1. Introduction
The liver play a significant role in drug metabolism. Scientific knowledges referring to the severity of liver cirrhosis, as a disease with a bad prognostic on the public health, is still not well characterized. [
1] Good to mention that in addition, in cirrhosis, liver fibrosis is a common fact, that can conduct into an irreversible process of cirrhosis with implications in developing of namely liver cancer. In recent years, there has been significant progress in basic and clinical research on liver cancer, leading to the identification of various signaling pathways involved in tumorigenesis and in disease progression.
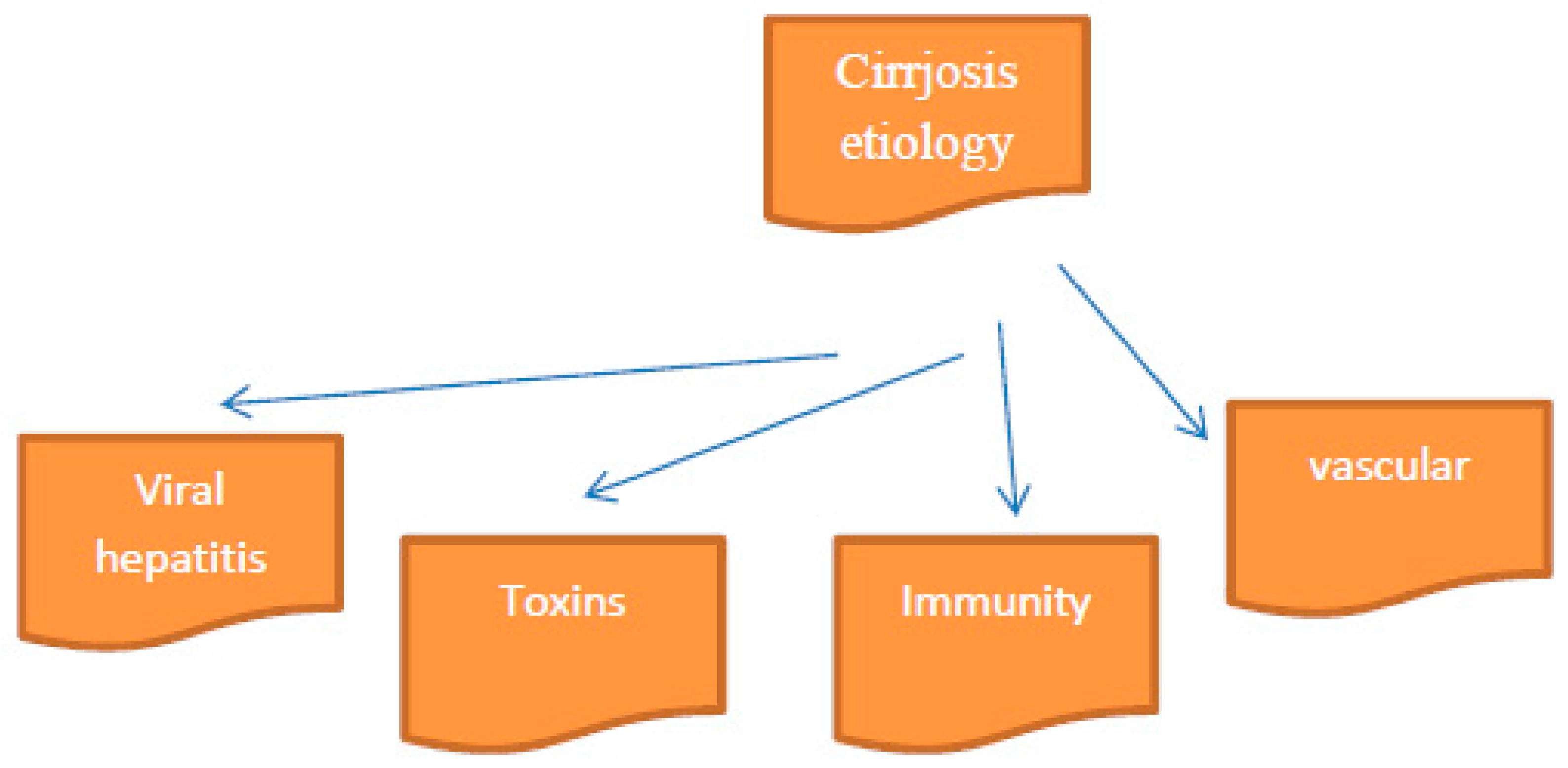
The signs and symptoms of patients diagnosed with cirrhosis, are promptly establish by medical specialists. Knowing the diagnostic in the ill patients, medical specialists could applay the proper treatment, carefully to the comorbidities.In idea that hepatic cirrhosis is hard or impossible to cure, we are waiting from future research dirrections and plans. [
Figure 1.]
