1. Introduction
Rehabilitation is a crucial aspect of healthcare for managing both acute and chronic conditions. It encompasses a range of interventions aimed at reducing the impact of these conditions by addressing physical disabilities and limitations. By alleviating pain and improving physical function, rehabilitation enables individuals to engage more fully in meaningful life roles, including employment. This enhanced participation, in turn, yields significant health, social, and economic benefits [
1]. Given the global aging population and the increasing prevalence of noncommunicable diseases, rehabilitation is now recognized as an essential health service [
2].
Osteoarthritis (OA), the most common form of arthritis worldwide [
3], is characterized by cartilage degeneration in joints, osteophyte formation, subchondral sclerosis, and weakening of the surrounding muscles [
4]. These pathological changes result in pain, functional limitations, and disability, imposing a significant burden on individuals and society. The primary symptoms of OA include joint pain, stiffness, and restricted range of motion. The condition commonly affects multiple joints, particularly the hips, knees, hands, feet, and spine [
5].
The demand for total hip arthroplasty (THA) is rising. In 2022, a total of 64,694 hip replacement surgeries were performed across Poland under agreements with the Polish National Health Fund (NFZ). This accounts for a significant 61% of all such operations conducted during that period. According to data collected by the NFZ, the three main reasons for primary hip replacement surgery were primary bilateral coxarthrosis, femoral neck fractures, and other primary coxarthroses. In the case of secondary hip replacement, the most common cause was mechanical complications related to internal joint prostheses [
6].
Persistent pain (PP) is the defining symptom of osteoarthritis, the most prevalent form of arthritis. This pain prompts individuals to seek medical care and significantly contributes to functional limitations and a diminished quality of life. Consequently, lower extremity OA is widely recognized as the leading cause of mobility impairment in older adults [
7]. PP lasting more than six months, along with long-term physical or mental conditions, is linked to poorer psychological well-being. The negative impact on psychological health is especially pronounced when mental conditions or multiple pain sites are involved, potentially affecting the individual's overall health status. As a result, it is essential to evaluate psychological well-being in those living with PP and chronic conditions. Additionally, there is a critical need to develop clinical strategies aimed at supporting individuals burdened by chronic conditions, PP, and diminished psychological well-being [
8]. Unfortunately, psychological evaluation and intervention have not yet become standard practice in orthopedic rehabilitation in Europe, despite strong evidence linking physical pain to mental well-being.
Gender is a key determinant of health, significantly affecting the power and control individuals have over various health determinants, such as socioeconomic status, roles, social rank, access to resources, and treatment within society. Consequently, gender plays a crucial role in determining susceptibility and exposure to various mental health risks. Numerous studies across different nations have shown that women are approximately twice as likely as men to develop symptoms of depression and anxiety. This heightened reactivity in women compared to men has been attributed to differences in biological responses, self-concepts, and coping styles [
9,
10].
Standard care for adults who have undergone THA for end-stage osteoarthritis includes postoperative rehabilitation aimed at optimizing function, reducing pain, and resuming normal activities of daily living (ADL). An expert consensus on optimal rehabilitation practices following THA strongly recommends engaging in therapeutic exercises for 4 to 8 weeks, with a frequency of three to five sessions per week [
11]. Rehabilitation programs are multifaceted, comprising various components such as resistance exercises and gait training. These interventions can begin at various stages after surgery, be provided at different frequencies and intensities, and be administered by a range of personnel in various settings. Furthermore, they can be customized to fit individual, social, and financial circumstances, as well as responses to surgery and rehabilitation. While rehabilitation following THA is generally effective, it is still uncertain which specific interventions or components are most beneficial and should be standardized in practice to achieve the best clinical outcomes and reduce the risk of avoidable complications or joint failures [
12].
Following THA, physiotherapy treatment typically includes passive and active mobilizations immediately after surgery, cryotherapy, and exercises aimed at enhancing the functionality and strength of the knee joint [
13]. However, traditional physiotherapy approaches, which often involve passive and analytical exercises, may be perceived by patients as monotonous and lacking in motivation, as they do not actively engage the patient in their rehabilitation. Additionally, the high socio-economic costs associated with these treatments can prevent some patients from continuing with the same regimen [
14].
Virtual reality (VR) is a technological innovation that allows users to fully immerse themselves in a simulated environment, providing a sense of presence through multimodal stimuli [
15]. The use of VR-based rehabilitation in orthopedic surgery, particularly for THA and total knee arthroplasty (TKA), has significantly increased [
16]. Various VR-based protocols have been suggested for post-operative rehabilitation following TKA and THA [
17]. Despite this, no studies have assessed the effectiveness of these VR-based interventions in alleviating stress, anxiety, or depression symptoms in osteoarthritis patients after undergoing TKA or THA. Therefore, the primary aim of the study was to determine the impact of virtual therapy on the psychological and functional state of patients participating in rehabilitation after total hip arthroplasty. We hypothesize that VR therapy significantly enhances both the psychological and functional states of patients, with a positive correlation between improvements in these two parameters.
