Submitted:
06 October 2024
Posted:
07 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
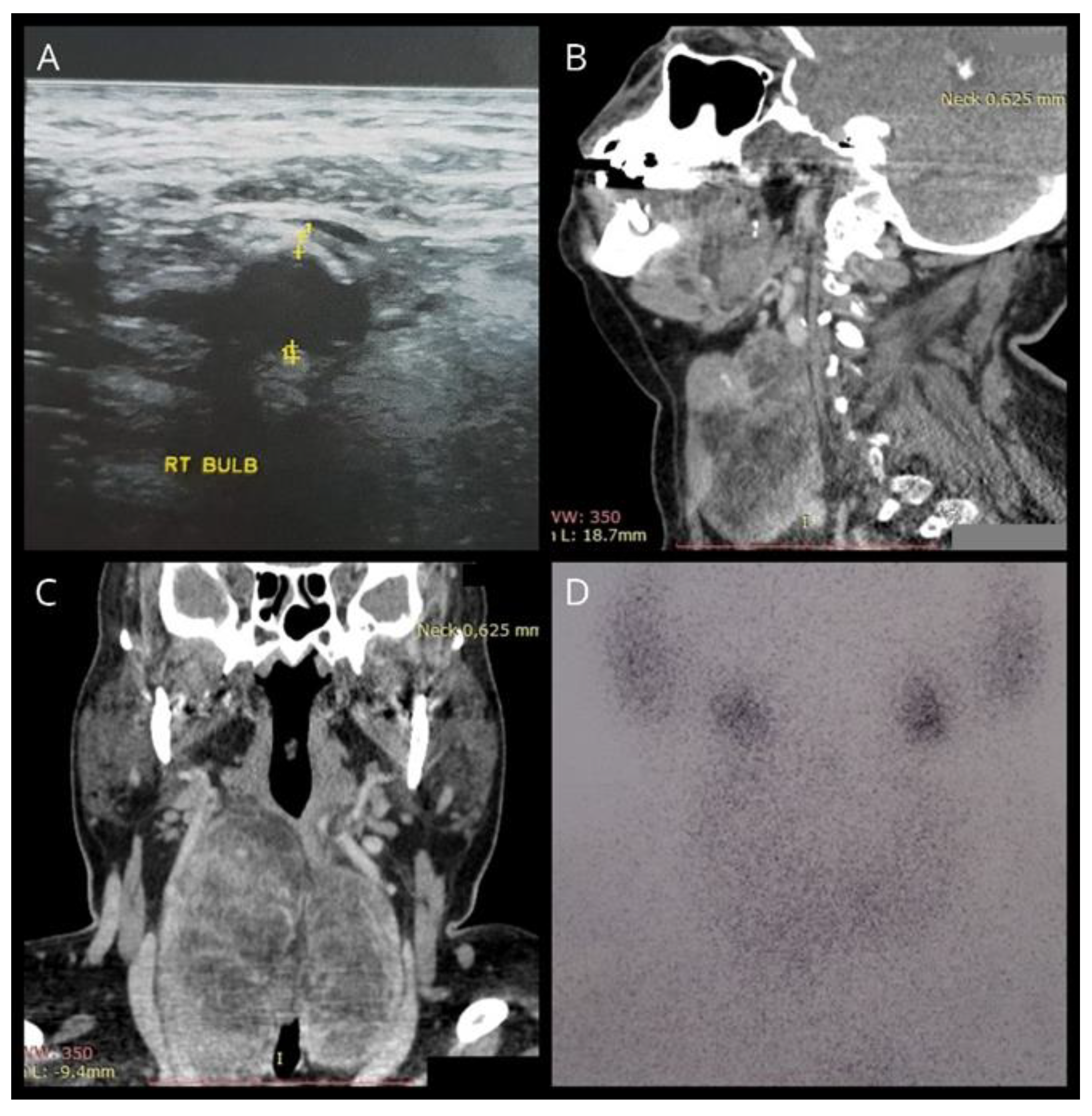
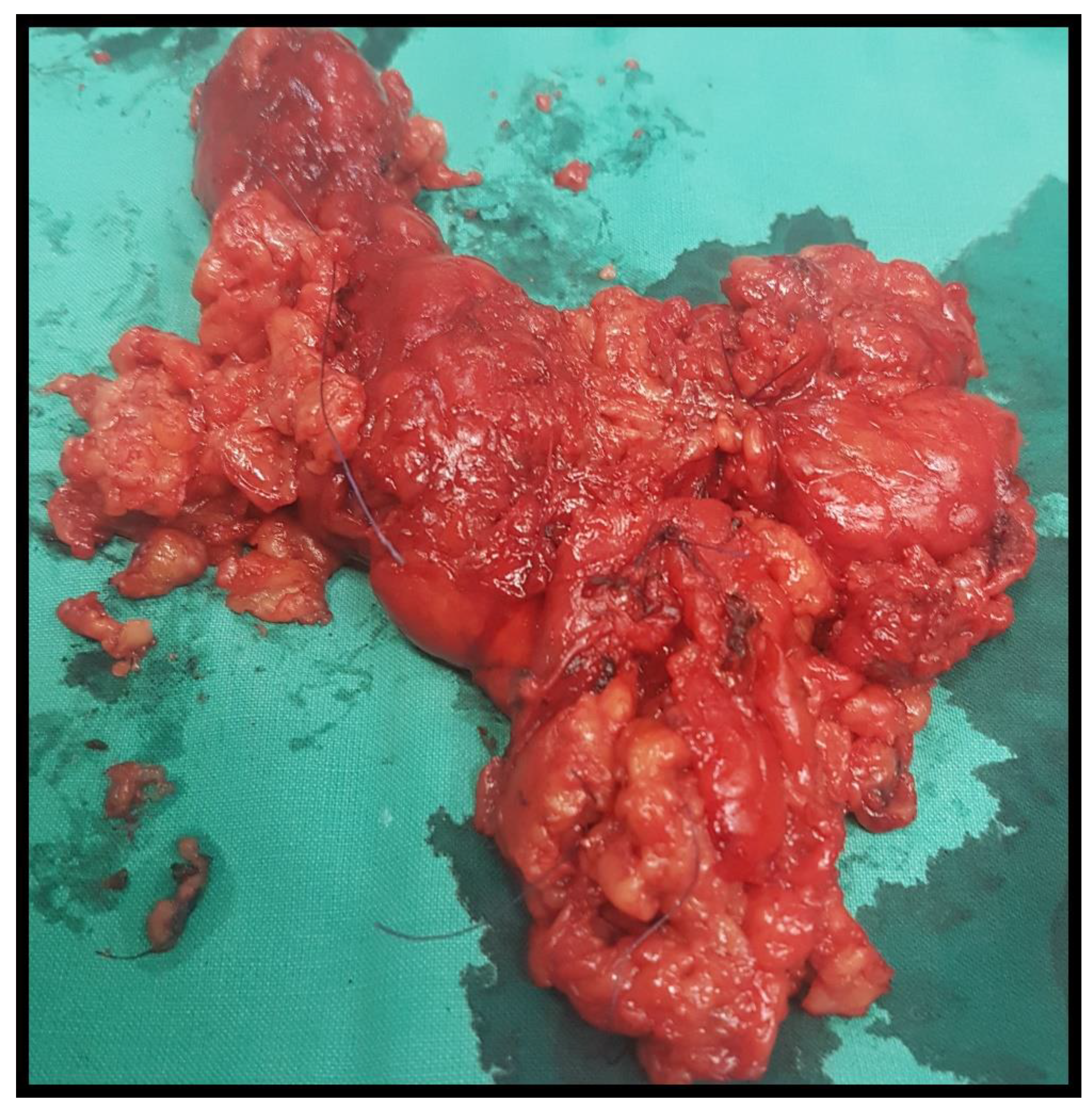
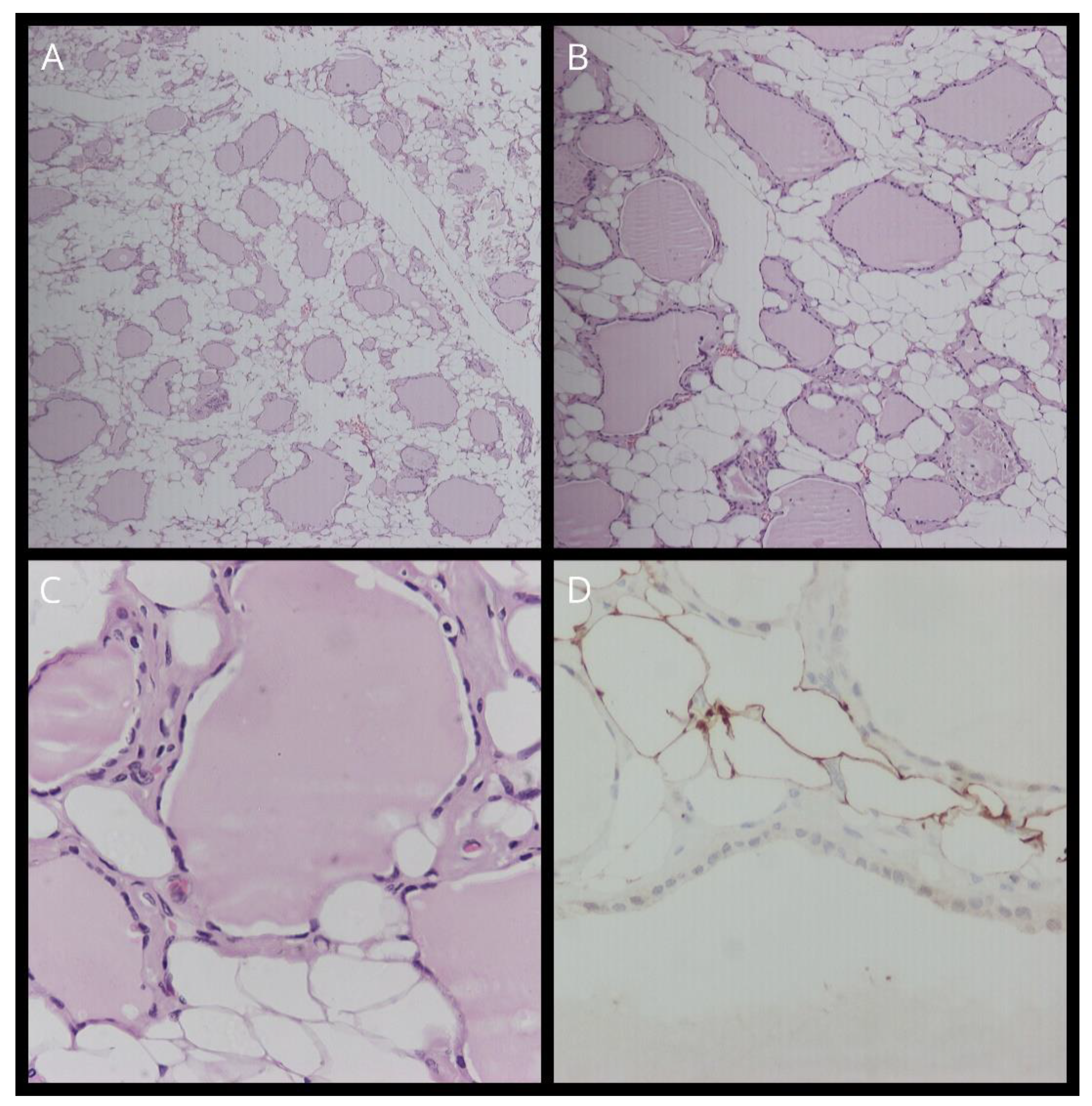
2. Case Report
3. Review
4. Discussion
5. Conclusions
Author Contributions
Funding
Author Disclosure Statement
Data Availability
References
- Ge, Y.; Luna, M.A.; Cowan, D.F.; Truong, L.D.; Ayala, A.G. Thyrolipoma and thyrolipomatosis: 5 case reports and historical review of the literature. Ann Diagn Pathol. 2009, 13, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Sanuvada, R.; Chowhan, A.; Rukmangadha, N.; Patnayak, R.; Yootla, M.; Amancharla, L. Thyrolipomatosis: an inquisitive rare entity. Gland Surgery . 2014, 3, E6–E9. [Google Scholar] [CrossRef] [PubMed]
- Nandyala, H.S.; Madapuram, S.; Yadav, M.; Katamala, S.K. Diffuse lipomatosis of the thyroid gland with papillary microcarcinoma: Report of a rare entity. Indian J Pathol Microbiol. 2015, 58, 348–350. [Google Scholar] [CrossRef] [PubMed]
