INTRODUCTION
The prevalence of obesity is increasing rapidly in all age groups worldwide. It is currently one of the fastest growing epidemics, affecting 10-40% of the adult population. Reduced life expectancy and obesity related complications may account for 5-10% of all health costs in the European countries [
1].Obesity increases the risk of adverse health conditions, the risk of metabolic and cardiovascular diseases, certain type of cancers, impaired quality of life, and (as recently discovered) complications from Covid-19 [
2].
During the normal ageing process, weight gain often occurs gradually over decades (about 0.4-0.5 kg per year), making it difficult for most people to perceive the specific causes [
3]. Prevention of obesity is not always easy; there are some essential contributing factors, i.e. genetic background, lifestyle, medication, environmental circumstances etc. Since weight stability requires balance between energy consumed and expended, in most of the cases, the advice to “eat less and exercise more” seems to be straightforward in the prevention [
4]. It should be started as early as possible; therefore interventions preferably in childhood could be implemented for prevention. Obesity management requires holistic approach, analysis of individual risk factors and it is a time consuming, not always successful process.
Excess body weight during childhood is associated with an increased risk of adult type 2 diabetes only if it continued until puberty or later ages [
5]. In addition to the robust evidence that obesity and excess body weight are strongly related to the incidence of metabolic diseases (type 2 diabetes, hypertension), the rate of weight gain could also contribute to the occurrence of these morbidities. The rate of weight gain was evaluated in studies among middle-aged and elderly populations over a few years of follow up periods [
6,
7]. None of the primary care studies focused to this phenomenon and it was the reason why our research started, initiated in the primary care setting, the first line of the health care system. Our first Hungarian lifelong study, in which the two main components of Metabolic Syndrome were evaluated [
8] and the following others found differences between the dynamics of weight gain among patients with obesity, diabetes and hypertension [
9,
10].
A medical setting is required to control laboratory parameters (plasma glucose level, lipid profile), blood pressure is often measured by the patients, while body weight and height are usually checked by the individuals themselves. Although many people regularly measure their own body weight, remember these data, they rarely store or compare these records.
The aims of this paper are to present and summarize our previous findings; how the weight gain trends to overweight and obesity in the younger decades and could be responsible for the onset of metabolic diseases and to explain why early primary care intervention is needed.
METHODS and PATIENTS
Study Design
A cross-sectional survey, combined with retrospective analysis.
Selection of Participants
Patients (aged between 60 and 70 years) who visited the offices of their family physicians/general practitioners or primary care outpatient clinics within the study period for any reason (having actual complaints, coming for regular screening, drug prescription, etc.) were consecutively selected.
Data Collection
Having been informed about the aim of the survey and given the proper instructions, the selected participants were asked to fill in a short one page questionnaire in the doctor’s office. The form contained questions regarding self-recorded data of body
weight in each decade of life (at 20, 30, 40, 50, and 60 years of age), the most recent and the highest values; body
height at 20 years and recently. For women, the weight before the first pregnancy, after the last delivery, before and after menopause was also requested. Primarily, if were available or recorded previously, data in the medical files were used, otherwise the self-reported data were considered. The recent corresponding measures were performed by the staff and they added the time of diagnoses as needed [
8,
9,
10]. In the international study, the questionnaire in English was translated to their respective national language by the family physicians, who participated in the national arms of the study in Germany, Hungary, Italy, Slovakia and Ukraine [
11]. (See Appendix A).
The protocol of the first Hungarian study [
8] was continuously improved using more developed methods in order to drop out unreliable data. Questions regarding pregnancy and menopause were added in the last (international) study [
11].
Settings
The participating practices were located in the suburb of Budapest, in Debrecen and Kecskemét (Hungary), Leipzig (East-Germany), in Rome, around Naples (South-Italy), in Bratislava (Slovakia) and near to Uzhgorod (West-Ukraine).
Practice sizes varied between 1200-1800 enrolled patients, 56-112 subjects participated from each practice. The duration of the study was usually one week.
Exclusion Criteria
The primary exclusion criteria were: serious visual, acoustic or mental impairment, participation in our previous studies or simple refusal to participate. In order to reduce methodological bias, the validity of self-reported data was checked. After completing the questionnaire, the participants’ current body weight and height were measured and subjects (approx.20%) were excluded if the difference between the self-reported and the recently recorded data exceeded 3 kg or 5cm.
Quantitative Variables
The participants were divided into four groups: patients with diabetes (DM), with hypertension (Hyp), or both (HyDm) and a control group (people having neither diabetes nor hypertension). For another comparison, patients with both illnesses were counted among diabetics.
After weight and height measurements the body mass index (BMI) was calculated. Percentage of weight change was calculated as weight at examined decade/ weight at previous decade. The overall incidence rate was calculated as the ratio between the numbers of cases. Hypertension and diabetes were used as an outcome measure. Independent variables included gender, age and BMI categories.
Statistics
In the different studies, the following statistical methods were used: Student t-test, logistic regression (OR and CI), ANOVA, Fisher and κ2 test, Cox-regression model, Schönefeld residual test. The analyses were performed using SPSS and later on STATA 10.1.softwares.
