Invasive candidiasis comprises both candidaemia and deep-seated tissue candidiasis and typically occurs among hospitalized patients. It has been reported to affect more than 250,000 people worldwide causing more than 50,000 deaths every year. Candidaemia is the most common manifestation of invasive candidiasis and is mentioned in the literature as the fourth most common bloodstream infection and a leading cause of nosocomial bloodstream infections, with very high morbidity and mortality (overall 90-day mortality: 43%) [
1,
2]. Detection of candidaemia by peripheral blood smear (PBS) is very rare and requires high yeast concentration ≥ 1-5x105 cfu/mL and evaluation by an experienced microscopist [
3]. It constitutes an emergency as it shows advanced infection and immediate treatment is required [
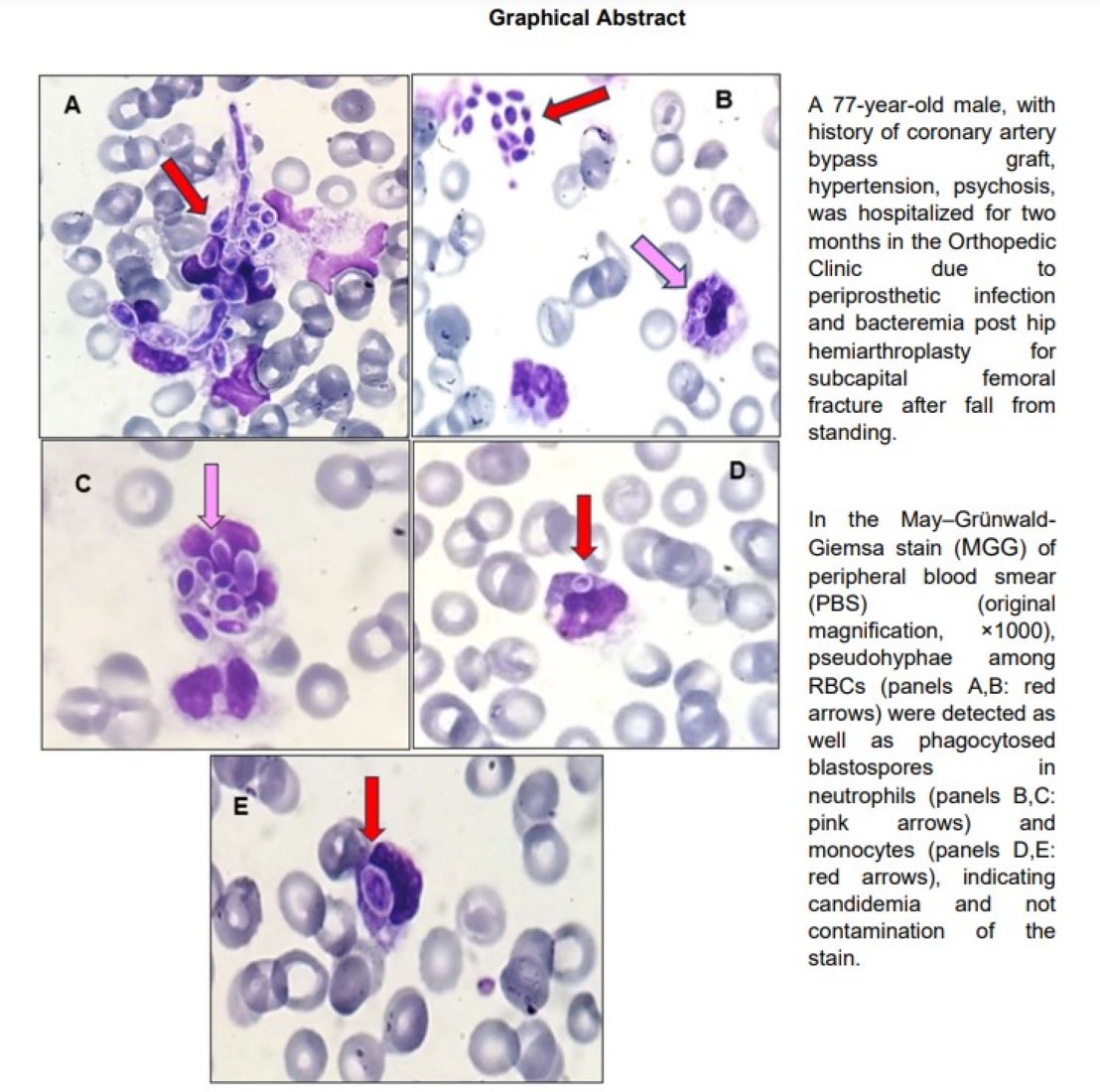
