1. Introduction
Subtrochanteric hip fractures account for 5-34% of proximal femoral fractures [
1]. The reported nonunion rate of these fractures is about 4-20% [
2,
3,
4,
5].
The subtrochanteric area of the proximal femur is located between the lesser trochanter of the femur and 5 cm below it [
6]. It is formed of thick cortical bone with a tenacious blood supply. The subtrochanteric area is the highest stressed zone in the human skeleton; the cantilever anatomy of the proximal femur creates an unequal distribution of stresses at proximal femur with the medial cortex exposed to compression stress 20% more than the tensile stress acting on the lateral cortex, creating varus bending stress on any fixation device with impending failure if bone healing does not go in the expected timely manner[
4].
The common treatment for subtrochanteric fractures is intramedullary nailing[
6]. Due to the anatomy of the region, it is common not to reduce them appropriately, leaving the proximal femur in varus[
7]. This increases greatly the varus bending stress applied, leading to nonunion and nail breakage[
7].
Nonunion is believed to occur mainly due to the high deforming forces in this region[
8]. Varus malalignment is considered a key points that lead to nonunion[
7]. To prevent this situation it has been recently remarked that a medial entry point when nailing subtrochanteric hip fractures is of paramount importance, to avoid varus[
9].
Other factors involved in nonunion in this area are residual displacement (gaps between bone ends) and poor vascularization[
7].
Current treatment of subtrochanteric nonunions is operative [
