1. Introduction
Diabetes mellitus (DM) affects over 19.4 million adults aged 20 to 79 years, with 4.5 million of them living in South Africa [
1]. Diabetic foot sepsis (DFS) is defined by the World Health Organization as a severe complication of diabetes and is characterised by: foot ulceration associated with neuropathy; varying degrees of ischemia; and infection [
2]. It usually affects 19-34% of diabetic patients and results in severe consequences like amputations [
3]. Diabetic foot sepsis predominantly affects males, particularly those with type 2 diabetes, and its prevalence in Africa exceeds the global average with higher rates of adverse outcomes, including major amputations and mortality [
5,
6,
7,
8,
9]. Most cases of DFS are preceded by a neuropathic, ischaemic or neuro-ischaemic ulcer and its complex pathogenesis results from a combination of factors including: poor glycaemic control; host-related elements; and microbial characteristics [
9]. Essentially, the hyperglycaemia, driven by either relative or absolute insulin deficiency, leads to neuropathy, vasculopathy and immunopathy which allows DFS to manifest and therefore adequate management is essential in its treatment to prevent adverse outcomes that affect the patient, in the form of amputation, and burden the health care system financially [
3].
It is crucial that, during the investigation of diabetic foot ulcers, an adequate specimen be collected to facilitate microbial culture, thereby enabling the determination of the organism’s susceptibility and resistance patterns. While the generation of this specific data requires time, clinical guidelines should advocate for empiric therapy targeting the most frequently implicated pathogens in the interim [
3]. Consequently, antibiograms, which illustrate the susceptibility profiles of the most specifically implicated organisms derived from cultures, are essential for the timely management of diabetic foot ulcers (DFS) [
10,
12]. This is particularly important as DFS often involves a diverse range of microorganisms, presenting as either mono- or polymicrobial infections, each with different susceptibility profiles [
10,
11].
The frequently isolated organisms in patients with DFS are aerobic gram-positive cocci, with Staphylococcus aureus being the most predominant species [
13]. Polymicrobial and chronic infections often involve anaerobic organisms and gram-negative aerobic bacilli such as Pseudomonas aeruginosa and Enterobacteriaceae [
11,
14]. Emergence of antimicrobial resistance is a growing concern and various strains including extended-spectrum β-lactamase-producing Enterobacteriaceae, methicillin-resistant Staphylococcus aureus (MRSA), specific Pseudomonas aeruginosa strains and vancomycin-resistant enterococci are implicated in DFS [
11,
13,
14].
Obtaining high-quality and representative samples for microscopy, culture, and targeted antibiotic therapy is crucial for the effective management of patients with infections, including diabetic foot infections (DFIs) [
12,
15]. This practice allows clinicians to initiate appropriate antibiotic therapy tailored to local microbial resistance patterns, ensuring better clinical outcomes. When antimicrobial treatment is based on accurate identification of pathogens, it minimizes the chances of administering inappropriate or broad-spectrum antibiotics. On the other hand, the inappropriate or excessive use of antimicrobials in non-specific conditions can significantly contribute to the rise of antimicrobial resistance. This not only complicates future treatment options but also imposes additional financial burdens on healthcare systems [
15,
16]. Thus, targeted treatment is critical for preventing the development and spread of resistant organisms, which can have far-reaching consequences on both individual patient health and public health outcomes. The primary goal of antibiograms is to support this targeted approach by providing data on local susceptibility patterns, thereby guiding clinicians in selecting the most effective antibiotics for each case [
17]. By integrating antibiogram data into clinical practice, healthcare providers can reduce the misuse of antibiotics and contribute to the global effort to curb antimicrobial resistance.
There are numerous methods available to obtain samples that accurately represent the causative organism in diabetic foot syndrome (DFS) infections. These include deep tissue biopsies, sampling adjacent bone near the infection site, pus swabs, blood cultures, and aspirates, to name a few. While the gold standard for diagnosis is a deep tissue biopsy, it is often acceptable to collect more superficial samples in certain cases. However, when there is suspicion of bone involvement, such as in osteomyelitis, a deeper sample may provide a more accurate representation of the infection, as superficial swabs might miss important pathogens. For example, skin commensals like Coagulase-negative staphylococci (CoNS), which may not be flagged in a superficial swab, could be identified as the primary cause of DFS if a deeper sample is obtained [
19]. In cases where there is no bone infection, superficial cultures are often sufficient for diagnosing diabetic foot infections (DFI). However, when osteomyelitis is suspected, obtaining deep cultures becomes critical, as relying solely on superficial swab cultures to identify the pathogens responsible for bone infections is less accurate, with detection rates falling below 40% [
20]. This discrepancy highlights the importance of using appropriate sampling techniques based on the clinical scenario to ensure accurate diagnosis and effective treatment. Moreover, accurate sampling helps to avoid inappropriate antimicrobial therapy, which can contribute to antimicrobial resistance and poor clinical outcomes. In this context, understanding the limitations of superficial swabs and prioritizing deeper tissue sampling when necessary is key to improving DFS management and patient outcomes.
