Submitted:
20 October 2024
Posted:
21 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
Artificial Intelligence
Artificial Intelligence Evolution
Important Turning Points in the Development of AI
Generative AI
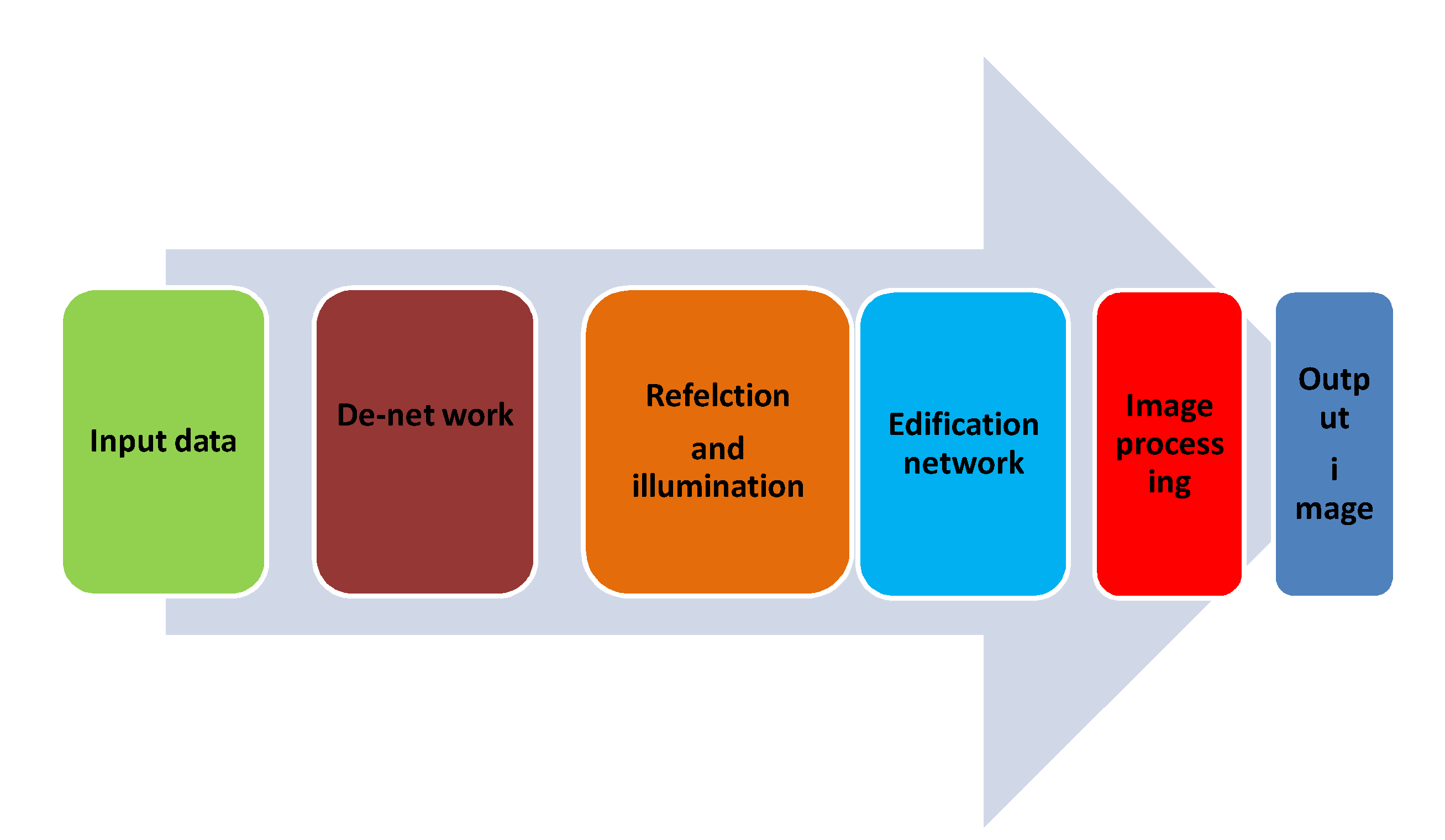
Image Enhancement
Image Segmentation
Slice by Slice Integration
Methods of Image Enhancement [34]
Spatial domain method
