1. Introduction
The field of medical sensors has experienced tremendous growth and transformation over the past few decades, driven by advancements in technology and an increasing demand for more efficient, personalized solutions. These sensors are engineered to detect and measure a variety of biological, chemical, and physical signals, converting these inputs into data that can be interpreted for medical analysis healthcare sensors can range from simple devices, like thermometers and blood pressure monitors, to more complex systems, such as glucose monitors, cardiac monitors, and advanced imaging technologies [
1]. Over the past few decades, the field has seen tremendous growth, fueled by technological advancements that have made sensors more accurate, reliable, and versatile [
2,
3,
4]. Initially developed in the mid-20th century as simple analog devices, medical sensors have evolved into sophisticated tools capable of playing a critical role in diagnostics, monitoring, and treatment. Recent breakthroughs in microfabrication, nanotechnology, and biocompatible materials have enhanced the functionality, sensitivity, and specificity of these sensors[
5].
With the evolving digital technology and microelectronics, modern sensors now offer non-invasive, highly precise solutions that can be tailored to individual patient needs [
6,
7]. The introduction of innovative sensor technologies, such as multifunctional complementary metal-oxide-semiconductor (CMOS) biosensors and neural probes, has further expanded the potential applications of medical sensors in fields like brain-machine interfaces and point-of-care diagnostics. As the medical industry continues to move toward personalized medicine and decentralized care, the role of medical sensors becomes increasingly vital [
8].
One notable advancement is the development of machine learning-based platforms for continuous glucose monitoring through sweat analysis, enabling non-invasive diabetes management [
9]. Additionally, smart bandages powered wirelessly are being introduced for chronic wound care, promoting healing without the need for constant external interventions [
10]. These innovations are transforming patient care by improving the accuracy and convenience of health monitoring.
Wearable biosensors have also emerged as key tools in health diagnostics and monitoring. For instance, laser-engraved sensors can now detect specific biomarkers such as uric acid and tyrosine in sweat, which are essential for metabolic and nutritional assessments [
11] . Electrochemical biosensors have similarly shown promise in tracking metabolites and nutrients in real-time, offering valuable insights for both fitness tracking and clinical diagnostics [
12]. Furthermore, digitally connected body platforms into wearable devices is enabling continuous, holistic health insights, illustrating the potential of fully integrated health monitoring systems [
13].
Beyond personal health management, wearable sensors are finding applications in clinical settings and disease prevention. The hospital bed systems equipped with load cell arrays provide continuous, non-invasive heart monitoring through ballisto-cardiogram (BCG) signals, improving patient care without the need for direct intervention [
14]. Wearable systems for the early detection of heat stroke and biosensors designed for continuous health tracking emphasize the role of sensors in preventive medicine and fitness tracking [
15,
16]. Together, these advancements highlight the growing impact of biosensors and wearable devices in shaping the future of healthcare, enabling more personalized, accurate, and real-time health solutions [
17,
18].
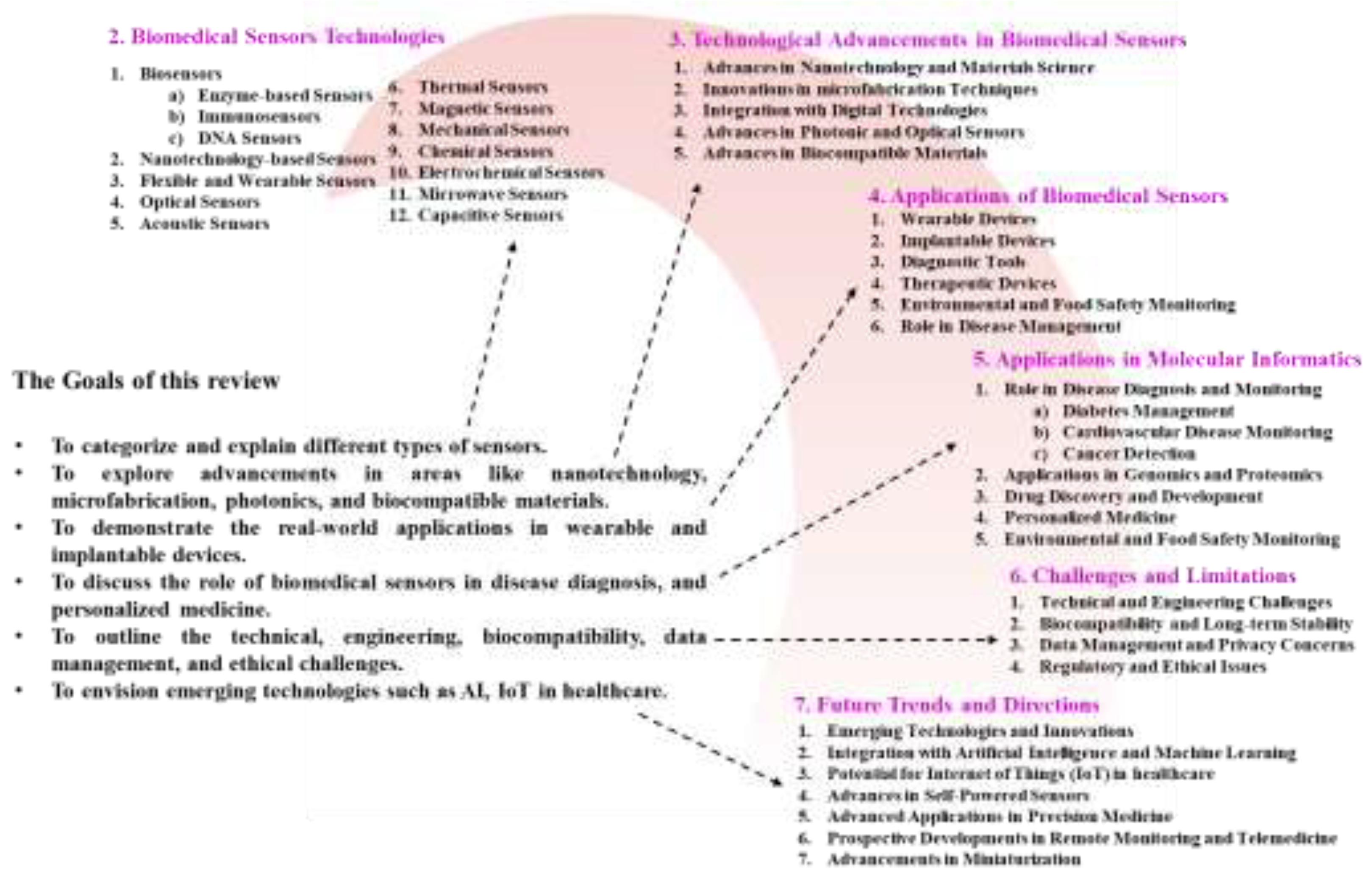
Figure 1 shows structural layout of this review.
The primary goal of this review is to provide a thorough overview of the current landscape of biomedical sensor technology, focusing on the key technological advancements that have fueled their progress. These advancements include innovations in microfabrication, nanotechnology, and the use of biocompatible materials, which have collectively improved the accuracy, reliability, and versatility of medical sensors. Additionally, the review explores the diverse applications of these sensors in molecular informatics, such as their roles in genomics, proteomics, drug discovery, and personalized medicine. Furthermore, the review will address the challenges and limitations that currently impede the full potential of biomedical sensors. These challenges include technical and engineering hurdles, biocompatibility issues, concerns over data management and privacy, and regulatory and ethical considerations. By identifying these obstacles, the review aims to suggest potential solutions and offer guidance for future research.
2. Biomedical Sensors Technologies
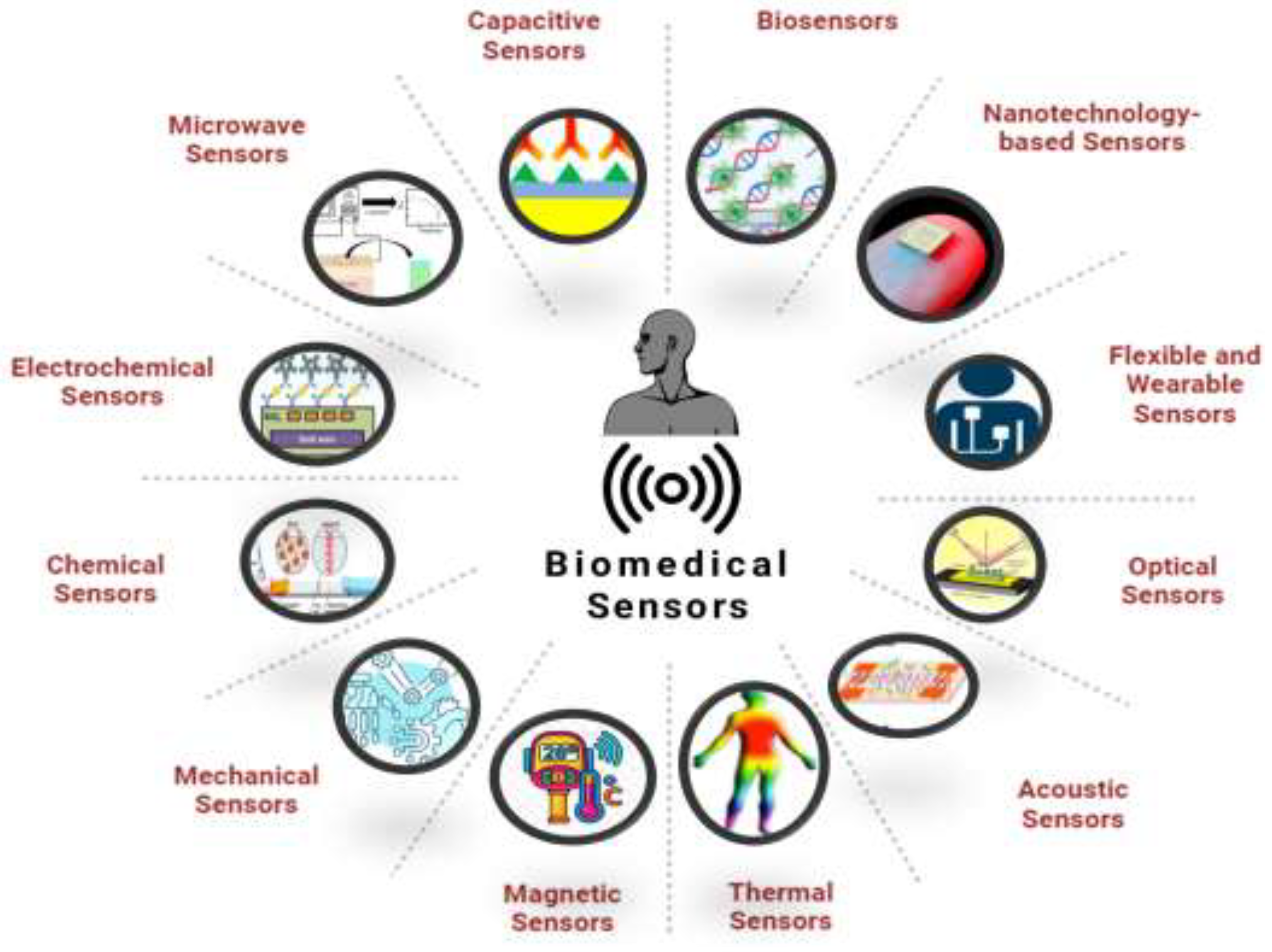
These sensors are now integral to non-invasive and real-time health monitoring, offering innovative solutions for managing chronic diseases, early disease detection, and personalized healthcare. The sensors convert physiological data into electronic signals that can be analyzed and interpreted, enabling medical professionals to diagnose, monitor, and treat medical conditions with greater accuracy and efficiency [
19]. The range of biomedical sensors includes various types, each tailored to specific applications and environments. Biosensors, for instance, are widely used for detecting specific biological molecules, making them crucial in diagnostics, especially for glucose monitoring in diabetes management [
20,
21]. Nanotechnology-based sensors leverage the unique properties of nanomaterials to enhance sensitivity and specificity, opening new frontiers in detecting and treating diseases at the molecular level [
22,
23,
24,
25]. Flexible and wearable sensors are revolutionizing patient monitoring by offering comfortable, continuous tracking of vital signs, allowing for real-time data collection without impeding the patient’s daily activities [
8,
26]. Other types include optical sensors, which are used in imaging and detecting optical changes in biological tissues, and electrochemical sensors, which are often employed in measuring ion concentrations and metabolic activities [
27,
28]. Thermal sensors detect temperature changes, crucial for monitoring inflammation or fever, while mechanical sensors measure forces and pressures within the body, essential in cardiovascular and orthopedic applications [
29,
30]. Magnetic, microwave, capacitive, chemical, and acoustic sensors each have specialized uses, from detecting magnetic fields in imaging technologies to monitoring chemical reactions and sound waves in the body [
34]. Collectively, these diverse sensor technologies form the backbone of modern diagnostic and therapeutic tools, continuously evolving to meet the growing demands of healthcare innovation [
31,
32,
33].
2.1. Biosensors
2.1.1. Enzyme-Based Sensors
Enzyme-based biosensors distinguished by their ability to utilize biological molecules for the highly specific detection of various analytes [
34]. These sensors integrate a biological recognition element—such as enzymes, antibodies, which converts the biological interaction into a measurable signal. The nanostructured materials like titanium oxide hybrids, have noticeably impacted the sensitivity and performance of these sensors, enabling faster and more accurate diagnosis. These nanomaterials increase the surface area for enzyme-analyte interactions, improving the efficiency of electrochemical biosensors. Additionally, innovations in materials for implantable enzyme-based sensors are enabling real-time, in-body monitoring for personalized diagnostics and treatments, offering continuous health insights and improving patient outcomes through advanced biosensing platforms [
35,
36,
37].