- Schroder, S.; Bocker, W.; Hiisselmann, H.; Dralle, H. Hrchows Archiv A Case Report Adenolipoma (Thyrolipoma) of the Thyroid Gland Report of Two Cases and Review of Literature. Vol 404.; 1984.
- Dombale, V.D.; jaValgi, A.P. Symmetric Diffuse Lipomatosis of the Thyroid Gland. Journal of Clinical and Diagnostic Research. 2011, 5, 867–868 wwwjcdrnet. [Google Scholar]
- Lau, E.; Freitas, P.; Costa, J.; et al. Loss of mitochondrial SDHB expression: What is its role in diffuse thyroid lipomatosis? Hormone and Metabolic Research. 2015, 47, 165–167. [Google Scholar] [CrossRef]
- Daboin, K.P.; Ochoa-Perez, V.; Luna, M.A. Adenolipomas of the head and neck: analysis of 6 cases. Ann Diagn Pathol. 2006, 10, 72–76. [Google Scholar] [CrossRef]
- Çelik, Z.E. Mature Fat Containing Thyroid Lesions. European Journal of General Medicine. 2015, 12, 353–355. [Google Scholar] [CrossRef]
- Citgez, B.; Uludag, M.; Yetkin, G.; et al. Amyloid goiter with diffuse lipomatosis. World Journal of Endocrine Surgery. 2011, 3, 97–99. [Google Scholar] [CrossRef]