Spatial Domain Method
Frequency Domain Method
2. Applications
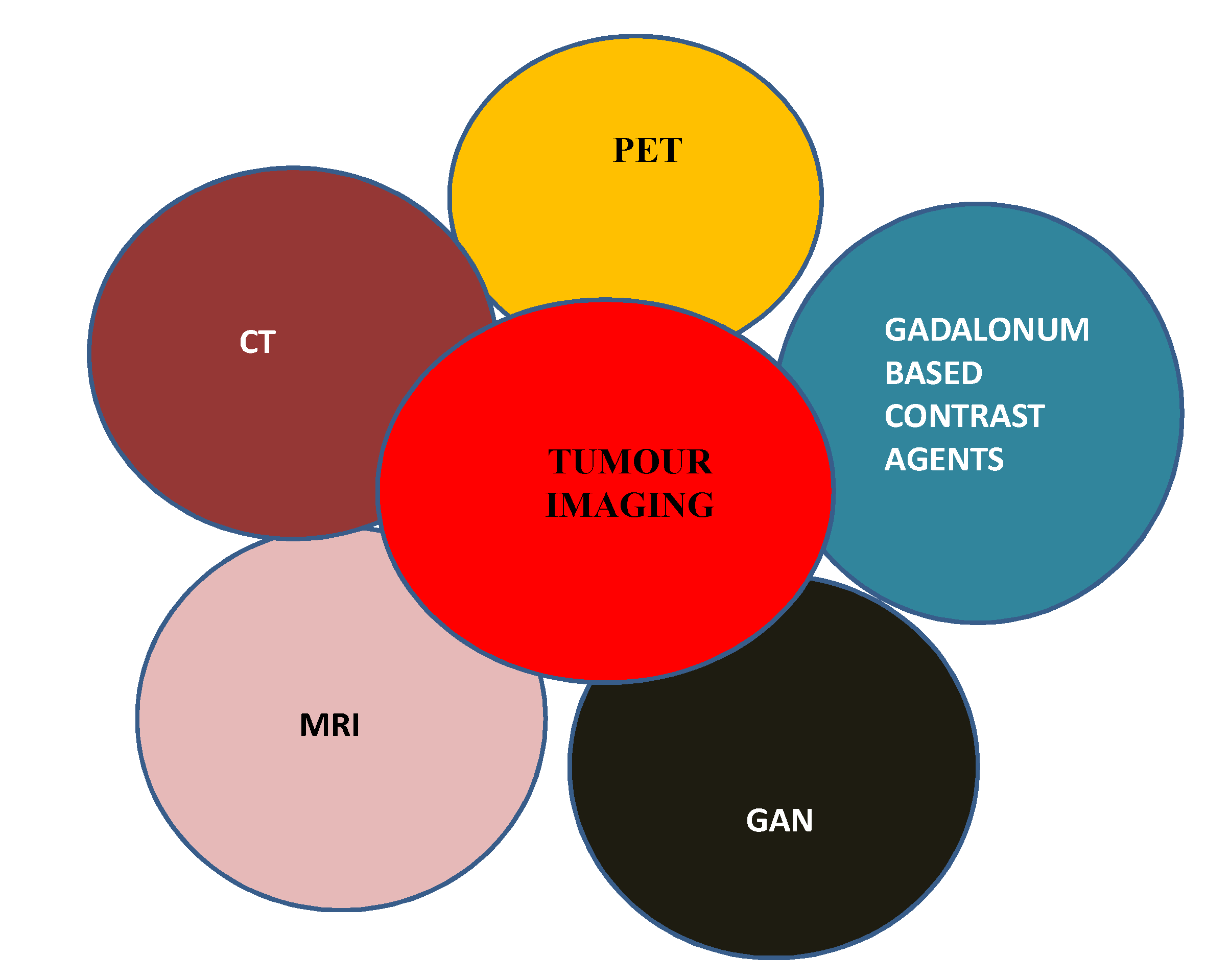
Tumour Imaging Using Generative AI [35]
Clinical Setting
Clinical Decision Support
Medical Imaging
Decision Support
COVID 19 and Drug Discovery
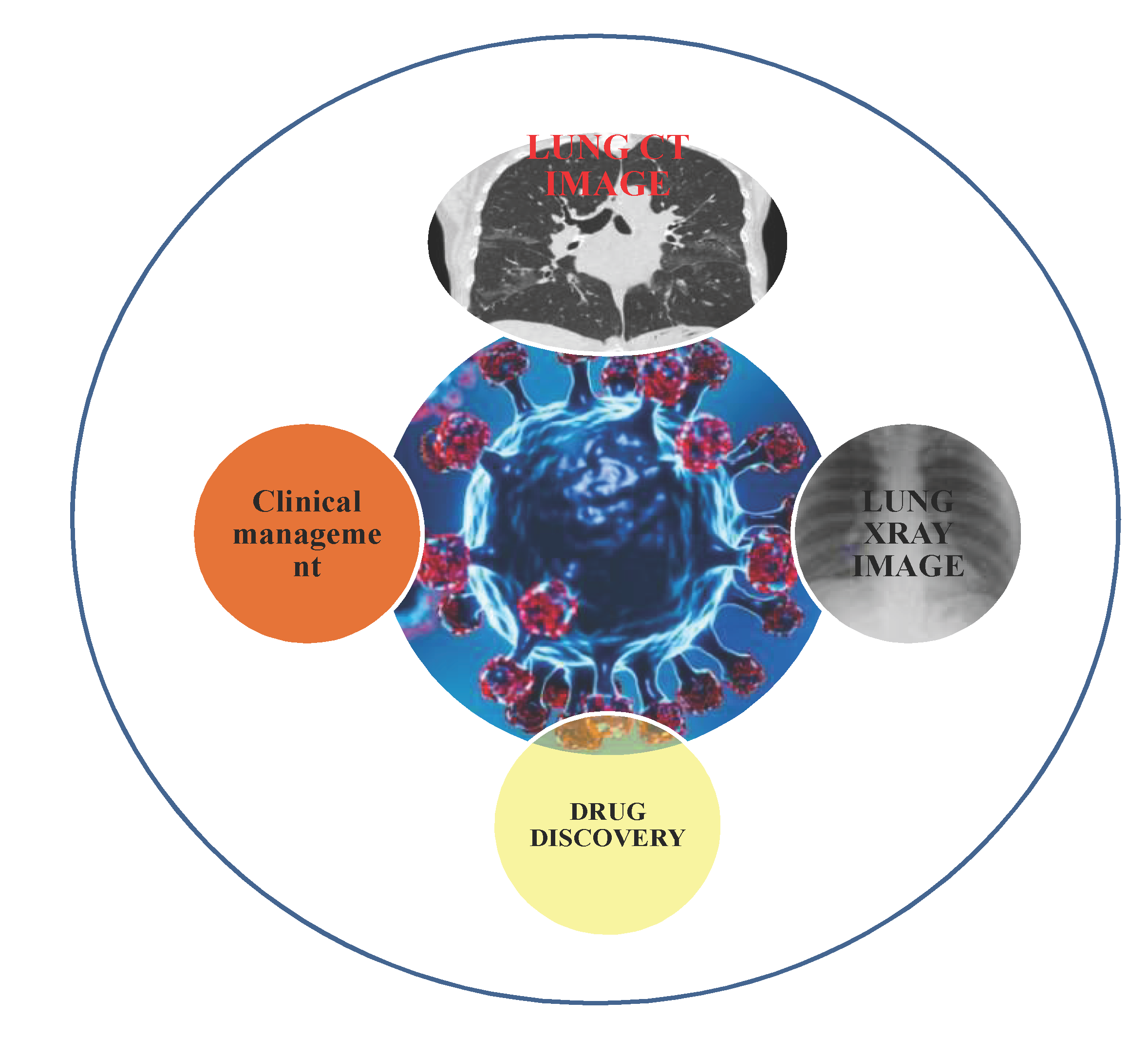
CT Imaging
Challenges
CT and MR Imaging in Oncology
Advancements in Medical Imaging
- Tissue slide mechanism another variant is tissue microarray (TMA). TMA technology is a potential tool for diagnosis, gives information with respect to progression of disease and patient information related to treatment. From histological specimen smaller cylinders are taken and arranged in a matrix configuration on a paraffin block and simultaneously analyzed.