2.1.2. Immunosensors
Immunosensors are a critical class of biosensors designed to detect specific antigens or antibodies through selective immune responses, making them highly valuable in diagnostics and real-time health monitoring. These sensors are commonly used for detecting disease biomarkers, offering a high degree of specificity and sensitivity, which is essential for accurate medical diagnostics. Recent advancements in immunosensors have leveraged innovative materials, such as piezoelectric and black phosphorus-based components, to enhance sensor performance. Piezoelectric immunosensors, for instance, utilize mechanical vibrations to detect biomolecules, providing highly sensitive measurements for both medical and environmental applications [
38].
Figure 2 shows various biomedical sensor types.
Black phosphorus-based electrochemical sensors have also emerged as promising platforms for immune sensing due to their excellent electrochemical activity and high sensitivity, which are particularly beneficial for biomedical diagnostics [
39]. Additionally, advances in multiplexed sensing formats and solid-state biosensors have improved the ability to measure multiple analytes simultaneously at low concentrations, enabling real-time biochemical monitoring [
39,
40,
41]. These innovations are driving the future of immunosensors, expanding their applications for more precise, durable, and effective disease detection and monitoring.
2.1.3. DNA Sensors
DNA (Deoxyribonucleic Acid) sensors are an advanced class of biosensors designed to detect specific sequences of DNA, making them essential tools for genetic diagnostics and molecular research. These sensors play a critical role in identifying genetic mutations, detecting pathogens, and monitoring disease progression. Recent advancements in DNA sensor technology have focused on improving sensitivity, specificity, and performance through innovative approaches, such as the integration of redox-active labels and advanced nanostructures. For instance, the use of common oxazine fluorophores as redox labels in electrochemical DNA sensors has been shown to enhance detection sensitivity, [
42]. Research into DNA-sensing inflammasomes has provided insights into their role in recurrent atherosclerotic stroke, highlighting potential therapeutic targets for preventing stroke recurrence [
43]. Similarly, DNA sensors have been used in studying tumor progression, as in the case of identifying mRNA expression signatures related to lung cancer through RNA sequencing [
44]. Furthermore, advances in Cas9-based biosensing technologies, using barcoded DNA nanostructures in solid-state nanopores, have opened up new possibilities for genetic diagnostics, particularly in detecting DNA mismatches [
45]. These innovations in DNA sensor technology continue to expand their applications, enabling more precise, real-time genetic analysis and disease monitoring.
2.2. Nanotechnology-Based Sensors
Nanotechnology-based sensors represent a cutting-edge class of biomedical sensors that utilize the unique properties of nanomaterials to achieve unprecedented sensitivity, specificity, and functionality in detecting a wide range of biological and chemical analytes. These sensors leverage materials at the nanoscale—such as nanoparticles, nanotubes, nanowires, and quantum dots—whose small size and large surface area-to-volume ratio enhance their interaction with target molecules, leading to more efficient and precise detection mechanisms. Nanotechnology-based sensors are used across various applications, including disease diagnostics, environmental monitoring, and drug development [
46]. For instance, gold nanoparticles are often used in colorimetric assays due to their ability to change color in response to binding events, while carbon nanotubes and silicon nanowires are employed in electronic sensors for their excellent conductivity and high surface reactivity [
47]. These sensors are particularly effective in detecting low concentrations of biomarkers, making them ideal for early disease detection, such as in cancer and infectious diseases, where early intervention is critical. The combination of nanotechnology with other advanced technologies, such as microfluidics and lab-on-a-chip systems, improve the capabilities of these sensors, enabling the development of portable, real-time diagnostic tools that can be used at the point of care. As research in nanotechnology continues to progress, nanotechnology-based sensors are expected to play an increasingly vital role in addressing global health challenges [
48,
49,
50,
51].
2.3. Flexible and Wearable Sensors
Flexible and wearable sensors represent a rapidly growing area within biomedical sensor technology, designed to conform to the body's contours and provide continuous, real-time monitoring of physiological parameters with minimal discomfort to the user. These sensors are constructed from flexible materials, such as stretchable polymers and conductive fabrics, which allow them to be integrated seamlessly into clothing, accessories, or directly onto the skin. The flexibility and adaptability of these sensors make them particularly well-suited for long-term monitoring applications, such as tracking heart rate, body temperature, hydration levels, and other vital signs during daily activities, sports, or rehabilitation [
52].
Wearable sensors have found widespread application in both consumer health and clinical settings. In consumer health, devices like fitness trackers and smartwatches equipped with flexible sensors provide users with insights into their physical activity, sleep patterns, and overall well-being. In clinical environments, wearable sensors enable continuous monitoring of patients with chronic conditions, such as diabetes or cardiovascular disease, reducing the need for frequent hospital visits and allowing for more personalized and proactive medical management. For instance, CGMs use flexible sensors to track blood glucose levels throughout the day, providing critical data that helps manage diabetes more effectively [
53]. As shown in
Table 1, each sensor type offers specific application specific advantages and limitations.
The use of these sensors with wireless communication technologies and mobile applications upgraded their utility by enabling real-time data transmission to healthcare providers or caregivers, facilitating timely interventions and better disease management. As technology advances, the development of self-powered sensors, improved biocompatibility, and enhanced data security measures will likely expand the potential applications of flexible and wearable sensors, making them an integral part of future systems focused on preventive care [
59,
60,
61,
62].
2.4. Optical Sensors
Optical sensors are a vital type of biomedical sensor that leverage light to detect and measure various biological and chemical properties within the body. By emitting light into a sample and analyzing the resulting interactions such as absorption, reflection, or fluorescence these sensors provide non-invasive, real-time data crucial for medical diagnostics and treatment. Widely used in technologies like pulse oximetry for measuring blood oxygen levels and glucose monitoring systems, these sensors are also central to advanced imaging techniques such as optical coherence tomography (OCT) and fluorescence microscopy, which allow for detailed visualization of tissues and early disease detection. Their versatility extends to therapeutic applications, including photodynamic therapy and laser surgery. Ongoing advancements in photonics, miniaturization, and fiber optics are enhancing the capabilities of optical sensors, making them indispensable tools in both diagnostic and therapeutic settings [
63,
64].
2.5. Acoustic Sensors
Acoustic sensors, also known as sound or ultrasonic sensors, are a specialized type of biomedical sensor that utilize sound waves to detect and measure various physiological parameters and biological processes. These sensors operate by emitting sound waves into the body and analyzing the reflected waves to gather information about internal structures or fluid dynamics. The most common application of acoustic sensors is in medical ultrasound imaging, where high-frequency sound waves create detailed images of organs, tissues, and blood flow, aiding in the diagnosis and monitoring of conditions such as heart disease, pregnancy, and abdominal disorders. Acoustic sensors are also used in non-invasive monitoring devices, such as those measuring blood pressure or detecting respiratory sounds [
65,
66,
67,
68].
2.6. Thermal Sensors
Thermal sensors sensors are widely used in medical diagnostics, wearable health monitoring devices, and therapeutic applications. Recent advancements in thermal sensor technology have focused on enhancing sensitivity, accuracy, and user comfort, particularly in wearable devices. One notable development is the use of stretchable composite conductive materials, such as graphene-hydrogel, which offer superior performance in thermal and humidity management. This double-layer material not only improves the linear sensing range but also enhances the comfort and flexibility of health monitoring systems, making it ideal for continuous, non-invasive monitoring of body temperature in wearable devices [
69].
These advancements in thermal sensor technology are essential for applications such as fever detection, monitoring metabolic changes, and managing chronic conditions. By integrating innovative materials and enhancing the responsiveness of thermal sensors, healthcare devices can provide more reliable and real-time temperature monitoring.
2.7. Magnetic Sensors
Magnetic sensors are widely used in medical imaging technologies, such as Magnetic Resonance Imaging (MRI), where they play a critical role in producing detailed images of the body's internal structures without the need for invasive procedures. Moreover, to imaging, magnetic sensors are utilized in tracking the movement of magnetic particles within the body, which is particularly useful in targeted drug delivery systems and in monitoring blood flow or detecting the presence of specific biomarkers. The high sensitivity and non-invasive nature of magnetic sensors make them ideal for applications in neurology, cardiology, and oncology, where precise monitoring and imaging are crucial. Advances in magnetic sensor technology, including the development of more compact and sensitive devices, continue to expand their capabilities and applications, making them indispensable tools in both clinical diagnostics and therapeutic interventions [
23,
70,
71].
2.8. Mechanical Sensors
Mechanical sensors are a critical category of biomedical sensors that detect and measure physical forces or mechanical changes within the body, providing essential data for a wide range of medical applications. These sensors operate by converting mechanical stimuli—such as pressure, strain, force, or displacement—into electrical signals that can be quantified and analyzed. Mechanical sensors are extensively used in monitoring vital signs, such as blood pressure and respiratory rate, where they measure the pressure exerted by blood flow or air movement. In orthopedics, mechanical sensors are employed to assess joint movement and load distribution, aiding in the diagnosis and rehabilitation of musculoskeletal conditions. They are also integral to cardiovascular devices, such as heart valves and stents, where they monitor the mechanical integrity and performance of implanted devices. Additionally, mechanical sensors are used in wearable technologies that track physical activity and body posture, contributing to personalized health monitoring and fitness tracking. With ongoing advancements in microfabrication and material science, mechanical sensors are becoming increasingly miniaturized, biocompatible, and sensitive, enhancing their effectiveness in both invasive and non-invasive medical applications. These developments continue to expand the role of mechanical sensors in improving patient care and enabling more precise and responsive healthcare interventions [
29,
72,
73].
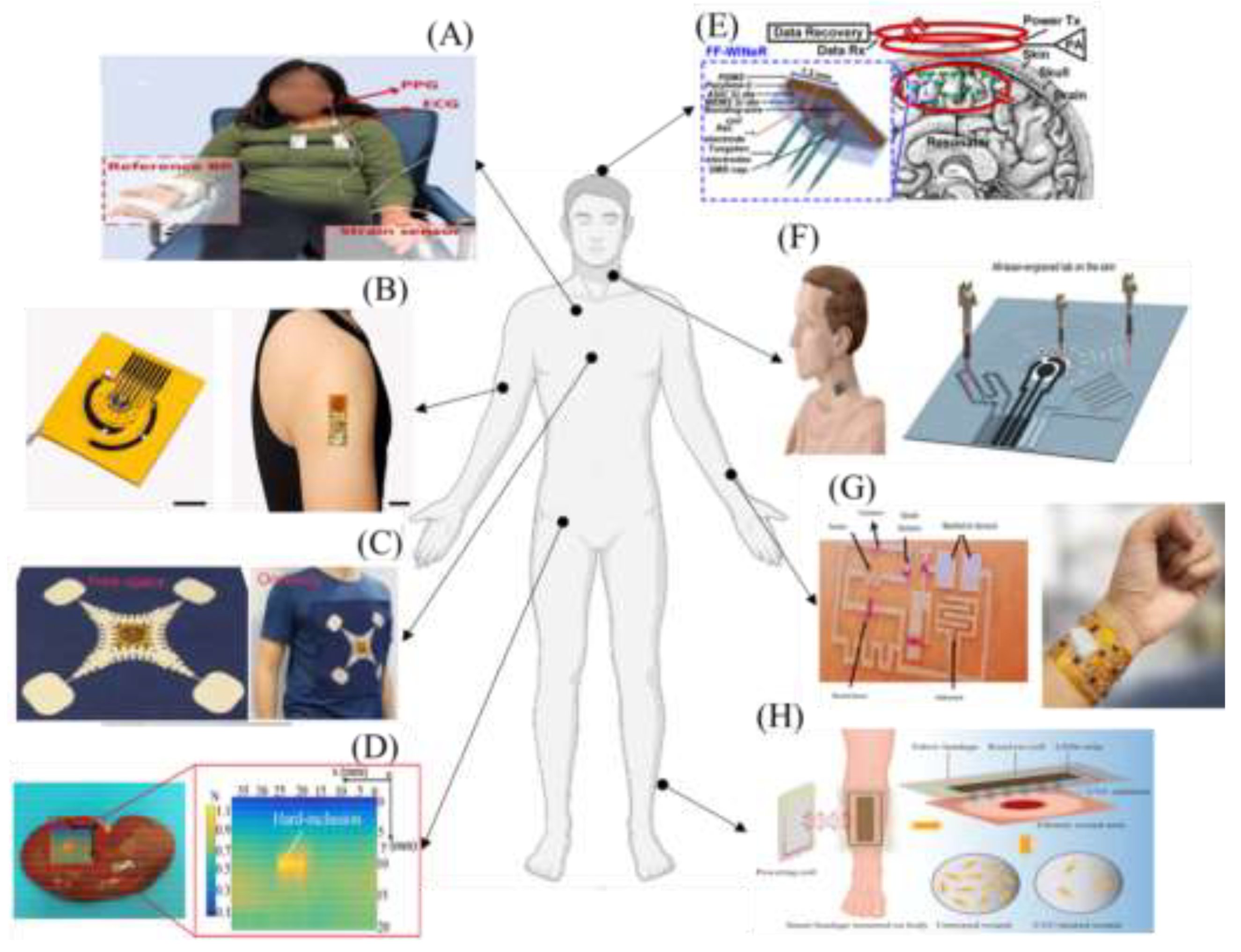
Figure 3 illustrates key body regions where biomedical sensors are applied for continuous monitoring, early diagnostics, and personalized treatments, showcasing a variety of sensor technologies.
2.9. Chemical Sensors
Chemical sensors are a vital type of biomedical sensor designed to detect and quantify specific chemical substances within the body or in biological samples. These sensors operate by interacting with the target chemical, such as ions, gases, or organic molecules, and converting this interaction into a measurable signal, often through electrochemical, optical, or mass-sensitive methods. Chemical sensors are widely used in clinical diagnostics, environmental monitoring, and point-of-care testing due to their ability to provide rapid, accurate, and specific detection of chemical analytes. In healthcare, they are commonly employed in blood gas analyzers, glucose monitors, and pH meters, where they measure critical parameters like blood oxygen levels, glucose concentration, and acidity, which are essential for managing conditions such as diabetes, respiratory diseases, and metabolic disorders. Chemical sensors are also integral to detecting biomarkers in bodily fluids, aiding in the early diagnosis of diseases, monitoring treatment efficacy, and personalizing medical interventions [
74,
75,
76,
77].
