1. Introduction
Managing cow's milk protein allergy (CMPA) involves strict avoidance of cow's milk protein and related products while ensuring adequate nutrition, typically achieved through specialised infant formulas. These include extensively hydrolyzed cow milk proteins formulas (EHF), amino acid formulas (AAF), hydrolysed rice formulas (HRF) or soy infant formulas (SF). While EHFs are often the first choice for CMPA management, HRF are recently emerging as alternatives. AAF are reserved for more severe cases or in infants with impaired nutritional status, anaphylaxis and eosinophilic esophagitis [
1]. Likewise, SF may also be considered as an alternative, especially for economic, cultural and palatability reasons. However, using SF is not recommended in Europe especially in infants below six months of age due to the risk of co-allergy and to the potential presence of phytoestrogens [
1,
2,
3,
4,
5,
6].
Acquiring tolerance to cow’s milk proteins (CMP) is also an important goal in CMPA management influenced by several factors such as the type of allergy (IgE vs. non-IgE mediated), the sensitizing protein(s) (casein vs. whey proteins) and the degree of sensitization. For these reasons, strategies have been developed to accelerate the acquisition of tolerance [
7]. Terracciano et al. found that infants and children with CMPA receiving HRF or SF achieved tolerance earlier than their peers fed EHFs [
8]. However, randomised controlled trials comparing HRF to EHF in terms of growth, tolerance and safety are lacking [
1].
Although HRF has demonstrated good tolerance in infants with CMPA[
9,
10], concerns persist regarding the low protein quality of rice-based formulas potentially impacting growth [
9,
10], as well as regarding the arsenic content of rice that may be present in HRF [
11].
The present study was initiated to compare outcomes between infants with CMPA fed with HRF and those fed with an EHF. The primary objective was to compare growth at 6, 9 and 12 months between the two randomised groups. Secondary objectives were to evaluate anthropometrics, protein status, safety, acquisition of tolerance to CMP and the risk of arsenic exposure.
2. Materials and Methods
2.1. Study Design
This multicentre prospective, randomised, double-blind trial was performed from 2014 to 2019 across six hospital paediatric clinics in Spain, France, and Belgium. Infants under 10 months old with confirmed diagnosis of CMPA were randomly assigned to receive HRF or EHF for 12 months. Data were collected using an electronic case report form completed by each investigator. The design of the study is illustrated in
Supplementary Figure S1
2.2. Study Population
Infants younger than 10 months old with confirmed CMP allergy diagnosed within two months prior to baseline (up to Grade II anaphylaxis [
12]) were eligible. Diagnosis required a positive challenge on the Double-Blind Placebo-Control Food Challenge (DBPCFC) [
13] with cow’s milk, positive specific IgE for CMP (alpha-lactalbumin, beta-lactoglobulin casein or whole milk) or the Milk Atopy Patch Test [
14].
Additional inclusion criteria were singleton birth, gestational age from 37 to 42 weeks, birth weight ≥2.500 g, and Apgar score >7 at 5 minutes post-partum. Written informed consent from parents or guardians was mandatory.
Exclusion criteria were infants with previous signs of allergy to any EHF, with a confirmed history of acute severe potentially life-threatening allergic reaction after isolated accidental ingestion of cow’s milk (Grade III or higher), with a daily formula intake less than 100 ml, the presence of major congenital malformations or neonatal diseases, severe concurrent or chronic diseases, intrauterine growth retardation, or neonatal infections. Breastfeeding was not an exclusion criterion.
Infants involved in other trials, with missing parental written informed consent, unable to adhere to the protocol, or exhibiting clinically relevant liver, kidney, or hematological abnormalities were also excluded.
2.3. Investigational Products
The HRF (this formula was commercialised under two brand names: Blemil Plus® hydrolysed rice, Laboratorios Ordesa and Modilac Riz®, Laboratoires Modilac) was developed for the dietary management of CMPA. It contains 100% partially hydrolysed rice protein supplemented with lysine and tryptophan in compliance with Directive 2006/141/EC. The EHF (Blemil Plus FH®; Laboratorios Ordesa) consisted of an extensively hydrolysed casein derived from cow’s milk. The composition of the formulas complied with requirements defined in European legislation (DE 2006/141/EC) at the time of the study.
To ensure blinding, investigational products were provided in identical packaging, with only the batch number and expiry date. Investigators, support staff and the infants’ families were blinded to the product's identity, known only to the Clinical Research Organisation or study sponsor representative. Sealed envelopes (code breaks) containing randomisation assignments were provided to the Principal Investigator at each site. The code could only be broken in case of serious adverse events requiring the principal investigator to initiate an appropriate treatment. Investigators and study staff remained blinded to study treatment assignments until the statistical analysis was complete.
2.4. Study Procedures
Eligible infants were consecutively enrolled and randomized in a 1:1 ratio to one of the two treatment arms. Parents were given diaries to record formula intake, tolerance, stool frequency/consistency, and adverse events. At Visit 0, infants were randomly assigned to one of the two treatment arms but underwent a three-week elimination diet and did not start the allocated formula until a positive DBPCFC was confirmed at Visit 1. If the test was negative, the infant was withdrawn from the study. The remaining infants started their allocated formula at Visit 1. In cases of formula intolerance, infants were withdrawn from the study. Data were collected during follow-up visits 2 to 7 (at 1, 2, 3, 6, 9 and 12 months), including a full clinical assessment, anthropometric data, adverse events and concomitant medications. (
Supplementary Figure S1). An open Oral Food Challenge (OFC) was performed at Visits 5, 6 and 7. Infants with negative OFC result were switched to standard formula and were followed until study completion. Urine and hair samples were taken at visits 0, 3 and 7 and blood samples at visits 0, 3, 5, 6 and 7. Urine and hair samples were obtained only from children exclusively or predominantly formula-fed.