- Optical coherence tomography (OCT) generates a series of cross sectional optical images of 3D fashion. Echo delay time and back scattered light in linearity measurement of internal tissues are performed.
-
X-imaging is one of the less expensive methods and also takes less time for image acquisition. In order to enhance the resolution of image, visibility iodinated contrast agents are used and administered into the interested areas.
- Phase contrast x- ray imaging method enhances soft tissue contrasting using the principle of phase shift.
- X- ray projection imaging is generally used in pervasion of cardiovascular , mammography and abdominal imaging purpose.
-
Ultra sound imaging utilizes pulse in 1-100 MHz this procedure is a non- invasive and less expensive method. It is a rapid method. In this method non- ionizing radiation is used. Acoustic pulse interacts with internal structure and echo is measured in order to construct medical image.
- Contrast enhanced ultrasound is enabling more image accuracy and contrast using micro bubbles.
- Ultrasound elasticity image is another tool for analyzing and measurement of tissue softness.
- 5.
- X- Ray CT imaging method takes scans like that of MRI where as CT constructs 3D images of 2 D axial slices of body. Like MRI, 4D scans are also possible by gating to ECG and respiration. Spatial resolution improvement to 0.25 mm is possible by this technique and also diagnosis. In traditional method of tissue staining, where the haemotoxylin and eosin stains are most commonly used stains. Using staining tissue morphology can be studies so that pathologist can interpret in accurate manner.
Medical Image Analysis
- Generative AI health care market
- b.
- Ethical issues
3. Challenges and Future Scope
4. Conclusion
References
- R. S. Michalski, J. G. Carbonell, and T. M. Mitchell, Eds., “Machine Learning: An Artificial Intelligence Approach,” Springer Science & Business Media, Apr. 17, 2013.
- R. Smith-Bindman, D. L. Miglioretti, and E. B. Larson, “Rising use of diagnostic medical imaging in a large integrated health system,” Health Affairs, vol. 27, no. 6, pp. 1491-1502, Nov. 2008.
- S. K. Zhou et al., “A review of deep learning in medical imaging: Imaging traits, technology trends, case studies with progress highlights, and future promises,” Proceedings of the IEEE, vol. 109, no. 5, pp. 820-838, Feb. 26, 2021.
- S. Sheikh, Ed., “Understanding the Role of Artificial Intelligence and Its Future Social Impact,” IGI Global, Jul. 17, 2020.
- P. R. Hiesinger, “The Self-Assembling Brain: How Neural Networks Grow Smarter,” Princeton University Press, May 4, 2021.
- M. Garnelo and M. Shanahan, “Reconciling deep learning with symbolic artificial intelligence: representing objects and relations,” Current Opinion in Behavioral Sciences, vol. 29, pp. 17-23, Oct. 1, 2019.
- S. Makridakis, “The forthcoming Artificial Intelligence (AI) revolution: Its impact on society and firms,” Futures, vol. 90, pp. 46-60, Jun. 1, 2017.
- C. Castaneda et al., “Clinical decision support systems for improving diagnostic accuracy and achieving precision medicine,” Journal of Clinical Bioinformatics, vol. 5, pp. 1-6, Dec. 2015.
