1. Introduction
Clinicians who conduct research whether clinical or fundamental, the so-called physician-scientists, serve as significant research catalysts that propel discovery in academia, government, and industry [
1]. Due to the conjunction of their clinical and research backgrounds, physician-scientists possess a distinctive ability to recognize gaps in medical knowledge that enhance clinical care and overall health outcomes [
2,
3,
4,
5].
Medical institutions play a crucial role in producing physicians, primarily through well-designed medical curricula [
6,
7,
8]. A physician-scientist profession necessitates a significant degree of formal training in scientific research whether clinical or fundamental. Formal research training can occur concurrently with medical curriculum (i.e., completion of a dual-degree MD-PhD program), or after medical school graduation (i.e., completion of a stand-alone Masters or PhD graduate program) [
1,
5,
8,
9,
10,
11,
12,
13].
Physician-scientists can establish an environment that fosters interest in a career that merges clinical care with research by serving as role models and inspiring students or other residents who may not possess significant prior research exposure. Additionally, it is important to offer a profound involvement in the quotidian aspects of the scientific realm, conviction in the significance of one’s endeavors, and ardor, while stimulating students’ for a challenge through active engagement in research activities [
14,
15,
16]. Most importantly, research forms an integral part of the CanMEDS framework, contributing to the development and maintenance of physicians across all roles [
17]. By staying current with advancements, critically evaluating information, applying new knowledge, and collaborating effectively, physicians can provide the highest quality care to their patients and contribute to a better healthcare system overall [
18,
19,
20,
21].
The physician-scientist workforce is suffering from dwindling figures [
8,
10,
11,
22,
23,
24,
25,
26,
27,
28] due to challenges of reduced funding, increased clinical and teaching obligations, prolonged curricular duration, excessive regulation, and the allure of more financially stable and profitable opportunities in the private health industry [
26,
29,
30,
31]. Therefore, it is imperative to develop enhanced methodologies for the recruitment and sustenance of a physician-scientist workforce that is diverse, equitable, adaptable, and resilient, throughout all phases of their careers. Undoubtedly, the pandemic serves as a poignant reminder that the forthcoming generation of doctors must receive comprehensive training in medicine, with an eye toward developing talent that can bridge the gap between science and medicine [
27,
31,
32,
33,
34].
The healthcare and research infrastructure in low- and middle-income countries (LMICs) suffer from socioeconomic instability, including inflation and political unrest [
35,
36,
37]. For instance, Lebanon is already burdened with an insufficient allocation of financial resources for the healthcare system thus limiting the flow of resources to medical research and development [
38,
39,
40]. Besides, the establishment of a stable physician scientist workforce is prevented by institutional challenges such as the lack of formal research roles and insufficient incorporation of research training into medical curricula. This is the case across LMICs where research is generally viewed as a peripheral activity, not as an integrated component of clinical practice. Nonetheless, research on physician-scientist training and medical research challenges within the Middle East, particularly Lebanon, remains limited in global literature.
A peculiar aspect of medical research in LMICs is that priorities are dictated by the interests of high-income countries and clinical trials by foreign institutions tend to target diseases that do not necessarily reflect the local healthcare needs of LMICs [
41,
42,
43]. This further perpetuates their underrepresentation in the global research agenda. Additionally, research capacity constraints are manifested in various ways; for example, lack of mentorship, limited training opportunities in advanced research techniques, and lack of institutional support [
44,
45,
46]. Although partnerships between high-income countries and LMICs on the training of researchers are valuable, they are conducive to ’brain drain’ because trained researchers tend to relocate to countries with better work conditions [
37,
45] – a trend that has been especially prominent in Lebanon across generations.
Despite these adversities, the importance of physician-scientists remains paramount. Crucially, there is a widespread lack of comprehensive understanding regarding their professional status and the major hurdles they face. Therefore, efforts to assess and support the physician-scientist community in such countries become increasingly crucial. Their involvement in research has the potential to positively shape the education and development of future physicians, fostering a culture of inquiry and ultimately advancing the quality of healthcare in the long run.
The study will utilize a survey to examine the challenges that physicians and residents have in incorporating research into their careers and medical student education, as well as the potential solutions to overcome these obstacles. The findings of this research will also contribute to a better understanding of the role of medical research in shaping the education and development of future physicians at one of Lebanon’s central university hospitals and highlight areas for improvement. Ultimately, the study seeks to foster a more seamless integration of research into the healthcare profession and medical education.