2.5. Study Variables
Length (cm) and weight (kg) were measured at Visits 5, 6, and 7, and the length-for-weight ratio was calculated. The primary outcome measure was the change from baseline over the study period in weight to height/length expressed as a Z-score.
Secondary anthropometric outcome measures included change from baseline in height and weight, change from baseline in head circumference (cm), triceps skin fold thickness (mm), mid-arm circumference (cm), arm muscle area (cm²) and BMI. Anthropometric measures were determined as absolute number or Z-scores. Reference values were obtained from the WHO MGRS study score [
15], except for head circumference, for which Z-scores were calculated using 1990 British growth reference values [
16].
Blood samples were drawn from all infants to determine specific IgEs for CMP (Specific IgE CAP test Thermofisher®), IgG, IgA, IgM, haemoglobin and haematocrit, alanine aminotransferase, urea, creatinine, albumin, ferritin and plasma amino acids. Urine samples were taken to measure creatinine, total and inorganic arsenic. Hair samples were taken to measure total arsenic, which was determined by the Institute of Agrochemistry and Food Technology (IATA) in Valencia, Spain.
Acquisition of tolerance was defined by a negative OFC and subsequent tolerance to standard cow’s milk. Time to acquisition of tolerance was defined as the time between visit 1 and the switch to a cow’s milk formula. The cumulative number of infants who acquired tolerance was documented in 3 time periods during the follow-up period, at 6, 9 and 12 months (i.e. when the OFC was performed). The infant’s age at acquisition of tolerance was documented for 77 children.
Digestive symptoms (including number of stools, regurgitations or episodes of colic) were identified from the parent diaries and were calculated for each between-visit interval.
All adverse events (AE) were documented by the investigators and listed by system-organ class and preferred term according to the MedDRA glossary (Version 26.1). These AEs were classified as serious or non-serious, and potentially related or unrelated to the study formulas.
2.6. Statistical Analyses
Data were analysed on and intent-to-treat (ITT) basis. The ITT population included all subjects, regardless of whether they satisfied the entry criteria, the treatment received, and subsequent withdrawal or deviation from the protocol. Missing data at individual time points were not replaced. Demographic data at baseline were summarized using mean values with standard deviation, or median values with range for continuous variables and frequency counts and percentages for categorical variables. Accepting an alpha risk of 0.05 and a power of 0.8 in a two-sided test 53 subjects are necessary in the first group and 53 in the second group to recognize statistically significant a difference greater than or equal to 1 units. The common standard deviation is assumed to be 1 and the correlation coefficient between the initial and the final measurement is assumed to be 0.005. A drop-out rate of 40% has been anticipated. The primary outcome variables (change from baseline in Z-scores) were compared between study arms using mixed models as random intercept models, random slope models and quadratic-order polynomial models as appropriate for the individual endpoint. Anthropometric parameter analysis was conducted as a worst-case scenario, excluding individuals with a negative OFC test at 9 and 12 months.
For the longitudinal models for secondary endpoints (triceps fold thickness, mid arm circumference, and arm muscle area), the time variable was corrected using “centered age” (age minus baseline mean age) because child growth is expected to be age dependent.
Tolerance acquisition was evaluated by Kaplan-Meier survival analysis and compared between groups using a Cox proportional hazard model. For episodes of colic and regurgitations, an ordinal logistic regression model was fitted with number of colics and regurgitations as dependent variable and visit and group as explanatory variables. Two-tailed
t-tests and 95% confidence intervals were used for comparing number of stools at 6, 9 and 12 months. One-tailed
t-tests and 95% confidence intervals were used for comparing arsenic levels in the population. Patients lost to follow-up were considered as still allergic at the end of the study (worst-case scenario). Statistical analyses were performed using Stata Statistical Software (Version 17) [
17].
3. Results
One hundred seventeen infants were enrolled and randomly assigned one of the study formulas. After randomisation, parents of 6 infants refused to participate and 4 didn't meet the requirements of clinical trial protocol. During the run-in period between baseline (V1) and visit V2, DBPCFC was performed to all patients. 5 infants with DBPCFC(-) and 1 with a severe reaction to study formula during DBPCFC were withdrawn from the trial.
One hundred and five infants were included in the intention-to-treat analysis (50 assigned to HRF group and 55 assigned to EHF group) at baseline visit. Eighty-six infants completed the 6-month visit, 79 completed the 9-month visit and 69 completed the final study visit at 12 months (Supplemementary
Figure S2). The baseline characteristics of the study population are presented in
Table 1.