Cytochrome P-450 (CYPs) is involved in the metabolism of drugs, chemicals and endogenous substrates. Hepatic CYPs also is involved in the pathogenesis of different liver diseases. Another specific point, good to mention, reffers to cytochrome P-450 (CYPs) and CYP-mediated activation of toxic drugs with their metabolites which induces hepatotoxicity. A strong relationship between the activity of CYPs and the severity of cirrhosis has been also demonstrated. More than, good to mention the usefulness of measuring CYP activity.[
2]
Liver diseases are associated with a decrease in hepatic drug elimination, but there is evidence that cirrhosis does not result in uniform changes of cytochrome P450 (CYP) isoenzymes. [
4,
5,
6] There are known that in research studies in liver pathologies, the prioritaire objectives were to determine the content and the activity of four CYP isoenzymes. Animal models play a significant role in liver pathology diagnosis. In rats with cirrhosis, CYP content was comparable with controls substrates.[
7,
8,
9] Studies results show that the content and the catalytic activity of individual CYP enzymes are differentially altered by cirrhosis in the rat and also suggest that drug probes could be useful to assess hepatic functional reserve.
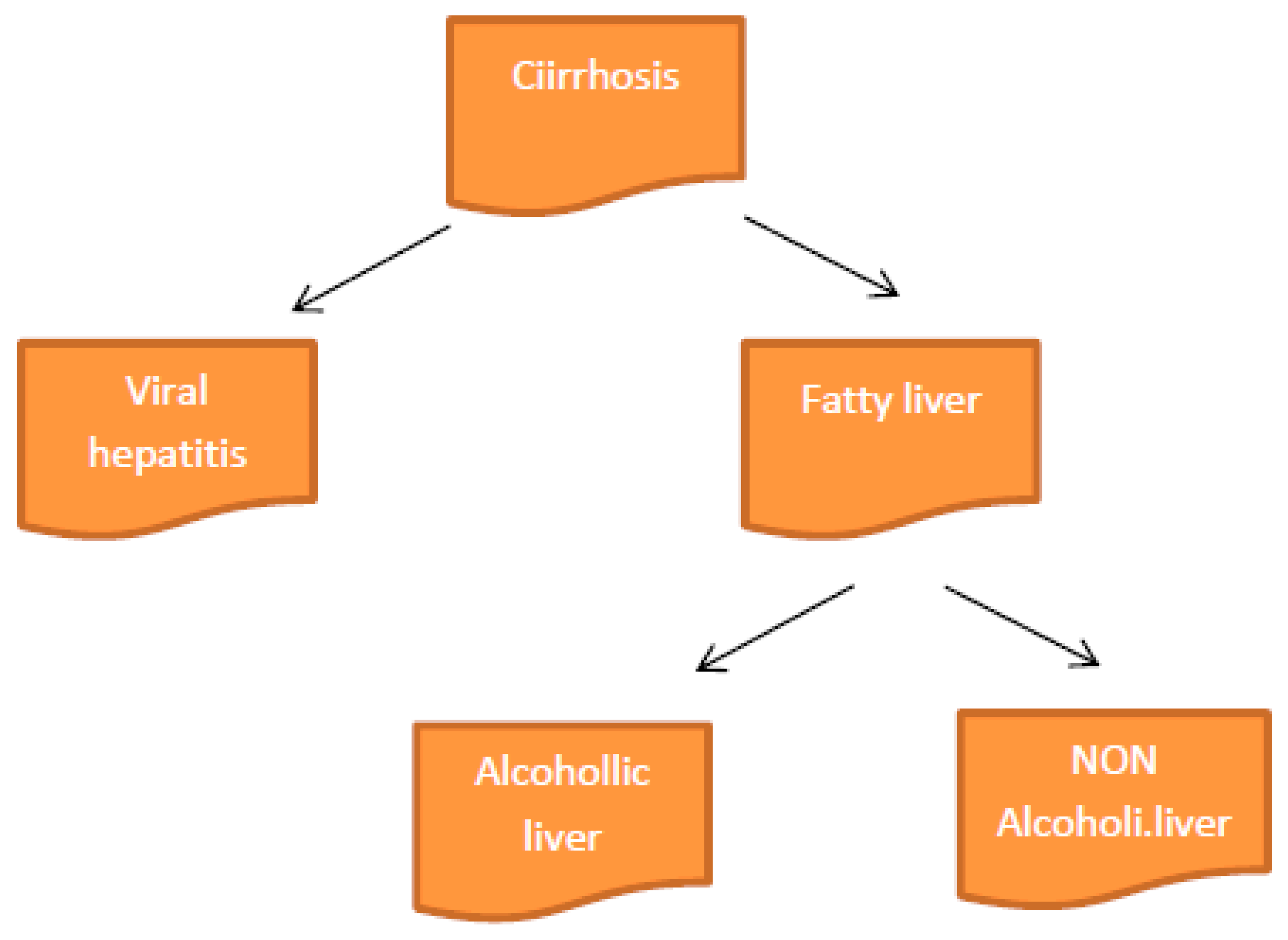
Taking in consideration the cause of cirrhosis could be possible a sub-classification as below.. [
Figure 2]
2. Cirrhosis and CYP Isoenzymes
Cirrhosis, as a nowadays disease, is characterized by fibrosis and neoformation noduls in the liver architecture. In addition, cirrhosis it is known as a chronic injury, which leads to alteration of the normal lobular organization of the liver. [
10,
11,
12] A complex of factors, such as life style, or environmental factors, can affect the liver, for better or for worse. [
13,
14] Finally, after a long term alterations in liver functionalitty, develop in time cirrhosis, as a complex diseases [
15,
16,
17] Ethiological key points of cirrhosis include autoimmune hepatitis, primary sclerosing cholangitis, alpha-1 antitrypsin deficiency, drug-induced liver cirrhosis, and chronic right-sided heart failure. [
15,
16,
17] The cause of morbidity and mortality in cirrhosis is the development of portal hypertension and hyperdynamic circulation. Portal hypertension develop secondary the fibrosis in hepatocytes and beside, vasoregulatory alterations. [
18,
19]
Liver fibrosis it is known as a stage with an excessive deposition of connective tissue proteins in annex gland structure. Interstitial collagens in the extracellular matrix of the liver has been discovered in this liver pathology. The long term stimuli involved in the initiation of fibrosis leads to oxidative stress. Next point that concure to disease, include mediators of molecular events involved in the pathogenesis of hepatic fibrosis. These