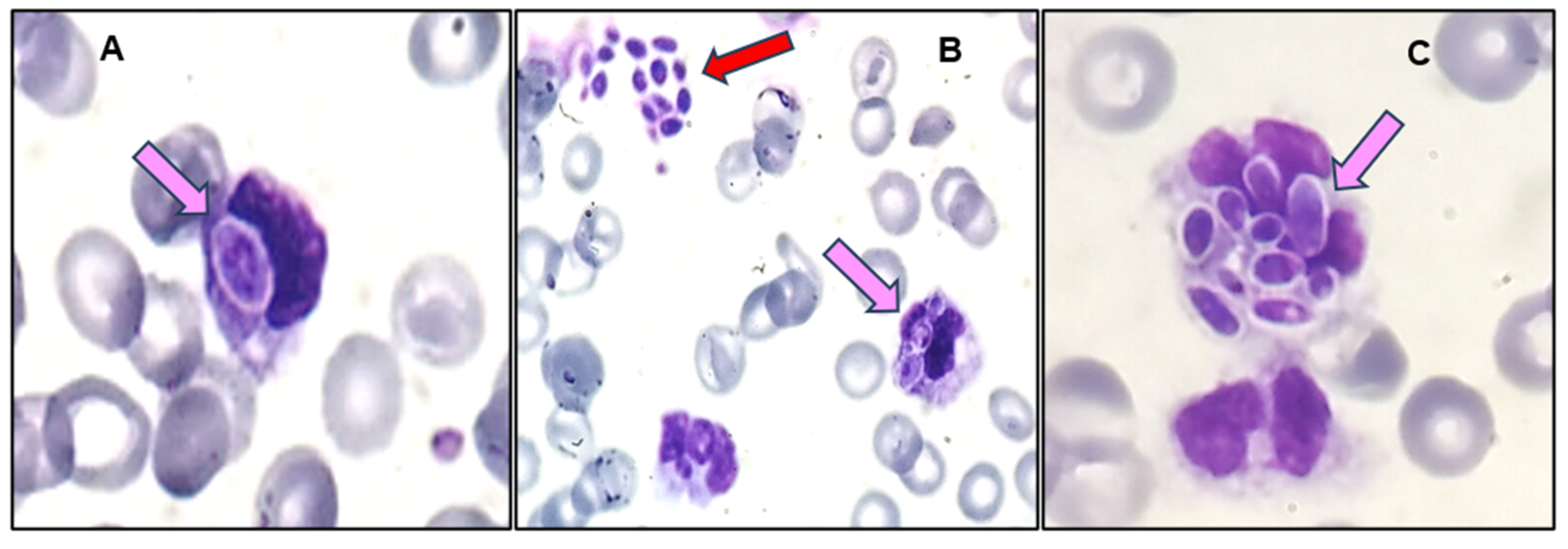
2]. Finding phagocytosed blastospores in the cytoplasm of leukocytes in addition to free blastospores and pseudohyphae is essential to exclude contamination of the stain and to confirm true candidaemia [
4].
Surgical Site Infection (SSI) is one of the major complications following hip or knee insertion, with early onset infection occurring within the first three months after surgery. The incidence of prosthetic joint infection (PJI) following primary total hip arthroplasty (THA) is lower than in knee arthroplasty and is estimated to be approximately 1%. The vast majority of PJI are bacterial, while fungal prosthetic joint infection (fPJI) constitutes about 1-2% of the total PJI and is usually caused by Candida spp. A total of 372 fPJI cases have been reported in the literature, with 161 of them being complication of THA [
5].
