1. Introduction
The hormone-derived signals are those of most intensively studied factors in carcinogenesis. However, the pathological hypersecretion of several hormones is the area of endocrinology, despite cross-talk with cancer and immunity. Furthermore, the immunoendocrinopathy shows balance between the pro- (hormonal) and anticancerous (immunity) pathways. In this context the organ-specific autoimmunity, such as autoimmune thyroid disease (AITD) may be a good model for looking for more specific immunotherapy than systemic immune checkpoint blockade. The role of the local niche seems to be underestimated, and research is mainly conducted on the intestinal microbiota [
1]. However, pulmonary microbiome is one additional pathogenetic factor (extremely variable) that affects overall survival in various ways [
2]. Furthermore, the immunity in patients with lung cancer may be difficult because the more microbial antigens from mycobacteria, fungi and viruses involve lymphocyte, sometimes inducing lymphoproliferative disease, but also induce cytokine storm and “spontaneous” regression [
3] . Currently, the research includes studies on patients with developed thyroid cancer (TC). Previous history, including AITD, is usually briefly described with taking into account only TSH level, antibodies against TSH receptor (TRAB) and Graves disease (GD). Higher incidence of thyroid carcinoma in patients with GD was studied in many cohort studies, but crucial issue is about a cause-and-effect relationship, not a statistical one. Although initial paradigm states that hyperthyroidism is a protective mechanism due to suppressed hormonal signal i.e. TSH. However, further statistical analyses showed higher coexistence of Graves disease (GD) with thyroid cancer, but high GD prevalence in thyroid cancer is only a statistical link (pathways are not described).[
4] For example, if TC coexists with GD, the immunogenetic background and the role of autoimmunity in TC were not explained [
5]. TSH, TRAB and manifestation are described only qualitatively. Therefore in such publications, the co-occurrence rather than the mutual influence of such processes is described. Thus, the correlation between GD and TC is controversial. For clinical immunologist and patient-centered care crucial is the question what is the cause is and what the effect? The patient time-lapse analysis may be a good tool for such observation. Very intensive immune response may be the cause of proliferative disease (precancerous state), but on the other hand -very beneficial immunity against tumor-specific antigens such as thyroglobulin (TG). Interestingly, most TCs have a small tumor size (about 50% is below 1 cm)[
6] without stroma, but immune response against thyroid antigens may be beneficial, since the most common adverse effect of immunotherapy (e.g. with interferons, immune-checkpoint blockade) is autoimmune thyroiditis.[
7,
8] Now we know that immune response is a critical surveillance against cancer, but immunity against cancer cells usually cross-reacts with host cells with severe outcome. Therefore, autoimmunity against organ/tissue specific antigens is a good model for immunotherapy-induced adverse drug reaction to assess risk-benefit ratio.
We looked for the cases with autoimmune endocrinopathy in the first stage, with presentation of cancer in the next step, coexisting with long-term infectious inflammation. (e.g. tuberculosis). This methodology precisely described in section 4 prompted to find temporal connections and pathways.
2. Results
This case-control study describes best documented cases of AITD course with various infectious and oncological complications and outcomes with overall survival (OS).
The time-lapse analysis of mutual biochemical, endocrine and immunological parameters is presented in
Table 1. Comparing our AITDs where hyperthyroidism, hypothyroidism, or both occur at different times, no clear effect of hypothyroidism and elevated TSH on TC and outcome can be seen.
First woman (BMI 15 kg/m2) with initial osteopenia (received vitamin D up to 4000 IU per day) was admitted to the outpatient clinic. Due to tachycardia and hypertension she was treated with beta-blockers, but the symptoms, weakness and fatigue were getting worse. The patient observed severe body weight loss (6.5kg over 6 months). The dispone was observed, x-ray of the chest showed small nodules. Tuberculosis was initially diagnosed because of positive QuantiFERON result and epidemiologic data. After CT the mediastinal lymphadenopathy and residual pleural effusion were observed. She received corticosteroids and underwent bronchoscopy. The bronchoalveolar examination showed cancerous cells, identified as NSCLC , with positive thyroid transcription factor-1 (TTF-1) expression (i.e. lung adenocarcinoma). The small amount of cancer cells was not enough for further analysis. Patient was qualified to sequential chemo radiotherapy. After the first course the patient deteriorated and significant hyperthyroidism was observed in spite of therapy with thiamazole. Bilateral pleural effusion and atrial fibrillation developed, symptoms progression, especially severe cachexia with the decrease of the quality of life were observed. In the next step the fine needle biopsy of the thyroid confirmed the cancerous cells with TTF-1 expression. The bone scintigraphy was negative for bone involvement. Due to coexistence of cardiac as well systemic symptoms (i.e. hypocalcemic tetany, cachexia) the woman was qualified to best supportive therapy (BST). Tuberculosis reactivation was observed later with unfavorable outcome. The retrospective analysis of endocrine status revealed previous low TSH (initially 4 years before). In spite of anti-thyroid peroxidase (anti-TPO 1:320) as well as anti-thyroglobulin titer (anti-TG 1:1280) the GD was not diagnosed, because associated with GD thyroid stimulating antibodies (TSA i.e. activator TRAb) were not observed. The patient occasionally received thyroid hormone from the endocrinologist (transient hypothyroidism with high TSH was observed later). Self-limiting inflammatory thyroiditis (de Quervain) was finally diagnosed because of transilient FT3/4 fluctuation, granulomatous disease and constellation of antibody against anti-thyroid antigens. Radioiodine uptake was not tested.
The second 71-year old woman was admitted to hospital due to fatigue, cough, severe decrease of body weight (4kg within 2 months; BMI 13.4), hypotension and respiratory depression with hypoxia. The initial symptoms were somnolence, nausea, myoclonus and reduced renal function. In past history, the woman was diagnosed with hypertension and had suffered from pneumonia 10 years earlier. She was also treated with radioactive iodine therapy -a safe and effective procedure for her GD-hyperthyroidism (with TSA above 1:1280) 3 years before admission. For a long time she was in good condition, received antihypertensive drugs and thyroid hormone supplementation. Laboratory analysis revealed high level of FT4=22pmol/l (Normal 9-19), TSH below detection limit (i.e. 6μIU/ml), low calcium level Ca++=1.12 mmol/l.
