1. Introduction
Tuberculosis (TB) and lung cancer (LC) are among the most pressing medical and social challenges worldwide. These issues arise from the widespread prevalence of these diseases, high mortality rates, and patient disability.
TB is an infection caused by the aerobic non-motile bacteria
Mycobacterium tuberculosis (
Mtb) which primarily affects the lungs but can also impact other organs and systems. The WHO estimates that in 2022, 10.6 million people worldwide fell ill with TB, of whom 0.41 million developed multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB), and 1.3 million died. Before the emergence of COVID-19, TB was the leading cause of death from a single infectious agent [
1].
Mtb can effectively evade the host's immune system, persisting intracellularly (in macrophages) and extracellularly (inside granulomas), allowing the infection to remain latent for extended periods [
2]. Only one in ten infected adults will develop active TB during their lifetime. Estimates suggest that one-quarter to one-third of the global population is infected with Mtb [1, 3]. TB diagnosis involves verification in patients with clinical and radiological signs, but negative results from diagnostic tests (microscopy, culture, PCR tests) do not rule out closed TB; they only indicate a lack of bacterial excretion [
3]. Patients without a confirmed diagnosis undergoing anti-TB treatment must accept the risks of toxic side effects from medications (primarily liver damage).
LC is one of the most common cancers and the leading cause of death from malignant neoplasms. In 2020, 2.21 million new cases of LC were registered globally, with 1.80 million deaths [
4]. The primary reason for the high mortality is late detection, as more than 70% of tumours are found at stages III and IV when therapeutic options are limited. Consequently, the average five-year survival rate after diagnosis of LC is only 10–20% in most countries [
5]. The main reasons for late detection are the asymptomatic course of the disease in its early stages, nonspecific symptoms, and rapid tumour progression. LC diagnosis requires a biopsy of the suspected tissue and histological examination for cancer cells. Existing methods of collecting biomaterial (tracheobronchoscopy, bronchoscopic lavage, thoracoscopy, transbronchial biopsy, pleural puncture, needle biopsy, etc.) are invasive and not always feasible. For some patients, morphological verification of the diagnosis is impossible due to severe comorbidities, age, or refusal of invasive procedures.
For both diseases, timely diagnosis is critical for successful treatment. However, due to the high prevalence of TB and the similar clinical and radiological presentation of diseases, many LC patients initially receive anti-TB treatment, resulting in diagnostic delays, tumour progression, and drug toxicity [
6]. Conversely, TB can be misdiagnosed as LC [6-8]. Cases of concomitant TB and LC are particularly problematic due to delayed diagnosis of one of the diseases and therapeutic limitations [7, 9].
These challenges in early and differential diagnosis of TB and LC have led to the search for new minimally invasive methods. MicroRNAs (miRNAs) are being explored as promising biomarkers for disease diagnosis. miRNAs are small single-stranded, non-coding RNAs that function as negative regulators of genes. Their biological significance, biogenesis, and mechanisms of action have been well described in previous works [10, 11].
miRNAs play an important role in
Mtb evasion of the host's immune system by influencing macrophage metabolism, suppressing inflammatory responses, and regulating apoptosis and autophagy, allowing the infection to persist in the body [
12]. Studies have demonstrated the potential of circulating miRNAs for diagnosing active TB [13-18], differentiating TB from COPD, pneumonia, and lung cancer [
13], distinguishing between latent and active forms of TB [14, 15], identifying drug-resistant TB [
19], and assessing treatment response [15, 20, 21].
The role of miRNAs in cancer development is well-established. miRNAs are involved in the onset, progression, and metastasis of malignant tumours and are therefore considered as promising cancer biomarkers [22, 23]. They enter the bloodstream directly from primary or metastatic tumours via active secretion, apoptosis, or necrosis, so changes in circulating miRNA levels can reflect the underlying pathological process [
24]. Many miRNAs have been recommended as plasma/serum diagnostic and prognostic markers for LC [25-34]. A significant issue with such studies is the low reproducibility of results across different investigations, possibly to population differences, lifestyle factors, and variations in collection, extraction, and quantification methodologies. Some studies indicate that the pathogenesis of cancer may have ethnic-specific features [35, 36], which also applies to the applicability of circulating miRNAs as markers [37, 38].
To our knowledge, no miRNA marker has yet been implemented in clinical practice, though many of them are currently undergoing prospective clinical trials targeted to confirm their utility for early LC detection (descriptions of clinical trials are available on ClinicalTrials.gov) [
39].
Our study aimed to evaluate the potential of circulating plasma miRNAs as biomarkers for the differential diagnosis of TB and LC in the population of Kazakhstan. We conducted a comparative quantitative analysis of plasma miRNA levels among three groups: LC patients (N = 64), TB patients (N = 35), and healthy controls (N = 39). In the first exploratory phase, we tested 188 candidate miRNAs on five pooled plasma samples and selected 14 promising candidates. In the second phase, we validated them using a total sample of individual plasma specimens.
2. Materials and Methods
2.1. Subjects
Venous blood sampling for the study was conducted at three medical institutions. Blood samples from 82 primary patients with histologically confirmed LC (LC patients) and 1 patient with laboratory-confirmed TB were collected at the Kazakh Research Institute of Oncology and Radiology, Almaty, Kazakhstan, before the start of therapy, from July 2022 to June 2023. Blood samples from 40 patients with laboratory-confirmed TB (TB patients) were collected at the National Scientific Center of Phthisiopulmonology, Almaty, Kazakhstan, before the start of therapy, from September to December 2022. Blood samples from 41 healthy donors (Controls) were collected at the Almaty Multidisciplinary Clinical Hospital between January and March 2023.
The study was approved by the local ethics committee of the Aitkhozhin Institute of Molecular Biology and Biochemistry.
2.2. Plasma preparation and RNA isolation
Before plasma extraction, the blood was stored for no more than 2 h at 4°C. After gentle mixing, the blood samples were centrifuged at 1000g for 15 min at 4 °C. The supernatant was then transferred to a new tube and subjected to a second centrifugation at 2500g for 15 min at 4 °C. The resultant plasma was divided into 100 μl aliquots and stored at -70 °C until further use.
Total RNA was isolated from 100 μl of plasma using a commercial MagMAX mirVana Total RNA Isolation Kit (Applied Biosystems, USA) according to the manufacturer’s protocol. Before RNA isolation, 2 fmol of the exogenous spike-in control ath-miR-159a was added to each sample.
2.4. Obtaining cDNA and quantitative PCR
Immediately after RNA isolation, cDNA synthesis and quantitative PCR reactions were performed. cDNA was synthesized using the TaqMan Advanced miRNA cDNA Synthesis Kit (Applied Biosystems) according to the manufacturer’s protocol. Quantitative PCR was carried out using specific primers and hydrolysis probes from the TaqMan Advanced miRNA Assays kit (Applied Biosystems) and the TaqMan Fast Advanced Master Mix reagent (Applied Biosystems) under the conditions recommended by the manufacturer on the StepOnePlus Real-Time PCR System (Applied Biosystems).
