Submitted:
21 October 2024
Posted:
24 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Ethical Considerations
2.3. Study Variables
2.3.1. Outcome Variables
2.3.2. SES and Place of Residence
2.4. Statistical Analysis
2.4.1. Erreygers Normalised Concentration Index (ENCI)
2.4.2. Theil Indices
3. Results
3.1. Descriptive Statistics
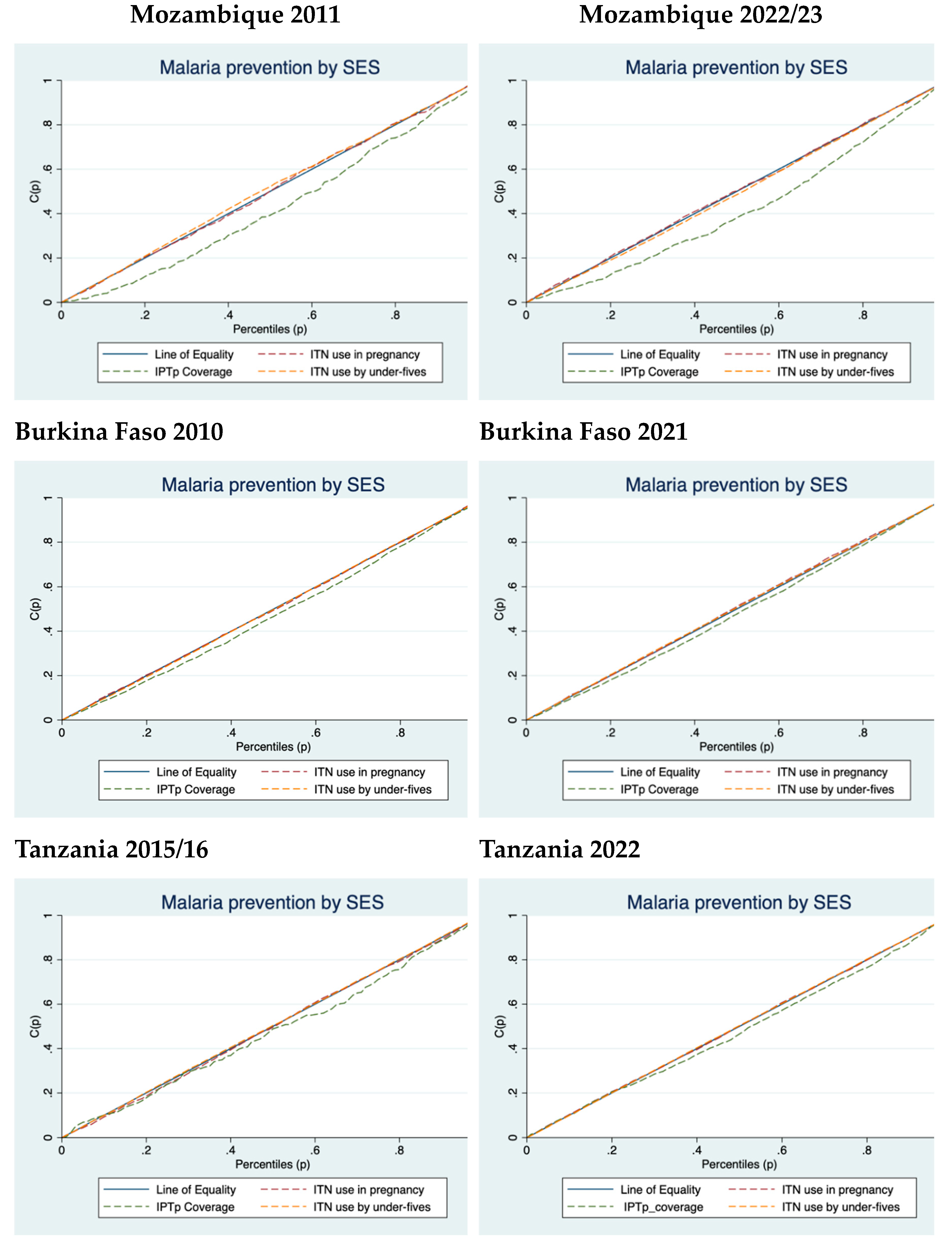
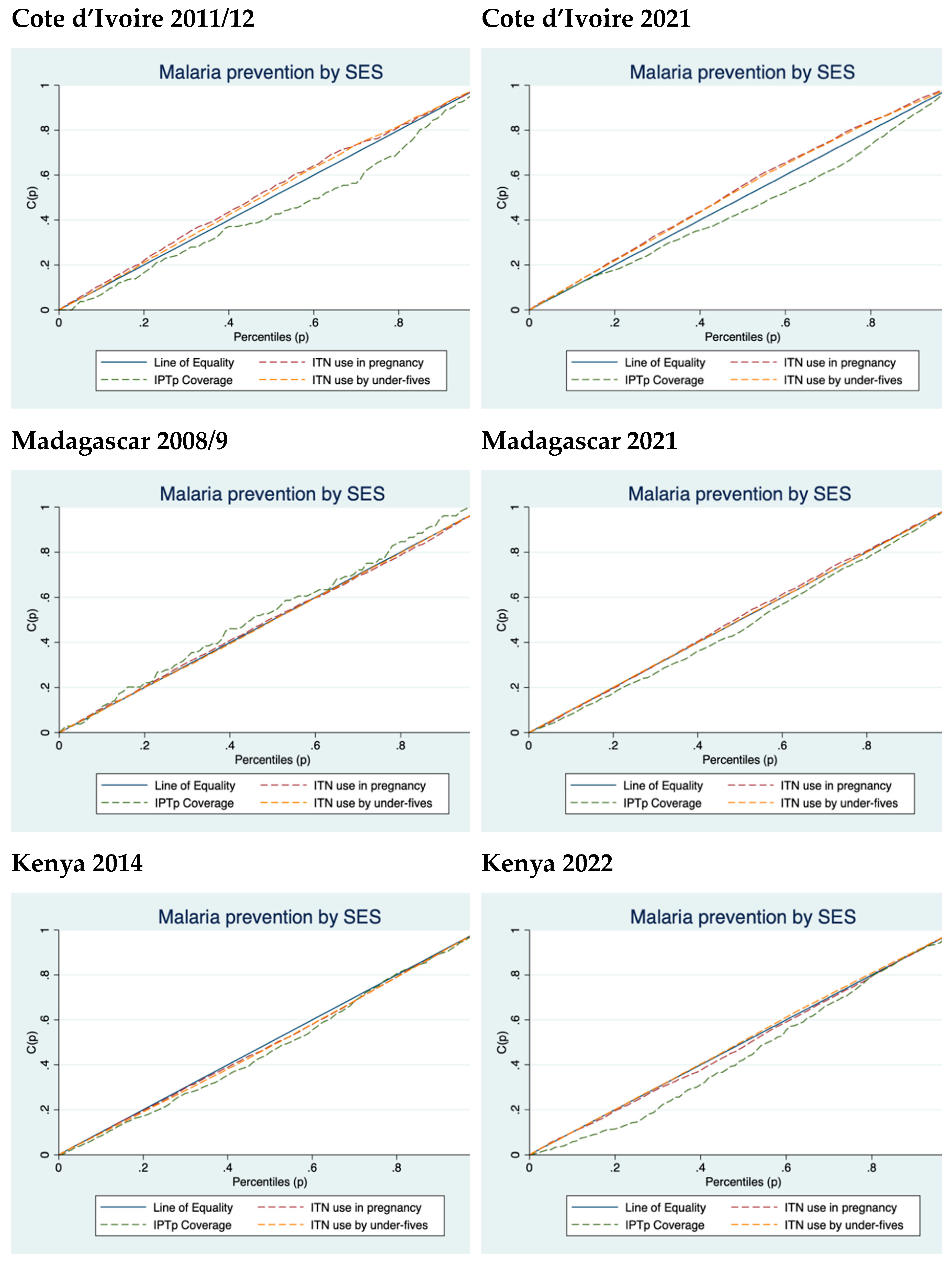
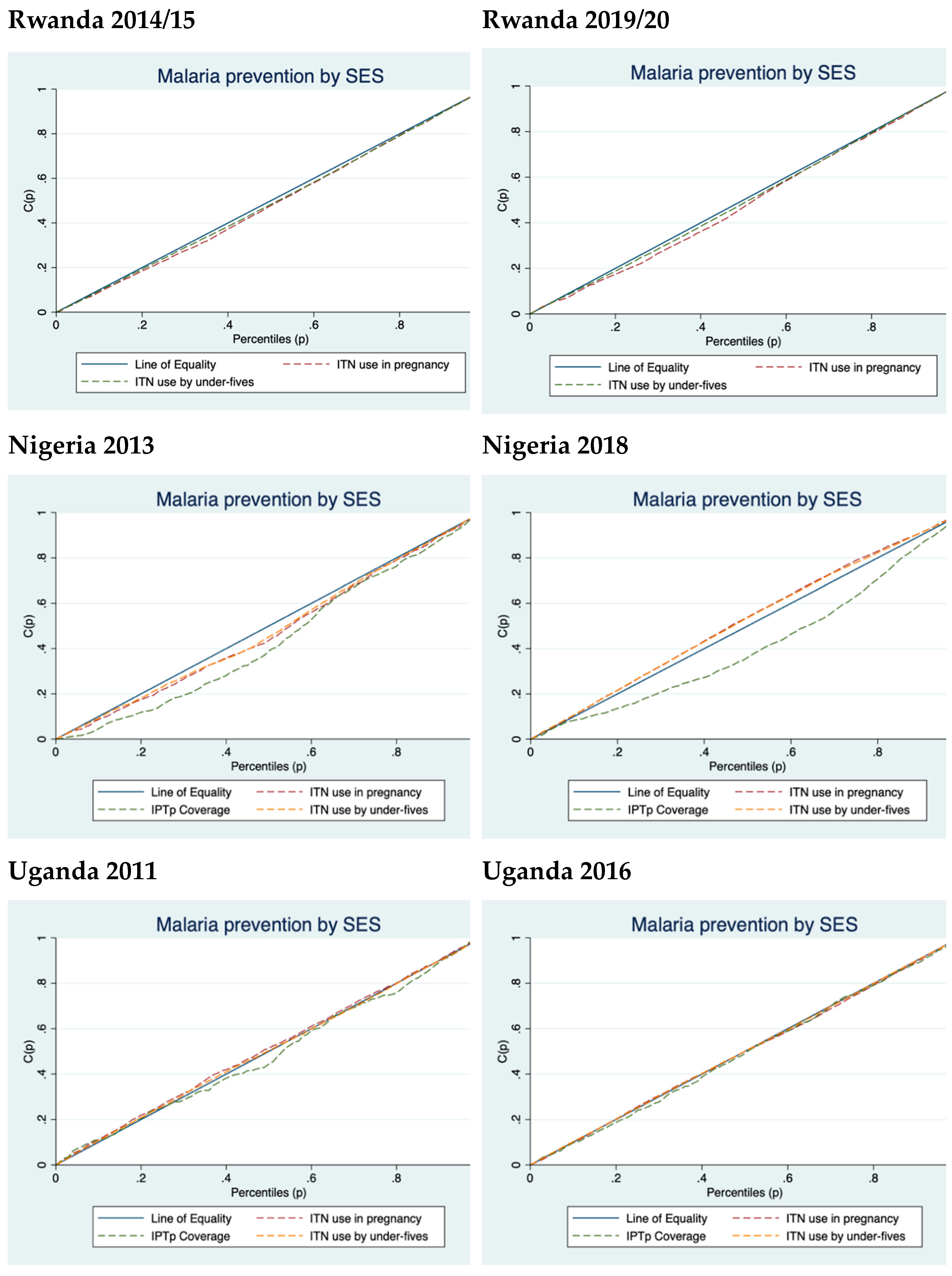
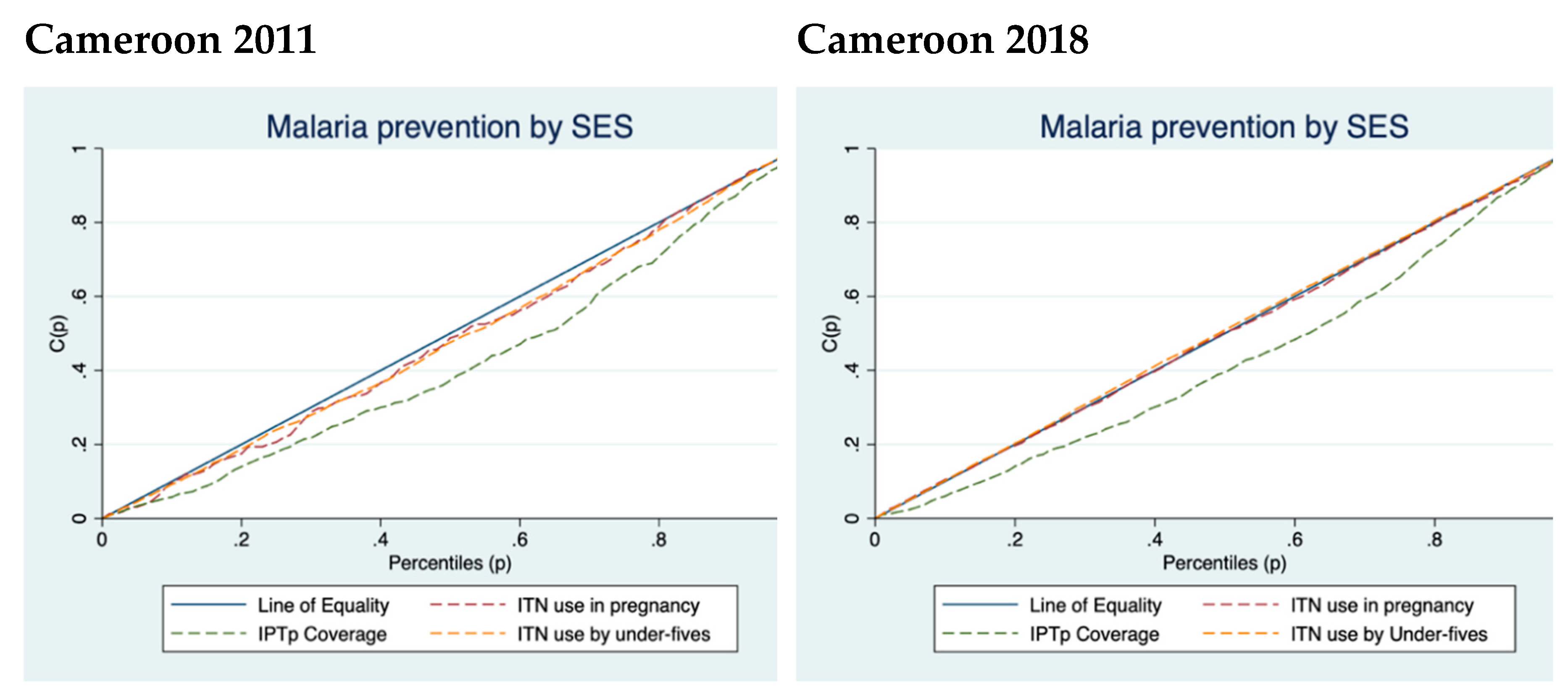
3.2. Concentration Indices and Curves
3.3. Theil Indices for ITN Use in Pregnancy, ITN Use by Under-Fives Distinguished by Place of Residence
3.4. Theil Indices for ITN Use in Pregnancy, ITN Use by Under-Fives Distinguished by SES
3.5. Decomposition of Theil Indices by Place of Residence
3.6. Decomposition of Theil Indices by SES
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. World malaria report 2023; eneva: World Health Organization; 2023. Licence: CC BY-NC-SA 3.0 IGO, 2023. [Google Scholar]
- Berchie, G.O.; Doe, P.F.; Azu, T.D.; Agyeiwaa, J.; Owusu, G.; Boso, C.M.; Yeboa, N.K.; Agyare, D.F.; Aboh, I.K.; Nabe, B. Uptake and Effectiveness of Intermittent Preventive Treatment with Sulfadoxine-Pyrimethamine during Pregnancy in Africa: A Scoping Review. Diseases 2024, 12, 203. [Google Scholar] [CrossRef] [PubMed]
- Galactionova, K.; Smith, T.A.; de Savigny, D.; Penny, M.A. State of inequality in malaria intervention coverage in sub-Saharan African countries. BMC medicine 2017, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. 2021.
