Introduction:
Sleep is a vital and indispensable physiological process in human life, crucial for physical development, mental recovery, and fatigue elimination1. Poor sleep quality significantly impacts college students' academic performance, daily life, and well-being. According to recent surveys, 12.92% to 52.81% of Chinese college students suffer from sleep disorders, which cause emotional fluctuations and cognitive impairments2.Many researches has demonstrated that physical activity exerts a pivotal role in the pathophysiology of neurological disorders and possesses the capacity to effectively mitigate a spectrum of sleep-related issues3,4. Physical activity can enhance energy expenditure and regulate metabolic capacity, thereby increasing sleep duration and the amount of slow-wave sleep5.Currently, exercise training, as a non-invasive, eco-friendly, and healthy intervention method, is often used in the treatment of mild sleep disorders. However, current research in this area is relatively limited, constrained by equipment constraints and a lack of thorough exploration into the regulatory effects and underlying mechanisms of diverse exercise types on sleep6.
Polysomnography (PSG) is considered the gold standard for diagnosing various sleep disorders, but it has inherent limitations3,7.Polysomnography (PSG) is considered the gold standard for diagnosing various sleep disorders, but it has inherent limitations4.In recent years, alternative sleep monitoring devices such as actigraphy, fitness trackers/watches, and smartphone applications have emerged, and their data accuracy and safety have improved significantly with technological advancements 8.
This study addresses prevalent sleep issues among college students, examining the effects of aerobic and resistance training on sleep quality through rigorous experiments. Personalized exercise prescriptions were provided, revealing benefits of aerobic exercise in prolonging sleep, improving oxygen saturation, and reducing nighttime awakenings, while resistance training uniquely enhanced deep and REM sleep. The study offers a scientific foundation for effective sleep interventions, aiming to improve students' overall well-being.
Methods:
Study Design and Ethical Approval: This research received approval from the Human Experimental Ethics Committee of Nanjing Sports Institute (Ethics Approval No: RT-2021-03). The study, conducted in two parts from March 7 to July 21, 2022, involved a prospective survey to assess the overall sleep quality of college students before the formal intervention experiment.
Part 1: Prospective Survey
In the initial part, a convenience sampling method was employed, and 182 college students on campus participated. The Pittsburgh Sleep Quality Index (PSQI) questionnaire was administered on-site to evaluate sleep quality.
Part 2: Intervention Experiment
Participants from the initial survey were screened based on inclusion and exclusion criteria:
Inclusion Criteria:
Ages 18 to 25 with no acute or major illnesses.
No use of sedatives or other sleep aids in the four weeks prior.
Pittsburgh Sleep Quality Index (PSQI) score of ≥7.
Experiencing less than 6 hours of total sleep time for at least 4 nights per week in the past 3 months.
Reported decreased sleep quality, insufficient depth of sleep, or ≥3 nightmares per week in the past 3 months.
Exclusion Criteria:
Failure to meet the inclusion criteria.
Presence of cardiovascular, respiratory, cardiac, renal, or other underlying diseases.
Poor cooperation and repeated unsuccessful communication.
Non-compliance with the study regulations.
Participant Enrollment and Randomization:
A total of 23 participants were recruited, as shown in
Figure 1. Informed consent was obtained from all participants. Participants were randomly assigned and numbered, with some initially allocated to the aerobic exercise group (12 participants, with 4 withdrawals) and others to the resistance exercise group (11 participants, with 3 withdrawals). Ultimately, 16 participants (8 in each group) completed the trial.
Table 1.
Description characteristics of participants in this study.
Table 1.
Description characteristics of participants in this study.
