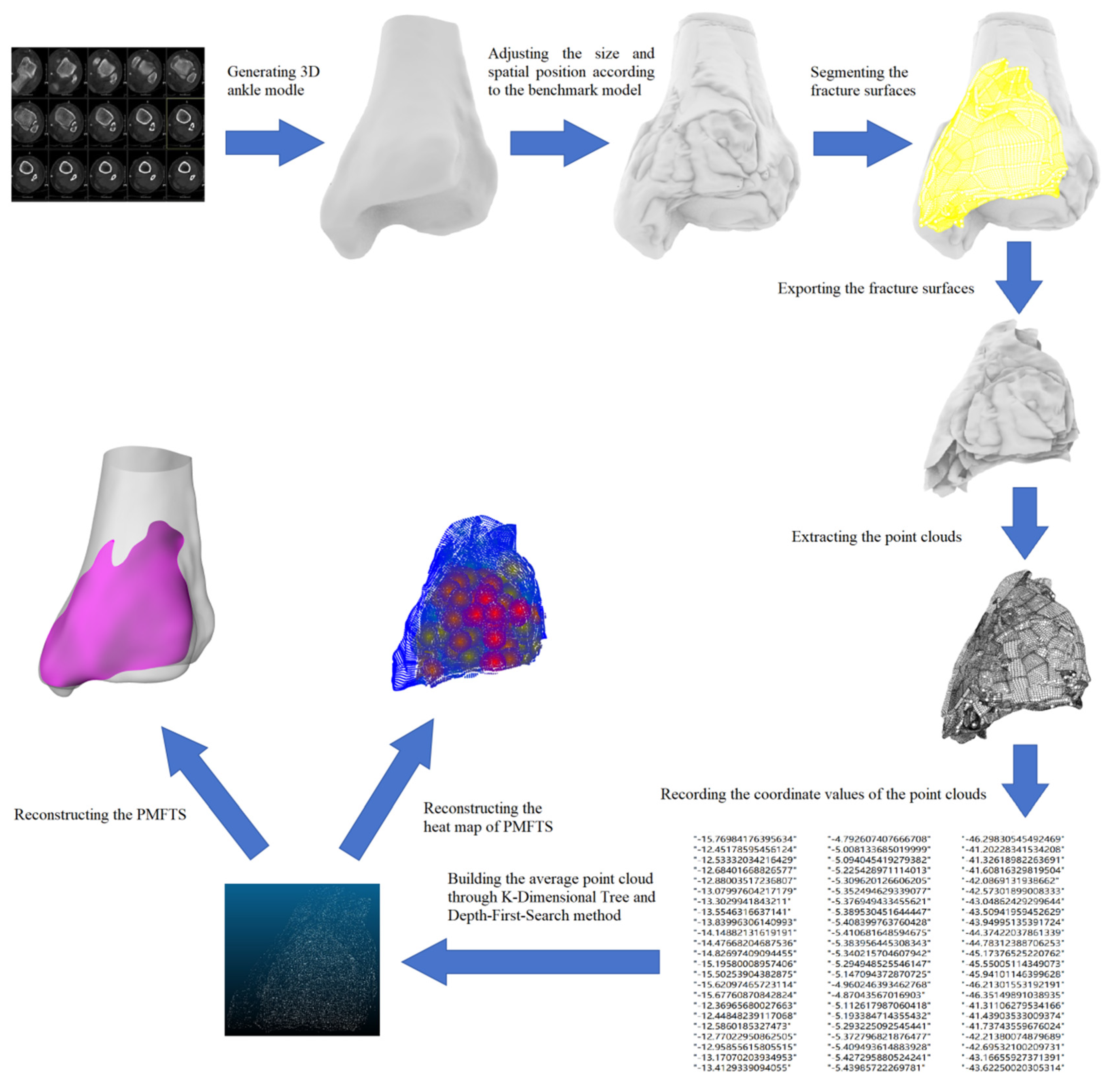
Generating the Trend Surface of PMFs
Results
Discussion
The Epidemiology of PMFs
The Classification of PMFs
The Morphology of PMFs
The Treatment of PMFs
Limitation and Strength
Conclusions