2. Materials and Methods
The Ethical considerations
All methodologies employed for data collection adhered to ethical standards, guaranteeing participant privacy, confidentiality, voluntary and informed participation, and prioritizing the well-being of individuals involved. The research team explicitly informed the targeted demographic that they possessed the right to choose whether or not to participate in the survey without encountering any repercussions. Additionally, participant identities were safeguarded throughout the entire data collection, analysis, and dissemination phases by abstaining from the collection of email addresses. The securely stored data resides on the researchers’ password-protected computers, with exclusive access restricted to the research team. Upon manuscript publication, a predetermined process mandates the deletion of all collected data. The study underwent thorough scrutiny and received approval from the Hotel Dieu de France Research Ethics Board (reference number: CEHDF file 2231), aligning with the principles of the Declaration of Helsinki.
Study design, setting and participants
This prospective, cross-sectional study surveyed the attending physicians and residents (from R1 till R5) of one of Lebanon’s central university hospitals, CHU Hotel-Dieu de France. The targeted population belonged to 34 medical departments: Anesthesiology and Reanimation, Cardiology, Dermatology, Emergency, Endocrinology and Metabolic Diseases, Family Medicine, Gastroenterology, General Surgery, Gynecology and Obstetrics, Hematology-Oncology, Infectious Diseases, Internal Medicine, Nephrology, Neurology, Neurosurgery, Oncology, Ophtalmology, Orthopedic Surgery, Otorhinolaryngology, Pathology, Pediatrics, Pediatric Surgery, Plastic and Maxillofacial Surgery, Plastic and Reconstructive Surgery, Psychiatry, Pulmonology, Pulmonology and Critical Care, Radiology, Radiotherapy, Rheumatology, Thoracic and Cardiovascular Surgery, Thoracic and Vascular Surgery, Urology, and Vascular Surgery.
The study survey was constructed to address knowledge gaps pertaining to physician-scientists in the target hospital as representative of Lebanon in general. It also aimed at identifying the impediments and prospects for physician-scientists, which serves as a basis for devising tactics to surmount obstacles and establish conducive surroundings. Furthermore, it aimed at acknowledging the influence of physician-scientists on medical education, promoting a climate of inquiry and incorporating research into curricula.
Questionnaire validation and data collection
The questionnaire was established based on an extensive literature review of previously published studies and its design drew on established frameworks and themes commonly used in medical education and physician-scientist research studies [
47,
48,
49,
50]. First, face validity was established by consulting a panel of ten experts in medical research and education, who reviewed the survey for clarity, relevance, and appropriateness of the content using a 4-point scale. The experts were eight physician-scientists, one professor in physiology, and one statistician, all of whom had more than ten years of experience in their respective fields. Then, to ensure content validity, the same experts assessed the comprehensiveness of the items, and the Lawshe Content Validity Ratios (CVR) were calculated for each item, achieving values of 0.8 and higher, and a Content Validity Index (CVI) value was drawn for the overall instrument, achieving a value of 0.976, indicating strong agreement among the experts. The internal consistency or reliability coefficient of the survey was verified, and Cronbach’s alpha was 0.72 which was considered reliable.
The survey consisted of 24 close-ended questions and statements regarding research involvement and one open-ended question (Supplemental data 1). The first 24 could be answered with provided multiple choice options or a five-point Likert agreeability scale. The first five questions assessed population demographics and medical specialties. The second 12 questions probed participants on the importance of research in medical practice, reasons for its significance in the medical field, personal research engagement frequency, views on ideal research frequency for medical doctors, encouragement of student research, staying current with research, collaboration with other researchers, and perspectives on how medical research enhances patient care. Additionally, participants were asked to identify valuable types of research, express views on incorporating research into the education of future physicians, and whether it should be mandatory. Furthermore, questions 18-20 explored the challenges in medical research for doctors, the integration of medical research into the education curriculum, and gathered opinions on the preparedness of medical education for clinical research. The last 4 questions looked at suggested measures for time constraints in medical research, solutions for limited funding, insights on overcoming challenges in accessing data/resources for research, and strategies for integrating medical research into education.
The survey concluded with one freeform open-ended question inviting the participants to share their thoughts on how best to overcome the obstacles in fostering a research culture among physicians.
Primary data was collected using Google Forms specifically for the research paper, and no secondary data was generated or used. The digital questionnaire was distributed by email by the primary investigators through the faculty of medicine departmental office. Once completed, all questionnaires were submitted to the primary investigators and anonymous data containing no identifiers was used for secondary analysis.
Sample size
Physicians (per 1,000 people) in Lebanon were reported at 2.617 in 2019, according to the World Bank collection of development indicators, compiled from officially recognized sources. However, since fall of 2019 doctors have been leaving the country at an alarming rate reaching up to 40% [
38,
51,
52,
53]. Based on this, the number of physicians was estimated at around 8000 with 2000 residents. The number of residents and physicians in CHU Hotel-Dieu de France is 450. Cochran’s sample size formula was used to calculate the necessary population size representative of the Lebanese physicians.
n = N.Z2.p.(1-p) / (N-1).E2 + Z2.p.(1-p)
Where: n is the required sample size; N is the population size; Z is the Z-score corresponding to the desired confidence level; p is the estimated proportion of the population with the characteristic of interest; E is the desired margin of error.