Primary data processing was performed using StepOnePlus 2.2.2 and ExpressionSuite v1.3 software. Relative quantification was conducted using the comparative Ct (ΔΔCt) method with modifications described by Königshoff et al., 2009 [
40]. Relative transcript abundance is expressed in ΔCt values (ΔCt = Ct
reference − Ct
target). The exogenous spike-in control ath-miR-159a was used as the reference. The ΔΔCt value (ΔΔCt = ΔCt
case − ΔCt
control) was interpreted as log
2 fold change (log
2FC).
2.5. Study design
The study consisted of two stages: exploratory miRNA profiling and validation. At the first exploratory stage, using TaqMan Advanced miRNA Human Serum/Plasma 96-well Plates (Applied Biosystems), we tested 188 miRNAs on five pooled plasma samples from the following groups: 10 patients with adenocarcinoma (AC), 10 patients with squamous cell carcinoma (SCC), 9 patients with small cell carcinoma (SCLC), 10 TB patients, and 10 healthy controls. The selection of promising candidate miRNAs was carried out in three stages: 1) selection based on amplification quality (amplification score > 0.6); 2) selection based on the magnitude of fold changes between groups (FC > 3); 3) selection according to the criteria of required classifiers. The amplification score was derived from the ExpressionSuite software.
To validate the results of the miRNA profiling, the selected miRNAs were tested on individual plasma samples from 68 LC patients, 38 TB patients, and 41 healthy controls.
2.6. Statistical analysis
Most statistical calculations were performed using Jamovi v2.2.5.0 software [
41]. To compare the characteristics of the studied groups, we applied the Student's t-test for quantitative data and Pearson’s chi-squared test (χ2-test) for nominal data. The statistical significance of differences in miRNA levels between the groups was assessed using the Mann-Whitney
U test.
P-values <0.05 were considered statistically significant. For multiple comparisons,
p-values were adjusted using the FDR online calculator [
42]. The characteristics of the markers were evaluated based on receiver operating characteristic (ROC) analysis, calculated using the Web tool for ROC analysis [
43] and the online ROC calculator [
44]. The optimal cut-off point was determined using Youden’s index method. Evaluation of classifiers by interpretation of the area under the ROC curve (AUC) was conducted as described by Muller et al., 2005 [
45]. Heatmap diagrams and boxplots were generated using the SRplot online platform [
46]. Venn diagrams were generated using the online tool [
47].
3. Results
3.1. Characteristics of the compared groups
The characteristics of the compared groups are presented in
Table 1. In all studied groups, the vast majority of individuals were Kazakhs, with other ethnic groups including Uyghurs, Russians, Tatars, Mari, and Dungans.
The exploratory set consisted of five groups: 10 AC patients, 10 SCC patients, 9 SCLC patients, 10 TB patients, and 10 healthy controls. The TB patients and controls did not differ in age, gender distribution, or number of smokers. The three LC patient groups did not differ significantly from each other but differed significantly in age from the TB patients (p = 0.011, 0.004, and 0.022, respectively) and from the controls (p = 0.001, 1.2×10−4, and 0.007, respectively). Males predominated in all groups. The proportion of smokers was significantly higher among the LC patients.
The validation set included 68 LC patients, 38 TB patients, and 41 healthy controls. The LC patients and controls did not differ significantly in age, gender distribution, or the number of smokers; however, both groups differed significantly from the TB patients in these parameters. On average, the TB patients were 20 years younger than the other two groups (p = 5.0×10⁻¹³ and 2.0×10⁻¹⁰, respectively). The gender ratio among TB patients was approximately equal, whereas there were significantly more males in the LC and control groups (p = 0.014 and 0.010, respectively). There were significantly fewer smokers among the TB patients compared to the controls, and especially compared to the LC patients (p = 0.012 and 1.4×10⁻⁴, respectively). The proportion of patients with drug-resistant TB was 26% of all TB patients, consistent with official statistical data for the Republic of Kazakhstan. Most LC patients (62%) had tumours at advanced stages (III or IV), which aligns with literature data indicating predominantly late detection of LC. The tumour-type distribution roughly matched the expected frequencies.
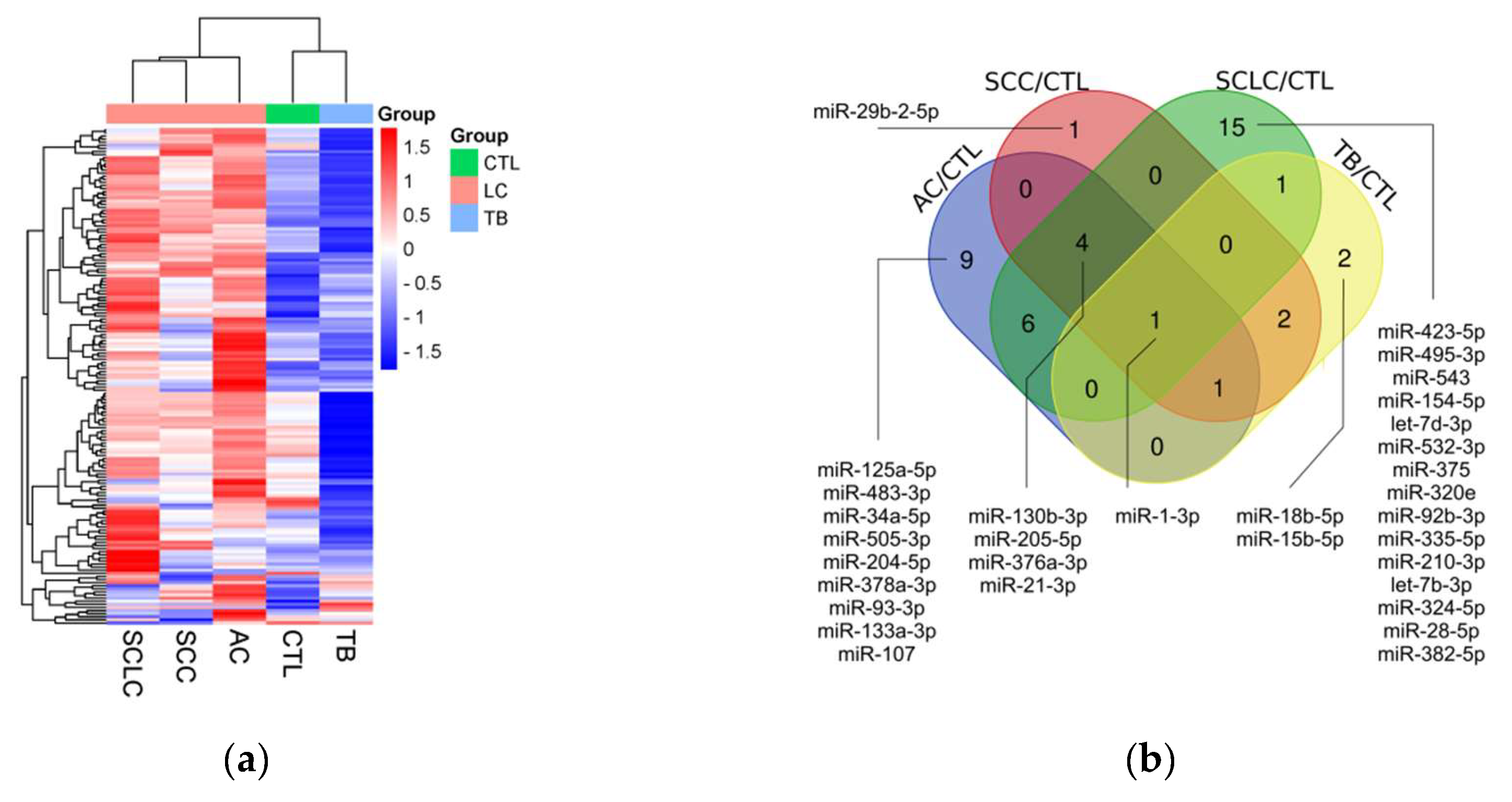
3.2. miRNA profiling
miRNA profiling results are shown in figure 1. Briefly, we compared the levels of 188 miRNAs in 5 pooled samples from 10 AC patients, 10 SCC patients, 9 SCLC patients, 10 TB patients, and 10 healthy controls. First, we filtered out all miRNAs without amplification or with Ct above the threshold of 35. Second, we excluded miRNAs with low amplification quality, using an Amplification score of 0.6 as the threshold. The remaining 161 miRNAs were included in the selection process (fig 1a). The groups were compared, and miRNAs with a difference of 3-fold or more between the groups were selected. From these 70 miRNAs, those potentially useful for diagnosing LC and TB (fig 1b), for the differential diagnosis of LC and TB (fig 1c), as well as for the differential diagnosis of SCLC and NSCLC (fig 1d), were chosen. In the end, 14 miRNAs were selected (fig 1e). The list could have been broader, but the number of available slots was limited.