2. Materials and Methods
2.1. Study Design, Setting and Participants
In accordance with the participant recruitment guidelines for pilot randomized trials outlined by Julious (2005) and Whitehead et al. (2015), we consecutively enrolled 24 female patients undergoing rehabilitation after hip arthroplasty at St. Hedwig Hospital in Trzebnica, Poland [
18,
19]. The recruitment period spanned from March to August 2023. The study was accepted by the Bioethics Committee at the Wroclaw Medical University (119/KB/2023). The protocol was registered in the ClinicalTrials.gov database (NCT06506760).
2.2. Interventions
Patients from both groups participated in a standard rehabilitation program following hip arthroplasty, lasting four weeks as an inpatient regimen. The program included kinesitherapy with two-hour daily gait training sessions, occupational therapy for 30 minutes each day, and physiotherapy treatments such as laser therapy, cryotherapy, magnetic field therapy, and electrotherapy, which were individually tailored to meet each patient's specific needs.
Additionally, patients in the experimental group participated in eight VR therapy sessions (2 times a Week), supplementing the standard rehabilitation. Each VR session lasted up to 20 minutes. The VR therapy was conducted using the VRTierOne medical device by Stolgraf® (Stanowice, Poland). This device was equipped with HTC VIVE VR goggles and an HTC VIVE controller that tracked the movements of the dominant wrist. The use of VRTierOne aimed to transport patients into a calm, virtual world, enabling relaxation and helping to soothe emotions. Each therapeutic session began at a gate through which patients entered a garden. With each session, the garden dynamically developed, becoming increasingly vibrant. In the middle of each therapeutic session, a mandala appeared in the garden, which the patients were tasked with coloring. The VR therapy was based on the principles of Ericksonian psychotherapy, utilizing metaphors, hypnosis, and symbolism. Additionally, the background of the VR therapy consisted of relaxation music, which changed as the therapy progressed. A detailed description of the VR therapy principles has been described in previous works [
15,
20,
21].
While both participants and intervention providers were aware of the group assignments throughout the trial, no deviations from the planned intervention were observed, given the trial's context.
2.3. Outcome Measures
Participants completed a custom questionnaire to collect basic sociodemographic data, including age, body mass, height, BMI, education level, and marital status. The study assessed both psychological and functional status through evaluations conducted at two time points: prior to the intervention (week 0) and upon its completion (week 4).
The primary outcome measure was the Hospital Anxiety and Depression Scale (HADS), which detects depressive and anxiety states [
22]. It consists of 14 questions, with 7 each related to anxiety and depression. Higher scores on the HADS indicate higher levels of anxiety and/or depression, with cut-off scores of 8 and above on each subscale suggesting elevated anxiety or depression, and scores above 10 indicating a pathological state.
Secondary outcome measures included assessments of psychological status using the Perception of Stress Questionnaire (PSQ), Generalized Self-Efficacy Scale (GSES), and Visual Analog Scale (VAS) for pain. The PSQ measures generalized stress levels through three components: Emotional Tension, External Stress, and Intrapsychic Stress, with overall scores ranging from 21 to 105 points [
23]. A subscale cut-off score of 20 points suggests a borderline average result, with higher scores indicating greater tension or stress. The GSES assesses the general sense of self-efficacy, evaluating whether patients can anticipate coping strategies for daily problems and adapt to stressful situations [
24]. Scores below 25 suggest low self-efficacy, while scores above 30 indicate high self-efficacy. The VAS for pain assessment ranges from 0 to 10, where 0 indicates no pain and 10 indicates the greatest possible pain [
25].
Functional evaluations included the Tinetti test, Barthel Index (BI), Rivermead Motor Assessment Gross Function Subscale (RMA-GF), and Short Physical Performance Battery (SPPB). Tinetti's Short Scale, a simplified version of the Performance-Oriented Mobility Assessment (POMA), evaluates a patient's gait and balance through tasks such as sitting to standing, standing still for 5 seconds, walking 3 meters, turning 180 degrees, and maintaining a sitting position [
26]. Each task is rated on a 3-point Likert scale, with total scores ranging from 0 to 15, where higher scores indicate better functional mobility. The BI analyzes patients' ability to perform daily living activities, awarding points on a scale from 0 to 10 for each activity, with a maximum score of 100 points [
27]. Higher scores indicate better functional status, while lower scores indicate greater limitations in daily activities. The RMA-GF was used to assess patient mobility, modified to exclude the 10-meter run and jumping tasks due to hip arthroplasty contraindications [
28]. The test included 11 tasks, with each correctly performed task earning one point, ranging from sitting independently to walking 40 meters and climbing stairs. Higher scores, up to a maximum of 11, indicated greater functional capabilities and lower disability. The SPPB assesses the physical fitness of older adults and consists of three different types of physical activities: balance maintenance, gait speed, and chair rising [
29]. A maximum score of 12 points can be achieved, and a low score may suggest potential mobility issues in the near future, possibly leading to the need for hospitalization or long-term care.
