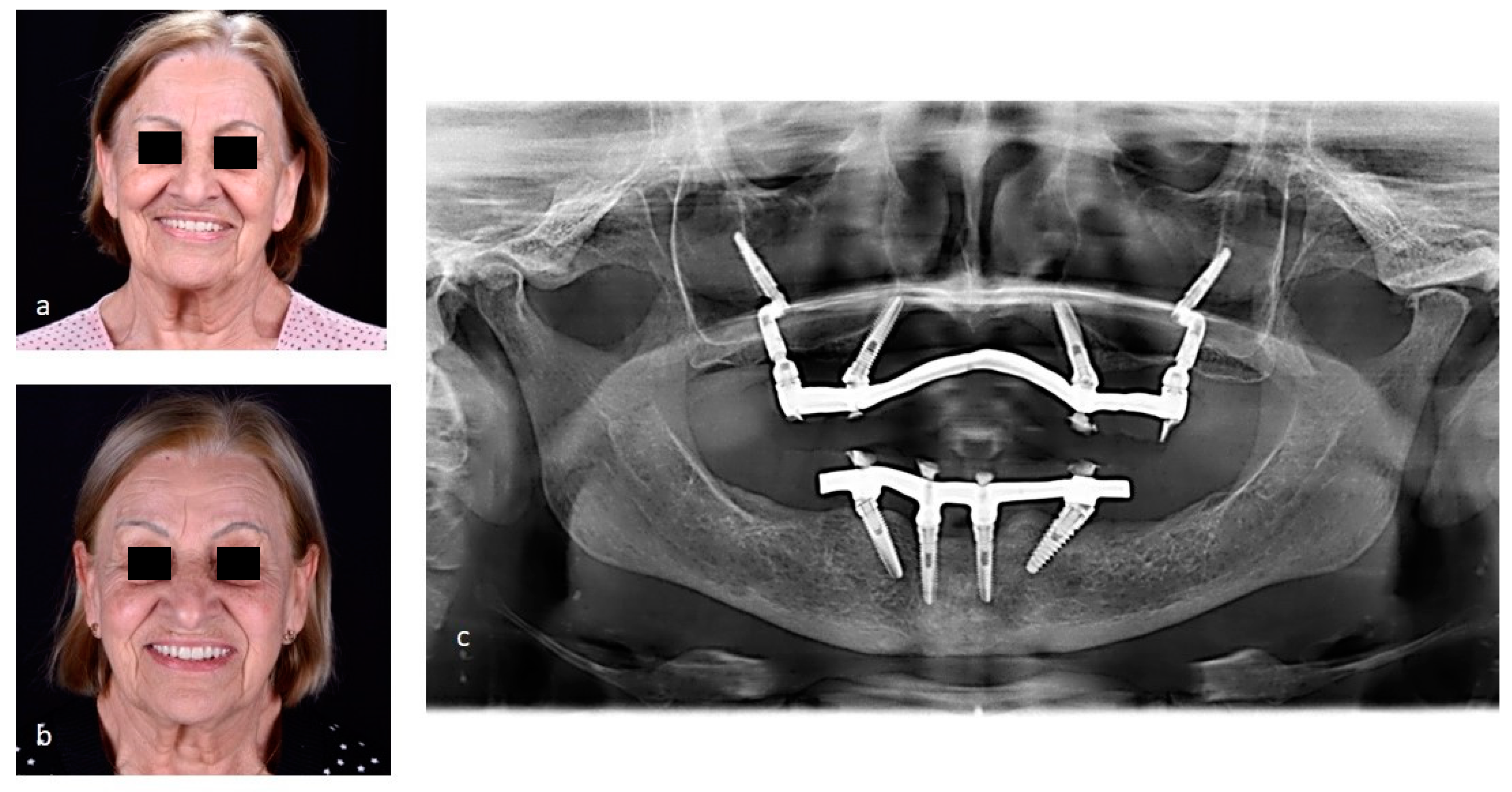
Figure 1.
Female patient, 63 years old, caucasian, with edentulous and atrophic maxilla, came to the dental office complaining that she had lost two previous implants that were placed using All-on-4 technique and reporting that she would not like to undergo a bone graft. The surgical planning was done through analysis of volume of maxilla and zygomas by computed tomography.The rehabilitative treatment of atrophic fully edentulous maxilla is considered a great challenge in dentistry [
1]. Most of patients who use complete dentures are dissatisfied with the treatment, because in many cases the dentures are not stable and masticatory efficiency is drastically reduced. As an alternative, bone reconstruction associated with implant-supported prostheses is the most used option, but it presents risks of morbidity and high cost. Another possibility is use of implants in zygomatic bone, as the zygomatic bone is not affected by alveolar bone resorption. Surgical intervention for placing zygomatic implants, with devices currently available on the market, is a challenging and requires general anesthesia. Despite the high success rates, it is considered a difficult treatment, which requires great expertise and ability from the professional, so it is common to have some postoperative complications such as sinusitis, paresthesia and peri-implant dehiscence [
2].
Figure 1.
Female patient, 63 years old, caucasian, with edentulous and atrophic maxilla, came to the dental office complaining that she had lost two previous implants that were placed using All-on-4 technique and reporting that she would not like to undergo a bone graft. The surgical planning was done through analysis of volume of maxilla and zygomas by computed tomography.The rehabilitative treatment of atrophic fully edentulous maxilla is considered a great challenge in dentistry [
1]. Most of patients who use complete dentures are dissatisfied with the treatment, because in many cases the dentures are not stable and masticatory efficiency is drastically reduced. As an alternative, bone reconstruction associated with implant-supported prostheses is the most used option, but it presents risks of morbidity and high cost. Another possibility is use of implants in zygomatic bone, as the zygomatic bone is not affected by alveolar bone resorption. Surgical intervention for placing zygomatic implants, with devices currently available on the market, is a challenging and requires general anesthesia. Despite the high success rates, it is considered a difficult treatment, which requires great expertise and ability from the professional, so it is common to have some postoperative complications such as sinusitis, paresthesia and peri-implant dehiscence [
2].