- Dhayagude, R.G. Case report: massive fatty infiltration in a colloid goiter. Arch Pathol (Chic) 1942, 33, 357–360. [Google Scholar]
- Bell, S.; Sosa, G.A.; del Valle Jaen, A.; Russo Picasso, M.F. Thyroid lipomatosis in a 36-year-old patient with rheumatoid arthritis and a kidney transplant. Endocrinol Diabetes Metab Case Rep. 2016, 2016. [Google Scholar] [CrossRef]
- Munzinger, U. Amyloid Goiter. Vol 104.; 1974.
- Willis, RA. The Borderland of Embryology and Pathology. Butterworth & Co.; 1958.
- Schroder, S.; Boeker, W. Lipomatous Lesions of the Thyroid Gland: A Review. Appl Pathol 1985, 3, 140–149. [Google Scholar] [PubMed]
- Trites, A.E.W. Thyrolipoma Thyrolipoma, Thymolipoma and Pharyngeal Lipoma: A Syndrome. Canad Med Ass J. 1966, 95, 1254–1259. [Google Scholar] [PubMed]
- Gellhorn, A.; Marks, P.A. The composition and biosynthesis of lipids in human adipose tissues. J Clin Invest 1961, 40, 925–932. [Google Scholar] [CrossRef] [PubMed]
- Derienzo D, Truong L. Thyroid Neoplasms Containing Mature Fat: A Report of Two Cases and Review of the Literature. Vol 2.; 1969.