2.4. Data Analysis
Statistical analysis was conducted using JASP software, version 0.18.3 (University of Amsterdam, Netherlands). Descriptive data for categorical variables were presented as frequencies and percentages. For continuous variables, the mean and standard deviation (SD) were calculated. Group characteristics were compared using the Chi-square test and the unpaired t-test. The Shapiro-Wilk test confirmed that the distribution of the obtained results was close to normal. The effects of the intervention between groups were evaluated using analysis of variance (ANOVA) supplemented by unpaired t-tests for independent groups (between-group effects) and dependent groups (within-group effects). The relationship between changes in psychological and functional parameters was examined using Spearman's rank correlation coefficient. Values of p < 0.05 were considered statistically significant.
3. Results
3.1. Participants Characteristics
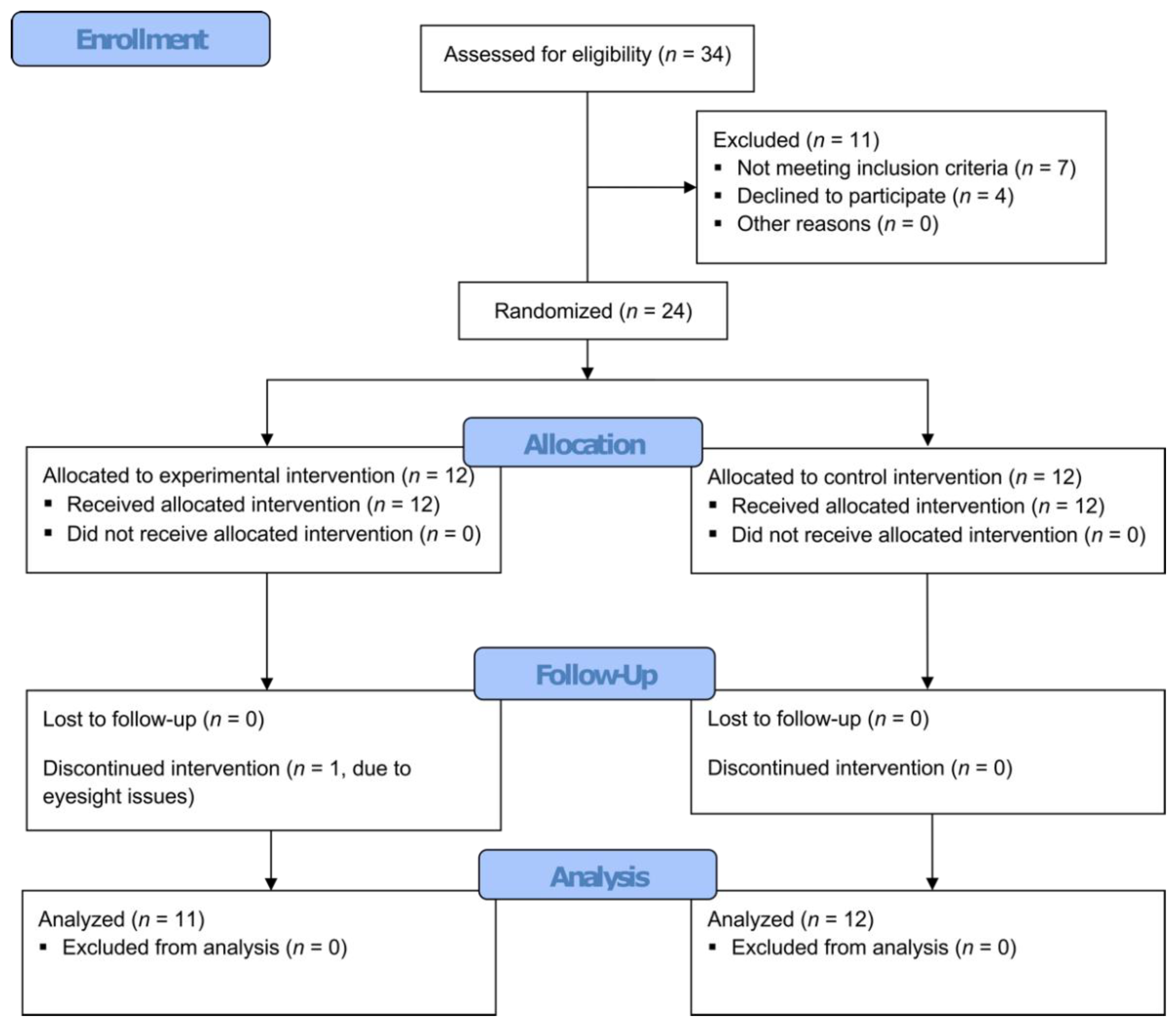
As illustrated in
Figure 1, following an initial eligibility assessment, 24 women were randomly allocated to one of two treatment groups. One patient from the experimental group did not finish the intervention due to eyesight problems in VR.