| Characteristic |
Aerobic exercise group |
Resistance training group |
| Age (years) |
20.50±1.06 |
20.25±1.16 |
| Gender (male/female) |
5/3 |
4/4 |
| BMI (kg/m2) |
23.05±1.42 |
23.12±1.53 |
| Number of subjects with exercise habits |
6 |
5 |
Intervention Methods:
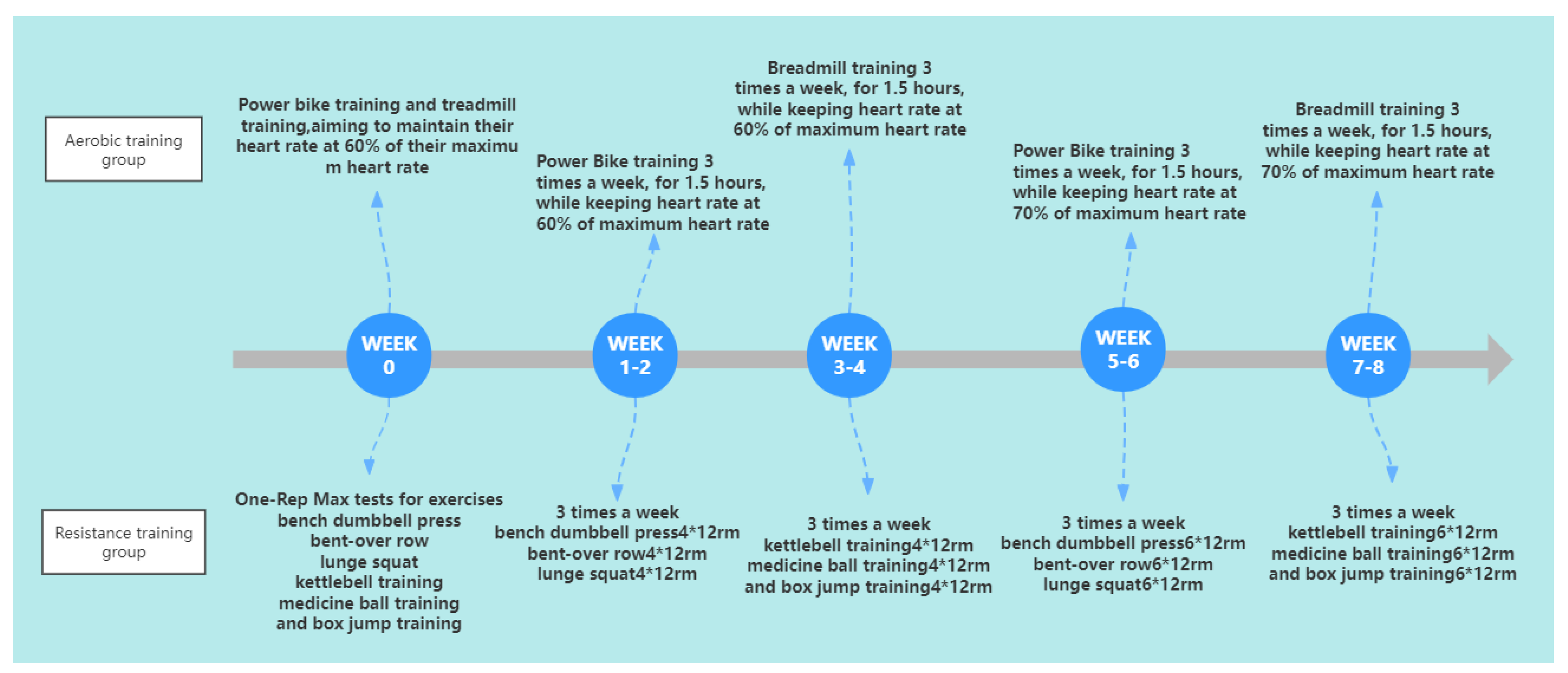
Before the trial commenced (week 0), all participants underwent a one-week adaptive training phase using Huawei Band 6 smart bands, obtained from Huawei Mall (
http://www.vmall.com). During this initial phase, the resistance training group underwent One-Rep Max tests for exercises, including bench dumbbell press, bent-over row, lunge squat, kettlebell training, medicine ball training, and box jump training. These assessments were conducted to determine the appropriate exercise intensity for the subsequent intervention. The aerobic training group utilized the smart wearable devices for power bike training and treadmill training, aiming to maintain their heart rate at 60% of their maximum heart rate during the sessions.At the start of the trial, all participants commenced the planned intervention training. The intervention spanned 8 weeks, consisting of three sessions per week, each lasting 1.5 hours. Before each session, participants conducted a warm-up routine to prepare. The resistance group engaged in six sets of resistance training with a 5-minute rest period, while the aerobic group completed two sets of intensive aerobic training, each lasting 30 minutes, with a 10-minute rest period. The detailed training program is outlined in
Figure 2.
Data Collection
The trial spanned a total of 9 weeks, during which the sleep data collected by the Huawei Band 6 smart bracelet was uploaded at the end of each week. Sleep data was collected from the pre-trial period (week 0) until the final week of the trial (week 8). Each participant was provided with a Huawei Band 6 smart bracelet, which had to be worn on the wrist during both exercise and sleep. All participants were required to have the Huawei Sports Health app installed on their phones, and the bracelet was connected to the phone via Bluetooth. The smart bracelet recorded participants' nightly sleep patterns and generated data on various sleep metrics, including bedtime, frequency of night awakenings, proportions of deep sleep and light sleep, REM sleep ratio, total sleep duration, calorie consumption, blood oxygen saturation levels, and weekly averages. Participants were instructed to avoid consuming sleep-disrupting beverages such as beer or strong tea, as well as excessively hot or fatty foods. They were also required to regularly submit their smart bracelet data as per the scheduled timeframe.
Statistical Methods
The SPSS 25.0 software (IBM Corp., Armonk, NY, USA) was utilized to perform all Friedman tests and t-tests. The data was presented as the mean ± standard deviation. To assess the differences within groups, intra-group t-tests were conducted. Inter-group differences were assessed through independent samples t-tests. The effectiveness was investigated using chi-square tests. Results with a P-value below 0.05 were considered statistically significant.Radar chart analysis was executed to visually illustrate the distinct intervention effects of aerobic and resistance training on sleep quality. Spearman correlation coefficients were calculated to explore relationships among sleep parameters. Positive and negative correlations were identified, and statistical significance was determined at p < 0.05.