- Chesky, V.E.; Dreese, W.C.; Hellwig, C.A. Adenolipomatosis of the thyroid: a new type of goiter. Surgery 1953, 34, 38–45. [Google Scholar]
- Gonulalan, G.; Esen, H.; Mehmet, E.; Cakir, M. Thyroid Lipomatosis. Internal Medicine. 2012, 51, 3383–3385. [Google Scholar] [CrossRef]
- Pradeep, P.V.; Kumar, R.; Ragavan, M.; Ramakrishna, B.A. Diffuse lipomatosis of thyroid with hyperthyroidism. J Postgrad Med. 2010, 56, 35–36. [Google Scholar] [CrossRef]
- Cavaco, D.R.; Alves Rafael, A.; Cabrera, R.; Vilar, H.; Leite, V. Case Report: A Rare Association of Diffuse Thyroid Lipomatosis with Amyloid Deposition. Eur Thyroid J. 2021, 10, 528–532. [Google Scholar] [CrossRef]
- Lo, R.; Donaldson, C. Diffuse Lipomatosis of the Thyroid Gland. Ultrasound Q. 2013, 29, 253–254 wwwultrasound. [Google Scholar] [CrossRef]
- Ben Gamra, O.; Romdhane, N.; Nefzaoui, S.; et al. Diffuse lipomatosis of the thyroid gland. Egyptian Journal of Ear, Nose, Throat and Allied Sciences. 2016, 17, 167–169. [Google Scholar] [CrossRef]
- Harisankar, C.N.B. A Rare Case of Thyrolipomatosis Presenting with Latent Hyperthyroidism. Indian J Nucl Med. 2018, 33, 237–238. [Google Scholar] [CrossRef]
- Ravinder, K.; Abhishek, B.; Gagan, J. Thyrolipomatosis: A Rare Fat Containing Lesion diffusely Infiltrating Throughout the Thyroid Gland. Journal of the Association of Physicians of India. 2019, 67, 77. [Google Scholar]
- Campion, T.; Maity, A.; Ali, S.; Richards, P.; Adams, A. Concurrent thyrolipomatosis and thymolipoma in a patient with myasthenia gravis: A case report and review of the literature. Ann R Coll Surg Engl. 2021, 103, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.; Goyal, A.; Kandasamy, D. Diffuse Thyroid Lipomatosis - a Rare Image. Indian Journal of Surgery. 2020, 82, 1310–1311. [Google Scholar] [CrossRef]
- Ahmed, J.; Amine REl Bouziane, C. Diffuse Lipomatosis of Thyroid—Case Report. Surg Sci. 2018, 09, 469–473. [Google Scholar] [CrossRef]
- Himmetoglu, C.; Yamak, S.; Tezel, G.G. Diffuse fatty infiltration in amyloid goiter. Pathol Int. 2007, 57, 449–453. [Google Scholar] [CrossRef]
- Hijazi, D.M.; Addas, F.A.; Alghanmi, N.M.; Marzouki, H.Z.; Merdad, M.A. An enlarged goiter presenting with a rare diffuse lipomatosis of the thyroid gland. American Journal of Case Reports 2018, 19, 808–811. [Google Scholar] [CrossRef]
- Ishida, M.; Kashu, I.; Morisaki, T.; et al. Thyrolipomatosis: A case report with review of the literature. Mol Clin Oncol. 2017, 6, 893–895. [Google Scholar] [CrossRef]
- Martí-Fernández, R.; Cassinello-Fernández, N.; Palomares-Casasús, S.; Gómez-Adrián, J.C.; Ferrández-Izquierdo, A. Diffuse Lipomatosis of the Thyroid Gland. American Surgeon. Published online 2021. [CrossRef]
- Kuk, M.; Kuo, C.J.; Nguyen, V.H.; Chen, C.C. Synchronous thyrolipoma and papillary thyroid carcinoma: A rare but significant event. Diagnostics. 2021, 11(8). [CrossRef]
- Kesici, U.; Karatepe, Y.K.; Isceviren, B. Concurrence of Thyrolipoma-tosis with Hyperthyroidism and Ectopic Thyroid Tissue. Journal of the College of Physicians and Surgeons Pakistan. 2022, 32, 1231–1232. [Google Scholar] [CrossRef]
- Simard, L.C. Une nouvelle forme de goître: la scléro-lympho-lipomatose thyroidiènne. Union Med Can 1945, 74, 884–991. [Google Scholar]
- Bielicki, F.; Dawiskiba, E.; Kasprzak, A.; Kawecki, K.; Zagrobelny, Z. [Struma lipomatosa]. Pol Tyg Lek (Wars). 1968, 23, 2018–2019. [Google Scholar]
- Dalforno, S.; Donna, A. Lipomatosi diffusa della tiroide (Struma lipomatose). Cancro 1959, 22, 613–617. [Google Scholar]
- Asirwatham, J.E.; Barcos, M.; Shimaoka, K. Hamartomatous adiposity of thyroid gland. J Med. 1979, 10, 197–206. [Google Scholar] [PubMed]
- Simha, M.R.; Doctor, V.M. Adenolipomatosis of the thyroid gland. Indian J Cancer. 1983, 20, 215–217. [Google Scholar]
- Téllez, R.; Le Cerf, P.; Araos, F.; Michaud, P. Diffuse fatty infiltration of the thyroid gland associated to amyloidosis in a patient with chronic renal failure. Rev Med Chil. 1996, 124, 1251–1255. [Google Scholar]