The average age of patients in the experimental group was 71.91 years, which was 0.26 years lower than that in the control group (
Table 1). The average height in the experimental group was 0.35 cm higher than in the control group (experimental 161.27cm and control 160.92cm). The average body mass of patients in the VR therapy group was 0.65 kg lower (experimental 74.18kg and control 74.83kg), and the average BMI was 0.38 lower than in the control group (experimental 28.69kg/m
2 and control 29.07kg/m
2). Among all patients, 5 had a normal BMI, 10 were overweight, and 8 were obese. Regarding education, 11 patients had vocational education, 9 had secondary education, and 3 had higher education. In terms of marital status, 15 patients were married, 7 were widows, and 1 was divorced. There were no statistically significant differences between the groups in the various variables.
3.2. Psychological State
As shown in
Table 2, in the context of psychological state, statistically significant changes were observed in all measured parameters between measurement points in the experimental group, except for HADS-D (p = 0.16). The overall HADS score significantly decreased by 53% (from 12.55 to 5.91; p = 0.03), while the anxiety component (HADS-A) significantly reduced by 58% (from 7.00 to 2.91; p = 0.01). The overall PSQ score significantly decreased by 43% (from 64.82 to 37.00; p < 0.001). Analysis of the individual stress components measured by the PSQ showed significant decreases: a 52% reduction in Emotional Tension (from 24.18 to 11.55; p < 0.001), a 31% reduction in External Stress (from 19.73 to 13.55; p = 0.01), and a 43% reduction in Intrapsychic Stress (from 20.91 to 11.91; p < 0.01). The GSES questionnaire results indicate a significant increase in self-efficacy after the intervention by 45% (from 26.73 to 38.82; p < 0.001). The analysis of the VAS scale results showed a significant reduction in the pain experienced by patients by 84% (from 4.55 to 0.73; p < 0.001).
Compared to the experimental group, no significant changes were observed between measurements in the control group regarding psychological state (
p > 0.05), except for the VAS scale results (
p = 0.02). Additionally, significant differences in intervention efficacy were observed between the groups in all measured psychological parameters, except for HADS-D (
p = 0.12,
Table 2), favoring the intervention used in the experimental group. Furthermore, the ANOVA results indicating significant group-by-time interactions with a high effect size (
η²p > 0.14;
Table 3) confirm the observed difference in the effectiveness of the applied interventions between the groups concerning psychological parameters.
3.3. Functional State
Statistical changes were observed in all measured parameters between the measurement points in the experimental group (
Table 4). After the intervention, the Tinetti Test score significantly increased by 200% (from 3.27 to 9.82;
p < 0.001). The same trend was observed in other functional tests: the Barthel Index score increased by 66.7% (from 55.91 to 93.18;
p < 0.001), the RMA-GF test score increased by 131.9% (from 4.27 to 9.91;
p < 0.001), and the SPPB test score increased by 143.2% (from 3.36 to 8.18;
p < 0.01). Similarly, in the control group a significant increase in functional parameter outcomes was observed after the intervention (
p < 0.001 for Tinetti, Barthel, RMA-GF tests, and
p < 0.01 for the SPPB test). Additionally, significant differences in intervention efficacy between the groups were observed across all measured functional parameters, except for SPPB (
p = 0.10,
Table 4), favoring the intervention applied in the experimental group.
Furthermore, the results of the analysis of variance (ANOVA) indicating significant interactions between group and measurement point with high effect size (
η²p > 0.14;
Table 3) confirm the observed difference in the efficacy of the interventions applied between the groups concerning functional parameters.