Results
Analysis of Prospective Survey:
In the initial phase of the study, a cohort of 182 college students underwent recruitment, and their PSQI total and item scores were assessed through a prospective survey (n=182). The findings, presented in
Table 2, revealed that the participants exhibited a significantly higher Total PSQI score (12.82±2.31) in comparison to the recommended threshold for optimal sleep quality (score of 6). Notably, there were remarkable increases in scores related to sleep latency (2.56±0.78), sleep quality (2.46±0.57), and daytime dysfunction (2.39±0.75). Importantly, it is noteworthy that none of the participants reported the use of any sleep medication. These results signify a considerable deviation from the optimal sleep parameters, highlighting pronounced challenges in various facets of sleep quality among the participants. The elevated scores across multiple dimensions, such as sleep latency, sleep quality, and daytime dysfunction, underscore the substantial sleep-related difficulties experienced by the participants.
Effect of Exercise Intervention on Sleep Quality and Sleep Parameters:
After screening, 16 subjects were finally included in the study.
Table 3 presents the comparison of sleep quality before and after exercise intervention.
The Total sleep duration significantly increased from 396.12±17.40 minutes to 422.83±16.80 minutes (p < 0.05). Similarly, the duration of deep sleep significantly increased from 106.00±3.93 minutes to 131.68±6.69 minutes (p < 0.05). However, there was no significant difference in the duration of light sleep (p > 0.05). The duration of REM sleep significantly increased from 80.85±4.56 minutes to 86.22±3.68 minutes (p < 0.05). The frequency of night waking significantly decreased from 2.08±0.37 times to 0.75±0.41 times (p < 0.05). Moreover, the sleep quality score significantly improved from 77.55±1.45 to 82.49±1.26 (p < 0.05). Oxygen saturation during sleep significantly increased from 93.96±0.49% to 97.91±0.57% (p < 0.05). Additionally, the energy expenditure during sleep significantly increased from 440.44±13.59 kcal to 525.81±11.83 kcal (p < 0.05).
These findings suggest that the exercise intervention positively impacted sleep quality. It led to significant improvements in sleep duration, duration of deep sleep, duration of REM sleep, and a reduction in the frequency of night waking. Furthermore, there were significant enhancements in the sleep quality score, oxygen saturation during sleep, and energy expenditure during sleep. These results indicate that exercise intervention can effectively enhance sleep structure, improve sleep quality, and promote physiological recovery and adaptation during sleep.
Differential Intervention Effects of Exercise Modalities on Sleep Quality:
The intervention effects of the aerobic exercise group and the resistance exercise group are presented in
Table 4. Both aerobic exercise and resistance training interventions led to significant improvements in sleep quality, REM sleep duration, night waking frequency, energy expenditure during sleep, duration of deep sleep, and oxygen saturation levels during sleep. These improvements were statistically significant, indicating that the observed changes were unlikely to occur by chance.Sleep quality scores significantly improved in both groups, with the aerobic exercise group increasing from 77.01±1.51 to 82.09±1.06 (p < 0.001) and the resistance exercise group increasing from 78.10±1.23 to 82.90±1.39 (p < 0.001). The duration of REM sleep significantly increased in the aerobic exercise group from 79.77±4.14 to 86.22±3.81 minutes (p < 0.05), while the resistance exercise group had a larger increase from 81.93±4.98 to 97.44±5.14 minutes (p < 0.05).Both groups showed a significant decrease in night waking frequency, with the aerobic exercise group decreasing from 2.07±0.40 to 0.82±0.39 times (p < 0.05) and the resistance exercise group decreasing from 2.09±0.37 to 0.68±0.43 times (p < 0.05). Energy expenditure during sleep significantly increased in both groups, with the aerobic exercise group increasing from 441.88±18.24 to 530.50±12.10 kcal (p < 0.05) and the resistance exercise group increasing from 439.00±7.63 to 521.13±10.16 kcal (p < 0.05).The duration of deep sleep significantly increased in both groups, with the aerobic exercise group increasing from 105.18±5.07 to 135.17±5.05 minutes (p < 0.05) and the resistance exercise group increasing from 106.84±2.41 to 128.21±6.52 minutes (p < 0.05). Oxygen saturation levels during sleep significantly improved in both groups, with the aerobic exercise group increasing from 93.99±0.51 to 98.40±0.22 (p < 0.05) and the resistance exercise group increasing from 93.93±0.90 to 97.43±0.33 (p < 0.05).
Table 3.
Comparison of Sleep Parameter Improvements Before and After Training.
Table 3.
Comparison of Sleep Parameter Improvements Before and After Training.
| Projects |
Pre |
Post |
| Total sleep duration |
396.12±17.40 |
422.83±16.80✳ |
| Duration of deep sleep |
106.00±3.93 |
131.68±6.69✳ |
| Duration of light sleep |
209.09±10.95 |
199.31±12.53 |
| Duration of REM |
80.85±4.56 |
86.22±3.68✳ |
| Frequency of night waking |
2.08±0.37 |
0.75±0.41✳ |
| Sleep Quality Score |
77.55±1.45 |
82.49±1.26✳ |
| Oxygen saturation during sleep |
93.96±0.49 |
97.91±0.57✳ |
| Energy expenditure during sleep |
440.44±13.59 |
525.81±11.83✳ |
Table 4.