processes lead to cellular injury and initiate inflammatory responses. As a response, cytokines and growth factors play a role as trigger activation and transformation of resting hepatic stellate cells into myofibroblast like cells. At the end of the ill liver pathologically process, could be observe an excessive synthesis of connective tissue proteins, including collagens. Uncontrolled and hepatocyte fibrosis results in distortion of lobular architecture of the liver. Pathologists show the nodular formations in the liver as a diagnosis of cirrhosis. Finally, develop hepatocellular carcinoma. In the pathogenesis of hepatic fibrosis, molecular mechanisms play a role. [
20,
21] This scientifically team, include a pathologist, a gastroenterologist, a liver surgeon and additionally specialists. Therapy methods and drugs, are more important, including antiviral medications in viral hepatitis, steroids, and immunosuppressant agents in autoimmune hepatitis.[
22,
23,
24] Diferential diagnostic in liver pathology as cirrhosis, include research directions reffering to various medical fields with implication in this way. For monitorisation of liver disease, abdominal ultrasonography is useful. [
25,
26] Liver transplantation (LT) is also an effective therapeutic option for the management of cirrhosis end-stage.[
Figure 3]
3. Trends in Cirrhosis Diagnosis
Telemedicine is a terminology encompassing several different practices including teleconsultation (imparting specialist knowledge to another practitioner through case presentation); telemonitoring (adopting technology such as wearables to remotely monitor signs and symptoms), and televisits (where patients can be assessed by a healthcare provider in a remote location). [
27]
The use of machine learning algorithms and potential artificial intelligence are also gaining momentum, although their application in decompensated cirrhosis is limited.[
28]
An estimated 1.5 billion people worldwide have chronic liver disease, with a marked 13% increase in cirrhosis cases noted in the last decade. [
29]
This translates into increased cirrhosis-associated morbidity, especially from acute decompensation events, and mortality. Whilst our understanding of the pathophysiological drivers of acute decompensation of cirrhosis has improved considerably over the last decade, the management still remains largely reactive, often necessitating intensive therapies and protracted hospital admissions in response to late presentations.[
30]
Complications accompanying hepatic cirrhosis are various and include, portal hypertension, edema in the abdomen and lower extremities, splenomegaly, infections, hepatic encephalopathy. For a medical team is a key point to investigate and to try to ameliorate cirrhosis comorbidities signs and simptoms.It is not easy but are differents medical methods in this direction.