- Willey, B.A.; Paintain, L.S.; Mangham, L.; Car, J.; Schellenberg, J.A. Strategies for delivering insecticide-treated nets at scale for malaria control: a systematic review. Bulletin of the World Health Organization 2012, 90, 672–684. [Google Scholar] [CrossRef]
- O'Connell, K.A.; Gatakaa, H.; Poyer, S.; Njogu, J.; Evance, I.; Munroe, E.; Solomon, T.; Goodman, C.; Hanson, K.; Zinsou, C. Got ACTs? Availability, price, market share and provider knowledge of anti-malarial medicines in public and private sector outlets in six malaria-endemic countries. Malaria journal 2011, 10, 1–14. [Google Scholar] [CrossRef]
- Steketee, R.W.; Eisele, T.P. Is the scale up of malaria intervention coverage also achieving equity? PLoS One 2009, 4, e8409. [Google Scholar] [CrossRef]
- Webster, J.; Lines, J.; Bruce, J.; Schellenberg, J.R.A.; Hanson, K. Which delivery systems reach the poor? A review of equity of coverage of ever-treated nets, never-treated nets, and immunisation to reduce child mortality in Africa. The Lancet Infectious Diseases 2005, 5, 709–717. [Google Scholar] [CrossRef]
- United Nations. Secretary-General announces ‘Roll Back Malaria Partnership’ on World Malaria Day. New York: United Nations Secretary-General (SG/SM/11531); 2008. Available online: https://press.un.org/en/2008/sgsm11531.doc.htm (accessed on 8 October).
- World Health Organization. Guidelines for the treatment of malaria; World Health Organization: 2006.