Comparison of Sleep Parameter Improvements Before and After Training in the Aerobic Exercise and Resistance Training Groups.
Table 4.
Comparison of Sleep Parameter Improvements Before and After Training in the Aerobic Exercise and Resistance Training Groups.
| Projects |
Aerobic training group |
Resistance training group |
| Pre |
Post |
Pre |
Post |
| Total sleep duration |
392.90±19.35 |
417.35±19.67✳ |
399.35±15.84 |
428.31±12.23✳ |
| Duration of deep sleep |
105.18±5.07 |
135.17±5.05✳ |
106.84±2.41 |
128.21±6.52✳Δ |
| Duration of light sleep |
207.61±11.79 |
195.96±12.22 |
210.58±10.62 |
202.66±12.71 |
| Duration of REM |
79.77±4.14 |
86.22±3.81✳ |
81.93±4.98 |
97.44±5.14✳Δ |
| Frequency of night waking |
2.07±0.40 |
0.82±0.39✳ |
2.09±0.37 |
0.68±0.43✳ |
| Sleep Quality Score |
77.01±1.51 |
82.09±1.06✳ |
78.10±1.23 |
82.90±1.39✳ |
| Oxygen saturation during sleep |
93.99±0.51 |
98.40±0.22✳ |
93.93±0.90 |
97.43±0.33✳Δ |
| Energy expenditure during sleep |
441.88±18.24 |
530.50±12.10✳ |
439.00±7.63 |
521.13±10.16✳ |
Effects of Different Exercise Modes on Sleep Quality: Insights from Radar Chart Analysis and Correlation Coefficients"
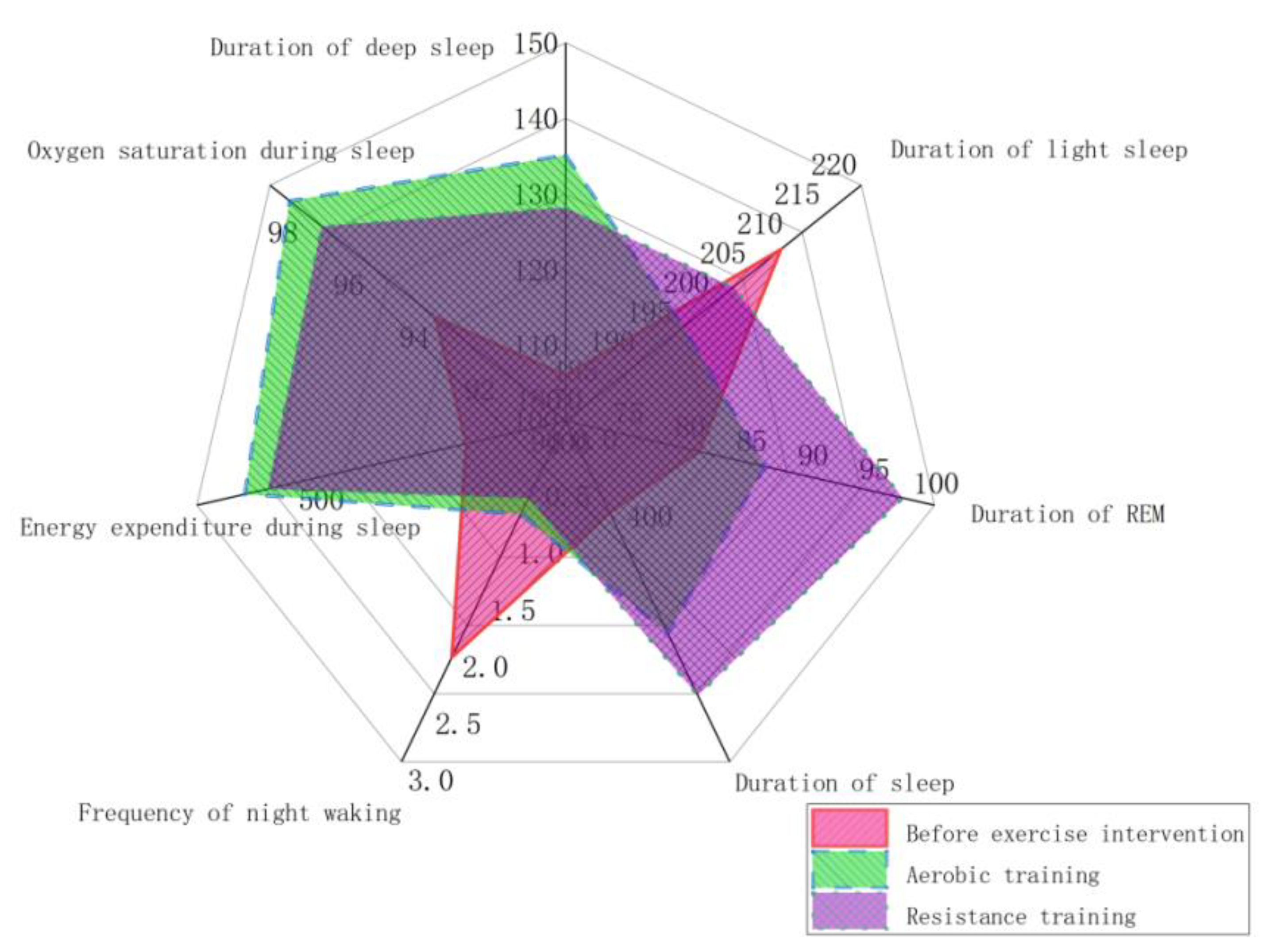
Figure 3 illustrates the impact of different exercise modes on sleep quality. The radar chart analysis clearly reveals that each type of exercise has distinct intervention effects. Aerobic training significantly improves sleep duration, deep sleep duration, and blood oxygen saturation, while also reducing wakefulness. These findings highlight the positive influence of aerobic training on sleep quality. On the other