1. Introduction
Esophageal atresia (EA) is the most prevalent congenital anomalies affecting the esophagus, occurring in approximately 1 in 3000 to 4000 live births. [
1,
2] This condition results from an embryonic defect characterized by a disruption in the normal development of the esophagus [
3], often involving multigenic factors and epigenetic modifications of genes. [
4,
5] As a consequence, various types of esophageal discontinuities can manifest, with or without the presence of a tracheoesophageal fistula (TEF), as classified by the Gross Classification system. [
6] It's not uncommon for EA patients to present with additional associated anomalies or defects affecting other organ systems, significantly impacting their management and prognosis. [
5,
7]
Advancements in intensive care, anaesthesia, ventilatory and nutritional support, and surgical techniques have all played pivotal roles in achieving a significant outcome enhancement for individuals with EA over the last two decades, with survival rates now surpassing 90%. [
1,
8,
9,
10]
Ongoing advancements in surgical technology and techniques, coupled with a multidisciplinary approach to care, are continuously refining our understanding and management of complex EA cases, further improving outcomes for affected individuals. Specifically, the introduction of thoracoscopy has revolutionized the approach to EA repair by offering a minimally invasive alternative to traditional thoracotomy. This technique presents several advantages, including reduced postoperative pain, minimal scarring, and a lower risk of skeletal deformities. [
11] However, it's important to note that thoracoscopy has not entirely replaced thoracotomy. While thoracoscopy offers numerous benefits, it remains a challenging technique that requires extensive training and expertise. Consequently, both approaches continue to be utilized based on individual patient characteristics and the preferences and skills of the surgical team.
As mortality rates for EA have decreased, there has been a growing emphasis on assessing functional outcomes and quality of life (QoL) in affected individuals. [
12,
13] Assessing QoL provides insights into the holistic well-being and functional status of individuals beyond mere survival outcomes. Various aspects of life can be significantly impacted by the long-term complications associated with EA spanning from gastrointestinal and respiratory function to nutrition, social activities, and relationships, ultimately influencing overall QoL. [
13]
To date, there are multiple studies evaluating QoL in EA patients, focusing on understanding how this congenital condition affects individuals over the long term [
14,
15] but none of the compares thoracoscopy and thoracotomy in terms of quality of life.
The aim of the study was to comprehensively analyze the long-term complications and outcomes in terms of QoL of children undergoing thoracotomy and thoracoscopy for type III EA repair.
2. Methods
A retrospective analysis involving children who underwent thoracotomy or thoracoscopy for repair of type III EA was carried out. The study included all children diagnosed with type III EA and treated by the same surgeon (GC) at the Pediatric Surgery Unit of Salesi Children's Hospital between 2014 and 2022, with a follow-up period of at least 1 years. Thoracoscopic esophageal atresia (EA) repair was introduced at our institution in 2016 following specialized training, and all patients treated with this method by one surgeon since then were included in the study.
Participants were categorized into two groups: those who underwent thoracotomy for repair of type III EA and those who underwent thoracoscopic repair for the same condition.
The medical records were carefully examined for personal and perinatal information, associated malformations, details of surgical interventions and complications, gastrointestinal and respiratory current symptoms, and actual anthropometric data. Additionally, Quality of Life (QoL) were investigated through Esophageal Atresia QoL (EA QoL) and Pediatric QoL (Peds QL) 4.0 standardized and validated questionnaires.
Prior to the start of the survey, all parents provided consent for the retrospective analysis of anonymized data for the purpose of clinical research, and prevention of esophageal atresia and related conditions.
2.1. Perinatal Data
Perinatal details such as sex, gestational age and birth weight were recorded for children with type III EA according to Gross classification [
6].
Associated anomalies were divided into cardiovascular, gastrointestinal, anorectal, urogenital, limb, skeletal, respiratory, central nervous system, and other malformations (eye, ear, VACTERL association, CHARGE syndrome, chromosomes trisomy).
2.2. Surgical Information
Primary surgery details included the type of procedure performed, such as primary repair, prior gastrostomy with delayed anastomosis, staged repair, and other procedures for associated malformations. Secondary surgery such as revisional surgery for recurrence of TEF, dilations for stenosis treatment, laparoscopic Nissen fundoplication surgery for gastroesophageal reflux were recorded.
We also analyzed post-surgical complications including recurrence of tracheoesophageal fistula, anastomotic stenosis or leakage, and diagnosis of gastroesophageal reflux.
2.3. Follow up and Clinical Outcome
Follow-up were scheduled every 3 months during the first year of life, every 6 months during the subsequent two years, and then annually until adolescence.
Digestive symptoms, feeding difficulties and respiratory disorders were assessed since the beginning of the study. Digestive symptoms included dysphagia, thoracic burn, painful swallowing, regurgitation, and vomiting problems. Feeding difficulties comprised avoiding certain foods, eating small portions, adjusting food consistency, needing more than 30 minutes per meal, increasing fluid intake during meals, nutrition through gastrostomy or infusion pump. Respiratory symptoms included cough, wheezing at physical activity, dyspnea at physical activity, airway infection, chest tightness and asthma.
