1. Introduction
Climate change is one of the greatest threats to our health and, therefore, a global priority. However, there is a paradoxical link between climate change and healthcare sector; on one hand, the latter is involved in the treatment of diseases closely related to and exacerbated by climate change; on the other hand, it significantly contributes to the emissions that negatively impact health. It is estimated that the healthcare sector is responsible for over 8% of national greenhouse gas emissions in economically advanced countries [
1]. Specifically, operating rooms are the primary source of emissions within hospital facilities [
2].
As a result, there is a need to adopt green strategies in the surgical field. To mitigate the environmental impact of surgical activity, the goals to pursue are defined by the "5 R's rule": reduce, reuse, recycle, rethink and research [
3]. Obviously, it is imperative to tackle sustainability without compromising the quality of care in any way.
Waste must be combated by planning water consumption through the installation of automatic or foot-operated taps, following the “rub, don’t scrub” principle, limiting the use of nitrile gloves and rationalizing the number of surgical instruments [4-6]. It is crucial to prefer reusable gowns, drapes and surgical instruments, whose carbon footprint is way smaller compared to the one of the single-use counterparts [
7]. If possible, it is essential to opt for waste segregation and to modify the flow of waste from operating rooms [
8], recycling non-infectious materials such as plastic. Moreover, anesthetic procedures should be reconsidered, favoring local anesthesia, total intravenous anesthesia (TIVA) or, when inhalation anesthesia is necessary, anesthetic gases with a low global warming potential (GWP), such as sevoflurane (better than isoflurane and desflurane) [9-11]. The appropriateness of surgical procedures should be reevaluated, where new approaches and technologies ensure the safety of the outcome. Finally, research is essential.
The Breast Surgery Clinic of the IRCCS Ospedale Policlinico San Martino specializes in both benign and malignant breast diseases and performs over 1,200 surgeries annually, with more than 700 of these specifically for breast cancer.
Breast cancer is the most frequently diagnosed cancer and the leading cause of cancer-related mortality in the female population. The net 5-year survival rate from diagnosis is 88% [
12]. Thanks to increased awareness among women and screening programs, a significant portion of breast cancers is diagnosed at an early stage, when surgical approaches can be more conservative and radiation or systemic therapy more effective. Currently, the standard loco-regional treatment for early-stage breast cancer consists of conservative surgery (quadrantectomy) combined with radiotherapy or radical surgery (mastectomy), depending on a variety of factors. Whenever possible, quadrantectomy combined with radiotherapy is the first-choice approach in women with stage I-II invasive breast cancer [13-14].
The primary endpoint of this study is to evaluate the reduction of the environmental impact of our surgical activity secondary to the adoption of the following measures: identification of the sentinel lymph node with indocyanine green (ICG); local anesthesia and intravenous sedation; waste reduction and minimization of waste production; use of reusable gowns, drapes and surgical instruments; separate collection of non-infectious plastic waste.
Moreover, the secondary endpoints of this study are to confirm the non-inferiority, in terms of detection rate, of ICG compared to technetium-99 metastable (99mTc) and to ascertain the correlation between the duration of the hospital stay and the type of anesthesia administered.
2. Materials and Methods
From September 2023 to May 2024, a single-center, prospective, two-arm study was conducted at the Breast Surgery Clinic of the IRCCS Ospedale Policlinico San Martino on 34 women with invasive breast cancer T1-2, cN0, who underwent quadrantectomy and sentinel lymph node biopsy (SNLB): 17 according to a standard approach, 17 according to a green approach, based on the "5 R's rule" (reduce, reuse, recycle, rethink, research).
Patients treated with the green approach underwent procedures that are already validated and well-established, therefore the preliminary approval from the ethics committee was not required.
Inclusion criteria: tumor with maximum size ≤ 50 mm (T1-T2); indication for unilateral breast-conserving surgery (BCS); axillary lymph nodes negative on pre-operative axillary ultrasound (cN0).