- Gelband, H.; Seiter, A. A global subsidy for antimalarial drugs. Defining and Defeating the Intolerable Burden of Malaria III: Progress and Perspectives: Supplement to Volume 77 (6) of American Journal of Tropical Medicine and Hygiene 2007.
- Gwatkin, D.R. Trends in health inequalities in developing countries. The Lancet Global Health 2017, 5, e371–e372. [Google Scholar] [CrossRef]
- World Health Organization. A strategic framework for malaria prevention and control during pregnancy in the African region; World Health Organization. Regional Office for Africa: 2004.
- Challis, K.; Osman, N.; Cotiro, M.; Nordahl, G.; Dgedge, M.; Bergström, S. Impact of a double dose of sulphadoxine–pyrimethamine to reduce prevalence of pregnancy malaria in southern Mozambique. Tropical Medicine & International Health 2004, 9, 1066–1073. [Google Scholar]
- Shulman, C.; Dorman, E.; Cutts, F.; Kawuondo, K.; Bulmer, J.; Peshu, N.; Marsh, K. Intermittent sulphadoxine-pyrimethamine to prevent severe anaemia secondary to malaria in pregnancy: a randomised placebo-controlled trial. The Lancet 1999, 353, 632–636. [Google Scholar] [CrossRef]
- Anchang-Kimbi, J.K.; Achidi, E.A.; Apinjoh, T.O.; Mugri, R.N.; Chi, H.F.; Tata, R.B.; Nkegoum, B.; Mendimi, J.-M.N.; Sverremark-Ekström, E.; Troye-Blomberg, M. Antenatal care visit attendance, intermittent preventive treatment during pregnancy (IPTp) and malaria parasitaemia at delivery. Malaria Journal 2014, 13, 1–9. [Google Scholar] [CrossRef]
- World Health Organization. World malaria report 2010; World Health Organization: 2010.