Chest CT revealed numerous nodules in the lung apexes and a left-sided infiltration in the middle part of the lower lobe (8x5 cm). After bronchoscopy bronchoalveolar lavage showed firstly positive bacterioscopy and polymerase chain reaction (PCR) determining the Mycobacterium tuberculosis complex (the result was confirmed by mycobacterial culture later). The standard anti-tuberculosis therapy was started. In the following weeks, the patient received medications, but required supportive therapy (oxygen, , anti-swelling and anti-inflammatory pain medications).
Histopathological examination revealed the presence of cancer cells in the bronchial specimen. Cancerous cells were identified as NSCLC. Further examinations showed positive TTF-1 and PD-L1 expression in 40% of cells.Magnetic resonance imaging of the head showed the presence of a focus (about 2cm) in the right hemisphere of the brain (the patient did not give consent to surgery).NSCLC (adenocarcinoma) in the T4N2M1b stage was disqualified from palliative radiotherapy due to severe progressive cachexia, somnolence and myoclonus. The woman died a shortly afterwards (3 months later receiving antituberculosis drug and BST). Unfortunately, the genetic background in NGS showed no mutation in EGFR, KRAS, nor in ALK and ROS1 rearrangement, but it did in BRAFV600E mutation i.e. T > A (V600E).
The third, 69-year-old woman, not an active smoker, previously suffering from hypertension, long-term overweight (BMI = 26.64) and osteoporosis was referred to a pulmonologist due to cough, shortness of breath and fatigue. In the initial period she took glucocorticosteroids (gks) (methylprednisolone 4-16mg/day) with improvement. CT scan revealed emphysematous bubbles in the apical and subapical segments, as well as numerous small (2-3 mm) nodules throughout the lungs. There was no lymphadenopathy detected. After gks dose reduction (to 4 mg) temporary deterioration was observed. After a year, the patient lost 6 kg in 5 months (despite insulin resistance, hyperglycemia and glycosuria). The TB-QuantiFERON test (QFT) showed a moderately positive (actually borderline) result.
Another CT scan revealed a clear two-centimeter tumor in the right lung (segment 2) with numerous projections and a bright center. No cancer cells or acid-fast bacilli were detected in BAL and brush biopsy. The mycobacterial culture was also negative.
The woman was qualified for thoracic surgery. In PET scanning, before the procedure, an irregular soft-tissue mass of several centimeters with deep decay was observed in segment 2 on the right side (SUV = 8.4). No lymphadenopathy was detected nor significant metabolic activity of the lymph nodes (neck nor chest). No attention was paid to the image of the thyroid gland. However, PET also showed a small thyroid gland, with an approximately 10-mm lesion in the right lobe (SUV=5.9).
Video-assisted thoracic surgery(VATS) was performed, including right upper lobectomy and systemic lymphadenectomy (without complications). After the lobectomy, the patient was referred to an endocrinologist. Ultrasound examination of the thyroid gland and verification were performed.
In both lobes there were several merging hypoechoic foci of irregular shape, the largest of them in the right lobe, measuring 13.6 x 9.8 mm with significant vascularization. There were no enlarged lymph nodes along the large cervical vessels. The patient had an inconclusive fine-needle aspiration biopsy (FNAB) result. The preparations were of extremely low cellularity: no follicular cells in the left lobe, scattered thyrocytes in the right lobe, colloidal content, inflammatory cells. The image was consistent with atrophic thyroiditis but local atypia, lymphoid cells and sign of cytotoxicity were observed. It corresponds with hormonal status and serology (
Table 1). Interestingly, histopathological examination showed no cancer nor typical granuloma, but massive caseous necrosis. Immunohistochemistry showed several acid-fast bacilli in necrotic mass. The tuberculosis was diagnosed taking into account the CT, QFT and acid fast bacilli. Unfortunately, the next verification did not confirm tuberculosis in PCR (in the same probe acid fast bacilli were positive), granuloma or mycobacterial staining in lymph nodes The environmental mycobacteria were probable, therefore treatment was not obligatory. In the next verification still no cancer cells were observed in pulmonary lobe nor in lymph nodes.
3. Discussion
The immune endocrinopathy shows balance between the pro- (hormonal) and anticancerous (immunity) pathways.The identified AITD susceptibility genes include immune-modulating genes, such as the Major Histocompatibility Complex, Cytotoxic T Lymphocyte Antigen-4 (CTLA-4), CD40 molecule, Protein Tyrosine Phosphatase-22, TSH receptor and Thyroglobulin (TG). In this context the organ-specific autoimmunity, such as autoimmune thyroiditis may be a good model for searching for more specific immunotherapy than systemic immune checkpoint blockade with severe autoimmune adverse reaction (e.g. anti-CTLA-4).
On the other hand, immunity in patients with NSCLC may be difficult because the more microbial antigens from microbiome (bacteria, fungi and viruses such as CMV) involve lymphocytes, sometimes inducing lymphoproliferative disease, but also induce cytokine storm [
9].
3.1. Epidemiological, Statistical versus Clinical Model
Endocrine cancer and immunity predisposition syndromes are inherited entities determined especially by germinal pathogenic variants. Most frequent thyroid cancer predisposition syndromes coexist with endocrinopathy (MEN II, familial adenomatous polyposis), but usually with immunogenetic background (primary immunodeficiency, Li Fraumeni syndrome, Ataxia-telangiectasia)[
10]. It is not a full list, because immunodeficiency and immune dysregulation is observed in the destruction of genome integrity, the DNA repair process, miRNA formation and maturation, various signaling pathways as well as predisposition to infectious diseases [
2,
10]. For example adenosine deaminase (ADA) may be crucial in specific immunity (mutation causes severe combined immunodeficiency) but in different conditions, such as in patients with tuberculosis, when ADA level in pleural effusion is high. Our patients showed pleural effusion, noteworthy, without cancer cells. Furthermore, thyroid hormone levels change in response to lymphocyte proliferation in patients with tuberculosis and bacterial infections as described previously [
11].
Higher incidence of thyroid carcinoma in patients with Graves disease was studied in many cohort studies. Correlation is still very controversial, but crucial issue is about a cause-and-effect relationship, not a statistical one. For example, two retrospective studies using the same methodology showed completely contradictory results: the first clearly indicated a poor prognosis and worse course of TC in patients with GD (including chronicity and recurrence rate)[
12], the second one- the opposite (much smaller tumor size in patients with GD)[
5]. The criteria for diagnosing AITD are non-homogenous, and TRAB themselves may be stimulating (TSA) or blocking, which is omitted in cohort studies. Nevertheless, high thyroid hormones do not determine the immune mechanism, as described here (see
Table 1) and anti-TG has no defined action as reviewed by Frohlich et al.. However, first publication is a simple comparison of GD+TC and euthyroid patients with TC [
13], but in GD the athyreosis may also be observed. TC is collectively named as differentiated thyroid cancer without subtype.