It is also important to note that various classification systems can guide management of DFS. There are various classification systems and no one is universally accepted. The use of a system depends on clinician knowledge of those systems as well as their usability as some may be more complex over another. It is important to use a system that takes into account the extent of the DFS, microbes implicated, level of ischaemia and diabetes [
21]. While the
Wagner-Meggitt system is widely used for its simplicity, it lacks detail about crucial factors like ischaemia and infection and only takes into account the depth of the ulcer and extent of gastrointestinal gangrene. This makes systems like the
University of Texas classifications potentially more valuable for guiding treatment despite their complexity as they include comments of the Wagner system and build on it by including ischaemia and infection [
21]. Another classification called the PEDIS is profoundly more accurate as they include components of DFS in its acronym: namely perfusion, extent, depth, infection and sensation. This system provides information about the risk of neuropathy and vascularity, which can influence the management of DFS [
21]. WIfI is an another classification that takes into account the severity of
peripheral arterial disease (PAD), wound characteristics, and
infection burden to determine the likelihood of wound healing and the risk of major amputation [
23]. Depending on the severity based on the classification, it can allow antibiotic duration to be determined [
23].
Effective treatment of diabetic foot syndrome (DFS) hinges on a comprehensive understanding of the microbiology and susceptibility patterns of infections commonly associated with DFS. Therefore, evaluating antimicrobial utilization and management trends in low- and middle-income settings is critical for developing effective treatment strategies for this growing health issue, which imposes not only functional constraints on patients but also significant financial burdens on the healthcare system. This challenge is especially pronounced in low- and middle-income countries, where limited resources, lack of access to advanced medical care, and suboptimal antibiotic stewardship exacerbate the problem. By addressing these gaps, healthcare providers can improve outcomes for patients suffering from DFS. Consequently, this study aimed to identify the primary causative organisms responsible for DFS infections and their susceptibility profiles in patients undergoing treatment at our institution
Our hope is that the findings from this research will contribute to enhancing patient care, optimizing antimicrobial usage, and supporting global efforts to combat the rise of antimicrobial resistance, which poses a serious threat to public health worldwide. The study also underscores the need for localized data in shaping evidence-based guidelines tailored to the specific challenges faced in resource-limited settings
2. Patients and Methods
This was a retrospective cross-sectional observational study focusing on patients aged 18 years and older who were admitted to the Department of Surgery at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) with DFS from 1st January 2017 to 31st December 2019. The study included patients with both primary and recurrent DFS. Data was obtained from weekly morbidity and mortality (M&M) meeting reports stored in the Research Electronic Data Capture (REDCap) database, discharge summaries, and hospital admission files. Data collected included age, sex, race, specimen collected for MC&S and results, antimicrobial(s) prescribed and overall outcome. The outcome data collected included the type of surgical intervention, level of amputation and death.
Descriptive statistical analysis was carried out using STATA SE 17.0 software. Data were tabulated and visually represented using Excel version 16.65, which included pie charts, dot and box plots, and histograms. Categorical data, such as types of specimens collected, antimicrobials prescribed, and resistance patterns of organisms, were presented as percentages. The study also examined resistance to antimicrobials in relation to gender and race, with confidence intervals determined using the exact method. Ethical clearance for the study was obtained from the Human Research Ethics Committee of University of the Witwatersrand (M210943).
3. Results
Hundred and sixty-eight (168) records met the inclusion criteria. The median age of the included patients was 59 years (IQR 54-67). The median age of male patients was 58.9 years compared to 61 years for females. Eighty-nine (53%) of the patients were black Africans, while 26% (44) were of Caucasians (26%). Majority, 94.6% of the patients had type II DM. Most cases, 95.8%, presented with wet gangrene of the toes or mid-foot (
Table 1).