- Paoletti, H.; Tourrette, J.; Terrier, J.; et al. [Diffuse thyroid lipomatosis]. J Radiol. 1997, 78, 1291–1294. [Google Scholar]
- Arslan, A.; Lent Alíç, B.; Kemal Uzunlar, A.; Seyin Büyü, H.; Sarí, I. Diffuse lipomatosis of thyroid gland. Auris Nasus Larynx, 1999; 26, 213–215. [Google Scholar]
- Di Scioscio, V.; Loffreda, V.; Feraco, P.; et al. Diffuse lipomatosis of thyroid gland. Journal of Clinical Endocrinology and Metabolism. 2008, 93, 8–9. [Google Scholar] [CrossRef]
- Gupta, R.; Arora, R.; Sharma, A.; Dinda, A. Diffuse lipomatosis of the thyroid gland: A pathologic curiosity. Indian J Pathol Microbiol. 2009, 52, 215. [Google Scholar] [CrossRef]
- Jacques, T.A.; Stearns, M.P. Diffuse lipomatosis of the thyroid with amyloid deposition. Journal of Laryngology and Otology. 2013, 127, 426–428. [Google Scholar] [CrossRef]
- Costa, J.; Pardal, J.; Máximo, V.; Gonçalves, F.; Eloy, C. Diffuse lipomatosis of thyroid: A case report. Virchows Archiv. 2013, 463, 155. [Google Scholar]
- Liyanaarachchi, N.; Lim, A.; Donaldson, E. Diffuse lipomatosis and amyloid deposition of the thyroid gland associated with poorly differentiated/insular carcinoma of the thyroid: report of a rare entity. Pathology. 2016, 48(81).
- Kumar, R.; Bhargava, A.; Jaiswal, G. A Case Report on Radiologic Findings of Thyrolipomatosis: a Rare Fat Containing Lesion diffusely Infiltrating throughout the Thyroid Gland. Journal of Kathmandu Medical College. 2016, 5, 71–73. [Google Scholar] [CrossRef]
- López-Muñoz, B.; Greco Bermúdez, L.; Marín-Jiménez, D.; et al. An Unusual Amyloid Goiter in a 48-Year-Old Woman with Rheumatoid Arthritis, Secondary Amyloidosis and Renal Failure. Case Rep Endocrinol. 2019, 2019. [Google Scholar] [CrossRef] [PubMed]
- Stanaway, A.; Lam, T. Consecutive cases of thyrolipomatosis and thymolipoma: a case report. ANZ J Surg. 2019, 89, 614–616. [Google Scholar] [CrossRef] [PubMed]
- Ayadi, S.; Hammami, B.; Boudaouara, O.; Boudawara, T.; Kallel, S.; Charfeddine, I. [Association of thyrolipoma and thyrolipomatosis: A case report]. Ann Pathol. 2021, 41, 326–329. [Google Scholar] [CrossRef]
- Xhemalaj, D.; Xhardo, E.; Gradica, F.; Lisha, L. Diffuse Lipomatosis of Thyroid Gland. Case Report and Review of Literature. Diagn Pathol. 2022, 7, 285. [Google Scholar] [CrossRef]
- Morado da Silva, E.M.; Ferreira RA da, C.; Lozada, A.R.C.; Duarte, J.M.S. A 54-Year-Old Woman with Papillary Thyroid Carcinoma Associated with Secondary Amyloid Goiter and Thyroid Lipomatosis. American Journal of Case Reports. 2022, 23, 1–4. [Google Scholar] [CrossRef]
- Kawai, C.; Miyao, M.; Kotani, H.; et al. Systemic amyloidosis with amyloid goiter: An autopsy report. Leg Med. 2023, 60(102167). [CrossRef]
- Paz-Ibarra, J.; Concepción-Zavaleta, M.; Mendoza-Quispe, D.; et al. Coexistence of thyrolipomatosis and tongue squamous cell carcinoma: A case report. touchREVIEWS in Endocrinology. 2023, 19, 103–107. [Google Scholar] [CrossRef]
- Alenezi, S.; Saleem, A.; Alhajri, O.; Alozairi, O. Thyrolipoma presentation as a huge multinodular goiter; A case report of an extremely rare entity. Int J Surg Case Rep. 2023, 112(108936). [CrossRef]
- Gonzalez-Gil, A.M.; Ruiz-Santillan, M.A.; Force, B.K.; Gaba, R. A Case of Diffuse Thyroid Lipomatosis With Amyloid Deposits Presenting With Thyrotoxicosis. JCEM Case Reports. 2024, 2, 1–5. [Google Scholar] [CrossRef]
- George, D.M.; Shah, S.N. Diffuse Thyroid Lipomatosis and Amyloid Goiter With Incidental Papillary Thyroid Carcinoma: A Rare Case Report. Cureus. Published online April 9, 2024. [CrossRef]
| 1 | School of Medicine, Aristotle University of Thessaloniki, 54124, Thessaloniki, Greece |
| 2 | Advancer Center of Endocrine Surgery, Genesis Hospital, 54301, Thessaloniki, Greece |
| 3 | Division of Endocrinology, European Interbalkan Medical Center, 55535, Thessaloniki, Greece |