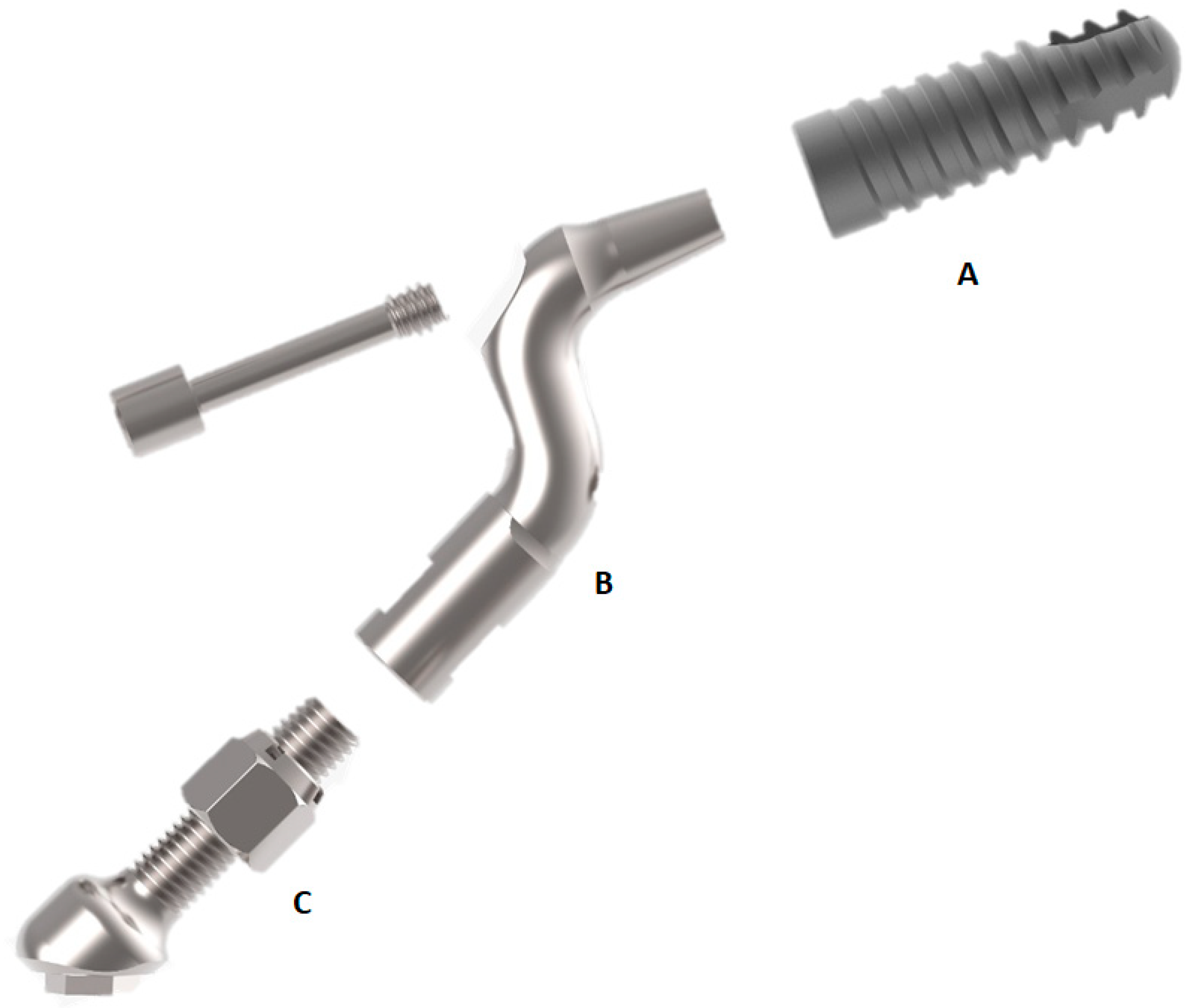
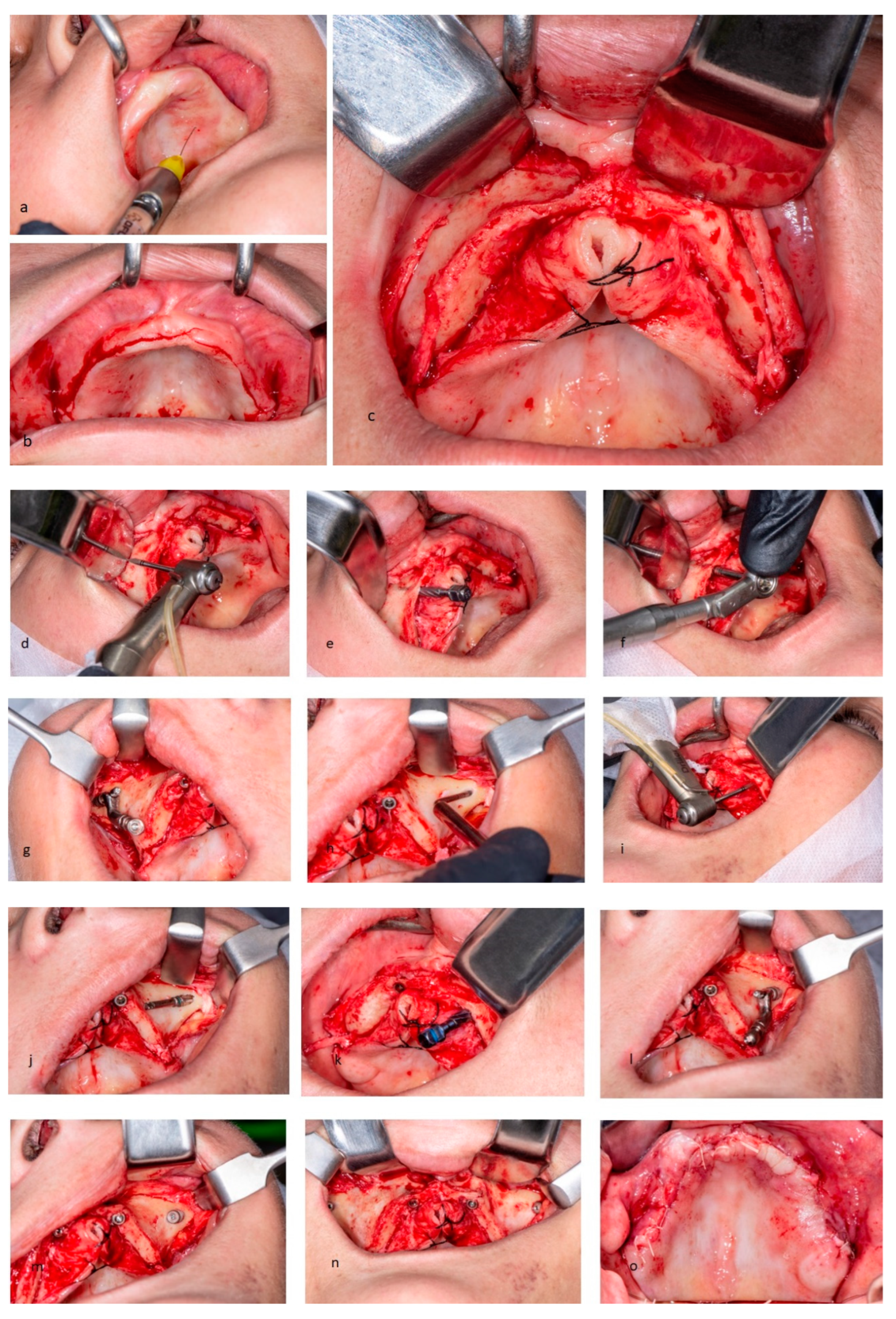
Figure 2.
A new alternative was proposed to her: placement of zygomatic implants using Facco technique with good prognostic. Facco technique advocates the placement of a traditional implant fully immersed in the zygomatic bone, following Branemark protocols [
3]. The big difference is to associate an intermediate component in a Z shape to perform a deviation of maxillary sinus, thus avoiding damage to synovial membrane and post-surgical sequelae. Consequently, implant's prosthetic platform is also buccally displaced to a more palatized position on alveolar crest, favoring less bulky rehabilitation and better designed prosthesis. Regarding the intermediate component, it is a Pilar Z with a specific design. It consists of three parts, made of commercially pure grade IV titanium (Implacil De Bortol): Part A is a morse taper implant with sandblasted surface with SLA acids. Part B is a smooth, polished, Z-angled pillar, with length of 18mm. At one extremity, it contains an internal morse taper connection without indexing and at the other extremity, it contains a connection with a 12-mm internal thread. There is also a passant screw of 1.4-mm diameter. Part C is a 15-mm long rod, with a 10-mm thread at one end that connects to part B. It contains a self-threading nut for height delimitation and an external hexagon prosthetic platform with a height of 0.7mm. Custom drills were also designed to allow the clinician to create a clean and safe tunnel preparation with minimal risk of membrane damage. Thus, a 17° to 60° angled multi-unit pillar provides the necessary emerging angle correction.
Figure 2.