Exclusion criteria: contraindication to unilateral BCS; axillary lymph nodes positive on both pre-operative axillary ultrasound and pre-operative cytologic-histologic examination; age ≥ 80 years (surgical staging of the axilla not necessary); neoadjuvant chemotherapy (requiring intraoperative frozen section examination of the sentinel lymph node, with consequent longer operating times); calcifications and/or parenchymal distortions (requiring intraoperative RX of the surgical specimen, with consequent longer operating times); hypersensitivity to ICG, sodium iodide, or iodine.
Patients treated with the standard approach underwent lymphoscintigraphy the day before or the day of surgery. This exam requires the subcutaneous injection - in the peritumoral area - of 99mTc, a radiotracer that reaches the axilla by lymphatic diffusion and deposits in the sentinel lymph node, which is visualizable with ease on lymphoscintigraphy and subsequently identifiable in the operating room with a specific probe. These patients then underwent mixed general anesthesia, which involves the combined administration of drugs both by inhalation and intravenously, with the placement of a laryngeal mask or, sometimes, orotracheal intubation.
Lastly, the standard, high environmental impact approach is mainly characterized by the significant production of waste, resulting from the inappropriate use of disposable non-sterile gloves by the operating room staff, the use of disposable gowns, drapes and surgical instruments, the orientation of the surgical specimen with disposable suture thread.
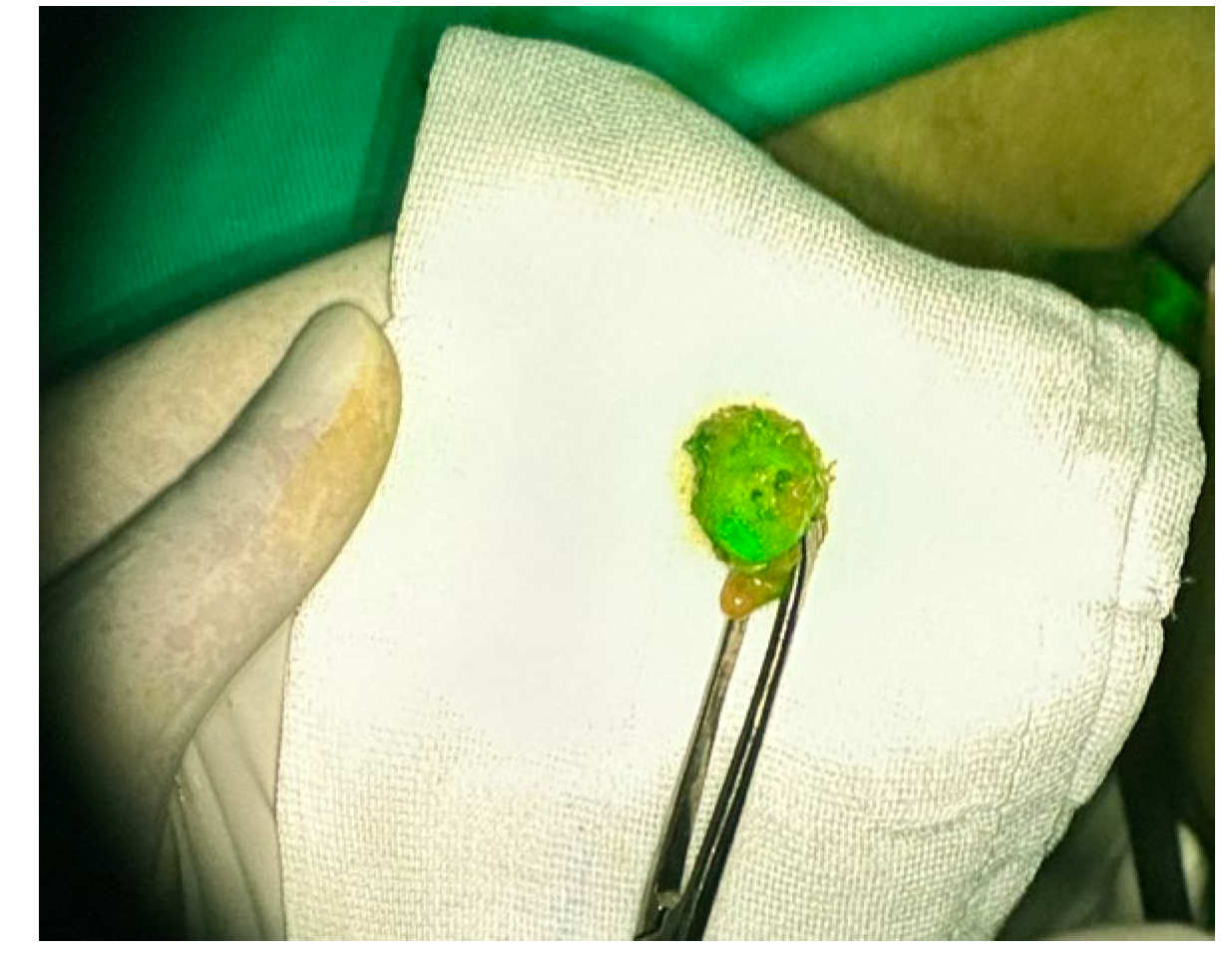
Conversely, patients treated with the green approach did not undergo lymphoscintigraphy: in this case, the identification of the sentinel lymph node required the subcutaneous injection - directly in the operating room, immediately before the skin incision, always in the peritumoral area - of 1 ml of ICG, a fluorescent tracer that, similar to 99mTc, reaches the axilla by lymphatic diffusion and deposits in the sentinel lymph node, which, located after 15-20 minutes using infrared optics, appears green and is easily recognizable.
During this procedure, a solution obtained by diluting a vial of 25 mg of powdered ICG (Verdye) in 5 ml of water for injection preparations was used. The concentration of the solution to be injected was kept constant for all the patients in the study. As mentioned above, the injection of ICG preceded the surgical act, which - otherwise - did not vary.