Given: Confidence level (Z): 90%, corresponding to a Z-score of 1.645; Confidence interval (E): 0.06; Population size (N) of physicians and residents in the hospital: 450; Estimated proportion of physicians who do research (p): 10%. The latter proportion was averaged as compared to US and Chinese physician scientists percentages [
10,
54,
55].
Therefore, the required sample size was calculated to be approximately 59 doctors to obtain a representative sample of the physician scientists’ population in Lebanon. The low-limit confidence level was used since we frame this study as a preliminary insight into an understudied area, providing a focused exploration of physician-scientist challenges within this institution as a representative case study for similar Lebanese contexts.
Statistical analysis
The statistical analysis was conducted using IBM SPSS Statistics version 25.0. Initially, descriptive statistics were performed, presenting all variables using frequencies and percentages. Subsequently, the chi-square test was employed to assess potential associations between participants’ opinions on the importance of research in physician’s practice and other factors assessed in the questionnaire. A p-value of less than 0.05 was considered statistically significant.
Since the questionnaire has categorical data, Multiple Correspondence Analysis (MCA) was then performed to explore the importance of medical research perceived by medical doctors, as well as challenges faced by them in conducting research, and the perceived benefits and improvements that could enhance research integration within medical practice and education. To reduce the dimensionality of the categorical survey data, MCA was performed on the dataset. This method was chosen to highlight relationships between different categories and dimensions, enabling us to identify which variables (challenges, benefits, or improvement strategies) contributed most to variations in the responses. The analysis yielded multiple dimensions, each explaining a portion of the variance in the dataset. To arrange the data for MCA, each categorical response was transformed into a suitable format, where binary coding was applied to each possible answer in the multiple-choice responses. R software (R4.4.1) was used with the Multivariate Exploratory Data Analysis and Data Mining (FactoMineR) and: Extract and Visualize the Results of Multivariate Data Analyses (factoextra) packages.
3. Results
3.1. Characteristics of the Participants
A total of seventy-eight physicians (n=78) participated in the survey, of whom 65.4% (n=51) were between 22 and 44 years old, 61.5% (n=48) were male, 41.0% (n=32) were residents, and 59.0% (n=46) completed their residency program in Lebanon. Further details regarding participant characteristics are provided in
Table 1.
3.2. Importance and Impact of Research in the Medical Field and in the Training of Future Doctors
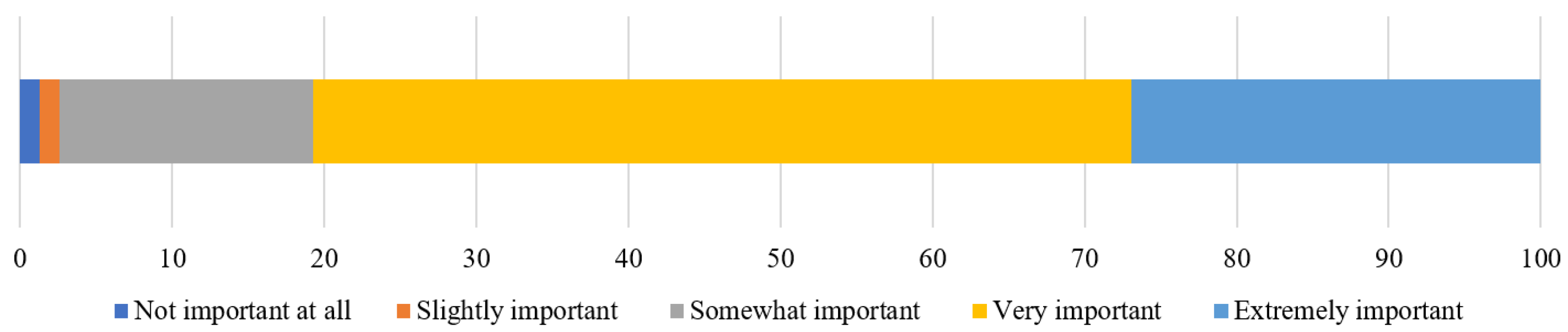
When asked about the importance of medical research in their own practice, 80.7% of participants (n=63) considered it to be very or extremely important (
Figure 1).
Participants’ responses on the impact of research on the medical field are presented in
Table 2. Regarding the reasons that make research important in the medical field, 91.0% considered that it improves patient care and outcomes (n=71), and 88.5% stated that it advances scientific knowledge (n=69). More than 80% of participants considered that medical research improves patient care through informing evidence-based guidelines, enhancing diagnostic accuracy, and identifying new treatment options. Clinical research was considered by 94.9% (n=74) of participants as the type of research providing the highest value in the medical field.