A new alternative was proposed to her: placement of zygomatic implants using Facco technique with good prognostic. Facco technique advocates the placement of a traditional implant fully immersed in the zygomatic bone, following Branemark protocols [
3]. The big difference is to associate an intermediate component in a Z shape to perform a deviation of maxillary sinus, thus avoiding damage to synovial membrane and post-surgical sequelae. Consequently, implant's prosthetic platform is also buccally displaced to a more palatized position on alveolar crest, favoring less bulky rehabilitation and better designed prosthesis. Regarding the intermediate component, it is a Pilar Z with a specific design. It consists of three parts, made of commercially pure grade IV titanium (Implacil De Bortol): Part A is a morse taper implant with sandblasted surface with SLA acids. Part B is a smooth, polished, Z-angled pillar, with length of 18mm. At one extremity, it contains an internal morse taper connection without indexing and at the other extremity, it contains a connection with a 12-mm internal thread. There is also a passant screw of 1.4-mm diameter. Part C is a 15-mm long rod, with a 10-mm thread at one end that connects to part B. It contains a self-threading nut for height delimitation and an external hexagon prosthetic platform with a height of 0.7mm. Custom drills were also designed to allow the clinician to create a clean and safe tunnel preparation with minimal risk of membrane damage. Thus, a 17° to 60° angled multi-unit pillar provides the necessary emerging angle correction.
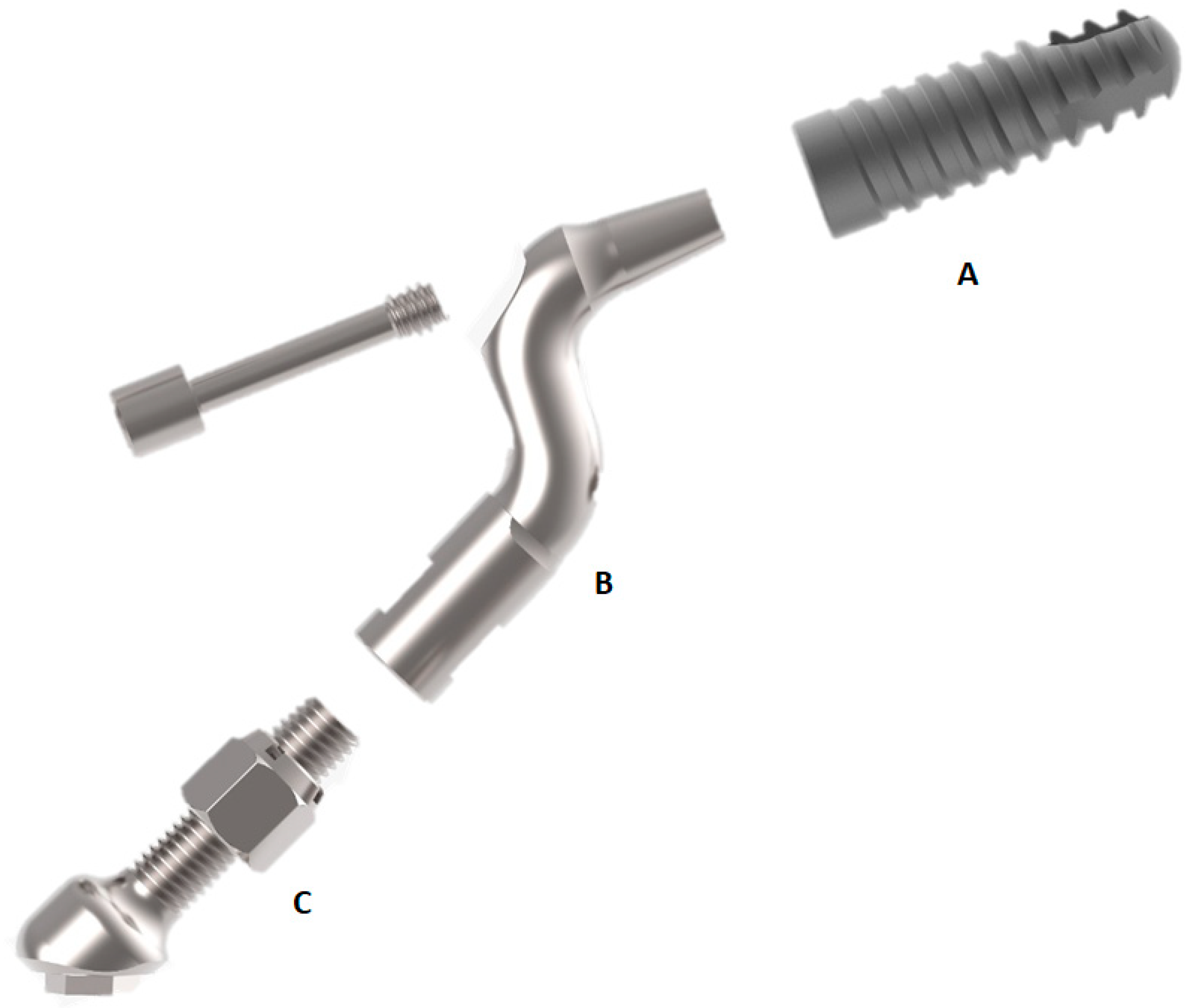
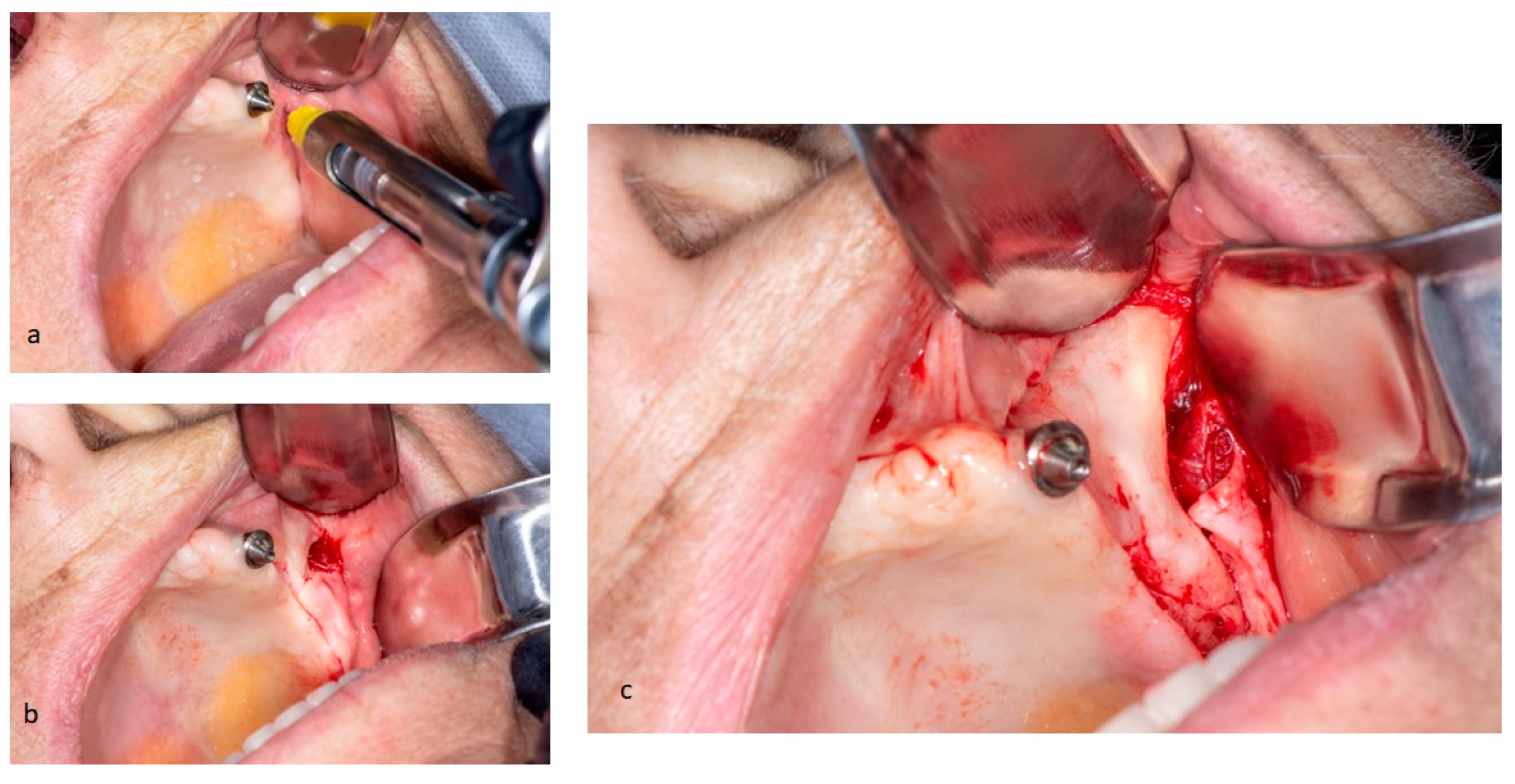
Figure 3.