3.1.1. Bias in Cohort Studies
Both cited publications (as an example) and previously published papers have a basic defect: patients with autoimmune thyroiditis were limited only to GD and the retrospective analysis included patients with diagnosed TC. Such selection bias is observed and undermines the reliability of statistical studies in the face of contradictory conclusions [
14]. The first criterion, i.e. TC, obstructs observation whether cancer develops more often in patients with thyroiditis (especially GD) and (if yes) after what time. Literature on AITD and TC association are based on preoperative FNA or post thyroidectomy histopathology reports, so at the data collection stage, patients are not representative [
15]. Conversely, AITD may be an antitumor immunity (the same antigens). Moreover, the presence of antibodies (anti-TPO, anti-TG or TSA) is very often found in healthy people. The TSA is transitory IgG1 with known effect, contrary to anti-TPO and anti-TG [
16].
3.1.2. Bias in High Specialisation Oncology
Lymph node involvement was found in 56% of patients with Graves' disease, in 23% of those with toxic goiter and distant metastases were found in one patient with Graves' disease only [
4]. In our observation the neck lymphadenopathy was not observed. Contrary to other cancers the lymphatic system seems to be negligible because thyroid gland has intensive vascularization. Noteworthy, last study showed novel loci containing genes that were previously implicated in thyroid cancer (e.g., HES1, SPATA13, DIRC3, ID4) and positive association of TSH with VEGFA expression [
17], therefore angiogenesis.. If we look at our patient with blood-derived metastasis it is clear, that pulmonary circulation is the first filter. Therefore, TNM staging is not a good model for TC, since many TC are nodule-free and without lymph node involvement.
In 2011, the International Association for the Study of Lung Cancer, American Thoracic Society and European Respiratory Society introduced papillary subtype of lung adenocarcinoma coexisting with very high TTF-1 expression (90-100%) and 5% BRAF mutation [
18]. However, BRAFV600E mutation showed a high specificity for papillary TC, especially the classic variant and extrathyroidal extension [
19], whereas it was never found in follicular and medullary thyroid carcinoma or in benign thyroid neoplasms. In high specialization era (according to this classification) our patients (especially the second one) were misdiagnosed with lung adenocarcinoma, since TTF-1 seemed to be the single best marker [
20]. The 5% BRAF-positive papillary lung adenocarcinoma might be metastatic TC. Furthermore, the TTF-1 is a protein that regulates transcription of genes specific for the thyroid, lung, and diencephalon. The publication shows the added value of serving as a pneumocyte marker that can help confirm a primary lung origin. Intrudingly this “Multidisciplinary Classification of Lung Adenocarcinoma” describes a helpful procedure in addressing the question of metastatic adenocarcinoma from the colon or breast, but not thyroid gland [
18]. Renal cell cancer and lung cancer are most common cancers metastazing to thyroid gland. It might also be possible in the case of patient 1. However, this is a less realistic scenario, because no other metastases were observed, and thyroid disease significantly preceded the diagnosis of lung cancer, and the patient was a non-smoker. Metastases to the thyroid gland from cancer elsewhere are not considered by most studies based on preoperative FNA or post thyroidectomy. Therefore, in clinical observation TC and NSCLC (adenocarcinoma) symptoms usually overlap and consequently differentiation is very difficult. It requires whole body examination (as presented here by PET) and searching for strict diagnosis of previous endocrinopathy and cancer predisposition syndromes as well as immunodeficiency with DNA sequencing. Patient no 2 is a good example. Unfortunately, the latest Polish study of genetic predisposition to TC in 1076 unrelated individuals did not describe BRAFV600E [
21].
3.1.3. Thyroid Cancer Diagnosis, Rerporting, Estimation in Public Health
Thyroid cancer “overdiagnosis” is part of “overmedicalization”, easy empiric therapy i.e. therapeutic intervention without final and confirmed diagnosis (usually preemptive therapy). Therapeutic “success” and diagnosis
ex juvantibus prompt overreporting TC in public health with financial consequences. Similar discrepancy and reporting, i.e. false statistics, arise wherever treatment is not preceded by thorough diagnostics, as in the three presented cases. All three patients were included in the cancer registry and tumor board decisions, but with misdiagnosis.A very similar process, but on a much larger scale, has been observed in the COVID'19 era [
22], particularly when we observe global overuse and empiric therapy with antibiotics [
23]. For example, hospitalization is finished; patient was treated according to guideline with initial diagnosis of tuberculosis before the final results of mycobacterial culture (it takes 6-8 weeks) (patient 3, finally with mycobacteriosis) or after thoracic surgery before the histopathological result was obtained. The first patient received treatment before the thyroid process was verified. The second patient diagnosed with NSCLC died before the genetic background was analyzed and the cause of death was not analyzed comprehensively.
Therefore, it is a paradigm that TC progresses slowly, causes symptoms only when advanced, and rarely causes death, since the most aggressive and metastatic form (see later) is classified as lung cancer .
3.1.4. Translational Medicine
Organs such as prostate, breast or thyroid gland are not critical (life is possible after complete resection). Best supportive care is not difficult, contrary to lung, pancreatic cancer etc. Consequently in case of TC it is easier to achieve five-year survival. Chemo-radiotherapy may be difficult when cancer coexists with severe cachexia and infectious process. Such disease-oriented treatment is prone to errors (like NSCLC instead of TC or mycobacterial process), prolongs PFS with OS shortening and decrease of quality of life, as shown here following to the previous tumor boards decision analysis [
24]. Our patients 1 and 2 have short OS as the result of misdiagnosis and infectious process with concomitant medication. Unfortunately, the crucial factor was overall status (WHO) and severe cachexia. On the other hand, this report sheds light on the underdiagnosis of TC, misdiagnosed as TTF-1+ lung adenocarcinoma. In consequence, the overall survival in TC is good, since many cancerous processes, with fast blood-derived spread (without nodule and goiter) was classified as lung cancer, noteworthy, with worse prognosis, since BRAF mutation very specific for TC was classified as NSCLC, papillary type (see above).