2.4. Anthropometric Data
Information on the children's current weight (in kilograms) and height (in centimeters) were collected. Growth percentile for weight and height was calculated on current age using CDC growth charts [
16].
2.5. Quality of Life Questionnaire
Since 2023, the quality of life in all patients has been systematically evaluated using the standardized and validated questionnaires Esophageal Atresia Quality of Life (EA QoL) and the Pediatric Quality of Life Inventory (Peds QoL) 4.0.
The specific scale EA QoL by Dellenmark-Blom et al. (2017) [
14], adapted for different age groups included:
EA-QoL version for children aged 2–7 years, completed by parents, encompassing 17 items including three categories: eating, physical health, social relations.
EA-QoL version for children aged 8–12 years, provided by parents, comprising 24 items covering four categories: eating, social relationships, body perception, and physical health".
Each item was scored on a 5-point Likert scale, with higher scores indicating better quality of life, and final scores were transformed to a 0 to 100 scale.
The generic scale Peds QoL 4.0 [
17] adapted for different age groups included:
Peds QoL version for infants aged 1–12 months, filled out by parents, including 36 items comprising physical functioning and symptoms, emotional, social, and cognitive functioning.
Peds QoL version for infants aged 13–24 months, completed by parents, containing 45 items involving physical functioning and symptoms, emotional, social, and cognitive functioning.
Peds QoL version for toddles aged 2-4 years, answered by parents, comprising 21 items covering physical functioning, emotional, social, and day care functioning.
Peds QoL version for young children aged 5-7 years, provided by parents, covering 23 items concerning physical functioning, emotional, social, and school functioning.
Peds QoL version for children aged 8-12 years, answered by parents, including 23 items about physical functioning, emotional, social, and day care functioning.
Each item was assessed reporting the frequency of each problem on a 5-point Likert scale, with higher scores indicating better quality of life, and final scores were transformed to a 0 to 100 scale.
2.6. Statistical Analysis
The demographic characteristics of patients with EA were summarized using descriptive statistics. For normally distributed quantitative data, we reported the mean ± standard deviation (SD). Independent sample t-tests were employed to compare differences between groups. For non-normally distributed quantitative data, we provided medians with interquartile ranges. Mann–Whitney U tests were utilized to compare differences between groups. Categorical data were compared between groups using chi-square (χ2) tests or Fisher’s exact tests. A significance level of P<0.05 was used for statistical significance. All statistical analyses were conducted using Graphpad Prism software.
3. Results
A total of 34 children, born with type III EA, were treated between 2014 and 2022 at the Pediatric Surgery Unit of Salesi Children's Hospital. Thirty-two patients answered the questionnaire, with a response rate of 94,1%, including 17 thoracotomy and 15 thoracoscopy.
3.1. Perinatal Data
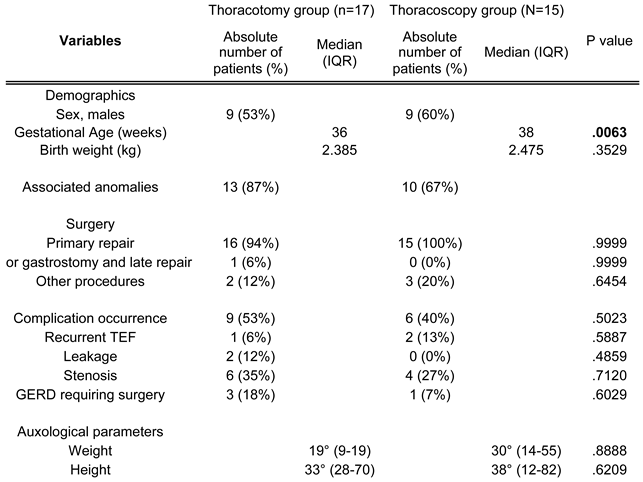
The gender was not statistically different between the two groups, including 9 (53%) males in the thoracotomy group (TCg) and 9 (60%) in the thoracoscopy group (TSg) (
Table 1).
Median birth weight was not significantly different between two groups (median [2.385;2.475] kg, p=.3529) while gestational age showed statistically difference (median [36;38] weeks, p=.0063), displaying that premature babies mostly underwent thoracotomy rather than thoracoscopy.
In the TCg, 13 (87%) patients had 15 associated malformations, comprising interatrial or interventricular defect with cardiac shunt (7), Fallot’s tetralogy (1), aortic arc anomalies (2), duodenal atresia (1), anorectal malformation (1), first metacarpal agenesis (1), tracheomalacia (2).