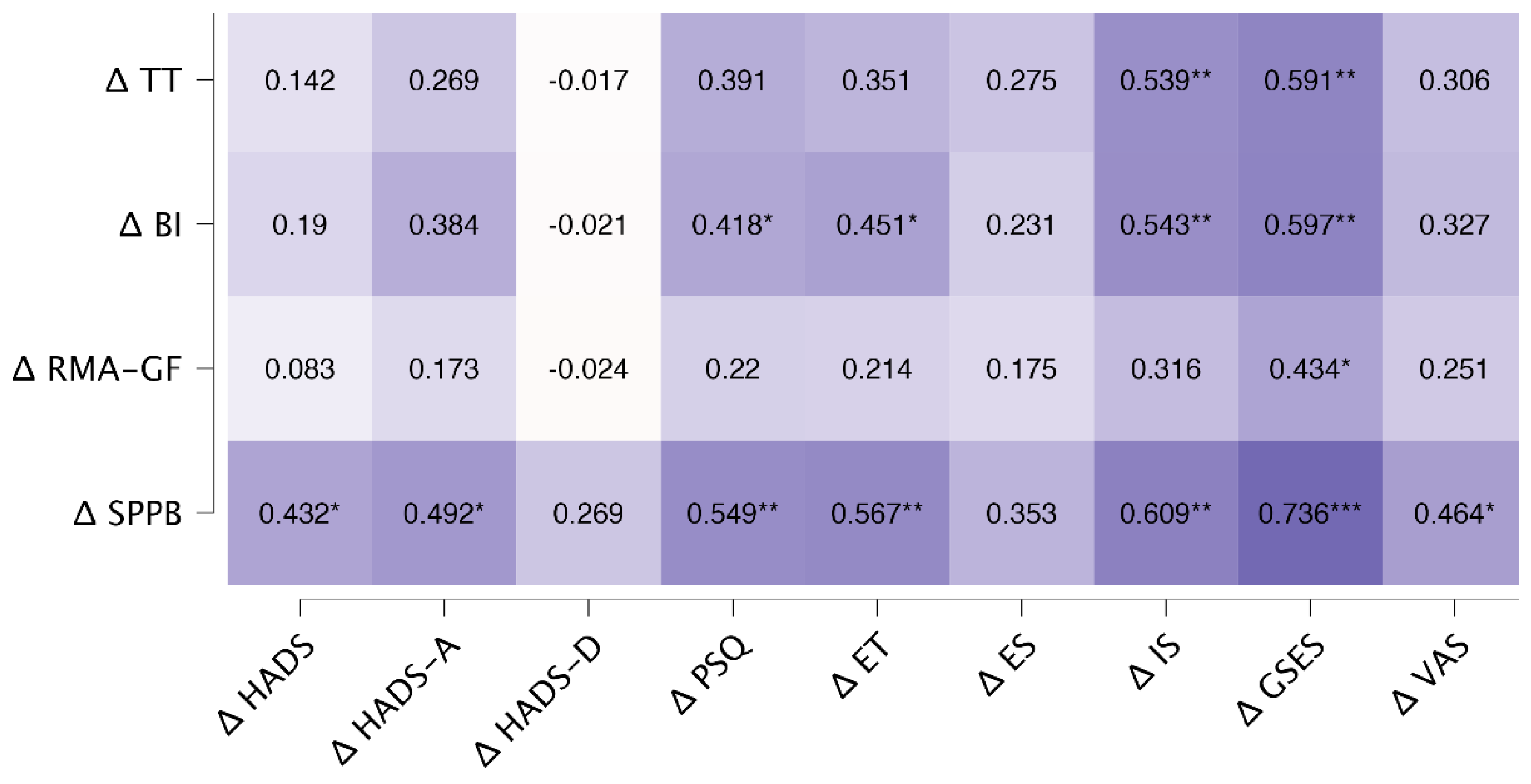
3.4. Correlations
Figure 2 shows the correlation between changes in psychological parameters and changes in functional parameters. Significant correlations were observed between the differences in psychological parameters and the following test results: SPPB (ranging from 0.43 to 0.74), BI (ranging from 0.42 to 0.60), and TT (ranging from 0.54 to 0.59). For the change in RMA-GF scores, a significant correlation of 0.43 was observed only with the change in GSES scores. All significant correlations were positive, suggesting that larger differences between measurements in psychological parameters correlated with greater differences in functional parameters, and vice versa.
4. Discussion
Previous research indicates that individuals with long-term and comorbid psychological conditions, such as depression, fear, or anxiety, tend to experience poorer healthcare outcomes, including longer treatment durations and higher hospitalization rates [
30]. This is likely due to factors such as an increased risk of additional physical health issues and limited socioeconomic resources, which can impede the independence of individuals whose mental health needs are not adequately addressed in the community. However, there is limited scientific evidence on how psychological needs affect healthcare outcomes in the context of inpatient orthopedic rehabilitation. Exploring this impact could help reduce unnecessary costs and resource consumption within healthcare services and identify areas where clinical best practices may need to be reviewed.
Another issue is that the current rehabilitation outcome evaluations frequently focus only on physical functionality. Additionally, there is a lack of research on the various methods used to identify psychological needs. As a result, the impact of broader psychological factors on other rehabilitation objectives remains uncertain. In our opinion, investigating these aspects is crucial for assessing the necessity of psychological screening tools and for improving the identification of needs and the achievement of rehabilitation goals.
Given the widespread psychological needs among women aged 65 and older with OA, the potential influence of mood, stress, pain, and psychological adjustment on rehabilitation engagement and outcomes, and the lack of standardized methods for assessing these needs, this study aimed to evaluate the effects of virtual therapy on the psychological and functional status of patients undergoing rehabilitation after THA. The study hypothesized that patients with identified psychological needs would demonstrate poorer rehabilitation outcomes. Patients with osteoarthritis who undergo surgery often participate in specialized inpatient rehabilitation programs to develop the physical skills and knowledge required to manage the complex and diverse challenges they encounter. Various personal factors—including gender, social support, pain intensity, obesity [
31], balance, cognitive function, and physical ability [
32]—as well as elements like accelerated rehabilitation and preoperative physiotherapy [
33], have been shown to influence both the accessibility and outcomes of rehabilitation. Psychological well-being, in particular, plays a critical role in rehabilitation success, as mental health challenges such as low mood, depressive symptoms, and anxiety are closely linked to increased pain and poorer physical health [
34,
35,
36,
37].