1]. Commonly used methods are based on correct reduction (avoiding varus) and new fixation with an intramedullary (cephalomedullary nail) or extramedullary device (plates)[
1]. Arthroplasty is considered only a salvage procedure when new fixation is impossible to perform[
1]. Recent reports indicate similar results after new osteosynthesis versus arthroplasty for patients older than 50 y.o.[
10]. Bone grafting[
11], Teriparatide[
12], and recombinant human bone morphogenetic protein (BMP)[
13] have been also used to aid the fixation, with promising results.
Nail fixation, with over-reaming of the canal, is the most commonly used technique, with an overall union rate of 98%[
1,
14]. Nevertheless, it is difficult to achieve a good correction, and shortening is a common problem [
1]. The combination of an external fixation or traction may solve this problem, but requires a long time and several interventions [
1].
Extramedullary fixation, after osteotomy and correction of deformity, is another approach to the problem. Fixed angle devices are the more commonly used (Condylar blade plates, condylar locking plates, 95º dynamic condylar screw plates, and so on), but recent reports indicate a failure rate with non-dynamic blade plates, of up to 29%[
15]. Most authors also use bone grafts to enhance healing[
5,
16], and an osteotomy to correct deformity[
1,
16]. Overall union rate is reported around 71-98% [
1,
5,
15,
16].
On the other hand, for nonunion of femoral neck fractures (between the head and the trochanteric area), the valgus trochanteric osteotomy is a well-known procedure that has achieved good results for decades and is now starting to be used for trochanteric nonunions [