Moreover, even after resolution of an acute decompensation event, re-admission to hospital with further complications is common, with 90-day readmission rates estimated at between 21–53%, based on the population and number of cirrhosis complications.[
31,
32]
Those with more advanced disease, prior encephalopathy and/or those who have previously received prophylactic antibiotics, have higher readmission rates, generating a substantial health and societal care cost.
In addition to optimal management of cirrhosis complications per the recent EASL guidelines,
patients with advanced liver disease also require support and management for substance/alcohol abuse, nutrition and frailty.[
33,
34]
This in turn requires a programme of education for patients and carers alike, following discharge from hospital back into the community. In this regard, the delivery of current management protocols is often wanton in ensuring adequate and equitable access to specialist advice, timely follow-up, and sufficient community support, following hospital discharge. This in an era when many other chronic disease management protocols, such as for heart failure, have turned to technology to help improve outcomes and patient engagement. This begs the question, what could aide early recognition of new cirrhosis complications and be used to provide effective community cirrhosis monitoring and management for patients at risk of decompensation.
4. Complications in Cirrhosis
Hepatic encephalopathy (HE) is an important major neuropsychiatric disorder in liver cirrhosis. There are known two types. So minimal hepatic encephalopathy (MHE), known as a cognitive deficit found in the ealier past time using specific psychological tests and Grade I HE. More than, also it is known about overt hepatic encephalopathy (OHE), with specific clinical symptoms.[
35,
36]
Ascites is knowing as a common complication in hepatic cirrhosis. Ascites is accompanied with portal hypertension. This previously mentioned complication in cirrhosis, it is known as a specific one, defined as an accumulation of a fluid quantity in the peritoneal cavity.[
37]
Ascites infection is a possible accompaning event for ill persons diagnosed with cirrhosis. Infection in ascitis is often known as a bacterial peritonitis (SBP) somethimes with accompaning fungal infections.[
38].[
39]
Variceal bleeding represent a relatively comon accompanied complication to patients diagnosed with cirrhosis. [
40] In liver damage as cirrhosis, esophageal and gastric variceal bleeding together with rectal variceal bleeding.[
41]
Hepatorenal syndrome and kidney injury represent a common complication to patients diagnosed with hepatic cirrhosis. [
42]
Infections are also relatively commons in hepatic cirrhosis. In differents parts of the body could be find after signs and simpotoms, infections as tissues infections,bacteremia, pneumonia, urinary tract infections. [
43,
44] From years ago,till nowadays,
infections caused by multidrug-resistant organisms (MDRO) play a significant role in liver damages such them from hepatic cirrhosis.[
45]
5. Paraclinic Key Points in Cirrhosis Diagnosis
In negative progression of liver pathology, into cirrhosis, it is know about AST/ALT ratio. As plaboratorytests for diagnostic in cirrhosis, are important results for alkaline phosphatase (ALP), 5'- nucleotidase, and gamma-glutamyl transferase (GGT). AST/ALT ratio in differents forms of chronic hepatitis with exception of alcoholic hepatitis, is less than 1. Laboratory results show us that in chronic hepatitis which conduct to cirrhosis, there is a reversal of this AST/ALT ratio. Another laboratory test namely alkaline phosphatase (ALP), 5'- nucleotidase, and gamma-glutamyl transferase (GGT) are important for diagnostic in liver pathology. [
46] More than, results from specific tests such as aminotransferase; aspartate aminotransferase (AST); alanine aminotransferase (ALT);play a great role in . cirrhosis diagnostic and in diferential diagnostic., [
47] Gamma fraction from immunoglobulins, is also good to mention in liver pathology diagnostic. [
48]
There are known about new specific laboratory tests performing for cirrhosis diagnostic. So, serology and genetical tests such as PCR technique and autoimmune antibodies including anti-nuclear antibodies (ANA) and anti-smooth muscle antibodies (ASMA), anti-liver-kidney microsomal antibodies type 1 (ALKM-1).. Ferritin and transferrin saturation for hemochromatosis, ceruloplasmin, Alpha 1-antitrypsin level, and protease inhibitor phenotype for alpha 1-antitrypsin deficiency, pley a great point in diagnostic of cirrhosis.