2.10. Electrochemical Sensors
Electrochemical sensors are widely used in various medical and clinical applications due to their high sensitivity, specificity, and rapid response time. One of the most common examples is the glucose sensor used in blood glucose monitors for diabetes management, where the sensor detects glucose levels through an enzymatic reaction that produces an electrical signal proportional to the glucose concentration. Additionally, electrochemical sensors are used in detecting electrolytes, pH levels, and other critical biomarkers in blood, urine, and other bodily fluids, providing essential information for diagnosing and monitoring a wide range of conditions, from metabolic disorders to cardiovascular diseases. The continued development of electrochemical sensors, including advances in nanomaterials and microfabrication, is enhancing their performance, making them more robust, portable, and capable of multiplexing—allowing simultaneous detection of multiple analytes. This makes electrochemical sensors an integral part of both point-of-care diagnostics and continuous monitoring systems [
78,
79,
80].
2.11. Microwave Sensors
Microwave sensors are a specialized type of biomedical sensor that utilize microwave radiation to detect and measure various physiological parameters within the body. These sensors operate by emitting microwaves and analyzing the reflected or transmitted signals, which are affected by the dielectric properties of the tissues they interact with. Microwave sensors are emerging as powerful tools in medical diagnostics and monitoring due to their ability to detect physiological changes non-invasively. These sensors operate by using microwave frequencies to monitor various health parameters, offering an alternative to traditional methods. One promising application is in blood glucose monitoring, where microwave biomedical sensors are being developed for stable and non-invasive glucose measurement. Preliminary studies have shown that microwave sensors could provide a reliable solution for continuous glucose monitoring, potentially improving diabetes management without the need for invasive procedures [
1]. Additionally, microwave sensors are being explored for use in neural implants and gastrointestinal devices, where they can enhance communication and sensing capabilities through on-chip transistor switching technology. This innovation allows for improved wireless sensing in medical implants, offering more efficient and reliable monitoring [
81]. Furthermore, advanced systems using phased-array radar sensors have demonstrated the ability to monitor vital signs such as heart rate and respiration. These microwave-based systems show great potential for applications in remote health monitoring, enabling continuous, multimodal health tracking in non-clinical settings [
82].
2.12. Capacitive Sensors
Capacitive sensors are particularly valued for their sensitivity and ability to detect subtle changes in proximity, pressure, and tissue composition, making them useful in a variety of medical applications. In healthcare, capacitive sensors are commonly used in touch-sensitive medical devices, as well as in monitoring physiological parameters such as heart rate, respiration, and body position. They are also employed in wearable devices to monitor hydration levels, skin conditions, and even in smart bandages that can track wound healing processes. The non-invasive nature and low power consumption of capacitive sensors make them ideal for continuous monitoring applications. Advances in sensor materials and miniaturization techniques continue to enhance the performance and versatility of capacitive sensors, expanding their role in the development of innovative medical devices [
83,
84,
85].
3. Technological Advancements in Biomedical Sensors
The field of biomedical sensors has witnessed significant technological advancements over the past few decades, driving the evolution of more sophisticated, accurate, and versatile devices that are integral to modern medicine. These advancements are the result of innovations across various domains, including materials science, microfabrication, nanotechnology, and digital integration, all of which have collectively enhanced the performance and broadened the applications areas.
One of the most transformative areas of advancement has been in nanotechnology. The development of nanoscale materials and structures has led to the creation of sensors with dramatically improved sensitivity and specificity. Nanomaterials such as nanoparticles, nanotubes, and nanowires have been integrated into sensors, enabling the detection of extremely low concentrations of biomarkers, which is crucial for the early diagnosis of diseases like cancer. Additionally, these nanostructures often exhibit unique properties, such as enhanced conductivity and reactivity, which can be exploited to improve the functionality of biosensors, optical sensors, and electrochemical sensors.
Another critical area of progress is in microfabrication techniques, which have allowed for the miniaturization of sensors, making them more portable, less invasive, and suitable for wearable and implantable devices. These techniques have enabled the production of MEMS, which are used in a variety of biomedical applications, from pressure sensors in cardiovascular devices to accelerometers in activity trackers. The ability to fabricate sensors at the microscale has also opened up possibilities for lab-on-a-chip technologies, which can perform complex analyses using only tiny amounts of biological samples, thus reducing the need for invasive procedures [
86,
87,
88,
89].
Furthermore, AI and ML algorithms can process the vast amounts of data generated by sensors, enabling real-time analysis, pattern recognition, and predictive modeling, to improve diagnostic accuracy and treatment personalization. Meanwhile, IoT connectivity allows sensors to communicate seamlessly with other devices and systems, facilitating continuous monitoring, remote patient management, and the development of smart medical environments [
55,
72,
90].
3.1. Advances in Nanotechnology and Materials Science
Advances in nanotechnology and materials science have revolutionized sensors design and development by enabling the development of highly sensitive, specific, and multifunctional devices. Nanomaterials like gold nanoparticles, carbon nanotubes, and graphene, with their unique properties such as high surface area-to-volume ratios and exceptional conductivity, show good performance in detecting ultra-low concentrations of biomarkers, crucial for early disease diagnosis. These materials are integral to improving the functionality of biosensors, optical sensors, and electrochemical sensors. Concurrently, breakthroughs in materials science have led to the creation of biocompatible, flexible, and durable materials, ideal for wearable and implantable sensors. These innovations ensure that sensors can operate effectively within the human body, offering continuous, non-invasive monitoring while maintaining stability and longevity. The synergy between nanotechnology and materials science is driving the evolution of next-generation advancements in sensor technologies [
91,
92].
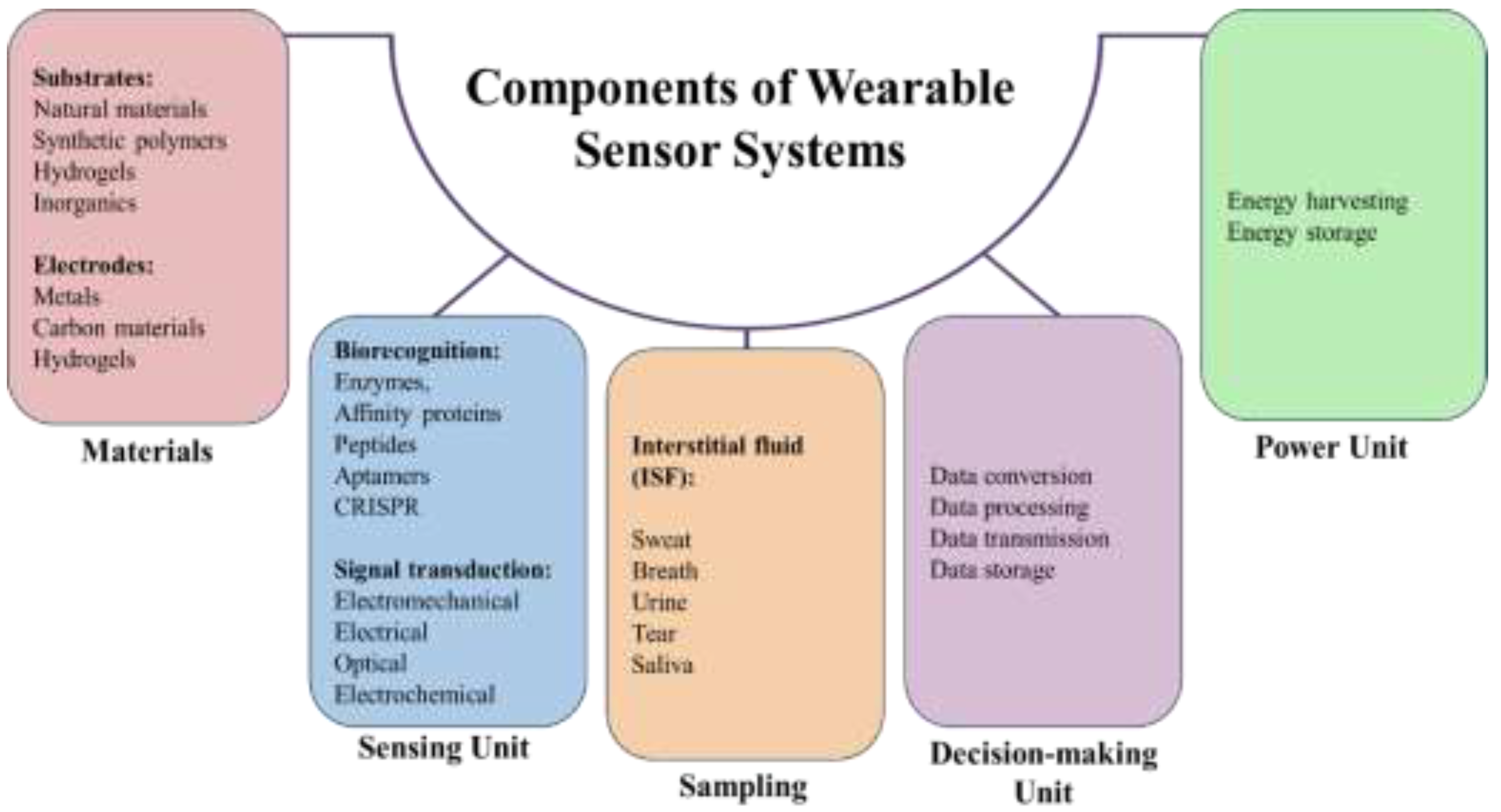
Figure 4 highlights the key components of wearable biomedical sensors design.
3.2. Innovations in Microfabrication Techniques
Microfabrication techniques have enabled more precise, sensitive, and non-invasive health monitoring solutions. One notable innovation is the introduction of MEMS-based technologies, such as the fingertip strain plethysmography technique for cuffless blood pressure estimation. This method allows for continuous and comfortable monitoring of blood pressure, offering a non-invasive alternative to traditional cuff-based systems [
67]. These approaches demonstrate the potential of microfabrication in creating compact, efficient, and wearable health monitoring devices.
In addition to MEMS technologies, the use of nano-structured sensing surfaces has revolutionized sensor fabrication. Nanotechnology has been instrumental in improving the sensitivity and performance of chemical and biological sensors, making them more effective for healthcare applications. These nano-structured surfaces enable sensors to detect biomolecules with higher accuracy and at lower concentrations, which is crucial for advanced diagnostics [
93]. Microfabrication innovations are being applied to biomolecular sensors for real-time physiological monitoring, helping improve the precision and reliability of health tracking systems, particularly for personalized healthcare solutions [
79]. These advances in microfabrication techniques are driving the future of biomedical sensor technology, enabling more effective, patient-centered healthcare.
3.3. Integration with Digital Technologies
Medical sensors with connectivity features such as Bluetooth, Wi-Fi, and cellular networks, data collected by these sensors can be transmitted instantly to healthcare providers, enabling continuous remote monitoring of patients [
94]. This connectivity is a cornerstone of the IoT in healthcare, where networks of interconnected devices provide comprehensive health insights and facilitate timely interventions [
95]. The application of AI and ML algorithms to the vast datasets generated by these sensors enhances diagnostic accuracy by identifying patterns and predicting outcomes with greater precision. These technologies also support the automation of data analysis, reducing the workload on health management and improving patient care efficiency [
96]. Additionally, digital platforms and mobile applications integrated with sensors empower patients to track their health metrics in real-time, fostering proactive health management and engagement [
55,
56,
72,
90].
3.4. Advances in Photonic and Optical Sensors
Advances in photonic and optical sensor technologies use used for the precision, sensitivity, and versatility of biomedical sensors, making them indispensable tools in modern healthcare. Photonic sensors operate by detecting and analyzing light interactions with biological tissues, providing non-invasive and real-time monitoring of various physiological parameters. Recent developments in this field have led to the creation of highly sensitive sensors capable of detecting minute changes in optical properties, which are crucial for early disease diagnosis and monitoring. Innovations such as OCT, fluorescence-based sensing, and Raman spectroscopy have expanded the applications of optical sensors in imaging, diagnostics, and therapeutic monitoring. These sensors are now widely used in ophthalmology for retinal imaging, oncology for tumor detection, and cardiology for assessing vascular health. Additionally, the miniaturization of photonic components and The incorporation of optical sensors with digital technologies have enabled the development of portable and wearable devices [
36,
97,
98].
3.5. Advances in Biocompatible Materials
Advances in biocompatible materials have been crucial in the evolution of biomedical sensors, enabling the development of devices that can safely and effectively interact with biological systems over extended periods. Biocompatible materials are designed to minimize adverse reactions when in contact with body tissues, making them essential for wearable and implantable sensors. Recent progress in materials science has led to the creation of new polymers, hydrogels, and nanocomposites that not only enhance the biocompatibility of sensors but also improve their mechanical properties, such as flexibility, stretchability, and durability. These materials allow sensors to conform to the dynamic movements of the body, ensuring consistent and accurate data collection without causing discomfort or irritation to the patient. Moreover, innovations in self-healing and biodegradable materials are paving the way for next-generation sensors that can repair themselves if damaged or safely dissolve after their intended use, reducing the need for surgical removal. The development of advanced biocompatible materials is thus a key driver in the creation of more reliable, long-lasting, and patient-friendly biomedical sensors, ultimately contributing to better health monitoring, diagnosis, and treatment outcomes [
65,
99,
100].