hand, resistance training shows more notable enhancements in deep sleep duration and REM sleep duration, accompanied by a significant decrease in wakefulness. These results emphasize the specific benefits of resistance training in enhancing sleep quality. Therefore, selecting appropriate exercise modalities based on individual needs and goals holds great potential for optimizing sleep quality and promoting overall well-being.
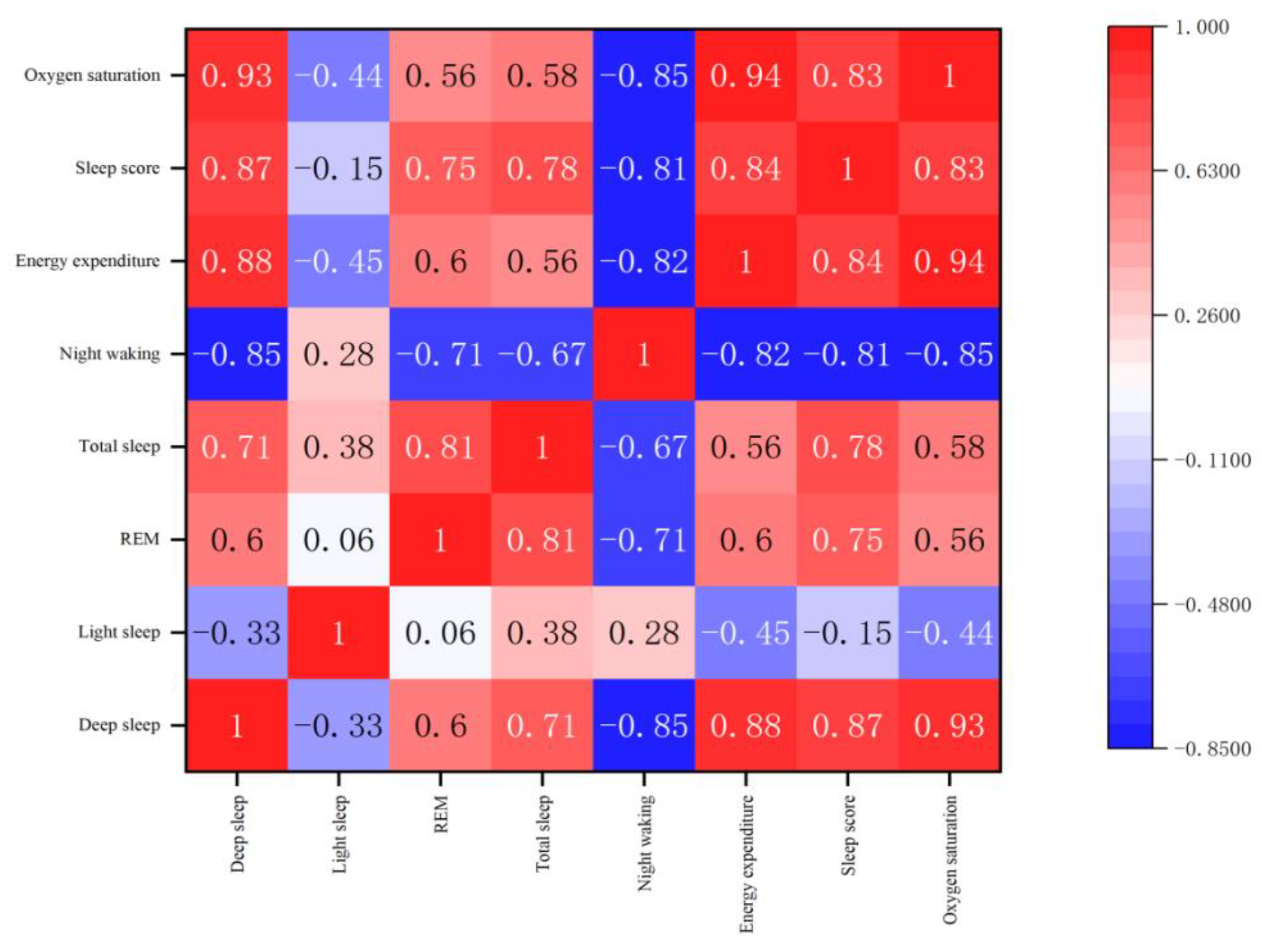
In
Figure 4, the Spearman correlation coefficients illuminate the intricate relationships among diverse sleep parameters. Positive correlations, particularly between deep sleep duration and crucial metrics like total sleep duration, energy expenditure during sleep, sleep score, and oxygen saturation during sleep, signify a cohesive association. This suggests that an augmentation in deep sleep duration positively corresponds to an overall enhancement in sleep quality, evidenced by extended total sleep duration, increased energy expenditure, improved sleep score, and heightened oxygen saturation during sleep. Conversely, notable negative correlations, especially with night waking frequency, indicate potential disruptions in sleep patterns. The robust negative correlation between night waking frequency and the duration of deep sleep, as well as energy expenditure during sleep, implies that an escalation in nocturnal waking incidents corresponds negatively with both deep sleep duration and energy expended during sleep. This underscores the substantial impact of nocturnal disturbances on the intricate architecture of sleep.