RESULTS
Altogether 2 468 persons, above 60 years participated in the four studies. Their distributions regarding referenced studies:
| Reference No |
All |
Men |
Women |
| 8 |
354 |
159 |
195 |
| 9 |
540 |
225 |
315 |
| 10 |
815 |
319 |
496 |
| 11 |
759 |
337 |
422 |
Within the results of the studies, there was no statistical difference between the mean ages of the established diagnoses. Diagnosing hypertension was 55.4 (±15.9) (median: 59) years in men and 53.8 (±15.7) (median: 56) in women, while diabetes was diagnosed at the age of 51.3 (±17.1) (median:53) years and 54.4 (± 13.1) (median: 50) years in males and females, respectively [
10]. Higher age at the recognition of diabetes 58.2 ± 8.7 years was recorded only in one study and only by men [
11].
Five hundred forty patients were involved in our second study [
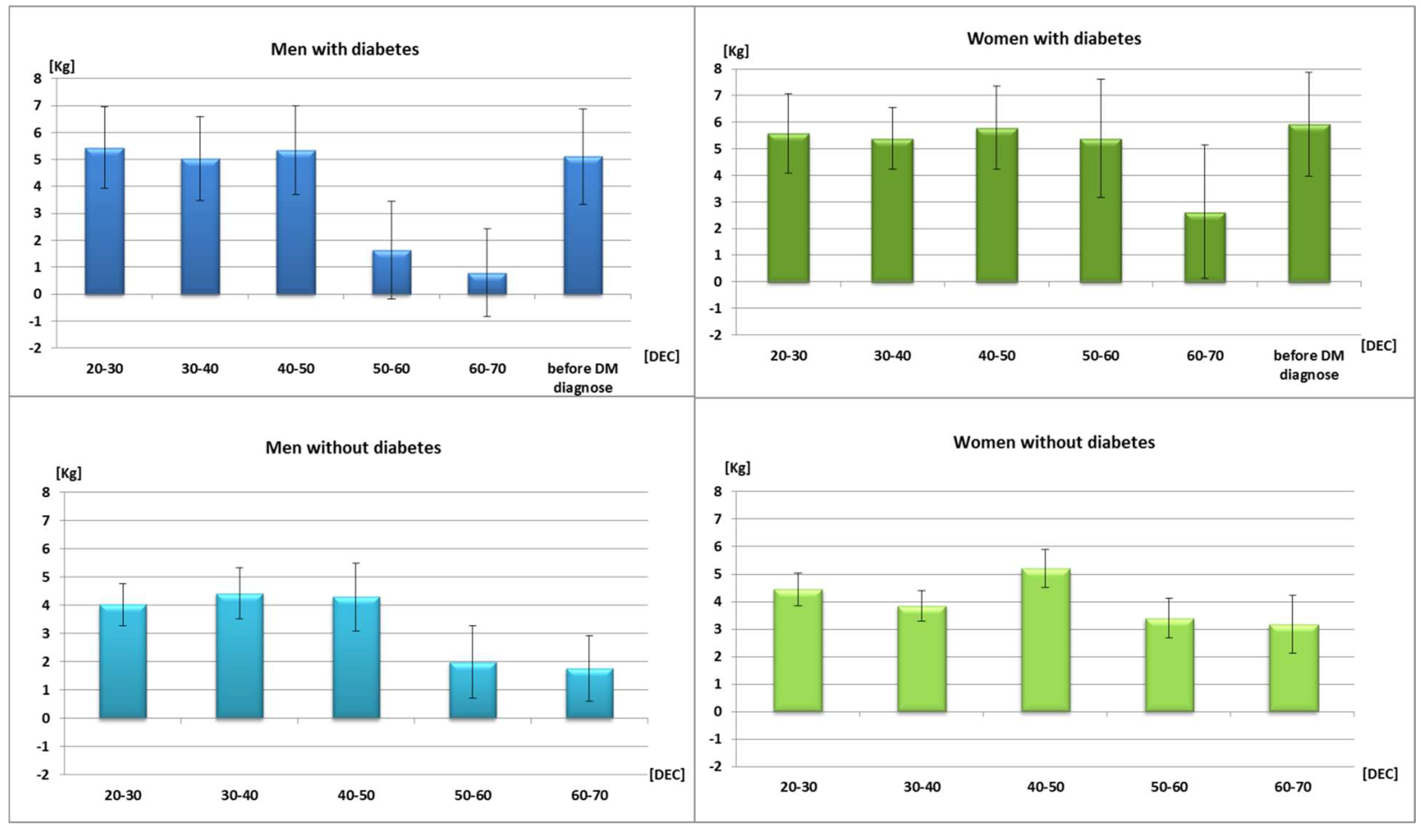
9]. The most important phenomena, the faster weight gain in the early decades by men with diabetes and hypertension were demonstrated on
Table 1. and by women on
Table 2.