Upon patient acceptance, she was admitted in an outpatient setting to undergo the surgical procedure, performed with local anesthesia. A small incision was made in the alveolar crest, from the right region of the first molar to the left, preserving the descending palatine artery, which, due to anatomical evolution of the atrophic maxilla, changes its position. Two posterior vestibular incisions were performed bilaterally, considering the appearance of Parotid duct, in order not to cause accidental injuries, and finally, a median release incision was made below the nasal column. Subsequently, a mucoperiosteal flap was simultaneously raised bilaterally along the entire incision. Reflection of mucoperiosteal flap may be performed in two different manners, depending on the surgical procedure involved: placement of only two implants in zygomatic bone or an all-on-four surgery. In surgical case of placement of two zygomatic implants, the mucoperiosteal flap is elevated to expose the alveolar crest, the anterolateral wall of maxillary sinus and the origin of zygomatic arch, where masseter muscle is inserted. However, in this case, mucoperiosteal flap from the paranasal region was elevated medially until the infraorbital nerve appeared. Infraorbital foramen is the posterior limit of mucoperiosteal reflection and visible bone, being exceeded only in special cases of need to reach the zygomatic notch and fully expose the external surface of the malar region, an area dedicated to implant site preparation.
Figure 3.
Upon patient acceptance, she was admitted in an outpatient setting to undergo the surgical procedure, performed with local anesthesia. A small incision was made in the alveolar crest, from the right region of the first molar to the left, preserving the descending palatine artery, which, due to anatomical evolution of the atrophic maxilla, changes its position. Two posterior vestibular incisions were performed bilaterally, considering the appearance of Parotid duct, in order not to cause accidental injuries, and finally, a median release incision was made below the nasal column. Subsequently, a mucoperiosteal flap was simultaneously raised bilaterally along the entire incision. Reflection of mucoperiosteal flap may be performed in two different manners, depending on the surgical procedure involved: placement of only two implants in zygomatic bone or an all-on-four surgery. In surgical case of placement of two zygomatic implants, the mucoperiosteal flap is elevated to expose the alveolar crest, the anterolateral wall of maxillary sinus and the origin of zygomatic arch, where masseter muscle is inserted. However, in this case, mucoperiosteal flap from the paranasal region was elevated medially until the infraorbital nerve appeared. Infraorbital foramen is the posterior limit of mucoperiosteal reflection and visible bone, being exceeded only in special cases of need to reach the zygomatic notch and fully expose the external surface of the malar region, an area dedicated to implant site preparation.