As anticipated in the initial hypotheses, the current findings show notable improvements in all assessed psychological outcomes for the experimental group after rehabilitation treatment with supporting VR therapy. In contrast, the control group's psychological status remained unchanged, and their HADS total score even significantly increased. These results align with our previous research across various rehabilitation areas [
15,
38]. Individuals with psychological needs might take longer to achieve similar rehabilitation outcomes. This could be because physical symptoms associated with low mood, anxiety, or negative appraisals slow down their progress. For example, low mood has been shown to increase pain levels, which can hinder participation and engagement in rehabilitation. While there is less research on the impact of anxiety compared to depression on rehabilitation outcomes, Le and Dorstyn note in a meta-analysis on patients with spinal cord injuries, that ongoing fear of secondary life-threatening conditions, such as autonomic dysreflexia, may arise during rehabilitation [
39].
It is also probable, that patients with psychological problems might have a greater overall need for rehabilitation. They could have more rehabilitation goals left to accomplish or might benefit from a more personalized rehabilitation program that considers their psychological health. Integrating psychological treatment with other therapies could help maximize their progress.
Ultimately, as hypothesized and consistent with Nguven et al. [
40], women with identified and treated psychological needs showed greater improvement in nearly all rehabilitation results. Therefore, having an identified psychological need does not universally or inevitably result in poorer rehabilitation outcomes. Early psychological screening can significantly enhance the effectiveness of inpatient physiotherapy. Future research should investigate specific factors that contribute to psychological needs, such as pre-existing mental health conditions or socio-demographic influences.
The study has several limitations that should be acknowledged. First, the relatively small sample size of 24 female participants limits the generalizability of the findings, as results may not be applicable to males or individuals from different demographic backgrounds. Additionally, the four-week duration of the rehabilitation program may not capture the long-term effects of the interventions, particularly for chronic conditions like osteoarthritis. Finally, all psychological assessments relied on self-reported scales, which can introduce bias due to participants' subjective perceptions and potential inaccuracies in self-assessment. Addressing these limitations in future research could improve the robustness and applicability of the findings.
5. Conclusions
VR treatment presents itself as an effective therapeutic option for women 65+ recovering from arthroplasty surgery and undergoing inpatient rehabilitation program, potentially becoming a standard component of treatment. Incorporating VR therapy into traditional rehabilitation protocols not only boosts patients' psychological well-being but also promotes better functional outcomes. It is essential to evaluate the psychological well-being of individuals experiencing PP and chronic conditions, and to create clinical strategies to aid those affected by these issues. Despite substantial evidence connecting physical pain with mental health, psychological assessment and intervention have not yet become standard practice in orthopedic rehabilitation in Europe.
Author Contributions
conceptualization, J.M., B.C. and J.S.-G.; methodology, J.M. and J.S.-G.; validation, J.M. and B.C.; formal analysis, A.W. and B.C.; investigation, J.M. and B.C.; resources, J.M., A.W. and J.S.-G.; data curation, J.M., A.W.; visualization, A.W. and B.C.; writing—original draft preparation, J.M., B.C. and A.W.; writing—review and editing, J.M. and J.S.-G.; supervision, J.S.-G.,J.M. and; R.G.; project administration, J.M.; J.S-G. and R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Bioethics Committee of the Wroclaw Medical University, Poland (119/KB/2023; June 27, 2023).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization Rehabilitation in Health Systems; World Health Organization, 2017; ISBN 978-92-4-154997-4.
- United Nation Disability and Development Report 2024 - Accelerating the Realization of the Sustainable Development Goals by, for and with Persons with Disabilities; 2024.
- Steinmetz, J.D.; Culbreth, G.T.; Haile, L.M.; Rafferty, Q.; Lo, J.; Fukutaki, K.G.; Cruz, J.A.; Smith, A.E.; Vollset, S.E.; Brooks, P.M.; et al. Global, Regional, and National Burden of Osteoarthritis, 1990–2020 and Projections to 2050: A Systematic Analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e508–e522. [Google Scholar] [CrossRef]
- Yunus, M.H.M.; Nordin, A.; Kamal, H. Pathophysiological Perspective of Osteoarthritis. Med. Kaunas Lith. 2020, 56, 614. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.M.; Santos, A.M.; Carvalho Nascimento, J.A.; Santana, C.C.; Oliveira, A.M.S.; Cezar, S.V.S.; Santos, A.B.; Frank, L.A.; Serafini, M.R. Devices for Osteoarthritis Symptoms Treatment: A Patent Review. Expert Rev. Med. Devices 2024, 21, 91–107. [Google Scholar] [CrossRef] [PubMed]
- Narodowy Fundusz Zdrowia (NFZ) Realizacja świadczeń endoprotezoplastyki stawowej w 2022 r. Available online: https://www.nfz.gov.pl/o-nfz/publikacje/ (accessed on 19 June 2024).