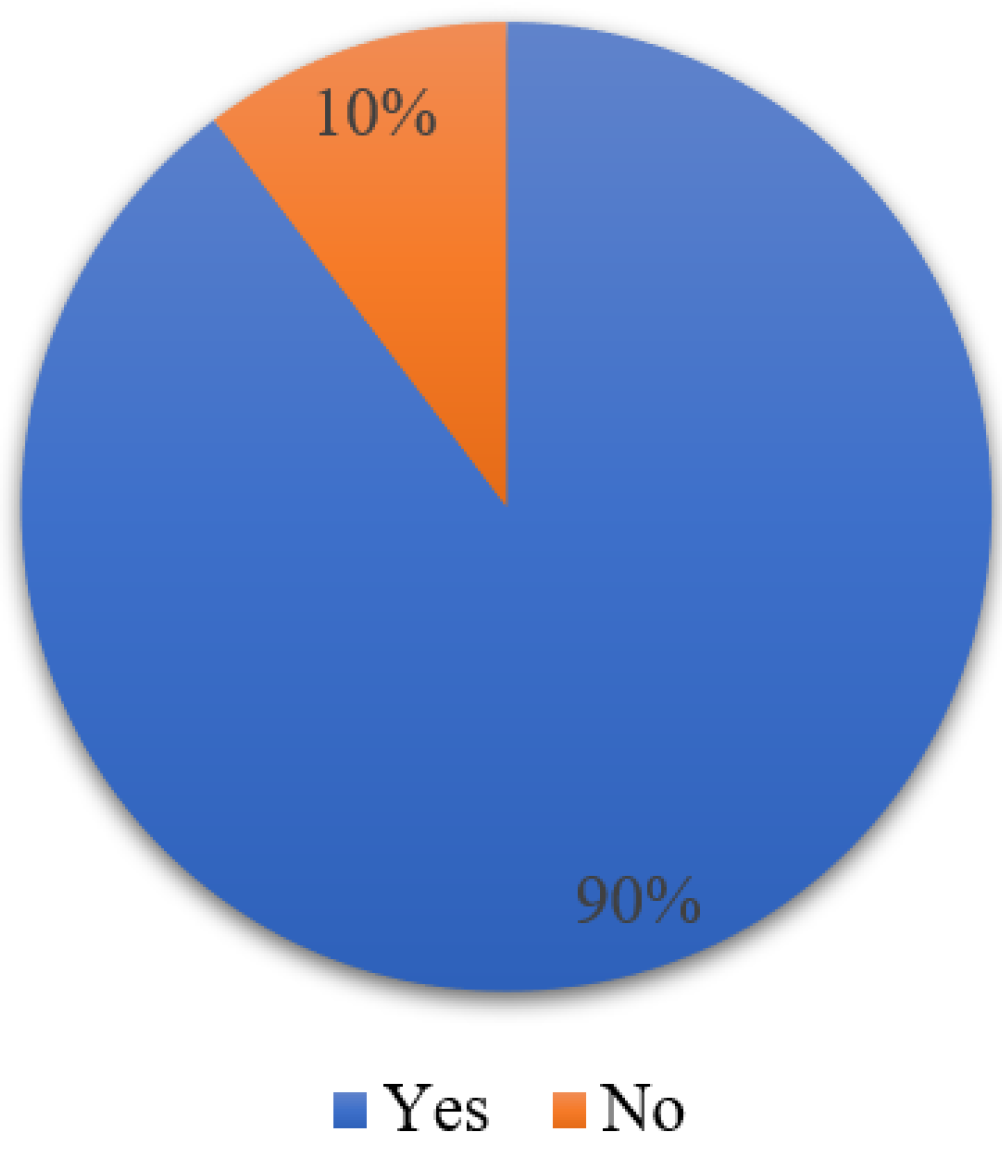
Eighty-nine-point seven percent of physicians (n=70) reported that medical research should be a mandatory part of medical education (
Figure 2).
3.3. Frequency of Medical Research
With regard to questions on the frequency of medical research (
Table 3), 38.5% reported practicing research continuously (n=30), and 20.6% conduct research only if recommended or when mandated. Eighty-three-point four percent encourage their students to conduct research regularly or constantly (n=65), and 76.9% stay up-to-date with research being conducted in their field (n=60).
3.4. The Challenges of Integrating Research into Medical Training and Practice
As for the integration of medical research into the medical education curriculum, 50.0% considered it moderately well-integrated (n=39), and 35.9% somewhat well-integrated (n=28), with only one participant considering it extremely well-integrated. Furthermore, only 12.8% of participants considered themselves to be well or extremely well-prepared to conduct medical research through the education they received (
Table 4).