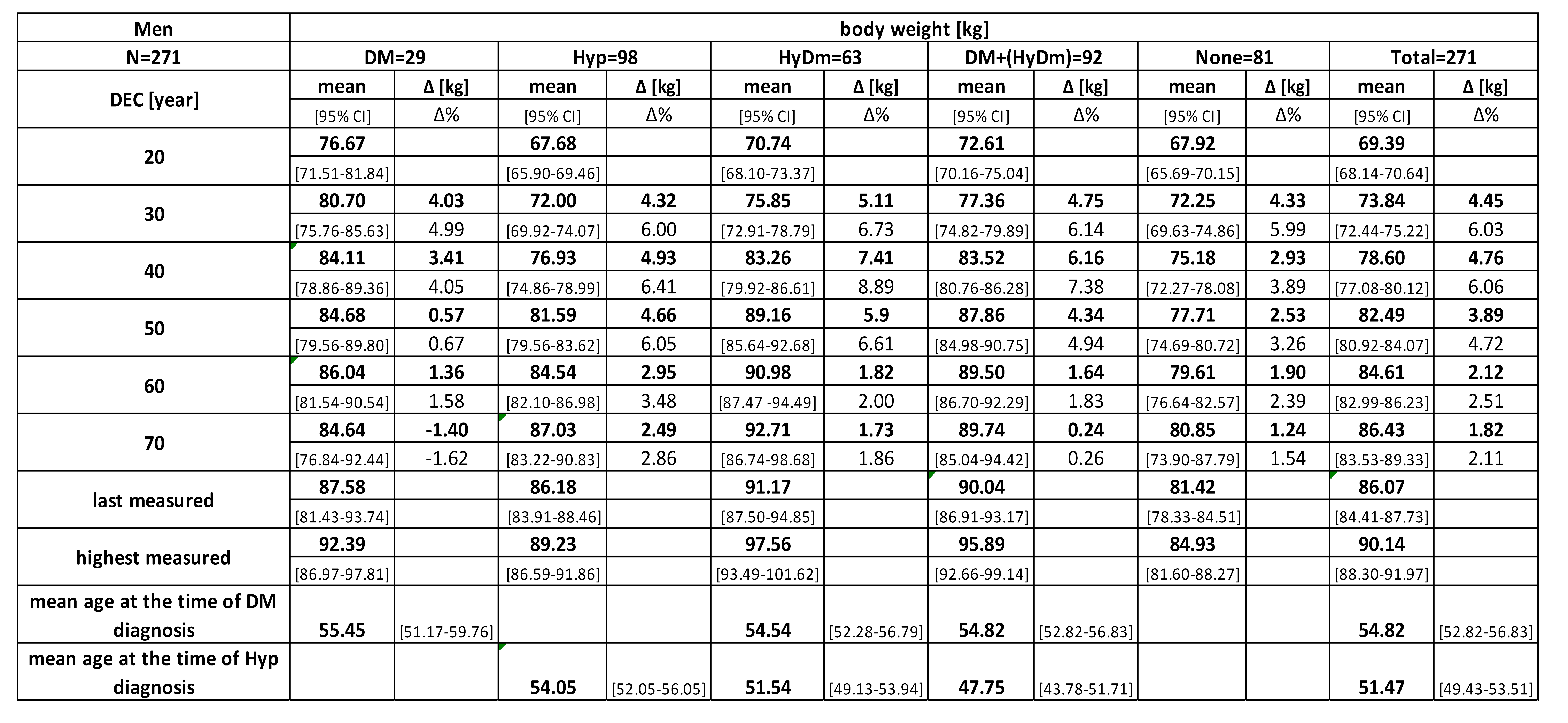
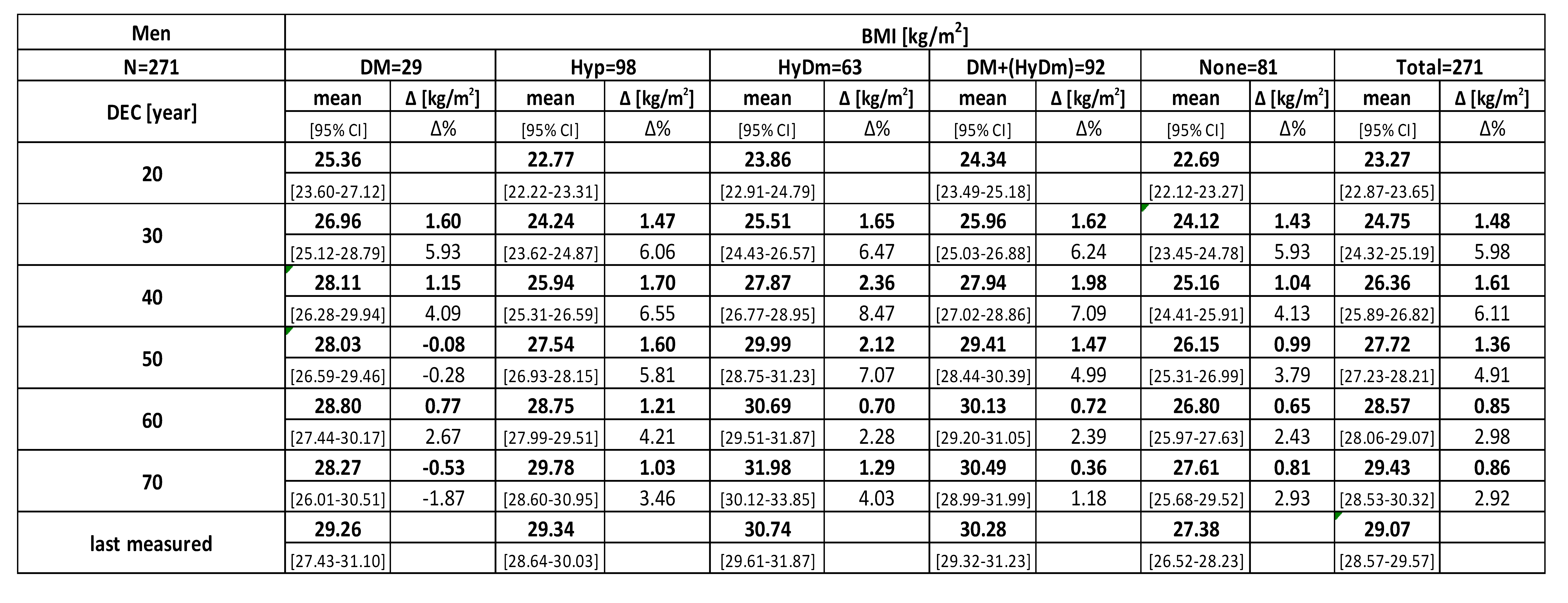
In the fourth study [
11] a lifelong body weight gains were observed in all diagnostic categories and genders (
Table 3). The last measured data were usually smaller then the “peaks” within previous decades.Diabetes and hypertension were diagnosed earlier among patients with both morbidities, while hypertension alone occurred later. Diabetic men reported their highest weight gain between 20-30y of age, when expressed both in [kg] and in