3.1.4. Misdiagnosis and False Survival
It is quite a strange phenomenon, that cancers with simple observation and biopsy have better prognosis, because are more likely to be diagnosed in the early stages (statistical increase is also observed). Several bias and overestimation in TC is well-known phenomenon in scientific literature. Increase of TC incidence is a direct consequence of ease surgery. Furthermore, histologically proven follicular epithelial dysplasia in the form of scattered micro follicles without colloid and irregularly shaped follicles in autoimmune thyroiditis was observed [
25]. FNAB assessment is quite more problematic, and results may be inconclusive in initial oncogenesis, as observed in patient no 3. Pathogenesis of TC in our patients coexisted with production of proinflammatory cytokines and oxidative stress in autoimmune thyroiditis and tuberculosis. Inflammatory-derived atypia, especially epithelial dysplasia is usually observed in papillary TC and in precancerous state as described previously [
26]. Interestingly, the same picture in our patient 3 corresponded with SUV=5 in PET in spite of small volume, low FT4 production and high TSH, that are first precancerous hormonal factors (
Table 1,
Figure 2). Higher SUV was observed in mycobacterial inflammation with oxidative stress and production of proinflammatory cytokines, especially TNF. Currently, another hypothesis considered for the pathogenesis of PTC in HT is solid cell nest (SCN)[
27]. It can be misinterpreted as papillary thyroid microcarcinoma, squamous metaplasia. Contrary to our report and description SCN is negative for TTF-1 but has strong reactivity for p63.
3.2. Clinical Model and Evidence-Based Medicine
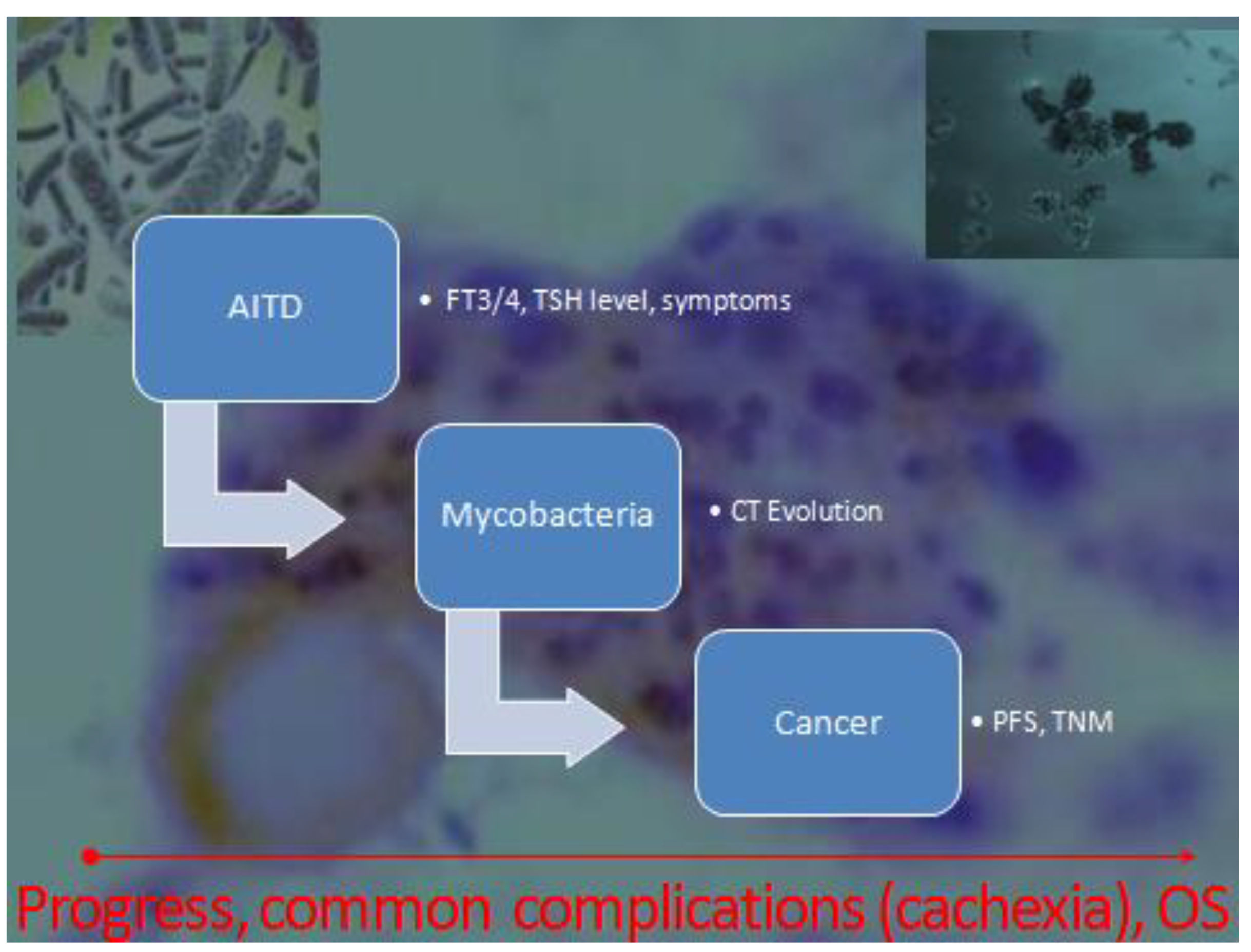
Our work is therefore methodologically different (case-control study). Firstly, it shows the development of the disease in time (
Figure 1) i.e. evolution of crucial parameters (
Table 1). Therefore, our observation and very high level of anti-TG indicate for the first time an antigenic target other than the previously indicated one, also present in all forms of AITD. Noteworthy, thyroglobulin is a known TC marker, extracellular target, observed in various types (
Table 1) as described by Fröhlich E and Wahl R. Therefore, the antigenic stimulation in TC and during inflammatory destruction is higher, contrary to intracellular enzyme (TPO) or TSH receptor with different expression (low in GD, normalized upon treatment)[
17]. Secondly, the aim was to recruit patients in whom the autoimmune process (AITD) preceded the development of cancer (even for years)(
Figure 1). Further: we did not limit the influence of AITD to TC only, but to broadly understood oncogenesis, since thyroid hormones affect all cells of the body
Finally, up to now, only childhood exposure to ionizing radiation has been fully recognized as the risk factor and conflicting results of potential or possible risk factors of TC indicate methodological bias.Therefore, lessons from individual clinical cases with time-lapse analysis, comprehensive, holistic approach can be all the more instructive, because the sequence of events is analyzed in a time perspective, i.e. the pathway [
28]
in vivo. It may be a good example for rare constellation and clinical presentation (many diseases).