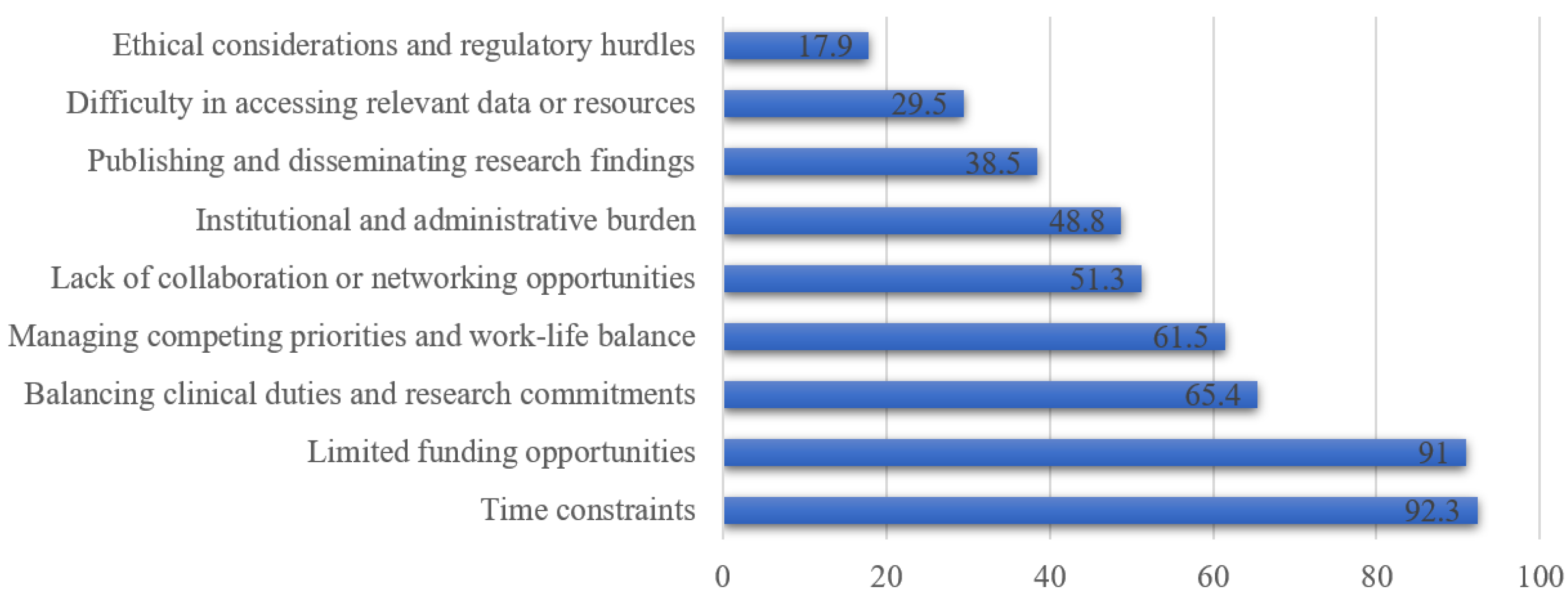
With regard to obstacles impeding optimum research achievements (
Figure 3), time constraints (92.3%, n=72), limited funding opportunities (91.0%, n=71), and difficulties in balancing clinical duties and research commitments (65.4%, n=51) were considered the main obstacles.
3.5. Solutions to Improve Medical Research and Its Integration into the Curriculum
Participants were also asked about solutions aiming to improve medical research. Eighty-seven-point two percent (n=68) and 78.2% (n=61) considered that providing dedicated research staff and encouraging collaboration between clinicians and researchers are measures that alleviate time constraints for medical doctors involved in research, respectively. As for funding constraints, 87.2% of participants (n=68) and 64.1% (n=50) considered that these can be mitigated by seeking grants or scholarships from international foundations and seeking private sector investments, respectively. Difficulty in accessing relevant data or resources for medical research can be overcome through the establishment of centralized research databases or repositories (74.4%, n=58), improvement of intra- and inter-institutional data sharing (73.1%, n=57), and other strategies presented in
Table 5. Furthermore, solutions to improve the integration of medical research into the medical education curriculum were also identified as presented in
Table 5.
Additional suggestions for improving the research culture among physicians were highlighted in the open-ended question. Participants stressed the need to integrate research early in medical training, to replace non-medical credits with research-oriented courses, and to provide structured educational programs on research methodologies. Institutional support is also vital, suggested by the creation of research support units, the motivation and valorization of research efforts, and the formation of dedicated research teams. Other recommendations included the importance of teamwork, effective time management, rewarding research results and ensuring adequate funding. The consensus underlined the essential role of institutional support and resource provision in fostering a dynamic research environment within the medical community.