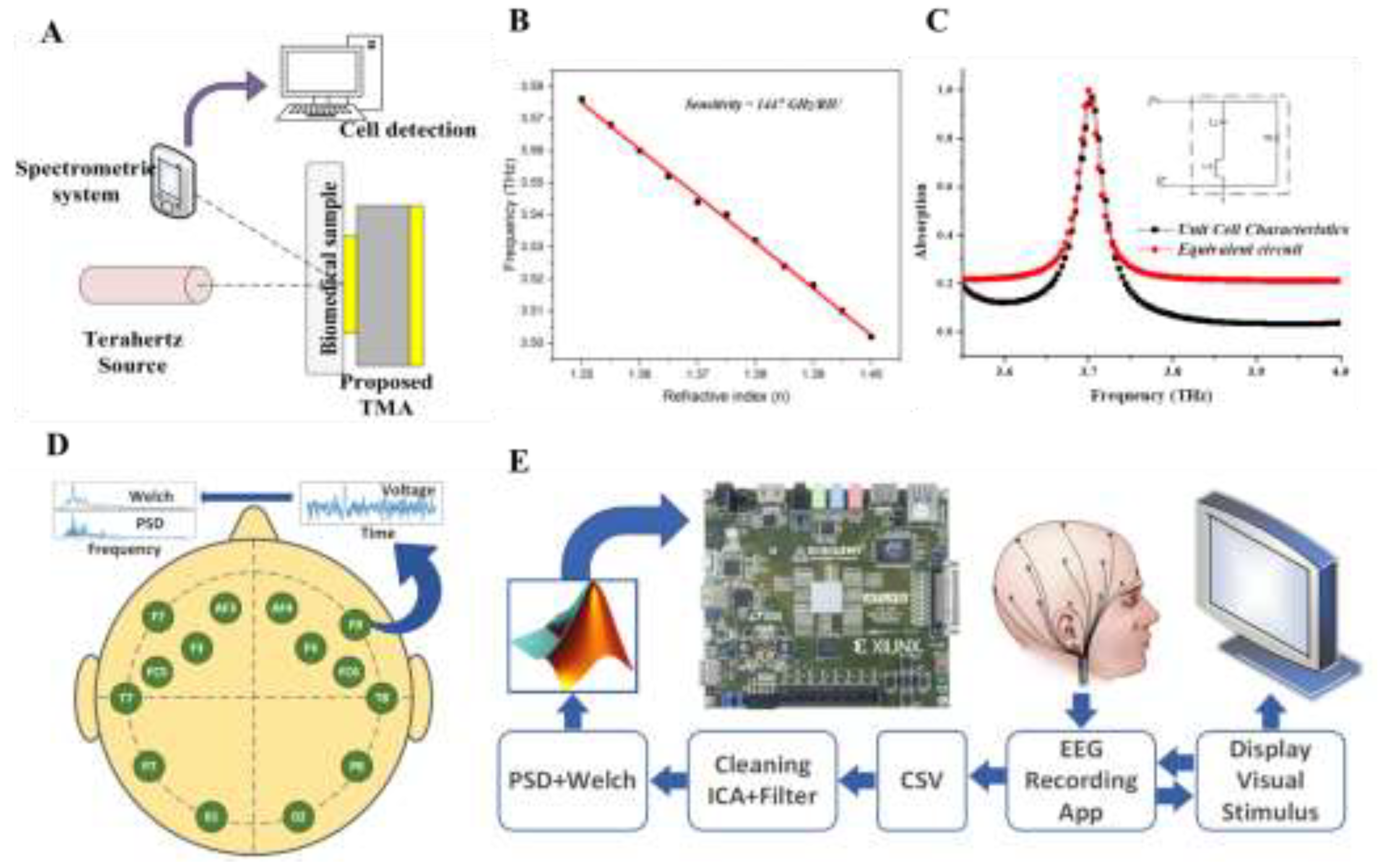
Figure 5 illustrates a variety of biomedical sensor systems, including a cancer cell detection system using terahertz metamaterial absorbers and an EEG data acquisition setup for brain activity monitoring.
4. Applications of Biomedical Sensors
Biomedical sensors provide real-time data and insights, offering patients and healthcare providers tools to manage chronic conditions and respond to health changes more efficiently [
102]. As these technologies evolve, their applications will continue to broaden, advancing healthcare outcomes and improving patient well-being. The primary applications of biomedical sensors include:
- o
Wearable Devices
- o
Implantable Devices
- o
Diagnostic Tools
- o
Therapeutic Devices
- o
Environmental and Food Safety Monitoring
- o
Role in Disease Management
Wearable devices, such as fitness trackers and smartwatches, monitor vital signs like heart rate, blood pressure, and glucose levels, enabling individuals to take proactive control of their health. These sensors are particularly valuable for chronic disease management, providing real-time data that facilitates early intervention. Additionally, implantable devices like pacemakers and CGMs offer continuous internal monitoring of critical health parameters. These technologies ensure precise management of chronic conditions, such as heart rhythm disorders and diabetes, by reducing the risk of complications through real-time feedback [
103,
104,
105].
Devices like blood glucose meters and blood gas analyzers support swift medical interventions, particularly in remote or resource-limited settings. Therapeutic devices, such as insulin pumps and neurostimulators, enhance treatment delivery by continuously monitoring physiological parameters and making real-time adjustments, ensuring personalized and precise therapy. Beyond healthcare, sensors are also used to monitor environmental and food safety, detecting contaminants, pathogens, and toxins. This ensures the safety of water, air, and food, preventing potential health hazards and protecting public health.
5. Applications in Molecular Informatics
Biomedical sensors are playing a transformative role in molecular informatics, a field that combines molecular biology with computational techniques to understand, analyze, and manipulate molecular and genetic information. These sensors are integral to various applications that involve the detection, analysis, and quantification of biomolecules, providing critical data that drives research and innovation in, genomics, proteomics, and drug discovery [
106]. One of the key applications of biomedical sensors in molecular informatics is in disease diagnosis and monitoring. Sensors capable of detecting specific biomarkers—such as proteins, nucleic acids, or metabolites—enable the early diagnosis of diseases like cancer, diabetes, and cardiovascular disorders [
107]. For instance, DNA sensors can detect genetic mutations associated with certain cancers, allowing for earlier and more targeted interventions.
Besides protein classification, biosensors are being developed and commercialized for detecting diagnostic biomarkers, contributing to early disease detection and personalized healthcare. These non-invasive biosensors enable real-time monitoring of disease markers, improving diagnostic capabilities and allowing for more targeted treatments [
108]. Advanced sensing technologies, such as the multimodal knee brace used for tracking rheumatoid arthritis progression, exemplify the integration of molecular informatics into wearable devices, offering non-invasive and accurate disease monitoring [
107]. Nanotechnology also plays a pivotal role in molecular informatics. The development of yellow emissive carbon dots as nanoprobes enables highly sensitive quantification of jaundice biomarkers, while also showing potential for targeting cancer cells in therapeutic applications [
109]. Mass spectrometry has advanced molecular diagnostics by improving the detection of biomarkers, facilitating more precise and individualized treatment strategies [
110]. These innovations in molecular informatics are driving the future of diagnostics and treatment monitoring.
5.1. Role in Disease Diagnosis and Monitoring
Molecular informatics plays an increasingly vital role in the diagnosis and monitoring of various diseases by leveraging advanced technologies and data-driven approaches. Infrared monitoring systems have been applied to track oxygenation processes in bedridden patients undergoing physical therapy, offering real-time data that significantly improves patient care and rehabilitation outcomes [
111]. This kind of real-time monitoring highlights the potential of integrating molecular informatics into routine clinical settings for enhanced patient management. Biomedical data mining techniques, combined with AI, data-driven insights allow for more precise diagnoses and individualized treatment plans [
112]. In the context of autoimmune diseases, immune informatics is being utilized to better understand immune system disorders, offering computational tools that assist in diagnosing and monitoring these complex conditions. These approaches support the development of personalized treatment strategies, improving outcomes for patients with immune-related disorders [
113]. Furthermore, modern technologies are being applied to global health challenges, particularly in the surveillance and control of zoonotic diseases. By integrating data-driven solutions, molecular informatics enhances global health response systems, improving the ability to monitor and control emerging infectious diseases [
114].
5.1.1. Diabetes Management
The real-time monitoring helps patients make informed decisions about insulin dosing, diet, and physical activity, thereby reducing the risk of hyperglycemia and hypoglycemia [
115]. Additionally, some CGMs are integrated with insulin pumps, creating a closed-loop system that automatically adjusts insulin delivery based on glucose readings, enhancing glycemic control. The inclusion of these sensors with mobile apps and digital health platforms allows for remote monitoring, where health services providers can access glucose data and provide timely interventions, making diabetes management more personalized and proactive [
116,
117,
118,
119,
120,
121].
5.1.2. Cardiovascular Disease Monitoring
Biomedical sensors play a vital role in the monitoring and management of cardiovascular diseases by providing continuous, real-time data on key physiological parameters such as heart rate, blood pressure, and cardiac rhythms [
14]. Wearable sensors, such as electrocardiogram (ECG) monitors and smartwatches with heart rate tracking capabilities, enable the early detection of arrhythmias, hypertension, and other cardiac abnormalities. These devices can alert patients and doctors to potential issues, allowing for prompt intervention and reducing the risk of severe cardiac events such as heart attacks or strokes [
122]. Additionally, implantable devices like pacemakers and defibrillators are equipped with sensors that monitor the heart's activity and deliver corrective electrical impulses when necessary, ensuring that the heart maintains a healthy rhythm. The data collected by these sensors can be remotely transmitted, facilitating continuous monitoring and more personalized care [
123]. As technology advances, the integration of AI and ML with cardiovascular sensors is expected to enhance predictive analytics, enabling even earlier detection and more precise management of cardiovascular conditions, ultimately improving patient outcomes [
112,
124,
125,
126].
5.1.3. Cancer Detection
For the early detection and monitoring of cancer using the identification of specific biomarkers associated with various types of tumors. Molecular informatics emerged as a new tool for early cancer diagnosis. One such development is the use of biomedical sensors based on terahertz metamaterial absorbers, which have shown high sensitivity in detecting cancer cells. For more accurate identification of malignant cells at earlier stages, which is crucial for improving patient outcomes [
54]. Also, Multimodal image fusion methods, such as those employing self-supervised transformers, have improved the embedding of medical images from different modalities, leading to enhanced image quality and better diagnostic insights. This approach helps medical professionals analyze complex cancer cases with greater precision, facilitating earlier and more reliable diagnoses [
127]. Furthermore, advanced sensor systems like the MRC-based double figure-of-eight coil sensor provide versatile and efficient detection capabilities across various medical applications, including cancer imaging and monitoring. These innovations in both sensor technology and imaging are paving the way for more effective cancer detection and management, offering new opportunities for early intervention and personalized treatment strategies [
128].
5.2. Applications in Genomics and Proteomics
Molecular informatics plays a vital role in advancing the fields of genomics and proteomics by enabling the detailed analysis of genetic and protein data. This has led to breakthroughs in understanding complex biological processes and disease mechanisms. They rely heavily on advanced sensors and bioinformatics tools to detect, analyze, and interpret large volumes of molecular data. Sensor technologies and wearable systems also highlight the growing intersection between bioinformatics and real-time human interaction. Wearable sensors such as spintronic systems integrated into human-computer interfaces demonstrate the versatility of sensing technologies. Though primarily designed for human interaction and accessibility [
129], such innovations reflect the broader trend of leveraging advanced sensing platforms to gather and analyze complex biological data, which can have applications in genomics and proteomics research.
5.3. Drug Discovery and Development
In the field of drug discovery and development, biosensors and advanced sensing technologies play a pivotal role in accelerating the identification and validation of new drug candidates. These sensors are designed to detect specific biological markers, enabling high-throughput screening and real-time monitoring of biochemical reactions, which are critical for early-stage drug discovery. Advances in electrochemical biosensors, for instance, have provided more sensitive and selective detection of biomarkers, facilitating more efficient testing of drug efficacy and safety [
27].
Moreover, wearable sensor technologies are becoming increasingly relevant in clinical trials and drug development. These devices allow for continuous, real-time health monitoring of participants, providing valuable data on the physiological effects of new drug treatments. Innovations like biodegradable and eco-friendly sensors offer sustainable solutions for clinical applications, ensuring that sensors are both versatile and environmentally responsible [
130]. Additionally, personalized sensing approaches, such as meta-learning models for wearable devices, are improving the adaptability and accuracy of health monitoring. These advancements enable more precise data collection, which is essential for evaluating drug effects and optimizing treatment protocols in a personalized manner [
131]. Overall, biosensors and wearable technologies in drug discovery and development is streamlining the process, enhancing the ability to monitor biological responses, and enabling more targeted therapeutic interventions.
5.4. Personalized Medicine
Personalized medicine, which aims to customize treatments based on individual patient characteristics, has greatly benefited from advancements in wearable sensor technology. These sensors allow for real-time, continuous monitoring of physiological parameters, providing critical data that supports more tailored treatment approaches. For instance, wearable sensors have been used to monitor blood volume decompensation, as demonstrated in a study utilizing a porcine model to assess hypovolemia. This research highlights the potential for personalized monitoring in trauma and critical care settings, where timely and accurate data is essential [
132]. In the management of chronic conditions like diabetes, wearable sensors are also proving to be transformative. A machine learning-based platform for on-demand sweat glucose monitoring offers a non-invasive solution for real-time glucose tracking, enabling better control of blood sugar levels through continuous monitoring [
9]. Furthermore, innovations in the design and integration of wearable sensors, particularly with data analytics, are pushing the boundaries of personalized clinical care. These sensors are increasingly being developed with a focus on flexibility, accuracy, and seamless data integration, enabling continuous health monitoring tailored to individual needs and improving overall patient outcomes [
133]. By empowering both patients and clinical care providers with real-time, actionable health data, wearable sensors are playing a pivotal role in the advancement of optimizing treatment strategies, and enhancing disease management.