The second main difference between the green approach and the standard one is represented by the type of anesthesia administered: indeed, patients treated with the green approach underwent a minimally invasive mixed technique, which combines local anesthesia, analgesia (with opioids) and intravenous sedation (with hypnotics such as propofol and benzodiazepines). The procedure can be conducted without any pain and in conditions of total unconsciousness, while avoiding any invasive maneuvers typical of general anesthesia and, thus, the impairment of respiratory function, which is maintained autonomously and spontaneously or supported by oxygen supplementation at a flow rate of 2-4 l/min as needed. The concept of minimal invasiveness was already implemented locally by applying an anesthetic cream based on lidocaine and prilocaine (Emla) to the marked surgical site, both breast and axillary region, approximately 45-60 minutes before the procedure; the short-term effect of the topical anesthetic can be prolonged by infiltrating the skin flaps with ropivacaine (Naropin) which, especially towards the end of the procedure, can allow for a reduction in the intravenous administration of both analgesics and hypnotics, speeding up the waking process. Obviously, this anesthetic technique requires a close intraoperative monitoring by the anesthetist, who adjusts the dose of the administered drugs depending on the phase of the procedure, the depth of the sedation (assessed by the Bispectral Index [BIS], which is derived from the electroencephalogram), the values of the vital parameters.
The third difference between the green approach and the standard one lies in waste reduction and minimization, achieved through both the use of reusable gowns, drapes and surgical instruments and the orientation of the surgical specimen with the same titanium clips (a standard pack contains 10 pieces) placed to outline the tumor bed.
Lastly, the green approach should be characterized by a sustainable management of non-infectious plastic waste, largely represented by the packaging of medical devices and common surgical instruments used during the peri- and intraoperative phase. In collaboration with the Department of Chemistry and Industrial Chemistry (DCCI) of the University of Genoa, a qualitative and quantitative analysis of the materials constituting the packaging collected in the operating room for each surgery was conducted, in order to quantify their environmental impact. The sampling phase, carried out within the operating room itself, was followed by the characterization phase of the materials, which had involved the use of three instrumental analysis techniques: Fourier Transform Infrared Spectroscopy (FT-IR), Thermogravimetric Analysis (TGA) and Differential Scanning Calorimetry (DSC).
3. Results
Among the patients treated with the standard approach, the average age was 59.7 years (range 37-79 years).
The sentinel lymph node was identified and removed in 100% of cases (17/17).
The average number of axillary lymph nodes removed was 1.9 per patient.