In the TSg there were 20 associated malformations in 10 (67%) patients, including interatrial or interventricular defect with cardiac shunt (6), hypoplastic left heart (1), pulmonary artery stenosis (1), cardiac isthmic stenosis (1), Hirschsprung disease (1), anorectal malformation (1), hydronephrosis (1), double renal ectopic kidney (1), cystic igroma (1), hemi vertebrae (2), subependymal cyst (1), vascular tracheal compression (1), preauricular appendix (1), George’s Syndrome (1). The number of associated malformations did not statistically differ between the two groups.
3.2. Surgical Information
In the TCg, 16 (94%) children underwent primary repair for EA, while 1 (6%) child required gastrostomy placement and delayed repair. Additionally, 2 (12%) children underwent other surgeries for associated malformations: one underwent a posterior sagittal anorectoplasty according to Pena for anorectal malformation, while the other underwent a duodenoduodeno-anastomosis according to Kimura for duodenal atresia.
In the TSg, 15 (100%) children underwent primary repair for EA. Among them, 3 (20%) children required other surgeries for associated malformations: one underwent colostomy followed by laparoscopic-assisted posterior sagittal anorectoplasty for anorectal malformation, another underwent tracheostomy followed by cardiac surgery for vascular tracheal compression causing respiratory failure, and the third underwent a laparoscopic-assisted endorectal pull-through for Hirschsprung disease.
Postoperative complications occurred in 9 (53%) patients in the TCg, including 1 (6%) case of recurrent TEF requiring revisional surgery and later on a dilatation program, 2 (12%) cases of leakages managed conservatively, and 6 (35%) cases of stenosis necessitating an endoscopic dilatation program.
In the TSg, 6 (40%) children experienced postoperative complications, comprising 2 (13%) cases of minimal recurrent TEF managed conservatively and 4 (27%) cases of stenosis requiring an endoscopic dilatation program. Additionally, one patient underwent thoracoscopic revision due to suspicion of recurrent TEF, which yielded negative results.
Furthermore, gastroesophageal reflux disease (GERD) required surgical correction with minimally invasive Nissen’s fundoplication in 3 (18%) children from TCg and 1 (7%) child from TSg, performed between the age of 1 and 7. The median number of dilatation required for stenosis was 5 (range 1-5) in the TCg and 2 (range 1-5) in the TSg. The number of concomitant surgeries for associated malformations and the number of postoperative complications did not statistically differ between the two groups.
3.3. Follow up and Clinical Outcome
The mean follow up was 7,3 ± 2,5 years for the TCg and 4,9 ± 1,7 years for the TSg.