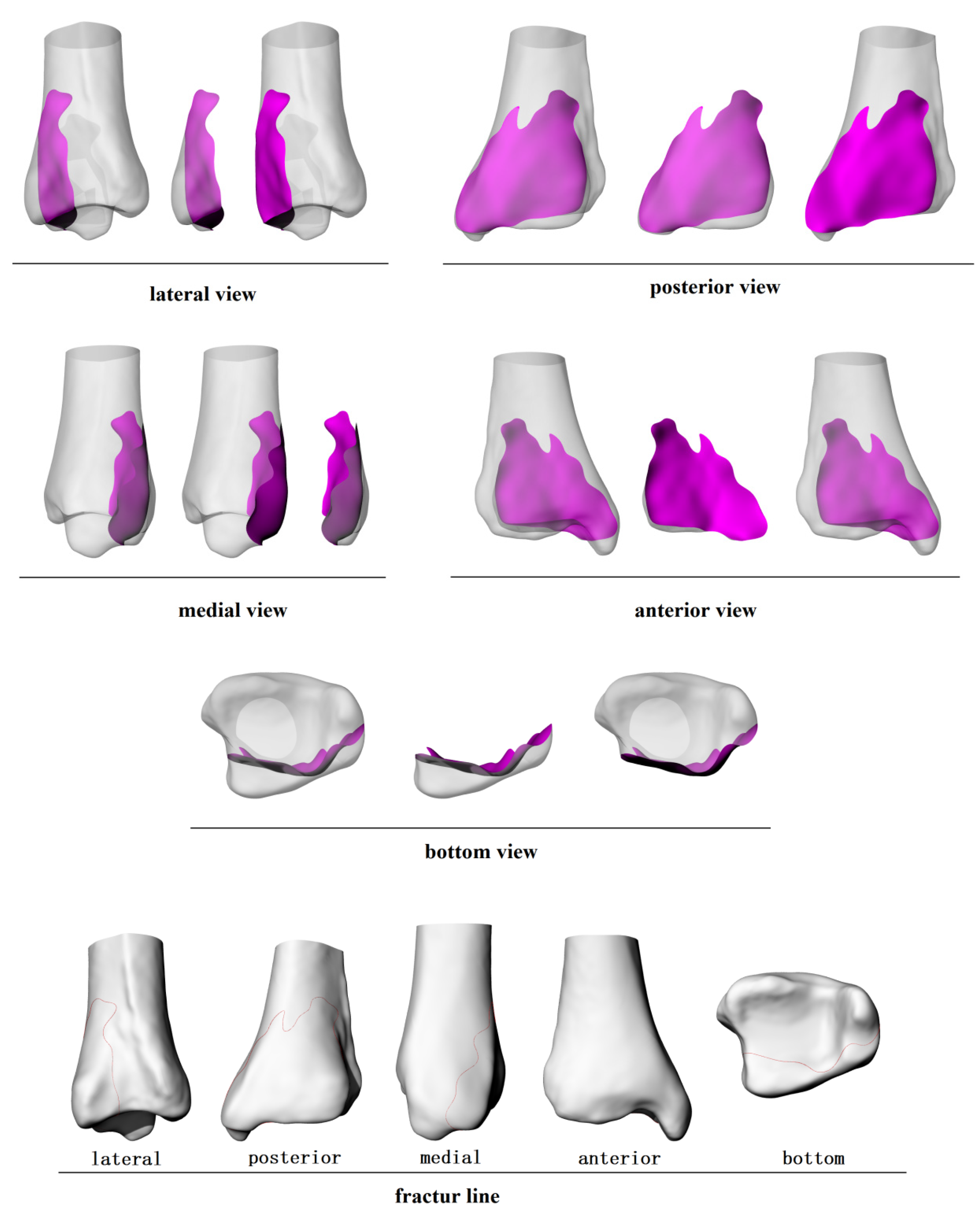
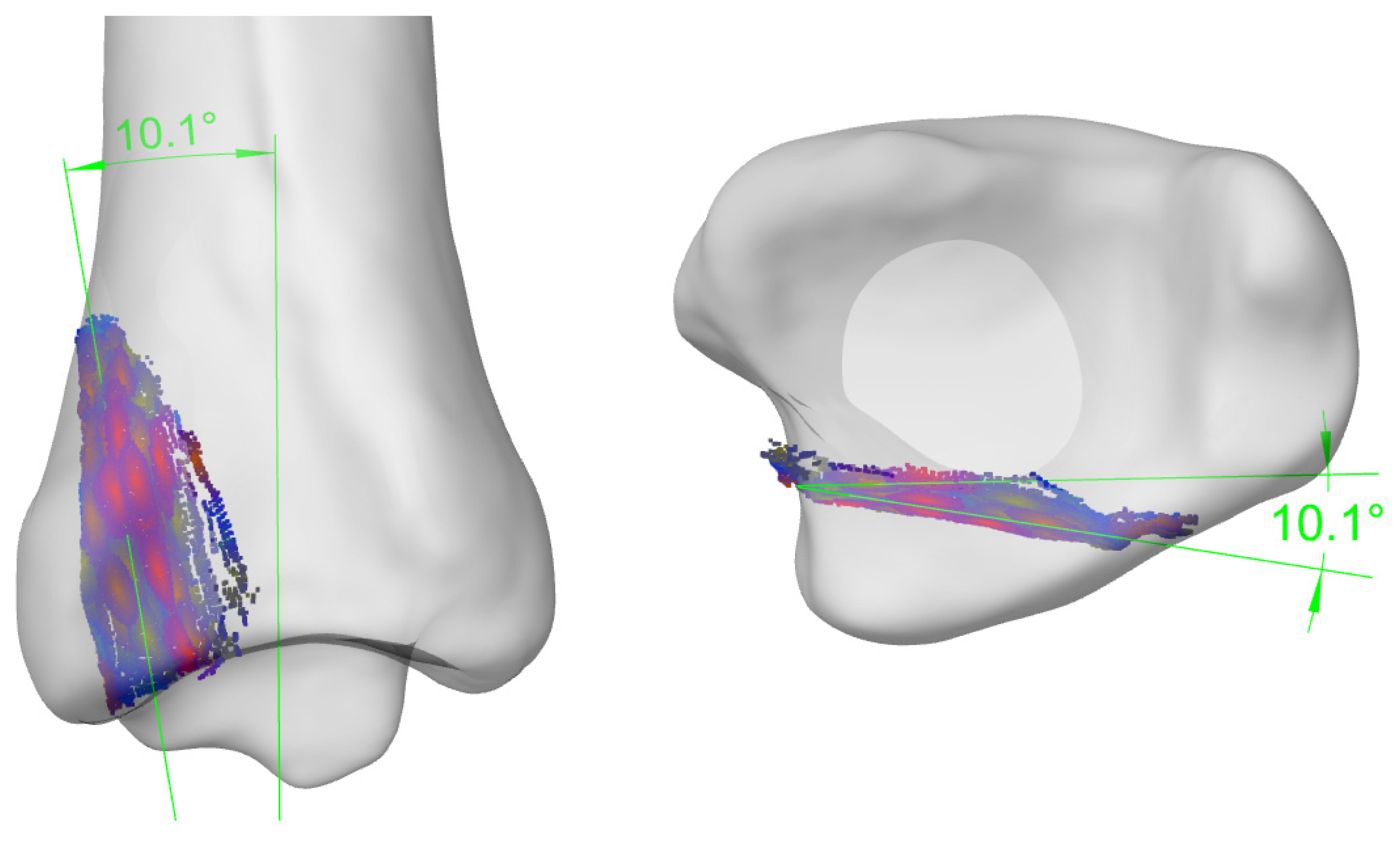
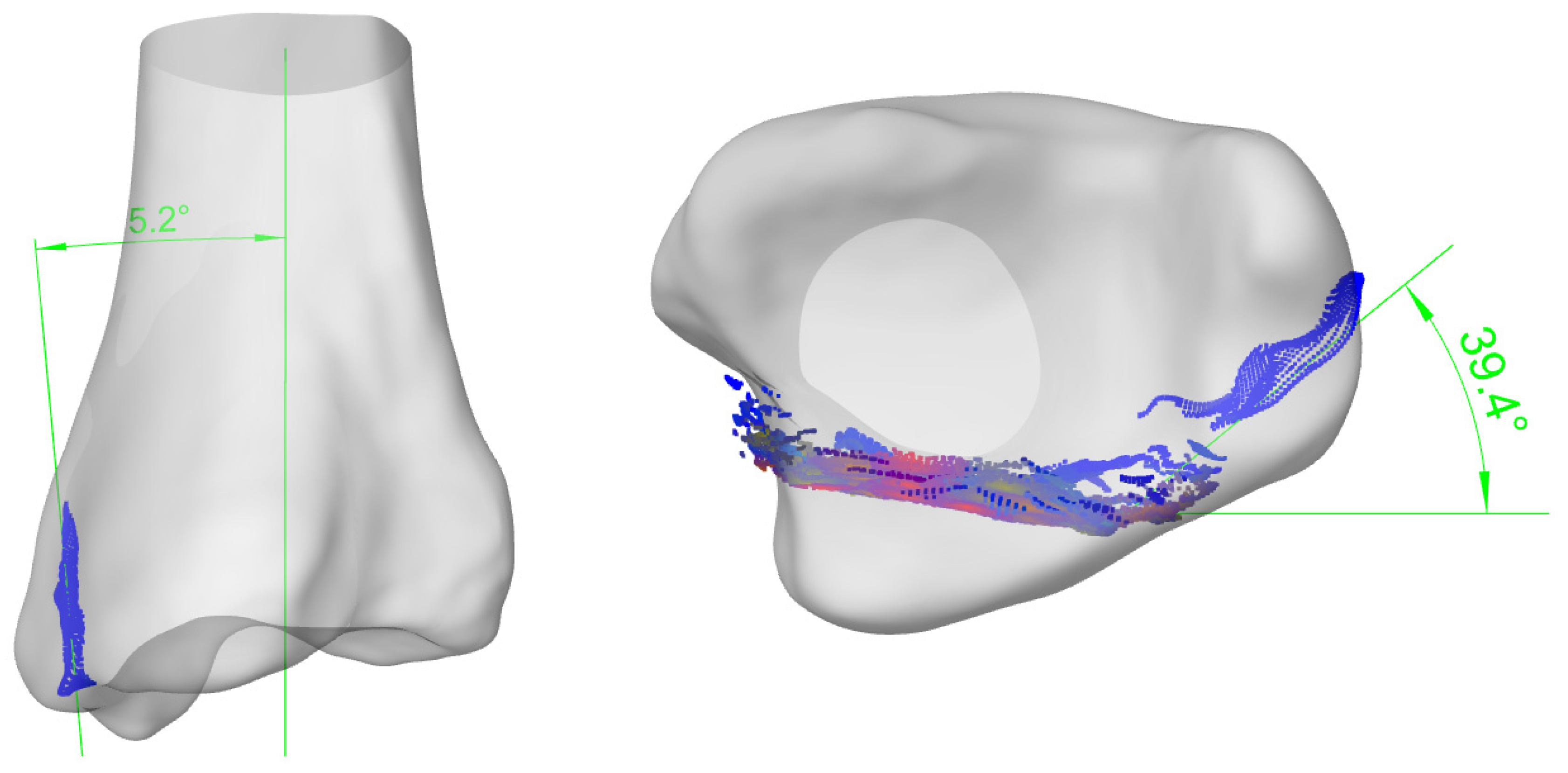
- The fracture lines on the bone surface give us the first impression of the fracture shape. However, these lines are actually the intersection lines of the fracture surface with the bone surface. They help us generate a stereoscopic model of the fracture surface in our brain, but this model may not be the same as the true fracture surface (Figure 3).