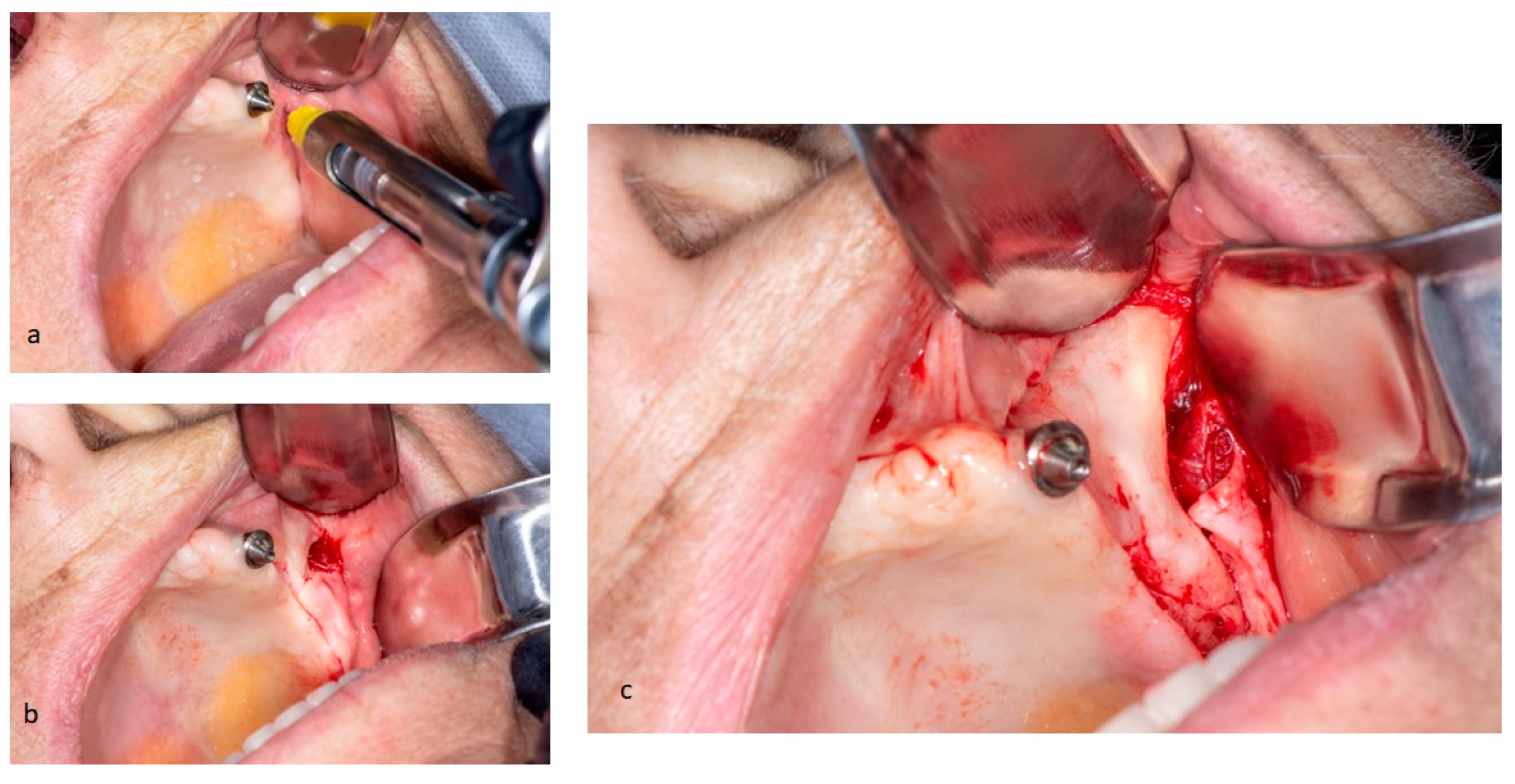
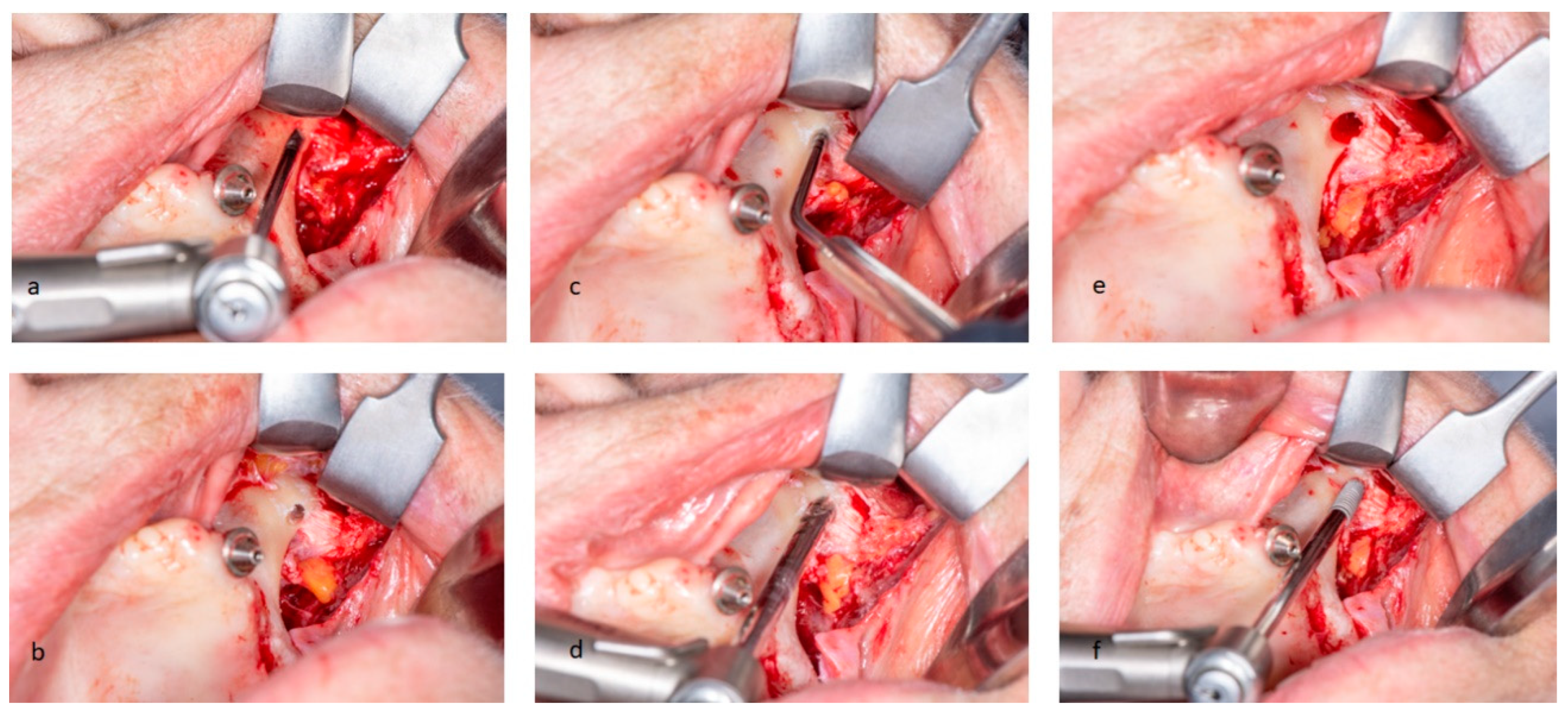
Figure 4.
The implant site was prepared with drills of 4-mm diameter, in a handpiece with a contra-angle. This step was facilitated due to positioning of implant in the posterior zygomatic bone distal to the region of maxillary second premolar. Anterolateral wall of maxillary sinus guided the definition of the most suitable place to position a Pilar Z. They were connected to intraoral emergence of the zygomatic implant previously determined using zygomatic drills for preparation of grooves. These drills have a non-working tip and a cylindrical diamond body with three different levels of sand (fine, medium, coarse). The non-functioning conical tip of the drill is inserted into the marking point that provides a valid support site for subsequent bone preparation in premolar and distal canine region, moving from thicker to thinner drill. The drill was further deepened with a tangential forward movement until it reached two thirds of its diameter. This procedure performed correctly respects the integrity of the membrane. In order not to tear sinus mucosa during the following actions, a gentle inward displacement of the membrane with the sinus and periosteum must be performed.
Figure 4.
The implant site was prepared with drills of 4-mm diameter, in a handpiece with a contra-angle. This step was facilitated due to positioning of implant in the posterior zygomatic bone distal to the region of maxillary second premolar. Anterolateral wall of maxillary sinus guided the definition of the most suitable place to position a Pilar Z. They were connected to intraoral emergence of the zygomatic implant previously determined using zygomatic drills for preparation of grooves. These drills have a non-working tip and a cylindrical diamond body with three different levels of sand (fine, medium, coarse). The non-functioning conical tip of the drill is inserted into the marking point that provides a valid support site for subsequent bone preparation in premolar and distal canine region, moving from thicker to thinner drill. The drill was further deepened with a tangential forward movement until it reached two thirds of its diameter. This procedure performed correctly respects the integrity of the membrane. In order not to tear sinus mucosa during the following actions, a gentle inward displacement of the membrane with the sinus and periosteum must be performed.