| Reference | Sex/Age | Clinical Features | Thyroid Function | Renal Failure | Initial Diagnosis | Treatment | Thyroid size/weight | Pathology | Amyloid deposition | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| 10 | M/32 | Local compression | NS (Not Stated) |
No | Diffuse goiter | Excision | 10 x 8 x 5.5 cm (R), 8 x 6 x 5.5cm (L)/ 500g | Diffuse infiltration of fibrous-fatty tissue, anomalous follicles, focal fibrosis |
NS | NS |
| 35 | F/11 | No | BMR (Basic metabolic rate) +3% (hyperthyroidism) | No | Diffuse goiter (since birth) | Excision | x5 normal thyroid size | Diffuse fat infiltration alongside small thyroid follicles and lobules with fibrous septa |
NS | NS |
| 18 | M/15 | No | Normal | No | Diffuse goiter (since birth) | Excision | 12 x 7 x 4 cm (R), 8 x 5 x 2.5cm (L)/ 253g | Diffuse fat infiltration, small and medium thyroid follicles, stromal edema |
NS | NS |
| 36 | M/58 | Local compression | Hyperthyroidism | No | Diffuse goiter | Excision | NS | Diffuse fat infiltration surrounding normal follicles, stromal fibrosis, lymphocyte aggregation |
NS | NS |
| 37 | F/51 | No | Normal | No | Diffuse goiter | Excision | NS | Diffuse fat infiltration surrounding normal follicles, stromal fibrosis |
NS | NS |
| 38 | F/73 | No | Normal | No | Diffuse goiter | Excision | NS/120g | Diffuse fat infiltration around normal follicles, lymphocyte aggregation |
NS | NS |
| 39 | M/12 | No | Normal | No | Right neck mass | Excision | 13 x 8 x 6.5cm (R)/415g | Diffuse fat infiltration surrounding normal thyroid follicles, presence of lymphocytes and fibrous tissue |
NS | NS |
| 40 | M/26 | Neck swelling, hoarseness, dysphagia | Normal | Yes | Cervical mass | Total thyroidectomy | NS | Diffuse infiltration of thyroid by fat | Yes | NS |
| 41 | F/77 | No | Normal | No | Cervical mass | Excision | NS/700g | Thyroid follicles surrounded by adipose cells | NS | NS |
| 42 | M/38 | Neck swelling | Normal | No | Diffuse enlargement of thyroid | Excision | 4 x 3 x 2cm (I), 13 x 7 x 3cm (R), 15 x 9 x 5cm (L)/465g | Mature adipose tissue surrounded the different sized but otherwise normal follicles of the thyroid | No | Well -post-operatively |
| 29 | F/58 | Neck swelling, dysphagia, hoarseness, hyperthermia | Hypothyroidism | Yes | Diffuse goiter | Total thyroidectomy | 9.5 x 7 x 5cm (R), 8 x 6 x 3.5cm (L)/230g | Diffuse fatty infiltration, loss of most thyroid follicles, eosinophilic substance deposition in the hyalinized stroma, lymphocytic thyroiditis | Yes | NS |
| 43 | M/64 | Enlarged thyroid, dyspnea |
Normal | Yes | Diffuse goiter | NS | NS | NS | NS | NS |
| 44 | M/45 | Neck swelling, respiratory distress | Normal | No | Diffuse thyroid enlargement | Subtotal thyroidectomy | 2 x 1.5 x 1cm (I), 9 x 7 x 4cm (R), 9 x 5 x 3.5cm (L), 4 x 3 x 2 (P)/225g | Colloid filled thyroid follicles, fatty infiltration of interfollicular stroma | No | NS |
| 1 | F/67 | Dysphagia | Normal | Yes | Enlarged nodular left thyroid lobe | Left thyroidectomy | 7 x 3.5 x 2cm (L)/41g | Thyroid follicles separated by fat, adipose tissue density varied from 30%-90% of total tissue, fat infiltration in adenomatous nodules | No | Well- 2 years after |
| 1 | F/59 | No | Hypothyroidism | No | Right thyroid mass | Right thyroid lobectomy and isthmusectomy/ left thyroidectomy | 7 x 4 x 1.2cm (R+I), 6 x 3 x 1.2cm (L)/56g | Nodular and diffuse pattern of fatty infiltration, presence of a 0.8cm papillary carcinoma | No | Well -6 years after |
| 20 | F/40 | No | Hyperthyroidism | No | Multinodular goiter | Excision | NS | Colloid filled thyroid follicles of various sizes, replacement of stroma by mature adipose tissue | No | Well -post-operatively |
| 9 | M/37 | Neck swelling, dyspnea | Normal | Yes | Diffuse thyroid enlargement | Total thyroidectomy | NS/304g | Widespread deposition of eosinophilic material with scarcity of thyroid follicles, diffuse lipomatosis and amyloidosis (secondary) | Yes | Well -3rd post-operative day |