17,
18]. It changes the forces in the nonunion site from shearing to compression. The nonunion site is not disturbed, no bone graft is needed, and union is usually achieved quickly. To date, no one has applied this principle to subtrochanteric nonunions.
So, for subtrochanteric nonunions, a dynamic valgus correction at the nonunion site (without osteotomy), fixed dynamically with an extramedullary device (dynamic hip screw), was developed, to enhance healing without graft, restore length, and initiate weight bearing immediately.
The objective of this paper is to show the surgical technique and results with the first three patients.
2. Materials and Methods
The objective of surgical technique is threefold: a) to get a valgus correction of the proximal fragment, to overcorrect to 150 degrees valgus; b) to get dynamic compression at the nonunion site; c) not to damage bone vascularization by adding osteotomies, but achieving the correction only by decompaction of the nonunion site.
Surgery is performed on a traction table, preoperative cefazolin (2 gr), and standard skin preparation is done as usual.
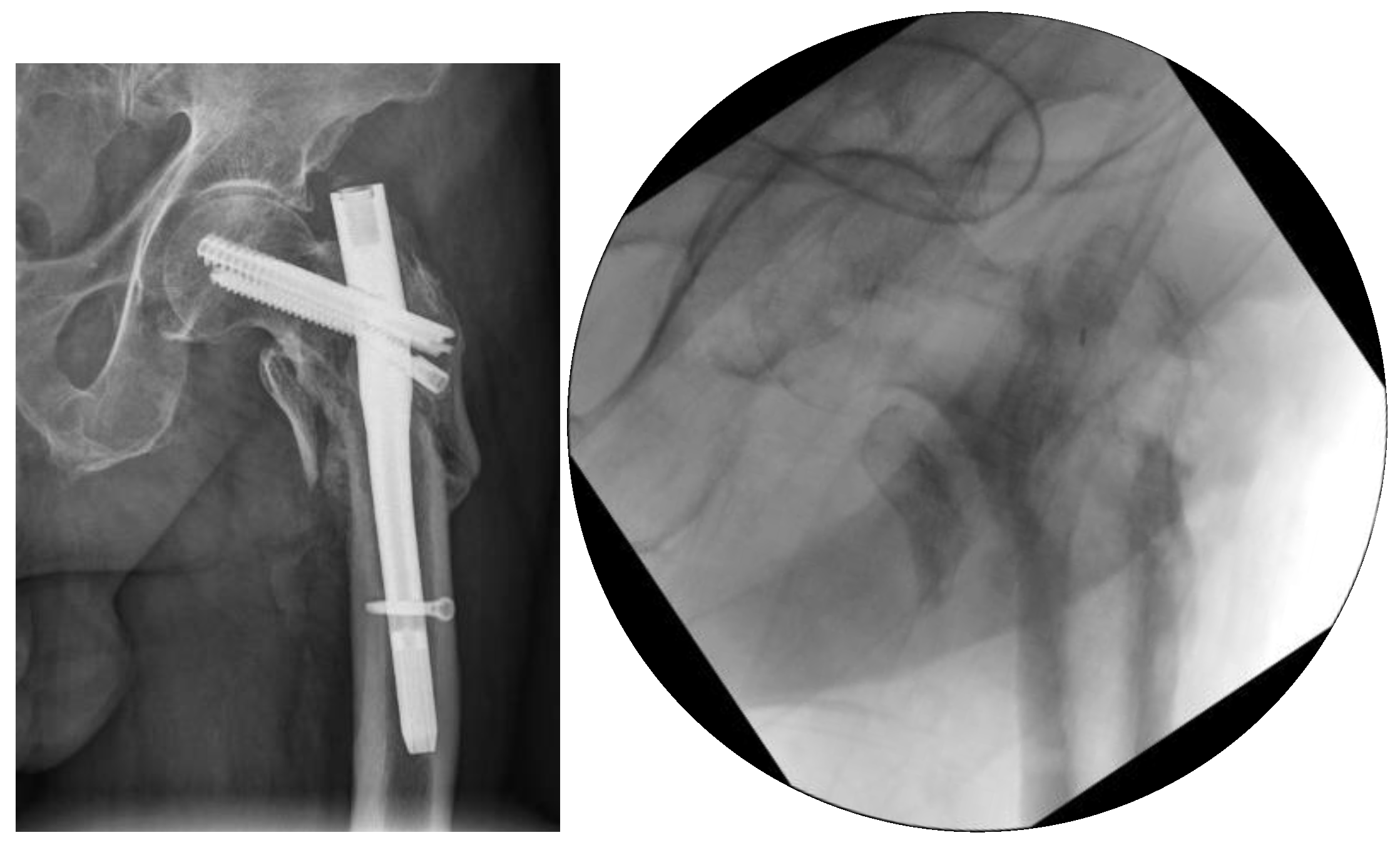
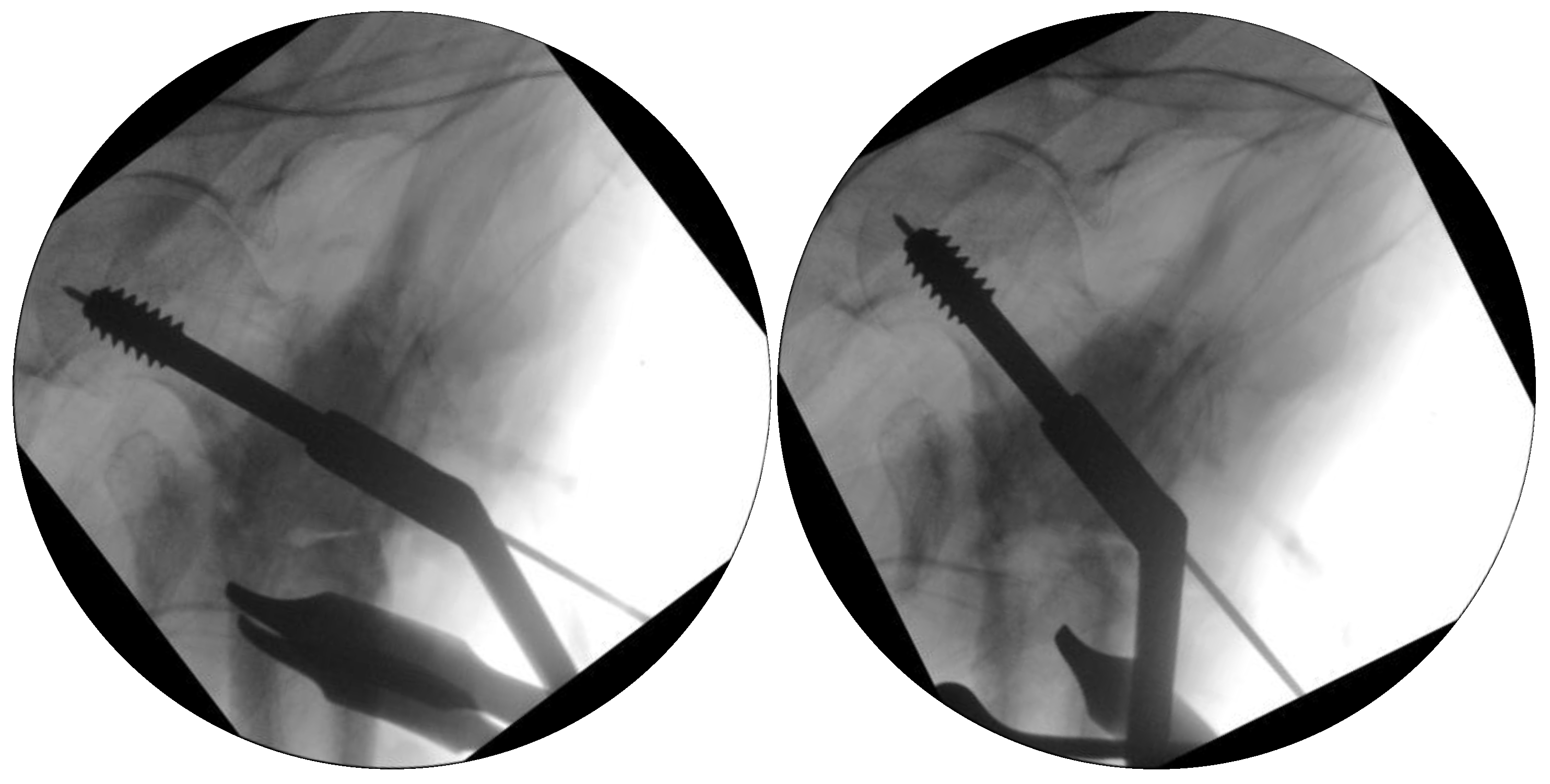
The first step is to withdraw the previous material (i.e. broken nail) with standard methods (
Figure 1)
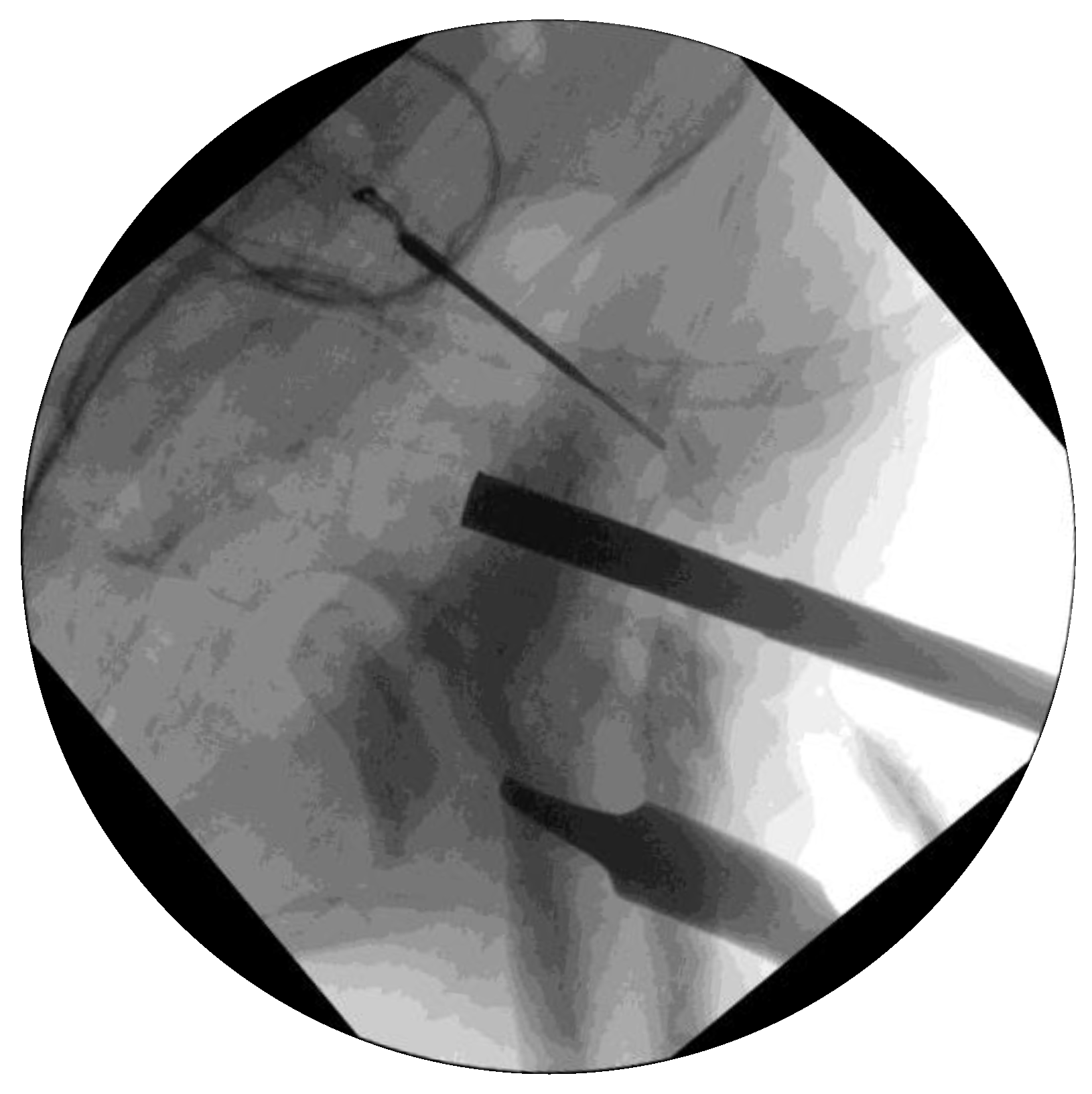
After that, a standard lateral approach is performed, through the skin, fascia lata, and subvastus approach (
Figure 2)
The third step is to take three samples of nonunion site for microbiological study, to discard infection.