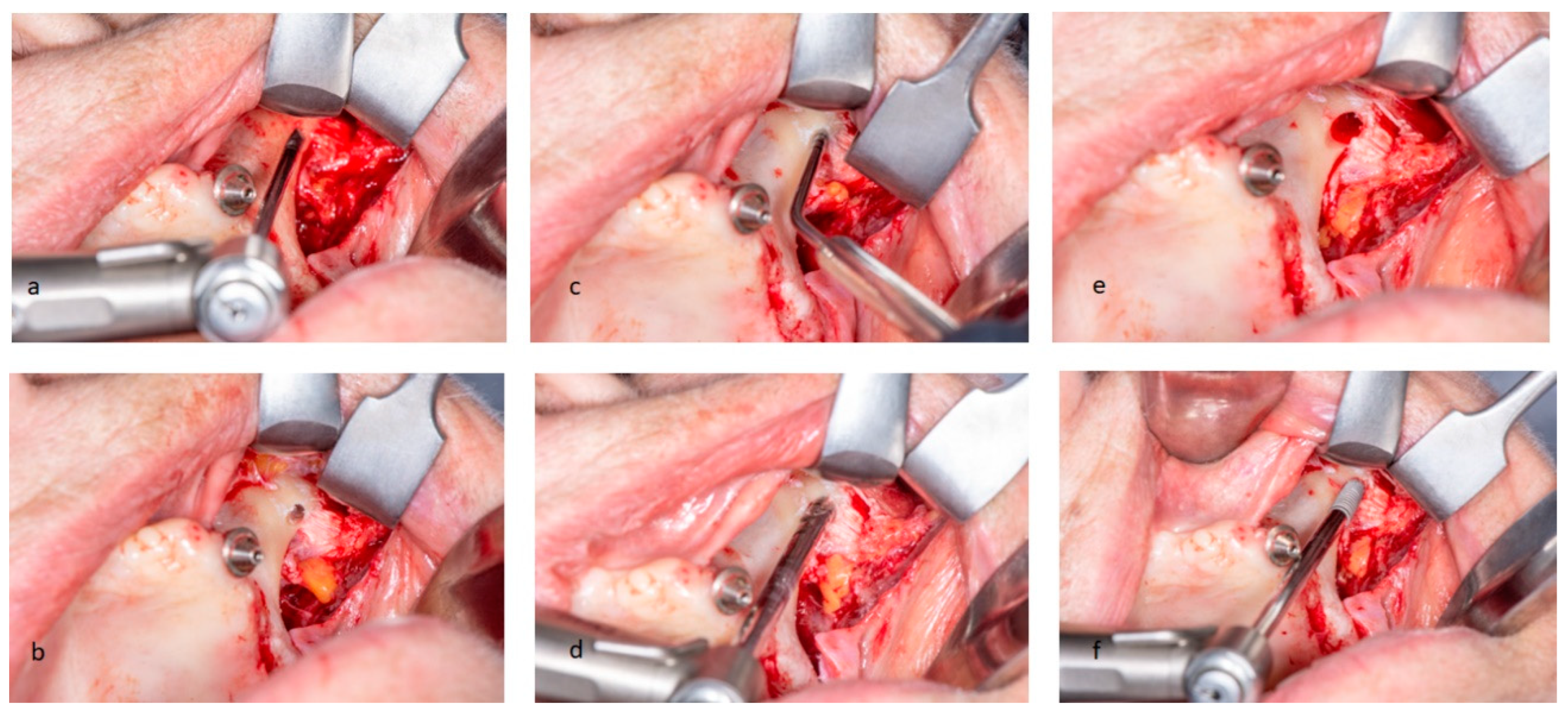
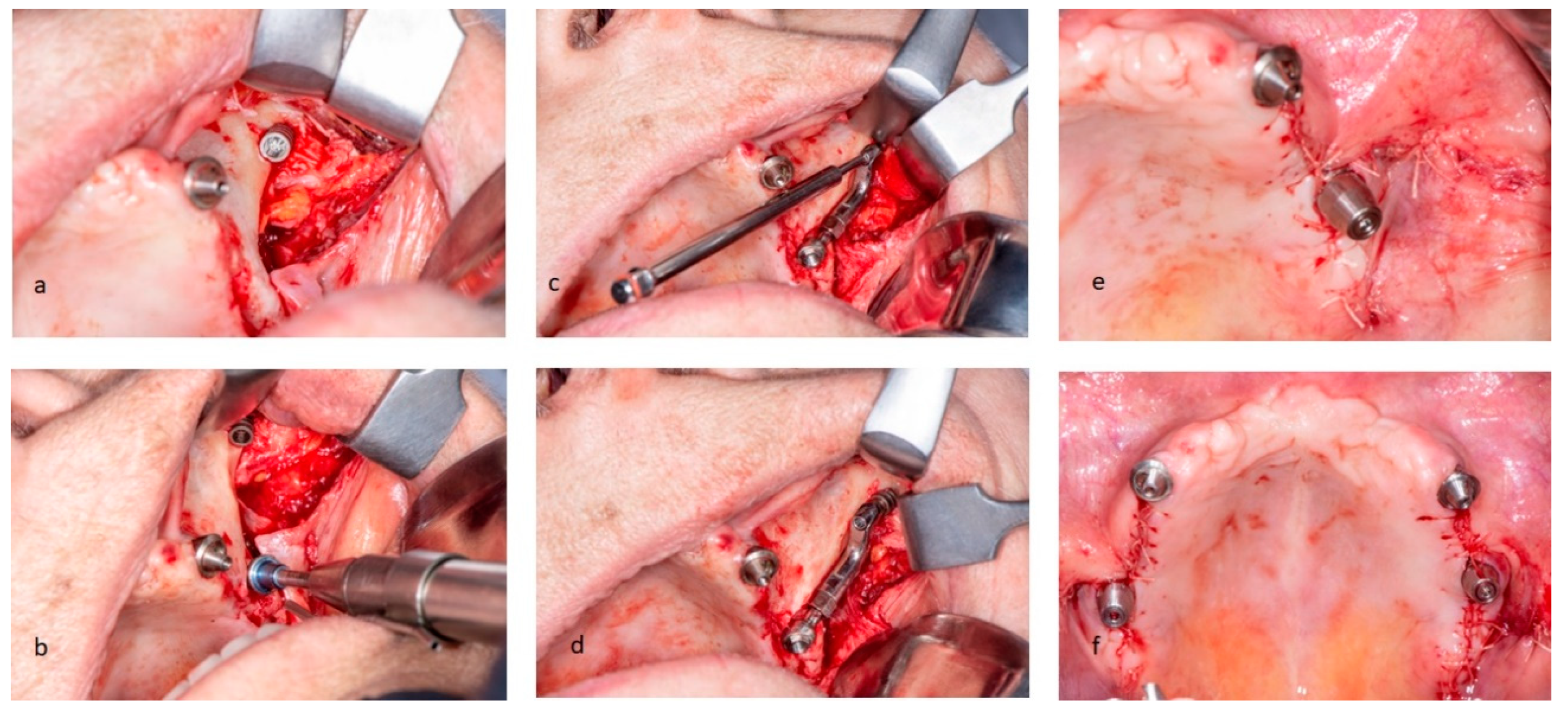
Figure 5.
Finally, a depth indicator was used to decide the correct length of zygomatic attachment. Depth gauge tip was located on the external cortical zygomatic bone. The diameter of final hole in zygomatic arch performed by the drills was approximately 2.2 mm in diameter, much smaller than the final circumferential size of the implant (3.2 mm). This difference avoids the risk of the zygoma device tip protruding from the bone during malar screwing, when looking for primary stability. Resorbable suture completed the surgical intervention.
Figure 5.
Finally, a depth indicator was used to decide the correct length of zygomatic attachment. Depth gauge tip was located on the external cortical zygomatic bone. The diameter of final hole in zygomatic arch performed by the drills was approximately 2.2 mm in diameter, much smaller than the final circumferential size of the implant (3.2 mm). This difference avoids the risk of the zygoma device tip protruding from the bone during malar screwing, when looking for primary stability. Resorbable suture completed the surgical intervention.
Figure 6.
The patient received post-surgical instructions and medications. New prosthetic protocols were installed right after the surgery process.
Figure 6.
The patient received post-surgical instructions and medications. New prosthetic protocols were installed right after the surgery process.