- Y. Xu et al., “Artificial intelligence: A powerful paradigm for scientific research,” The Innovation, vol. 2, no. 4, Nov. 28, 2021.
- S. Hussain et al., “Modern diagnostic imaging technique applications and risk factors in the medical field: a review,” BioMed Research International, vol. 2022, Jun. 6, 2022.
- B. J. Pichler, H. F. Wehrl, A. Kolb, and M. S. Judenhofer, “Positron emission tomography/magnetic resonance imaging: the next generation of multimodality imaging?,” Seminars in Nuclear Medicine, vol. 38, no. 3, pp. 199-208, May 1, 2008.
- S. Pacilè, J. Lopez, P. Chone, T. Bertinotti, J.M. Grouin, and P. Fillard, “Improving breast cancer detection accuracy of mammography with the concurrent use of an artificial intelligence tool,” Radiology: Artificial Intelligence, vol. 2, no. 6, pp. e190208, Nov. 4, 2020.
- Sechopoulos, J. Teuwen, and R. Mann, “Artificial intelligence for breast cancer detection in mammography and digital breast tomosynthesis: State of the art,” in Seminars in Cancer Biology, vol. 72, pp. 214-225, Academic Press, Jul. 1, 2021.
- Rodríguez-Ruiz, E. Krupinski, J.J. Mordang, K. Schilling, S.H. Heywang-Köbrunner, I. Sechopoulos, and R.M. Mann, “Detection of breast cancer with mammography: effect of an artificial intelligence support system,” Radiology, vol. 290, no. 2, pp. 305-314, Feb. 2019.
- S.K. Zhou, H. Greenspan, C. Davatzikos, J.S. Duncan, B. Van Ginneken, A. Madabhushi, J.L. Prince, D. Rueckert, and R.M. Summers, “A review of deep learning in medical imaging: Imaging traits, technology trends, case studies with progress highlights, and future promises,” Proceedings of the IEEE, vol. 109, no. 5, pp. 820-838, Feb. 26, 2021.
- A.S. Panayides, A. Amini, N.D. Filipovic, A. Sharma, S.A. Tsaftaris, A. Young, D. Foran, N. Do, S. Golemati, T. Kurc, and K. Huang, “AI in medical imaging informatics: current challenges and future directions,” IEEE Journal of Biomedical and Health Informatics, vol. 24, no. 7, pp. 1837-1857, May 29, 2020.
- P. Savadjiev, J. Chong, A. Dohan, M. Vakalopoulou, C. Reinhold, N. Paragios, and B. Gallix, “Demystification of AI-driven medical image interpretation: past, present and future,” European Radiology, vol. 29, pp. 1616-1624, Mar. 2, 2019.
- N. Degrauwe, A. Digklia, and R. Duran, “Theranostics in interventional oncology: versatile carriers for diagnosis and targeted image-guided minimally invasive procedures,” Frontiers in Pharmacology, vol. 10, article 447271, , 2019. 9 May.
- H. Su, K.W. Kwok, K. Cleary, I. Iordachita, M.C. Cavusoglu, J.P. Desai, and G.S. Fischer, “State of the art and future opportunities in MRI-guided robot-assisted surgery and interventions,” Proceedings of the IEEE, vol. 110, no. 7, pp. 968-992, , 2022. 3 May.
- C.A. Linte, J. White, R. Eagleson, G.M. Guiraudon, and T.M. Peters, “Virtual and augmented medical imaging environments: Enabling technology for minimally invasive cardiac interventional guidance,” IEEE Reviews in Biomedical Engineering, vol. 3, pp. 25-47, Sep. 30, 2010.
- P. Lambin, R.T.H. Leijenaar, T.M. Deist, J. Peerlings, E.E. De Jong, J. Van Timmeren, S. Sanduleanu, R.T.H. Larue, A.J.G. Even, A. Jochems, and Y. Van Wijk, “Radiomics: the bridge between medical imaging and personalized medicine,” Nature Reviews Clinical Oncology, vol. 14, no. 12, pp. 749-762, Dec. 2017.