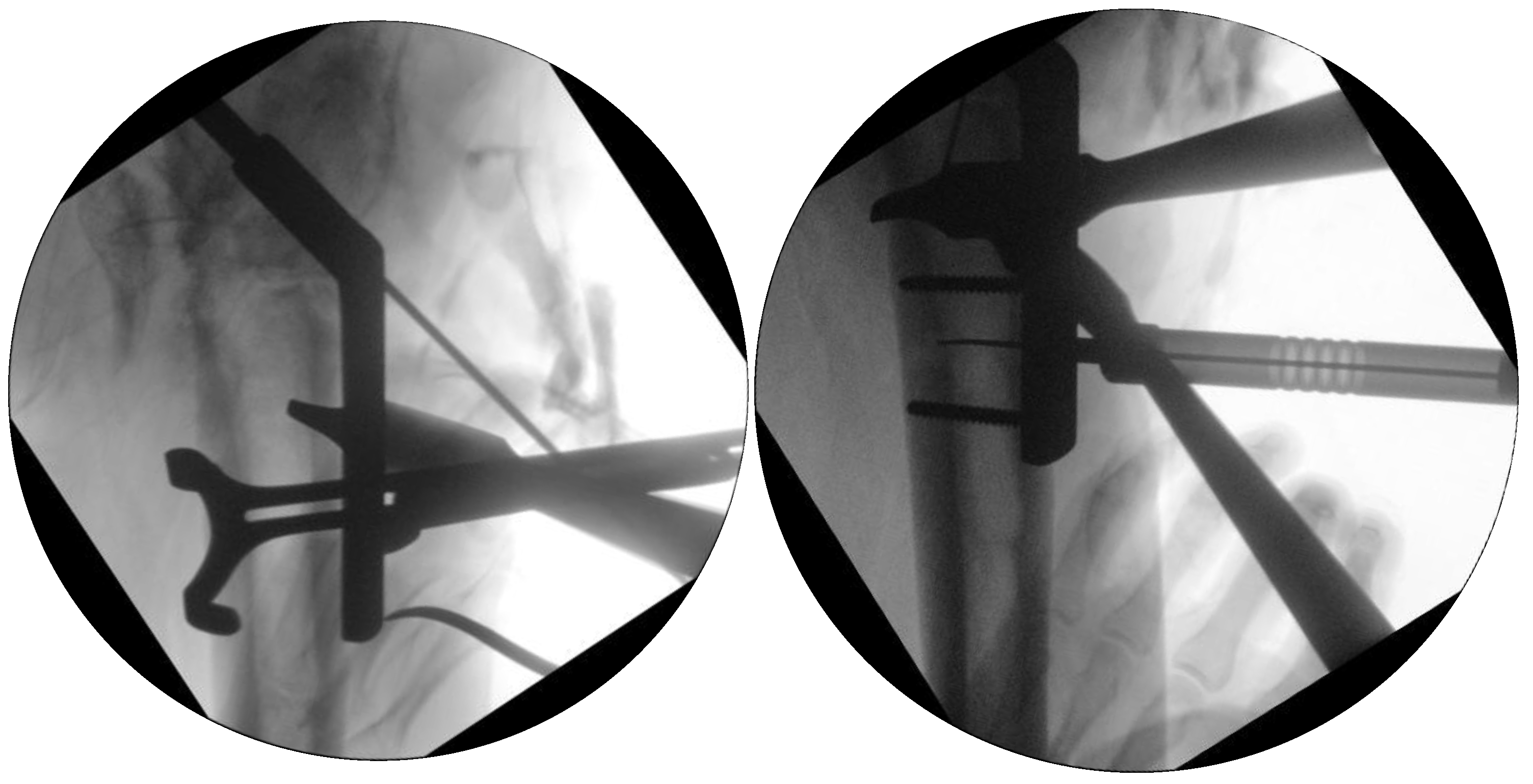
The fourth step is to fill the void in the head due to previous fixation material, with an allogenic bone graft (40gr spongiosa bone from the tissue bank). Impacted into the head (
Figure 3).
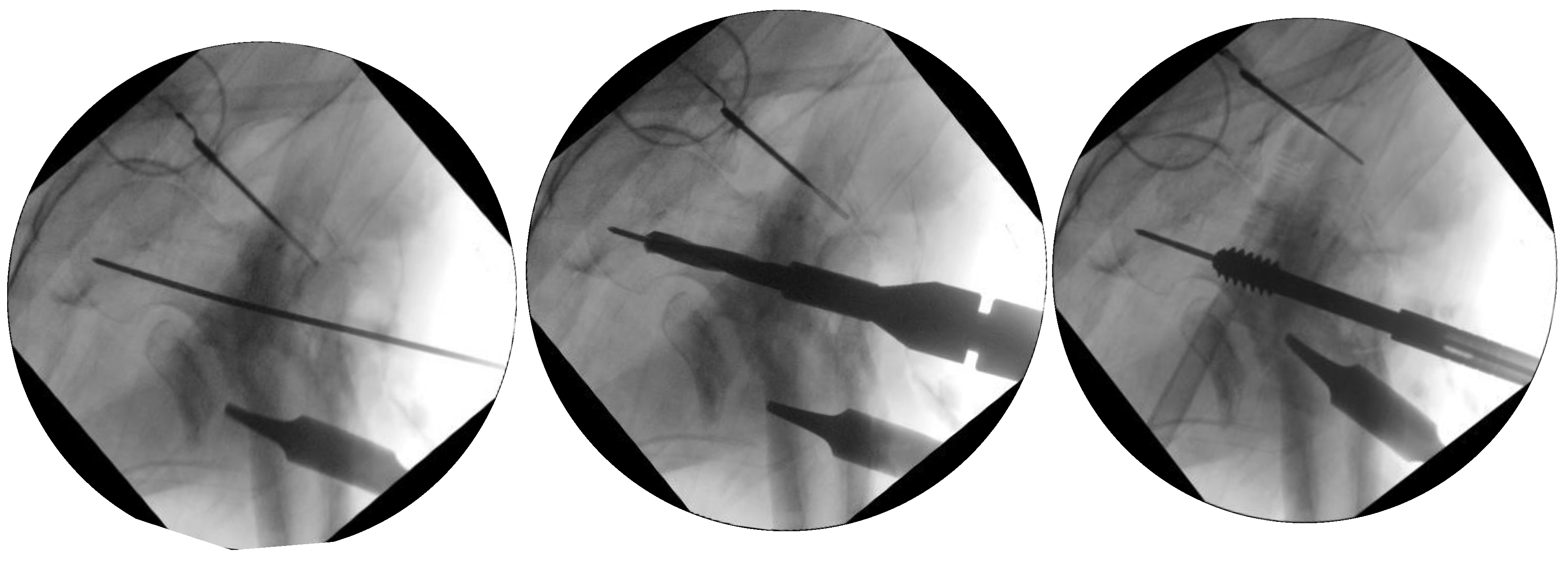
Next, measurements are done to get 150 degrees of valgus to the femoral neck. In this case, a 135-degree DHS implant is to be used, so, as 110 degrees is now found at the neck, the guide wire for the head screw is to be inserted in 15 degrees of varus related to the neck (to achieve a final valgus of 135 + 15 = 150 degrees). 135 degrees DHS is preferred, as in this plate, head screw purchase low and through intact bone
Figure 4
After that, decompaction of the nonunion site is performed. It is paramount not to damage vascularization at this site, trying to be as minimally invasive as possible. A Chisel is inserted through the nonunion site for the decompaction of both bone ends. It is quite important to open the medial site to aid in later valgus correction (
Figure 5). No bone graft is added to the nonunion site.