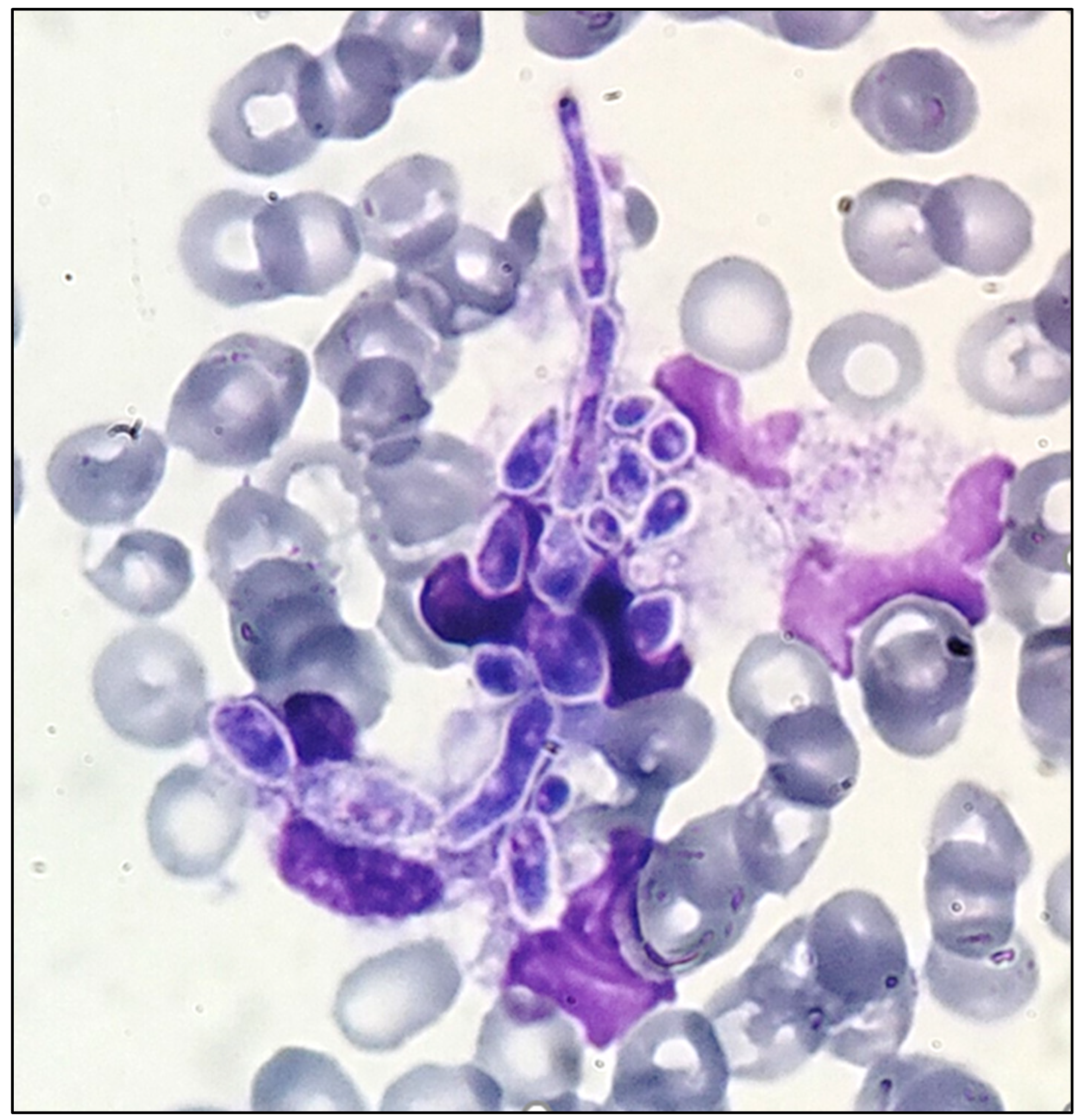
An elderly male, with a history of coronary artery bypass graft (CABG) and hypertension was hospitalized in the Orthopaedic Clinic due to periprosthetic joint infection (PJI) and bacteraemia post hip hemiarthroplasty. The patient was initially admitted for subcapital femoral fracture after fall from standing, while there was also a history of a recent hospitalization due to SARS-CoV-2 infection, treated with remdesivir and dexamethasone. He was discharged postoperatively with instructions for mobilisation and wound cleansing, however, follow-up revealed the presence of periprosthetic infection. Surgical debridement of the arthroplasty, initially performed, failed to control the infection. Finally, the patient underwent removal of the prothesis (Girdlestone procedure), vac drainage, and placement of a central venous line (CVL), for coverage with targeted antibiotic therapy against pathogens isolated from blood (MRSA) and wound (tissue, pus) cultures (MRSA, P. aeruginosa, P. mirabilis), while transfusions and fluid/electrolyte replenishment were also needed. The patient initially improved and became hemodynamically stable but gradually the complete blood count (CBC) revealed signs of myelosuppression. Low grade fever reoccurred, and the latest CBC showed severe thrombocytopenia. The urine analysis showed blastospores and a peripheral blood smear (PBS) was prepared to confirm the findings of the CBC. In the May–Grünwald-Giemsa stain (MGG) of PBS pseudohyphae and free blastospores were coincidentally detected (
Figure 1).
Further assessment of the smear confirmed our initial findings, as a phagocytosed blastospore was detected in the cytoplasm of a monocyte: the first blastospore that was detected in a WBC (
Figure 2).