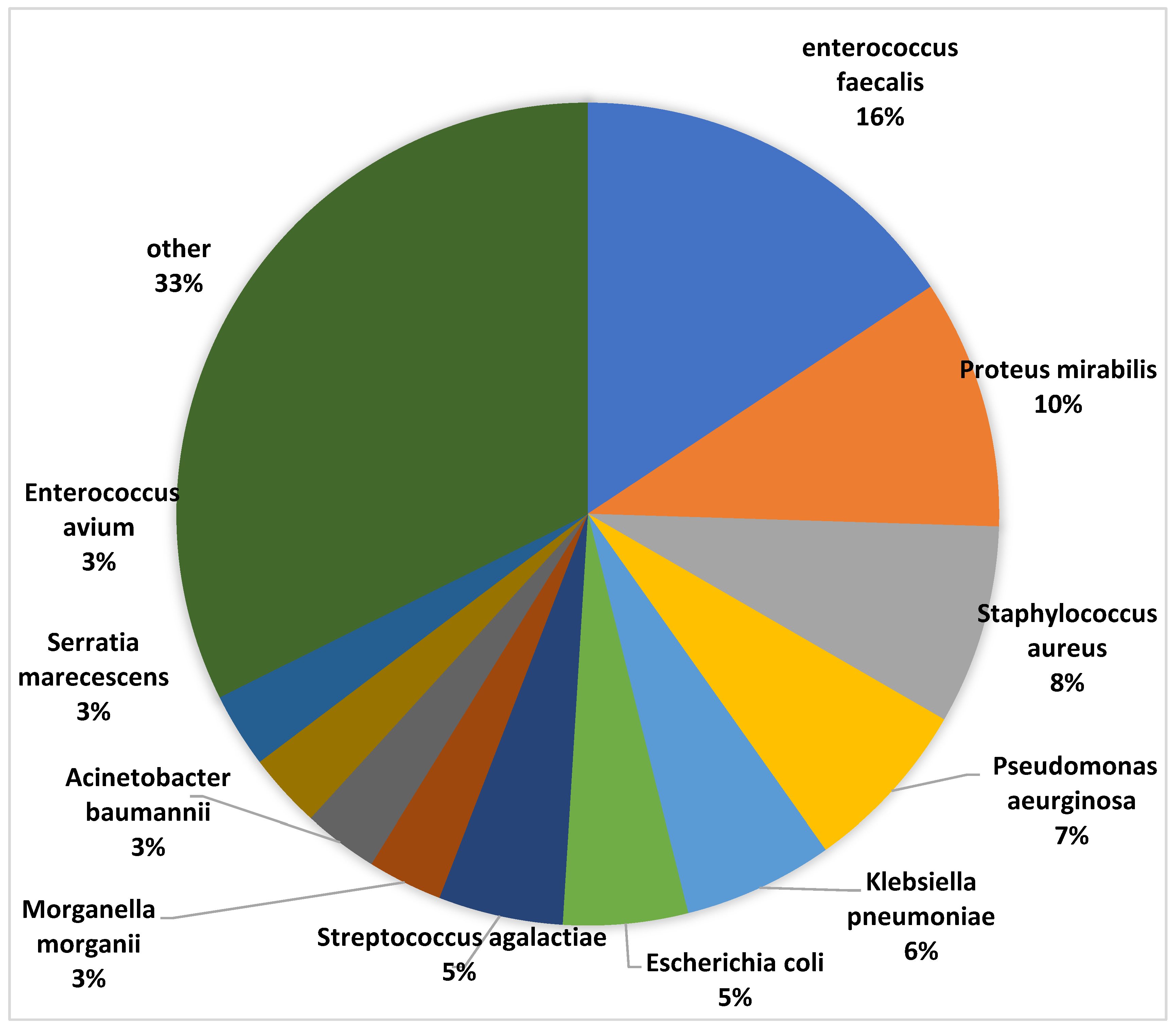
The top 5 commonly isolated organisms were Enterococcus faecalis (16%), Proteus mirabilis (10%), Staphylococcus aureus (8%), Pseudomonas aeruginosa (7%) and Klebsiella pneumoniae (5%) (
Figure 1).
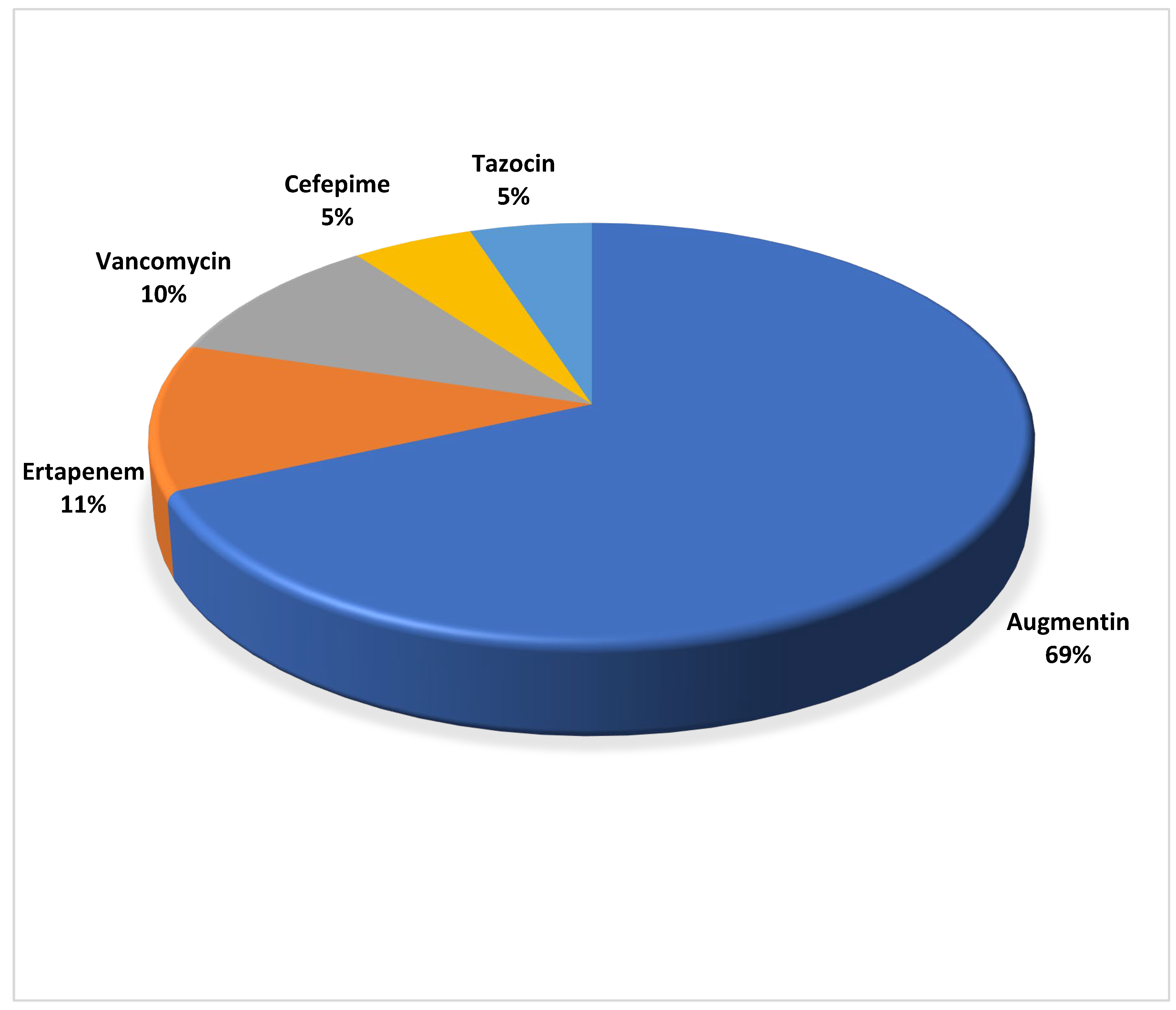
Of the top 11 identified organisms, Klebsiella pneumoniae, Morganella morganii, and Actinobacteria baumanii exhibited the highest proportion of antibiotic resistance, with 100% resistant. Staphylococcus aureus demonstrated 88% resistance rate (95% CI [0.47-0.99]), followed by Proteus mirabilis which exhibited an 80% resistance rate (95% CI [0.44-0.97]) and Pseudomonas aeruginosa with a 71% resistance rate (95% CI [0.29-0.96]). Enterococcus faecalis, the most commonly isolated organism, displayed the least antibiotic resistance of 6.7% (95% CI [0.0-0.32]). Record of intravenous antimicrobials prescription were traced in 45.2% (73/168) of the cases and Amoxicillin/Clavulanic acid was prescribed in 69% (50/73) of the patients (
Figure 2).
Ertapenem was prescribed in 11%, followed by Vancomycin at 10%, Piperacillin/Tazobactam and Cefepime at 5% each. Other broad-spectrum antimicrobials and combinations were prescribed in less than 2% of cases each. Ampicillin/amoxicillin was tested against the top 11 most cultured organisms, and demonstrated 100% resistance against most of them and 8.3% against Enterococcus faecalis. All cases of Serratia marcescens and Morganella morganii were resistant to Amoxicillin-Clavulanic acid while Klebsiella pneumoniae, Proteus mirabilis, and Escherichia coli displayed resistance rates of 80%, 50%, and 25%, respectively. Ertapenem, the second most commonly prescribed