- Neogi, T. The Epidemiology and Impact of Pain in Osteoarthritis. Osteoarthr. Cartil. OARS Osteoarthr. Res. Soc. 2013, 21, 1145–1153. [Google Scholar] [CrossRef]
- Tang, L.H.; Andreasson, K.H.; Thygesen, L.C.; Jepsen, R.; Møller, A.; Skou, S.T. Persistent Pain and Long-Term Physical and Mental Conditions and Their Association with Psychological Well-Being; Data from 10,744 Individuals from the Lolland-Falster Health Study. J. Multimorb. Comorbidity 2022, 12, 26335565221128712. [Google Scholar] [CrossRef] [PubMed]
- Abate, K.H. Gender Disparity in Prevalence of Depression Among Patient Population: A Systematic Review. Ethiop. J. Health Sci. 2013, 23, 283. [Google Scholar] [CrossRef] [PubMed]
- Shawon, M.S.R.; Hossain, F.B.; Hasan, M.; Rahman, M.R. Gender Differences in the Prevalence of Anxiety and Depression and Care Seeking for Mental Health Problems in Nepal: Analysis of Nationally Representative Survey Data. Glob. Ment. Health Camb. Engl. 2024, 11, e46. [Google Scholar] [CrossRef]
- Westby, M.D.; Brittain, A.; Backman, C.L. Expert Consensus on Best Practices for Post–Acute Rehabilitation After Total Hip and Knee Arthroplasty: A Canada and United States Delphi Study. Arthritis Care Res. 2014, 66, 411–423. [Google Scholar] [CrossRef]
- Konnyu, K.J.; Pinto, D.; Cao, W.; Aaron, R.K.; Panagiotou, O.A.; Bhuma, M.R.; Adam, G.P.; Balk, E.M.; Thoma, L.M. Rehabilitation for Total Hip Arthroplasty: A Systematic Review. Am. J. Phys. Med. Rehabil. 2023, 102, 11. [Google Scholar] [CrossRef]
- Jenkins, C.; Lowe, C.M.; Barker, K.L. Early Post-Operative Physiotherapy Rehabilitation after Primary Unilateral Unicompartmental Knee Replacement: A Systematic Review. Physiotherapy 2023, 118, 39–53. [Google Scholar] [CrossRef]
- Fatoye, F.; Gebrye, T.; Fatoye, C.; Mbada, C. A Systematic Review of Economic Models for Cost Effectiveness of Physiotherapy Interventions Following Total Knee and Hip Replacement. Physiotherapy 2022, 116, 90–96. [Google Scholar] [CrossRef]
- Szczepańska-Gieracha, J.; Jóźwik, S.; Cieślik, B.; Mazurek, J.; Gajda, R. Immersive Virtual Reality Therapy as a Support for Cardiac Rehabilitation: A Pilot Randomized-Controlled Trial. Cyberpsychology Behav. Soc. Netw. 2021, 24, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Zeng, Y.; Wu, Y.; Si, H.; Shen, B. Virtual Reality-Based Rehabilitation in Patients Following Total Knee Arthroplasty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Chin. Med. J. (Engl.) 2021, 135, 153–163. [Google Scholar] [CrossRef] [PubMed]
- García-Sánchez, M.; García-Robles, P.; Osuna-Pérez, M.C.; Lomas-Vega, R.; Obrero-Gaitán, E.; Cortés-Pérez, I. Effectiveness of Virtual Reality-Based Early Postoperative Rehabilitation after Total Knee Arthroplasty: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Appl. Sci. 2023, 13, 4597. [Google Scholar] [CrossRef]
- Julious, S.A. Sample Size of 12 per Group Rule of Thumb for a Pilot Study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Whitehead, A.L.; Julious, S.A.; Cooper, C.L.; Campbell, M.J. Estimating the Sample Size for a Pilot Randomised Trial to Minimise the Overall Trial Sample Size for the External Pilot and Main Trial for a Continuous Outcome Variable. Stat. Methods Med. Res. 2016, 25, 1057–1073. [Google Scholar] [CrossRef]
- Jóźwik, S.; Wrzeciono, A.; Cieślik, B.; Kiper, P.; Szczepańska-Gieracha, J.; Gajda, R. The Use of Virtual Therapy in Cardiac Rehabilitation of Male Patients with Coronary Heart Disease: A Randomized Pilot Study. Healthc. Basel Switz. 2022, 10, 745. [Google Scholar] [CrossRef] [PubMed]
- Cieślik, B.; Juszko, K.; Kiper, P.; Szczepańska-Gieracha, J. Immersive Virtual Reality as Support for the Mental Health of Elderly Women: A Randomized Controlled Trial. Virtual Real. 2023, 1–9. [Google Scholar] [CrossRef]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The Validity of the Hospital Anxiety and Depression Scale. An Updated Literature Review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Plopa, M.; Makarowski, R. The Perception of Stress Questionnaire. Manual; Vizja Press & IT: Warsaw, Poland, 2010; ISBN 978-83- 61086-79-6. [Google Scholar]