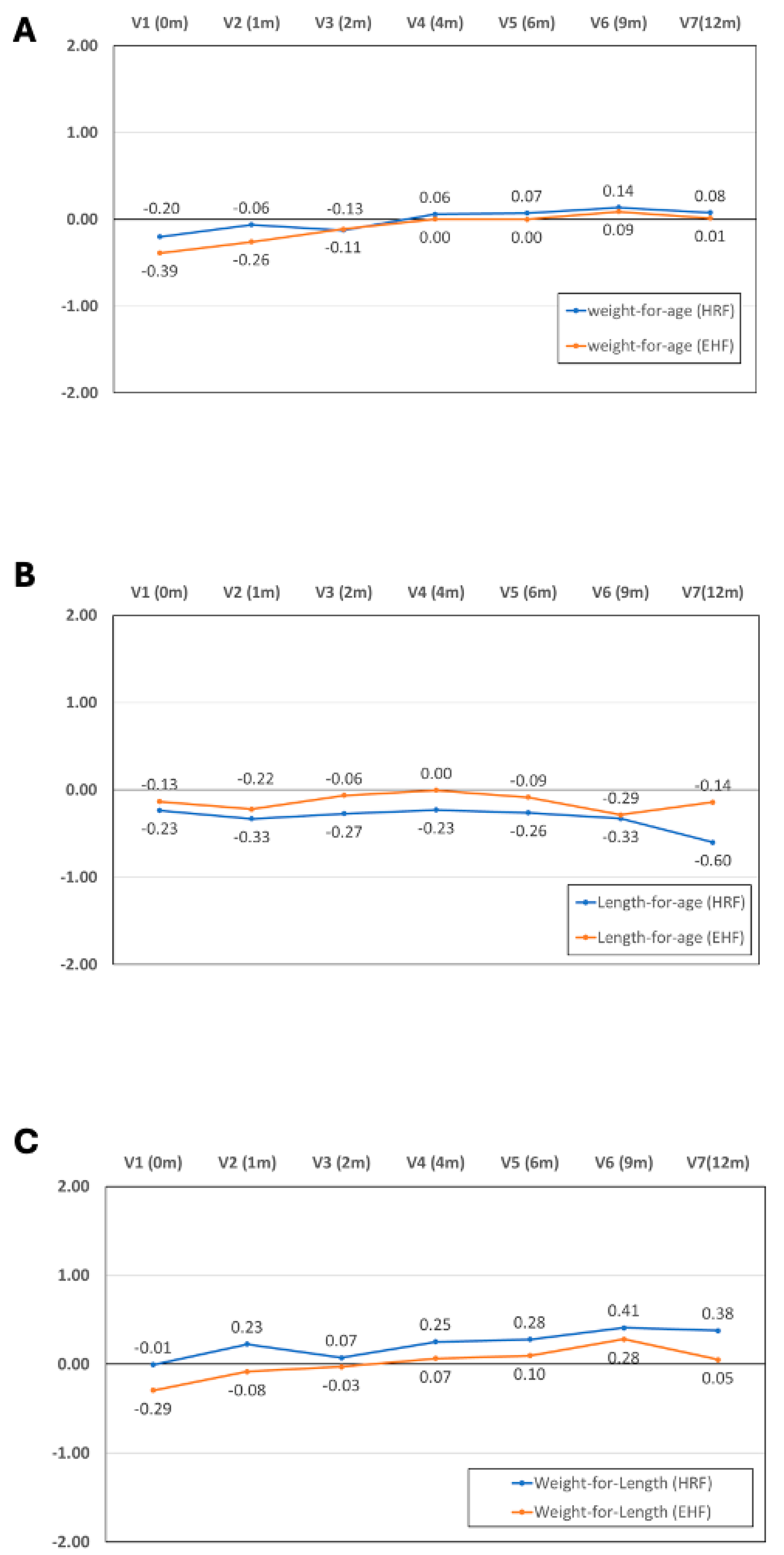
3.1. Primary Outcome Measure
The Z-score for weight for length ratio increased significantly over the course of the study in both treatment arms (p = 0.001 for visit effect between baseline and 12 months in both groups). No significant difference in Z-score was observed between the two study groups (p = 0.28) and “no visit × group” interaction was observed (p = 0.52). Similar patterns were observed for both components of the primary outcome measure: for weight Z-score, the visit effect was significant (p <0.001), but not the group effect (p = 0.69) or the “visit × group” interaction (p = 0.86). For length Z-score, the visit effect was significant (p =0.04), but not the group effect (p = 0.64) or the “visit × group” interaction (p = 0.14). No size effect or very small size effects were found out for all primary endpoints and visits (At 12 month, Cohen’s d=0.015 for weight Z-score, d= 0.24 for length Z-score, and d=0.13 for weight-for-length Z score). A mixed-effect model was conducted to quantify changes in weight and length trajectories at 12 month of follow-up adjusting for covariates such as type of formula, visit, and IgE (mediated/non-mediated). In both analysis, there were not significant effect of type of formula and IgE, but the visit effect was significant.
Changes over time for Z-scores for weight, length and weight for length ratio are presented in
Figure 1. Full data on all anthropometric parameters and sample size that allowed the Z score calculations are presented by study visit in supplementary
Table 1.