antibiotic, exhibited 50% resistance against E. coli and Klebsiella pneumoniae and no resistance against Proteus mirabilis and Morganella morganii. Cefepime displayed high resistance rates, with 100% resistance against P. mirabilis, Pseudomonas aeruginosa, E. coli, and Acinetobacter baumanii; 75% resistance against Klebsiella pneumoniae; and 50% resistance against Serratia marcescens. Tazobactam-Piperacillin showed high resistance rates against Klebsiella pneumoniae (100%), Acinetobacter baumannii (100%), Pseudomonas aeruginosa (50%), and Morganella morganii (50%), but exhibited nil resistance against Proteus mirabilis. Gram-negative specimens displayed 100% resistance to ampicillin/amoxicillin, gentamycin, ampicillin, ceftriaxone, cefuroxime, cefoxitin, trimethoprim, and trimethoprim/sulfamethoxazole. They also showed some degree of resistance to other common antimicrobials such as amikacin, tobramycin, amoxicillin, amoxicillin/clavulanic acid, piperacillin/tazobactam, cefepime, cefotaxime, ceftriaxone, cefoxitin, ceftazidime, ciprofloxacin, and tigecycline, with at least one bacterial sample demonstrating 100% resistance to these antimicrobials. Ertapenem and imipenem showed promising results, with resistance levels recorded at 50% and 60%, respectively, for gram-negative specimens. Gram-positive specimens exhibited lower resistance rates per antibiotic. Ampicillin showed 100% resistance against S. aureus and E. faecalis, the only gram-negative bacteria it was tested against. Other penicillin drugs, except for amoxicillin, displayed at least one 100% resistant sample when tested. Macrolides, clindamycin, cefotaxime/ceftriaxone, and trimethoprim/sulfamethoxazole had no resistance.