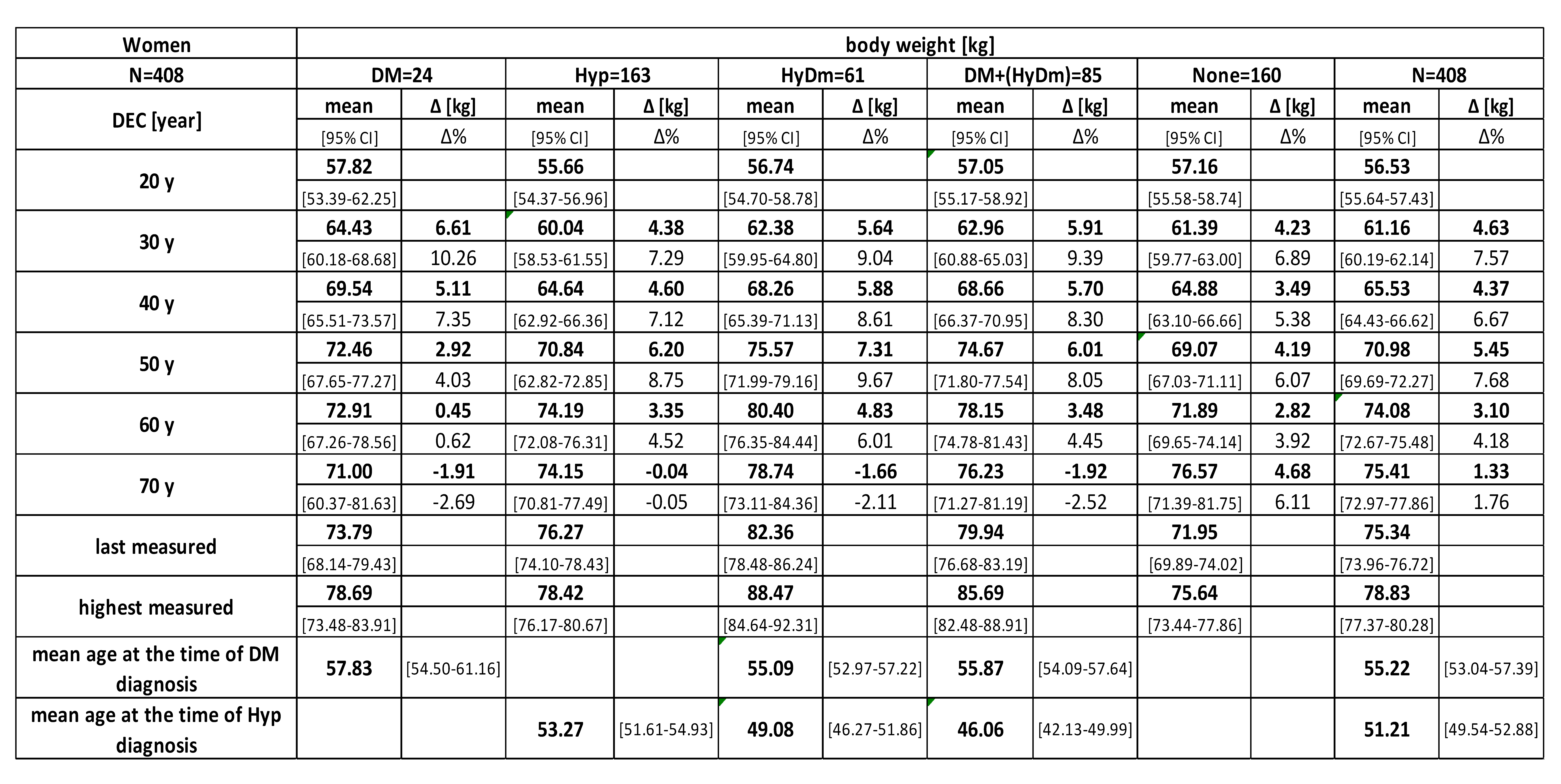
percent of the weight at 20y. It was usually followed another fast weight gain in the last decade before diabetes was diagnosed. The highest early increase was recorded among men with both morbidities. Patients with hypertension had higher, but not always significant differences through decades than the control group had. These changes were more markedly reflected in the figures of BMI (
Table 4). Similar data of women are presented on the
Table 5 and
Table 6.