3.3. Validation
The results of the exploratory stage were validated on individual samples from 68 LC patients, 38 TB patients, 4 patients with suspected LC, 9 patients with suspected TB, and 41 healthy controls (
Supplementary Table S1). Comparative quantitative statistics between the three groups are presented in
Table 2. A comparison of the levels of the studied miRNAs between the groups is shown in
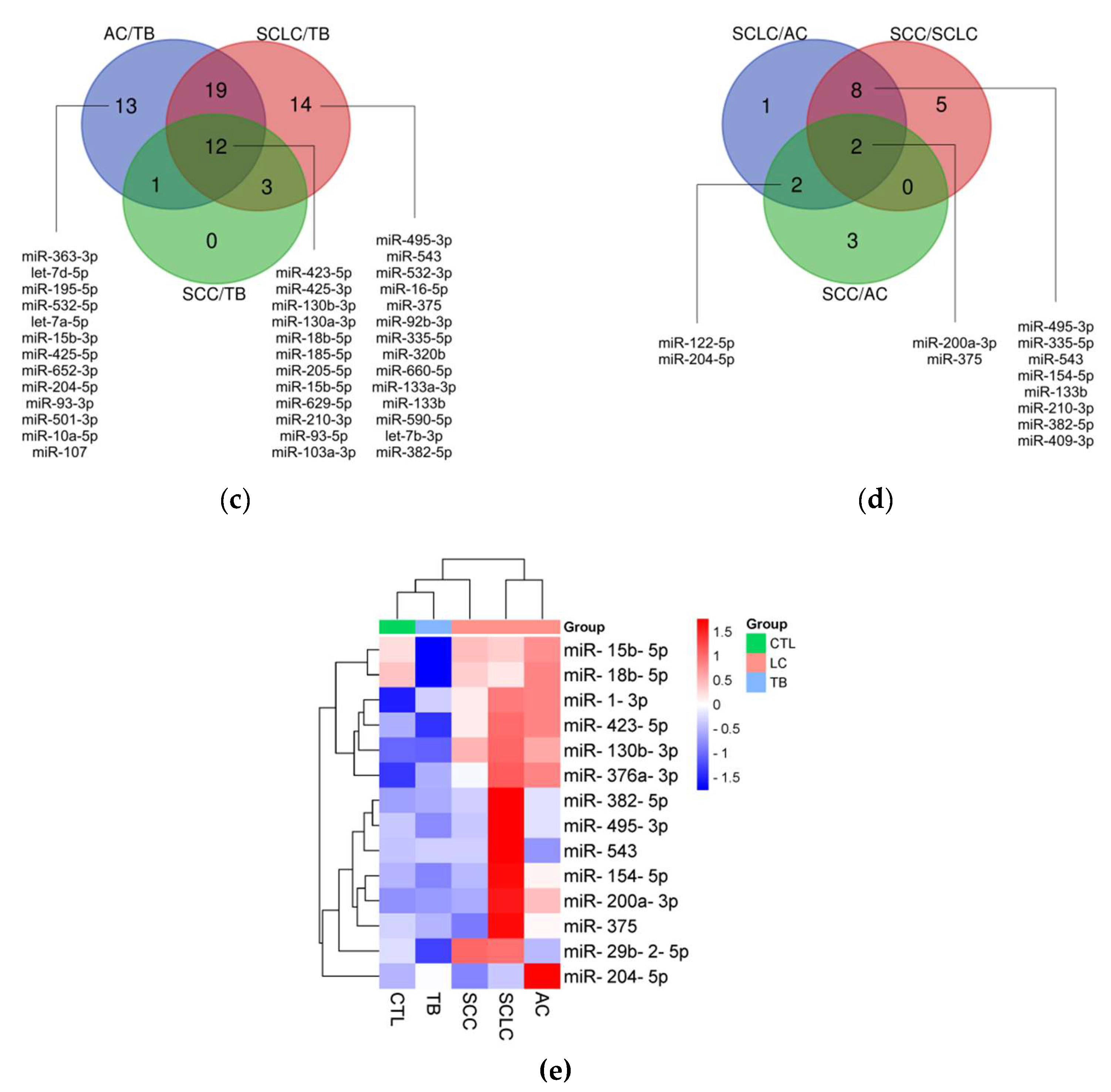
Figure 2.
The levels of miR-130b-3p, miR-1-3p, miR-423-5p, miR-200a-3p, miR-15b-5p, miR-18b-5p, miR-376a-3p, miR-375-3p, miR-154-5p, miR-29b-2-5p, miR-382-5p, and miR-495-3p were significantly elevated in the plasma of LC patients compared to controls, with log2FC ranging from 0.9 for miR-495-3p to 3.2 for miR-15b-5p. Ten out of the twelve significant differences remained significant after adjustment for multiple testing. The levels of miR-543 and miR-204-5p showed no significant changes in LC patients compared to controls.
The level of miR-376a-3p was significantly elevated, and the level of miR-15b-5p was significantly reduced in TB patients compared to controls; however, log2FC was small in both cases. Both differences remained significant after adjustment for multiple testing. The levels of the remaining 12 miRNAs showed no significant changes in TB patients compared to controls.
The levels of miR-130b-3p, miR-423-5p, miR-15b-5p, miR-18b-5p, miR-1-3p, miR-200a-3p, miR-29b-2-5p, miR-154-5p, miR-375-3p, miR-495-3p, miR-382-5p, miR-376a-3p, and miR-543 were significantly elevated in LC patients compared to TB patients, with log2FC ranging from 0.76 for miR-376a-3p to 4.31 for miR-15b-5p. Twelve out of the thirteen significant differences remained significant after adjustment for multiple testing. The level of miR-204-5p showed no significant changes between LC and TB patients.