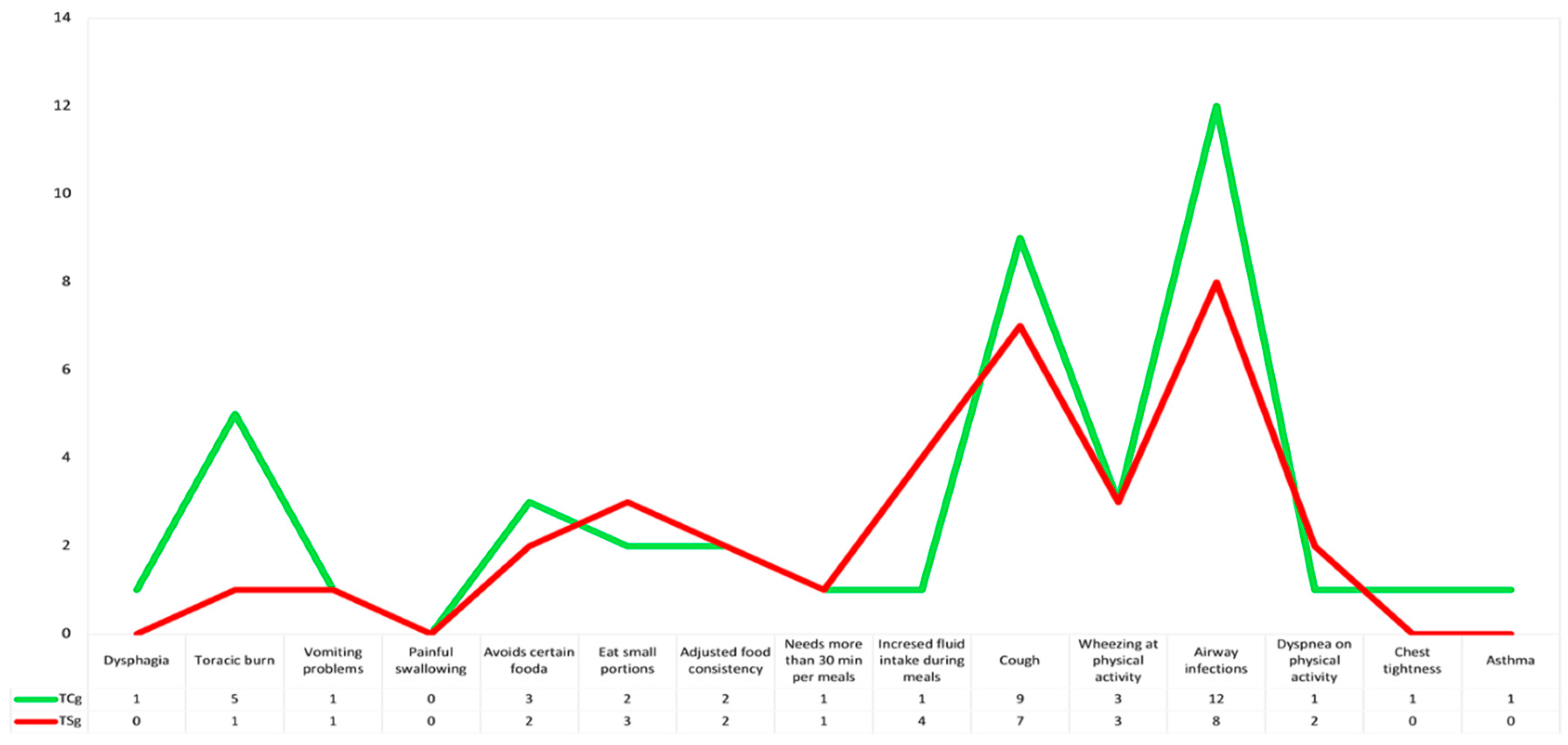
During the last year of follow-up, 13 (76%) children in the TCg had 43 symptoms: 5 patients had digestive symptoms (1 dysphagia, 5 thoracic burn and 1 vomiting problems), 4 patients had feeding difficulties (3 avoiding certain foods, 2 eating small portions, 2 adjusting food consistency, 1 needing more than 30 minutes per meal and 1 increasing fluid intake during meals) and 12 children had respiratory symptoms (9 cough, 3 wheezing at physical activity, 1 dyspnea at physical activity, 12 airway infection, 1 chest tightness and 1 asthma) (
Figure 1).
In the TSg 13 (87%) children had 34 symptoms in the last year: 2 patients had digestive symptoms (1 thoracic burn and 1 vomiting problems), 6 patients had feeding difficulties (2 avoiding certain foods, 3 eating small portions, 2 adjusting food consistency, 1 needing more than 30 minutes per meal and 4 increasing fluid intake during meals) and 12 children had respiratory symptoms (7 cough, 3 wheezing at physical activity, 2 dyspnea at physical activity, 8 airway infection) (
Figure 1).
Digestive and respiratory symptoms, as well as feeding difficulties, did not show statistically significant differences between the two groups (respectively, p=0.4025, p=0.6911, p=0.4501)
3.4. Anthropometric Data
The patient’s mean age was 6,7 ± 2,4 years in the TCg and 4,5 ± 1,6 years in the TSg.
In the TCg the average weight of the population was 23,4 ± 8,5 Kg located at the 19 (IQR 9-19) percentile, while the average height was 118,7 ± 22,2 cm found at the 33 (IQR 28-70) percentile.
In the TSg, 16,1 ± 3,2 Kg was the average weight of the population, located at the 30 (IQR 14-55) percentile, while 104,4 ± 12,0 cm was the average height, placed at the 38 (IQR 12-82) percentile.
3.5. Quality of Life Questionnaire
Both the EA QoL and the Peds QoL questionnaires were completed by parents. In the TCg, 12 parents (71%) were mothers, with a mean age of 43.6 ± 7.9 years. In the TSg, 13 parents (87%) were mothers, with a mean age of 37.7 ± 6.5 years.
EA QoL in the TCg showed a median of 91 (IQR 88-97) for eating, 83 (IQR 83-95) for physical health and 100 (IQR 100) for social relations in children between 2 and 7 years, while there was a median of 94 (IQR 84-97) for eating, 80 (IQR 75-82) for physical health, 100 (IQR 83-100) for social relations and 100 (IQR 97,5-100) for body perception in children between 8 and 9 years.
The total score for EA QoL in children undergoing thoracotomy for EA repair was 91 (IQR 89-93).
EA QoL in the TSg revealed a median of 97 (IQR 88-100) for eating, 96 (IQR 88-100) for physical health and 100 (IQR 100) for social relations in children between 2 and 7 years.
The total score for EA QoL in children undergoing thoracoscopic EA repair was 96 (IQR 91-99).