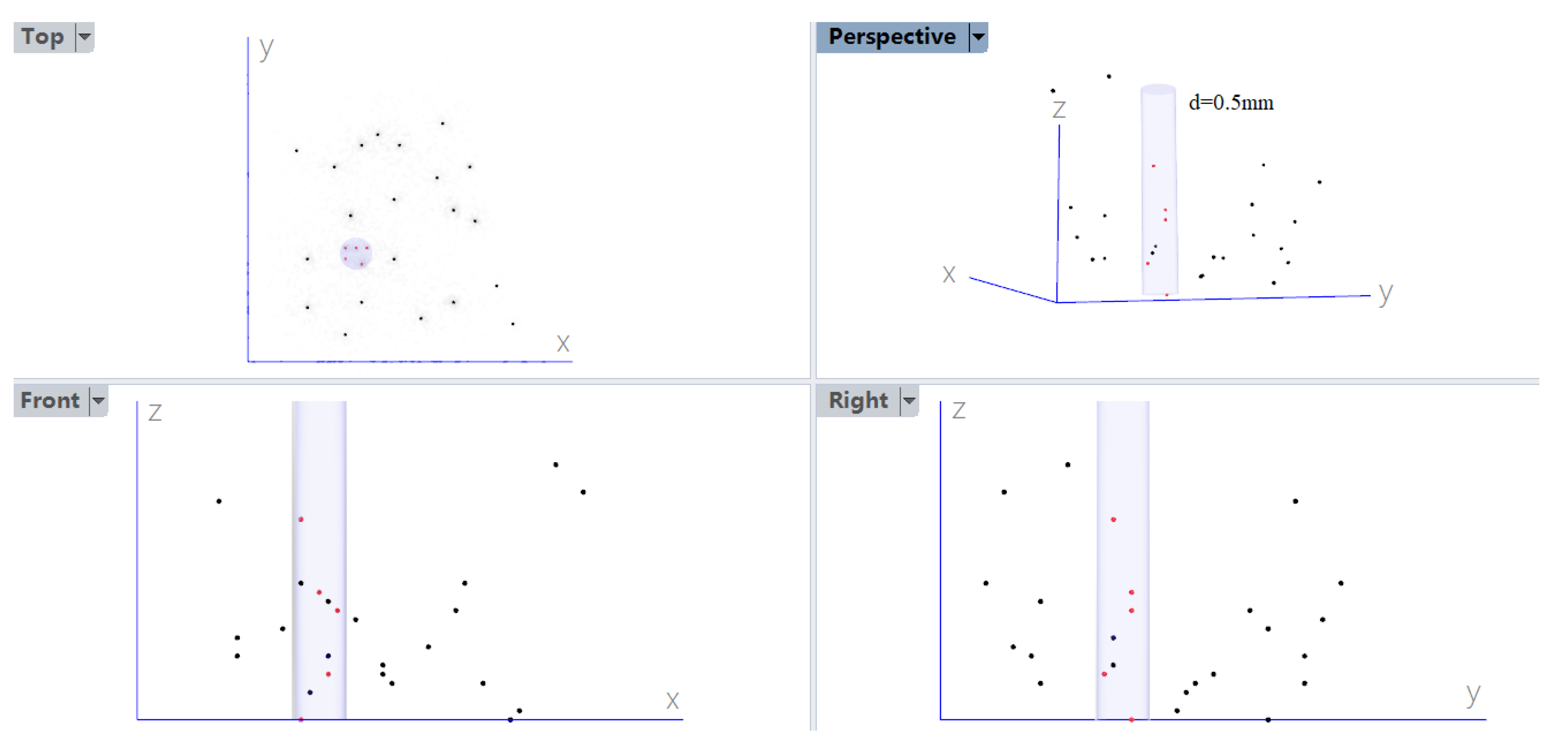
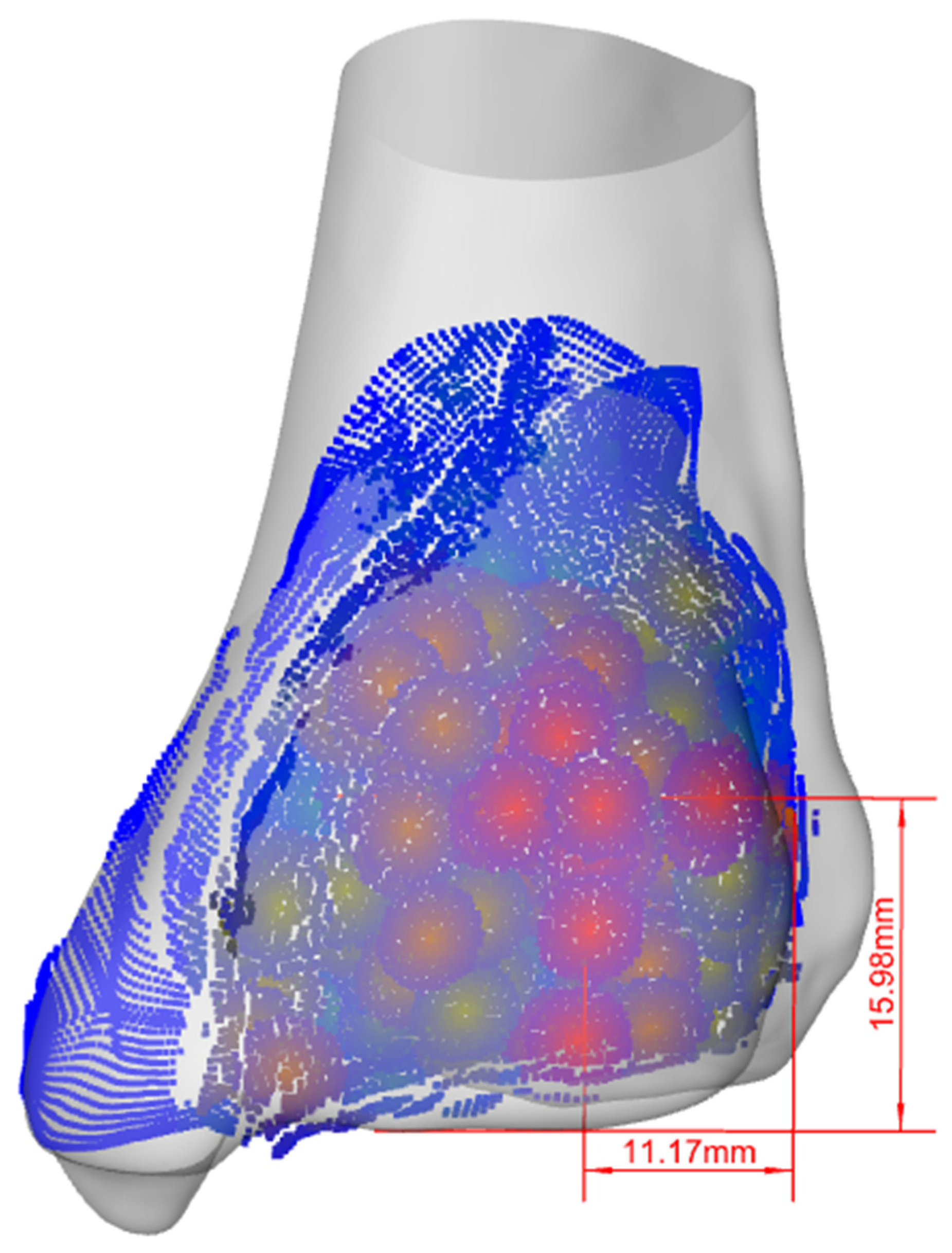
- In A-P fluoroscopic view, 16.0mm away from the posterior malleolar distal edge and 11.2mm medial to the posterior margin of the fibular notch were the high frequency regions where the fracture surfaces passed through (Figure 6).