Considering the potential use of miRNA markers in the early diagnosis of LC, we examined the levels of our miRNAs in stage I LC patients. All miRNAs that were significantly elevated in the overall group of LC patients were also significantly elevated in stage I LC patients when compared to TB patients and healthy controls (
Supplementary Table S2).
In addition, 22 significant differences in miRNA levels were identified between groups with different clinicopathological parameters; however, after adjustment for multiple testing, only 3 of them remained significant (
Supplementary Table S3). The levels of miR-200a-3p and miR-375-3p were significantly elevated in AC patients compared to SCC patients. The levels of miR-18b-5p, miR-154-5p, miR-375-3p, and miR-29b-2-5p were significantly elevated in SCLC patients compared to AC patients. The levels of miR-18b-5p, miR-375-3p, miR-154-5p, miR-130b-3p, miR-200a-3p, and miR-495-3p were significantly elevated in SCLC patients compared to SCC patients. The levels of miR-18b-5p, miR-375-3p, miR-154-5p, miR-130b-3p, miR-29b-2-5p, miR-495-3p, and miR-15b-5p were significantly elevated in SCLC patients compared to NCLC patients. The level of miR-375-3p was significantly elevated in LC patients with metastasis compared to those without metastasis. The level of miR-204-5p was significantly elevated in TB patients who are smokers compared to non-smokers. The level of miR-423-5p was significantly elevated in healthy smokers compared to healthy non-smokers. There were no significant differences in miRNA levels between genders in the three groups, or between patients with drug-sensitive and drug-resistant TB.
To assess the impact of age on differences in miRNA levels between groups, we conducted regression analysis and partial correlation analysis. Both methods indicated that age did not affect the observed differences in the levels of most miRNAs (
Supplementary Table S4).
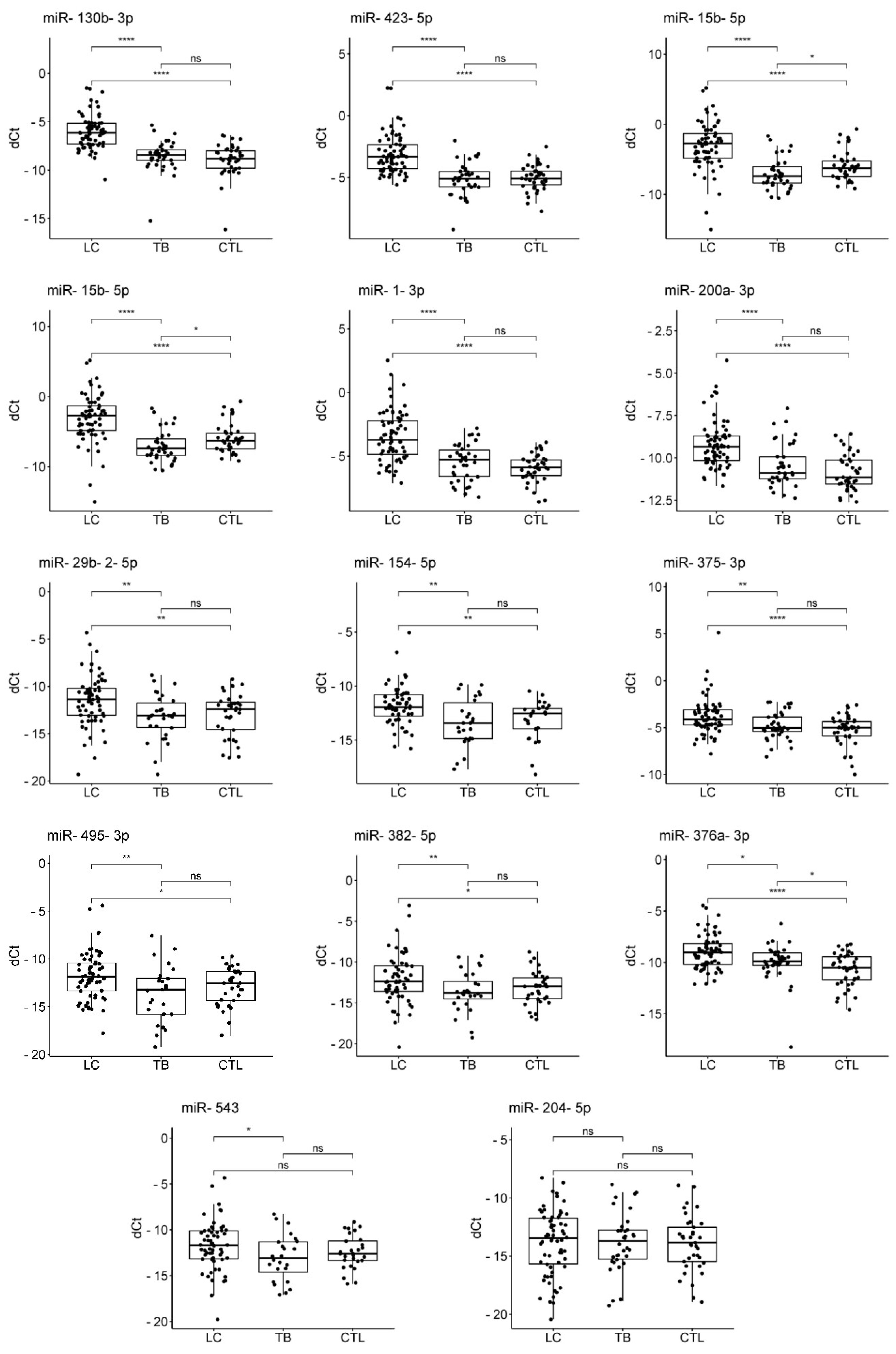
3.4. ROC-analysis
To assess the diagnostic abilities of miRNAs that showed significant differences in levels between groups, we conducted ROC analysis. The evaluation of the discriminative ability of potential markers by interpretation of AUC was conducted as described by Muller et al., 2005 [
46]: excellent discrimination, AUC of ⩾0.90; good discrimination, 0.80 ⩽ AUC < 0.90; fair discrimination, 0.70 ⩽ AUC < 0.80; and poor discrimination, AUC of <0.70.
We tested six potential applications of the miRNA marker. The results of the ROC analysis are presented in
Supplementary Table S5. The analysis showed that miRNAs have a good ability to discriminate between LC patients and healthy individuals (
Figure 1a), between LC and TB patients (
Figure 1c), and between SCLC and non-small cell LC (NSCLC) patients (
Figure 1e); a fair ability to discriminate between LC patients with and without metastasis (
Figure 1d); and a poor ability to discriminate between TB patients and healthy individuals (
Figure 1b), and between AC and SCC patients (
Figure 1f).
Additionally, miRNAs exhibit good ability to discriminate between stage I LC patients and healthy controls, as well as between stage I LC patients and TB patients. These results suggest that miRNAs have potential for early LC diagnosis and for differential diagnosis between early LC and TB.