- Holtz, T.H.; Patrick Kachur, S.; Roberts, J.M.; Marum, L.H.; Mkandala, C.; Chizani, N.; Macheso, A.; Parise, M.E. Use of antenatal care services and intermittent preventive treatment for malaria among pregnant women in Blantyre District, Malawi. Tropical Medicine & International Health 2004, 9, 77–82. [Google Scholar]
- Kiwuwa, M.S.; Mufubenga, P. Use of antenatal care, maternity services, intermittent presumptive treatment and insecticide treated bed nets by pregnant women in Luwero district, Uganda. Malaria Journal 2008, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Bouyou-Akotet, M.K.; Mawili-Mboumba, D.P.; Kombila, M. Antenatal care visit attendance, intermittent preventive treatment and bed net use during pregnancy in Gabon. BMC Pregnancy and Childbirth 2013, 13, 1–6. [Google Scholar] [CrossRef]
- Mubyazi, G.; Bloch, P.; Kamugisha, M.; Kitua, A.; Ijumba, J. Intermittent preventive treatment of malaria during pregnancy: a qualitative study of knowledge, attitudes and practices of district health managers, antenatal care staff and pregnant women in Korogwe District, North-Eastern Tanzania. Malaria journal 2005, 4, 1–10. [Google Scholar] [CrossRef]
- Ndyomugyenyi, R.; Neema, S.; Magnussen, P. The use of formal and informal services for antenatal care and malaria treatment in rural Uganda. Health policy and planning 1998, 13, 94–102. [Google Scholar] [CrossRef]
- Carrasco-Escobar, G.; Fornace, K.; Benmarhnia, T. Mapping socioeconomic inequalities in malaria in Sub-Sahara African countries. Scientific reports 2021, 11, 15121. [Google Scholar] [CrossRef]
- Apeagyei, A.E.; Patel, N.K.; Cogswell, I.; O’Rourke, K.; Tsakalos, G.; Dieleman, J. Examining geographical inequalities for malaria outcomes and spending on malaria in 40 malaria-endemic countries, 2010–2020. Malaria Journal 2024, 23, 206. [Google Scholar] [CrossRef]
- Taylor, C.; Florey, L.; Ye, Y. Equity trends in ownership of insecticide-treated nets in 19 sub-Saharan African countries. Bulletin of the World Health Organization 2017, 95, 322. [Google Scholar] [CrossRef]
- Njau, J.D.; Stephenson, R.; Menon, M.; Kachur, S.P.; McFarland, D.A. Exploring the impact of targeted distribution of free bed nets on households bed net ownership, socio-economic disparities and childhood malaria infection rates: analysis of national malaria survey data from three sub-Saharan Africa countries. Malaria journal 2013, 12, 1–15. [Google Scholar] [CrossRef]
- World Health Organization. World Malaria Report 2023; 2023; p. 283.
- Croft, T.N.; Marshall, A.M.; Allen, C.K.; Arnold, F.; Assaf, S.; Balian, S. Guide to DHS statistics. Rockville: ICF 2018, 645, 292–303. [Google Scholar]
- van Eijk, A.M.; Hill, J.; Alegana, V.A.; Kirui, V.; Gething, P.W.; ter Kuile, F.O.; Snow, R.W. Coverage of malaria protection in pregnant women in sub-Saharan Africa: a synthesis and analysis of national survey data. Lancet Infect. Dis. 2011, 11, 190–207. [Google Scholar] [CrossRef] [PubMed]
- Kebede, W.; Tolcha, A.; Soboksa, N.E.; Negassa, B.; Kanno, G.G.; Aregu, M.B. Utilization of insecticide-treated nets in households for Under-5 children and associated factors in east Mesekan District, Gurage zone, Southern Ethiopia. Environmental Health Insights 2023, 17, 11786302231164287. [Google Scholar] [CrossRef] [PubMed]
- Florey, L. Preventing malaria during pregnancy in sub-Saharan Africa: determinants of effective IPTp delivery. 2013.
- Martin, M.K.; Venantius, K.B.; Patricia, N.; Bernard, K.; Keith, B.; Allen, K.; Godfrey, A.; Rogers, T.; Damazo, K.T.; Dathan, B.M. Correlates of uptake of optimal doses of sulfadoxine-pyrimethamine for prevention of malaria during pregnancy in East-Central Uganda. Malaria Journal 2020, 19, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Erreygers, G. Correcting the concentration index. J. Health Econ. 2009, 28, 504–515. [Google Scholar] [CrossRef]
- Conceição, P.; Ferreira, P. The young person's guide to the Theil index: Suggesting intuitive interpretations and exploring analytical applications. 2000.
- Maghendji-Nzondo, S.; Nzoughe, H.; Lemamy, G.J.; Kouna, L.C.; Pegha-Moukandja, I.; Lekoulou, F.; Mbatchi, B.; Toure-Ndouo, F.; Lekana-Douki, J.B. Prevalence of malaria, prevention measures, and main clinical features in febrile children admitted to the Franceville Regional Hospital, Gabon. Parasite 2016, 23. [Google Scholar] [CrossRef]
- Bhatt, S.; Weiss, D.; Cameron, E.; Bisanzio, D.; Mappin, B.; Dalrymple, U.; Battle, K.; Moyes, C.; Henry, A.; Eckhoff, P. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 2015, 526, 207–211. [Google Scholar] [CrossRef]
- Degarege, A.; Fennie, K.; Degarege, D.; Chennupati, S.; Madhivanan, P. Improving socioeconomic status may reduce the burden of malaria in sub Saharan Africa: A systematic review and meta-analysis. PloS one 2019, 14, e0211205. [Google Scholar] [CrossRef]
- Talipouo, A.; Ngadjeu, C.S.; Doumbe-Belisse, P.; Djamouko-Djonkam, L.; Sonhafouo-Chiana, N.; Kopya, E.; Bamou, R.; Awono-Ambene, P.; Woromogo, S.; Kekeunou, S. Malaria prevention in the city of Yaoundé: knowledge and practices of urban dwellers. Malaria Journal 2019, 18, 1–13. [Google Scholar]
- Sumari, D.; Dillip, A.; Ndume, V.; Mugasa, J.P.; Gwakisa, P.S. Knowledge, attitudes and practices on malaria in relation to its transmission among primary school children in Bagamoyo district, Tanzania. MalariaWorld Journal 2016, 7. [Google Scholar]
- Kalu, G.O.; Francis, J.M.; Ibisomi, L.; Chirwa, T.; Kagura, J. Factors associated with the uptake of Intermittent Preventive Treatment (IPTp-SP) for malaria in pregnancy: Further analysis of the 2018 Nigeria Demographic and Health Survey. PLOS Global Public Health 2023, 3, e0000771. [Google Scholar] [CrossRef]
- Ochieng, W.; Munsey, A.; Kinyina, A.; Assenga, M.; Onikpo, F.; Binazon, A.; Adeyemi, M.; Alao, M.; Aron, S.; Nhiga, S. Antenatal care services in Benin and Tanzania 2021/2022: an equity analysis study. BMJ public health 2024, 2. [Google Scholar] [CrossRef] [PubMed]
- Gizaw, Z.; Astale, T.; Kassie, G.M. What improves access to primary healthcare services in rural communities? A systematic review. BMC Primary Care 2022, 23, 313. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.; Clarke, S.E.; Gosling, R.; Hamainza, B.; Killeen, G.; Magill, A.; O’Meara, W.; Price, R.N.; Riley, E.M. “Asymptomatic” malaria: a chronic and debilitating infection that should be treated. PLoS medicine 2016, 13, e1001942. [Google Scholar] [CrossRef] [PubMed]
- Baciu, A.; Negussie, Y.; Geller, A.; Weinstein, J.N.; National Academies of Sciences, E.; Medicine. The root causes of health inequity. In Communities in action: Pathways to health equity; National Academies Press (US): 2017.