Candidaemia is associated with multiple risk factors [
6,
7]. Communication with the attending orthopaedic surgeon concerning the patient’s history raised higher suspicion, as it confirmed the co-existence of many, among them: precedent surgery, CVL and Foley, prolonged hospitalization, concomitant bacterial infection, and broad-spectrum antibiotics. Meticulous examination of the blood smear further revealed: phagocytosed blastospores in both monocytes and neutrophils, as well as another site of free blastospores among red blood cells (
Figure 3). An echinocandin was administered, according to the guidelines, as empiric treatment for suspected candidiasis [
8,
9]. Due to the emergence of non-albicans Candida spp. and the coexistence of previous hospitalizations, increasing the risk of possible exposure to C. auris, the use of an azole was avoided. Blood cultures were immediately obtained after communication and were urgently processed using Film Array multiplex PCR, identifying C. albicans. Candida is routinely initially detected in the Gram stain of positive blood cultures, and prompt notification of the clinician is required to start empirical antifungal treatment. Isolation from positive blood cultures remains the gold standard for diagnosing candidaemia [
7] Identification and antifungal susceptibility testing, using Vitek2, showed fluconazole sensitive C. albicans in both the urine and the blood culture of the patient. Despite echinocandin administration and CVL removal, the patient passed away within the first 24 hours after the initial diagnosis [
10].
Author Contributions
Conceptualization, S.C.; methodology, writing—original draft preparation, E.S; methodology, visualization, L.M.G., I.C, N.J.T.; investigation, N.P.; writing—review and editing, E.S., S.C.; supervision, S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable
Informed Consent Statement
Patient consent was waived due to fatality, the patient could not grant consent. Only microscope images were included, and patient-identifying details were omitted.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Acknowledgments
Authors are greatly thankful to Giannis Kotsalis for his contribution in the investigation of the case.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kullberg, B.J.; Arendrup, M.C. Invasive Candidiasis. N. Engl. J. Med. 2015, 373, 1445–56. [Google Scholar] [CrossRef] [PubMed]
- Hirai, Y.; Asahata, S.; Ainoda, Y.; et al. Candidemia Diagnosed from Peripheral Blood Smear: Case Report and Review of Literature 1954-2013. Mycopathologia 2015, 180, 111–6. [Google Scholar] [CrossRef] [PubMed]
- Branda, J.A.; Ferraro, M.J.; Kratz, A. Sensitivity of peripheral blood smear review for the diagnosis of Candida fungemia. Arch Pathol Lab Med. 2007, 131, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Garg, N.; Gupta, R.J.; Siroha, A.; Kumar, S. Peripheral Blood Smear: Hematologist Buddy to Catch Dangerous Budding: A Report of Two Cases. J Microsc Ultrastruct. 2022, 10, 211–213. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sambri, A.; Zunarelli, R.; Fiore, M.; Bortoli, M.; et al. Epidemiology of Fungal Periprosthetic Joint Infection: A Systematic Review of the Literature. Microorganisms 2022, 11, 84. [Google Scholar] [CrossRef] [PubMed]
- Thomas-Rüddel, D.O.; Schlattmann, P.; Pletz, M.; Kurzai, O.; Bloos, F. Risk Factors for Invasive Candida Infection in Critically Ill Patients: A Systematic Review and Meta-analysis. Chest 2022, 161, 345–355. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alves, J.; Alonso-Tarrés, C.; Rello, J. How to Identify Invasive Candidemia in ICU-A Narrative Review. Antibiotics 2022, 11, 1804. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hoenigl, M.; Salmanton-García, J.; Egger, M.; Gangneux, J.P.; et al. ECMM Candida III Study Group. Guideline adherence and survival of patients with candidaemia in Europe: results from the ECMM Candida III multinational European observational cohort study. Lancet Infect Dis. 2023, 23, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Garnacho-Montero, J.; Díaz-Martín, A.; Cantón-Bulnes, L.; Ramírez, P.; et al. Initial Antifungal Strategy Reduces Mortality in Critically Ill Patients With Candidemia: A Propensity Score-Adjusted Analysis of a Multicenter Study. Crit Care Med. 2018, 46, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Detection of candidemia in May-Grünwald/Giemsa stain of peripheral blood smear. Spatha, E.; Gheorghe, L.M.; Chaliori, I. Detection of candidemia in May-Grünwald/Giemsa stain of peripheral blood smear. Spatha, E.; Gheorghe, L.M.; Chaliori, I.; et al. Infectious Disease World Conference, Proceedings of the Infectious Disease World Conference (IDWC 2024), California, USA, 7-8/9/2024. www.infectiousworldconference.com, Day 2, Poster 3, p.51-52.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).