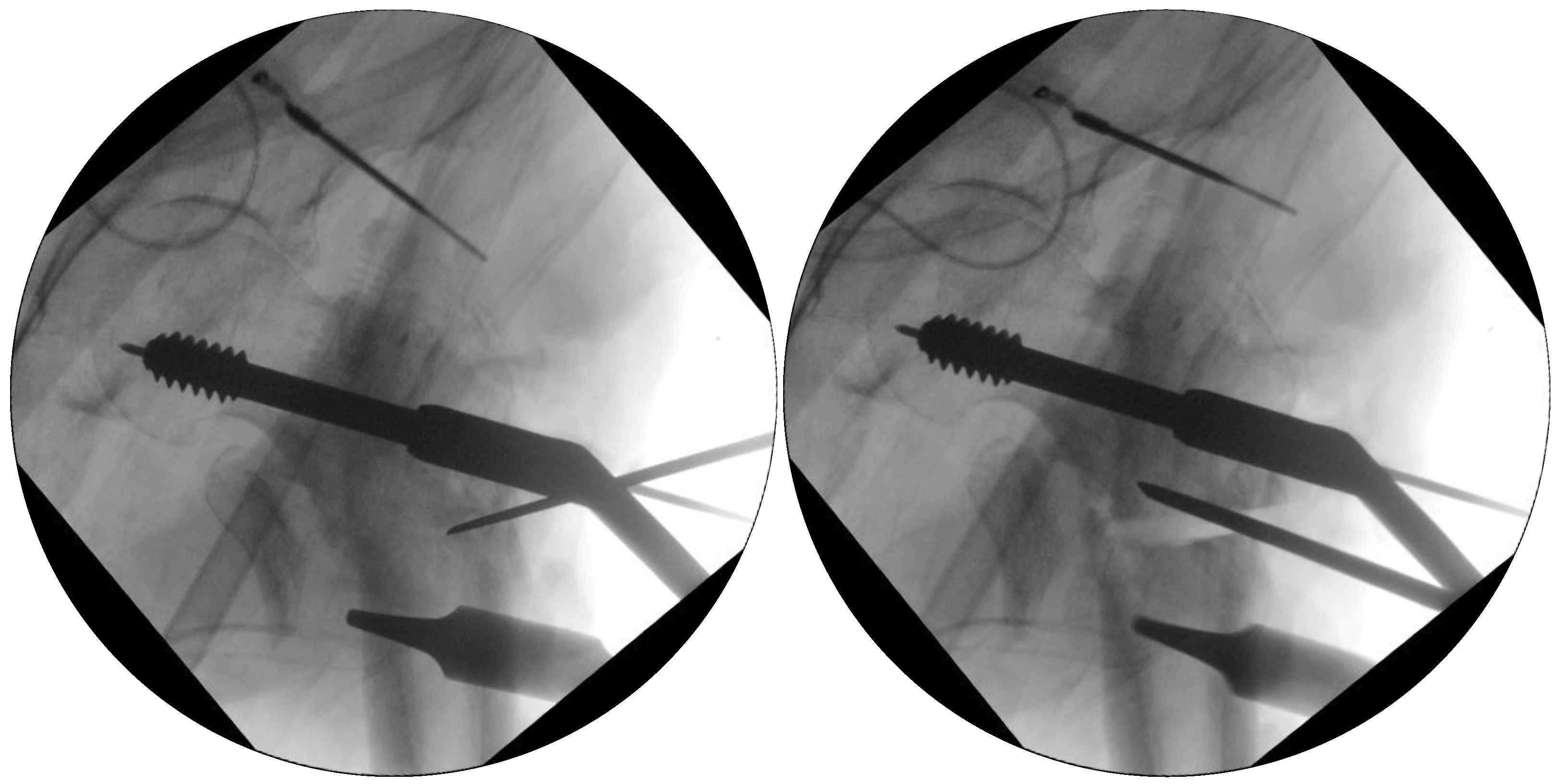
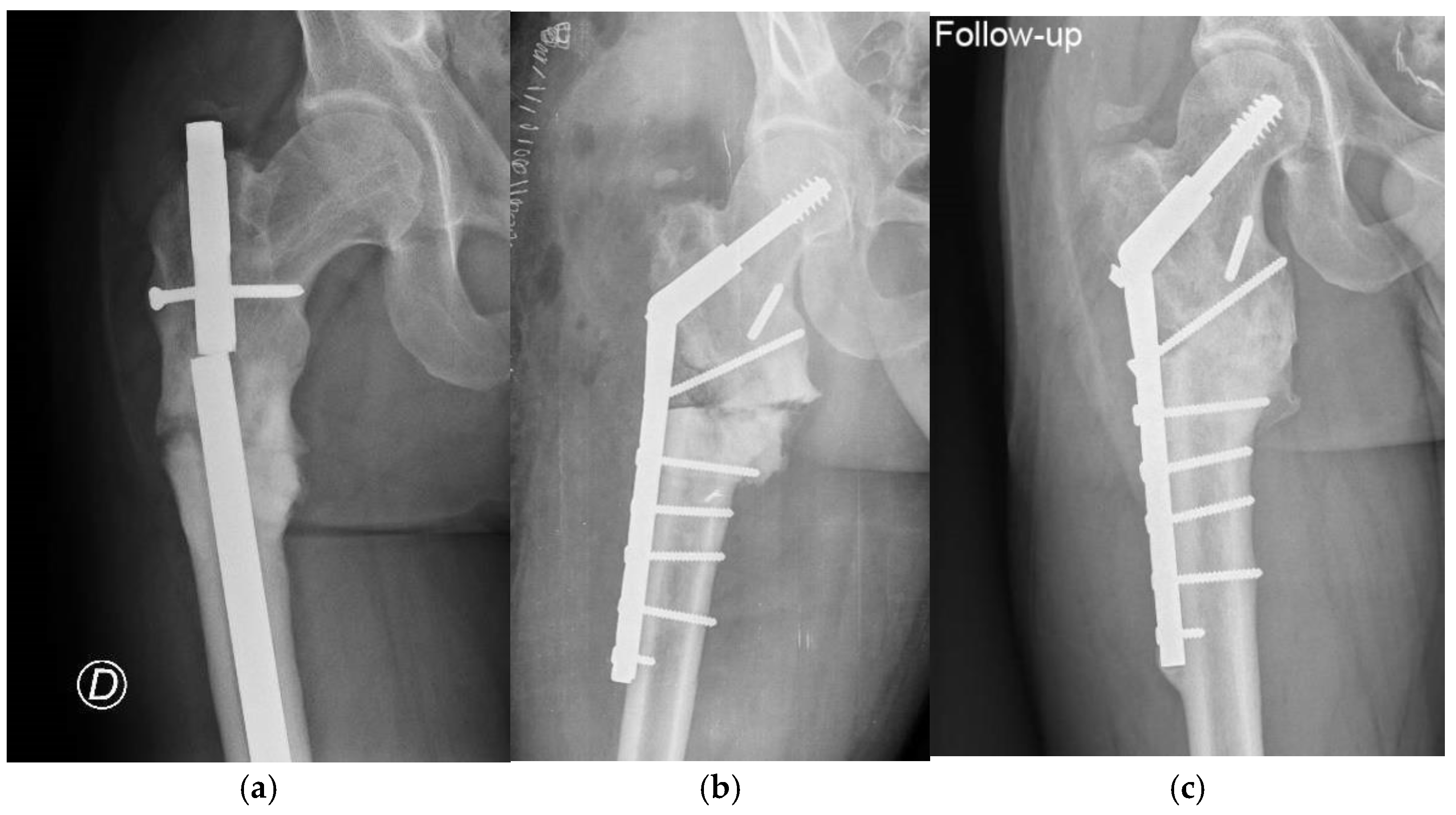
Finally, reduction is achieved by introducing the plate and joining it to the femoral shaft. Care should be taken to make this slowly and progressively, to avoid intraoperative cut-out (
Figure 6)
Finally, screws are applied to the plate (
Figure 7), and the wound is routinely closed.