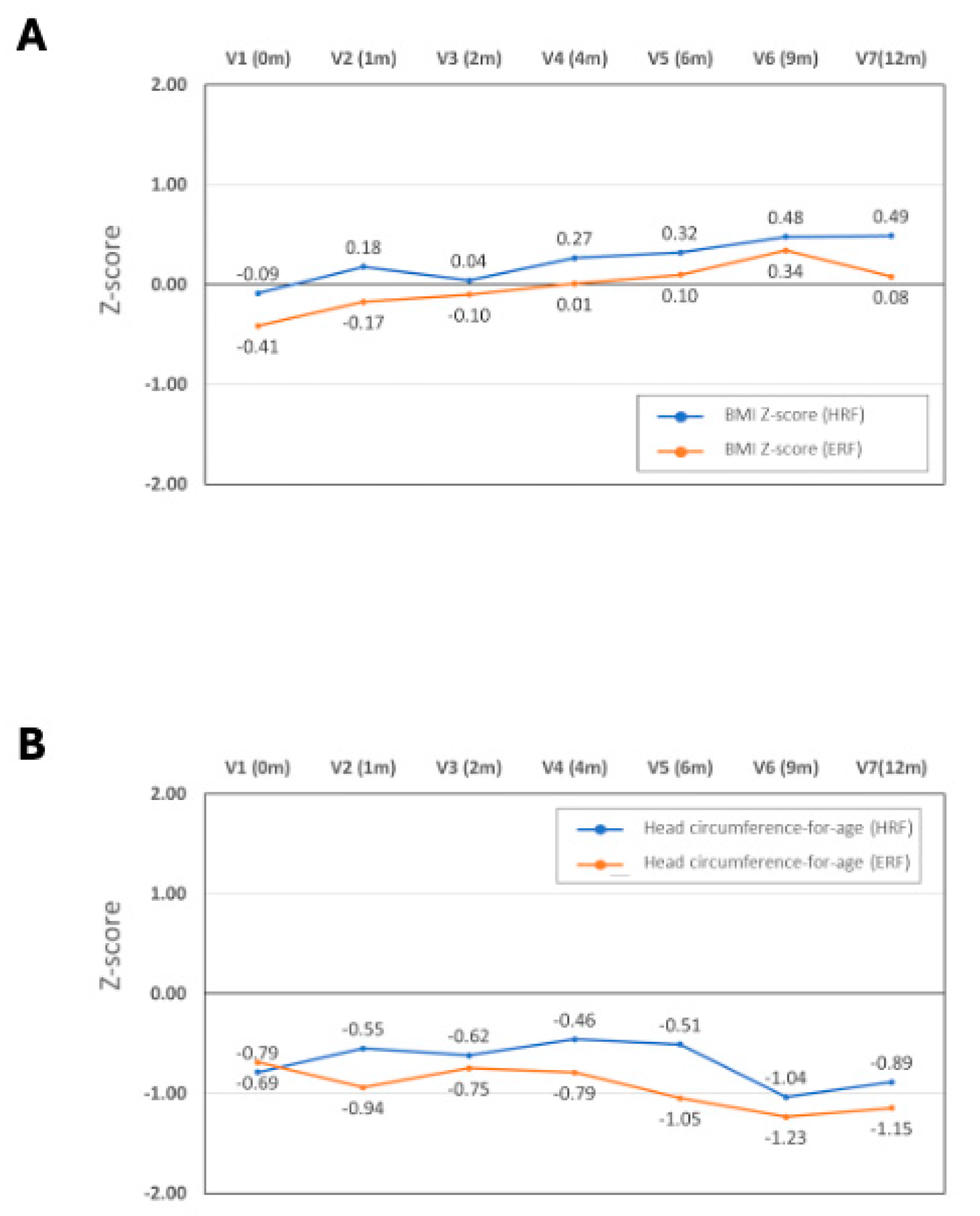
3.2. Secondary Anthropometric Outcome Measures
For BMI Z-score, the visit effect was significant (p <0.0001), but not the group effect (p = 0.22) or the “visit × group” interaction (p = 0.11). For head circumference, no significant visit effect (p = 0.17), group effect (p = 0.49) or the “visit × group” interaction (p = 0.90) were observed. The distributions of Z-scores for BMI and head circumference across study visits are presented in
Figure 2.
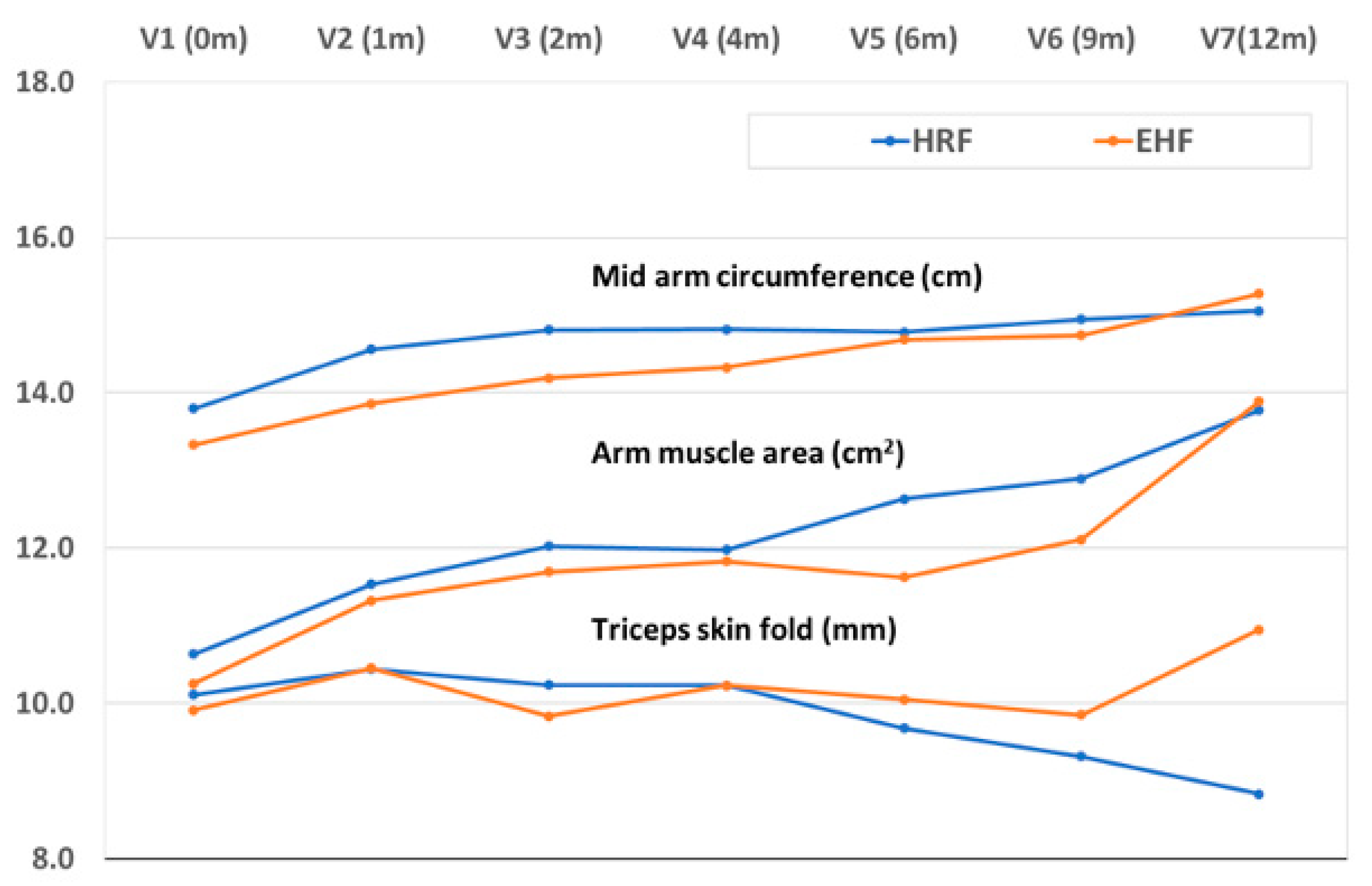
No size effect or very small size effects were found out for all secondary endpoints and visits (At 12 month, Cohen’s d=0.48 for BMI) In addition, the effect group and “age x group” interaction were not significant in mid arm circumference (p=0.206, p=0.088), arm muscle area (p=0.893, p=0.991) nor triceps skin fold (p=0.452, p=0.088, respectively) during the follow-up and a significant effect of age were observed in mid arm circumference (p <0.001), arm muscle area (p<0.001) but not in triceps skin fold (p=0.309) (
Figure 3).
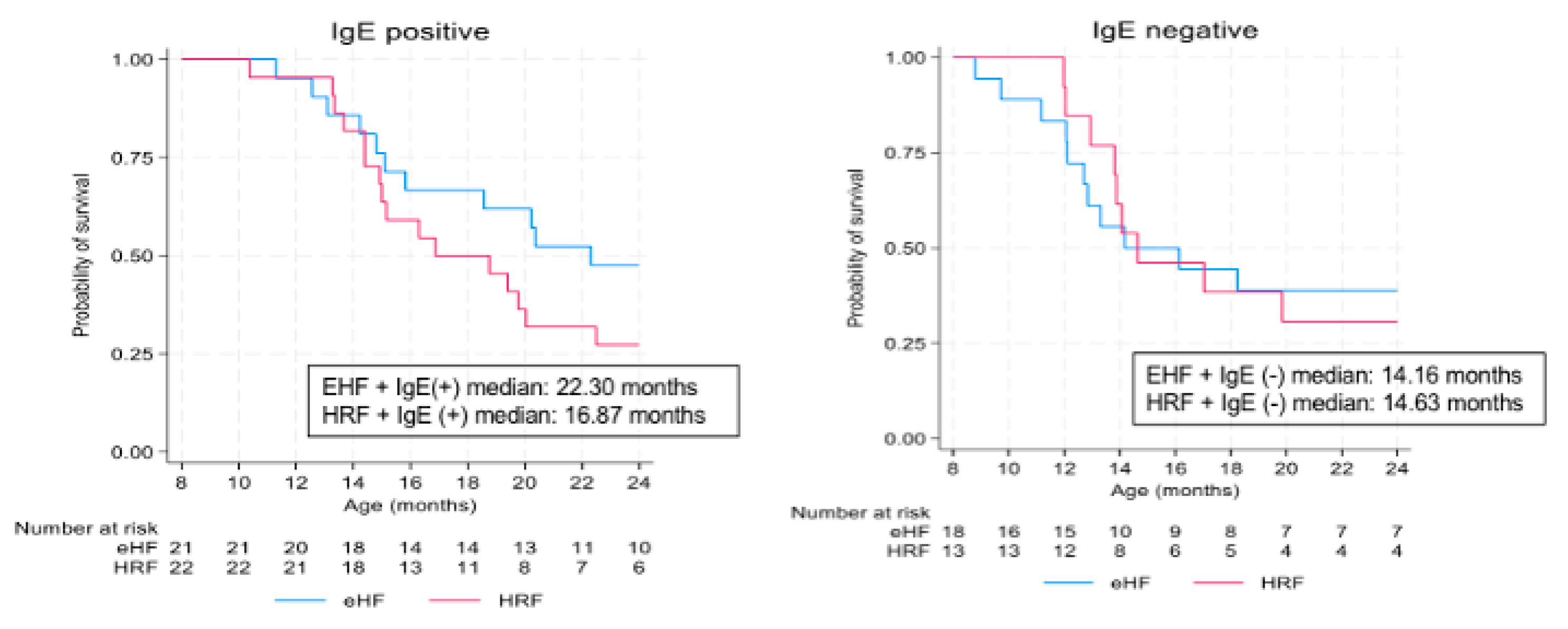
3.3. Tolerance to Cow’s Milk Proteins
During the follow-up period, tolerance to CMP was documented in the 77 infants with reported age values (36 in the HRF group and 41 in the EHF group). No significant difference was observed in the proportion of infants acquiring tolerance: 26/36 infants (72.2%) in the HRF group and 22/41(53.7%) in the EHF group (p = 0.09; χ² test). Kaplan-Meier survival curves for tolerance acquisition of are presented in
Figure 4.