4. Discussion
TB and LC remain significant health issues worldwide, particularly in Kazakhstan. The challenges in diagnosing these and other pulmonary diseases with similar clinical and radiological presentations underscore the need for new minimally invasive methods for early and differential diagnosis. In our study, we evaluated the potential of plasma-circulating miRNAs as biomarkers for the early and differential diagnosis of TB and LC in the Kazakhstani population. To achieve this, we examined and validated the plasma miRNA profiles of LC and TB patients in comparison with each other and with healthy controls. Our findings indicate that plasma miRNAs hold a high potential for diagnosing LC (including early detection) and for distinguishing between LC and TB. Contrary to previous reports proposing miRNAs as biomarkers for TB [13-21], our study did not find significant miRNAs with diagnostic utility specifically for TB.
The greatest potential for the differential diagnosis of LC and TB was shown by miR-130b-3p and miR-423-5p. A literature search indicates that these two miRNAs play a significant role in the pathogenesis of LC. Chen et al. [
48] showed that miR-130b-3p promotes immune escape and metastasis in NSCLC by down-regulating the tumour suppressor STK11. Guo et al. [
49] demonstrated that miR-130b-3p is overexpressed in NSCLC and that miR-130b-3p, conveyed through mesenchymal stem cell-derived extracellular vesicles, advances LC progression by inhibiting the FOXO3/NFE2L2/TXNRD1 axis. Studies have shown that increased miR-130b-3p expression enhances angiogenesis and tumour progression in various cancers [50, 51, 52]. Elevated miR-130b-3p expression has been observed in oral cancer [
51], gastric cancer [
53], liver cancer [
50], colorectal cancer [
54], bladder cancer [
55], and prostate cancer [
56]. These studies align with our findings, reinforcing the role of miR-130b-3p as a relevant biomarker and a potential therapeutic target.
In contrast to our findings and the studies mentioned above, Lv et al. [
57] report a protective role of miR-130b-3p in NSCLC. They found that miR-130b-3p inhibits DEPDC1 expression, which, via the TGF-β signalling pathway, leads to reduced proliferation, migration, and apoptosis suppression in cancer cells; additionally, a decrease in serum exosomal miR-130b-3p was noted in NSCLC patients. In our study, we observed the opposite effect—a more than six-fold increase in plasma miR-130b-3p levels compared to the control group.
There are fewer studies on miR-423-5p, but sufficient evidence suggests its significant role in carcinogenesis. Huang et al. [
58] identified it as a promoter of lung AC through inhibition of CADM1, facilitating cell proliferation and invasion. Wang et al. [
59] demonstrated that miR-423-5p accelerates NSCLC progression by targeting SLIT2. Sun et al. [
60] found that elevated miR-423-5p expression in lung AC contributes to brain metastasis by directly inhibiting MTSS1. In contrast to these studies, which support our findings, the work of Yu et al. [
61] and Li et al. [
62] reports a protective role of miR-423-5p in LC through inhibition of the oncogenes CEACAM1 and MYBL2.
Particularly relevant to our study is the work by Kang et al. [
63], which examines both miR-130b-3p and miR-423-5p in the context of TB and LC interaction. The authors demonstrated that TB promotes the proliferation of cancer cells through the influence of exosomal miR-130b-3p and miR-423-5p, which enhance the expression of Cyclin D1 and p65. The study reports a high concentration of these miRNAs in exosomes from pleural effusion; however, blood plasma was not examined. In another study, Tu et al. [
16] reported increased serum levels of miR-423-5p in TB patients. The authors found that miR-423-5p is linked to TB through its inhibitory effect on autophagosome-lysosome fusion in macrophages – a crucial immune defence process – by directly targeting VPS33A, which may facilitate TB infection. According to our data, the concentration of miR-130b-3p and miR-423-5p in the blood plasma of TB patients is not elevated, in contrast to LC patients, which enables differentiation between the two conditions.
In addition to miR-130b-3p and miR-423-5p, our study identified other miRNAs with valuable diagnostic applications. Compared to these two, miR-15b-5p demonstrated lower specificity for distinguishing LC from healthy controls, while miR-1-3p was less specific for differentiating LC from TB. MiR-18b-5p displayed strong discriminatory power in differentiating SCLC from NSCLC, which is important for selecting appropriate treatment strategies.
Notably, the miRNAs we propose are valuable for early and differential diagnosis of early LC, as they retained strong discriminatory power when comparing only stage I LC patients to healthy controls and TB patients.
Several studies have explored miRNAs as differential diagnostic markers for some lung diseases, but such research remains sparse. Previously, miRNA biomarkers were investigated for distinguishing TB from pneumonia, LC and COPD [
13], LC from COPD [25, 64], LC from bronchiectasis [
25], LC from pneumonia [25, 65], and LC from benign lung lesions [
34]. To our knowledge, only a single study by Zhang et al. [
13] examined miRNAs specifically for differentiating TB from LC. The scarcity of such studies emphasizes the importance of our findings, which add valuable data to the limited research on miRNA-based differential diagnostics in pulmonary diseases.
The commercial kit we used in the exploratory phase, consisting of two 96-well plates, is specifically optimized for profiling 188 miRNAs in blood serum/plasma. We suggest that this design allowed for broad coverage of circulating miRNAs, facilitating the identification of relevant biomarkers.
Although our findings are supported by existing literature, reproducibility in miRNA studies remains a challenge. This variability may arise from biological factors, such as inter-population differences, or from methodological inconsistencies that are often unreported. Standardizing protocols could address many of these discrepancies. However, population-specific factors, including genetic background and environmental exposures, likely contribute to variability in miRNA expression, underscoring the need for biomarker validation in specific populations.
Further studies are necessary to confirm the clinical applicability of our results. Future research should expand the sample size, increase the range of different pulmonary diseases and, where appropriate, explore additional confounding variables. Additionally, longitudinal studies could assess the predictive value of these biomarkers for disease progression, treatment response, and prognosis, thereby contributing to personalized treatment strategies.
5. Conclusion
In summary, our study shows that while circulating miRNAs have limited use in TB diagnostics, they hold strong potential for early detection of LC and distinguishing LC from TB. These findings highlight the value of miRNAs as biomarkers in improving diagnostics for pulmonary diseases.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Table S1: Database; Table S2: Comparative statistics of the levels of 15 miRNAs among stage I LC patients, TB patients, and healthy controls; Table S3: Significant differences in miRNA levels between groups with different clinicopathological characteristics; Table S4: Results of regression analysis and partial correlation analysis to assess the impact of age on differences in miRNA levels between groups; Table S5: ROC-analysis results; Figure S1: ROC curves showing the ability of miRNAs to distinguish stage I LC patients.
Author Contributions
Conceptualization, Y.A., G.U., K.S. (Kamalidin Sharipov) and N.J.; methodology, Y.A., A.A., K.S. (Kantemir Satken), and I.P.; formal analysis, K.S. (Kantemir Satken) and Y.A.; investigation, K.S. (Kantemir Satken), A.A., D.K., N.K., A.Y., L.Y. and A.K; resources, A.Y., L.Y. and A.K.; data curation, I.P.; writing—original draft preparation, Y.A., N.K. and I.P.; writing—review and editing, G.U., A.Y., L.Y., A.K., A.A., D.K., N.J. and K.S. (Kamalidin Sharipov); visualization, K.S. (Kantemir Satken); supervision, G.U.; project administration, K.S. (Kamalidin Sharipov); funding acquisition, Y.A. and N.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Science Committee of the Ministry of Science and Higher Education of the Republic of Kazakhstan (Grant No. AP13068414).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the local ethics committee of the Aitkhozhin Institute of Molecular Biology and Biochemistry (protocol No. 9 dated 8 December 2021).