5.5. Environmental and Food Safety Monitoring
Biosensor technology, originally developed for healthcare, is now extending its reach into environmental and food safety monitoring, offering advanced solutions for detecting contaminants and ensuring safety. Biosensors designed for real-time monitoring can detect harmful substances such as pathogens, toxins, and pollutants, providing immediate feedback to prevent contamination and ensure food safety. The use of spintronic sensors, although primarily applied in fields like assistive technology [
134], demonstrates the versatility of sensor technologies in non-healthcare domains. In environmental monitoring, sensors track pollutants such as heavy metals, volatile organic compounds, and particulate matter, helping to prevent environmental contamination and protect public health. The portability and ease of use of these sensors make them particularly valuable in field applications, allowing for on-site testing and immediate response to potential hazards. As sensor technology advances, their sensitivity, specificity, and integration with digital platforms continue to improve, making environmental and food safety monitoring more effective and accessible, ultimately contributing to a safer and healthier environment. As illustrated in
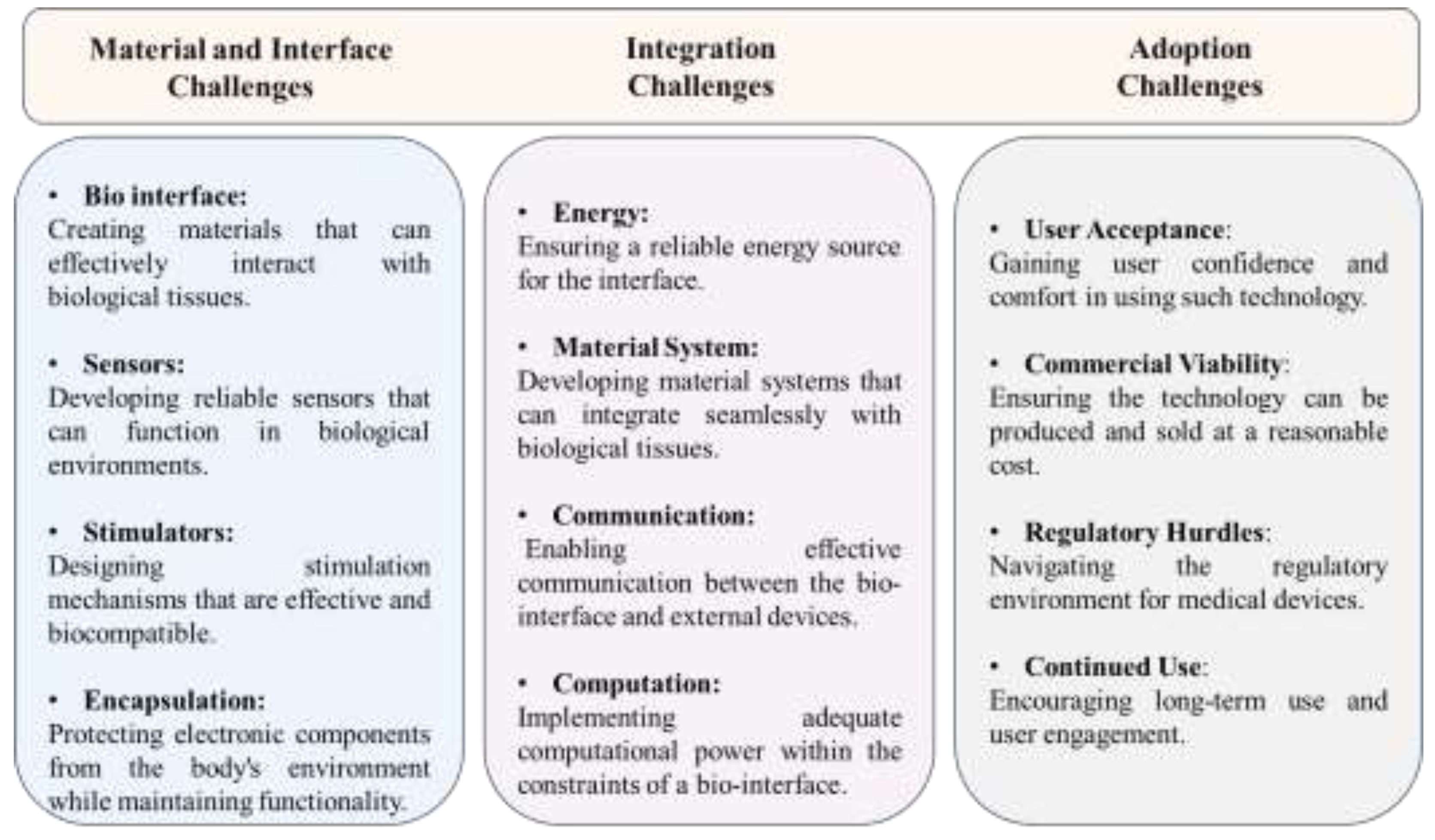
Figure 6, the primary obstacles to advancing bio-interface technologies include material compatibility, system integration, and widespread adoption in clinical settings.
6. Challenges and Limitations
Biomedical sensing technologies face several challenges related to material properties, environmental sensitivity, and long-term reliability. While conducting polymer hydrogels are promising due to their biocompatibility and conductivity, they present difficulties in maintaining stability and durability within the body over time [
3]. This is particularly problematic for wearable and implantable devices, which require consistent performance in diverse biological environments. Material degradation can impair sensor function, limiting their effectiveness in continuous monitoring. Additionally, the sensitivity of these devices to external factors, such as fluctuations in pH and temperature, complicates the development of long-lasting solutions.
Another challenge stems from external interference and the precision required for certain medical diagnostics. Piezoelectric tactile devices, used for tissue hardness measurements, depend on highly accurate readings [
135]. However, external vibrations, such as those experienced in dynamic environments or during physical activity, can disrupt the sensor’s performance, leading to inaccurate data. Seismo-cardiogram signals used in cardiac monitoring are particularly vulnerable to interference, making it difficult to ensure accurate and reliable measurements in real-world scenarios [
58]. Improving sensor design to reduce such interference is essential for maintaining high precision in medical diagnostics.
The health-related systems pose technical and logistical difficulties, particularly regarding data security and system interoperability. As electrochemical biosensors and IoT-enabled devices become more prevalent in health treatment, concerns over data privacy and security are growing [
136]. Ensuring the protection of sensitive health data from cyber threats while facilitating seamless communication between sensors, and patient records remains a challenge. Additionally, achieving interoperability between different sensor technologies and medical devices, such as robotic systems for home care [
137], is crucial for creating integrated, efficient solutions.
6.1. Technical and Engineering Challenges
Biomedical sensors face several technical and engineering challenges that impact their performance and adoption, particularly in the areas of miniaturization, power efficiency, and durability. As sensors become smaller, maintaining accuracy and reliability while integrating multiple sensing functions becomes increasingly complex, requiring advanced microfabrication techniques. Power efficiency is another critical challenge, especially for implantable devices that need to operate continuously over long periods, often necessitating innovative solutions like energy harvesting [
74]. Additionally, ensuring signal stability and noise reduction, along with developing materials that are both biocompatible and durable, is essential for sensors intended for long-term use in the body [
130]. Overcoming these challenges is vital to enhancing the effectiveness and reliability of biomedical sensors [
29,
138,
139].
6.2. Biocompatibility and Long-Term Stability
Biocompatibility and long-term stability are critical challenges, especially for those designed for implantable or long-term use. Biocompatibility refers to the sensor’s ability to function without eliciting an adverse reaction from the body, such as inflammation, immune response, or tissue rejection. Achieving biocompatibility requires the use of materials that are not only non-toxic and non-reactive with body tissues but also capable of withstanding the physiological environment over extended periods. Long-term stability, on the other hand, involves ensuring that the sensor maintains its accuracy, sensitivity, and functionality over time, despite being exposed to various biological fluids, mechanical stress, and potential biofouling, where proteins or cells adhere to the sensor's surface, impairing its performance. Developing sensors that can endure these challenges without degradation or loss of performance is a significant hurdle, requiring advanced materials science, innovative design strategies, and thorough testing to ensure both safety and reliability in clinical applications [
140,
141,
142].
6.3. Data Management and Privacy Concerns
Data management and privacy concerns present challenges in the deployment of biomedical sensors, particularly as these devices generate vast amounts of sensitive health data. Efficiently handling and storing this data requires robust data management systems capable of processing large volumes of information while ensuring accuracy and accessibility for patient care providers. As wearable sensors and biosensing technologies become more integrated into healthcare and other sectors, the volume of collected data continues to grow exponentially, raising concerns around data management and privacy. The collection of sensitive physiological data, such as those from wearable accelerometers used to predict soldier performance, highlights the importance of securely managing large datasets while ensuring privacy [
57]. In healthcare, these devices continuously monitor vital signs, and the potential exposure of personal health information necessitates stringent data protection protocols.
Additionally, the use of advanced sensing technologies, such as those for indoor occupancy detection or tactile classification in robotics, presents challenges in securely storing and transmitting sensor data [
143,
144]. Data management systems must be optimized to handle the vast amounts of data generated by these sensors while protecting user privacy. The challenge lies in balancing the need for real-time data accessibility with robust encryption methods to safeguard sensitive information. Addressing these concerns is critical for maintaining trust in wearable technologies and biosensors, especially as they are increasingly applied in personalized medicine, smart environments, and other data-intensive fields.
6.4. Regulatory and Ethical Issues
Wearable biosensors, increasingly used in healthcare and fitness monitoring, present few regulatory and ethical challenges that must be addressed to ensure their safe and responsible use. Devices that quantify tremor severity in essential tremor patients or recognize human motions raise concerns about the accuracy, safety, and privacy of the collected data. Regulatory standards are needed to ensure these sensors meet clinical requirements for patient safety and effective treatment monitoring [
145,
146]. Additionally, ethical issues such as data security, informed consent, and equitable access must be prioritized to prevent misuse of personal health information and ensure that all individuals benefit from these technologies without exploitation. Addressing these regulatory and ethical concerns is crucial for the continued advancement and integration of wearable biosensors. Ethical issues also play a critical role, particularly concerning informed consent, data ownership, and the potential for misuse of sensitive health information. Patients must be fully informed about how their data will be used, who has access to it, and the potential risks involved
7. Future Trends and Directions
The future of biomedical sensors is set to evolve through several transformative trends, driven by advancements in technology and the growing demand for more personalized, efficient, and accessible medical services. Digital transformation technologies, including AI, ML, and nanorobotics, are reshaping medical care systems to provide more efficient, signaling a leap toward Healthcare 5.0 [
147].
Another promising trend is the development of self-powered and energy-efficient sensors, aimed at addressing the challenge of maintaining power in wearable and implantable devices. Energy harvesting technologies, such as capturing energy from body movements or ambient heat, will allow sensors to operate continuously without the need for frequent battery replacements. This advancement will greatly improve the practicality of sensors for long-term use. Additionally, the IoT will play a pivotal role in the future of sensing systems, creating a connected ecosystem where sensors can communicate seamlessly with other devices, and even patients’ personal health records. Precision medicine will be another focus, leading to the development of sensors tailored to individual genetic and biological profiles. This will enable highly personalized healthcare interventions that align with the broader goals of personalized and precision medicine. Computational approaches will play a crucial role in integrating experimental data with computational models to drive innovations in fields such as regenerative medicine, where personalized therapies are critical [
148,
149]. As shown in
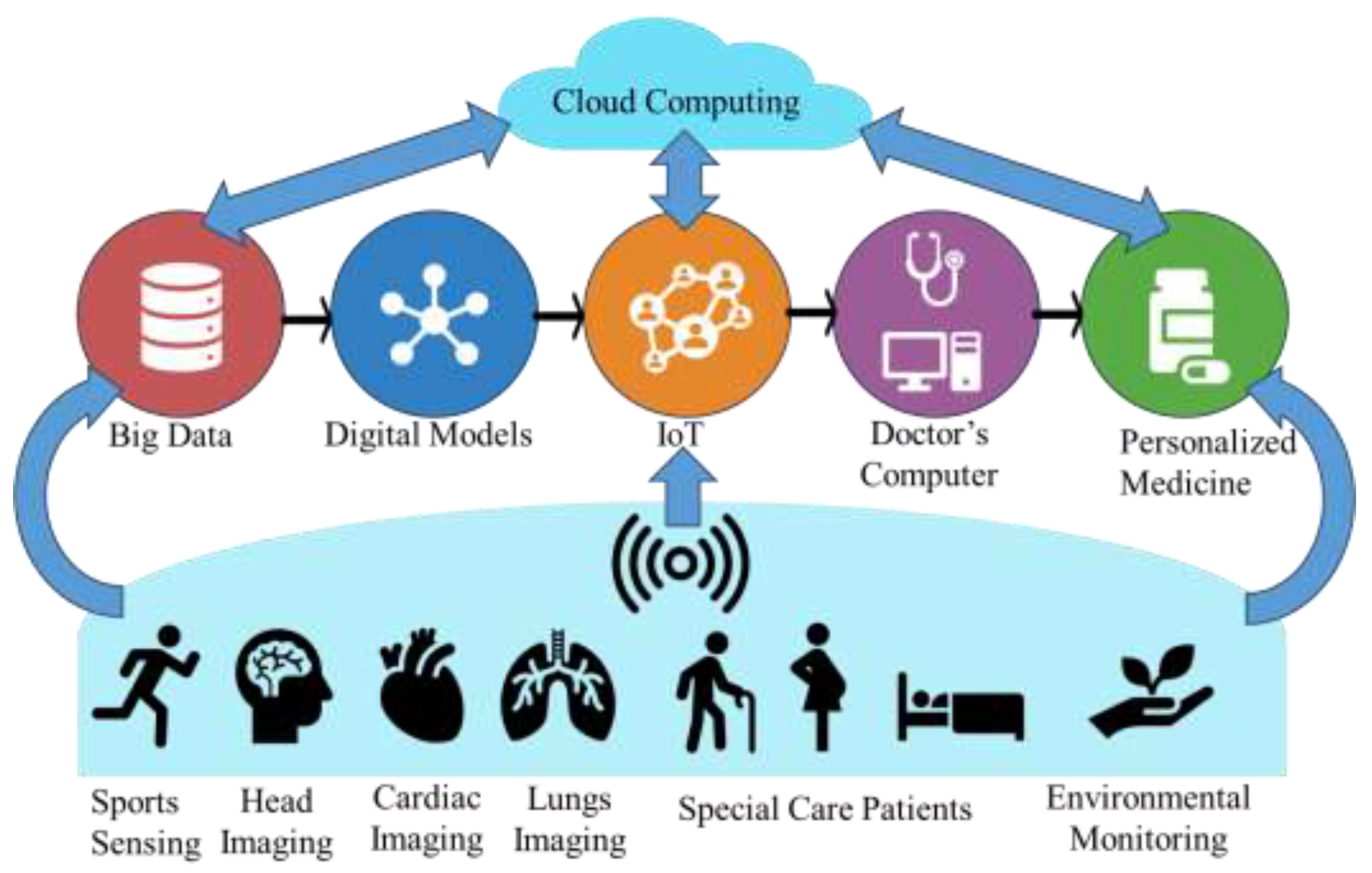
Figure 7, cloud computing AI, IoT, big data and medical sensors plays crucial role in supporting future diagnostics, treatment, and remote patient monitoring, enhancing overall healthcare delivery.