The total duration of the surgery was ≤ 60 minutes in 82.3% of cases (14/17), > 60 minutes but ≤ 90 minutes in 11.8% of cases (2/17), > 90 minutes in 5.9% of cases (1/17); the average duration was 53 minutes (range 35-95 minutes).
As for the length of hospital stay, all the 17 patients treated with the standard approach were discharged on the first postoperative day.
Among the patients treated with the green approach, the average age was 58.8 years (range 43-79 years).
The sentinel lymph node was identified and removed in 94.1% of cases (16/17); in 5.9% of cases (1/17), it could not be identified due to the tracer’s failure to move through the lymphatic pathways.
The time to visualize the sentinel lymph node (ICG administration at t0) was ≤ 15 minutes in 18.7% of cases (3/16), > 15 minutes but ≤ 20 minutes in 56.3% of cases (9/16), > 20 minutes in 25.0% of cases (4/16).
The average number of axillary lymph nodes removed was 1.6 per patient.
The total duration of the surgery was ≤ 60 minutes in 47.1% of cases (8/17), > 60 minutes but ≤ 90 minutes in 35.3% of cases (6/17), > 90 minutes in 17.6% of cases (3/17); the average duration was 71 minutes (range 40-180 minutes).
As for the length of hospital stay, among the 17 patients treated with the green approach, 10 (58.8%) were discharged on the same day of surgery, 6 (35.3%) on the first postoperative day and 1 (5.9%) on the second postoperative day.
Figure 1.
Sentinel lymph node removed from a patient who received ICG.
Figure 1.
Sentinel lymph node removed from a patient who received ICG.
4. Discussion
Taking as an example the quadrantectomy and SLNB procedure, recommended for women affected by invasive breast cancer, T1-2, cN0, three critical issues were identified: preoperative lymphoscintigraphy, mixed general anesthesia, lack of separate collection of non-infectious plastic waste.
Lymphoscintigraphy is a non-invasive diagnostic imaging technique recommended for studying the lymphatic system and visualizing axillary lymph nodes in patients undergoing SLNB. Although it is the gold standard with an estimated diagnostic accuracy of 96%, it presents some logistical and economic limitations: the need for nuclear medicine to provide and administer the radiotracer, the risk associated with the use of the radiotracer, the need for radioprotection, high costs. Therefore, the scientific community has been working to find alternative tracers that can overcome these limitations without compromising diagnostic accuracy.
Currently, in oncological surgery, the injection of ICG in the peritumoral area is approved for identifying the sentinel lymph node in cases of oropharyngeal, colon, prostate, uterus and breast cancer [
15]; it is performed in the operating room, soon after the induction of general anesthesia or, as in our study, intravenous sedation, with great benefits for both the environment and the patients, who are spared a hospital visit the day before the surgery and the administration of a radiotracer. Additionally, costs are reduced.
According to the most recent literature, ICG allows the identification of the sentinel lymph node in 96-99% of cases [
16]. It is recognized as the only recommended alternative to radioisotopes by both the European Society of Medical Oncology (ESMO) and the Japanese Breast Cancer Society (JBCS) [17-18]. In our experience, the sentinel lymph node was identified in 100% of patients who received 99mTc and in 94.1% of patients who received ICG. This percentage gap can be justified by the small population examined. Furthermore, the administration of ICG seems to correlate with an increase in the average duration of surgery, which was 71 minutes in cases treated with the green approach and 53 minutes in cases treated with the standard approach. Operating times were ≤ 60 minutes in 47.1% of cases treated with the green approach and in 82.3% of cases treated with the standard approach. This bias between the two approaches is the result of an inaccurate selection of patients in the study, especially regarding the evaluation of BMI, possible alterations in the lymphatic transport index, previous surgeries, etc.
Regarding the anesthetic approach, the current standard typically involves patients eligible for BCS receiving mixed general anesthesia, which includes both intravenous and inhalational drugs. These latter are potent greenhouse gases with a significant carbon footprint. To reduce their environmental impact, it is essential to abandon mixed general anesthesia, which also necessitates the placement of a laryngeal mask or orotracheal intubation and the use of drugs that cause respiratory risks in the immediate postoperative period, often requiring at least one night of hospitalization as a precaution.