3.6. Elements Associated with the Perception on the Importance of Research in the Physician’s Practice
Table 6 shows that the more researchers perceive research as important in their practice, the more frequently they practice it and the more they recommend it to their students (p<0.05). In fact, 46.6% (n=29) of the participants considering research as very or extremely important regularly do research versus only 6.7% of those giving less importance to research (n=1). Furthermore, 88.9% of physicians perceiving research as very or extremely important regularly or constantly recommend it to their students (n=56) versus 60% of those granting less importance to research (n=9).
3.6. Factors Influencing Research Engagement Among Physicians: An MCA Analysis
MCA was conducted to identify key dimensions explaining variability in respondents’ answers by reducing the dimensionality of the categorical data. Eigenvalues were used to select the first two dimensions, which captured the majority of the variance. Each dimension represents patterns in respondents’ research engagement, with high-contributing categories analyzed in terms of research frequency, importance, and collaboration. Variable coordinates and contributions were calculated to reveal clusters of respondents.
The first two dimensions of the MCA explained 15.28% of the total variance, with Dimension 1 accounting for 9.43% and Dimension 2 for 5.85%. Dimension 1 distinguished respondents based on research engagement, with low involvement marked by categories like “Never conduct research” and “Research is not important,” while frequent researchers clustered separately. Dimension 2 captured differences in collaboration and barriers, with infrequent collaborators and those facing time constraints contributing positively. Two clusters emerged: Cluster 1, composed of research-active, frequent collaborators with fewer barriers, and Cluster 2, including less engaged participants facing more obstacles like time constraints and lack of funding. Research frequency and importance influenced Dimension 1, while collaboration and barriers shaped Dimension 2.
4. Discussion
The confluence of clinical practice and biomedical research has long been fertile ground for advances in patient care and medical knowledge. At the heart of this intersection are physician-researchers, whose dual role enables them to translate complex research findings into tangible clinical applications. However, the path to becoming a physician-scientist and subsequent research practice is fraught with pitfalls, especially in developing countries. Our study highlights for the first time the essential role of medical research in improving patient care and advancing knowledge in Lebanon. It reveals key challenges, including time restrictions and funding shortfalls, and suggests methods for strengthening the integration of research into medical education. More importantly, the perceived value of research has a positive impact on its incorporation into clinical practice and education, highlighting the crucial need for systemic support and innovation in medical education and practice.
Positioning this study as both foundational and regionally relevant, we suggest that while the findings align with global literature, they uniquely highlight Lebanon’s physician-scientist landscape, shaped by recent economic and systemic pressures. To the best of our knowledge, this is the first study conducted in Lebanon focusing on these barriers. Existing studies may not fully capture Lebanon-specific challenges, such as intense funding constraints exacerbated by ongoing crises, and we aimed to provide a foundation for understanding these dynamics.
Echoing the literature [
1,
2,
3,
4,
5], our study affirms the indispensable role of physician-scientists in translating research into meaningful clinical advances and underline the widespread recognition among Lebanese physicians of the intrinsic value of research. Surprisingly, despite the multifaceted crisis engulfing Lebanon [
38,
39,
40,
51,
52], the physicians recognized the importance of medical research at a high percentage emphasizing their resilience and dedication even in times of profound instability. The study also highlights the quality of the educational system at the country’s leading medical schools, which seems to instill a deep appreciation of the role of research in advancing medical science and patient care. This result is particularly remarkable when juxtaposed with the literature, which often correlates research output and attitudes towards research with the stability and funding opportunities present in a country [
10,
54,
56,
57,
58,
59]. It further suggests that with a stable environment and adequate funding similar to that of developed countries, Lebanon could potentially achieve remarkable research results.
More importantly, the results of our study emphasize for the first time the value of research in the training of future physicians, albeit without being in an MD-PhD training context. In fact, most of the literature focuses on MD-PhD programs and their improvement without emphasizing the critical importance of research for MD students [
6,
7,
8,
12]. In addition, early exposure to research can also encourage MD students to pursue careers that combine clinical practice with scientific research, thereby maintaining the vital pipeline of physician-scientists. Such integration not only prepares medical students for the complexities of modern healthcare, but also equips them with the tools needed for lifelong learning and contribution to the advancement of medicine.
Most participants favored clinical research as essential, indicating a trend within the Lebanese medical community that may apply globally. This preference doesn’t lessen basic research’s value but suggests combining it with applied and translational research could hasten lab discoveries into clinical practice, enhance treatment innovation, and improve patient outcomes. As for the practical commitment to research, the study highlighted a positive attitude, with remarkably high figures of up to 60%. This trend is particularly noteworthy and in sharp contrast to the global biomedical research landscape, which has undergone profound transformations, particularly in terms of funding dynamics. For example, the percentage of US physicians declaring research as their main professional activity declined from 1.6% in 2011 to 1.3% in 2020 [
32,
34,
54]. A similar decline in the number of physician-researchers is noted in several developed countries [
22,
60,
61,
62,
63], whereas medical research in developing countries has experienced a notable boom in recent decades, marked by increased investment in the development of medical research. However, this positive trend is not universal in all developing countries [
9,
23,
57,
58,
64,
65].