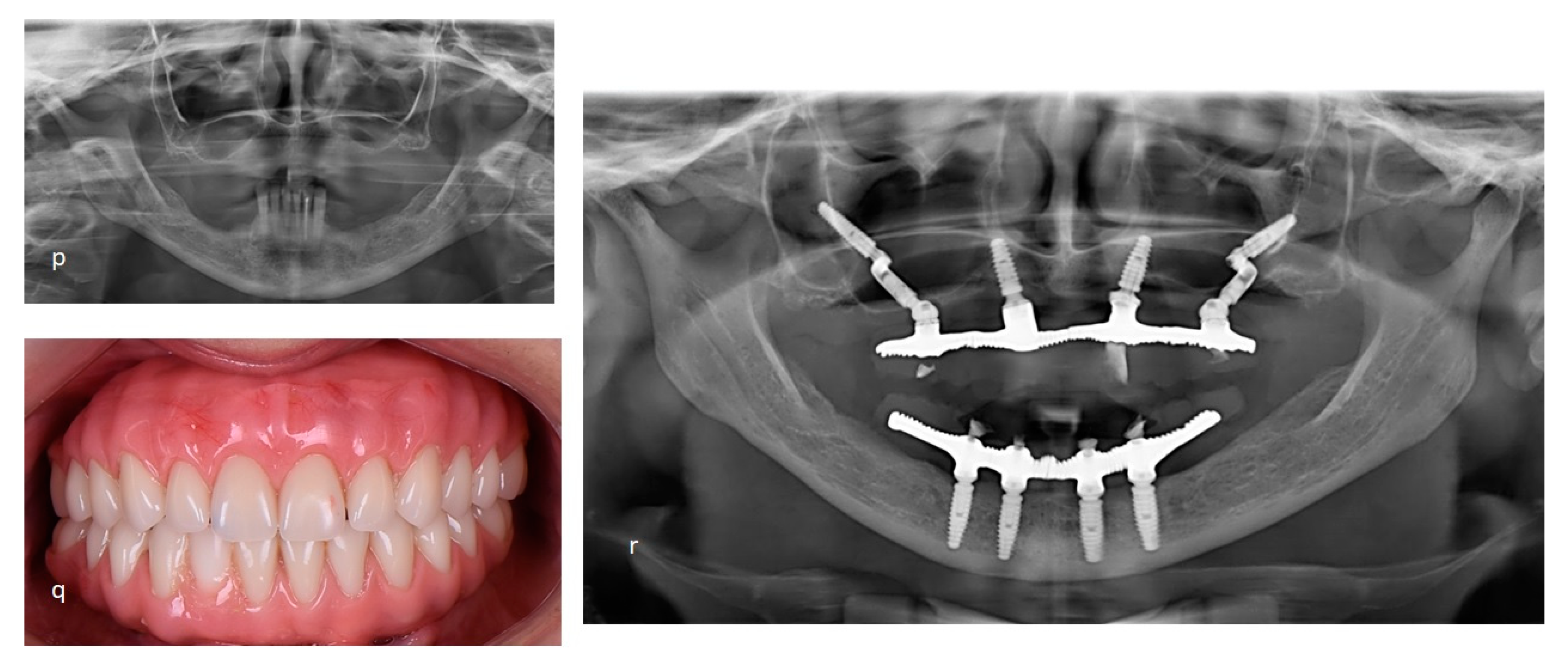
Figure 7.
The second case report shows the Facco technique used to rehabilitate a female patient, 58 years, without teeth or implants at atrophic maxilla and monitoring by 36 months after the surgical. A. Infiltrative anestesia at zygomatic arch. B. Incisions nealy zygomatic arch. C. Displacement gingival flap and suture to facilitate access at zygomatic area. D-G. Surgical sequence at right side until the setup pilar Z. H. Initial evaluation of the zygomatic boné. I. Milling cavity at zygomatic arch. J-M. Surgical sequence at left side. N. Implants positions favoring the posterior prosthetic rehabilitation. P. Initial panoramic radiography showing atrophic maxilary. Q. Final photo. R. Panoramic radiography final showing all-on-4 by Facco techinique.
Figure 7.
The second case report shows the Facco technique used to rehabilitate a female patient, 58 years, without teeth or implants at atrophic maxilla and monitoring by 36 months after the surgical. A. Infiltrative anestesia at zygomatic arch. B. Incisions nealy zygomatic arch. C. Displacement gingival flap and suture to facilitate access at zygomatic area. D-G. Surgical sequence at right side until the setup pilar Z. H. Initial evaluation of the zygomatic boné. I. Milling cavity at zygomatic arch. J-M. Surgical sequence at left side. N. Implants positions favoring the posterior prosthetic rehabilitation. P. Initial panoramic radiography showing atrophic maxilary. Q. Final photo. R. Panoramic radiography final showing all-on-4 by Facco techinique.
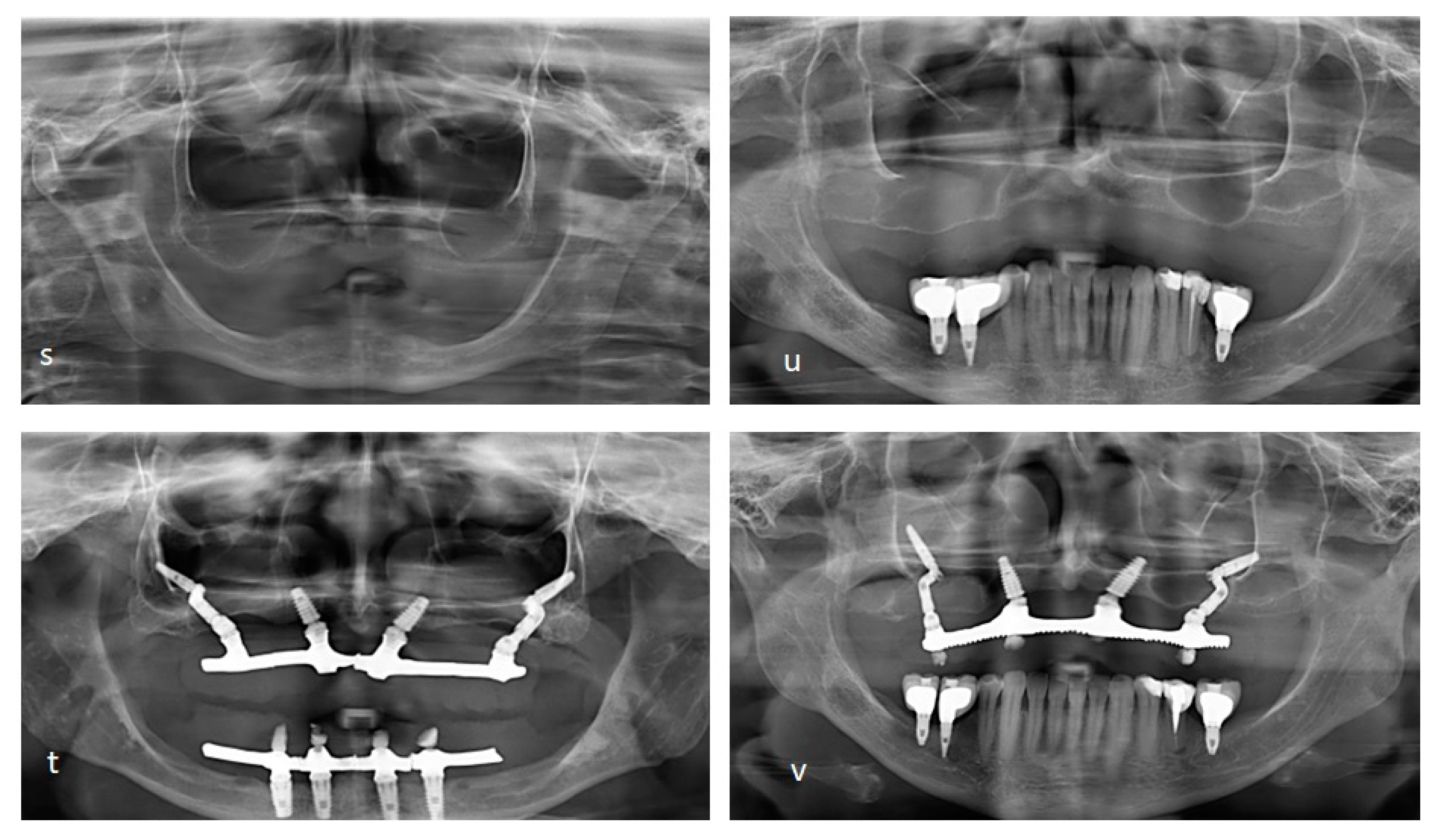
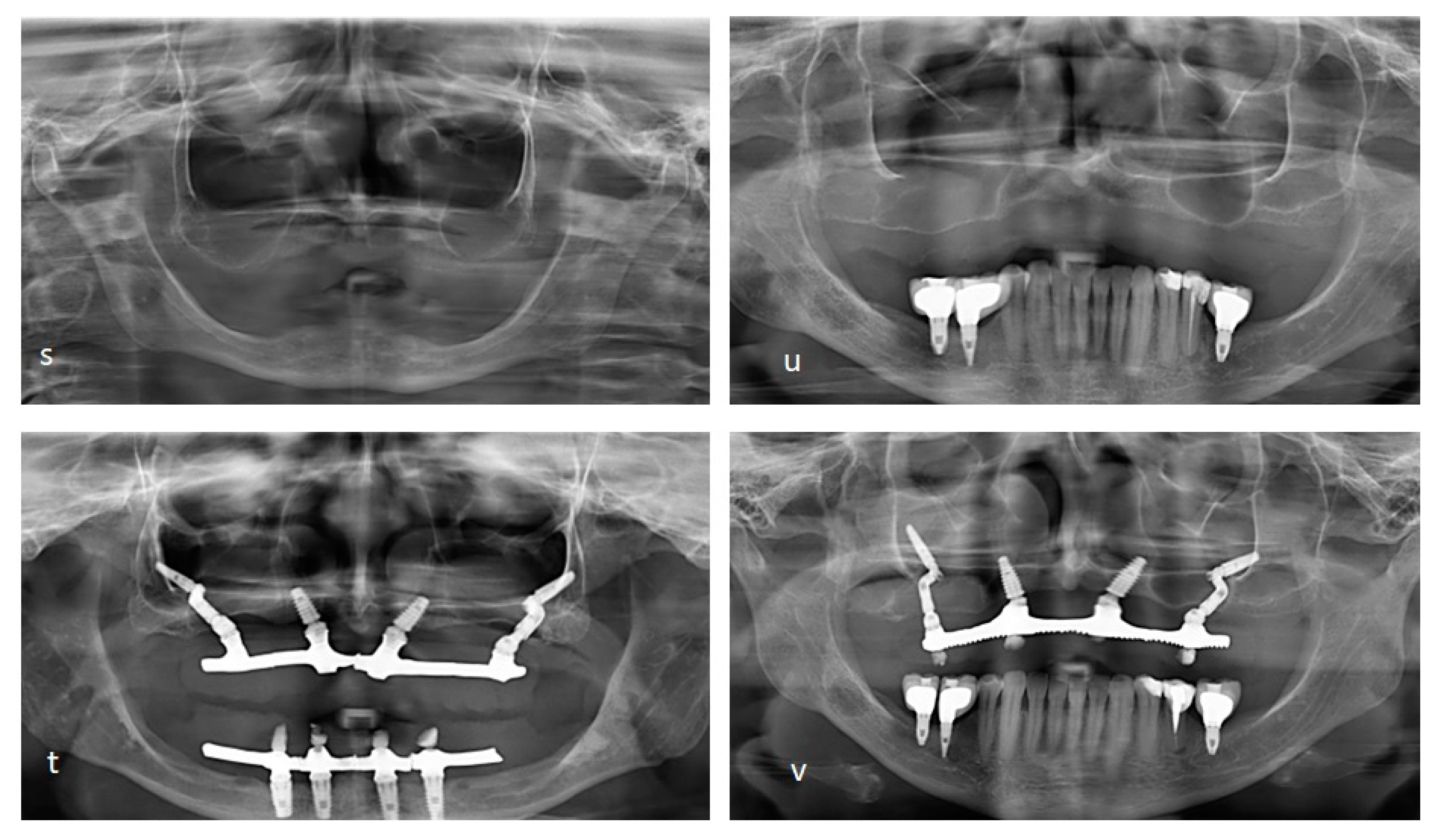
Figure 8.
The initial condition, monitoring by 26 months after the surgical of a male patient, at 66 years (s-t) and a female patient at 60 years with monitoring by 36 month (u-v). It is possible to use the Facco technique with different angles between the zygomatic bone and the lateral wall of the maxilla. Based on the classification for zygomatic implant patient based on the zygoma anatomy guided approach [
3], type 0 and 1 can be performed through a groove to access the maxillary sinus and move it. It is possible to achieve better anchorage using a more favorable angle for this maneuver compared to the traditional zygomatic implant technique. For type 2, the Pilar Z makes it possible to move the sinus wall slightly to insert the implant in the closest ideal position. Access to the sinus wall is not necessary for types 3 and 4. With all these adaptations provided by using the Pilar Z, it is possible to reduce and avoid post-surgical complications resulting from installing an implant in the zygomatic bone, as well as rhinitis and sinusitis, difficulty and discomfort when using the prostheses, the appearance of implant threads and perio-implant problems resulting from tissue recession, or musosites. These gains are mainly possible due to part C of the component, which is thinner than traditional zygomatic implants and is positioned with at least half of its length inside the bone, allowing better adaptation in the wider region of the zygomatic bone (approximately 4.1mm) [