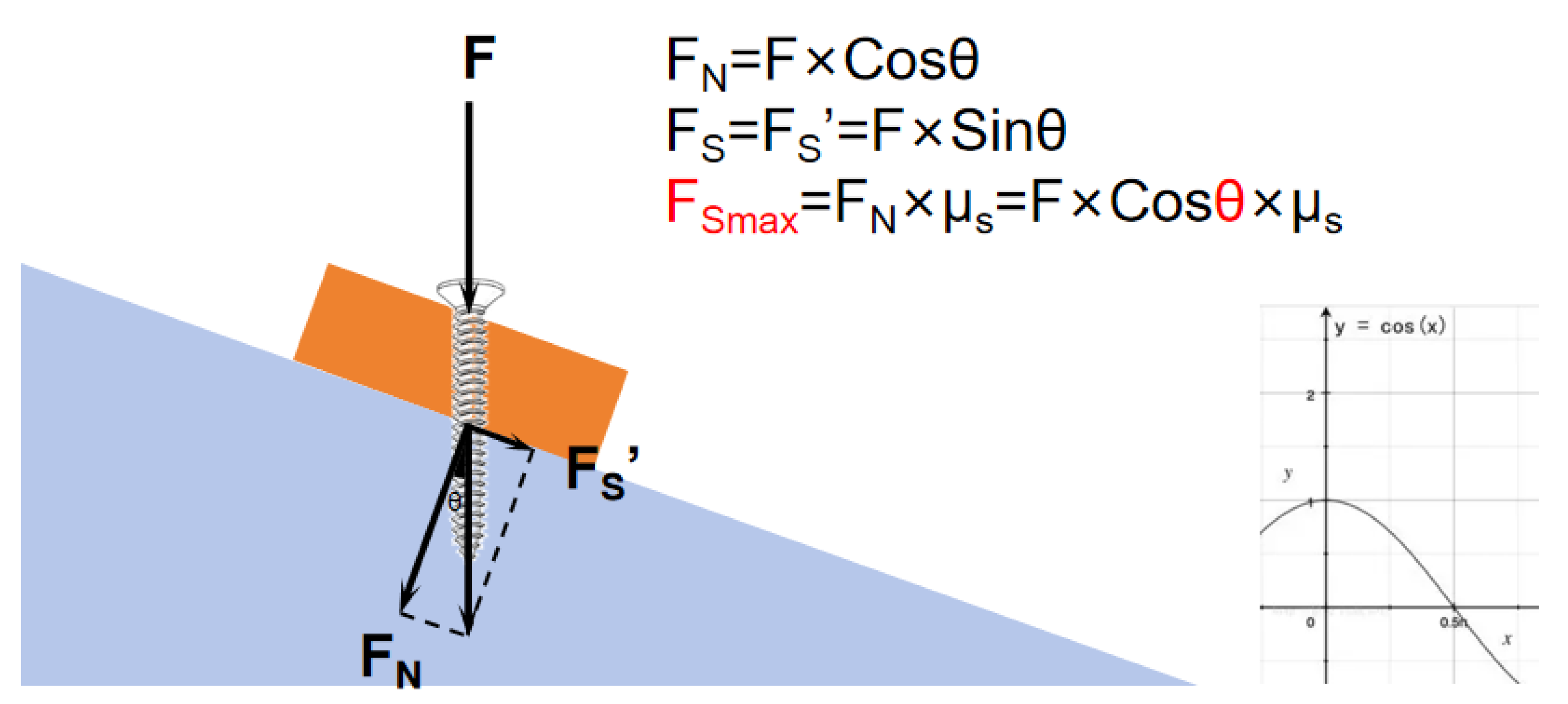
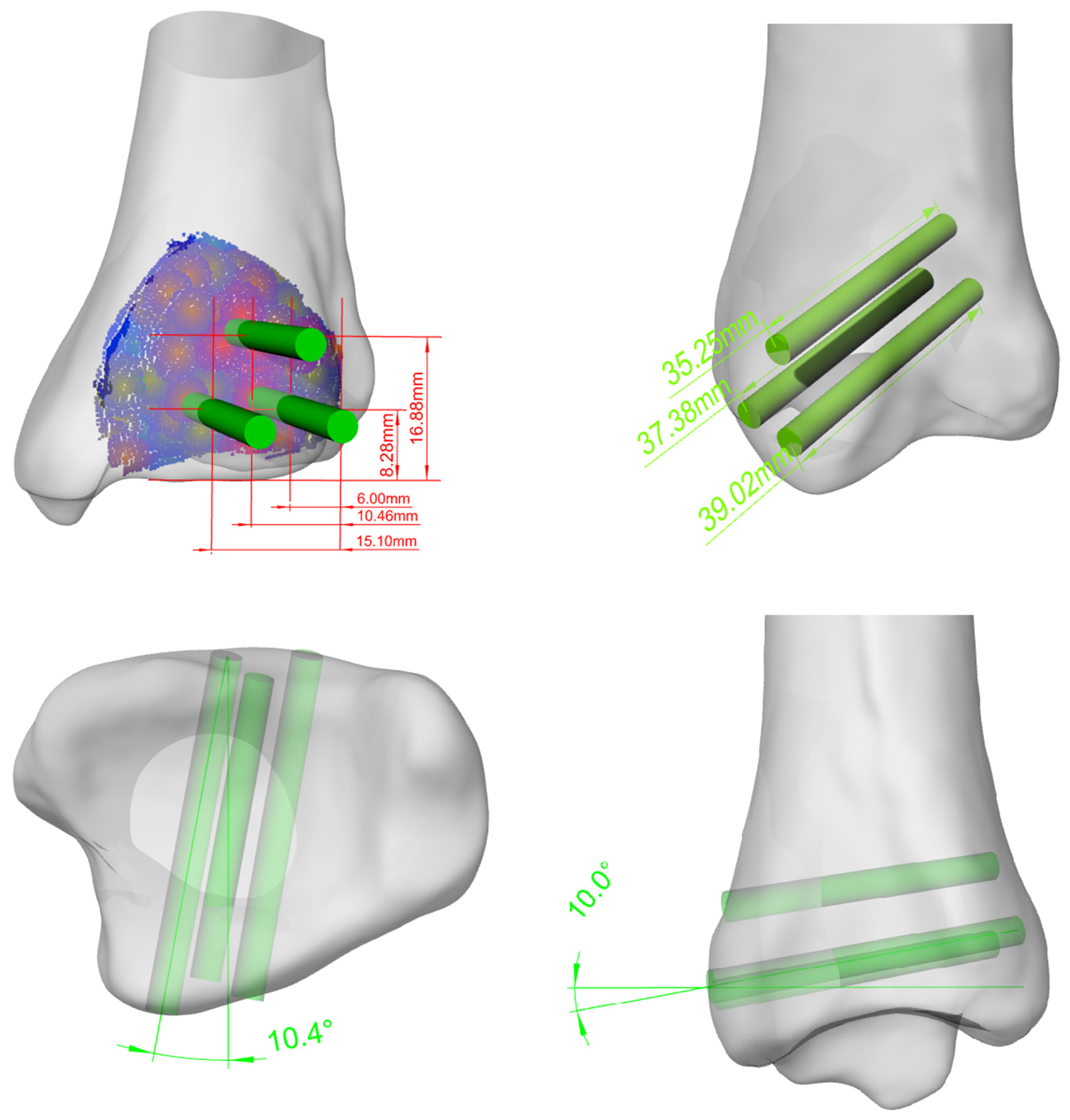
- To firmly hold the posterolateral PMF at the reduction place, 3 key screws should be parallelly inserted into the distal tibia through the fragment, oriented medially 10.4°, cephalad 10°. The insertion points of the screws, in back view, are individually identified at 8.3mm, 16.9mm, 8.3mm superior to the inferior margin of the posterior malleolus, and 6.0mm,10.5mm, 15.1mm posterior to the posterior margin of the fibular notch. The depth of the screws should be no more than 40mm to avoid irritating the anterior tendons, vessels and nerves(Figure 8).