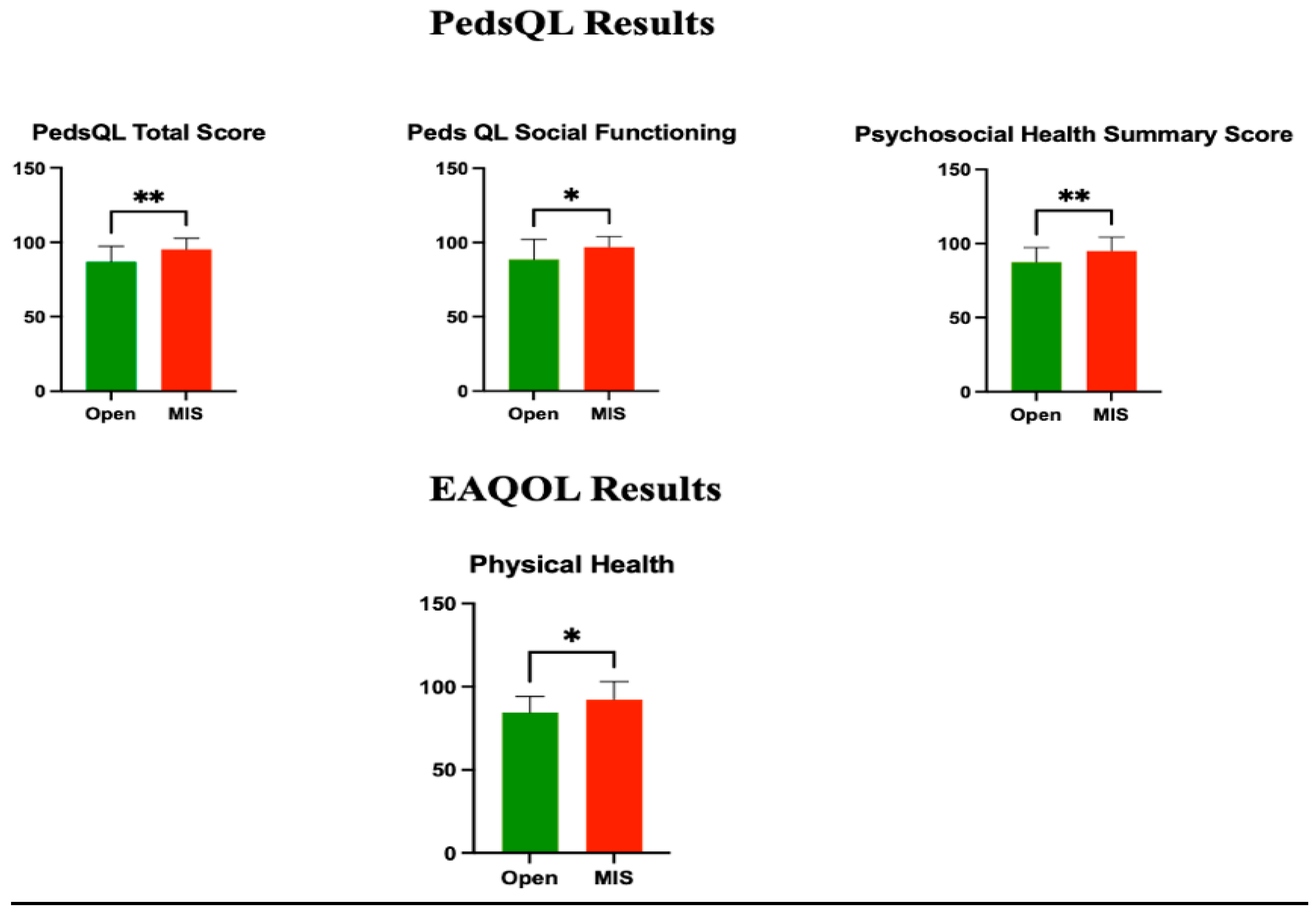
Analyzing EA QoL, there was no statistical difference in social relations (p=0.3473), eating (p=0.5749), and total score ( p=0.1710), but we found statistically significant difference in physical health between the two groups (p=0.0119), demonstrating that thoracoscopic repair has a significant impact on physical health (
Figure 2).
In the TCg, the Peds QoL assessment revealed the following medians and interquartile ranges (IQRs): 91 (IQR 75-100) for physical functioning, 95 (IQR 80-100) for emotional functioning, 90 (IQR 80-100) for social functioning, and 90 (IQR 73-100) for school functioning. The physical health summary score was 91 (IQR 75-100), the psychosocial health summary score was 88 (IQR 85-93), and the total score was 91 (IQR 82-94).
In the TSg, the Peds QoL assessment found the following medians and IQRs: 100 (IQR 95-100) for physical functioning, 100 (IQR 90-100) for emotional functioning, 100 (IQR 100) for social functioning, and 100 (IQR 95-100) for school functioning. The physical health summary score was 100 (IQR 96-100), the psychosocial health summary score was 98 (IQR 95-100), and the total score was 99 (IQR 93-100).
There was no statistically significant difference between the two groups in physical functioning (p=0.0706), emotional functioning (p=0.1631), and school functioning (p=0.1310). However, social functioning was found to be significantly different (p=0.0474) between the thoracotomy and thoracoscopy groups, showing that thoracoscopic repair has a significantly positive effect on social functioning. When comparing the Peds QoL summary scores between the two groups, statistically significant differences were observed in the psychosocial health summary score (p=0.0069) and the total score (p=0.0043) in favor of thoracoscopy, while no significant difference was found for the physical health summary score (p=0.0706) (
Figure 2).