A significant number of DFS patients had polymicrobial infections, with males having a higher polymicrobial culture load compared to females at 79% and 50%, respectively. The most common isolated organisms in males were Enterococcus faecalis (16.9%), followed by Staphylococcus aureus (9.2%), Klebsiella pneumoniae (7.7%), and Proteus mirabilis (7.7%). In females, Enterococcus faecalis, Proteus mirabilis, and Pseudomonas aeruginosa were all at 14.3% each, followed by Streptococcus agalactiae (8.6%) and Staphylococcus aureus (5.7%). Notably, no isolates of Serratia marcescens were found in females (
Table 3).
The top three organisms varied based on race. In the Black population, the most common organisms were Enterococcus faecalis (18.5%), Proteus mirabilis (9.3%), and Klebsiella pneumoniae (7.4%). Among Caucasians, Staphylococcus aureus (20%) was the most common, followed by Proteus mirabilis (15%), and a tie for third place between Enterococcus faecalis, Pseudomonas aeruginosa, and Morganella morganii, all at 10%. In the Indian population, the most common organisms were Pseudomonas aeruginosa (18.2%), followed by Enterococcus faecalis (13.6%), and a tie for third place between Proteus mirabilis, Klebsiella pneumoniae, and Escherichia coli, all at 9%.
4. Discussion
The increasing prevalence of diabetes, combined with improved diabetes management, has led to a longer duration of diabetes and an elevated risk of diabetic complications, including DFS [
18]. In this study, the mean age of patients with DFS was 59 years, falling within the range reported in similar studies conducted in Kenya and the United States [
21,
22]. Notably, a higher proportion of complications occurs in the 45-64 years age group, aligning with the mean age in this study [
18]. The earlier onset of complications and variable age of complications in males may be attributed to multiple risk factors, including concurrent conditions such as hypertension, smoking habits and diabetes control, as well as healthcare-seeking behaviours [
18]. However, these factors were not extensively examined in this study.
The prevalence of polymicrobial infections in DFS patients in this study, with 77% of cases presenting with multiple microbial species, is notable. This high incidence could be associated with the severity of presentations, previous non-compliant antimicrobial use, and extended hospital stays. While some studies have reported a predominance of monomicrobial growth in DFS samples, the higher rate of polymicrobial infections observed here suggests a more complex disease profile in this specific patient population [
24,
25].
The observed differences in polymicrobial aetiology between men and women could be attributed to variations in exposure to environmental pathogens, differences in health management behaviours, and cultural factors [
11,
14]. While external factors, such as prehospital care and hygiene practices, may have influenced the diversity of organisms based on race, these findings highlight the importance of considering individual and cultural factors in managing DFS. It is essential to remain vigilant regarding trends and their implications for patient care
The most isolated organism in this study was Enterococcus faecalis, which differs from the findings of a global meta-analysis by McDonald et al., where Staphylococcus aureus was identified as the predominant isolate in diabetic foot infections [
26]. This variation may be due to patients in the quaternary hospital setting presenting at more advanced stages of the disease and with greater immunocompromise, which could allow unusual commensals like Enterococcus faecalis to predominate [
17]. Notably, the resistance patterns of Enterococcus faecalis in this study align with South African resistance patterns found by Shobo et al., with resistance to Vancomycin and little resistance to peenicillins [
27]. This study also shows that Enterococcus spp. are also isolated in patients that require prolonged antibiotic therapies and can be mirrored to those with severe DFS who often get more than one infection and require prolonged treatment. The data also indicates that combination therapy is more effective, with the resistance rate to ampicillin/amoxicillin being 8,3%. This is particularly significant, given the propensity of Enterococcus faecalis to develop resistance [
28].
Although not specifically tested against E. faecalis in this study, macrolides, ceftriaxone, cefotaxime, and clindamycin showed
0% resistance against Staphylococcus aureus. Given the close relationship between these two Gram-positive cocci and their often-overlapping resistance patterns [
29], this finding suggests that macrolides and clindamycin might also demonstrate promising susceptibility against E. faecalis. However, further testing is required to confirm this.