The tables demonstrate that both men and women who became diabetics later on had higher body weight and BMI at the age of 20. For diabetes, the highest increases were reported in the third, for hypertension in the fourth life decades and the increase also continued in the fifth decade. For most of the affected patients, high increase was recorded in the last decade prior to diagnosis. No differences were found between countries. After 60y, a small decrease was observed by both genders in all of the studies. The differences between weight gains of diagnostic groups were more visible, when diabetics and patients with diabetes and hypertension were merged into one group and were compared with the control group (
Figure 1).
In the third study [
10], patients were divided into
quintiles (N=127-141) according to the distribution of data of weight changes between the respective and baseline decades, as seen in
Table 7 Data of other quintiles (q) were compared to that of
q1 and between genders. There were lower differences between data in the first decade therefore only three groups were formed here. Incidence rate (IR) and hazard ratio (HR) of both illnesses were the highest in the group
q5 where the largest increases were registered. HR was even higher when both hypertension and diabetes were diagnosed.
Higher increase in body weight also resulted in the changes between BMI categories. Patients who belonged to the normal BMI category, had 2.80 odds ratio (OR) (95% CI: 1.24-6.25; p=0.013) for diabetes when changing to overweight and 3.23 OR (95% CI: 1.19-8.76; p=0.022) when moving into the obese category.
Comparing the date of weight change between the initial and the respective decades, the higher the weight change was, the higher HR for diabetes and hypertension were calculated.
Table 8 presents these ratios only for 10% and 30% increases in weight between decades. Early increase of body weight was related to higher HR for men for developing diabetes and for women for developing hypertension. In many cases, the increases were much higher than 30%, often exceeding 50%.
Among women, weight changes around delivery and menopause had also an impact on the development of diabetes and hypertension. The means of body weight, registered by the participants at the last delivery and at the age when menopause related symptoms occurred, correlated significantly with diabetes and/or hypertension resulting higher probabilities for developing the diseases (
Table 9). There were no significant differences between numbers of children and the weight gain of the mother.
DISCUSSION
Main Findings
Early weight gain resulting overweight and obesity is significantly associated to the incidence of metabolic diseases. Patients with diabetes recorded the highest increase expressed in body weight, in BMI and in percent of the weight at 20y. Body weight and BMI changes over decades, was the highest in men with diabetes, higher among patients with hypertension and the less within control groups in both gender. Among patients with diabetes and hypertension, both diagnoses were set up earlier, than by patients having only one of them.
Although minimal differences were proven between surveys, the trend was clear, confirming the harmful effects of early weight gain in the younger decades, with small differences between genders. Significant weight gain around the (last) delivery and menopause increase the chance for diabetes and/or hypertension as well.
Strengths and Limitations
Decade-long comparison of data could be mentioned as the real strength of this study.
The most important methodological limitation was the reliability of data based on memory and personal records, which could err in both directions. The medical records used could not counterbalance this bias with certainty. Unfortunately, regular body weight measurement is not part of the routine medical practice. People usually remember better at what age and what life event they started to gain more weight (e.g. marriage, divorcing, graduation, changing work places or accommodation, pregnancies, menopause, required changes of “wardrobe”, quitting smoking, getting ill or hospitalized, etc.). Although there could be some unreliability of the reported data, the trends could be clearly verified, in our national and in international studies as well.
There were only a few decades’ long studies, because most of the researchers are not able to conduct studies over decades, following the patients for a lifelong period, and correctly registering their anthropometric parameters. This is the reason, why other studies with exactly measured anthropometric data covered only years and never decades. The accuracy of data and longevity of follow-up need some compromise.
There are other theoretical and practical limitations of our studies such as:
- therapy and interventions started at a younger age may have modified the findings, although there was not such a wide variety of drugs available for this generation, compared to more effective medications recently used,
- genetic elements and other risk factors remained undiscovered,
- patient’s inclusion was not standardized and those who are affected by metabolic diseases represent the largest proportion of persons attending primary care surgeries, hence they were overrepresented. Their ratio in this study was much higher than in the general population, and could not be considered as representative, although both urban and rural inhabitants were involved,
- if data would be available, weight at birth, eating habits, socioeconomic circumstances, sleep duration, physical activity and their changes could be analyzed as well. More information about the time of menarche, on lactation, medication, surgical menopause or hormonal replacement therapy could also be useful, so were unable to exclude all of the confounding factors.
- decade, as a threshold limit, does not always reflect biological or pathological changes properly.