| 5 | M/62 | Neck swelling, dyspnea | Normal | No | Nodular goiter | Near total thyroidectomy | 12 x 10 x 6cm (R), 15 x 8 x 6cm(L)/285g | Colloid filled thyroid follicles, diffuse infiltration of stroma with mature adipose tissue, scarce lymphocytic infiltration | No | NS |
| 19 | M/43 | Neck swelling, dyspnea | Normal | Yes | Enlarged thyroid | Total thyroidectomy | 6 x 2 x 1cm (I), 7.5 x 6 x 4.5cm (R), 6.5×4.5×2 (L)/160g | Scattered thyroid follicles in a dense mature fat stroma | Yes | NS |
| 45 | M/55 | Neck swelling, cough | Normal | Yes | Diffuse goiter | Total thyroidectomy | 4 x 2 x 1cm (I), 9 x 6 x 4cm (R), 7 x 5 x 2.5cm (L)/ 148g | Infiltration of thyroid by adipose tissue, small amounts of colloid filled follicles remained | Yes | Well post-operatively |
| 22 | F/52 | No | Normal | NS | Diffuse lipomatosis | NS | NS | NS | NS | Difficulty breathing – 3 years later |
| 46 | M/46 | NS | Hypothyroidism | No | Cervical mass | Partial thyroidectomy (same procedure at 3 years of age) | NS | Infiltration of thyroid by mature adipocytes. Same results as 43 years before | No | NS |
| 2 | F/32 | Neck swelling | Hyperthyroidism | No | Toxic multinodular goiter | Total thyroidectomy | 11 x 5 x 2cm(total)/88g | Thyroid follicles filled with colloid, diffuse fatty infiltration of stroma | No | NS |
| 3 | M/37 | Neck swelling | NS | No | Nodular goiter | Total thyroidectomy | 5 x 11 x 15 cm (total)/NS | Thyroid tissue replaced by mature adipocytes, papillary thyroid carcinoma | NS | NS |
| 6 | M/47 | NS | Hypothyroidism | No | Fatty infiltration of thyroid | Excision | 16.5 x 8 x 5.5cm (total)/250g | Atrophic follicles of thyroid alongside mature adipose tissue infiltration, SDHB loss of expression (follicular or adipose cells) | No | NS |
| 8 | M/25 | NS | Hypothyroidism | NS | NS | NS | NS | Various sizes of thyroid follicles, abundant distribution of mature fat around thyroid tissue | NS | NS |
| 8 | F/19 | NS | Hypothyroidism | NS | NS | NS | NS | Various sizes of thyroid follicles, abundant distribution of mature fat around thyroid tissue | NS | NS |
| 8 | M/63 | NS | Normal | NS | NS | NS | NS | Preservation of a few thyroid follicles, abundant distribution of mature fat around follicles | NS | NS |
| 47 | M/69 | Hoarseness, exertional dyspnea | NS | Yes | Diffuse fatty conversion and solid/cystic nodule of thyroid | Right hemithyroidectomy /completion thyroidectomy | NS | Diffuse infiltration of thyroid stroma by mature fat, insular carcinoma | Yes | NS |
| 23 | F/67 | Neck swelling, respiratory distress | Hyperthyroidism | Yes | Diffuse goiter | Total thyroidectomy | 2 x 2cm (I), 12 x 6 x 3.5cm (R), 10 x 5 x 2.5cm (L)/215g | Infiltration of thyroid by mature fat, scarcity of colloid follicles | No | Well- post-operatively |
| 11 | F/36 | Dyspnea | Normal | Yes | Multinodular goiter | Excision | 9.8 x 9.5 x 4.5cm (total)/144g | Replacement of normal thyroid tissue by mature adipocytes except from small remnants of normal colloid filled follicles | Yes | NS |
| 48 | M/73 | Neck swelling, dyspnea, hoarseness | Normal | No | Thyrolipomatosis | Near Total thyroidectomy | NS | Thyrolipomatosis | NS | NS |
| Present Study | F/61 | Neck swelling, dyspnea, dysphagia | Normal | Yes | Diffuse Goiter | Total thyroidectomy | NS | Fatty infiltration of thyroid, degeneration of follicles | NS | Dead – after 3 years (due to kidney failure) |
| 31 | F/68 | NS | Normal | No | Diffuse goiter | Total thyroidectomy | NS | Fatty infiltration of thyroid, hyperplastic follicles alongside stromal sclerosis and calcification | No | Well- after 3 months |
| 24 | F/49 | Neck swelling | Subclinical hyperthyroidism | No | Diffuse goiter | Radioiodine ablation (RAI)/ total thyroidectomy | NS | Infiltration of thyroid stroma by fat | NS | Well – post-operatively |
| 30 | F/53 | Local compression, dysphagia | Normal | Yes | Non-toxic diffuse multinodular goiter | Total thyroidectomy | 2.5 x 2 x 1.5cm (I), 5 x 2.5 x 2cm (R), 11 x 7 x 3.5cm (L)/415g | Admixture of adipocytes with follicular cells | NS | NS |