- Assele, V.; Ndoh, G.E.; Nkoghe, D.; Fandeur, T. No evidence of decline in malaria burden from 2006 to 2013 in a rural Province of Gabon: implications for public health policy. BMC public health 2015, 15, 1–8. [Google Scholar] [CrossRef]
- Imboumy-Limoukou, R.K.; Maghendji-Nzondo, S.; Sir-Ondo-Enguier, P.N.; Niemczura De Carvalho, J.; Tsafack-Tegomo, N.P.; Buekens, J.; Okouga, A.P.; Mouinga-Ondeme, A.; Kwedy Nolna, S.; Lekana-Douki, J.-B. Malaria in children and women of childbearing age: infection prevalence, knowledge and use of malaria prevention tools in the province of Nyanga, Gabon. Malaria journal 2020, 19, 1–8. [Google Scholar] [CrossRef]
- Dahab, R.; Sakellariou, D. Barriers to accessing maternal care in low income countries in Africa: a systematic review. Int. J. Environ. Res. Public Health 2020, 17, 4292. [Google Scholar] [CrossRef]
- Kabudula, C.W.; Houle, B.; Collinson, M.A.; Kahn, K.; Tollman, S.; Clark, S. Assessing changes in household socioeconomic status in rural South Africa, 2001–2013: a distributional analysis using household asset indicators. Social indicators research 2017, 133, 1047–1073. [Google Scholar] [CrossRef]
- Ataguba, J.E.-O.; McIntyre, D. Who benefits from health services in South Africa? Health Economics, Policy and Law 2013, 8, 21–46. [Google Scholar] [CrossRef]
- Alaba, O.; Chola, L. Socioeconomic inequalities in adult obesity prevalence in South Africa: a decomposition analysis. Int. J. Environ. Res. Public Health 2014, 11, 3387–3406. [Google Scholar] [CrossRef]
- Saddiq, A.; Saleh, J.-E.A.; Wondimagegnehu, A.; Mpazanje, R.; Audu, B.M. Universal Access to Malaria Prevention, Diagnosis and Treatment as a Strategy toward Disease Control and Elimination: A Critical Look at Northeastern Nigeria. Open Access Library Journal 2019, 6, 1–12. [Google Scholar] [CrossRef]
- Naserrudin, N.A.; Lin, P.Y.P.; Monroe, A.; Baumann, S.E.; Adhikari, B.; Miller, A.C.; Sato, S.; Fornace, K.M.; Culleton, R.; Cheah, P.Y. Disentangling the intersection of inequities with health and malaria exposure: key lessons from rural communities in Northern Borneo. Malaria Journal 2023, 22, 343. [Google Scholar] [CrossRef]
- Ahorlu, C.S.; Adongo, P.; Koenker, H.; Zigirumugabe, S.; Sika-Bright, S.; Koka, E.; Tabong, P.T.-N.; Piccinini, D.; Segbaya, S.; Olapeju, B. Understanding the gap between access and use: a qualitative study on barriers and facilitators to insecticide-treated net use in Ghana. Malaria journal 2019, 18, 1–13. [Google Scholar] [CrossRef]
- Jenkins, S.P.; Van Kerm, P. The measurement of economic inequality. 2011.
- Wagstaff, A.; O'Donnell, O.; Van Doorslaer, E.; Lindelow, M. Analyzing health equity using household survey data: a guide to techniques and their implementation; World Bank Publications: 2007.
| Country | Year | ITN use in pregnancy % [95% CI] |
% change in ITN use in pregnancy | ITN use by under-fives % [95% CI] |
% change in ITN use in under-fives | IPTp coverage % [95% CI] |
% change in IPTp coverage |
|---|---|---|---|---|---|---|---|
| Mozambique | 2011 | 61.07 [56.60;65.53] | +18.80 | 65.15 [62.77;67.53] | +19.63 | 9.63 [8.16;11.11] | +159.40 |
| 2022/3 | 72.55 [67.70;77.39] | 77.94 [75.42;80.45] | 24.98 [22.75;27.21] | ||||
| Burkina Faso | 2010 | 76.65 [73.40;79.89] | +8.39 | 76.99 [75.20;78.77] | +13.46 | 40.95 [38.79;43.10] | +38.41 |
| 2021 | 83.08 [80.37;85.79] | 87.35 [86.16;88.54] | 56.68 [54.21;59.14] | ||||
| Tanzania | 2015/16 | 74.40 [70.69;78.11] | +13.74 | 76.71 [74.67;78.75] | +13.86 | 7.87 [6.71;9.03] | +299.87 |
| 2022 | 84.62 [81.24;88.00] | 87.34 [86.20;88.49] | 31.47 [29.13;33.81] | ||||
| Côte d'Ivoire | 2011/12 | 57.11 [52.11;62.12] | +36.89 | 59.61 [56.79;62.41] | +29.56 | 8.16 [6.64;9.67] | +322.18 |
| 2021 | 78.18 [74.49;81.88] | 77.23 [74.72;79.73] | 34.45 [31.70;37.20] | ||||
| Madagascar | 2008/09 | 75.86 [71.94;79.78] | +1.78 | 80.38 [78.46;82.31] | +5.54 | 1.93 [1.36;2.49] | +1504.15 |
| 2021 | 77.21 [73.81;80.62] | 84.83 [83.20;86.46] | 30.96 [28.80;33.11] | ||||
| Kenya | 2014 | 76.30 [72.93;79.67] | -1.85 | 80.97 [79.72;82.20] | -1.52 | 10.55 [9.25;11.85] | -38.86 |
| 2022 | 74.89 [71.29;78.49] | 79.74 [78.36;81.12] | 6.45 [5.68;7.22] | ||||