3.3. Pathway and Time-Lapse Observation
3.3.1. Hormonal Signal and Homeostasis
Another underestimated phenomenon is the impact on water management and the action of calcium ions (
Table 1). The most common complication after surgery was transient hypocalcemia (36%), observed in our patients [
29]. Furthermore, the level of calcium as well as of other thyroid hormones (calcitonin) may be useful for the differentiation of TC type. High level of calcitonin and procalcitonin is typical for MTC (medullary TC [
30]). Furthermore, as presented in patient 2 calcinosis may be crucial, since the incidence of TC is higher when local calcinosis is observed [
31]. BMI at the time of diagnosis was directly related to the risk of thyroid cancer in females [
32], but not to OS (presented here). The role of estrogen in the development of thyroid cancer is still a matter of debate with inconsistent conclusions. The main idea is the observation that TC mainly affects women. If we look at the epidemiological data and the trend in thyroid cancer incidence, we see a similar increase in women and men aged >65 years, even though earlier AITD affected a vast majority of women [
32]. However, this is not a simple relationship. The same is appropriate for autoimmunity, IgM levels, or other X-linked traits, such as CD154-40 axis, mentioned among the susceptibility genes, key in the differentiation of B lymphocytes [
33]. Fetal micro chimerism refers to the presence within the maternal organism of a small population of cells originating from the fetus is proposed as a cause of women predisposition [
34], but in our observation there is no difference between multiparous and childless women. Finally, IPEX is X-linked immune dysregulation with autoimmune thyroid disease and opportunistic infections, but , interestingly as in our report, with extremely different presentation of hypothyroidism or thyrotoxicosis [
35]. Therefore, the final presentation of AITD may be individual and it is not a simple lack of immune tolerance, as presented here. Insulin regulates thyroid gene expression and stimulates thyrocyte proliferation, differentiation, and transformation. Insulin resistance was usually observed in TC females [
36]. Hyperinsulinemia, therefore, may be a risk factor for thyroid cancer [
33,
36]. The key issue is the gks overuse, which, on the one hand, blocks immunization, but also promotes osteoporosis, insulin resistance and corticoliberin, known TSH-inhibitor [
28]. It strictly corresponds with our third case, with high fasting glucose, TSH and hypocalcemia. Intriguingly, patients under influence of gks (partly by insulin resistance) develop secondary immunodeficiency with opportunistic infection with non-tuberculous mycobacteria. (MOT)(
Figure 2). This is an additional target for further research.
Figure 2.
Modification of unique balance between pro- and anti-cancerous factors (i.e. hormonal and inflammatory signal respectively) by microbiota (mycobacteria) and steroids.
Figure 2.
Modification of unique balance between pro- and anti-cancerous factors (i.e. hormonal and inflammatory signal respectively) by microbiota (mycobacteria) and steroids.
Thyroid hormone affects the functioning of nearly all of body organs and pleural effusion is one of more severe complications of AITD, of note, with very high anti-TPO, anti-TG antibodies, but without TSA [
37]. Some authors conducted literature search and found that kidney dysfunction and hypothyroidism could impact one another. Common coexisting conditions are: respiratory failure, heart disease, facial paralysis and pituitary hyperplasia, as well as myopathy with high non-cardiac creatine kinase level (about 1014 U/L in presented case). It corresponds with our observations in the first patient, (with de Quervain thyroiditis), but the hypocalcemic tetany and cachexia were not described previously. The pleural effusion may correspond with FT3 and FT4 level in tuberculosis (FT3 and FT4 levels in patients with effusion were significantly higher). Furthermore, conversion of T4 to T3 occurs also in the lung and the activity of Type I iodothyronine 5' deiodinase is statistically significantly lower in lung cancer than in peripheral lung tissue [
38].
3.3.2. Various Autoimmunity
It has been suggested that Hashimoto thyroiditis, primary myxedema or AITD and Graves’ disease are a basically similar autoimmune processes with personal diversity and that various clinical presentations depend on individual immunity in specific environmental setting [
39]. Basic genetic predispositions are highly polymorphic and individual genes from the immunoglobulin superfamily, such as major and minor histocompatibility complex (MHC), female sex, and genetic variants of proteins that are the antigenic target of AITD (
Figure 2). Unfortunately, statistical studies of TC risk ignore immunogenetic aspects. Although HLA-DR8 and -DQB1*0302 are associated with atrophic thyroiditis, it is little understood why only in some people with a specific haplotype the antibodies block the TSH receptor, while in others (GD) they stimulate it. An environmental factor, such as tuberculosis infection, or perhaps medications, seems to be important.
An indirect evidence is the history of patient 3 i.e. with a predominance of the inflammatory process over tumorigenesis and hormonal stimuli. She was not diagnosed with tuberculosis, but with non-tuberculous mycobacteria (MOT). It is self-limiting infection in immunocompetent persons. Importantly: this patient had a very high TSH (
Table 1), although high TSH is considered a positive hormonal signal for carcinogenesis. This confirms the unique nature of immune-endocrine balance (
Figure 2). Furthermore, granulomatous destruction, such as de Quervain thyroiditis, is an extremely rare diagnosis. This disease requires not only antibody testing but also time-lapse observation (
Table 1) and the manifestations may be various. The clinical paradigm describes sustained inflammatory response and in AITD it may act as carcinogen. Of note, the rare disease such as de Quervain thyroiditis is not described in the TC context. Intrudingly, the in vitro study showed the specific reaction of TSA with TC cells [
40].
Interestingly, the observed nodules were not the initial state of oncogenesis, since among cancer-proven patients about 25% (5/19pts) were nodule-free and had smaller tumor size and earlier stage TC in comparison to patients without GD [
41]
3.3.3. Genetic Background and Immunity
Cassella’s team study [
42] indicated advantage of surgery (total thyroidectomy) contrary to radioactive iodine therapy in thyrotoxicosis (e.g. GD), but our observation (case 2) indicate the contrary overbalance in patients with probability of metastatic TC. On the other hand, the “radical” oncosurgery in NSCLC or TC gives opportunity for strict genetic diagnosis with individualized, patient-centered therapeutic regimen. This was missing in the described patients with short OS.