| 28 | F/55 | Neck swelling, hoarseness | Normal | No | Diffuse goiter | Total thyroidectomy | 1.5 x 1cm (I), 5.5 x 3.5 x 3cm (R), 4 x 2.5 x 2.2cm (L)/NS |
Replacement of thyroid tissue by mature fat , few distended thyroid follicles | No | Well- post-operatively |
| 49 | F/48 | Dysphagia | Subclinical hyperthyroidism | Yes | Amyloid Goiter | Total Thyroidectomy | 13.5 x 4.5, 6.5 x 3.5 3.5 x 2.5 cm/NS | Adipose metaplasia of thyroid stroma | Yes | Well- post-operatively |
| 50 | M/20 | Dysphagia | Normal | No | Follicular nodule | Left hemithyroidectomy | NS | Diffuse fatty infiltration of thyroid | NS | NS |
| 25 | M/73 | Neck swelling, dyspnea, hoarseness | Normal | No | Diffuse lipomatosis of thyroid | Total thyroidectomy | NS | Diffuse presence of fat cells in the thyroid | No | NS |
| 27 | M/72 | No | NS | Yes | Diffuse lipomatosis of thyroid | No | NS | NS | NS | NS |
| 21 | M/46 | Dyspnea, hoarseness, dysphagia | Normal | No | Diffuse goiter | Total thyroidectomy | 10.5 x 6.5 x 4.3 (R), 11.1 x 4 x 2.6cm (L)/237g | Normal follicular architecture, fat infiltration of stroma | Yes | Well- post-operatively |
| 32 | F/52 | No | Normal | No | Goiter/suspicious nodule | Left hemithyroidectomy | 6 x 4 x 2cm (L)/26g | Fatty infiltration of stroma, predominance of adipocytes in most regions | NS | Well – after 6 months |
| 51 | M/48 | Neck swelling | Normal | Yes | Multinodular goiter | Total thyroidectomy | NS | Diffuse and nodular infiltration of thyroid by adipose cells, scarce thyroid follicles | No | Well- after 12 months |
| 26 | M/40 | Neck swelling | Normal | No | Thyrolipoma and thymolipoma | Total thyroidectomy | NS | Thyroid follicular cells surrounded by mature adipocytes | No | Well – after 2 weeks |
| 52 | F/69 | Neck swelling, dyspnea, dysphagia, hoarseness | Normal | No | Multinodular goiter | Total thyroidectomy | 1.5 x 1 x 1cm (I), 6.5 x 5 x 3cm (R), 5 x 3 x 2.5cm (L)/NS | Diffuse infiltration of adipocytes and replacement of normal thyroid follicles | NS | Well – post-operatively |
| 53 | F/54 | Neck swelling, hoarseness, dysphagia | Normal | Yes | Diffuse lipomatosis of thyroid and follicular neoplasm | Total thyroidectomy | 2.6 x 4.5 x 2cm (I), 4.5 x 7.5 x 3.4cm (R), 3.2 x 6.7 x 2.8cm (L)/81g | Papillary thyroid carcinoma, admixture of thyroid follicles with mature adipose tissue | Yes | Dead – after 5 months (urinary tract infection -sepsis) |
| 34 | F/57 | Dyspnea, dysphagia, local compression | Hyperthyroidism | No | NS | Total thyroidectomy | NS | NS | NS | NS |
| 54 | F/60 | NS | Hyperthyroidism | Yes | NS | Autopsy | NS | Replacement of normal thyroid follicles by diffuse fat deposits | Yes | Deceased |
| 55 | F/44 | Tongue mass, dysphagia, weight loss | NS | No | Multinodular goiter | Right hemithyroidectomy | 6 x 3.5 x 2cm (R)/15g | Diffuse fat metaplasia of stromal thyroid tissue indicative of thyrolipomatosis | No | Dead – after 5 months (septic shock after metastasis of squamous cell carcinoma of the tongue to the remaining left thyroid lobe) |
| 56 | F/78 | Neck swelling, dysphagia, hoarseness | Normal | Yes | Multinodular goiter | Total thyroidectomy | 22.4 x 8.5 x 5cm/ 300g | Infiltration of the gland by mature adipocytes, a few extended thyroid follicles and a stroma filled with adipocytes and fibrotic tissue | NS | Well – post-operatively |
| 57 | F/64 | Weight loss, fatigue, enlarged thyroid | Hyperthyroidism | Yes | Diffuse Thyroid Lipomatosis | Methimazole | NS | Benign adipose tissue with entrapped thyroid follicles (biopsy) | Yes | NS |
| 58 | F/51 | NS | NS | Yes | Multinodular goiter | Total thyroidectomy | 9.4 x 6.6 x 5.7cm (R), 8.5 x 5.2 x 4.7cm (L), 2.2 x 1.2 x 1cm (I)/ NS | Lobules of adipocytes with few areas of atrophic thyroid follicles, papillary carcinoma | Yes | Well – after 6 months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