Moreover, innovations in materials informatics, powered by AI tools like MatGPT, will drive the design and testing of new sensor materials with enhanced properties. AI is transforming materials science, helping predict outcomes and facilitating the development of smarter, more durable sensors that meet the evolving needs of biomedical applications [
150,
151]. As these trends converge, biomedical sensors will become increasingly integral to the delivery of personalized, predictive, and preventative healthcare, ultimately revolutionizing healthcare delivery and improving patient outcomes.
7.1. Emerging Technologies and Innovations
The transformation of healthcare informatics is being propelled by modern technologies that are reshaping critical areas such as data management, patient monitoring, and clinical decision-making. One major development is the rise of smart systems that enable real-time health tracking and remote care through interconnected devices. These advancements are improving the ability to monitor patients continuously and make timely clinical decisions.
Along with these innovations, the integration of healthcare informatics with big data analytics is opening new avenues for improving outcomes and efficiency. Predict disease trends, and enhance clinical operations. Predictive modeling is becoming a critical tool in anticipating needs, optimizing treatment plans, and improving patient care. However, challenges such as data integration and ensuring the security of sensitive patient information remain, and addressing these will be key to fully realizing the potential of data-driven medical services [
147,
152,
153].
7.2. Integration with Artificial Intelligence and Machine Learning
Advancements in AI and ML are driving significant progress in genomics. The development of the Deep-4mCGP model has improved the accuracy of predicting epigenetic sites in microbial genomes, such as in Geobacter pickeringii, using correlation-based feature selection. This enhances the understanding of microbial gene regulation and its implications in microbial genomics[
154]. Similarly, machine learning methods have been applied to predict promoters in bacterial strains like Agrobacterium tumefaciens, which has strengthened research in gene regulation and biotechnology applications [
155]. AI tools are improving diagnostics and advancing personalized treatment strategies, particularly in microbial disease management [
156]. Additionally, the application of these technologies in next-generation sequencing (NGS) has improved genomic data analysis, contributing to precision medicine efforts [
157]. In drug discovery, AI models have been instrumental in identifying drug candidates and predicting therapeutic outcomes, streamlining drug development despite the inherent challenges in the field [
158].
7.3. Potential for Internet of Things (IoT) in Healthcare
IoT technologies, such as wireless communication and sensing systems, are being developed for sustainable healthcare solutions, particularly in community health settings. These systems allow for continuous health monitoring and data collection, promoting proactive health management and improving access to services, especially in remote or underserved areas. By integrating IoT devices with systems, patients and providers can benefit from real-time data that supports timely interventions and better overall health outcomes [
159,
160].
IoT’s ability to generate vast amounts of data also complements big data analytics, which can be used for preventive healthcare. By leveraging IoT devices, clinical care providers can gather critical information for early diagnosis and disease prevention. This integration allows for continuous health monitoring and predictive analytics, enabling personalized care through Health 4.0 smart systems. The use of IoT in conjunction with machine learning enhances real-time data processing, making medical care delivery more efficient and targeted to individual patient needs, ultimately improving patient outcomes and the overall quality of care [
161,
162].
7.4. Advances in Self-Powered Sensors
Advances in self-powered sensors are revolutionizing healthcare by enabling energy-efficient devices that operate without external power sources. Utilizing innovative fabrication techniques like printable electronics, these sensors can harvest energy from their surroundings or the human body, making them ideal for long-term applications such as wearables and implantable devices. This continuous, battery-free operation enhances real-time health monitoring and reduces the need for frequent maintenance. Furthermore, machine learning models into sensor systems has improved their sensitivity and precision, allowing for more accurate detection of various stimuli. Although currently applied in areas like perfumery and environmental monitoring, these technologies hold potential, particularly in early disease detection and personalized health management [
61,
163].
7.5. Advanced Applications in Precision Medicine
Precision medicine is increasingly benefiting from advanced technologies, enabling more tailored and effective health treatment solutions. One key area of innovation is the use of molecular docking techniques in drug discovery, which allows researchers to predict drug-target interactions with high accuracy. This approach enables the development of personalized therapies based on individual patient profiles, optimizing treatment outcomes by selecting the most suitable drugs for each patient. These advancements are driving progress in personalized medicine, where treatments are specifically designed for individual genetic and biological characteristics [
164]. Additionally, genomics and other technologies, such as proteomics and metabolomics, is advancing precision medicine. These technologies contribute to a deeper understanding of disease mechanisms at the molecular level, enabling more accurate diagnostics and more personalized therapeutic strategies. The application of these biotechnological advancements in drug discovery is shaping the future of pharmaceutical biotechnology, offering more targeted and effective solutions for personalized medical assistance [
165].
7.6. Prospective Developments in Remote Monitoring and Telemedicine
The future of remote monitoring and telemedicine is poised for growth, driven by technological advancements that promise to enhance patient care and accessibility. In fields such as obstructive sleep apnea (OSA) treatment, telemedicine offers the potential for more effective remote diagnosis and continuous monitoring, improving patient outcomes while increasing access to care through telehealth platforms. These innovations address challenges related to in-person consultations, making healthcare more accessible, especially for patients in remote or underserved areas. Emerging technologies, such as blockchain and AI, are also transforming remote health services. These tools can improve data security and patient privacy while streamlining health management delivery, making telemedicine services more efficient and reliable. As demonstrated by the Telemechron study, ongoing advancements in telehealth technologies are reshaping the landscape of remote monitoring, with trends indicating growth in accessibility and quality of care [
166,
167,
168]. These prospective developments highlight telemedicine’s potential to become an integral component of healthcare delivery in the future.
7.7. Advancements in Miniaturization
Advancements in miniaturization are playing a crucial role in revolutionizing healthcare, enabling the development of smaller, more precise medical devices and technologies. Micro-robotics is transforming medical interventions by offering highly precise tools for surgeries and diagnostics, especially in hard-to-reach areas of the body. These micro-robots are designed to perform minimally invasive procedures, improving patient outcomes and reducing recovery times, though challenges related to design, technical complexities, and regulatory frameworks remain [
169]. Similarly, advancements in sensor technology are allowing for the creation of compact, yet highly effective devices for managing chronic conditions like heart failure, with remote monitoring systems helping to enhance patient care and disease management [
170].
In addition to robotics and sensors, emerging technologies like THz waves and Immuno-Rolling Circle Amplification (Immuno-RCA) are expanding the possibilities for non-invasive diagnostics and precise biomarker detection. THz waves are enabling high-resolution, non-invasive imaging that could transform diagnostic procedures, while Immuno-RCA offers a powerful biosensing technique with high sensitivity for detecting critical biomarkers in various medical applications [
171,
172,
173]. These miniaturized technologies, coupled with the integration of IoT and AI for real-time monitoring, are driving the future of personalized and precision healthcare, offering greater accuracy and efficiency in patient care [
174].
8. Conclusion
Biomedical sensors have significantly advanced healthcare, offering transformative tools for real-time monitoring, diagnostics, and personalized treatment. Over the past decade, substantial progress has been made in integrating sensors with flexible, wearable, and implantable medical devices, as well as utilizing innovative materials such as conducting polymer hydrogels, nanotechnology, and electrochemical biosensors. These advancements have revolutionized disease management in areas like cardiovascular monitoring, diabetes management, and early cancer detection, leading to more effective and timely clinical care interventions. Despite these achievements, several challenges remain, including technical limitations related to sensor miniaturization, biocompatibility, and power efficiency. Data privacy concerns and regulatory hurdles also pose barriers to the widespread adoption of these technologies. Ensuring the security of sensitive health information while maintaining sensor reliability in diverse environmental conditions is critical to overcoming these limitations. Moreover, achieving interoperability between different sensor platforms and healthcare systems is essential for seamless integration in clinical applications. Looking ahead, future trends point towards increased adoption of AI and IoT-enabled sensor systems, self-powered devices, and further miniaturization of sensors for long-term, non-invasive monitoring. By addressing current challenges through multidisciplinary research and innovation, biomedical sensors will continue to play a central role in advancing personalized medicine, improving patient outcomes, and driving healthcare innovation.
Author Contributions
Ali Raza: Conceptualization, methodology, software, investigation, data curation, writing—original draft, project administration, funding acquisition. Hasan Zulfiqar: writing—review & editing, visualization, supervision. Zheng Gong: methodology, conceptualization, review & editing. Yanzheng Chen: methodology, investigation, review & editing. Yifan Chen: validation, formal analysis, investigation, resources, writing—review & editing, visualization, supervision, project administration, funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
Financial support from startup funding number (U03220127) of Yangtze Delta Region Institute (Huzhou), University of Electronic Science and Technology of China, Huzhou, Zhejiang, China is gratefully acknowledged.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
All the authors are in agreement and declare that there is no conflict of interest.
References
- Costanzo, S. Microwave Biomedical Sensors With Stable Response: Basic Idea and Preliminary Numerical Assessments for Blood Glucose Monitoring. IEEE Access 2023, 1, 99058–99069. [Google Scholar] [CrossRef]
- Ovando, A. Biomedical Sensing - A Sensor Fusion Approach For Improved Medical Detection & Monitoring. SoutheastCon 2023, 2023, 450–455. [Google Scholar]
- Gamboa, J. Recent Progress in Biomedical Sensors Based on Conducting Polymer Hydrogels. ACS Appl Bio Mater, 2023, 6, 1720–1741. [Google Scholar] [CrossRef]
- Zulfiqar, H. Deep-STP: a deep learning-based approach to predict snake toxin proteins by using word embeddings. Frontiers in Medicine, 2024, 10, 1291352. [Google Scholar] [CrossRef]
- Mohankumar, P. Recent developments in biosensors for healthcare and biomedical applications: A review. Measurement, 2021. 167.
- Yeon, P. Microfabrication, coil characterization, and hermetic packaging of millimeter-sized free-floating neural probes. IEEE Sensors Journal, 2021, 21, 13837–13848. [Google Scholar] [CrossRef]
- Lee, D. A Multi-Functional CMOS Biosensor Array With On-Chip DEP-Assisted Sensing for Rapid Low-Concentration Analyte Detection and Close-Loop Particle Manipulation With No External Electrodes. IEEE Trans Biomed Circuits Syst, 2023, 17, 1214–1226. [Google Scholar] [CrossRef] [PubMed]
- Baryeh, K. Introduction to medical biosensors for point of care applications, in Medical Biosensors for Point of Care (POC) Applications. 2017. p. 3-25.
- Sankhala, D. A machine learning-based on-demand sweat glucose reporting platform. Sci Rep, 2022, 12, 2442. [Google Scholar] [CrossRef] [PubMed]
- Ullah, I. Wirelessly Powered Drug-Free and Anti-Infective Smart Bandage for Chronic Wound Care. IEEE Trans Biomed Circuits Syst, 2023, 17, 900–915. [Google Scholar] [CrossRef]
- Yang, Y. A laser-engraved wearable sensor for sensitive detection of uric acid and tyrosine in sweat. Nat Biotechnol, 2020, 38, 217–224. [Google Scholar] [CrossRef]
- Wang, M. A wearable electrochemical biosensor for the monitoring of metabolites and nutrients. Nat Biomed Eng, 2022, 6, 1225–1235. [Google Scholar] [CrossRef]
- Gutruf, P. , Towards a digitally connected body for holistic and continuous health insight. Communications Materials, 2024. 5(1).
- Jung, H. Accurate Ballistocardiogram Based Heart Rate Estimation Using an Array of Load Cells in a Hospital Bed. IEEE J Biomed Health Inform, 2021, 25, 3373–3383. [Google Scholar] [CrossRef] [PubMed]
- Yaldiz, C.O. Early Prediction of Impending Exertional Heat Stroke With Wearable Multimodal Sensing and Anomaly Detection. IEEE J Biomed Health Inform, 2023, 27, 5803–5814. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y. Recent developments in sensors for wearable device applications. Anal Bioanal Chem, 2021, 413, 6037–6057. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, D. Biosensors and their widespread impact on human health. Sensors International, 2024. 5.
- Kim, J. Wearable biosensors for healthcare monitoring. Nat Biotechnol, 2019, 37, 389–406. [Google Scholar] [CrossRef]
- Gao, F. Wearable and flexible electrochemical sensors for sweat analysis: a review. Microsyst Nanoeng, 2023, 9, 1. [Google Scholar] [CrossRef]
- Le, V.T. A review on graphene-based electrochemical sensor for mycotoxins detection. Food Chem Toxicol, 2021, 148, 111931. [Google Scholar] [CrossRef]
- Mehrotra, P. , Biosensors and their applications - A review. J Oral Biol Craniofac Res, 2016, 6, 153–9. [Google Scholar] [CrossRef]
- Abo-Hamad, A. Ionic Liquid-Carbon Nanomaterial Hybrids for Electrochemical Sensor Applications: a Review. Electrochimica Acta, 2016, 193, 321–343. [Google Scholar] [CrossRef]
- Shetti, N.P. Nanostructured titanium oxide hybrids-based electrochemical biosensors for healthcare applications. Colloids Surf B Biointerfaces, 2019, 178, 385–394. [Google Scholar] [CrossRef]
- Naresh, V. and N. Lee, A Review on Biosensors and Recent Development of Nanostructured Materials-Enabled Biosensors. Sensors (Basel), 2021. 21(4).
- Ghorbanizamani, F. Material Design in Implantable Biosensors toward Future Personalized Diagnostics and Treatments. Applied Sciences, 2023. 13(7).