Informed Consent Statement
Informed consent was obtained from all subjects whose biomaterial was used in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Global Tuberculosis Report 2023, 1st ed.; World Health Organization: Geneva, 2023.
- Getahun, H.; Matteelli, A.; Chaisson, R. E.; Raviglione, M. Latent Mycobacterium Tuberculosis Infection. N Engl J Med 2015, 372, 2127–2135. [Google Scholar] [CrossRef] [PubMed]
- Pai, M.; Nicol, M. P.; Boehme, C. C. Tuberculosis Diagnostics: State of the Art and Future Directions. Microbiol Spectr 2016, 4, 4–5. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R. L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J Clinicians 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Nikšić, M.; Bonaventure, A.; Valkov, M.; Johnson, C. J.; Estève, J.; Ogunbiyi, O. J.; et al. Global Surveillance of Trends in Cancer Survival 2000–14 (CONCORD-3): Analysis of Individual Records for 37 513 025 Patients Diagnosed with One of 18 Cancers from 322 Population-Based Registries in 71 Countries. The Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef]
- Xiang, Y.; Huang, C.; He, Y.; Zhang, Q. Cancer or Tuberculosis: A Comprehensive Review of the Clinical and Imaging Features in Diagnosis of the Confusing Mass. Front. Oncol. 2021, 11, 644150. [Google Scholar] [CrossRef] [PubMed]
- Preda, M.; Tănase, B. C.; Zob, D. L.; Gheorghe, A. S.; Lungulescu, C. V.; Dumitrescu, E. A.; Stănculeanu, D. L.; Manolescu, L. S. C.; Popescu, O.; Ibraim, E.; Mahler, B. The Bidirectional Relationship between Pulmonary Tuberculosis and Lung Cancer. IJERPH 2023, 20, 1282. [Google Scholar] [CrossRef] [PubMed]
- Hang, T.-X.; Fang, G.; Huang, Y.; Hu, C.-M.; Chen, W. Misdiagnosis of a Multi-Organ Involvement Hematogenous Disseminated Tuberculosis as Metastasis: A Case Report and Literature Review. Infect Dis Poverty 2020, 9, 66. [Google Scholar] [CrossRef]
- Varol, Y.; Varol, U.; Unlu, M.; Kayaalp, I.; Ayranci, A.; Dereli, M. S.; Guclu, S. Z. Primary Lung Cancer Coexisting with Active Pulmonary Tuberculosis. int j tuberc lung dis 2014, 18, 1121–1125. [Google Scholar] [CrossRef]
- Moreno-Moya, J. M.; Vilella, F.; Simón, C. MicroRNA: Key Gene Expression Regulators. Fertility and Sterility 2014, 101, 1516–1523. [Google Scholar] [CrossRef]
- Mohr, A.; Mott, J. Overview of MicroRNA Biology. Semin Liver Dis 2015, 35, 003–011. [Google Scholar] [CrossRef]
- Wang, L.; Xiong, Y.; Fu, B.; Guo, D.; Zaky, M. Y.; Lin, X.; Wu, H. MicroRNAs as Immune Regulators and Biomarkers in Tuberculosis. Front. Immunol. 2022, 13, 1027472. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Guo, J.; Fan, S.; Li, Y.; Wei, L.; Yang, X.; Jiang, T.; Chen, Z.; Wang, C.; Liu, J.; Ping, Z.; Xu, D.; Wang, J.; Li, Z.; Qiu, Y.; Li, J.-C. Screening and Identification of Six Serum microRNAs as Novel Potential Combination Biomarkers for Pulmonary Tuberculosis Diagnosis. PLoS ONE 2013, 8, e81076. [Google Scholar] [CrossRef] [PubMed]
- Lyu, L.; Zhang, X.; Li, C.; Yang, T.; Wang, J.; Pan, L.; Jia, H.; Li, Z.; Sun, Q.; Yue, L.; Chen, F.; Zhang, Z. Small RNA Profiles of Serum Exosomes Derived From Individuals With Latent and Active Tuberculosis. Front. Microbiol. 2019, 10, 1174. [Google Scholar] [CrossRef] [PubMed]
- Ndzi, E. N.; Nkenfou, C. N.; Mekue, L. M.; Zentilin, L.; Tamgue, O.; Pefura, E. W. Y.; Kuiaté, J.-R.; Giacca, M.; Ndjolo, A. MicroRNA Hsa-miR-29a-3p Is a Plasma Biomarker for the Differential Diagnosis and Monitoring of Tuberculosis. Tuberculosis 2019, 114, 69–76. [Google Scholar] [CrossRef]
- Tu, H.; Yang, S.; Jiang, T.; Wei, L.; Shi, L.; Liu, C.; Wang, C.; Huang, H.; Hu, Y.; Chen, Z.; Chen, J.; Li, Z.; Li, J. Elevated Pulmonary Tuberculosis Biomarker miR-423-5p Plays Critical Role in the Occurrence of Active TB by Inhibiting Autophagosome-Lysosome Fusion. Emerging Microbes & Infections 2019, 8, 448–460. [Google Scholar] [CrossRef]
- Uno, S.; Nishimura, T.; Nishio, K.; Kohsaka, A.; Tamizu, E.; Nakano, Y.; Kagyo, J.; Nakajima, Y.; Arai, R.; Hasegawa, H.; Arakawa, K.; Kashimura, S.; Ishii, R.; Miyazaki, N.; Uwamino, Y.; Hasegawa, N. Potential Biomarker Enhancing the Activity of Tuberculosis, Hsa-miR-346. Tuberculosis 2021, 129, 102101. [Google Scholar] [CrossRef]
- Li, X.; Xu, Y.; Liao, P. Diagnostic Performance of microRNA-29a in Active Pulmonary Tuberculosis: A Systematic Review and Meta-Analysis. Clinics 2023, 78, 100290. [Google Scholar] [CrossRef]
- Wang, C.; Liu, C.-M.; Wei, L.-L.; Shi, L.-Y.; Pan, Z.-F.; Mao, L.-G.; Wan, X.-C.; Ping, Z.-P.; Jiang, T.-T.; Chen, Z.-L.; Li, Z.-J.; Li, J.-C. A Group of Novel Serum Diagnostic Biomarkers for Multidrug-Resistant Tuberculosis by iTRAQ-2D LC-MS/MS and Solexa Sequencing. Int. J. Biol. Sci. 2016, 12, 246–256. [Google Scholar] [CrossRef]
- Wagh, V.; Urhekar, A.; Modi, D. Levels of microRNA miR-16 and miR-155 Are Altered in Serum of Patients with Tuberculosis and Associate with Responses to Therapy. Tuberculosis 2017, 102, 24–30. [Google Scholar] [CrossRef]
- Barry, S. E.; Ellis, M.; Yang, Y.; Guan, G.; Wang, X.; Britton, W. J.; Saunders, B. M. Identification of a Plasma microRNA Profile in Untreated Pulmonary Tuberculosis Patients That Is Modulated by Anti-Mycobacterial Therapy. Journal of Infection 2018, 77, 341–348. [Google Scholar] [CrossRef]