Time to tolerance acquisition did not differ significantly between the two study groups (9.7 months after V1 in the HRF group and 13.8 months in the EHF group; p = 0.18; logrank test). The median age at tolerance acquisition was 16.3 months in the HRF group and 20.4 months in the EHF group (p = 0.18; Logrank test). At the end of the follow-up (12-month), similar proportion of infants in the HRF group acquired CMP tolerance compared to the EHF group: 72.2% in the HRF group and 53.7% in the EHF group (p = 0.09; χ² test) with a median time to tolerance acquisition of 10-14 months after starting HRF or EHF, corresponding to an age of 16 – 20 months. Regarding the type of cow's milk protein allergy, there were differences, though not statistically significant. In patients with IgE-mediated CMPA, tolerance was achieved earlier in the group treated with HRF (
Figure 5).
3.4. Digestive Tolerance
Digestive tolerance was assessed by the evaluation of the number of stools, regurgitations and episodes of colic. No differences were seen between study groups and between baseline and each time points. Overall, there were no differences between groups for colics (p=0.97) or regurgitations (p=0.506).
3.5. Arsenic
The presence of arsenic was evaluated using hair and urine samples in both groups of patients at baseline, V3 and V7. Arsenic concentrations were low for both formulas. In hair, total arsenic concentrations were <0.07 mg/kg in all samples from both groups. The median arsenic concentration in urine was similar between groups, 2.24 [95%CI: 1.79 – 3.13] µg/L in the HRF group vs 2.3 [95%CI: 1.56 – 2.63] µg/l in the EHF group (p = 0.48; Wilcoxon test).
3.6. Adverse Events
Sixteen serious AEs were reported in both groups, occurring in 3 infants in the HRF group and 4 infants in the EHF group. None of these AEs were deemed related to the study treatment by the investigators. Fifteen of these events were classified as severe since they required hospitalisation, but all serious AEs resolved satisfactorily (
Supplementary Table S2).
One infant in the EHF group exhibited clinical intolerance to the product, as evidenced by an immediate reaction, whereas no infants showed allergic reaction to the HRF. Additionally, the frequency of reported adverse events (AEs) was comparable between the two groups.
Twenty-nine adverse events considered potentially related to the product were reported by 15 patients (
Supplementary Table S3). None of the events were considered as severe. Details of the 29 potentially related AEs are presented in
Supplementary Table S4.
4. Discussion
This study showed that infants in both the HRF and EHF groups exhibited normal growth over the 12-month follow-up period, with no significant differences in anthropometric measures. This challenges previous suggestions that rice formulas might lead to suboptimal growth compared to cow's milk or breast milk [
18,
19] but is consistent with other reports where infants fed HRF showed similar growth parameters to EHF [
3,
9]. Recent guidelines consider HRF equivalent to EHF for feeding infants with CMPA [
1,
20]. Moreover, the results of this study confirmed the ability of a HRF to sustain normal growth, as shown in previous studies in healthy infants [
21,
22]. The nutritional quality of rice proteins is suitable for use in infant formulas since it is supplemented in certain amino acids that may be lacking in rice, typically lysine, threonine and tryptophan [
10].
Acquisition of tolerance is an important milestone in the outcome of children with CMPA, and is observed between the ages of 3 to 4 years in 80% of children in the majority of previous studied [
23]. In the current study, acquisition of tolerance appeared for more than half the infants before two years age, which suggests that avoiding CMP entirely in favour of HRF formulas might facilitate earlier tolerance acquisition. These results can be compared with previous observations from a randomised and prospective study [
7], which found, that infants and children with CMPA who had received HRF or a SF for the dietary management of their condition achieved tolerance significantly earlier than their peers receiving EHF. These findings align with prior research by Terracciano et al [
8], indicating that infants and children managed with HRF or a SF achieved CMPA tolerance earlier than those receiving EHF.
Safety analysis showed comparable rates of adverse events in both groups, predominantly consisting of expected infant issues unrelated to treatment, such as fever and cough. None of the sixteen serious adverse events reported in this study was considered related to the product. Digestive tolerance, regurgitations and colic episodes, did not differ between groups. Stool frequency and the incidence of colic remained stable over the study period, while the frequency of regurgitations decreased with age. These safety findings mirror those of previous research [
9]. Arsenic exposure was low and comparable in both formulas, meeting safety thresholds [
11,
24,
25] and results are comparable with those documented by Reche et al [
9].