The same BMI does not mean the same body weight and height in different life periods. Due to the normal decrease in body height and
sarcopenia, the same weight in the elderly means a higher BMI [
6]. While we had data only of recent measurement and self-reports on heights at 20y, it may result some slight differences in BMI values.
Comparison with Previous Studies
Using questionnaires has been an acceptable tool for data recording. Epidemiological studies using similar method, questionnaire-reported and staff-measured weights were highly correlated. In the famous “
The Nurses’ Health Study I. and II.” and “
The Health Professionals Follow-up Study” body weight was also questioned only, beside data on other lifestyle practices (nutritional habit, physical activity, sleep duration, “screen-watching time”) and medical history [
3].
The similarities of weight gain between the control and hypertensive groups may be due to the high prevalence of hypertension among elderly. Steady weight or slow increases in body weight have been seen more often among people without diabetes. Perhaps due to the treatment, a slight body weight decrease was observed among diabetics after 60years.
History of lifelong weight change may contribute to our understanding of why some obese older people are metabolically healthy but others are not [
12]. Physical activity should also influence long-term weight gain, but evidence to support this expectation has been surprisingly inconsistent [
13,
14,
15]. In addition, the duration of television viewing and of sleep may influence energy consumption, energy expenditure, or both [
15,
16]. In most of the epidemiological studies different lifestyle behaviours have often been evaluated separately, thus limiting relative comparisons or the quantification of combined effects. In addition, most studies of long-term weight gain have evaluated current behaviours, but changes in behaviour over time may be more relevant in terms of both their biologic effects on long-term weight gain and their translation into prevention strategies.
The increasing prevalence of obesity has led to several attempts to counter this epidemic by various types of intervention. The most promising approaches are targeting children, because prevention programmes in early life are more likely to be successful and childhood obesity tracks into adulthood [
17]. Outcomes of 71 European community-based initiatives against childhood obesity starting between 2005 and 2011 were critically evaluated. There were common characteristics: application of integrated actions at a local level, aimed at changing the environment and the children’s behaviour directly. Evidence supporting effectiveness on weight indicators is available, although the design and conduct of most of these studies were suboptimal (i.e. no control group, a small sample size, not random) [
18]. Focusing for the whole family, not only for children, the
Feel4Diabetes project ran in primary schools and local communities, considering the socio-economic status of parents as well, discovered new patients with (pre)diabetes among them [
19,
20]. In the past decades, after realizing childhood obesity as a real public health threat, many public and governmental initiatives were started. Most of them presented good outcomes, but usually over short time period. Besides these programmes and studies, new governmental strategies were implemented in some affected countries [
21,
22]. Since 2013, in Hungarian primary schools a daily physical exercise hour is a part of the curriculum. It will hopefully increase the level of physical activity of the population and decrease the prevalence of obesity.
Obesity management was in the focus of some interventions in the primary care. In a regional project in Hungary, most of the obese patients lost weight, laboratory parameters improved and blood pressure decreased [
23]. In other, patients were faced to their own cardiovascular risk assessment and this impression facilitated changes in health behavior and lifestyle [
24].
Sustained improvement in risk factor status requires ongoing risk communication with health care providers.Individualized lifestyle counselling improves health behaviour and reduces total cardiovascular risk among middle-aged men [
25]. Primary care counselling for healthy young people driving their attention on current behaviors might elicit their proactive role to improve lifestyle, getting immediate advantages such as well-being improvement and the possibility to manage stress better [
26]. Changing dietary habits is still the first step in the treatment of obesity with a focus on components of the Mediterranean diet and to avoid a high intake of ultra-processed food because it has been related to an increased risk of obesity and obesity-associated comorbidities [
27].
The simple obesity prevention differs from weight-loss trials. Weight-loss trials have typically enrolled obese or overweight persons who attempted substantial short-term weight loss on specialized diets, thus limiting the generalizability of the findings to non-obese populations and to the factors that determine long-term, gradual weight gain [
3]. When obesity already developed, utilization of counselling was lower and insufficient achieving 5% or greater weight loss at the population level [
28]. In the UK, where more resources were available in primary care, the nationwide
COUNTERWEIGHT project was longer and supported by other health care professionals and by networks of “Patients’ clubs” [
29]. Appropriate financial incentives were implemented to motivate the primary care providers [
30].
CONCLUSIONS
The patient-doctor collaboration and confidence is the closest in primary care. Family physicians are in higly responsible position in all health care systems, they should not just be inactive observers of their patients’ weight gain; they must act in due time. Instead of restrospective analyses of mass-data, we have to act earlier at individual level. All patients with visible weight gain should be systematically and individually examined, exploring the reasons and determine the type of intervention. Applying financial incentives for appropriate obesity management could be a useful tool as well. Regular anthropometric measurement should be incorporated into routine medical practice. GPs should focus also on the younger generations, who rarely visit medical settings and should provide them advice for obesity management, if needed. Our retrospective findings can initiate interventions much earlier. Primary care capacity and workforce should be linked with the global need for prevention.