Our case report showed significant role of immunoendocrinopathy in the presentation and development of extra-thyroid TC. The BRAFV600E mutation shows a high specificity for PTC, especially the classic variant, whereas it was never found in follicular and medullary thyroid carcinoma or in benign thyroid neoplasms [
42] Latest finding showed the role of BRAFV600E mutation i.e. T > A (V600E), mutant allele frequency was significantly correlated with tumor size and extrathyroidal invasion without difference in pathological lymph node metastasis [
43]. It was linked to an increased risk of thyroid capsule penetration, recurrence, and concurrent mutations [
44]. Our retrospective analysis confirms the observation. Of note, most of literature data described lymphadenopathy as a sign of malignancy. Our patients without goiter, significant primary tumor (small nodules only) or lymphadenopathy were initially diagnosed by excision of metastatic focus and misdiagnosed as lung cancer in the clinical picture of these observations. In spite of early radioiodine therapy the recurrence was observed in our second patient. Our observation showed time-line with earlier overlooked and ignored symptoms of immune response against thyroid antigens (especially anti-TG). AITD with tissue destruction preceded the manifestation of cancer for a long time (2-3 years). Concomitant cachexia related to various mechanisms (tuberculosis, intense immune response, thyrotoxicosis and cancer) may be a valuable indicator because it is a final symptom of these overlapping processes. This is an important indicator for patients with autoimmune thyroiditis, but common interpretation of GD and TC incidence indicate the tumor promoting inflammatory mechanism as a paradigm. However, the negative correlation of GD with tumor size indicates defense forces immunity over tumorigenesis in the initial period of oncogenesis in patients with deep autoimmune process. (
Figure 2). It may be a local process only. The unique niche in the lungs (tumor, numerous bacteria and immunomodulatory microbiome)[
1,
2] creates good conditions for the development of TC elsewhere.
4. Materials and Methods
4.1. Material
The observational study comprised the history of 942 cancer patients described previously [
24]. Thus, the data from patients with mis-differentiation, without clinical and laboratory criteria (i.e. symptoms with microbiological and serological confirmation) were not included in the study. Consequently, most of patients were disqualified (
Figure 3).
Only patients diagnosed with well-documented autoimmunity (clinical criteria) and chronic (≥6 months) infection were included in an interview. The patients were a heterogeneous group of various stages and development of inflammatory and neoplastic processes. To exclude common inflammatory complications of cancer or chemotherapy we include only patients with previously diagnosed inflammatory disease.
Secondly, the patients with severe and systemic autoimmunity usually were treated with immunosuppressive drugs (e.g. corticosteroids). Therefore, the study yielded confusing results. Patients with local organ-specific autoimmunity were not subject to mandatory immunosuppressive therapy (e.g. autoimmune-thyroiditis). This allows, on one hand, to look for less disturbing immunotherapy (local antigens) and, on the other hand, to monitor the scale of the immune response with specific biochemical parameters.
4.2. Methods Time-Lapse Data Collection
We analyzed selected clinical parameters most representative of the three diseases (imaging, biochemical, serological tests) linking them to the parallel progression (progression/regression) of pathological processes and the impact on overall survival. The flow chart of the systematic clinical observation and data collection before and after transplantation was presented in
Figure 1.
5. Conclusions
Numerous statistical studies on the etiology of AITD and TC ignore infectious agents. The only exception is granulomatous (de Quervain) thyroiditis. The temporal association of AITD and TC with mycobacterial infections is quite rare in our observation (3 cases out of less than a thousand). In comparison with the prevalence of malignancy in nodular thyroiditis (4-5%) it may indicate a protective role of the inflammatory and autoimmune process and symptoms may be secondary to substances secreted by the tumor (TG) or may be a result of antibodies directed against tumors that cross-react with other tissue [
45]. In presented report, critical cachexia, autoimmunity and osteoarthropathy that preceded the discovery of the cancer by weeks to years [
45].
Despite numerous studies and statistical correlations, the described potential risk factors of TC coincide with the proposed factors responsible for the increase in all cancer incidence. However, medical intervention must be very careful due to bias (as presented here). The TC incidence growth may be a simple derivative of development and the number of performed procedures because, contrary to other autoimmune diseases, only AITD is treated surgically or with radioisotope. This, however, does not solve the problem of hidden oncogenesis, since TC rarely metastasizes to lymph nodes, and the lung is the first filter that gives an apparent image of NSCLC as in the presented report. And the standard should be strict and holistic diagnosis of all lung cancers in non-smokers, as it is with cancer of unknown origin [
46]. Unfortunately, the crucial gap is narrow observation of the chest: holistic approach and knowledge from various specialties are indispensable.
Author Contributions
P.Z. Conceptualization, collection and analyzing data, wrote the manuscript. He was a doctor treating patients, A.W. funding acquisition, histopathological examination.
Funding
This work was supported by the statutory activity of University and from private funds of the first author.
Acknowledgments
Many thanks to Janina Grycewicz for the linguistic proofreading and Marcin Tereszewski (native speaker) for final correction of our manuscript.
Conflicts of Interest
The author declares no conflict of interest.
Ethics approval and consent to participate
Not applicable: retrospective nature of the study.
Informed Consent Statement
Patient consent was waived due to retrospective analysis of 300 patient histories with anonymization of data. Written and informed contents were received from P1-P3 for the publication of the diagnostic chain.
References
- Zdziarski P: Paściak M, Gamian A. Microbiome Analysis and Pharmacovigilance After Inhaled Glucocorticoid: Oral Dysbiosis With the Isolation of Three Rothia Species and Subsequent Sjögren's Syndrome. Front Pharmacol. 2022;13:636180. Published 2022 Apr 1. [CrossRef]
- Zdziarski P, Wzorek A. Respiratory microbiota as a good predictor of outcome in humoral immunodeficiency. Methodological and conceptual difficulties in comprehensive microbiome analysis. Pol Merkur Lekarski. 2022;50(299):287-293.
- Zdziarski P. Veillonella atypica in tumor as a tripartite interaction: commensal - tumor - patient. Pol Merkur Lekarski. 2020 Dec 22;48(288):452-456.