- Luszczynska, A.; Scholz, U.; Schwarzer, R. The General Self-Efficacy Scale: Multicultural Validation Studies. J. Psychol. 2005, 139, 439–457. [Google Scholar] [CrossRef]
- Heller, G.Z.; Manuguerra, M.; Chow, R. How to Analyze the Visual Analogue Scale: Myths, Truths and Clinical Relevance. Scand. J. Pain 2016, 13, 67–75. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Williams, T.F.; Mayewski, R. Fall Risk Index for Elderly Patients Based on Number of Chronic Disabilities. Am. J. Med. 1986, 80, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. FUNCTIONAL EVALUATION: THE BARTHEL INDEX. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Collen, F.M.; Wade, D.T.; Robb, G.F.; Bradshaw, C.M. The Rivermead Mobility Index: A Further Development of the Rivermead Motor Assessment. Int. Disabil. Stud. 1991, 13, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Lauretani, F.; Ticinesi, A.; Gionti, L.; Prati, B.; Nouvenne, A.; Tana, C.; Meschi, T.; Maggio, M. Short-Physical Performance Battery (SPPB) Score Is Associated with Falls in Older Outpatients. Aging Clin. Exp. Res. 2019, 31, 1435–1442. [Google Scholar] [CrossRef]
- Siddiqui, N.; Dwyer, M.; Stankovich, J.; Peterson, G.; Greenfield, D.; Si, L.; Kinsman, L. Hospital Length of Stay Variation and Comorbidity of Mental Illness: A Retrospective Study of Five Common Chronic Medical Conditions. BMC Health Serv. Res. 2018, 18, 498. [Google Scholar] [CrossRef]
- Simões, J.L.; Soares, S.; Sa-Couto, P.; Lopes, C.; Magina, D.; Melo, E.; Voegeli, D.; Bolhão, I. The Influence of Presurgical Factors on the Rehabilitation Outcome of Patients Following Hip Arthroplasty. Rehabil. Nurs. J. 2019, 44, 189. [Google Scholar] [CrossRef] [PubMed]
- Folden, S.; Tappen, R. Factors Influencing Function and Recovery Following Hip Repair Surgery. Orthop. Nurs. 2007, 26, 234–241. [Google Scholar] [CrossRef]
- Sharma, V.; Morgan, P.M.; Cheng, E.Y. Factors Influencing Early Rehabilitation after THA: A Systematic Review. Clin. Orthop. 2009, 467, 1400–1411. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, M.H. The Link Between Depression and Physical Symptoms. Prim. Care Companion J. Clin. Psychiatry 2004, 6, 12–16. [Google Scholar]
- Brenes, G.A. Anxiety, Depression, and Quality of Life in Primary Care Patients. Prim. Care Companion J. Clin. Psychiatry 2007, 9, 437–443. [Google Scholar] [CrossRef] [PubMed]
-
National Collaborating Centre for Mental Health (UK) Depression in Adults with a Chronic Physical Health Problem: Treatment and Management; National Institute for Health and Care Excellence: Guidelines; British Psychological Society (UK): Leicester (UK), 2010; ISBN 978-1-904671-86-2.
- Gerdle, B.; Åkerblom, S.; Brodda Jansen, G.; Enthoven, P.; Ernberg, M.; Dong, H.-J.; Stålnacke, B.-M.; Äng, B.O.; Boersma, K. Who Benefits from Multimodal Rehabilitation – an Exploration of Pain, Psychological Distress, and Life Impacts in over 35,000 Chronic Pain Patients Identified in the Swedish Quality Registry for Pain Rehabilitation. J. Pain Res. 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, J.; Cieślik, B.; Wrzeciono, A.; Gajda, R.; Szczepańska-Gieracha, J. Immersive Virtual Reality Therapy Is Supportive for Orthopedic Rehabilitation among the Elderly: A Randomized Controlled Trial. J. Clin. Med. 2023, 12, 7681. [Google Scholar] [CrossRef] [PubMed]
- Le, J.; Dorstyn, D. Anxiety Prevalence Following Spinal Cord Injury: A Meta-Analysis. Spinal Cord 2016, 54, 570–578. [Google Scholar] [CrossRef]
- Nguyen, U.-S.D.T.; Perneger, T.; Franklin, P.D.; Barea, C.; Hoffmeyer, P.; Lübbeke, A. Improvement in Mental Health Following Total Hip Arthroplasty: The Role of Pain and Function. BMC Musculoskelet. Disord. 2019, 20, 307. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).