Physician-scientist careers are fraught with significant challenges, in both developed and developing countries. These obstacles, ranging from financial and time constraints to a lack of adequate preparation, have been widely documented in the literature [
7,
9,
22,
24,
66,
67,
68]. Our study underlines these persistent challenges and a moderate integration of research into medical education, highlighting insufficient preparation of physicians to fully embrace research careers. Most importantly, the uniqueness of Lebanon’s socio-economic and political factors due to economic crises and currency devaluation inflicts significant strain and instability on the healthcare system as well as research and medical education. These factors restrict healthcare funding, which limits the allocation of resources for research initiatives. Besides, these instabilities have severely impacted medical students’ education in both public and private universities, limiting access to essential resources, increasing tuition burdens, and reducing opportunities for practical training and research due to strained institutional budgets. Furthermore, the outmigration of skilled professors (brain drain) further diminishes research capacity, as trained physician-scientists seek opportunities in more stable environments.
In developed countries, physician-scientists face increased pressure due to extended training periods and the difficulty of balancing clinical duties with research commitments. These challenges are exacerbated by major financial barriers, including the burden of student debt and competition for limited funding [
7,
68]. On the other hand, developing countries, as in our case, face unique challenges in developing physician-scientists. The dearth of structured, supervised research training for medical students and early-career physicians hinders research output and physician-scientist training [
9]. These barriers are exacerbated by the prohibitive costs of establishing biomedical research laboratories and inadequate remuneration for those who choose the research path, making it a less attractive career compared to clinical opportunities [
66].
Facing the recurring challenges that physician-scientists encounter, our study highlights pragmatic solutions to overcome these obstacles and improve the integration of medical research into the academic curriculum. The establishment of a supportive environment with dedicated research support staff and encouragement for collaboration between clinicians and researchers are widely endorsed, suggesting that these measures could significantly alleviate the time constraints on physicians engaged in research as previously highlighted [
68]. Furthermore, seeking grants or scholarships from international foundations and looking for private sector investments are seen as viable solutions to address financial limitations. The creation of centralized databases and the improvement of intra- and inter-institutional data sharing are also emphasized as effective means to facilitate access to necessary resources for medical research. To these solutions can be added the establishment of a network including non-profit, academic, and clinical institutions that could advocate for faculty support, and funding opportunities throughout the career [
32,
69,
70].
To further tailor the proposed solutions within Lebanon’s context, research funding recommendations should consider leveraging alternative financing sources, such as partnerships with local non-governmental organizations and regional collaborations with Middle Eastern academic institutions. Another potential approach involves community-based participatory research, where local communities and stakeholders are engaged in setting research priorities, ensuring that medical studies directly address local health needs and enhance community support for research initiatives [
45,
46,
71]. Encouraging private sector engagement and philanthropic support from the Lebanese diaspora could further create alternative funding channels in light of limited government budgets. Also, expanding the recommendation for mentorship programs within Lebanon’s medical schools would also help to sustain research interest despite economic pressures [
72]. These programs could be supported by international partnerships with institutions in LMICs facing similar socio-economic issues, allowing for an exchange of knowledge and resources that reflect shared challenges and innovative, context-specific solutions.
Most importantly, our study points out a critical issue relevant worldwide: the inadequate integration of research in medical education, underscoring the importance of early and continuous research initiatives in training programs. Introducing MD-PhD or residency-PhD programs could enhance the research culture, but developing countries face two main challenges: motivating medical students for research and ensuring the availability of necessary infrastructure. The lack of early research exposure and formal MD-PhD programs in regions like the Middle East leads students to pursue PhDs post-MD, which is less ideal for those aiming to merge clinical practice with research due to the lengthy commitment and potential clinical skill stagnation [
9,
57,
58,
64]. Furthermore, the financial burden of PhD programs necessitates solutions like loan repayment schemes and sufficient financial aid.