- C. Cappelli, M. Braga, E.D. Martino, M. Castellano, E. Gandossi, B. Agosti, et al. Outcome of Patients Surgically Treated for Various Forms of Hyperthyroidism with Differentiated Thyroid Cancer: Experience at an Endocrine Center in Italy Surg Today, 36 (2) (2006), pp. 125-130.
- Gopinath C, Crow H, Panthi S, Bantis L, Burman KD, Choudhary C. Characteristics, staging and outcomes of differentiated thyroid cancer in patients with and without Graves' disease. J Clin Transl Endocrinol. 2023 Jul 26;33:100321. [CrossRef]
- Elisei R., Viola D., Torregrossa L., Giannini R., Romei C., Ugolini C., Molinaro E., Agate L., Biagini A., Lupi C., Valerio L., Materazzi G., Miccoli P., Piaggi P., Pinchera A., Vitti P., Basolo F. The BRAFV600E mutation is an independent, poor prognostic factor for the outcome of patients with low-risk intrathyroid papillary thyroid carcinoma: single-institution results from a large cohort study. J Clin Endocrinol Metab. 2012;97:4390–4398.
- Obołończyk Ł, Siekierska-Hellmann M, Wiśniewski P, Lewczuk A, Berendt-Obołończyk M, Lakomy A, Michalska Z, Radowska D, Moszkowska G, Bianek-Bodzak A, Sworczak K. Epidemiology, risk factors and prognosis of Interferon alpha induced thyroid disorders. A Prospective Clinical Study. Postepy Hig Med Dosw (Online). 2017 Sep 25;71(0):842-849. [CrossRef]
- Nikiforova MN , Kimura ET , Gandhi M , Biddinger PW , Knauf JA , Basolo F , Zhu Z , Giannini R , Salvatore G , Fusco A , Santoro M , Fagin JA , Nikiforov YE 2003 BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab 88 : 5399 – 5404.
- Zdziarski P, Gamian A, Dworacki G. A case report of lymphoid intestitial pneumonia in common variable immunodeficiency: Oligoclonal expansion of effector lymphocytes with preferential cytomegalovirus-specific immune response and lymphoproliferative disease promotion. Medicine (Baltimore). 2017 Jun;96(23):e7031. [CrossRef]
- Balinisteanu I, Panzaru MC, Caba L, Ungureanu MC, Florea A, Grigore AM, Gorduza EV. Cancer Predisposition Syndromes and Thyroid Cancer: Keys for a Short Two-Way Street. Biomedicines. 2023 Jul 29;11(8):2143. [CrossRef]
- Peng Q, Kong K, Tu Q, Wang Y, Wang X. The role of thyroid hormones in the differential diagnosis of tuberculous and parapneumonic pleural effusions. Am J Med Sci. 2022 Jun;363(6):495-501. [CrossRef]
- Pellegriti G., Mannarino C., Russo M., Terranova R., Marturano I., Vigneri R., Belfiore A. Increased Mortality in Patients With Differentiated Thyroid Cancer Associated With Graves’ Disease J Clin Endocrinol Metab, March 2013, 98(3):1014–1021 . [CrossRef]
- PellegritiG,BelfioreA,GiuffridaD,LupoL,VigneriR.Outcomeof differentiated thyroid cancer in Graves’ patients. J Clin Endocrinol Metab. 1998;83:2805–2809.
- Gabalec F, Srbova L, Nova M, Hovorkova E, Hornychova H, Jakubikova I, Ryska A, Cap J. Impact of Hashimoto's thyroiditis, TSH levels, and anti-thyroid antibody positivity on differentiated thyroid carcinoma incidence. Endokrynol Pol. 2016;67(1):48-53. [CrossRef]
- Anand A, Singh KR, Kushwaha JK, Hussain N, Sonkar AA. Papillary Thyroid Cancer and Hashimoto's Thyroiditis: An Association Less Understood. Indian J Surg Oncol. 2014 Sep;5(3):199-204. [CrossRef]
- Fröhlich E and Wahl R Thyroid Autoimmunity: Role of Anti-thyroid Antibodies in Thyroid and Extra-Thyroidal Diseases. Front. Immunol.2017; 8:521. [CrossRef]
- Gudmundsson J, et al. Discovery of common variants associated with low TSH levels and thyroid cancer risk. Nat. Genet. 2012;44:319–322. [CrossRef]
- Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, Beer DG, Powell CA, Riely GJ, Van Schil PE, Garg K, Austin JH, Asamura H, Rusch VW, Hirsch FR, Scagliotti G, Mitsudomi T, Huber RM, Ishikawa Y, Jett J, Sanchez-Cespedes M, Sculier JP, Takahashi T, Tsuboi M, Vansteenkiste J, Wistuba I, Yang PC, Aberle D, Brambilla C, Flieder D, Franklin W, Gazdar A, Gould M, Hasleton P, Henderson D, Johnson B, Johnson D, Kerr K, Kuriyama K, Lee JS, Miller VA, Petersen I, Roggli V, Rosell R, Saijo N, Thunnissen E, Tsao M, Yankelewitz D. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011 Feb;6(2):244-85. [CrossRef]
- Nam JK, Jung CK, Song BJ, Lim DJ, Chae BJ, Lee NS, Park WC, Kim JS, Jung SS, Bae JS. Is the BRAF(V600E) mutation useful as a predictor of preoperative risk in papillary thyroid cancer? Am J Surg. 2012 Apr;203(4):436-41. [CrossRef]
- Kargi A, Gurel D, Tuna B. The diagnostic value of TTF-1, CK 5/6, and p63 immunostaining in classification of lung carcinomas. Appl Immunohistochem Mol Morphol. 2007;15:415–420.
- Borowczyk M, Sypniewski M, Szyda J, et al. Genetic predisposition to differentiated thyroid cancer in the Polish population. Pol Arch Intern Med. 2024; 134: 16654. [CrossRef]
- Rossi G, Salmanton-García J, Cattaneo C, et al. Age, successive waves, immunization, and mortality in elderly COVID-19 hematological patients: EPICOVIDEHA findings. Int J Infect Dis. 2023;137:98-110. [CrossRef]
- Zdziarski P, Simon K, Majda J. Overuse of high stability antibiotics and its consequences in public and environmental health. Acta Microbiol Pol. 2003;52(1):5-13.