Imagistical methods including ultrasound, CT, MRI, and transient elastography compose a specific part in the paraclinic diagnostic of cirrhosis Ultrasonography is a easier, faster and method for descovering demages in the liver structure.With this method, is possible to detect specific nodularity and beside also an increased echogenicity in liver structure.. [
49] Aas a great curently imagistical method, MRI can also be used for detection liver alterations. For example, with MRI coud be possible to detect specific fat deposits in the liver consisit of hemochromatosis, steatosis, and possible others . [
50,
51]
6. Conclusions
Patient lifestyle changes, unfortunately cannot cure cirrhosis. Lifestyle changes, and a proper diet, conduct to amelioration of diseases simptoms. Regulate protein intake according to specialised doctor's indications and some medical recommandations, will be proper in the treatment of cirrhosis. Relatively recently research investigations try to elucidate the signal transduction pathways that link hepatocytes alterations including cellular disfunctionality. For next coming period of time, hope to find and apply educational programs in order to induce alcoholic persons to renounce to this dangerous consumtions witch play a role in liver damages with cirrhosis instalation.
References
- Kleinbloesem CH, van Harten J, Wilson JP, Danhof M, van Brummelen P, Breimer DD. Nifedipine: kinetics and hemodynamic effects in patients with liver cirrhosis after intravenous and oral administration. Clin Pharmacol Ther. 1986;40:21–8. [CrossRef]
- Morgan DJ, McLean AJ. Clinical pharmacokinetic and pharmacodynamic considerations in patients with liver disease. An update. Clin Pharmacokinet. 1995;29:370–91. [CrossRef]
- Lamba JK, Lin YS, Schuetz EG, Thummel KE. Genetic contribution to variable human CYP3A-mediated metabolism. Advanced Drug Delivery Reviews. 2002;54:1271–94. [CrossRef]
- George J, Liddle C, Murray M, Byth K, Farrell GC. Pre-translational regulation of cytochrome P450 genes is responsible for disease-specific changes of individual P450 enzymes among patients with cirrhosis. Biochem Pharmacol. 1995;49:873–81. [CrossRef]
- Guengerich FP, Turvy CG. Comparison of levels of several human microsomal cytochrome P-450 enzymes and epoxide hydrolase in normal and disease states using immunochemical analysis of surgical liver samples. J Pharmacol Exp Ther. 1991;256:1189–94.
- Lown K, Kolars J, Turgeon K, Merion R, Wrighton SA, Watkins PB. The erythromycin breath test selectively measures P450IIIA in patients with severe liver disease. Clin Pharmacol Ther. 1992;51:229–38. [CrossRef]
- Kleinbloesem CH, van Brummelen P, Faber H, Danhof M, Vermeulen NP, Breimer DD. Variability in nifedipine pharmacokinetics and dynamics: a new oxidation polymorphism in man. Biochem Pharmacol. 1984 Nov 15;33(22):3721–3724. [CrossRef]
- Kleinbloesem CH, Van Harten J, Van Brummelen P, Breimer DD. Liquid chromatographic determination of nifedipine in plasma and of its main metabolite in urine. J Chromatogr. 1984 Jun 8;308:209–216. [CrossRef]
- van Harten J, van Brummelen P, Wilson JH, Lodewijks MT, Breimer DD. Nisoldipine: kinetics and effects on blood pressure and heart rate in patients with liver cirrhosis after intravenous and oral administration. Eur J Clin Pharmacol. 1988;34:387–94. [CrossRef]
- Bircher J, Benhamou JP, McIntyre N, Rizzetto M, Rodes J, editors. Oxford Textbook of Clinical Hepatology. 2nd Edition Oxford University Press; 1999.