Statement of Ethics
The partners of the international study declared that no detailed approval was necessary according to their national regulations, since there were only anonymous data and there was no intervention or influence on the patient and the respective medical care process. In Hungary, ethical permission was issued by the South- Budapest Ethical Committee (Jahn Ferenc Hospital, on 21 August 2000) and was updated by the Hungarian Committee on Scientific and Research Ethics (ETT-TUKEB 20928-I). All of the patients signed the informed consent form linked to the data-sheet. The data were processed anonymously by the respective family physicians.
Author Contributions
IR- conceptualization, methodology, investigation, writing: ZJ, EK, PT, CM writing, organizing their own studies and searched literature, PT, KLR contributed in the validation, investigation and editing.
All authors have read and agreed to the submitted version of the manuscript
Funding
There was no funding for these studies.
Data Availability Statement
Data of all studies were deposited as electronic files at the Department of Family and Occupational Medicine, University of Debrecen. Hard copies of questionnaires were deposited also here and in the offices of the leading authors of the respective studies.
Acknowledgement
Authors are thankful to the contributing family physicians for collecting and providing data. Special thanks to Tibor Deutsch, Endre Szigethy, Tímea Ungvári for the statistical analysis presented in the different surveys.
Conflicts of Interest
The authors declare no conflict of interest.
APPENDIX A
The questionnaire of the last survey
Dear Patient !
Please contribute to our international scientific evaluation and provide some information on you filling the boxes of the questionnaire.
Please give data about your body weight in [kg] and height in [cm] at your different age periods, based on your memory, private records ore most preferably medical records, hospital reports, discharge letter etc.
Your date will be handled confidentially, known only by our staff, but because of health regulation we need your signature on a different sheet, as an informed consent.
If you are not sure one of the data, you can leave this box empty.
Year of born: 19_ _ your gender: Male/ Female
|
Recent body weight according to your measurement |
kg |
Recent body heightaccording to your measurement |
cm |
|
Body weight at: 20 years |
|
Body height at |
|
|
30 years |
|
|
|
|
40 years |
|
|
|
|
50 years |
|
|
|
|
60 years |
|
|
|
|
70 years |
|
|
|
| your highest body weight |
kg |
it was measured at the age of _ _ _ years |
|
By FEMALEs Only number of deliveries: last delivery at the age of: year last regular menstruation : at the age of: year |
|
Recent body weight and height measured by the practice staff
|
kg |
|
cm |
| |
|
|
|
|
|
|
Doctors records: : Practice ID:
diagnosed diabetes at the age of: year, none
hypertonia at the age of: year, none
Date: 201_ ___.... _____
Thanks for your contribution Your family physician
References
- Astrup, A. The Healthy lifestyles in Europe: prevention of obesity and type II diabetes by diet and physical activity. Public Health Nutrition 2001;4(2B):499-515. [CrossRef]
- Wadden TA, Tsai AG. Addressing Disparities in the Management of Obesity in Primary Care Settings.
- N Engl J Med. 2020;383(10):977-978. [CrossRef]
- Mozaffarian D, Hao T, Rimm EB Willett WC, Frank B, Hu N: Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men. Engl J Med. 2011;364:2392-2404.
- Patel SR, Hu FB: Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16:643-53.
- Bjerregaard LG, Jensen BW, Ängquist L, Osler M, Sørensen TIA, Baker JL. Change in Overweight from Childhood to Early Adulthood and Risk of Type 2 Diabetes N Engl J Med. 2018;378:1302-12.
- Donini LM, Savina C, Gennaro E, DeFelice MR, Rosano M, Pandolfo MM, DelBalzo V, Cannella C, Ritz P, Chumlea WMC. A systematic review of the literature concerning the relationship between obesity and mortality in the elderly. J Nutr Health Aging. 2012; 16: 89-98. 7. Yu-Cheng Lin, Jong-Dar Chen, Pau-Chung Chen: Excessive 5-year weight gain predicts metabolic syndrome development in healthy middle-aged adults. World J Diabetes. 2011. [Google Scholar]
- Yu-Cheng Lin, Jong-Dar Chen, Pau-Chung Chen: Excessive 5-year weight gain predicts metabolic syndrome development in healthy middle-aged adults. World J Diabetes. 2011;2:8-15.
- Rurik I, Sandholzer H, Kalabay L: Does the dinamicity of weight gain predict the elements of metabolic syndrome? Med Sci Monit. 2009;15(2): CR40-44.
- Jancsó Z, Halmy E, Rurik I: Differences in weight gain in hypertensive and diabetic elderly patients. Primary care study. J Nutr Health Aging. 2012;16: 592-6.
- Kovács E, Jancsó Z, Móczár Cs, Szigethy E, Frese T, Rurik I. Life-long Weight Change can Predict Metabolic Diseases. Exp Clin Endocrinol Diab. 2012;120: 573-8.
- Rurik I, Móczár Cs, Buono N, Frese T, Kolesnyk P, Mahlmeister J, Jancsó Z. Early and menopausal weight gain and its relationship with the development of diabetes and hypertension. An international study on lifelong weight gain and manifestation of metabolic diseases. Exp Clin Endocrinol Diab. 2017;125:241-250.
- Alley DE, Chang VW. Metabolic syndrome and weight gain in adulthood. J Gerontol A Biol Sci Med Sci. 2010; 65:111-7.