The patient is allowed full weight bearing from the first day after correction is checked (
Figure 8)
3. Results
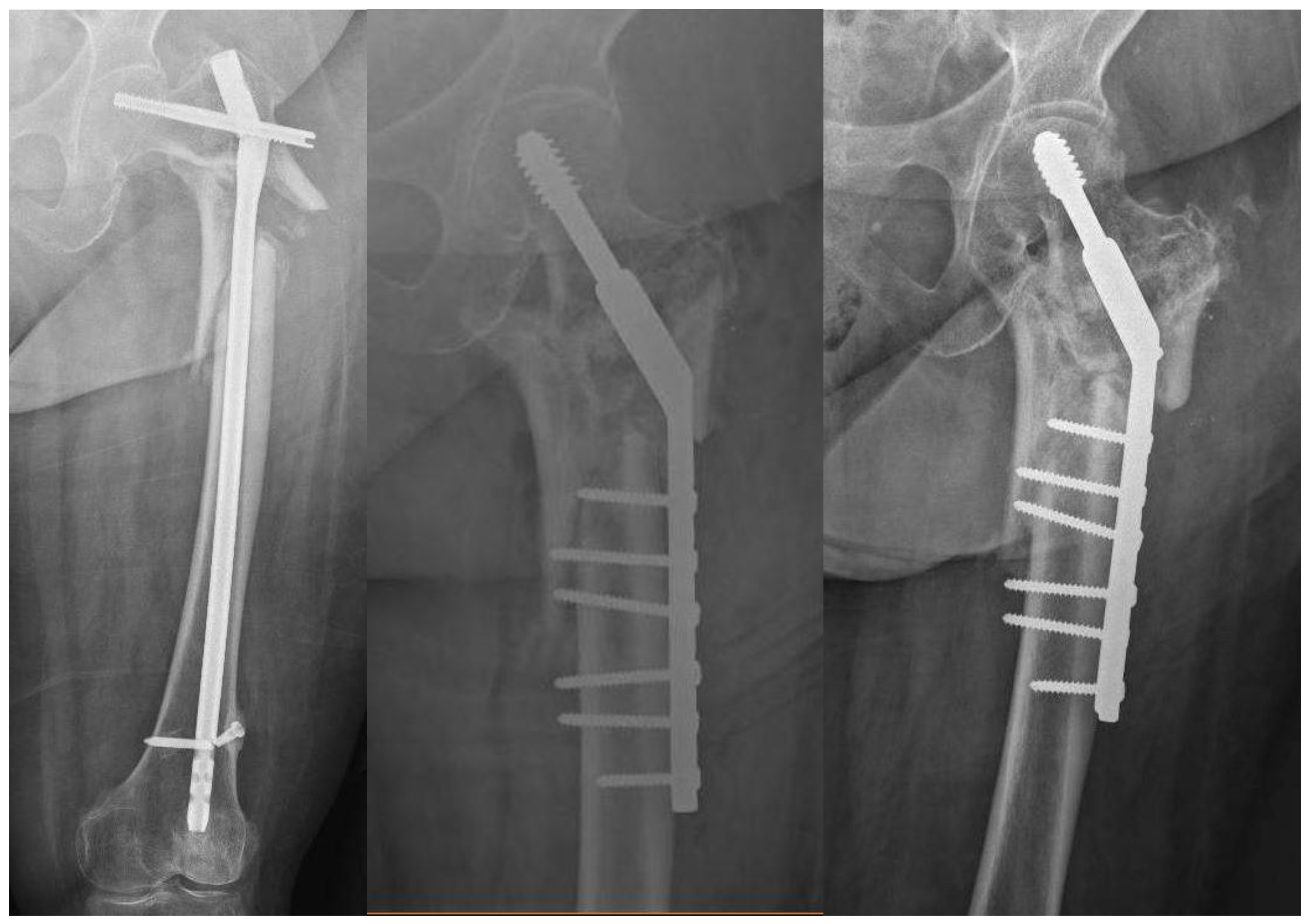
The mean age of patients was 57 (range 34-85). 2 women, and one man. Three fractures were subtrochanteric. The younger patient was 34 years old and had been operated on several times by nail exchanges (
Figure 9).