The strengths of the study include its double-blind, randomised controlled design and confirmation of CMPA with double-blind OFC. Limitations include the relatively small sample size and the enrolment of infants at a relatively older age, potentially influenced by prior infant formula consumption.
In conclusion, this study confirms that HRF can be used as a first line alternative to cow’s milk for feeding infants with CMPA, resulting in normal growth, acquisition of tolerance, and no clinically relevant safety issues compared to the EHF formula.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Figure S1: Study design.; Figure S2: Patient flow diagram; Table S1: Anthropometric data by study visit; Table S2: Severe adverse events; Table S3: Adverse events related to the formula; Table S4: Details of adverse events (AE) by formula.
Author Contributions
Conceptualization, A.L., A.N.G., Á.M., and V.M.N.-L.; methodology, A.L., A.N.G., Á.M., and V.M.N.-L.; formal analysis, A.L., H.S., D.S., N.K.; investigation, A.N.G., M.N.C., B.E., Á.M., H.S., D.S., N.K., V.M.N.-L.; resources, R.D-C.M.; data curation, R.d.C.S.; writing—original draft preparation, J.D.O. and R.d.C.S.; writing—review and editing, A.L., A.N.G., B.E., Á.M., H.S., D.S., N.K.,J.D.O.; R.d.C.S. and V.M.N.-L.; project administration, R.d.C.S.; funding acquisition, R.d.C.S..
Funding
This study was funded by Modilac Laboratory (France) and Ordesa Laboratory (Spain). Role of Funder: Laboratoires Modilac (France) and Laboratorios Ordesa (Spain) initiated the study, were responsible for data collection and coordinated the analysis. They brought together a scientific committee of pediatricians to advise on the design of the study, data collection and analyses and on the interpretation of the results.
Institutional Review Board Statement
The study was performed according to all relevant international and national legislation, and according to the ICH E6 Guidelines for Good Clinical Practice. The study was approved by the Ethics Committee of all participating centres, and written informed consent was obtained from each infant´s parents or guardian. This study is listed on clinicaltrials.gov with identifier NCT02405923.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Conflicts of Interest
A-L: none to declare. A.N.G.: none to declare. M.N.C: none to declare. B.E.: has received honoraria for lectures from Alter, Mead Johnson, Ferrer, Nestle, Nutricia/Danone, Hero and Abbott, and has participated in advisory boards for Mead Johnson, Nutricia/Danone, Ferrer and Abbott. A.M.: none to declare. H.S.: is an employee of Laboratoires Modilac (France) which co-funded the study. D.S.: none to declare. N.K: Study honorarium and presentation with conferences expenses Laboratory of Modilac France, Laboratory of NIH, France, Laboratory of Nutricia, France, Laboratory of Dr Falk, France. J.D.O.: was an employee of Laboratorios Ordesa (Spain) which co-funded the study. R.d.C.S.: is an employee of Ordesa Laboratory (Spain) which co-funded the study. V.M.N.L.: has received honoraria for lectures from Mead Johnson, Ferrer, Nestle, Nutricia/Danone, Hero and Abbott
References
- Vandenplas, Y.; Broekaert, I.; Domellöf, M.; Indrio, F.; Lapillonne, A.; Pienar, C.; Ribes-Koninckx, C.; Shamir, R.; Szajewska, H.; Thapar, N.; et al. An ESPGHAN Position Paper on the Diagnosis, Management, and Prevention of Cow’s Milk Allergy. J. Pediatr. Gastroenterol. Nutr. 2024, 78, 386–413. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Castrellon, P.G.; Rivas, R.; Gutiérrez, C.J.; Garcia, L.D.; Jimenez, J.E.; Anzo, A.; Hegar, B.; Alarcon, P. Safety of Soya-Based Infant Formulas in Children. Br. J. Nutr. 2014, 111, 1340–1360. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, C.; Fiocchi, A.; Riva, E.; Terracciano, L.; Sarratud, T.; Martelli, A.; Lodi, F.; D’Auria, E.; Zuccotti, G.; Giovannini, M. Growth of Infants with IgE-Mediated Cow’s Milk Allergy Fed Different Formulas in the Complementary Feeding Period. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2007, 18, 599–606. [Google Scholar] [CrossRef]
- Klemola, T.; Vanto, T.; Juntunen-Backman, K.; Kalimo, K.; Korpela, R.; Varjonen, E. Allergy to Soy Formula and to Extensively Hydrolyzed Whey Formula in Infants with Cow’s Milk Allergy: A Prospective, Randomized Study with a Follow-up to the Age of 2 Years. J. Pediatr. 2002, 140, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Zeiger, R.S.; Sampson, H.A.; Bock, S.A.; Burks, A.W.; Harden, K.; Noone, S.; Martin, D.; Leung, S.; Wilson, G. Soy Allergy in Infants and Children with IgE-Associated Cow’s Milk Allergy. J. Pediatr. 1999, 134, 614–622. [Google Scholar] [CrossRef]