- C. Coolens, M.N. Gwilliam, P. Alcaide-Leon, I.M. de Freitas Faria, and F. Ynoe de Moraes, “Transformational role of medical imaging in (radiation) oncology,” Cancers, vol. 13, no. 11, p. 2557, May 23, 2021. 23 May.
- Castiglioni, L. Rundo, M. Codari, G. Di Leo, C. Salvatore, M. Interlenghi, F. Gallivanone, A. Cozzi, N.C. D’Amico, and F. Sardanelli, “AI applications to medical images: From machine learning to deep learning,” Physica Medica, vol. 83, pp. 9-24, Mar. 1, 2021.
- V. Sorin, Y. Barash, E. Konen, and E. Klang, “Creating artificial images for radiology applications using generative adversarial networks (GANs)–a systematic review,” Academic Radiology, vol. 27, no. 8, pp. 1175-1185, Aug. 1, 2020.
- Barragán-Montero, U. Javaid, G. Valdés, D. Nguyen, P. Desbordes, B. Macq, S. Willems, L. Vandewinckele, M. Holmström, F. Löfman, and S. Michiels, “Artificial intelligence and machine learning for medical imaging: A technology review,” Physica Medica, vol. 83, pp. 242-256, Mar. 1, 2021.
- K. Koshino, R.A. Werner, M.G. Pomper, R.A. Bundschuh, F. Toriumi, T. Higuchi, and S.P. Rowe, “Narrative review of generative adversarial networks in medical and molecular imaging,” Annals of Translational Medicine, vol. 9, no. 9, May 2021.
- L.K. Sundar, O. Muzik, I. Buvat, L. Bidaut, and T. Beyer, “Potentials and caveats of AI in hybrid imaging,” Methods, vol. 188, pp. 4-19, Apr. 1, 2021.
- G. Wang, J.C. Ye, and B. De Man, “Deep learning for tomographic image reconstruction,” Nature Machine Intelligence, vol. 2, no. 12, pp. 737-748, Dec. 2020.
- M. Yaqub, F. Jinchao, K. Arshid, S. Ahmed, W. Zhang, M.Z. Nawaz, and T. Mahmood, “Deep learning-based image reconstruction for different medical imaging modalities,” Computational and Mathematical Methods in Medicine, vol. 2022, 2022.
- D. Kornish, S. Ezekiel, and M. Cornacchia, “DCNN augmentation via synthetic data from variational autoencoders and generative adversarial networks,” in 2018 IEEE Applied Imagery Pattern Recognition Workshop (AIPR), Oct. 9, 2018, pp. 1-6.
- H. Hricak, D.J. Brenner, S.J. Adelstein, D.P. Frush, E.J. Hall, R.W. Howell, C.H. McCollough, F.A. Mettler, M.S. Pearce, O.H. Suleiman, and J.H. Thrall, “Managing radiation use in medical imaging: a multifaceted challenge,” Radiology, vol. 258, no. 3, pp. 889-905, Mar. 2011.
- R. Khan, S. Akbar, A. Khan, M. Marwan, Z.H. Qaisar, A. Mehmood, F. Shahid, K. Munir, and Z. Zheng, “Dental image enhancement network for early diagnosis of oral dental disease,” Scientific Reports, vol. 13, no. 1, p. 5312, Mar. 31, 2023.
- M. Eliezer, G. Poillon, C. Maquet, A. Gillibert, J. Horion, J.P. Marie, J.P. Guichard, N. Magne, and A. Attyé, “Sensorineural hearing loss in patients with vestibular schwannoma correlates with the presence of utricular hydrops as diagnosed on heavily T2-weighted MRI,” Diagnostic and Interventional Imaging, vol. 100, no. 5, pp. 259-268, May 1, 2019.
- A.M. Grigoryan and S.S. Agaian, “Transform-based image enhancement algorithms with performance measure,” Advances in Imaging and Electron Physics, vol. 130, pp. 165-242, May 1, 2004.