| Nigeria | 2013 | 29.82 [26.82;32.81] | +173.88 |
31.48 [29.16;33.80] | +153.97 | 7.02 [6.17;7.88] | +136.75 |
| 2018 | 81.67 [79.67;83.68] | 79.95 [78.70;81.19] | 16.62 [15.51;17.72] | ||||
| Uganda | 2011 | 71.14 [66.79;75.48] | +11.12 | 71.58 [69.42;73.74] | +14.64 | 10.57 [9.07;12.07] | +57.24 |
| 2016 | 79.05 [76.53;81.57] | 82.06 [80.79;83.32] | 17.40 [16.16;18.63] | ||||
| Cameroon | 2011 | 46.44 [39.86;53.01] | +67.44 | 51.17 [47.80;83.32] | +56.65 | 12.13 [10.90;13.36] | +168.26 |
| 2018 | 77.76 [74.04;81.48] | 80.16 [78.22;82.10] | 32.54 [30.26;34.83] | ||||
| Rwanda | 2014/15 | 87.72 [85.31;90.12] | -6.76 | 86.69 [85.48;87.90] | -3.20 | - | - |
| 2019/20 | 81.79 [78.13;85.46] | 83.92 [82.42;85.43] | - |
| Country | Year | ENCI | p-values | Robust standard errors |
|---|---|---|---|---|
| Mozambique | 2011 | -0.003 | 0.934 | 0.040 |
| 2022/3 | 0.000 | 0.995 | 0.040 | |
| Burkina Faso | 2010 | -0.003 | 0.914 | 0.029 |
| 2021 | -0.023 | 0.334 | 0.024 | |
| Tanzania | 2015/16 | -0.006 | 0.862 | 0.035 |
| 2022 | -0.008 | 0.761 | 0.027 | |
| Côte d'Ivoire | 2011/12 | -0.117 | 0.003 | 0.040 |
| 2021 | -0.216 | 0.000 | 0.028 | |
| Madagascar | 2008/09 | -0.002 | 0.950 | 0.031 |
| 2021 | -0.049 | 0.108 | 0.030 | |
| Kenya | 2014 | 0.069 | 0.009 | 0.026 |
| 2022 | 0.052 | 0.063 | 0.028 | |
| Rwanda | 2014/15 | 0.109 | 0.000 | 0.026 |
| 2019/20 | 0.122 | 0.001 | 0.036 | |
| Nigeria | 2013 | 0.067 | 0.010 | 0.026 |
| 2018 | -0.156 | 0.000 | 0.018 | |
| Uganda | 2011 | -0.037 | 0.330 | 0.038 |
| 2016 | 0.025 | 0.248 | 0.022 | |
| Cameroon | 2011 | 0.090 | 0.148 | 0.061 |
| 2018 | 0.020 | 0.543 | 0.034 |
| Country | Year | ENCI | p-values | Robust standard errors |
|---|---|---|---|---|
| Mozambique | 2011 | 0.043 | 0.001 | 0.011 |
| 2022/3 | 0.149 | 0.000 | 0.018 | |
| Burkina Faso | 2010 | 0.084 | 0.000 | 0.017 |
| 2021 | 0.082 | 0.000 | 0.021 | |
| Tanzania | 2015/16 | 0.016 | 0.113 | 0.010 |
| 2022 | 0.033 | 0.085 | 0.019 | |
| Côte d'Ivoire | 2011/12 | 0.035 | 0.004 | 0.012 |
| 2021 | 0.117 | 0.000 | 0.019 | |
| Madagascar | 2008/09 | -0.003 | 0.611 | 0.005 |
| 2021 | 0.062 | 0.001 | 0.019 | |
| Kenya | 2014 | 0.016 | 0.080 | 0.009 |
| 2022 | 0.019 | 0.005 | 0.008 | |
| Nigeria | 2013 | 0.026 | 0.000 | 0.006 |
| 2018 | 0.115 | 0.000 | 0.010 | |
| Uganda | 2011 | 0.012 | 0.329 | 0.012 |
| 2016 | 0.008 | 0.454 | 0.011 | |
| Cameroon | 2011 | 0.080 | 0.000 | 0.012 |
| 2018 | 0.178 | 0.000 | 0.019 |
| Country | Year | ENCI | p-values | Robust standard errors |
|---|---|---|---|---|
| Mozambique | 2011 | -0.059 | 0.006 | 0.022 |
| 2022/3 | 0.054 | 0.006 | 0.020 | |
| Burkina Faso | 2010 | 0.003 | 0.843 | 0.014 |
| 2021 | -0.022 | 0.020 | 0.010 | |
| Tanzania | 2015/16 | 0.052 | 0.003 | 0.018 |
| 2022 | 0.009 | 0.381 | 0.011 | |
| Côte d'Ivoire | 2011/12 | -0.090 | 0.000 | 0.021 |
| 2021 | -0.183 | 0.000 | 0.014 | |
| Madagascar | 2008/09 | 0.020 | 0.148 | 0.014 |
| 2021 | -0.005 | 0.642 | 0.012 | |
| Kenya | 2014 | 0.086 | 0.000 | 0.010 |
| 2022 | 0.027 | 0.006 | 0.010 | |
| Rwanda | 2014/15 | 0.068 | 0.000 | 0.011 |
| 2019/20 | 0.080 | 0.000 | 0.013 | |
| Nigeria | 2013 | 0.060 | 0.002 | 0.019 |
| 2018 | -0.139 | 0.000 | 0.011 | |
| Uganda | 2011 | 0.010 | 0.535 | 0.016 |
| 2016 | 0.010 | 0.300 | 0.010 | |
| Cameroon | 2011 | 0.083 | 0.014 | 0.034 |
| 2018 | -0.044 | 0.009 | 0.017 |
| Country | Year | ITN use in pregnancy | IPTp coverage | ITN use by under-fives | |||
|---|---|---|---|---|---|---|---|
| Urban GE(2) |
Rural GE(2) |
Urban GE(2) |
Rural GE(2) |
Urban GE(2) |
Rural GE(2) |
||
| Mozambique | 2011 | 0.215 | 0.444 | 0.326 | 0.674 | 0.236 | 0.345 |
| 2022/3 | 0.164 | 0.221 | 1.005 | 1.874 | 0.099 | 0.189 | |
| Burkina Faso | 2010 | 0.171 | 0.138 | 0.552 | 0.694 | 0.159 | 0.134 |
| 2021 | 0.120 | 0.090 | 0.331 | 0.390 | 0.088 | 0.067 | |
| Tanzania | 2015/16 | 0.145 | 0.164 | 4.386 | 7.084 | 0.130 | 0.162 |
| 2022 | 0.094 | 0.103 | 1.077 | 1.639 | 0.077 | 0.080 | |
| Côte d'Ivoire | 2011/12 | 0.429 | 0.295 | 5.161 | 7.592 | 0.407 | 0.285 |
| 2021 | 0.172 | 0.096 | 0.940 | 1.207 | 0.186 | 0.090 | |
| Madagascar | 2008/09 | 0.136 | 0.166 | 22.53 | 22.26 | 0.093 | 0.131 |
| 2021 | 0.187 | 0.127 | 1.083 | 1.008 | 0.086 | 0.086 | |