In this study it was also found that gram negative bacteria predominate over gram positives in infections that presented to our tertiary hospital and this is in keeping with other low-middle income Asian countries’ with severe DFS [
17]. According to global data, diabetic foot sepsis infections are predominantly caused by gram-positive cocci such as Staphylococcus aureus (including MRSA) and β-haemolytic streptococcus species [
9,
10,
30]. Chronic and polymicrobial infections often involve anaerobic and gram-negative aerobic bacilli, including Pseudomonas aeruginosa and Enterobacteriaceae [
30]).
Intriguingly, a significant portion of patients in this study did not receive intravenous antibiotic prescriptions. Intravenous antimicrobials were only used in severe deep infections, systemic inflammatory response syndrome (SIRS), or septicaemia with antimicrobials. This prescription trend is in keeping with a general approach to DFS using the WIFi classification and a multidisciplinary team [
31,
32,
33]. Most sepsis cases in the study were localised to the forefoot and midfoot, and the analysis did not include prophylactic antimicrobials. Some DFS cases were chronic wounds with significant biofilm, thus managed with local antiseptic measures and dressing, including negative pressure therapy [
34].
It is important to highlight that the top three organisms identified belong to distinct bacterial groups:
Enterococcus spp.,
Streptococcus spp., and
Enterobacteriaceae spp. Due to their varying resistance and susceptibility profiles, the use of a broad-spectrum antibiotic is recommended as an initial treatment option. Broad-spectrum antibiotics, which are effective against a wide range of Gram-positive and Gram-negative aerobes and anaerobes, have been shown to be efficacious against all three groups. Examples include carbapenems and combination antibiotics such as piperacillin-tazobactam and amoxicillin-clavulanate. However, while these agents are critical in initial management, their use should be restricted to empiric therapy. Prompt de-escalation to targeted antibiotics, guided by resistance profiles obtained through proper specimen collection, should be strongly advocated [
35]. This approach is crucial for preventing the emergence of multidrug-resistant organisms, as it ensures that more effective antibiotics can be utilized for improved source control [
35].
This retrospective study presents critical limitations that must be carefully weighed when interpreting the findings. Foremost, the quality and completeness of the data drawn from medical records, discharge summaries, and hospital files may have introduced variations and influenced result robustness. A significant limitation arises from the relatively modest sample size. This limitation raises concerns about the generalizability of the findings, potentially omitting a more comprehensive spectrum of diabetic foot sepsis cases. Furthermore, the non-standardised culture methods employed in the study introduce variability in specimen collection and analysis, potentially impacting result accuracy. This methodological variability may have led to the collection of superficial skin colonisers rather than the specific pathogens associated with diabetic foot sepsis. These limitations underscore the need for future research with more extensive and diverse patient populations, standardised culture methods, and prospective data collection to provide a more comprehensive understanding of diabetic foot sepsis.
5. Conclusion
This study provides valuable insights into the management of diabetic foot sepsis (DFS), highlighting several key findings. A notable gender difference was observed, with DFS being more common in males. Amoxicillin/clavulanic acid was the most frequently prescribed antimicrobial, despite over 47% of patients receiving antibiotics without prior specimen collection for microbiology, culture, and sensitivity (MC&S). This underscores the need for more targeted and evidence-based treatment strategies to mitigate the risk of antimicrobial resistance. The microbiological analysis revealed Enterococcus faecalis and Proteus mirabilis as the most commonly isolated organisms, with more than 67% of the isolates exhibiting resistance to at least one antimicrobial agent. These findings stress the importance of routine specimen collection for MC&S to guide appropriate antibiotic therapy. Moreover, the prevalence of polymicrobial infections and high rates of resistance in this study highlight the need for improved stewardship in antimicrobial use, emphasizing de-escalation strategies after empiric therapy. To better inform clinical practice, future prospective, multicenter studies, particularly in low- to middle-income settings, are essential. Such research can help develop region-specific guidelines and enhance the overall management of DFS, improving patient outcomes while minimizing the threat of multidrug-resistant organisms
Author Contributions
“Conceptualization, SP,EJ,CG,OM,AS, WN,GM and TEL.; methodology, SP,EJ,CG,OM,AS, WN,GM and TEL.; formal analysis, SP,EJ,CG,OM,AS, WN,GM,MSM and TEL; investigation, SP,EJ,CG,OM,AS, WN,GM and TEL; resources, SP,EJ,CG,OM,AS, WN,GM and TEL; data curation, SP, MSM and TEL; writing—original draft preparation, SP, MSM and TEL; writing—review and editing, SP,EJ,CG,OM,AS, WN,GM,MSM and TEL,; supervision, TEL; project administration, SP. All authors have read and agreed to the published version of the manuscript
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. Ethical clearance was obtained from the Human Research Ethics Committee (Medical) of University of the Witwatersrand (M210943).
Informed Consent Statement
Patient consent was waived as the study was retrospective and was based on review of already collected records.
Data Availability Statement
Data supporting results in this study will be made available on request.