- Sempionatto, J.R. Wearable chemical sensors for biomarker discovery in the omics era. Nat Rev Chem, 2022, 6, 899–915. [Google Scholar] [CrossRef]
- Bollella, P. Beyond graphene: Electrochemical sensors and biosensors for biomarkers detection. Biosens Bioelectron, 2017. 89(Pt 1): p. 152-166.
- Mahato, K. and J. Wang, Electrochemical sensors: From the bench to the skin. Sensors and Actuators B: Chemical, 2021. 344.
- Lu, Z., X. Gao, and H. Yu, GTac: A Biomimetic Tactile Sensor With Skin-Like Heterogeneous Force Feedback for Robots. IEEE Sensors Journal, 2022, 22, 14491–14500. [Google Scholar]
- Jeong, H.K. Quantifying Asymmetry Between Medial and Lateral Compartment Knee Loading Forces Using Acoustic Emissions. IEEE Trans Biomed Eng, 2022, 69, 1541–1551. [Google Scholar] [CrossRef]
- Gao, W. A High-Resolution MEMS Capacitive Force Sensor With Bionic Swallow Comb Arrays for Ultralow Multiphysics Measurement. IEEE Transactions on Industrial Electronics, 2023, 70, 7467–7477. [Google Scholar] [CrossRef]
- Bhalla, N. Introduction to biosensors. Essays Biochem, 2016, 60, 1–8. [Google Scholar] [PubMed]
- Ahmad, R. and K.N. Salama, Physical sensors for biomedical applications. 2018 IEEE SENSORS, 2018: p. 1-3.
- Park, H., W. Park, and C.H. Lee, Electrochemically active materials and wearable biosensors for the in situ analysis of body fluids for human healthcare. NPG Asia Materials, 2021. 13(1).
- Kaur, J. Enzyme-based biosensors, in Bioelectronics and Medical Devices. 2019. p. 211-240.
- Wiswedel, R. Beta-Barrel Nanopores as Diagnostic Sensors: An Engineering Perspective. Biosensors (Basel), 2024. 14(7).
- Ansari, M.I.H. Microfluidic-integrated DNA nanobiosensors. Biosens Bioelectron, 2016, 85, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Skládal, P. , Piezoelectric biosensors. TrAC Trends in Analytical Chemistry, 2016, 79, 127–133. [Google Scholar] [CrossRef]
- Li, Q. Recent advances in black phosphorus-based electrochemical sensors: A review. Anal Chim Acta, 2021, 1170, 338480. [Google Scholar] [CrossRef]
- Annese, V.F. Micromolar Metabolite Measurement in an Electronically Multiplexed Format. IEEE Trans Biomed Eng, 2022, 69, 2715–2722. [Google Scholar] [CrossRef]
- Tabata, M. and Y. Miyahara, From new materials to advanced biomedical applications of solid-state biosensor: A review. Sensors and Actuators B: Chemical, 2022. 352.
- Smiljanic, M. Introducing common oxazine fluorophores as new redox labels for electrochemical DNA sensors. Bioelectrochemistry, 2024, 155, 108582. [Google Scholar] [CrossRef]
- Cao, J. DNA-sensing inflammasomes cause recurrent atherosclerotic stroke. Nature, 2024: p. 1-9.
- Yan, B. Analysis and identification of mRNAsi-related expression signatures via RNA sequencing in lung cancer. Oncology Letters, 2024, 28, 1–10. [Google Scholar] [CrossRef]
- Sandler, S.E. Sensing the DNA-mismatch tolerance of catalytically inactive Cas9 via barcoded DNA nanostructures in solid-state nanopores. Nature Biomedical Engineering, 2024, 8, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani Zamani, F. Current trends in the development of conducting polymers-based biosensors. TrAC Trends in Analytical Chemistry, 2019, 118, 264–276. [Google Scholar] [CrossRef]
- Sharma, P. Aptamer Based on Silver Nanoparticle-Modified Flexible Carbon Ink Printed Electrode for the Electrochemical Detection of Chikungunya Virus. Biosensors (Basel), 2024. 14(7).
- Goswami, A. Nanotechnology-Based Biosensors for Biomedical Applications. Journal of The Electrochemical Society, 2024.
- Gezahegn, T.F. Breakthroughs in nanostructured-based chemical sensors for the detection of toxic metals. Talanta Open, 2024: p. 100354.
- Kushwaha, R.K., S. Kumar, and B. Kattigenahalli, Nanoparticles and their Applications in Agriculture. SHINEEKS: p. 77.
- Poria, R. 11 Soft nanoferrites as. Soft Nanoferrites for Biomedical and Environmental Applications, 2024: p. 142.
- Koydemir, H.C. and A. Ozcan, Wearable and Implantable Sensors for Biomedical Applications. Annu Rev Anal Chem (Palo Alto Calif), 2018. 11(1): p. 127-146.
- Ji, N. Recommendation to Use Wearable-Based mHealth in Closed-Loop Management of Acute Cardiovascular Disease Patients During the COVID-19 Pandemic. IEEE J Biomed Health Inform 2021, 25, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S. A Biomedical Sensor for Detection of Cancer Cells Based on Terahertz Metamaterial Absorber. IEEE Sensors Letters, 2022. 6(6): p. 1-4.
- Wu, L. and Y. Wang, Stationary and Moving Occupancy Detection Using the SLEEPIR Sensor Module and Machine Learning. IEEE Sensors Journal, 2021. 21(13): p. 14701-14708.
- Liu, Z., P. Wu, and G. Li, A Multibeam and Surface Plasmonic Clothing With RF Energy-Localized Harvester for Powering Battery-Free Wireless Sensor. IEEE Internet of Things Journal, 2022. 9(15): p. 13955-13964.
- Lin, D.J. Predicting Soldier Performance on Structured Military Training Marches With Wearable Accelerometer and Physiological Data. IEEE Sensors Journal, 2024. 24(1): p. 403-413.
- Lin, D.J. Reducing the Impact of External Vibrations on Fiducial Point Detection in Seismocardiogram Signals. IEEE Trans Biomed Eng, 2022. 69(1): p. 176-185.
- Wan, H. Biomedical sensors, in Biomedical Information Technology. 2020. p. 51-79.
- Cao, J. Ultrasensitive Flexible Strain Sensor Made with Carboxymethyl-Cellulose-Anchored Carbon Nanotubes/MXene for Machine-Learning-Assisted Handwriting Recognition. ACS Applied Materials & Interfaces, 2024.
- Dhatterwal, J.S., K. S. Kaswan, and N. Kumar, Self-powered integrated sensor system for printable fabrication, in Self-Powered Sensors. 2025, Elsevier. p. 187-235.
- Hariprasath, S. Stretchable and flexible wearable sensors based on carbon and textile for health monitoring, in Self-Powered Sensors. 2025, Elsevier. p. 93-108.
- Alfihed, S. Non-Invasive Brain Sensing Technologies for Modulation of Neurological Disorders. Biosensors (Basel), 2024. 14(7).
- Cennamo, N. Pollen-based natural nanostructures to realize nanoplasmonic biochips for single-molecule detection. Sensors and Actuators B: Chemical, 2024: p. 136404.
- Peng, Y., Y. M. Shkel, and T.J. Hall, A Tactile Sensor for Ultrasound Imaging Systems. IEEE Sens J, 2016. 16(4): p. 1044-1053.
- Lee, C.S. An Acoustic System of Sound Acquisition and Image Generation for Frequent and Reliable Lung Function Assessment. IEEE Sensors Journal, 2024. 24(3): p. 3731-3747.
- Shokouhmand, A. MEMS Fingertip Strain Plethysmography for Cuffless Estimation of Blood Pressure. IEEE J Biomed Health Inform, 2024. 28(5): p. 2699-2712.
- Xia, W. , Biomedical Photoacoustics: Technology and Applications. 2024: Springer Nature.
- Wang, Y. Double-layer stretchable composite conductive graphene-hydrogel with wide-range linear sensing and thermal-humidity management for health monitoring. Chemical Engineering Journal, 2024: p. 155808.
- Aslam, N. Quantum sensors for biomedical applications. Nat Rev Phys, 2023. 5(3): p. 157-169.
- Zheng, W. Recent Advancements in Sensor Technologies for Healthcare and Biomedical Applications. Sensors (Basel), 2023. 23(6).
- Sanchez-Perez, J.A. Enabling Continuous Breathing-Phase Contextualization via Wearable-Based Impedance Pneumography and Lung Sounds: A Feasibility Study. IEEE J Biomed Health Inform, 2023. 27(12): p. 5734-5744.
- Li, T., A. Pan, and H. Ren, Reaction Force Mapping by 3-Axis Tactile Sensing With Arbitrary Angles for Tissue Hard-Inclusion Localization. IEEE Trans Biomed Eng, 2021. 68(1): p. 26-35.
- Kumashi, S. A CMOS Multi-Modal Electrochemical and Impedance Cellular Sensing Array for Massively Paralleled Exoelectrogen Screening. IEEE Trans Biomed Circuits Syst, 2021. 15(2): p. 221-234.
- Hu, Z. Recent Progress in Organic Electrochemical Transistor-Structured Biosensors. Biosensors (Basel), 2024. 14(7).
- Jiang, Y. Electrochemical Platform Based on the Bi2Te3 Family of Topological Insulators for the Detection of SARS-CoV-2 Pathogenic Factors. Langmuir, 2024.
- Riedl, V. Detection of Sulfonamide Antibiotics Using an Elastic Hydrogel Microparticles-Based Optical Biosensor. ACS Applied Materials & Interfaces, 2024.
- Shetti, N.P. ZnO-based nanostructured electrodes for electrochemical sensors and biosensors in biomedical applications. Biosens Bioelectron, 2019. 141: p. 111417.
- Flynn, C.D. Biomolecular sensors for advanced physiological monitoring. Nat Rev Bioeng, 2023: p. 1-16.
- Ensafi, A.A. , An introduction to sensors and biosensors, in Electrochemical Biosensors. 2019. p. 1-10.
- Sangodoyin, S. Leveraging On-Chip Transistor Switching for Communication and Sensing in Neural Implants and Gastrointestinal Devices. IEEE Trans Biomed Eng, 2022. 69(1): p. 377-389.
- Fang, Z. Wide Field-of-View Locating and Multimodal Vital Sign Monitoring Based on ${X}$ -Band CMOS-Integrated Phased-Array Radar Sensor. IEEE Transactions on Microwave Theory and Techniques 2020, 68, 4054–4065. [Google Scholar] [CrossRef]
- Ye, S. Recent Progress in Wearable Biosensors: From Healthcare Monitoring to Sports Analytics. Biosensors (Basel), 2020. 10(12).
- Shandhi, M.M.H. Estimation of Instantaneous Oxygen Uptake During Exercise and Daily Activities Using a Wearable Cardio-Electromechanical and Environmental Sensor. IEEE J Biomed Health Inform, 2021. 25(3): p. 634-646.
- Liu, J. PCA-Based Multi-Wavelength Photoplethysmography Algorithm for Cuffless Blood Pressure Measurement on Elderly Subjects. IEEE J Biomed Health Inform, 2021. 25(3): p. 663-673.
- Sezgintürk, M.K. , Introduction to commercial biosensors, in Commercial Biosensors and Their Applications. 2020. p. 1-28.
- Wang, J. 3D Printing of Metals with sub-10 µm Resolution. Small: p. 2406518.
- Sarath, A. , Investigating Microwave-Synthesized Nanoferrites as Core Materials for RF On-Chip Inductors. 2024.
- Sciberras, T. SOI MEMS Electro-Thermal Actuators for Biomedical Applications: Operation in 0.9% NaCl Solution. Micromachines, 2024. 15(7): p. 881.
- Jung, H. Estimation of Tidal Volume Using Load Cells on a Hospital Bed. IEEE J Biomed Health Inform, 2022. 26(7): p. 3330-3341.
- Bewdor, N. , Crystalline liquids: Dynamic responsive materials for future devices. Journal of Molecular Liquids, 2024: p. 125926.
- Verma, R. Introduction to soft nanoferrites, in Soft Nanoferrites for Biomedical and Environmental Applications. CRC Press. p. 1-13.
- Paladiya, C. and A. Kiani, Nano structured sensing surface: Significance in sensor fabrication. Sensors and Actuators B: Chemical, 2018. 268: p. 494-511.
- Emad-Ud-Din, M. Bayes Filter-Based Occupancy Detection Using Networked SLEEPIR Sensors. IEEE Sensors Journal, 2023, 23, 22832–22844. [Google Scholar] [CrossRef]
- Emad-ud-Din, M. Indoor Occupancy Estimation Using Particle Filter and SLEEPIR Sensor System. IEEE Sensors Journal, 2022, 22, 17173–17183. [Google Scholar] [CrossRef]
- Sebkhi, N. Evaluation of a Head-Tongue Controller for Power Wheelchair Driving by People With Quadriplegia. IEEE Trans Biomed Eng, 2022, 69, 1302–1309. [Google Scholar] [CrossRef]
- Molloy, A. Challenges to the Development of the Next Generation of Self-Reporting Cardiovascular Implantable Medical Devices. IEEE Rev Biomed Eng, 2022, 15, 260–272. [Google Scholar] [CrossRef]
- Michalska, J.M. Imaging brain tissue architecture across millimeter to nanometer scales. Nat Biotechnol, 2024, 42, 1051–1064. [Google Scholar] [CrossRef]
- Zhang, L. Learning-Based Quantitative Microwave Imaging With a Hybrid Input Scheme. IEEE Sensors Journal, 2020. 20(24): p. 15007-15013.
- Liu, S. Development of a Handheld Volumetric Photoacoustic Imaging System With a Central-Holed 2D Matrix Aperture. IEEE Trans Biomed Eng, 2020. 67(9): p. 2482-2489.
- Gonzalez, H.A. BioCNN: A Hardware Inference Engine for EEG-Based Emotion Detection. IEEE Access, 2020. 8: p. 140896-140914.
- Zhang, J.X. and K. Hoshino, Molecular sensors and nanodevices: principles, designs and applications in biomedical engineering. 2018: Academic Press.