Examining PedsQL, total score (p=0.0043), social functioning (p=0.0474) and psychosocial-health score (p=0.0069) were statically significant different, while analyzing EAQoL we found statistically significant difference in physical health (p=0.0119).
4. Discussion
EA stands as one of the most severe congenital gastrointestinal developmental anomalies, necessitating neonatal surgical intervention.
The optimal surgical approach remains a topic of debate and ongoing research within the medical community [
18]
. To determine the potential superiority of one surgical method over another and to establish consensus among experts, it is crucial to consider post-operative outcome and long-term prognosis.
Postoperative EA patients face potential gastrointestinal and respiratory complications, impacting the long-term prognosis and affecting the children’s life [
19]. Consequently, the health-related quality of life subsequent to surgical correction has emerged as a primary focus for both follow-up and research endeavors.
QoL can be defined as the individuals' perception of daily life encompassing their physical, mental, and social functioning, influenced by both the disease itself and medical interventions, within the context of the culture and value systems in which they live [
20]. The QoL could be assessed using generic and condition-specific tools: generic instruments offer broader applicability, facilitating comparisons between patients and healthy individuals, like the Ped QoL 4.0 [
17], while condition-specific tools analyze specifically the clinical factors influencing a precise disease, as in our case the EA QoL [
14]. This combination of tools allows for a more comprehensive assessment, capturing both broader aspects of quality of life applicable across populations and more tailored insights specific to the challenges faced by EA patients.
To date, numerous studies in the literature have explored the EA QoL, but this study stands out as the first to compare QoL outcomes between thoracotomy and thoracoscopy, aiming to understand how the selection of surgical approach might impact long-term patient outcomes.
In our research the two groups were similar in patient’s numbers, gender, and birth weight, while the gestational age was significantly different, showing that premature babies are more often treated by thoracotomy EA repair,
consistent with previous findings in the literature. [
21,
22]
The most recent metanalysis between thoracotomy and thoracoscopy, including 1043 patients, showed non-significant difference in literature in postoperative anastomotic leakage, esophageal stricture, needing for endoscopic esophageal dilatation and mortality, between the two technique [
23]. In our report, the rate of revisional surgery for recurrent TEF suspicion did not differ between the groups, while all the other complications were managed conservatively or with an esophageal dilatation program. Strictures were the most common complications, in both groups, with a slight prevalence in the TCg (35% vs 27%). This finding aligns with the literature, although reported percentages often hover around 40% [
24]. The frequency of endoscopic dilatations needed for stenosis and the requirement for Nissen fundoplication for GERD were more common in the TCg, although statistical significance was not observed.
In the past year, a significant portion of children in both groups exhibited symptoms, with slightly higher occurrences noted in TCg compared to TSg. The number of children with respiratory symptoms was equal in both groups, prevailing over digestive symptoms in both cases, although with minor distinctions in the types of respiratory issues. The observed pulmonary health challenges across all subgroups might stem from disrupted respiratory tract development and maturation, potentially influenced by factors like tracheomalacia, airway infections, and asthma, [
25,
26]
and it’s probably not related with the type of surgical technique adopted. Gastrointestinal symptoms, slightly higher in TCg, were mainly dysphagia, gastroesophageal reflux and feeding difficulties. The abnormal motility of the esophagus continues to be the primary pathophysiological factor contributing to digestive morbidity in children with EA, indeed it is crucial not only for the movement of food from the mouth to the stomach but also plays a pivotal role in protecting the esophagus against gastric reflux. The etiology of esophageal dysmotility could be mainly attributed to an abnormal development of esophageal smooth muscle, intrinsic innervation, and issues with the vagus nerve, but it's worth noting that surgical interventions, with fibrotic scarring, and postoperative complications, may exacerbate esophageal dysmotility [
26,
28]. In our series, it appears that the surgical technique does not significantly influence the occurrence of esophageal dysmotility, however, further prospective studies involving larger patient cohorts are necessary to thoroughly investigate this aspect.
Despite the complexity of EA, the recent literature shows a quite good quality of life of EA patients, often comparable to that of their peers without EA [
29,
30], probably because children with chronic conditions seems to cope better with everyday health related problems compared to healthy children [
31,
32].
It has been shown that generic QoL decrease in cases of prematurity, cardiac malformation, complex esophageal surgery, digestive and respiratory symptoms [
13,
29,
33,
34], while only digestive and respiratory symptoms tend to influence the condition specific QoL [
32,
34].
Physical health is one of the most affected domains, likely associated with frequent hospitalizations for complications such as anastomotic stenosis, in addition to other medical issues like heart defects, tracheomalacia, and recurrent respiratory symptoms [
29]. Analyzing the specific score EA QoL, we found that the physical health score was positively and significatively influenced by the minimally invasive approach in children, with a better score in the EA patient undergoing thoracoscopic EA repair. Even if there wasn’t a statistically significant difference, in the TSg eating and total specific score were higher than the TCg.