Acknowledgments
We sincerely appreciate the valuable inputs from the assessors of the Undergraduate Students Research at the Unit of Undergraduate Medical Education of University of the Witwatersrand during protocol development and presentation of the results.
Conflicts of Interest
The authors declare no conflicts of interest.”.
References
- Kamerman, P. Underdiagnosis of hypertension and diabetes mellitus in South Africa. S Afr Med J. 2022, 112, 53–60. [Google Scholar] [CrossRef]
- Tuttolomondo, A.; Maida, C.; Pinto, A. Diabetic foot syndrome: Immune-inflammatory features as possible cardiovascular markers in diabetes. World J Orthop. 2015, 6, 62–76. [Google Scholar] [CrossRef] [PubMed]
- Carro, G.V.; Saurral, R.; Saguez, F.S.; Witman, E.L. ‘Diabetic foot infections: Bacterial isolates from the centers and hospitals of Latin American countries’. The International Journal of Lower Extremity Wounds 2020, 21, 562–573. [Google Scholar] [CrossRef] [PubMed]
- Rossboth, S.; Lechleitner, M.; Oberaigner, W. Risk factors for diabetic foot complications in type 2 diabetes-A Systematic review. Endocrinol Diabetes Metab. 2020, 4, e00175. [Google Scholar] [CrossRef]
- Yu, Mk.; Lyeles, C.R.; Bent-Shaw, L.A.; Young, B.A. Sex disparities in diabetes process of care measures and self-care in high risk patients. J Diabetes Res. 2013, 2013, 575814. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017, 49, 106–116. [Google Scholar] [CrossRef]
- Abbas, Z.; Gill, G.; Archibald, L. The epidemiology of diabetic limb sepsis: an African perspective. Diabet Med. 2002, 19, 895–899. [Google Scholar] [CrossRef]
- Hicks, C.; Selvarajah, S.; Mathioudakis, N.; Sherman, R.; Hines, K.; Black, J.; et al. Burden of Infected Diabetic Foot Ulcers on Hospital Admissions and Costs. Ann Vasc Surg. 2016, 33, 149–158. [Google Scholar] [CrossRef]
- Spichler, A.; Hurwitz, B.; Armstrong, D.; Lipsky, B. Microbiology of diabetic foot infections: from Louis Pasteur to ‘crime scene investigation’. BMC Med. 2015, 13, 2. [Google Scholar] [CrossRef]
- Richard, J.; Lavigne, J.; Sotto, A. Diabetes and foot infection: more than double trouble. Diabetes Metab Res Rev. 2012, 28, 46–53. [Google Scholar] [CrossRef]
- Lipsky, B.; Berendt, A.; Cornia, P.; Pile, J.; Peters, E.; Armstrong, D.; Deery, G.; Embil, J.M.; Joseph, W.S.; Karchmer, A.W.; Pinzur, M.S.; Senneville, E. 2012 Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis. 2012, 54, e132–e173. [Google Scholar] [CrossRef] [PubMed]
- Law, T.; Chibabhai, V.; Nana, T. Analysis and comparison of cumulative antibiograms for the Charlotte Maxeke Johannesburg Academic Hospital adult intensive care and high-care units, 2013 and 2017. S Afri Med J. 2019, 110, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Nicolau, D.; Stein, G. Therapeutic Options for Diabetic Foot Infections; a review with emphasis on tissue penetration characteristics. J Am Podiatr Med Assoc. 2010, 100, 52–63. [Google Scholar] [PubMed]
- Lipsky, B. Diabetic Foot Infections: Microbiology Made Modern? Array of hope. Diabetes Care. 2007, 30, 2171–72. [Google Scholar] [CrossRef]
- Bhardwaj, S.; Mehra, P.; Dhanjal, D.S.; Sharma, P.; Sharma, V.; Singh, R.; Nepovimova, E.; Chopra, C.; Kuca, K. Antibiotics and antibiotics resistance-Flip sides of the same coin. Curr Pharm Des. 2022, 28, 3212–2329. [Google Scholar] [CrossRef] [PubMed]
- Pang, Z.; Raudonis, R.; Glick, B.R.; Lin, T.J.; Cheng, Z. Antibiotic resistance in Pseudomonas aeruginosa: mechanism and alternative therapeutic strategies. Biotechnol Adv. 2019, 37, 177–192. [Google Scholar] [CrossRef]
- Sultana, R.; Ahmed, I.; Saima, S.; Salam, M.T.; Sultana, S. Diabetic foot ulcer-a systematic review on relevant microbial etiology and antibiotic resistance in Asian countries. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 2023, 17, 102783. [Google Scholar] [CrossRef]
- Gregg, E.W.; Sattar, N.; Ali, M.K. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016, 4, 537–547. [Google Scholar] [CrossRef]
- Laakso, M.; Kiiski, J.; Karppelin, M.; Helminen, M.; Kaartinen, I. Pathogens causing diabetic foot infection and the reliability of the superficial culture. Surgical Infection 2021, 22, 334–339. [Google Scholar] [CrossRef]