Furthermore, different exercise modalities exhibit distinct impacts on sleep quality. Aerobic exercise significantly impacts sleep quality by notably enhancing blood oxygen saturation, a key factor contributing to extended total sleep duration, increased energy expenditure during sleep, improved sleep score, and heightened oxygen saturation during sleep.On the other hand, resistance training modulates sleep quality by regulating energy expenditure, resulting in increased duration of deep sleep and an overall improvement in sleep quality. These distinct effects empower individuals to tailor their approach based on specific objectives and personal wellness goals.
Figure 3.
Radar chart of the effects of different modes of exercise on sleep intervention.
Figure 3.
Radar chart of the effects of different modes of exercise on sleep intervention.
Figure 4.
Heat map of Spearman correlation coefficient of sleep architecture.
Figure 4.
Heat map of Spearman correlation coefficient of sleep architecture.
Discussion
The present study aimed to evaluate the efficacy of an eight-week exercise intervention, incorporating both aerobic and resistance exercises, on enhancing sleep quality among university students. The findings of our study indicated that both forms of exercise led to substantial improvements in sleep quality, with aerobic exercise promoting cardiovascular wellness and resistance training augmenting nocturnal sleep efficiency, ultimately contributing to enhanced daytime performance and emotional equilibrium.
In recent years, the prevalence of depression among university students has been on the rise, largely due to social development and lifestyle changes9. As a result, exercise therapy has gained acceptance among younger populations as an effective intervention10. The results from the PSQI scale, reflecting subjective sleep quality, indicate a significant improvement in the experimental group after 8 weeks of exercise intervention. Aerobic and resistance exercises may represent effective non-pharmacological approaches to improving sleep quality. The energy expenditure from exercise interventions induces moderate muscle fatigue, which directly influences sleep efficiency and sleep quality factors. Aerobic exercise enhances cardiovascular function and physical health in university students, effectively alleviating sleep disturbances caused by respiratory and physical discomfort. Resistance training improves nocturnal sleep efficiency by allowing the brain to adequately replenish and restore energy reserves depleted during wakefulness. This, in turn, enhances daytime work and study efficiency, stabilizes emotional states, and reduces daytime functional disturbances.
Polysomnography (PSG) is widely acknowledged as the foremost method for objectively assessing sleep data and diagnosing various sleep disorders11.Despite its recognition, PSG has inherent limitations, requiring execution in designated outpatient facilities with costly and intricate instruments12. Subjects often experience discomfort, particularly during electrode installation, introducing confounding factors affecting the authenticity of sleep monitoring13.Subjects often experience discomfort, particularly during electrode installation, introducing confounding factors affecting the authenticity of sleep monitoring14.Wearable devices, including Huawei's Band B3, have shown commendable accuracy, with an average percentage error of approximately 0.10% across metrics such as heart rate, walking steps, exercise distance, and sleep duration15.Using Huawei Band for sleep monitoring in our study provided accurate and convenient data collection, addressing the complexity associated with traditional methods16. Additionally, it facilitated effective monitoring during exercise interventions, ensuring participants' safety throughout physical activity17.In our study, we used the Huawei Band smart wearable device to accurately monitor participants' sleep stages, duration, and exercise parameters. Its high accuracy and ease of use facilitated reliable and comprehensive monitoring, enabling rigorous analysis of exercise interventions' effects on sleep quality.This approach highlights the benefits of using wearable devices like Huawei Band for comprehensive and practical sleep research.