| Kenya | 2014 | 0.113 | 0.186 | 4.080 | 4.300 | 0.095 | 0.141 |
| 2022 | 0.151 | 0.159 | 6.467 | 7.657 | 0.139 | 0.118 | |
| Nigeria | 2013 | 0.891 | 1.273 | 6.905 | 7.281 | 0.834 | 1.145 |
| 2018 | 0.179 | 0.093 | 1.880 | 2.848 | 0.179 | 0.106 | |
| Uganda | 2011 | 0.097 | 0.209 | 5.272 | 4.777 | 0.148 | 0.205 |
| 2016 | 0.109 | 0.137 | 2.689 | 2.363 | 0.089 | 0.113 | |
| Cameroon | 2011 | 0.426 | 0.645 | 2.579 | 4.279 | 0.383 | 0.488 |
| 2018 | 0.159 | 0.178 | 0.733 | 1.443 | 0.138 | 0.126 | |
| Rwanda | 2014/15 | 0.046 | 0.079 | - | - | 0.045 | 0.086 |
| 2019/20 | 0.058 | 1.275 | - | - | 0.066 | 0.107 | |
| Country | Year | ITN use in pregnancy | IPTp coverage | ITN use by under-fives | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Poor GE(2) | Middle GE(2) | Rich GE(2) | Poor GE(2) | Middle GE(2) | Rich GE(2) | Poor GE(2) | Middle GE(2) | Rich GE(2) | ||
| Mozambique | 2011 | 0.374 | 0.277 | 0.374 | 6.964 | 5.116 | 3.970 | 0.269 | 0.257 | 0.345 |
| 2022/3 | 0.190 | 0.226 | 0.194 | 2.315 | 1.714 | 0.994 | 0.179 | 0.162 | 0.130 | |
| Burkina Faso | 2010 | 0.141 | 0.153 | 0.145 | 0.791 | 0.654 | 0.551 | 0.146 | 0.132 | 0.140 |
| 2021 | 0.094 | 0.086 | 0.110 | 0.445 | 0.365 | 0.313 | 0.065 | 0.068 | 0.083 | |
| Tanzania | 2015/16 | 0.167 | 0.120 | 0.173 | 6.688 | 7.531 | 5.287 | 0.142 | 0.162 | 0.158 |
| 2022 | 0.104 | 0.078 | 0.109 | 1.584 | 1.458 | 1.320 | 0.074 | 0.080 | 0.083 | |
| Côte d'Ivoire | 2011/12 | 0.268 | 0.369 | 0.450 | 7.923 | 9.047 | 4.405 | 0.280 | 0.283 | 0.432 |
| 2021 | 0.063 | 0.153 | 0.285 | 1.335 | 1.187 | 0.684 | 0.071 | 0.147 | 0.258 | |
| Madagascar | 2008/09 | 0.155 | 0.203 | 0.149 | 20.80 | 24.32 | 23.30 | 0.127 | 0.120 | 0.117 |
| 2021 | 0.119 | 0.137 | 0.161 | 1.201 | 0.815 | 0.922 | 0.084 | 0.089 | 0.087 | |
| Kenya | 2014 | 0.184 | 0.164 | 0.120 | 4.664 | 3.289 | 4.114 | 0.153 | 0.112 | 0.095 |
| 2022 | 0.186 | 0.106 | 0.146 | 8.606 | 5.975 | 6.331 | 0.120 | 0.094 | 0.150 | |
| Nigeria | 2013 | 1.403 | 0.852 | 1.047 | 10.06 | 4.841 | 6.422 | 1.244 | 0.800 | 0.961 |
| 2018 | 0.072 | 0.121 | 0.226 | 3.649 | 2.465 | 1.541 | 0.085 | 0.125 | 0.215 | |
| Uganda | 2011 | 0.163 | 0.204 | 0.197 | 5.365 | 4.259 | 4.671 | 0.173 | 0.245 | 0.186 |
| 2016 | 0.130 | 0.185 | 0.104 | 2.482 | 2.394 | 2.338 | 0.104 | 0.126 | 0.103 | |
| Cameroon | 2011 | 0.650 | 0.542 | 0.445 | 4.851 | 3.796 | 2.281 | 0.527 | 0.426 | 0.375 |
| 2018 | 0.171 | 0.199 | 0.150 | 1.566 | 1.120 | 0.649 | 0.113 | 0.146 | 0.143 | |
| Rwanda | 2014/15 | 0.127 | 0.044 | 0.045 | - | - | - | 0.100 | 0.081 | 0.052 |
| 2019/20 | 0.184 | 0.094 | 0.076 | - | - | - | 0.128 | 0.087 | 0.078 | |
| Country | Year | ITN use in pregnancy | IPTp coverage | ITN use by under-fives | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall inequality GE(2) |
(%Contr) | (%Contr) | Overall inequality GE(2) |
(%Contr) | (%Contr) | Overall inequality GE(2) |
(%Contr) | (%Contr) | ||
| Mozambique | 2011 | 0.353 | 0.009 (2.55%) | 0.344 (97.45%) | 5.01 | 0.021 (0.42%) | 4.989 (99.58%) | 0.301 | 0.002 (0.33%) | 0.300 (99.67%) |
| 2022/3 | 0.199 | 0.000 (0%) | 0.199 (100%) | 1.517 | 0.026 (1.71%) | 1.491 (98.29) | 0.151 | 0.002 (1.32%) | 0.149 (98.68%) | |
| Burkina Faso | 2010 | 0.145 | 0.000 (0%) | 0.145 (100%) | 0.659 | 0.001 (0.15%) | 0.658 (99.85) | 0.140 | 0.000 (0%) | 0.140 (100%) |
| 2021 | 0.099 | 0.000 (0%) | 0.099 (100%) | 0.372 | 0.001 (0%) | 0.372 (100%) | 0.073 | 0.000 (0%) | 0.073 (100%) | |
| Tanzania | 2015/16 | 0.159 | 0.000 (0%) | 0.159 (100%) | 6.202 | 0.021 (0.34%) | 6.181 (99.66%) | 0.153 | 0.000 (0%) | 0.153 (100%) |
| 2022 | 0.101 | 0.000 (0%) | 0.101 (100%) | 1.449 | 0.010 (0.69%) | 1.439 (99.31%) | 0.080 | 0.000 (0%) | 0.080 (100%) | |
| Côte d'Ivoire | 2011/12 | 0.334 | 0.003 (0.60%) | 0.332 (99.40%) | 6.555 | 0.016 (0.24%) | 6.539 (99.76%) | 0.321 | 0.002 (0.62%) | 0.319 (99.38%) |
| 2021 | 0.126 | 0.002 (1.59%) | 0.124 (98.41%) | 1.088 | 0.004 (0.37%) | 1.084 (99.63%) | 0.123 | 0.003 (1.63%) | 0.121 (98.37%) | |
| Madagascar | 2008/09 | 0.160 | 0.000 (0%) | 0.160 (100%) | 22.12 | 0.000 (0%) | 22.12 (100%) | 0.122 | 0.000 (0%) | 0.122 (100%) |
| 2021 | 0.136 | 0.001 (0%) | 0.136 (100%) | 1.021 | 0.000 (0%) | 1.021 (100%) | 0.086 | 0.000 (0%) | 0.086 (100%) | |