4].
Figure 8.
The initial condition, monitoring by 26 months after the surgical of a male patient, at 66 years (s-t) and a female patient at 60 years with monitoring by 36 month (u-v). It is possible to use the Facco technique with different angles between the zygomatic bone and the lateral wall of the maxilla. Based on the classification for zygomatic implant patient based on the zygoma anatomy guided approach [
3], type 0 and 1 can be performed through a groove to access the maxillary sinus and move it. It is possible to achieve better anchorage using a more favorable angle for this maneuver compared to the traditional zygomatic implant technique. For type 2, the Pilar Z makes it possible to move the sinus wall slightly to insert the implant in the closest ideal position. Access to the sinus wall is not necessary for types 3 and 4. With all these adaptations provided by using the Pilar Z, it is possible to reduce and avoid post-surgical complications resulting from installing an implant in the zygomatic bone, as well as rhinitis and sinusitis, difficulty and discomfort when using the prostheses, the appearance of implant threads and perio-implant problems resulting from tissue recession, or musosites. These gains are mainly possible due to part C of the component, which is thinner than traditional zygomatic implants and is positioned with at least half of its length inside the bone, allowing better adaptation in the wider region of the zygomatic bone (approximately 4.1mm) [
4].
Author Contributions
All authors (EFAC, CAMD, PHRA, MMP) have read and agreed to the published version of the manuscript.
Funding
This research was funding by Dr. Elton Facco.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to it is a retrospective case report, which did not impact the management of the patient.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Acknowledgments
We appreciate the support of Implacil De Bortol.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rosenstein J, Dym H. Zygomatic Implants: A Solution for the Atrophic Maxilla. Dent Clin North Am [Internet]. 2020;64(2):401–9. [CrossRef]
- Agliardi EL, Panigatti S, Romeo D, Sacchi L, Gherlone E. Clinical outcomes and biological and mechanical complications of immediate fixed prostheses supported by zygomatic implants: a retrospective analysis from a prospective clinical study with up to 11 years of follow-up. Clin Implant Dent Relat Res 2021;23(4):612-24. [CrossRef]
- Aparicio C. A proposed classification for zygomatic implant patient based on the zygoma anatomy guided approach (ZAGA): a cross-sectional survey. Eur J Oral Implantol 2011;4(3):269-75.
- Costa EFA, Penteado MM, Maior BS. Comparative analysis of biomechanical response between zygomatic implant and Facco technique through the three-dimensional finite element method. J Clin Exp Dent. 2023;15(2):e96-101. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).