- Bhatia, J.; Greer, F. ; American Academy of Pediatrics Committee on Nutrition Use of Soy Protein-Based Formulas in Infant Feeding. Pediatrics 2008, 121, 1062–1068. [Google Scholar] [CrossRef]
- Schoemaker, A.A.; Sprikkelman, A.B.; Grimshaw, K.E.; Roberts, G.; Grabenhenrich, L.; Rosenfeld, L.; Siegert, S.; Dubakiene, R.; Rudzeviciene, O.; Reche, M.; et al. Incidence and Natural History of Challenge-Proven Cow’s Milk Allergy in European Children--EuroPrevall Birth Cohort. Allergy 2015, 70, 963–972. [Google Scholar] [CrossRef]
- Terracciano, L.; Bouygue, G.R.; Sarratud, T.; Veglia, F.; Martelli, A.; Fiocchi, A. Impact of Dietary Regimen on the Duration of Cow’s Milk Allergy: A Random Allocation Study. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2010, 40, 637–642. [Google Scholar] [CrossRef]
- Reche, M.; Pascual, C.; Fiandor, A.; Polanco, I.; Rivero-Urgell, M.; Chifre, R.; Johnston, S.; Martín-Esteban, M. The Effect of a Partially Hydrolysed Formula Based on Rice Protein in the Treatment of Infants with Cow’s Milk Protein Allergy. Pediatr. Allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2010, 21, 577–585. [Google Scholar] [CrossRef]
- Dupont, C.; Bocquet, A.; Tomé, D.; Bernard, M.; Campeotto, F.; Dumond, P.; Essex, A.; Frelut, M.-L.; Guénard-Bilbault, L.; Lack, G.; et al. Hydrolyzed Rice Protein-Based Formulas, a Vegetal Alternative in Cow’s Milk Allergy. Nutrients 2020, 12, 2654. [Google Scholar] [CrossRef]
- Hojsak, I.; Braegger, C.; Bronsky, J.; Campoy, C.; Colomb, V.; Decsi, T.; Domellöf, M.; Fewtrell, M.; Mis, N.F.; Mihatsch, W.; et al. Arsenic in Rice: A Cause for Concern. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Sampson, H.A. Anaphylaxis and Emergency Treatment. Pediatrics 2003, 111, 1601–1608. [Google Scholar] [PubMed]
- Bock, S.A.; Sampson, H.A.; Atkins, F.M.; Zeiger, R.S.; Lehrer, S.; Sachs, M.; Bush, R.K.; Metcalfe, D.D. Double-Blind, Placebo-Controlled Food Challenge (DBPCFC) as an Office Procedure: A Manual. J. Allergy Clin. Immunol. 1988, 82, 986–997. [Google Scholar] [CrossRef] [PubMed]
- Turjanmaa, K. “Atopy Patch Tests” in the Diagnosis of Delayed Food Hypersensitivity. Allerg. Immunol. (Leipz.) 2002, 34, 95–97. [Google Scholar]
- WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development 2006.
- Cole, T.J.; Freeman, J.V.; Preece, M.A. British 1990 Growth Reference Centiles for Weight, Height, Body Mass Index and Head Circumference Fitted by Maximum Penalized Likelihood. Stat. Med. 1998, 17, 407–429. [Google Scholar]
- Stata Press StataCorp. Stata 17 Base Reference Manual. 2021.
- Keller, M.D.; Shuker, M.; Heimall, J.; Cianferoni, A. Severe Malnutrition Resulting from Use of Rice Milk in Food Elimination Diets for Atopic Dermatitis. Isr. Med. Assoc. J. IMAJ 2012, 14, 40–42. [Google Scholar]
- Savino, F.; Castagno, E.; Monti, G.; Serraino, P.; Peltran, A.; Oggero, R.; Fanaro, S.; Vigi, V.; Silvestro, L. Z-score of Weight for Age of Infants with Atopic Dermatitis and Cow’s Milk Allergy Fed with a Rice-hydrolysate Formula during the First Two Years of Life. Acta Paediatr. 2005, 94, 115–119. [Google Scholar] [CrossRef]
- Fiocchi, A.; Bognanni, A.; Brożek, J.; Ebisawa, M.; Schünemann, H. ; WAO DRACMA guideline group World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines Update - I - Plan and Definitions. World Allergy Organ. J. 2022, 15, 100609. [Google Scholar] [CrossRef]
- Girardet, J.-P.; Rivero, M.; Orbegozo, J.; David, T.; Boulanger, S.; Moisson de Vaux, A.; Johnston, S.; Marin, V. [Growth and tolerance in infants fed an infant formula based on hydrolyzed rice proteins]. Arch. Pediatr. Organe Off. Soc. Francaise Pediatr. 2013, 20, 323–328. [Google Scholar] [CrossRef]
- Lasekan, J.B.; Koo, W.W.K.; Walters, J.; Neylan, M.; Luebbers, S. Growth, Tolerance and Biochemical Measures in Healthy Infants Fed a Partially Hydrolyzed Rice Protein-Based Formula: A Randomized, Blinded, Prospective Trial. J. Am. Coll. Nutr. 2006, 25, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Fiocchi, A.; Schünemann, H.J.; Brozek, J.; Restani, P.; Beyer, K.; Troncone, R.; Martelli, A.; Terracciano, L.; Bahna, S.L.; Rancé, F.; et al. Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA): A Summary Report. J. Allergy Clin. Immunol. 2010, 126, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Scientific Opinion on Arsenic in Food. EFSA J. 2009. [CrossRef]
- European Commission Publication Office. Commission Regulation (EU) 2023/915 of on Maximum Levels for Certain Contaminants in Food and Repealing Regulation (EC) No 1881/2006. 2023. 25 April.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).