- Wagner A, Simon C, Ducimetiere P, Montaye M, Bongard V, Yarnell J, Bingham A, Hedelin G, Amouyel P, Ferrières J, Evans A, Arveiler D. Leisure-time physical activity and regular walking or cycling to work are associated with adiposity and 5 y weight gain in middle-aged men: the PRIME Study. 9: Int J Obes Relat Metab Disord 2001;25, 2001.
- Gordon-Larsen P, Hou N, Sidney S. Fifteen-year longitudinal trends in walking patterns and their impact on weight change. Am J Clin Nutr. 2009;89:19-26.
- Lee IM, Djousse L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. 1: JAMA 2010;303, 2010.
- Juonala M, Magnussen CG, Berenson GS. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876-85.
- Pigeot I, Baranowski T, De Henauw S. and the IDEFICS Intervention Study Group. The IDEFICS intervention trial to prevent childhood obesity: design and study methods. Obes Reviews. 2015;16 (Suppl. 4: 2).
- Bemelmans WJE, Wijnhoven TMA, Verschuuren M, Breda J. Overview of 71 European community-based initiatives against childhood obesity starting between 2005 and 2011: general characteristics and reported effects. BMC Public Health. 2014,14:758 http://www.biomedcentral. 1471.
- Latomme J, Huys N, Cardon G, Morgan PJ, Lateva M, Chakarova N, Kivelä J, Lindström J, Androutsos O, González-Gil EM, De Miguel-Etayo P, Nánási A, Kolozsvári LR, Manios Y, De Craemer M; on behalf of the Feel4Diabetes-study group.Do physical activity and screen time mediate the association between European fathers' and their children's weight status? Cross-sectional data from the Feel4Diabetes-study. Int J Behav Nutr Phys Act. 2019;16:100. [CrossRef]
- Manios Y, Mavrogianni C, Lambrinou CP, Cardon G, Lindström J, Iotova V, Tankova T, Civeira F, Kivelä J, Jancsó Z, Shadid S, Tsochev K, Gallego R, Radó S, Dafoulas G, Makrilakis K, Androutsos O, on behalf of the Feel4Diabetes-study group. Two-stage, school and community-based population screening successfully identifies individuals and families at high-risk for type 2 diabetes: the Feel4Diabetes-study. BMC Endocrine Disorders. 1: 2020;20(Suppl 1), 2020. [CrossRef]
- National Institute for Health and Care Excellence (2015). NICE public health guidance 47: Managing overweight and obesity among children and young people: lifestyle weight management services. Available at https://www.nice.org.uk/guidance/qs94.
- Kliche T, Krüger C, Koch U, Mann R, Goldapp C, Stander V, Töppich J.(2006). Germany: preventive care for obese children and adolescents - qualities and deficiencies of programs and interventions. In A. Mathieson & T. Koller (Hrsg.), Addressing the socioeconomic determinants of healthy eating habits and physical activity levels among adolescents. http://www.euro.who.int/Document/e89375.pdf (S. 43-49). Copenhagen: WHO Regional Office of Europe/HBSC Forum.
- Móczár C, Borgulya G, Kovács E, Rurik I. Could primary care dietary intervention combined with lifestyle changes be effective in the cardiovascular prevention? Acta Alimentaria 2012;41:248– 256. [CrossRef]
- Ocsovszky Z, Martos T, Otohal J, Berényi B, Merkely B, Csabai M, Bagyura Z. Relationship between cardiovascular risk assessment and health behavior in the light of psychosocial factors. Orv Hetil. 2023;164:119-131.
- Reijo Siren R, Eriksson JG, Vanhanen H.Observed changes in cardiovascular risk factors among high-risk middle-aged men who received lifestyle counselling: a 5-year follow-up.Scand J Prim Health Care. 2016;34:336-342. [CrossRef]
- Lucini D, Pagani E, Capria F; Galiano M, Marchese M, Cribellati S, Parati G. Age Influences on Lifestyle and Stress Perception in theWorking Population. Nutrients. 2023, 15, 399. [CrossRef]
- Gómez-Ambrosi, J. Recent Progress in the Management of Obesity. Nutrients. 2023, 15, 2651 ttps://doiorg/103390/ nu15122651. [Google Scholar] [CrossRef]
- Henderson J, Ehlers AP, Lee JM, Kraftson AT, Piehl K, Richardson CR, Griauzde DH. Weight Loss Treatment and Longitudinal Weight Change Among Primary Care Patients With Obesity. JAMA Netw Open. 2024 Feb 5;7(2):e2356183. [CrossRef]
- Counterweight Project Team, McQuigg M, Brown JE, Broom JI, Laws RA, Reckless JP, Noble PA, Kumar S, McCombie EL, Lean ME, Lyons GF, Mongia S, Frost GS, Quinn MF, Barth JH, Haynes SM, Finer N, Haslam DW, Ross HM, Hole DJ, Radziwonik S. Engaging patients, clinicians and health funders in weight management: the Counterweight Programme. Fam Pract. 2008;25-S1:i79-86. [CrossRef]
- NHS-QOF. Available at https://www.england.nhs.uk/wp-content/uploads/2021/03/B0456-update-on-quality-outcomes-framework-changes-for-21-22-.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).