Following the implementation of the exercise intervention, our results demonstrated notable decreases in both the overall Pittsburgh Sleep Quality Index (PSQI) scores and the scores of individual sleep quality factors across both the aerobic and resistance exercise groups. Although both exercise modalities exhibited favorable impacts on sleep, they presented distinct patterns of improvement across various sleep parameters. While diverse combined exercise protocols contributed to lowered total PSQI scores and individual factor scores, their effects varied.Sleep latency, which indicates the challenge in initiating sleep, was reduced in the resistance exercise group18. This may be attributed to the relatively higher exercise load in the resistance group, where prolonged resistance training induced physical fatigue, thereby facilitating shorter sleep onset19. Daytime dysfunction reflects participants' daytime fatigue and their ability to concentrate during study or work.Our findings revealed that the aerobic exercise group experienced a decrease in daytime dysfunction scores. This enhancement can be attributed to the integration of aerobic and mind-body exercises in the intervention, which effectively managed participants' negative emotions and mental stress, balanced the autonomic nervous system function, and aided sleep initiation20. These findings are consistent with our prior observations. Sleep duration, representing participants' subjective sense of sleep length, exhibited a significant reduction in scores in the resistance group21. This could be because resistance exercise decreased the frequency and duration of nighttime awakenings, thereby augmenting effective sleep time and leading participants to perceive an extension of their sleep duration18.
Our study delved into the contrasting effects of aerobic exercise versus resistance training on sleep quality among college students. The results demonstrate that the aerobic exercise group significantly extended sleep duration and increased blood oxygen saturation during sleep, which may be attributed to aerobic exercise's enhancement of cardiorespiratory efficiency and potentiation of parasympathetic nervous system activity during restful hours.Further analysis revealed that the aerobic exercise group exhibited significantly longer sleep duration and higher blood oxygen levels during sleep compared to the resistance exercise group, while the resistance group demonstrated higher REM levels and greater energy expenditure during sleep. These differences may be related to the regulatory effects of different exercise types. Studies have shown that sleep quality improves with increased parasympathetic nervous system activity. Regular aerobic exercise can significantly reduce catecholamine concentrations in the body, enhance parasympathetic activity during nighttime rest, and shift autonomic nervous system regulation toward parasympathetic dominance22,23. Consistent physical activity helps establish a balanced exercise-rest lifestyle, reducing the negative effects caused by lifestyle disruptions13,24.Resistance training involves the contraction of skeletal muscles, either through single-joint or multi-joint movements, leading to increased muscle volume and a greater number of muscle fibers25. During skeletal muscle contraction, a large amount of cytokine IL-6 is released, which plays a role in regulating the immune system. Relevant studies have also confirmed a significant interaction between the immune system and sleep. Inflammatory cytokines, such as IL-1β and TNF-α, released by the immune system, have been proven to be key substances involved in the regulation of sleep26. These findings align with intervention studies conducted on university students and other populations, confirming that combined exercise interventions can objectively improve the sleep quality of students with sleep disorders7,27,28.
Nonetheless, this study is subject to certain limitations. Firstly, the limited sample size may restrict the broad applicability of our findings. To confirm these observations in various populations, future research should aim to increase sample sizes. Secondly, while we utilized smart wearables such as fitness trackers for sleep and exercise monitoring, their precision and dependability, especially in intricate sleep environments, require additional verification. Consequently, incorporating multiple sleep assessment methods (e.g., polysomnography, PSG) would enhance the study's robustness and reliability.
To address these limitations and advance the field, we propose the following recommendations: First, expand sample sizes and ensure participant diversity to enhance the representativeness and universality of research outcomes. Second, employ multiple technological approaches to comprehensively assess sleep quality, thereby improving monitoring precision. Third, investigate the long-term impacts and physiological mechanisms underlying distinct exercise modalities on sleep quality, fostering the development of more tailored and scientifically grounded exercise interventions. Lastly, address individual variability by crafting personalized exercise prescriptions, tailoring them to meet the specific needs of college students and optimizing the effectiveness and relevance of intervention strategies.
Conclusion
In conclusion, our study elucidates the intricate interplay between exercise modalities and sleep quality among college students. Aerobic exercise enhances respiratory and circulatory efficiency, improving sleep duration and quality, while resistance training positively impacts deep sleep duration. Both interventions exhibit distinct yet beneficial effects on various sleep parameters, emphasizing the importance of personalized exercise prescriptions. The findings underscore exercise as a non-pharmacological intervention for enhancing sleep outcomes. As college students navigate unique challenges affecting sleep, tailored exercise regimens offer a holistic approach to promote overall well-being. Further research should explore individualized strategies to optimize sleep quality and address specific needs within this demographic.
Data availability Statement
All data supporting this study’s findings are available from the corresponding author upon reasonable request.