- Sherlock S, Dooley J, editors. Diseases of the Liver and Biliary System. 11th Edition Blackwell Science; Oxford, UK; Malden, MA: 2002.
- Schiff ER, Sorrell MF, Maddrey EC, editors. Schiff’s Diseases of the Liver. 9th Edition Lippincott, Williams & Wilkins; Philadelphia: 2003.
- Desmet VJ, Roskams T. Cirrhosis reversal: a duel between dogma and myth. J Hepatol. 2004;40:860–7. [CrossRef]
- Wanless IR, Nakashima E, Sherman M. Regression of human cirrhosis. Morphologic features and the genesis of incomplete septal cirrhosis. Arch Pathol Lab Med. 2000;124:1599–607. [CrossRef]
- Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825–32. [CrossRef]
- Bellentani S, Pozzato G, Saccoccio G, et al. Clinical course and risk factors of hepatitis C virus related liver disease in the general population: report from the Dionysos study. Gut. 1999;44:874–80. [CrossRef]
- Bellentani S, Saccoccio G, Costa G, et al.The Dionysos Study Group Drinking habits as cofactors of risk for alcohol induced liver damage. Gut. 1997;41:845–50. [CrossRef]
- Fracanzani AL, Fargion S, Romano R, et al. Portal hypertension and iron depletion in patients with genetic hemochromatosis. Hepatology. 1995;22:1127–31. [CrossRef]
- Conn H, Atterbury C. Cirrhosis. In: Schiff L, Schiff E, editors. Diseases of the Liver. 7th edition Lippencott Company, Philadelphia; Philadelphia: 1993. pp. 875–934.
- Dienstag JL, Goldin RD, Heathcote EJ, et al. Histological outcome during long-term lamivudine therapy. Gastroenterology. 2003;124:105–17. [CrossRef]
- Everson GT. Management of cirrhosis due to chronic hepatitis C. J Hepatol. 2005;42(Suppl1):S65–74. [CrossRef]
- Lok AS, McMahon BJ. Practice Guidelines Committee, American Association for the Study of Liver Diseases (AASLD). Chronic hepatitis B: update of recommendations. Hepatology. 2004;39:857–61. 23. [CrossRef]
- Van Thiel DH, Gavaler JS, Schade RR. Liver disease and the hypothalamic pituitary gonadal axis. Semin Liver Dis. 1985;5:35–45. 24. [CrossRef]
- Tangerman A, Meuwese-Arends MT, Jansen JB. Cause and composition of foetor hepaticus. Lancet. 1994;343:483. [CrossRef]
- Di Lelio A, Cestari C, Lomazzi A, Beretta L. Cirrhosis: Diagnosis with sonographic study of the liver surface. Radiology. 1989;172:389–92. [CrossRef]
- Tchelepi H, Ralls PW, Radin R, Grant E. Sonography of diffuse liver disease. J Ultrasound Med. 2002;21:1023–32. [CrossRef]
- Jansen C., Chatterjee D.A., Thomsen K.L.Al-Kassou B., Sawhney R., Jones H., et al., Significant reduction in heart rate variability is a feature of acute decompensation of cirrhosis and predicts 90-day mortality. Aliment Pharmacol Ther. 2019; 50: 568-579. [CrossRef]
- Moreau R., Jalan R., Gines P., Pavesi M., Angeli P., Cordoba J., et al., Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis.Gastroenterology. 2013; 144 (37 e1-9): 1426-1437. [CrossRef]
- Moon A.M., Singal A.G., Tapper E.B., Contemporary epidemiology of chronic liver disease and cirrhosis.Clin Gastroenterol Hepatol. 2020; 18: 2650-2666. [CrossRef]
- Trebicka J., Fernandez J., Papp M., Caraceni P., Laleman W., Gambino C., et al. The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J Hepatol. 2020; 73: 842-854. [CrossRef]
- Tapper E.B., Halbert B., Mellinger J., Rates of and reasons for hospital readmissions in patients with cirrhosis: a multistate population-based cohort study. Clin Gastroenterol Hepatol. 2016; 14: 1181-8 e2. [CrossRef]
- Bajaj J.S., Reddy K.R., Tandon P., Wong F., Kamath P.S., Garcia-Tsao G. et al. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016; 64: 200-208. [CrossRef]