- Reddy, K. B. MicroRNA (miRNA) in Cancer. Cancer Cell Int 2015, 15, 38. [Google Scholar] [CrossRef] [PubMed]
- Schwarzenbach, H. Clinical Relevance of Circulating, Cell-Free and Exosomal microRNAs in Plasma and Serum of Breast Cancer Patients. Oncol Res Treat 2017, 40, (7–8). [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Shi, K.; Yang, S.; Liu, J.; Zhou, Q.; Wang, G.; Song, J.; Li, Z.; Zhang, Z.; Yuan, W. Effect of Exosomal miRNA on Cancer Biology and Clinical Applications. Mol Cancer 2018, 17, 147. [Google Scholar] [CrossRef] [PubMed]
- Nadal, E.; Truini, A.; Nakata, A.; Lin, J.; Reddy, R. M.; Chang, A. C.; Ramnath, N.; Gotoh, N.; Beer, D. G.; Chen, G. A Novel Serum 4-microRNA Signature for Lung Cancer Detection. Sci Rep 2015, 5, 12464. [Google Scholar] [CrossRef] [PubMed]
- Powrózek, T.; Krawczyk, P.; Kowalski, D. M.; Kuźnar-Kamińska, B.; Winiarczyk, K.; Olszyna-Serementa, M.; Batura-Gabryel, H.; Milanowski, J. Application of Plasma Circulating microRNA-448, 506, 4316, and 4478 Analysis for Non-Invasive Diagnosis of Lung Cancer. Tumor Biol. 2016, 37, 2049–2055. [Google Scholar] [CrossRef]
- Arab, A.; Karimipoor, M.; Irani, S.; Kiani, A.; Zeinali, S.; Tafsiri, E.; Sheikhy, K. Potential Circulating miRNA Signature for Early Detection of NSCLC. Cancer Genetics 2017, 216–217, 150–158. [Google Scholar] [CrossRef]
- Zhang, H.; Mao, F.; Shen, T.; Luo, Q.; Ding, Z.; Qian, L.; Huang, J. Plasma miR-145, miR-20a, miR-21 and miR-223 as Novel Biomarkers for Screening Early-Stage Non-Small Cell Lung Cancer. Oncology Letters 2017, 13, 669–676. [Google Scholar] [CrossRef]
- Shao, C.; Yang, F.; Qin, Z.; Jing, X.; Shu, Y.; Shen, H. The Value of miR-155 as a Biomarker for the Diagnosis and Prognosis of Lung Cancer: A Systematic Review with Meta-Analysis. BMC Cancer 2019, 19, 1103. [Google Scholar] [CrossRef]
- Tao, S.; Ju, X.; Zhou, H.; Zeng, Q. Circulating microRNA-145 as a Diagnostic Biomarker for Non-Small-Cell Lung Cancer: A Systemic Review and Meta-Analysis. Int J Biol Markers 2020, 35, 51–60. [Google Scholar] [CrossRef]
- Shen, X.; Li, L.; Zhang, L.; Liu, W.; Wu, Y.; Ma, R. Diagnostic and Prognostic Value of microRNA-486 in Patients with Lung Cancer: A Systematic Review and Meta-Analysis. Int J Biol Markers 2022, 37, 377–385. [Google Scholar] [CrossRef]
- Wang, W.; Li, X.; Liu, C.; Zhang, X.; Wu, Y.; Diao, M.; Tan, S.; Huang, S.; Cheng, Y.; You, T. MicroRNA-21 as a Diagnostic and Prognostic Biomarker of Lung Cancer: A Systematic Review and Meta-Analysis. Bioscience Reports 2022, 42, BSR20211653. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhang, J.; Yang, J.; Wei, Y.; Peng, J.; Fu, C.; Huang, M.; Wang, R.; Wang, P.; Sun, G.; Xie, S. MiR -205-5p Promotes Lung Cancer Progression and Is Valuable for the Diagnosis of Lung Cancer. Thoracic Cancer 2022, 13, 832–843. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.; Peng, M.; Gong, J.; Li, C.; Cheng, H.; Li, Y.; Tang, Y. Circulating Exosomal microRNA-4497 as a Potential Biomarker for Metastasis and Prognosis in Non-Small-Cell Lung Cancer. Exp Biol Med (Maywood) 2023, 248, 1403–1413. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, B. C.; Dotto, G.-P. Racial Differences in Cancer Susceptibility and Survival: More Than the Color of the Skin? Trends in Cancer 2017, 3, 181–197. [Google Scholar] [CrossRef]
- Tuasha, N.; Petros, B. Heterogeneity of Tumors in Breast Cancer: Implications and Prospects for Prognosis and Therapeutics. Scientifica 2020, 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nassar, F. J.; Talhouk, R.; Zgheib, N. K.; Tfayli, A.; El Sabban, M.; El Saghir, N. S.; Boulos, F.; Jabbour, M. N.; Chalala, C.; Boustany, R.-M.; Kadara, H.; Zhang, Z.; Zheng, Y.; Joyce, B.; Hou, L.; Bazarbachi, A.; Calin, G.; Nasr, R. microRNA Expression in Ethnic Specific Early Stage Breast Cancer: An Integration and Comparative Analysis. Sci Rep 2017, 7, 16829. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Guan, Z.; Cuk, K.; Zhang, Y.; Brenner, H. Circulating MicroRNA Biomarkers for Lung Cancer Detection in East Asian Populations. Cancers 2019, 11, 415. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ (accessed on 29 October 2024).
- Königshoff, M.; Kramer, M.; Balsara, N.; Wilhelm, J.; Amarie, O. V.; Jahn, A.; Rose, F.; Fink, L.; Seeger, W.; Schaefer, L.; Günther, A.; Eickelberg, O. WNT1-Inducible Signaling Protein–1 Mediates Pulmonary Fibrosis in Mice and Is Upregulated in Humans with Idiopathic Pulmonary Fibrosis. J. Clin. Invest. 2009, JCI33950. [Google Scholar] [CrossRef]
- Jamovi. Available online: https://www.jamovi.org/ (accessed on 29 October 2024).
- FDR online calculator. Available online: https://www.sdmproject.com/utilities/?show=FDR (accessed on 29 October 2024).
- Center for Diagnostics & Telemedicine: Web Tool for ROC Analysis. Available online: https://roc-analysis.mosmed.ai (accessed on 29 October 2024).
- Statistics Kingdom: ROC Calculator. Available online: https://www.statskingdom.com/roc-calculator.html (accessed on 29 October 2024).