The second patient was a woman, 85 y.o., with a varus nonunion (
Figure 10)
The duration of surgery was 102 min (63-123). The femoral neck angle before surgery was 125º (122-128), and after surgery 147º (142-150). Offset was 50 mm (42-59) before surgery and 20 mm (19-24) after surgery. Leg length was increased by 8,6 mm (6-12). Harris hip score was 37,33 (30-42) before surgery, and 93,33 (88-96) after it. All patients healed and were asymptomatic after 12 months of follow-up.
Detailed data of patients is shown in
Table 1.
4. Discussion
Most subtrochanteric nonunions are due to technical errors during osteosynthesis. Varus mal-alignment is the most common factor. This varus mal-alignment means that high shear forces are applied to the fracture site when walking, making the fracture unable to heal. Nearly all treatments of subtrochanteric nonunions involve some degree of varus correction [
4,
5].
So, to correct nonunion, is key to achieve valgus overreduction to get compression forces at the nonunion site [
1].
This overcorrection is quite difficult (if not impossible) to perform with a nail. You need to insert a nail in a too-medial entry point, which is most times impossible to get [
7]. The only way to get overcorrection is with an extramedullary system.
Most extramedullary systems described to date can correct varus but are not able to apply dynamic compression at the nonunion site. Silva et al [
17] published a case series of trochanteric nonunions treated with valgus subtrochanteric osteotomy and several forms of fixation, most of them non-dynamic. Nevertheless, they achieved union in 16 out of 17 patients reported. Vienti et al [
5] reported 8 subtrochanteric nonunions with no varus malalignment treated with a 95-degree blade plate, bone, and RIA graft. 7 nonunions healed, and the other one was operated again with the same system and more fixation (double plate), achieving union.
Non-dynamic compression has the problem of the reabsorption of bone ends after osteotomy. This makes this zone less stiff and applies bending forces to the plate that can make it break or fail. That’s the reason to use this system, to apply dynamic compression. In all cases some impaction of the nonunion site occurred, demonstrating that the system is dynamic and promotes union through mechanical compression at the nonunion site.
Vidyadhara et al [
18] developed a closing lateral wedge valgus osteotomy fixed with a dynamic hip screw for trochanteric nonunion. They achieved union in all seven patients treated. The philosophy (valgus correction) and fixation method (dynamic compression) are quite similar to ours. The differences are that they did not use it for subtrochanteric fractures, and they performed a closing wedge osteotomy to correct valgus. In our study, we did not perform an osteotomy (just decompaction of the nonunion site to allow correction). In this way, we did not alter the vascularization of the zone, and we achieved an elongation of the limb (shortened by the nonunion).
Valgus correction and dynamic compression have been also indicated in recent papers. El Alfy et al [
4] performed a valgus osteosynthesis to subtrochanteric nonunions through a modification of a 95-degree blade plate. They performed a removal of the nonunion site and claimed a dynamic compression at the fracture site. This technique is somehow similar to ours, as it overcorrects varus, but it is fixed with another system that applies less compression to the nonunion site. Moreover, they removed the nonunion site, creating some vascular deficit in this situation, and used bone graft in some cases (8 out of 26). Nevertheless, they achieved union in nearly all cases (25 out of 26).
This technique has some limitations. The main limitation is the small number of patients treated to date. This nonunion is not quite usual, so to get a large number of patients is difficult. The objective of this paper is to publish a standardized method to be used by other centers and to get a bigger number of patients.
In conclusion, Valgus correction with a dynamic hip screw is a useful technique for a nonunion of a subtrochanteric hip fracture. This zone is well vascularized, so just dynamic mechanical compression at the fracture site is needed. This variation in the technique makes surgery easier to perform.
Author Contributions
Conceptualization, Delgado-Martinez; methodology, Delgado-Martinez; formal analysis, Delgado-Martinez, and Cañada-Oya.; investigation, Delgado-Martinez, and Cañada-Oya.; writing—original draft preparation, Delgado-Martinez and Cañada-Oya.; writing—review and editing, Delgado-Martinez and Cañada-Oya.. All authors have read and agreed to the published version of the manuscript
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted following the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Hospital Universitario de Jaén (protocol code INV-2022-023, approved on Feb 4, 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Moreover, written informed consent has been obtained from all three patients to publish this paper.
Data Availability Statement
Data from all patients remains in the computers of the institution. Access to these data is confidential, but authors can provide data as necessary.
Acknowledgments
To all members of staff and residents of the Department of Orthopedic Trauma from our institution, for their kind support
Conflicts of Interest
The authors declare no conflicts of interest.