- J.E. Park, P. Vollmuth, N. Kim, and H.S. Kim, “Research highlight: use of generative images created with artificial intelligence for brain tumor imaging,” Korean Journal of Radiology, vol. 23, no. 5, p. 500, May 2022. 20 May.
- J. Li, Y. Tao, and T. Cai, “Predicting lung cancers using epidemiological data: A generative-discriminative framework,” IEEE/CAA Journal of Automatica Sinica, vol. 8, no. 5, pp. 1067-1078, Feb. 19, 2021.
- J. Rudolph, C. Huemmer, F.C. Ghesu, A. Mansoor, A. Preuhs, A. Fieselmann, N. Fink, J. Dinkel, V. Koliogiannis, V. Schwarze, and S. Goller, “Artificial intelligence in chest radiography reporting accuracy: added clinical value in the emergency unit setting without 24/7 radiology coverage,” Investigative Radiology, vol. 57, no. 2, pp. 90-98, Feb 1. 2022.
- P. Zhang and M.N. Kamel Boulos, “Generative AI in medicine and healthcare: Promises, opportunities and challenges,” Future Internet, vol. 15, no. 9, p. 286, Aug. 24, 2023.
- Kolli S, Patro P, Sharma R, Sharma A. Classification and Diagnosis of Heart Diseases Using Fuzzy Logic Based on IoT. Advances in Fuzzy-Based Internet of Medical Things (IoMT). 2024 Jun 28:149-62.
- S.K. Sen, S.K. Pani, A.C. Ojha, and S. Dash, “Meta-Learning in Data Classification: An Analysis,” IUP Journal of Computer Sciences, vol. 9, no. 1, p. 14, 2015.
- K. Vembandasamy, R. Sasipriya, and E. Deepa, “Heart diseases detection using Naive Bayes algorithm,” International Journal of Innovative Science, Engineering & Technology, vol. 2, no. 9, pp. 441-444, Sep. 2015.
- Sarwar and, V. Sharma, “Comparative analysis of machine learning techniques in prognosis of type II diabetes,” AI & Society, vol. 29, pp. 123-129, Feb. 2014.
- Top of Form.
- H. Liu, Z. Zhang, Y. Xu, N. Wang, Y. Huang, Z. Yang, R. Jiang, and H. Chen, “Use of BERT (bidirectional encoder representations from transformers)-based deep learning method for extracting evidences in Chinese radiology reports: development of a computer-aided liver cancer diagnosis framework,” Journal of Medical Internet Research, vol. 23, no. 1, p. e19689, Jan. 12, 2021.
- Ali AH, Al-Khalidi FQ. A review of covid-19 detection and diagnosis methods based on deep learning. InAIP Conference Proceedings 2022 Oct 25 (Vol. 2398, No. 1). AIP Publishing.
- N. A. Christakis, Apollo’s Arrow: The Profound and Enduring Impact of Coronavirus on the Way We Live. Hachette UK, Oct. 27, 2020. 2020; 27.
- Y. Karbhari, A. Basu, Z.W. Geem, G.T. Han, and R. Sarkar, “Generation of synthetic chest X-ray images and detection of COVID-19: A deep learning based approach,” Diagnostics, vol. 11, no. 5, p. 895, May 18, 2021.
- N.R. Mannuru, S. Shahriar, Z.A. Teel, T. Wang, B.D. Lund, S. Tijani, C.O. Pohboon, D. Agbaji, J. Alhassan, J. Galley, and R. Kousari, “Artificial intelligence in developing countries: The impact of generative artificial intelligence (AI) technologies for development,” Information Development, pp. 02666669231200628, Sep. 14, 2023.
- C. Gong, C. Jing, X. Chen, C.M. Pun, G. Huang, A. Saha, M. Nieuwoudt, H.X. Li, Y. Hu, and S. Wang, “Generative AI for brain image computing and brain network computing: a review,” Frontiers in Neuroscience, vol. 17, p. 1203104, Jun. 13, 2023.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