- Nyamu, P.N.; Otieno, C.F.; Amayo, E.O.; McLigeyo, S.O. Risk factors and prevalence of diabetic foot ulcers at Kenyatta National Hospital, Nairobi. East Afr Med J. 2003, 80, 36–43. [Google Scholar] [CrossRef]
- Ghotaslou, R.; Memar, M.Y.; Alizadeh, N. Classification, microbiology and treatment of diabetic foot infections. Journal of Wound Care 2018, 27, 434–441. [Google Scholar] [CrossRef] [PubMed]
- McNeely, M.J.; Boyko, E.J.; Ahroni, J.H.; Stensel, V.L.; Reiber, G.E.; Smith, D.G.; Pecoraro, R.F. The independent contributions of diabetic neuropathy and vasculopathy in foot ulceration: How great are the risks? Diabetes Care. 1995, 18, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.W.; Canner, J.K.; Mathioudakis, N.; Sherman, R.; Malas, M.B.; Black 3rd, J.H.; Abularrage, C.J. The Society for Vascular Surgery Wound, ischemia, and foot infection (WIFI) classification system correlates with cost of care for diabetic foot ulcers treated in a multidisciplinary setting. Journal of Vascular Surgery 2018, 67, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Usman, Y.; Bakari, A.; Abdullahi, I.N.; Ahmad, A.; Sani-Bello, F.; Sagay, A.; Olayinka, A.T. Phenotypic profile and antibiogram of biofilm-producing bacteria isolates from diabetic foot ulcers in Zaria, Nigeria. Niger Postgrad Med J. 2021, 28, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Sasikumar, K.; Vijayakumar, C.; Jagdish, S.; Kadambari, D.; Kumar, N.R.; Biswas, R.; Parija, S.C. Clinico-microbiological profile of septic diabetic foot with special reference to anaerobic infection. Cureus. 2018, 10, e2252. [Google Scholar] [CrossRef]
- Macdonald, K.E.; Boeckh, S.; Stacey, H.J.; Jones, J.D. The microbiology of diabetic foot infections: a meta-analysis. BMC Infect Dise. 2021, 21, 770. [Google Scholar] [CrossRef]
- Shobo, C.O.; Essack, S.Y.; Bester, L.A. Enterococcal contamination of hospital environment in Kwazulu-Natal South Africa. J Appl Microbiol. 2022, 132, 654–664. [Google Scholar] [CrossRef]
- Garcia-Solache, M.; Rice, L.B. The enterococcus: a Model of Adaptability to Its Environment. Clin Microbiol Rev. 2019, 32, e00058. [Google Scholar] [CrossRef]
- Osei Sekyere, J.; Mensah, E. Molecular epidemiology and mechanisms of antibiotic resistance inenterococcus spp., staphylococcus spp., and streptococcus spp. in Africa: A systematic review from a one health perspective. Annals of the New York Academy of Sciences 2019, 1465, 29–58. [Google Scholar] [CrossRef]
- Serra, R.; Grande, R.; Butrico, L.; Rossi, A.; Settimio, U.F.; Amato, B.; et al. Chronic wound infections: the role of pseudomonas aeruginosa and staphylococcus aureus. Expert Rev Anti Infect Ther. 2015, 13, 605–13. [Google Scholar] [CrossRef]
- Darling, J.D.; McCallum, J.C.; Soden, P.A.; Guzman, R.J.; Wyers, M.C.; Hamdan, A.D.; Verhagen, H.J.; Schermerhorn, M.L. Predictive ability of the Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system after first-time lower extremity revascularization. J Vasc Surg. 2017, 65, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Cull, D.L.; Manos, G.; Hartley, M.C.; et al. An early validation of the Society for Vascular Surgery Lower Extremity Threatened Limb Classification System. J Vasc Surg. 2014, 60, 1535–41. [Google Scholar] [CrossRef] [PubMed]
- Darling, J.D.; McCallum, J.C.; Soden, P.A.; et al. Predictive ability of the Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system following infrapopliteal endovascular interventions for critical limb ischaemia. J Vasc Surg. 2016, 64, 616–22. [Google Scholar] [CrossRef] [PubMed]
- Snyder, R.J.; Bohn, G.; Hanft, J.; Harkless, L.; Kim, P.; Lavery, L.; Schultz, G.; Wolcott, R. Wound biofilm: Current perspectives and strategies on Biofilm disruption and treatment. Wounds. 2017, 29, S1–S17. [Google Scholar]
- Kollef, M.H.; Shorr, A.F.; Bassetti, M.; Timsit, J.-F.; Micek, S.T.; Michelson, A.P.; Garnacho-Montero, J. Timing of antibiotic therapy in the ICU. Critical Care 2021, 25. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).