References
- DeRogatis MJ, Kanakamedala AC, Egol KA. Management of Subtrochanteric Femoral Fracture Nonunions. JBJS Rev. 2020 Jun;8(6):e1900143. [CrossRef] [PubMed]
- Prasarn ML, Ahn J, Helfet DL, Lane JM, Lorich DG. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res. 2012 Aug;470(8):2295-301. Epub 2012 Jun 6. [CrossRef] [PubMed] [PubMed Central]
- de Vries JS, Kloen P, Borens O, Marti RK, Helfet DL. Treatment of subtrochanteric nonunions. Injury. 2006 Feb;37(2):203-11. Epub 2006 Jan 18. [CrossRef] [PubMed]
- El-Alfy B, Abououf A, Darweash A, Fawzy S. The effect of valgus reduction on resistant subtrochanteric femoral non-unions: a single-centre report of twenty six cases. Int Orthop. 2024 Apr;48(4):1105-1111. Epub 2024 Jan 16. [CrossRef] [PubMed] [PubMed Central]
- Vicenti G, Solarino G, Bizzoca D, Simone F, Maccagnano G, Zavattini G, Ottaviani G, Carrozzo M, Buono C, Zaccari D, Moretti B. Use of the 95-degree angled blade plate with biological and mechanical augmentation to treat proximal femur non-unions: a case series. BMC Musculoskelet Disord. 2022 Feb 28;22(Suppl 2):1067. [CrossRef] [PubMed] [PubMed Central]
- Gargallo Verge EJ, Villalon Ogallar J, Perez-Nuñez MI. Fracturas subtrocantéreas y diafisarias del fémur. In: Delgado-Martinez AD, Cirugia Ortopédica y traumatologia. 6th ed. Editorial Médica Panamericana. pp 809-818, 2024.
- Kainth GS, Nebhani N, Shah B, Kumar G, Kapoor B. Varus mal-alignment and residual displacement are associated with delayed union in subtrochanteric femur fracture- A retrospective observational study. J Orthop. 2023 Oct 30;46:64-69. [CrossRef] [PubMed] [PubMed Central]
- Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002 Nov;84(8):1093-110. [CrossRef] [PubMed]
- Nakken ER, Achor TS, Berkes MB. Medialized Trochanteric Entry Nailing Is a Safe and Effective Method for High-Energy Subtrochanteric Femur Fracture Treatment. J Orthop Trauma. 2022 Dec 1;36(12):458-462. [CrossRef] [PubMed]
- Khanna A, MacInnis BR, Cross WW, Andrew Sems S, Tangtiphaiboontana J, Hidden KA, Yuan BJ. Salvage of failed subtrochanteric fracture fixation in the elderly: revision internal fixation or hip arthroplasty? Eur J Orthop Surg Traumatol. 2024 Aug 26. Epub ahead of print. [CrossRef] [PubMed]
- Giannoudis PV, Ahmad MA, Mineo GV, Tosounidis TI, Calori GM, Kanakaris NK. Subtrochanteric fracture non-unions with implant failure managed with the "Diamond" concept. Injury. 2013 Jan;44 Suppl 1:S76-81. [CrossRef] [PubMed]
- Kim JT, Jeong HJ, Lee SJ, Kim HJ, Yoo JJ. Adjuvant Teriparatide Therapy for Surgical Treatment of Femoral Fractures; Does It Work? Hip Pelvis. 2016 Sep;28(3):148-156. Epub 2016 Sep 30. [CrossRef] [PubMed] [PubMed Central]
- Haubruck P, Kammerer A, Korff S, Apitz P, Xiao K, Büchler A, Biglari B, Zimmermann G, Daniel V, Schmidmaier G, Moghaddam A. The treatment of nonunions with application of BMP-7 increases the expression pattern for angiogenic and inflammable cytokines: a matched pair analysis. J Inflamm Res. 2016 Sep 22;9:155-165. [CrossRef] [PubMed] [PubMed Central]
- Dietze C, Brand A, Friederichs J, Stuby F, Schneidmueller D, von Rüden C. Results of revision intramedullary nailing with and without auxillary plate in aseptic trochanteric and subtrochanteric nonunion. Eur J Trauma Emerg Surg. 2022 Jun;48(3):1905-1911. Epub 2021 Apr 16. [CrossRef] [PubMed] [PubMed Central]
- Rehme-Röhrl J, Brand A, Dolt A, Grünewald D, Hoffmann R, Stuby F, Schweigkofler U, von Rüden C. Functional and Radiological Results Following Revision Blade Plating and Cephalomedullary Nailing in Aseptic Trochanteric and Subtrochanteric Nonunion. J Clin Med. 2024 Jun 19;13(12):3591. [CrossRef] [PubMed] [PubMed Central]
- Dheenadhayalan J, Sanjana N, Devendra A, Velmurugesan PS, Ramesh P, Rajasekaran S. Subtrochanteric femur nonunion - Chasing the elusive an analysis of two techniques to achieve union: Nail-plate fixation and plate-structural fibula graft fixation. Injury. 2024 Jun;55(6):111462. Epub 2024 Feb 28. [CrossRef] [PubMed]
- Silva P, Coelho DL, Curi C Jr, de Oliveira LA, de Moraes FB, do Amaral RA, Rebello PR. Proximal femoral valgus subtrochanteric osteotomy for nonunion of throcahnteric fractures. Rev Bras Ortop. 2015 Nov 16;47(1):37-42. [CrossRef] [PubMed] [PubMed Central]
- Vidyadhara S, Rao SK, Pandian S, Gnanadoss J. Closing lateral wedge valgus osteotomy with dynamic hip screw for the treatment of varus nonunion of pertrochanteric fracture: can restoration of biomechanics and stabilization alone heal? Arch Orthop Trauma Surg. 2009 Jun;129(6):827-32. Epub 2008 Dec 24. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).