Moreover, a reduced score in the social functioning is observed when the issue of postoperative esophageal motor dysfunction becomes more pronounced and affects the social life [
29,
32].
Investigating the general score PedsQL, we discovered that the psychosocial-health score was clearly statically different between the groups, underling that thoracoscopic repair have a positive influence on the psychic and social field of these children.
Furthermore, the total generic QoL score was significantly superior in patients treat by minimally invasive surgery.
The current study presented some limitations. First of all, it was adopted only a parent-proxy questionnaire because the older children able to answer the questionnaire were only in the TCg, therefore, although some studies indicate good agreement between parents and children, there's still the possibility of differences in perception Secondly, it was a single-center pilot study with a limited sample size and a specific population, thus it's essential to recognize that the findings may not be fully generalizable to other populations or settings.
Moving forward, expanding the sample size and collaborating with other centers can enhance the study's robustness and validate the findings across diverse populations.
5. Conclusions
Based on the findings of the current study, it seems that thoracoscopic surgery offers EA patients improved QoL in both physical and psychosocial health domains. Nevertheless, confirmation of these results would benefit from multicenter studies involving larger sample sizes.
Author Contributions
Conceptualization, D.D.F., E.B., and G.C.; Methodology, D.D.F. and A.C.; Software; D.D.F.; Validation, D.D.F., E.B., and G.C.; Formal Analysis, D.D.F. and E.B.; Investigation, D.D.F., F.M. and A.C.; Resources, D.D.F. and F.M.; Data Curation, D.D.F.; Writing – Original Draft Preparation, D.D.F.; Writing – Review & Editing, A.C., E.B., and G.C.; Visualization, D.D.F., E.B.; Supervision, G.C.; Project Administration, G.C.
Funding
This research received no external funding.
Informed consent
Informed consent was obtained from all subjects involved in the study.
Conflicts of interest
The authors declare no conflict of interest.
Abbreviations
EA = Esophageal atresia
TEF = Tracheoesophageal fistula
QoL = Quality of life
EAQoL = Esophageal Atresia QoL
PedsQL = Pediatric QoL 4.0
TCg = Thoracotomy group
TSg = Thoracoscopic group
GERD = Gastroesophageal reflux disease
SD = Standard deviation
IQR = Interquartile range
References
- Pedersen RN, Calzolari E, Husby S, Garne E; EUROCAT Working group. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child. 2012;97:227-232. [CrossRef]
- Pini Prato A, Carlucci M, Bagolan P, et al. A cross-sectional nationwide survey on esophageal atresia and tracheoesophageal fistula. J Pediatr Surg. 2015;50:1441-1456. [CrossRef]
- Bogs T, Zwink N, Chonitzki V, et al. Esophageal Atresia with or without Tracheoesophageal Fistula (EA/TEF): Association of Different EA/TEF Subtypes with Specific Co-occurring Congenital Anomalies and Implications for Diagnostic Workup. Eur J Pediatr Surg. 2018;28:176-182. [CrossRef]
- Ioannides AS, Copp AJ. Embryology of oesophageal atresia. Semin Pediatr Surg. 2009;18:2-11. [CrossRef]
- Smigiel R, Lebioda A, Blaszczyński M, et al. Alternations in genes expression of pathway signaling in esophageal tissue with atresia: results of expression microarray profiling. Dis Esophagus. 2015;28:229-233. [CrossRef]
- Gross, R.E. The Surgery of Infancy and Childhood: Its Principles and Techniques; W.B. Saunders Company, Ed.; W.B. Saunders Company: Philadelphia, PA, USA, 1953.
- Cassina M, Ruol M, Pertile R, et al. Prevalence, characteristics, and survival of children with esophageal atresia: A 32-year population-based study including 1,417,724 consecutive newborns. Birth Defects Res A Clin Mol Teratol. 2016;106:542-548. [CrossRef]
- Bell JC, Baynam G, Bergman JEH, et al. Survival of infants born with esophageal atresia among 24 international birth defects surveillance programs. Birth Defects Res. 2021;113:945-957. [CrossRef]
- Lacher M, Froehlich S, von Schweinitz D, et al. Early and long term outcome in children with esophageal atresia treated over the last 22 years. Klin Padiatr. 2010;222:296-301. [CrossRef]
- Di Fabrizio D, Bindi E, Cruccetti A, et al. Chest tube-related complications after a staged thoracoscopic repair of a long-gap esophageal atresia: A case report, J Pediatr Surg Case Rep. 2024. [CrossRef]
- Rothenberg S. Thoracoscopic repair of esophageal atresia and tracheo-esophageal fistula in neonates: the current state of the art. Pediatr Surg Int. 2014;30:979-985. [CrossRef]
- Dingemann C, Eaton S, Aksnes G, et al. ERNICA Consensus Conference on the Management of Patients with Esophageal Atresia and Tracheoesophageal Fistula: Follow-up and Framework. Eur J Pediatr Surg. 2020;30:475-482. [CrossRef]
- Dellenmark-Blom M, Quitmann J, Dingemann J, et al. Clinical Factors Affecting Condition-Specific Quality-of-Life Domains in Pediatric Patients after Repair of Esophageal Atresia: The Swedish-German EA-QOL Study. Eur J Pediatr Surg. 2020;30:96-103. [CrossRef]
- Dellenmark-Blom M, Abrahamsson K, Quitmann JH, et al. Development and pilot-testing of a condition-specific instrument to assess the quality-of-life in children and adolescents born with esophageal atresia. Dis Esophagus. 2017;30:1-9. [CrossRef]
- Dellenmark-Blom M, Dingemann J, Witt S, et al. The Esophageal-Atresia-Quality-of-life Questionnaires: Feasibility, Validity and Reliability in Sweden and Germany. J Pediatr Gastroenterol Nutr. 2018;67:469-477. [CrossRef]
- Growth Charts—2000 CDC Growth Charts—United States. Available online: https://www.cdc.gov/growthcharts/cdc_charts. Html.