A possible solution is the use of a minimally invasive mixed technique, combining topical and infiltrative local anesthesia with intravenous sedation. This approach focuses on personalizing procedures based on the patient’s type (pain threshold, individual pharmacokinetics, etc.) and the phase of the surgery, requiring maximum synergy between the surgeon and the anesthetist and optimizing peri- and intraoperative processes. During surgery, the anesthetist must appropriately adjust the drug infusion to the minimum necessary dosage, based on intraoperative parameters such as blood pressure, heart rate, respiratory rate, pupillary reaction, etc.
This avoids standardized administration based solely on body weight and accelerates anesthetic recovery times, affecting both the duration of the procedure and the total number of operations that can be performed during the surgical session. Additionally, patients can consume both solids and liquids as soon as they return to the ward. This contributes to a "softer" care experience, potentially concluding within 6-8 hours. Obviously, the length of stay also depends on the time of day the surgery is performed: discharge is usually possible on the same day for procedures performed in the morning, whereas it is evaluated on a case-by-case basis for procedures performed in the afternoon.
In our experience, 58.8% of patients undergoing this anesthetic technique were discharged the same day, whereas 100% of patients undergoing mixed general anesthesia spent one night in the hospital. This resulted in a halving of hospitalization times and a reduction in healthcare costs.
Lastly, according to our experience, for a single quadrantectomy and SLNB, it is possible to collect up to 500 g of plastic material, of which - as shown in
Table 1 - only 228.6 g is recyclable (45.7%). Considering that a single procedure lasts about 60 minutes and up to 8 procedures can be performed per day, it is expected that our operating room generates up to 475.5 kg of recyclable plastic waste per year. This figure pertains exclusively to our surgical activities: to understand its real scope, it is sufficient to extend it to all surgical settings across the entire national territory.
In cases where recycling is not possible, the collected consumable materials allow for energy production through waste-to-energy plants: this solution represents one of the key strategies of the European Union for a virtuous and sustainable waste cycle management, which includes, in order, the reduction of waste production, the reuse of objects, material recycling, energy recovery and landfill disposal [
19]. Through combustion, waste-to-energy plants generate energy that can be used to provide electricity or district heating; the electricity fed into the grid replaces a portion of centralized power production, avoiding its associated environmental impacts, expressed as primary energy consumption and atmospheric emissions; similarly, the provision of heat through district heating allows for the replacement of the operation of thermal power plants by consumers.
Moreover, even though combustion also produces emissions, from the perspective of climate change, waste-to-energy plants have an impact that is 8 times lower than that of landfills, which occupy space for centuries, produce leachate that must be treated and emit methane gas, which is significantly more impactful than the CO2 produced by combustion [
20].
5. Conclusions
The impact of climate change is now undeniable: the extreme weather events we repeatedly witness are direct consequences and represent a threat to our health. Given this dramatic scenario and the significant environmental impact of the healthcare sector, surgical activity is surely one of the main contributors. Therefore, it is essential to adopt strategies in the operating room that have a positive impact on the environment and, if possible, provide benefits to patients. However, there is still a lack of awareness on this issue among healthcare professionals: it would be desirable to establish dedicated interdisciplinary teams to implement appropriate measures, which should be periodically discussed with all team members.
Author Contributions
Conceptualization, R.A. and P.F.; methodology, R.A., S.V., C.B. and P.F.; data curation, R.A., S.V., C.B., R.D., L.C., F.M., F.D., C.C., C.M., C.B., M.P., S.F., M.C. and M.A.; writing—original draft preparation R.A., S.V., C.B., R.D. and P.F.; writing—review and editing, R.A., M.G., R.D. and P.F.; supervision, M.G., F.D.C. and P.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study: all patients underwent procedures that are already validated and well-established.