- Muller, M. P.; Tomlinson, G.; Marrie, T. J.; Tang, P.; McGeer, A.; Low, D. E.; Detsky, A. S.; Gold, W. L. Can Routine Laboratory Tests Discriminate between Severe Acute Respiratory Syndrome and Other Causes of Community-Acquired Pneumonia? CLIN INFECT DIS 2005, 40, 1079–1086. [Google Scholar] [CrossRef]
- Tang, D.; Chen, M.; Huang, X.; Zhang, G.; Zeng, L.; Zhang, G.; Wu, S.; Wang, Y. SRplot: A Free Online Platform for Data Visualization and Graphing. PLoS ONE 2023, 18, e0294236. [Google Scholar] [CrossRef]
- Bioinformatics & Evolutionary Genomics: Calculate and Draw Custom Venn Diagrams. Available online: http://bioinformatics.psb.ugent.be/webtools/Venn (accessed on 29 October 2024).
- Chen, Y.; Chen, X.; Li, Z.; Zhu, Y.; Liu, F.; Cai, J. CircDENND2D Inhibits PD-L1-Mediated Non-Small Cell Lung Cancer Metastasis and Immune Escape by Regulating miR-130b-3p/STK11 Axis. Biochem Genet 2023, 61, 2691–2709. [Google Scholar] [CrossRef] [PubMed]
- Guo, Q.; Yan, J.; Song, T.; Zhong, C.; Kuang, J.; Mo, Y.; Tan, J.; Li, D.; Sui, Z.; Cai, K.; Zhang, J. microRNA-130b-3p Contained in MSC-Derived EVs Promotes Lung Cancer Progression by Regulating the FOXO3/NFE2L2/TXNRD1 Axis. Molecular Therapy - Oncolytics 2021, 20, 132–146. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.; Wang, C.; Yang, Z.; Liu, W.; Yuan, Y.; Li, K.; Zhang, Y.; Wang, Y.; Shi, Y.; Qiu, Y.; Zuo, D.; He, W.; Qiu, J.; Guan, X.; Yuan, Y.; Li, B. Dysregulated Sp1/miR-130b-3p/HOXA5 Axis Contributes to Tumor Angiogenesis and Progression of Hepatocellular Carcinoma. Theranostics 2020, 10, 5209–5224. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Wang, Y.; Chen, Y.; Guo, Y.; Li, Q.; Wei, X. Exosomal miR-130b-3p Promotes Progression and Tubular Formation Through Targeting PTEN in Oral Squamous Cell Carcinoma. Front. Cell Dev. Biol. 2021, 9, 616306. [Google Scholar] [CrossRef]
- Li, H.; Liu, P.; Li, D.; Wang, Z.; Ding, Z.; Zhou, M.; Chen, X.; Miao, M.; Ding, J.; Lin, W.; Liu, Y.; Zha, X. STAT3/miR-130b-3p/MBNL1 Feedback Loop Regulated by mTORC1 Signaling Promotes Angiogenesis and Tumor Growth. J Exp Clin Cancer Res 2022, 41, 297. [Google Scholar] [CrossRef]
- Qian, X.; Xie, F.; Wei, H.; Cui, D. Identification of Key Circulating Exosomal microRNAs in Gastric Cancer. Front. Oncol. 2021, 11, 693360. [Google Scholar] [CrossRef]
- Song, D.; Zhang, Q.; Zhang, H.; Zhan, L.; Sun, X. MiR-130b-3p Promotes Colorectal Cancer Progression by Targeting CHD9. Cell Cycle 2022, 21, 585–601. [Google Scholar] [CrossRef]
- Wang, J.; Zhao, L.; Peng, X.; Liu, K.; Zhang, C.; Chen, X.; Han, Y.; Lai, Y. Evaluation of miR-130 Family Members as Circulating Biomarkers for the Diagnosis of Bladder Cancer. Clinical Laboratory Analysis 2020, 34, e23517. [Google Scholar] [CrossRef]
- Liang, H.; Lu, Y.; Huang, X.; Ye, T. LncRNA BRCAT54 Is Downregulated and Inhibits Cancer Cell Proliferation by Downregulating miR-130b-3p through Methylation in Prostate Cancer. J Biochem & Molecular Tox 2024, 38, e23552. [Google Scholar] [CrossRef]
- Lv, M.; Li, X.; Zheng, C.; Tian, W.; Yang, H.; Yin, Z.; Zhou, B. Exosomal miR-130b-3p Suppresses Metastasis of Non-Small Cell Lung Cancer Cells by Targeting DEPDC1 via TGF-β Signaling Pathway. International Journal of Biological Macromolecules 2024, 275, 133594. [Google Scholar] [CrossRef]
- Huang, Y.; Feng, G. MiR-423-5p Aggravates Lung Adenocarcinoma via Targeting CADM1. Thoracic Cancer 2021, 12, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Ye, J.; Dang, Y.; Xu, S. LncRNA PGM5-AS1 Inhibits Non-Small Cell Lung Cancer Progression by Targeting miRNA-423-5p/SLIT2 Axis. Cancer Cell Int 2024, 24, 216. [Google Scholar] [CrossRef] [PubMed]
- Sun, G.; Ding, X.; Bi, N.; Wu, L.; Wang, J.; Zhang, W.; Dong, X.; Lv, N.; Song, Y.; Zhan, Q.; Wang, L. MiR-423-5p in Brain Metastasis: Potential Role in Diagnostics and Molecular Biology. Cell Death Dis 2018, 9, 936. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Cai, W.; Zhou, T.; Men, B.; Chen, S.; Tu, D.; Guo, W.; Wang, J.; Zhao, F.; Wang, Y. CEACAM1 Increased the Lymphangiogenesis through miR-423-5p and NF- kB in Non-Small Cell Lung Cancer. Biochemistry and Biophysics Reports 2024, 40, 101833. [Google Scholar] [CrossRef]
- Li, W.; Zhang, B.; Jia, Y.; Shi, H.; Wang, H.; Guo, Q.; Li, H. LncRNA LOXL1-AS1 Regulates the Tumorigenesis and Development of Lung Adenocarcinoma through Sponging miR-423-5p and Targeting MYBL2. Cancer Medicine 2020, 9, 689–699. [Google Scholar] [CrossRef]
- Kang, H.-J.; Yun, S.; Shin, S.-H.; Youn, D. H.; Son, G.-H.; Lee, J. J.; Hong, J. Y. Tuberculous Pleural Effusion-Derived Exosomal miR-130b-3p and miR-423-5p Promote the Proliferation of Lung Cancer Cells via Cyclin D1. IJMS 2024, 25, 10119. [Google Scholar] [CrossRef]
- Halvorsen, A. R.; Bjaanæs, M.; LeBlanc, M.; Holm, A. M.; Bolstad, N.; Rubio, L.; Peñalver, J. C.; Cervera, J.; Mojarrieta, J. C.; López-Guerrero, J. A.; Brustugun, O. T.; Helland, Å. A unique set of 6 circulating microRNAs for early detection of non-small cell lung cancer. Oncotarget 2016, 7, 37250–37259. [Google Scholar] [CrossRef]
- Zhu, W.; Zhou, K.; Zha, Y.; Chen, D.; He, J.; Ma, H.; Liu, X.; Le, H.; Zhang, Y. Diagnostic Value of Serum miR-182, miR-183, miR-210, and miR-126 Levels in Patients with Early-Stage Non-Small Cell Lung Cancer. PloS one 2016, 11, e0153046. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).