References
- Liu, K. Y. et al. Noradrenergic-dependent functions are associated with age-related locus coeruleus signal intensity differences. Nat Commun 11, 1712 (2020). [CrossRef]
- Melvin, S., Jamal, A., Hill, K., Wang, W. & Young, S. D. Identifying Sleep-Deprived Authors of Tweets: Prospective Study. JMIR Ment Health 6, e13076 (2019). [CrossRef]
- Xu, Y., Ou, Q., Cheng, Y., Lao, M. & Pei, G. Comparative study of a wearable intelligent sleep monitor and polysomnography monitor for the diagnosis of obstructive sleep apnea. Sleep Breath 27, 205–212 (2023). [CrossRef]
- Bai, Y. et al. Comprehensive comparison of Apple Watch and Fitbit monitors in a free-living setting. PLoS ONE 16, e0251975 (2021). [CrossRef]
- Wang, F. & Bíró, É. Determinants of sleep quality in college students: A literature review. Explore (NY) 17, 170–177 (2021). [CrossRef]
- Becker, S. P. et al. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4, 174–181 (2018). [CrossRef]
- Wendt, A., Flores, T. R., Silva, I. C. M. & Wehrmeister, F. C. Association of physical activity with sleep health: A systematic review. Revista Brasileira de Atividade Física & Saúde 23, 1–26 (2018). [CrossRef]
- Xintarakou, A., Sousonis, V., Asvestas, D., Vardas, P. E. & Tzeis, S. Remote Cardiac Rhythm Monitoring in the Era of Smart Wearables: Present Assets and Future Perspectives. Front Cardiovasc Med 9, 853614 (2022). [CrossRef]
- Veldi, M., Aluoja, A. & Vasar, V. Sleep quality and more common sleep-related problems in medical students. Sleep Med 6, 269–275 (2005). [CrossRef]
- Memon, A. R. et al. Sleep and physical activity in university students: A systematic review and meta-analysis. Sleep Med Rev 58, 101482 (2021). [CrossRef]
- Aristimunha, B., Bayerlein, A. J., Cardoso, M. J., Pinaya, W. H. L. & De Camargo, R. Y. Sleep-Energy: An Energy Optimization Method to Sleep Stage Scoring. IEEE Access 11, 34595–34602 (2023). [CrossRef]
- Depner, C. M. et al. Wearable technologies for developing sleep and circadian biomarkers: a summary of workshop discussions. Sleep 43, zsz254 (2020). [CrossRef]
- Laursen, L., Inturi, R., Østergaard, S. & Jemth, P. Determinants of affinity, specificity, and phase separation in a supramodule from Post-synaptic density protein 95. iScience 25, 105069 (2022). [CrossRef]
- Haba-Rubio, J. et al. Objective sleep structure and cardiovascular risk factors in the general population: the HypnoLaus Study. Sleep 38, 391–400 (2015). [CrossRef]
- An, B. W. et al. Smart sensor systems for wearable electronic devices. Polymers 9, (2017). [CrossRef]
- Xie, J. et al. Evaluating the Validity of Current Mainstream Wearable Devices in Fitness Tracking Under Various Physical Activities: Comparative Study. JMIR Mhealth Uhealth 6, e94 (2018). [CrossRef]
- Zr, G. et al. A catalog of validity indices for step counting wearable technologies during treadmill walking: the CADENCE-Kids study. The international journal of behavioral nutrition and physical activity 18, (2021).
- Wang, S. et al. Prospective association between 24-hour movement behaviors and mental health among overweight/obese college students: a compositional data analysis approach. Front Public Health 11, 1203840 (2023). [CrossRef]
- Mohammadieh, A., Sutherland, K. & Cistulli, P. A. Sleep disordered breathing: management update. Intern Med J 47, 1241–1247 (2017). [CrossRef]
- Yang, C.-M., Wu, C.-H., Hsieh, M.-H., Liu, M.-H. & Lu, F.-H. Coping with sleep disturbances among young adults: a survey of first-year college students in Taiwan. Behav Med 29, 133–138 (2003). [CrossRef]
- Mohammadi, S. et al. Association between Mediterranean dietary pattern with sleep duration, sleep quality and brain derived neurotrophic factor (BDNF) in Iranian adults. Sci Rep 13, 13493 (2023). [CrossRef]
- Rastelli, M., Cani, P. D. & Knauf, C. The Gut Microbiome Influences Host Endocrine Functions. Endocr Rev 40, 1271–1284 (2019). [CrossRef]
- Deng, J. et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res 301, 113863 (2021). [CrossRef]
- Feng, G. et al. Control of Sleep Onset by Shal/Kv4 Channels in Drosophila Circadian Neurons. J Neurosci 38, 9059–9071 (2018).
- Harris, T. et al. A primary care nurse-delivered walking intervention in older adults: PACE (pedometer accelerometer consultation evaluation)-Lift cluster randomised controlled trial. PLoS Med 12, e1001783 (2015). [CrossRef]
- Gupta, L., Morgan, K. & Gilchrist, S. Does Elite Sport Degrade Sleep Quality? A Systematic Review. Sports Med 47, 1317–1333 (2017). [CrossRef]
- Reid, K. J. et al. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med 11, 934–940 (2010). [CrossRef]
- M, K., Sw, C., Tb, W., Cs, R. & Jw, K. Associations Between Systemic Inflammatory Markers Based on Blood Cells and Polysomnographic Factors in Obstructive Sleep Apnea. Clinical and experimental otorhinolaryngology 16, (2023).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).