Abbreviations
| PMFs = Posterior malleolar fractures |
| PMFTS = Posterior malleolar fracture trend surface |
| SER = supination external rotation |
| PER = pronation external rotation |
| AP = anterior-posterior |
| PA = posterior-anterior |
References
- Lauge-Hansen, N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch Surg. 1950, 60, 957–985. [Google Scholar] [CrossRef]
- Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of Posterior Malleolar Fractures of the Ankle. Journal of Bone & Joint Surgery American Volume. 2006, 88, 1085–1092. [Google Scholar]
- Bartonicek J, StefanKostlivy, KarelVanecek, VaclavKlika, DanielTresl, Ivo. Anatomy and classification of the posterior tibial fragment in ankle fractures. Anatomy and classification of the posterior tibial fragment in ankle fractures. Archives of orthopaedic and trauma surgery. 2015, 135. [Google Scholar]
- Su QH, Liu J, Zhang Y, Tan J, Yan MJ, Zhu K, et al. Three-dimensional computed tomography mapping of posterior malleolar fractures. World journal of clinical cases. 2020, 8, 29–37. [Google Scholar] [CrossRef]
- Quan Y, Lu H, Xu H, Liu Y, Xie W, Zhang B, et al. The Distribution of Posterior Malleolus Fracture Lines. Foot & ankle international. 2021, 42, 959–966. [Google Scholar]
- Yu T, Zhang Y, Zhou H, Yang Y. Distribution of posterior malleolus fracture lines in ankle fracture of supination-external rotation. Revue de chirurgie orthopedique et traumatologique. 2021, 107, 103000. [Google Scholar]
- Guo Z, Liu H, Shi H, Li F, Guo X, Cheng B. KD-Tree-Based Euclidean Clustering for Tomographic SAR Point Cloud Extraction and Segmentation. IEEE Geoscience and Remote Sensing Letters. 2023, 20, 1–5. [Google Scholar]
- Yen SH, Shih CY, Chang HW, Li TK, editors. Nearest neighbor searching in high dimensions using multiple KD-trees. International conference on signal processing, computational geometry and artificial visionISCGAV ‘10; 2011.
- Song, L. Epidemiological study of ankle fractures and risk factors of surgical site infection for adult ankle fractures [Doctor]: Hebei Medical University; 2019.
- Scheer RC, Newman JM, Zhou JJ, Oommen AJ, Uribe JA. Ankle Fracture Epidemiology in the United States: Patient-Related Trends and Mechanisms of Injury. The Journal of Foot and Ankle Surgery. 2020, 59, 479–483. [Google Scholar] [CrossRef]
- Bartoníček J, Rammelt S, Tuček M, Naňka O. Posterior malleolar fractures of the ankle. European journal of trauma and emergency surgery: official publication of the European Trauma Society. 2015, 41, 587–600. [Google Scholar] [CrossRef]
- Li Y, Luo R, Li B, Xia J, Zhou H, Huang H, et al. Analysis of the epidemiological characteristics of posterior malleolus fracture in adults. Journal of orthopaedic surgery and research. 2023, 18, 507. [Google Scholar] [CrossRef]
- Hou Z, Zhang Q, Zhang Y, Li S, Pan J, Wu H. A occult and regular combination injury: the posterior malleolar fracture associated with spiral tibial shaft fracture. The Journal of trauma. 2009, 66, 1385–1390. [Google Scholar]
- Stringfellow TD, Walters ST, Nash W, Ahluwalia R, Thomas P. Management of posterior malleolus fractures: A multicentre cohort study in the United Kingdom. Foot and Ankle Surgery. 2020, 27, 629–635.