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800-812. [CrossRef]
- van Lennep M, Singendonk MMJ, Dall'Oglio L, et al. Oesophageal atresia [published correction appears in Nat Rev Dis Primers. 2024 Mar 22;10(1):24]. Nat Rev Dis Primers. 2019;5:26. Published 2019 Apr 18. [CrossRef]
- Sulkowski JP, Cooper JN, Lopez JJ, et al. Morbidity and mortality in patients with esophageal atresia. Surgery. 2014;156:483-491. [CrossRef]
- The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41:1403-1409. [CrossRef]
- Marquart JP, Bowder AN, Bence CM, et al. Thoracoscopy versus thoracotomy for esophageal atresia and tracheoesophageal fistula: Outcomes from the Midwest Pediatric Surgery Consortium. J Pediatr Surg. 2023;58:27-33. [CrossRef]
- Zani A, Wolinska J, Cobellis G, et al. Outcome of esophageal atresia/tracheoesophageal fistula in extremely low birth weight neonates (<1000 grams). Pediatr Surg Int. 2016;32:83-88. [CrossRef]
- Drevin G, Andersson B, Svensson JF. Thoracoscopy or Thoracotomy for Esophageal Atresia: A Systematic Review and Meta-analysis. Ann Surg. 2021 Dec 1;274:945-953. [CrossRef] [PubMed]
- Lal DR, Gadepalli SK, Downard CD, et al. Perioperative management and outcomes of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg. 2017;52:1245-1251. [CrossRef]
- Fragoso AC, Martinez L, Estevão-Costa J, Tovar JA. Lung maturity in esophageal atresia: Experimental and clinical study. J Pediatr Surg. 2015;50:1251-1259. [CrossRef]
- Dellenmark-Blom M, Örnö Ax S, Öst E, et al. Postoperative morbidity and health-related quality of life in children with delayed reconstruction of esophageal atresia: a nationwide Swedish study. Orphanet J Rare Dis. 2022;17:239. Published 2022 Jun 20. [CrossRef]
- Faure C, Righini Grunder F. Dysmotility in Esophageal Atresia: Pathophysiology, Characterization, and Treatment. Front Pediatr. 2017;5:130. Published 2017 May 31. [CrossRef]
- Davies MR. Anatomy of the extrinsic motor nerve supply to mobilized segments of the oesophagus disrupted by dissection during repair of oesophageal atresia with distal fistula. Br J Surg. 1996;83:1268-1270.
- Lepeytre C, De Lagausie P, Merrot T, Baumstarck K, Oudyi M, Dubus JC. Medium-term outcome, follow-up, and quality of life in children treated for type III esophageal atresia. Arch Pediatr. 2013;20:1096-1104. [CrossRef]
- Feng Z, Zhu H, He W, et al. Health-related quality of life in children after surgical repair of esophageal atresia: a cross-sectional study in China. Front Pediatr. 2024;11:1332979. Published 2024 Jan 9. [CrossRef]
- Hampel P, Rudolph H, Stachow R, et al. Coping among children and adolescents with chronic illness. Anxiety Stress Copin 2005;18:145–55. [CrossRef]
- Flieder S, Dellenmark-Blom M, Witt S, et al. Generic Health-Related Quality of Life after Repair of Esophageal Atresia and Its Determinants within a German-Swedish Cohort. Eur J Pediatr Surg. 2019;29:75-84. [CrossRef]
- Legrand C, Michaud L, Salleron J, et al. Long-term outcome of children with oesophageal atresia type III. Arch Dis Child. 2012;97:808-811. [CrossRef]
- Leibovitch L, Zohar I, Maayan-Mazger A, Mazkereth R, Strauss T, Bilik R. Infants Born with Esophageal Atresia with or without Tracheo-Esophageal Fistula: Short- and Long-Term Outcomes. Isr Med Assoc J. 2018;20:161-166.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).