| Kenya | 2014 | 0.158 | 0.002 (0.67%) | 0.157 (99.37%) | 4.227 | 0.000 (0%) | 4.227 (100%) | 0.124 | 0.001 (0.81%) | 0.123 (99.19%) |
| 2022 | 0.156 | 0.000 (0%) | 0.156 (100%) | 7.214 | 0.003 (0%) | 7.212 (100%) | 0.125 | 0.000 (0%) | 0.125 (100%) | |
| Nigeria | 2013 | 0.148 | 0.007 (4.73%) | 1.141 (95.27%) | 7.152 | 0.000 (0%) | 7.152 (100%) | 1.036 | 0.005 (0.48%) | 1.031 (99.52%) |
| 2018 | 0.116 | 0.002 (1.72%) | 0.114 (98.28%) | 2.412 | 0.016 (0.66%) | 2.396 (99.34%) | 0.128 | 0.001 (0.78%) | 0.127 (99.22%) | |
| Uganda | 2011 | 0.182 | 0.003 (1.65%) | 0.179 (98.35%) | 4.879 | 0.001 (0.02%) | 4.878 (99.98) | 0.189 | 0.000 (0%) | 0.189 (100%) |
| 2016 | 0.131 | 0.000 (0%) | 0.131 (100%) | 2.417 | 0.000 (0%) | 2.417 (100%) | 0.108 | 0.000 (0%) | 0.108 (100%) | |
| Cameroon | 2011 | 0.544 | 0.006 (1.10%) | 0.538 (98.90%) | 3.411 | 0.025 (0.73%) | 3.386 (99.27%) | 0.440 | 0.002 (0.45%) | 0.438(99.55%) |
| 2018 | 0.169 | 0.000 (0%) | 0.169 (100%) | 1.051 | 0.026 (2.47%) | 1.025 (97.53%) | 0.132 | 0.000 (0%) | 0.132 (100%) | |
| Rwanda | 2014/15 | 0.071 | 0.000 (0%) | 0.071 (100%) | - | - | - | 0.075 | 0.000 (0%) | 0.075 (100%) |
| 2019/20 | 0.109 | 0.001 (0.92%) | 0.108 (99.08%) | - | - | - | 0.096 | 0.000 (0%) | 0.096 (100%) | |
| Country | Year | ITN use in pregnancy | IPTp coverage | ITN use by under-fives | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall inequality GE(2) |
(%Contr) | (%Contr) | Overall inequality GE(2) |
(%Contr) | (%Contr) | Overall inequality GE(2) |
(%Contr) | |||
| Mozambique | 2011 | 0.353 | 0.001 (0.28%) | 0.352 (99.72%) | 5.010 | 0.024 (0.48%) | 4.986 (99.52%) | 0.300 | 0.001 (0%) | 0.300 (100%) |
| 2022/3 | 0.200 | 0.000 (0%) | 0.200 (100%) | 1.517 | 0.041 (2.70%) | 1.476 (97.30%) | 0.151 | 0.000 (0%) | 0.151 (100%) | |
| Burkina Faso | 2010 | 0.145 | 0.000 (0%) | 0.145 (100%) | 0.659 | 0.004 (0.61%) | 0.655 (99.39%) | 0.140 | 0.000 (0%) | 0.140 (100%) |
| 2021 | 0.099 | 0.000 (0%) | 0.099 (100%) | 0.372 | 0.002 (0.54%) | 0.370 (99.46%) | 0.073 | 0.000 (0%) | 0.073 (100%) | |
| Tanzania | 2015/16 | 0.159 | 0.001 (0.63%) | 0.158 (99.37%) | 6.202 | 0.008 (0.13%) | 6.194 (99.87%) | 0.152 | 0.000 (0%) | 0.152 (100%) |
| 2022 | 0.100 | 0.000 (0%) | 0.100 (100%) | 1.449 | 0.002 (0.07%) | 1.448 (99.93%) | 0.079 | 0.000 (0%) | 0.079 (100%) | |
| Côte d'Ivoire | 2011/12 | 0.334 | 0.004 (1.20%) | 0.330 (98.80%) | 6.555 | 0.042 (0.64%) | 6.513 (99.36%) | 0.321 | 0.003 (0.93%) | 0.318 (99.07%) |
| 2021 | 0.126 | 0.008 (7.14%) | 0.117 (92.86%) | 1.088 | 0.019 (1.84%) | 1.068 (98.16%) | 0.123 | 0.006 (4.88%) | 0.117 (95.12%) | |
| Madagascar | 2008/09 | 0.160 | 0.000 (0%) | 0.160 (100%) | 22.13 | 0.002 (0.05%) | 22.12 (99.95%) | 0.122 | 0.000 (0%) | 0.122 (100%) |
| 2021 | 0.136 | 0.000 (0%) | 0.136 (100%) | 1.022 | 0.006 (0.59%) | 1.016 (99.41%) | 0.086 | 0.000 (0%) | 0.086 (100%) | |
| Kenya | 2014 | 0.158 | 0.001 (5.07%) | 0.157 (94.93%) | 4.227 | 0.007 (0.17%) | 4.220 (99.83%) | 0.124 | 0.001 (0.81%) | 0.123 (99.19%) |
| 2022 | 0.156 | 0.001 (0%) | 0.156 (100%) | 7.214 | 0.011 (0.17%) | 7.202 (99.83%) | 0.124 | 0.000 (0%) | 0.124 (100%) | |
| Nigeria | 2013 | 1.147 | 0.010 (0.87%) | 1.137 (99.13%) | 7.152 | 0.038 (0.52%) | 7.115 (99.48%) | 1.036 | 0.007 (0.68%) | 1.029 (99.32%) |
| 2018 | 0.116 | 0.004 (4.31%) | 0.111 (95.69%) | 2.412 | 0.050 (2.07%) | 2.362 (97.93%) | 0.128 | 0.004 (2.34%) | 0.125 (97.66%) | |
| Uganda | 2011 | 0.181 | 0.000 (0%) | 0.181 (100%) | 4.879 | 0.003 (0.06%) | 4.876 (99.94%) | 0.190 | 0.001 (0%) | 0.190 (100%) |
| 2016 | 0.130 | 0.000 (0%) | 0.130 (100%) | 2.417 | 0.000 (0%) | 2.417 (100%) | 0.108 | 0.000 (0%) | 0.108 (100%) | |
| Cameroon | 2011 | 0.544 | 0.004 (0.74%) | 0.540 (99.26%) | 3.411 | 0.045 (2.32%) | 3.366 (98.68%) | 0.440 | 0.002 (0.68%) | 0.437 (99.32%) |
| 2018 | 0.169 | 0.000 (0%) | 0.169 (100%) | 1.051 | 0.034 (3.24%) | 1.017 (96.76%) | 0.131 | 0.000 (0%) | 0.131 (100%) | |
| Rwanda | 2014/15 | 0.071 | 0.002 (2.82%) | 0.069 (97.18%) | _ | _ | _ | 0.076 | 0.001 (1.32%) | 0.075 (98.68%) |
| 2019/20 | 0.110 | 0.003 (2.73%) | 0.107 (97.27%) | _ | _ | _ | 0.096 | 0.001 (1.04%) | 0.095 (98.96%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