- European Association for the Study of the Liver EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. Hepatol. 2018; 69: 406-460. [CrossRef]
- Macdonald S., Jepsen P., Alrubaiy L., Watson H., Vilstrup H., Jalan R., Quality of life measures predict mortality in patients with cirrhosis and severe ascites. Aliment Pharmacol Ther. 2019; 49: 321-330. [CrossRef]
- Häussinger D, Dhiman RK, Felipo V, Görg B, Jalan R, Kircheis G, Merli M, Montagnese S, Romero-Gomez M, Schnitzler A, Taylor-Robinson SD, Vilstrup H. Hepatic encephalopathy. Nat Rev Dis Primers. 2022;8:43. [CrossRef]
- Ridola L, Faccioli J, Nardelli S, Gioia S, Riggio O. Hepatic Encephalopathy: Diagnosis and Management. J Transl Int Med. 2020;8:210–219. [CrossRef]
- European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397–417. [CrossRef]
- Gravito-Soares M, Gravito-Soares E, Lopes S, Ribeiro G, Figueiredo P. Spontaneous fungal peritonitis: a rare but severe complication of liver cirrhosis. Eur J Gastroenterol Hepatol. 2017;29:1010–1016. [CrossRef]
- Fiore M, Chiodini P, Pota V, Sansone P, Passavanti MB, Leone S, Aurilio C, Pace MC. Risk of spontaneous fungal peritonitis in hospitalized cirrhotic patients with ascites: a systematic review of observational studies and meta-analysis. Minerva Anestesiol. 2017;83:1309–1316. [CrossRef]
- Alqahtani SA, Jang S. Pathophysiology and Management of Variceal Bleeding. Drugs. 2021;81:647–667. Baiges. [CrossRef]
- A, Hernández-Gea V. Management of Liver Decompensation in Advanced Chronic Liver Disease: Ascites, Hyponatremia, and Gastroesophageal Variceal Bleeding. Clin Drug Investig. 2022;42:25–31. [CrossRef]
- Molleston JP, Bennett WE Jr. Mortality, Risk Factors and Disparities Associated with Esophageal Variceal Bleeding in Children's Hospitals in the US. J Pediatr. 2021;232:176–182. [CrossRef]
- Van der Merwe S, Chokshi S, Bernsmeier C, Albillos A. The multifactorial mechanisms of bacterial infection in decompensated cirrhosis. J Hepatol. 2021;75 Suppl 1:S82–S100. [CrossRef]
- udry N, Sasso R, Rockey DC. Infection in Hospitalized Cirrhosis Patients: Changing Epidemiology and Clinical Features. Am J Med Sci. 2022;363:114–121. [CrossRef]
- Fernández J, Piano S, Bartoletti M, Wey EQ. Management of bacterial and fungal infections in cirrhosis: The MDRO challenge. J Hepatol. 2021;75 Suppl 1:S101–S117. [CrossRef]
- Ballard HS. The hematological complications of alcoholism. Alcohol Health Res World. 1997;21(1):42-52.
- Ellis G, Goldberg DM, Spooner RJ, Ward AM. Serum enzyme tests in diseases of the liver and biliary tree. Am J Clin Pathol. 1978 Aug;70(2):248-5. [CrossRef]
- Tanaka S, Okamoto Y, Yamazaki M, Mitani N, Nakqjima Y, Fukui H. Significance of hyperglobulinemia in severe chronic liver diseases--with special reference to the correlation between serum globulin/IgG level and ICG clearance. Hepatogastroenterology. 2007 Dec;54(80):2301-5.
- Tchelepi H, Ralls PW, Radin R, Grant E. Sonography of diffuse liver disease. J Ultrasound Med. 2002 Sep;21(9):1023-32; quiz 1033-4. [CrossRef]
- Regev A, Berho M, Jeffers LJ, Milikowski C, Molina EG, Pyrsopoulos NT, Feng ZZ, Reddy KR, Schiff ER. Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection. Am J Gastroenterol. 2002 Oct;97(10):2614-8. [CrossRef]
- Halfon P, Munteanu M, Poynard T. FibroTest-ActiTest as a non-invasive marker of liver fibrosis. Gastroenterol Clin Biol. 2008 Sep;32(6 Suppl 1):22-39. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).