- Zdziarski P. [Importance of the Tumor Boards' decisions for the patientcentered care - case studies in the COVID-19 era]. Pol Merkur Lekarski. 2022 Apr 19;50(296):78-85.
- Bogović Crnčić T, Ilić Tomaš M, Girotto N, Grbac Ivanković S. Risk Factors for Thyroid Cancer: What Do We Know So Far?. Acta Clin Croat. 2020;59(Suppl 1):66-72. [CrossRef]
- Kholová I, Kalfert D, Lintusaari J, Rajakorpi E, Ludvíková M. Follicular Epithelial Dysplasia as Hashimoto Thyroiditis-Related Atypia: a Series of 91 Specimens. Endocr Pathol. 2021 Sep;32(3):368-374. [CrossRef]
- Anand A, Singh KR, Kushwaha JK, Hussain N, Sonkar AA. Papillary Thyroid Cancer and Hashimoto's Thyroiditis: An Association Less Understood. Indian J Surg Oncol. 2014 Sep;5(3):199-204. [CrossRef]
- Zdziarski P, Ricciardi L and Paganelli R Editorial: Case reports in respiratory pharmacology 2022. Front. Pharmacol. 2023; 14:1242273. [CrossRef]
- Casella C, Morandi R, Verrengia A, Galani A, Molfino S, Cuka D, Groppo G, Cappelli C, Portolani N. Thyroid Cancer and Nodules in Graves' Disease: A Single Center Experience. Endocr Metab Immune Disord Drug Targets. 2021;21(11):2028-2034. [CrossRef]
- Kaczka K, Mikosiński S, Fendler W, Celnik A, Pomorski L. Calcitonin and procalcitonin in patients with medullary thyroid cancer or bacterial infection. Adv Clin Exp Med. 2012 Mar-Apr;21(2):169-78. PMID: 23214280.
- Ali A. A Lump in the Throat: Thyroid Cancer. Medscape Drugs & Diseases. Updated September 13, 2024. Available at: https://reference.medscape.com/slideshow/thyroid-cancer-6006981?ecd=wnl_critimg_241004_mscpref_etid6878122&uac=103670FR&impID=6878122#1 Accessed October 8, 2024.
- Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013;2013:965212. [CrossRef]
- Vargas-Uricoechea, H., Bonelo-Perdomo, A., Sierra-Torres, C.H., Meza-Cabrera, I. (2016). Autoimmune Thyroid Disease (Flajani-Parry-Graves-von Basedow Disease): Etiopathogenesis, Clinical Manifestations and Diagnosis. In: Imam, S., Ahmad, S. (eds) Thyroid Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-25871-3_5.
- Płoski R, Szymański K, Bednarczuk T. The genetic basis of graves' disease. Curr Genomics. 2011 Dec;12(8):542-63. [CrossRef]
- -Skowronek I. IPEX Syndrome: Genetics and Treatment Options. Genes (Basel). 2021;12(3):323. Published 2021 Feb 24. [CrossRef]
- Rezzónico J. N., Rezzónico M., Pusiol E., Pitoia F., and Niepomniszcze H., Increased prevalence of insulin resistance in patients with differentiated thyroid carcinoma, Metabolic Syndrome and Related Disorders. (2009) 7, no. 4, 375–380, 2-s2.0-68549090727. [CrossRef]
- Wang J, Li X, Shen B, Wang S, He J and Wang Y (2022) The therapeutic effect of glucocorticoids on type II respiratory failure, heart failure, and massive pericardial effusion caused by hypothyroidism: A case report. Front. Pharmacol. 13:900701. [CrossRef]
- Wawrzynska L, Sakowicz A, Rudzinski P, Langfort R, Kurzyna M. The conversion of thyroxine to triiodothyronine in the lung: comparison of activity of type I iodothyronine 5' deiodinase in lung cancer with peripheral lung tissues. Monaldi Arch Chest Dis. 2003 Apr-Jun;59(2):140-5.
- Jara, L.J., Vera-Lastra, O., Medina, G. (2008). Atrophic Thyroiditis. In: Shoenfeld, Y., Cervera, R., Gershwin, M.E. (eds) Diagnostic Criteria in Autoimmune Diseases. Humana Press. https://doi.org/10.1007/978-1-60327-285-8_42.
- S. Filetti, A. Belfiore, S.M. Amir, G.H. Daniels, O. Ippolito, R. Vigneri, et al. The role of thyroid-stimulating antibodies of Graves' disease in differentiated thyroid cancerN Engl J Med, 318 (12) (1988), pp. 753-759.
- Casella C, Morandi R, Verrengia A, Galani A, Molfino S, Cuka D, Groppo G, Cappelli C, Portolani N. Thyroid Cancer and Nodules in Graves' Disease: A Single Center Experience. Endocr Metab Immune Disord Drug Targets. 2021;21(11):2028-2034. [CrossRef]
- Nam JK, Jung CK, Song BJ, Lim DJ, Chae BJ, Lee NS, Park WC, Kim JS, Jung SS, Bae JS. Is the BRAF(V600E) mutation useful as a predictor of preoperative risk in papillary thyroid cancer? Am J Surg. 2012 Apr;203(4):436-41. [CrossRef]
- Cheng SP, Hsu YC, Liu CL, Liu TP, Chien MN, Wang TY, Lee JJ. Significance of allelic percentage of BRAF c.1799T > A (V600E) mutation in papillary thyroid carcinoma. Ann Surg Oncol. 2014 Dec;21 Suppl 4:S619-26. [CrossRef]
- Huang J, Wang J, Xv J, Wang J, Wang G, Zhao Y. Genetic alterations and allele frequency of BRAF V600E and TERT mutation in papillary thyroid carcinoma with intermediate-to-high recurrence risk: a retrospective study. Clin Exp Med. 2024 Apr 12;24(1):76. [CrossRef]
- Gale RP. Paraneoplastic syndromes. Merck Manual Professional Version, Sep 2024. Accessed September 01, 2024. https://www.merckmanuals.com/professional/hematology-and-oncology/overview-of-cancer/paraneoplastic-syndromes?query=paraneoplastic%20syndromes%20cancer.
- Gale RP. Metastatic Carcinoma of Unknown Primary Origin. Merck Manual Professional Version, Sep 2024. Accessed September 01, 2024. https://www.merckmanuals.com/professional/hematology-and-oncology/overview-of-cancer/metastatic-carcinoma-of-unknown-primary-origin?query=cancer%20unknown%20origin.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).