- Shi, C., X. Peng, and Y. Feng, Hydrogel Surface/Coating for Smart Drug Delivery and Medical Devices. 2024, MDPI. p. 592.
- Nagarajan, P. Self-powered wearable implantable smart sensor and medical electronics based on nanogenerator, in Self-Powered Sensors. 2025, Elsevier. p. 59-75.
- Wang, F. Optical Fiber Microvibration Sensor Design for Wearable Multi-Point Breathing Monitoring. IEEE Sensors Journal, 2024.
- Zulfiqar, H. Identification of cyclin protein using gradient boost decision tree algorithm. Computational and Structural Biotechnology Journal, 2021. 19: p. 4123-4131.
- Richardson, K.L. Quantifying Rheumatoid Arthritis Disease Activity Using a Multimodal Sensing Knee Brace. IEEE Trans Biomed Eng, 2022. 69(12): p. 3772-3783.
- Yarman, A., S. Kurbanoglu, and F.W. Scheller, Noninvasive biosensors for diagnostic biomarkers, in Commercial Biosensors and Their Applications. 2020. p. 167-181.
- Sasikumar, K. Yellow Emissive Carbon Dots–A Robust Nanoprobe for Highly Sensitive Quantification of Jaundice Biomarker and Mitochondria Targeting in Cancer Cells. ACS Applied Bio Materials, 2024.
- Son, A. Mass Spectrometry Advancements and Applications for Biomarker Discovery, Diagnostic Innovations, and Personalized Medicine. International Journal of Molecular Sciences, 2024. 25(18): p. 9880.
- Lay-Ekuakille, A. Infrared Monitoring of Oxygenation Process Generated by Robotic Verticalization in Bedridden People. IEEE Sens J, 2021. 21(13): p. 14426-14433.
- Wu, Y. and M. Wu, Biomedical Data Mining and Machine Learning for Disease Diagnosis and Health Informatics. 2024, MDPI. p. 364.
- Gangwar, S., N. Sharma, and D. Toor, Immunoinformatics for the Diagnosis and Monitoring of Autoimmune Diseases, in Concepts in Pharmaceutical Biotechnology and Drug Development. 2024, Springer. p. 247-264.
- Zhang, L., W. Guo, and C. Lv, Modern technologies and solutions to enhance surveillance and response systems for emerging zoonotic diseases. Science in One Health, 2024. 3: p. 100061.
- Das, A. Predicting the Macronutrient Composition of Mixed Meals From Dietary Biomarkers in Blood. IEEE J Biomed Health Inform, 2022. 26(6): p. 2726-2736.
- Matboli, M. Comprehensive machine learning models for predicting therapeutic targets in type 2 diabetes utilizing molecular and biochemical features in rats. Frontiers in Endocrinology, 2024. 15: p. 1384984.
- Emam, M. Comparative evaluation of multiomics integration tools for the study of prediabetes: insights into the earliest stages of type 2 diabetes mellitus. Network Modeling Analysis in Health Informatics and Bioinformatics, 2024. 13(1): p. 8.
- Echajei, S. Exploring the Intersection of Machine Learning and Causality in Advanced Diabetes Management: New Insight and Opportunities, in Engineering Applications of Artificial Intelligence. 2024, Springer. p. 237-262.
- Chen, Y. Combination of Evidence from Bibliometrics and Bioinformatics Analysis Identifies miR-21 as a Potential Therapeutical Target for Diabetes. Metabolites, 2024. 14(8): p. 403.
- Ahmed, E.M. Computational Analysis of Deleterious nsSNPs in INS Gene Associated with Permanent Neonatal Diabetes Mellitus. Journal of Personalized Medicine, 2024. 14(4): p. 425.
- Singla, R. Mechanistic investigation of quercetin in the management of diabetic foot ulcer by network pharmacology and molecular docking. Pharmacological Research-Modern Chinese Medicine, 2024. 10: p. 100373.
- Mabrouk, S., D. Whittingslow, and O.T. Inan, Robust Method for Mid-Activity Tracking and Evaluation of Ankle Health Post-Injury. IEEE Trans Biomed Eng, 2021. 68(4): p. 1341-1350.
- Li, Y. A Segmentation-Denoising Network for Artifact Removal From Single-Channel EEG. IEEE Sensors Journal, 2023, 23, 15115–15127. [Google Scholar] [CrossRef]
- Paul, V.V. and J.A.I.S. Masood, Exploring Predictive Methods for Cardiovascular Disease: A Survey of Methods and Applications. IEEE Access, 2024.
- Drouard, G. Exploring machine learning strategies for predicting cardiovascular disease risk factors from multi-omic data. BMC Medical Informatics and Decision Making, 2024. 24(1): p. 116.
- Koloi, A. Predicting early-stage coronary artery disease using machine learning and routine clinical biomarkers improved by augmented virtual data. European Heart Journal-Digital Health, 2024: p. ztae049.
- Zhang, J. Multimodal Image Fusion via Self-Supervised Transformer. IEEE Sensors Journal, 2023, 23, 9796–9807. [Google Scholar] [CrossRef]
- Wang, W. MRC-Based Double Figure-of-Eight Coil Sensor System With Triple-Mode Operation Capability for Biomedical Applications. IEEE Sensors Journal, 2021. 21(13): p. 14491-14502.
- Tanwear, A. Spintronic Eyeblink Gesture Sensor With Wearable Interface System. IEEE Trans Biomed Circuits Syst, 2022. 16(5): p. 779-792.
- Baldo, T.A. Wearable and Biodegradable Sensors for Clinical and Environmental Applications. ACS Applied Electronic Materials, 2020. 3(1): p. 68-100.
- Akbari, A., J. Martinez, and R. Jafari, A Meta-Learning Approach for Fast Personalization of Modality Translation Models in Wearable Physiological Sensing. IEEE J Biomed Health Inform, 2022. 26(4): p. 1516-1527.
- Kimball, J.P. Unifying the Estimation of Blood Volume Decompensation Status in a Porcine Model of Relative and Absolute Hypovolemia Via Wearable Sensing. IEEE J Biomed Health Inform, 2021. 25(9): p. 3351-3360.
- Ates, H.C. End-to-end design of wearable sensors. Nat Rev Mater, 2022. 7(11): p. 887-907.
- Tanwear, A. Spintronic Sensors Based on Magnetic Tunnel Junctions for Wireless Eye Movement Gesture Control. IEEE Trans Biomed Circuits Syst, 2020. 14(6): p. 1299-1310.
- Yue, W. Dynamic Piezoelectric Tactile Sensor for Tissue Hardness Measurement Using Symmetrical Flexure Hinges and Anisotropic Vibration Modes. IEEE Sensors Journal, 2021. 21(16): p. 17712-17722.
- Wu, J. Device integration of electrochemical biosensors. Nat Rev Bioeng, 2023. 1(5): p. 346-360.
- Yang, G. Homecare Robotic Systems for Healthcare 4.0: Visions and Enabling Technologies. IEEE J Biomed Health Inform, 2020, 24, 2535–2549. [Google Scholar] [CrossRef] [PubMed]
- Shao, G. and Y.-X. Guo, Hybrid Wireless Positioning and Charging With Switched Field Helmholtz Coils for Wireless Capsule Endoscopy. IEEE Transactions on Microwave Theory and Techniques, 2020. 68(3): p. 904-913.
- Wei, R. Stereo Dense Scene Reconstruction and Accurate Localization for Learning-Based Navigation of Laparoscope in Minimally Invasive Surgery. IEEE Trans Biomed Eng, 2023. 70(2): p. 488-500.
- Mao, T. Online Test-Time Adaptation for Patient-Independent Seizure Prediction. IEEE Sensors Journal, 2023. 23(19): p. 23133-23144.
- Leelaarporn, P. Sensor-Driven Achieving of Smart Living: A Review. IEEE Sensors Journal, 2021. 21(9): p. 10369-10391.
- Yan, Y. UKF-Based Motion Estimation of Cable-Driven Forceps for Robot-Assisted Surgical System. IEEE Access, 2020. 8: p. 94912-94922.
- Wu, L. and Y. Wang, Performance Optimization of the SLEEPIR Sensor Towards Indoor Stationary Occupancy Detection. IEEE Sensors Journal, 2021. 21(21): p. 23776-23786.
- Gupta, A.K. Spatio-Temporal Encoding Improves Neuromorphic Tactile Texture Classification. IEEE Sensors Journal, 2021. 21(17): p. 19038-19046.
- Kim, J. Fitts' Law Based Performance Metrics to Quantify Tremor in Individuals With Essential Tremor. IEEE J Biomed Health Inform, 2022. 26(5): p. 2169-2179.
- Wang, Z. Research on the Human Motion Recognition Method Based on Wearable. Biosensors (Basel), 2024. 14(7).
- Mishra, S.K., J. Jeba Praba, and J.J. Georrge, An emerging trends of bioinformatics and big data analytics in healthcare. Digital Transformation in Healthcare 5.0: Volume 2: Metaverse, Nanorobots and Machine Learning, 2024: p. 159.
- Wang, J. Bioinformatics and biomedical informatics with ChatGPT: Year one review. Quantitative Biology, 2024.
- Chandra, A. Stem cell based informatics development and approaches, in Computational Biology for Stem Cell Research. 2024, Elsevier. p. 41-50.
- Panja, A.K., A. Mukherjee, and N. Dey, Introduction, in Biomedical Sensors and Smart Sensing. 2022. p. 1-14.
- Wang, Z. MatGPT: A vane of materials informatics from past, present, to future. Advanced Materials, 2024, 36, 2306733. [Google Scholar] [CrossRef] [PubMed]
- Damaj, I.W., Y. Iraqi, and H.T. Mouftah, Modern development technologies and health informatics: Area transformation and future trends. IEEE Internet of Things Magazine, 2020. 3(4): p. 88-94.
- Pramanik, M.I. Healthcare informatics and analytics in big data. Expert Systems with Applications, 2020. 152: p. 113388.
- Zulfiqar, H. Deep-4mCGP: a deep learning approach to predict 4mC sites in Geobacter pickeringii by using correlation-based feature selection technique. International Journal of Molecular Sciences, 2022, 23, 1251. [Google Scholar] [CrossRef]
- Zulfiqar, H. Computational prediction of promotors in Agrobacterium tumefaciens strain C58 by using the machine learning technique. Frontiers in Microbiology, 2023. 14: p. 1170785.
- Huo, D. and X. Wang, A new era in healthcare: The integration of artificial intelligence and microbial. Medicine in Novel Technology and Devices, 2024: p. 100319.
- Niranjan, V.; Vishal, A.; Setlur, A.S. Integration of Artificial Intelligence, Machine Learning and Deep Learning Techniques in Genomics: Review on Computational Perspectives for NGS Analysis of DNA and RNA Seq Data. Current Bioinformatics 2024, 19, 825–844. [Google Scholar]
- Chakraborty, C. The changing scenario of drug discovery using artificial intelligence (AI) to deep learning (DL): Recent advancement, success stories, collaborations, and challenges. Molecular Therapy-Nucleic Acids, 2024.
- Acharjya, D. and K. Ma, Computational Intelligence in Healthcare Informatics. 2024: Springer.
- Salam, A. , Internet of things for sustainable human health, in Internet of Things for Sustainable Community Development: Wireless Communications, Sensing, and Systems. 2024, Springer. p. 217-242.
- Šajnović, U. Internet of Things and Big Data Analytics in Preventive Healthcare: A Synthetic Review. Electronics, 2024, 13, 3642. [Google Scholar] [CrossRef]
- Darwish, D. , Machine Learning and IoT in Health 4.0, in IoT and ML for Information Management: A Smart Healthcare Perspective. 2024, Springer. p. 235-276.
- Liu, J. Machine Learning Driven Atom-Thin Materials for Fragrance Sensing. Small, 2024: p. 2401066.
- Khare, N. and P. Khare, Personalised Medicine and Molecular Docking: Tailoring Drug Discovery for Individual Patients. 2024.
- Sindelar, R.D. , Genomics, other “OMIC” technologies, precision medicine, and additional biotechnology-related techniques, in Pharmaceutical Biotechnology: Fundamentals and Applications. 2024, Springer. p. 209-254.
- Bailly, S. The Future of Telemedicine for Obstructive Sleep Apnea Treatment: A Narrative Review. Journal of Clinical Medicine, 2024. 13(9): p. 2700.
- Bansal, H., D. Gupta, and D. Anand, Blockchain and Artificial Intelligence in Telemedicine and Remote Patient Monitoring. Handbook on Augmenting Telehealth Services, 2024: p. 279-294.
- Morelli, S. , et al. Under the Tech Umbrella: Assessing the Landscape of Telemedicine Innovations (Telemechron Study). in Healthcare. 2024. MDPI.
- Moshayedi, A.J. Micro robot as the feature of robotic in healthcare approach from design to application: the State of art and challenges. EAI Endorsed Transactions on AI and Robotics, 2024. 3.
- Manavi, T., H. Zafar, and F. Sharif, An Era of Digital Healthcare—A Comprehensive Review of Sensor Technologies and Telehealth Advancements in Chronic Heart Failure Management. Sensors, 2024. 24(8): p. 2546.
- Mohanty, M. Terahertz Waves in Biomedicine: Pioneering Imaging and Sensing for Healthcare Revolution, in Next Generation Wireless Communication: Advances in Optical, mm-Wave, and THz Technologies. 2024, Springer. p. 341-360.
- Rani, S. , The role of IoT devices and Artificial Intelligence-based health care monitoring systems, in Convergence of Artificial Intelligence and Internet of Things for Industrial Automation. 2024, CRC Press. p. 74-85.
- Zhang, L. Immuno-Rolling Circle Amplification (Immuno-RCA): Biosensing Strategies, Practical Applications, and Future Perspectives. Advanced Healthcare Materials: p. 2402337.
- Glaudemans, A.W. The first international network symposium on artificial intelligence and informatics in nuclear medicine:“The bright future of nuclear medicine is illuminated by artificial intelligence”. European journal of nuclear medicine and molecular imaging, 2024, 51, 336–339. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).