- Van Wessem KJP, Leenen LPH. A rare type of ankle fracture: Syndesmotic rupture combined with a high fibular fracture without medial injury. Injury-international Journal of the Care of the Injured. 2016, 47, 766–775. [CrossRef] [PubMed]
- Haraguchi N, Armiger RS. Mechanism of posterior malleolar fracture of the ankle: A cadaveric study. OTA International. 2020, 3, e060.
- Mason LW, Marlow WJ, Widnall J, Molloy AP. Pathoanatomy and Associated Injuries of Posterior Malleolus Fracture of the Ankle. Foot & ankle international. 2017, 38, 1229. [Google Scholar]
- Terstegen J, Weel H, Frosch KH, Rolvien T, Schlickewei C, Mueller E. Classifications of posterior malleolar fractures: a systematic literature review. Archives of Orthopaedic and Trauma Surgery. 2022, 143, 4181–4220. [CrossRef]
- Yao L, Zhang W, Yang G, Zhu Y, Zhai Q, Luo C. Morphologic characteristics of the posterior malleolus fragment: a 3-D computer tomography based study. Archives of Orthopaedic & Trauma Surgery. 2014, 134, 389–394. [Google Scholar]
- Zhang L, Yang Y, Peng X, Xiong J, Sun X, Xia Z, et al. The Influence of Sagittal Angle of Posterior Malleolus Fracture on Ankle Joint Stability: A Retrospective Study of 120 Cases. Orthopaedic surgery. 2023, 15, 1799–1805. [Google Scholar] [CrossRef]
- Meijer DTD, J. N.Sierevelt, I. N.Mallee, W. H.van Dijk, C. N.Kerkhoffs, G. M.Stufkens, S. A. Guesstimation of posterior malleolar fractures on lateral plain radiographs. Injury 2015, 46, 2024–2029. [CrossRef]
- Rammelt S, Bartoníček J. Posterior Malleolar Fractures: A Critical Analysis Review. JBJS reviews. 2020, 8, e19.00207. [Google Scholar]
- Erinç S, Cam N. Does It Matter the Fixation Method of The Posterior Malleolar Fragment in Trimalleolar Fractures? Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2021, 88, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Anwar A, Lv D, Zhao Z, Zhang Z, Lu M, Nazir MU, et al. Finite element analysis of the three different posterior malleolus fixation strategies in relation to different fracture sizes. Injury-international Journal of the Care of the Injured. 2017, 48, 825–832. [Google Scholar] [CrossRef] [PubMed]
- Sun D, Shi G, Du K. Biomechanical study of different fixation methods for posterior malleolus fracture. Computer methods in biomechanics and biomedical engineering. 2024, 27, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Anwar A, Hu Z, Adnan A, Gao Y, Li B, Nazir MU, et al. Comprehensive biomechanical analysis of three clinically used fixation constructs for posterior malleolar fractures using cadaveric and finite element analysis. Scientific reports. 2020, 10, 18639. [Google Scholar] [CrossRef]
- Su YC, Wang YY, Fang CJ, Tu YK, Chang CW, Kuan FC, et al. Insights into optimal surgical fixation for posterior malleolar fractures. Bone & joint open. 2024, 5, 227–235. [Google Scholar]
- Chong LSL, Khademi MA, Reddy KM, Anderson GH. Ten year outcomes after non-fixation of the smaller posterior malleolar fragment: A retrospective cohort study. The Foot. 2024, 59, 102091. [CrossRef]
- Odak S, Ahluwalia R, Unnikrishnan P, Hennessy M, Platt S. Management of Posterior Malleolar Fractures: A Systematic Review. Journal of Foot & Ankle Surgery. 2016, 55, 140–145. [Google Scholar]
- Serlis A, Konstantopoulos G, Poulios P, Konstantinou P, Ditsios K, Aftzoglou M. The Management of Posterior Malleolus Fractures in Unstable Ankle Injuries: Where Do We Stand Now? Cureus. 2022, 14. [Google Scholar]
- Sánchez CA, Correal N, Caro D. PA Screw Versus Plate Fixation for Posterior Malleolar Fracture, Systematic Review and Meta-analysis of Complications and Functional Results. The Journal of foot and ankle surgery: official publication of the American College of Foot and Ankle Surgeons. 2024.
- Meijer DT, Gevers Deynoot BDJ, Stufkens SA, Sierevelt IN, Goslings JC, Kerkhoffs GMMJ, et al. What Factors Are Associated With Outcomes Scores After Surgical Treatment Of Ankle Fractures With a Posterior Malleolar Fragment? Clinical Orthopaedics and Related Research® 2019, 477, 863–869. [CrossRef]
- Stake IK, Bryniarski AR, Brady AW, Miles JW, Dornan GJ, Madsen JE, et al. Effect of Posterior Malleolar Fixation on Syndesmotic Stability. The American journal of sports medicine. 2023, 51, 997–1006. [Google Scholar] [CrossRef]
- Stake IK, Douglass BW, Husebye EE, Clanton TO. Methods for Biomechanical Testing of Posterior Malleolar Fractures in Ankle Fractures: A Scoping Review. Foot & ankle international. 2023, 44, 348–362. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