Informed Consent Statement
Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available in this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA 2009, 302, 1970. [Google Scholar] [CrossRef]
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 2017, 1, 381–388. [Google Scholar] [CrossRef]
- Kagoma Y, Stall N, Rubinstein E, Naudie D. People, planet and profits: the case for greening operating rooms. Can Med Assoc J 2012, 184, 1905. [Google Scholar] [CrossRef]
- Gaspar GG, Menegueti MG, Lopes AER, Santos ROC, De Araújo TR, Nassiff A, et al. Alcohol-based surgical hand preparation: translating scientific evidence into clinical practice. Antimicrob Resist Infect Control 2018, 7, 80. [Google Scholar] [CrossRef]
- Wilson J, Prieto J, Singleton J, O’Connor V, Lynam S, Loveday H. The misuse and overuse of non-sterile gloves: application of an audit tool to define the problem. J Infect Prev 2015, 16, 24–31. [Google Scholar] [CrossRef]
- Chasseigne V, Leguelinel-Blache G, Nguyen TL, De Tayrac R, Prudhomme M, Kinowski JM, et al. Assessing the costs of disposable and reusable supplies wasted during surgeries. Int J Surg 2018, 53, 18–23. [CrossRef]
- Weiss A, Hollandsworth HM, Alseidi A, Scovel L, French C, Derrick EL, et al. Environmentalism in surgical practice. Curr Probl Surg 2016, 53, 165–205. [Google Scholar] [CrossRef]
- Shaner H, McRae G. Invisible costs/visible savings: innovations in waste management for hospitals. Surgical Services Management 1996, 2, 17–21. [Google Scholar]
- Bernat M, Boyer A, Roche M, Richard C, Bouvet L, Remacle A, et al. Reducing the carbon footprint of general anaesthesia: a comparison of total intravenous anaesthesia versus a mixed anaesthetic strategy in 47.157 adult patients. Anaesthesia 2024, 79, 309–317. [Google Scholar] [CrossRef]
- Sherman J, Le C, Lamers V, Eckelman M. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg 2012, 114, 1086–1090. [Google Scholar] [CrossRef]
- McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth 2020, 125, 680–692. [Google Scholar] [CrossRef]
- AIOM. I numeri del cancro in Italia 2023. Available at: https://www.aiom.it/i-numeri-del-cancro-in-italia/.
- Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002, 347, 1233–1241. [Google Scholar] [CrossRef]
- Litière S, Werutsky G, Fentiman IS, Rutgers E, Christiaens MR, Van Limbergen E, et al. Breast conserving therapy versus mastectomy for stage I–II breast cancer: 20-year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol 2012, 13, 412–419. [Google Scholar] [CrossRef]
- Xiong L, Gazyakan E, Yang W, Engel H, Hünerbein M, Kneser U, et al. Indocyanine green fluorescence-guided sentinel node biopsy: a meta-analysis on detection rate and diagnostic performance. Eur J Surg Oncol 2014, 40, 843–9. [Google Scholar] [CrossRef]
- Pellini F, Bertoldi L, Deguidi G, Perusi N, Caldana M, De Flaviis M, et al. The use of indocyanine green as the only tracer for the identification of the sentinel lymph node in breast cancer: safety and feasibility. Gland Surg 2022, 11, 1139–1147. [Google Scholar] [CrossRef]
- Senkus E, Kyriakides S, Penault-Llorca F, Poortmans P, Thompson A, Zackrisson S, et al. ESMO Guidelines Working Group. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013, 24 (Suppl 6), vi7–23. [Google Scholar] [CrossRef]
- Jinno H, Inokuchi M, Ito T, Kitamura K, Kutomi G, Sakai T, et al. The Japanese Breast Cancer Society clinical practice guideline for surgical treatment of breast cancer, 2015 edition. Breast Cancer 2016, 23, 367–77. [Google Scholar] [CrossRef]
- Directive 2008/98/EC of the European Parliament and of the Council of 19 November 2008 on waste and repealing certain Directives. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:02008L0098-20180705.
- Cernuschi S, Grosso M, Viganò F, Zanetti MC, Panepinto D, Ragazzi M, et al. Libro bianco sull’incenerimento dei rifiuti urbani. 2020. Available at: https://www.utilitalia.it/ambiente/studi-e-ricerche/list/2daa7be0-39cd-46a3-8e71-edbf1d121380.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).