Finally, a positive correlation was found between doctors’ valuing of research and their involvement in research activities, as well as their encouragement of students to follow this path. This clearly indicates the impact of the perception of research on its integration into medical practice and teaching. So, to revitalize the career path of physician-researchers, a comprehensive strategy is essential. This strategy involves fostering immersive research experiences as part of medical training, alleviating financial barriers through initiatives such as debt-free education and living wages, emphasizing the role of educators and mentors, and establishing a strong network for physician-scientists that spans the non-profit, academic and clinical sectors. Such a network is essential to promote curriculum improvement, faculty support and access to funding at all stages of a physician-scientist’s career. The aim is to train a new wave of physician-scientists who are not only diverse and dedicated to advancing biological knowledge, but also deeply committed to research and patient care. Furthermore, the MCA underscored the importance of addressing the structural challenges that prevent greater research participation. Interestingly, certain variables, such as the importance of research in practice and the frequency of collaborative activities, exhibited low variance. This indicates a strong consensus among participants, suggesting that medical professionals overwhelmingly recognize the importance of research and actively engage in collaborative work. The low variability in these responses simplifies the interpretation of the data and affirms that the participants are aligned with current best practices in medical research. Moreover, this uniformity reflects the standardization of research values and practices across the institution, which aligns with the goals of promoting evidence-based medicine.
A drawback of this study is that it relies on self-reported responses, which may add bias owing to social desirability or recollection errors. Furthermore, while the study’s cross-sectional approach gives a picture of physician-scientists’ present opinions and concerns, it does not allow for the assessment of long-term changes or the establishment of causal links. The use of a low confidence level of 90% instead of alternative sample size estimates, such as the most common 95% confidence level (for broader or national samples) is also a limitation. Nevertheless, while conducted at a single center, the study encompassed a broad range of specialties across 34 departments, capturing a diverse representation of Lebanon’s physician-scientist population. Besides, with the lack of centralized data for hospitals in Lebanon, the 10% estimate for physicians who conduct research might be an overestimation since very few hospitals in Lebanon have embedded medical research, even less with the ongoing war and crisis, which might compensate the low confidence level in the sample size calculation. Given the limited data on physician-scientist challenges in Lebanon, we frame this study as a preliminary insight into an understudied area, laying the groundwork for larger, multi-center studies to produce more generalizable results. This is especially relevant for Lebanon, where physician emigration and research funding limitations create a context distinct from other regions.
5. Conclusions
This study underscores the vital role of physician-scientists in healthcare innovation and medical knowledge advancement, highlighting the link between doctors’ appreciation for research and their promotion of it among students. Despite challenges like training, funding, and balancing duties, especially in crisis-hit Lebanon, doctors still highly value medical research. Our research suggests pragmatic solutions to these issues, including early integration of research into medical curricula, support structures, financial aid, and better access to research resources. These strategies aim to foster a new generation of physician-researchers equipped to address global health challenges and enhance medical knowledge and patient care.
6. Strengths and Future Work
This study has several strengths. It is one of the first to explore physician-scientist challenges within Lebanon, offering a foundational analysis that underscores the role of socio-economic factors in shaping the physician-scientist landscape. The inclusion of diverse specialties across a central university hospital contributes to a broad understanding of these challenges, even within a single-center study.
For future work, a multi-center study is recommended across various hospitals in Lebanon to increase the sample size and enhance generalizability. Expanding the study would allow for a deeper exploration of barriers and solutions applicable across different institutional settings. Additionally, longitudinal studies could provide insights into how evolving socio-political factors impact the physician-scientist pipeline in Lebanon. Finally, establishing a formal network of physician-scientists in Lebanon, potentially in collaboration with international bodies, could offer long-term solutions to sustain research careers despite economic and systemic challenges.
Author Contributions
YS: conceptualized and designed the study, collected data, conducted the analyses, prepared the first and revised drafts of the article. MM: conducted the statistical analyses, prepared the first draft of the article. EN: supervised the study, approved the final draft. NF: conceptualized and designed the study, supervised the study, revised the first draft of the article and approved the final one.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Hotel Dieu de France (protocol code CEHDF file 2231; 07/11/2023).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon reasonable request.
Acknowledgments
The authors would like to acknowledge all the participants in this survey.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ologunde, R.; Di Salvo, I.; Khajuria, A. The CanMEDS Scholar: The Neglected Competency in Tomorrow’s Doctors. Adv Med Educ Pract 2014, 5, 383–384. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.R. The Role of the Physician-Scientist in Our Evolving Society. Rambam Maimonides Med J 2011, 2, e0063. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.A. Physician-Scientists: The Bridge between Medicine and Science. Am J Respir Crit Care Med 2012, 185, 595–596. [Google Scholar] [CrossRef] [PubMed]
- Varki, A.; Holmes, E.; Yamada, T.; Agre, P.; Brenner, S. Physician-Scientists Are Needed Now More than Ever. Nature 2006, 440, 740. [Google Scholar] [CrossRef]
- Harding, C.V.; Akabas, M.H.; Andersen, O.S. History and Outcomes of 50 Years of Physician-Scientist Training in Medical Scientist Training Programs. Acad Med 2017, 92, 1390–1398. [Google Scholar] [CrossRef]
- Permar, S.R.; Ward, R.A.; Barrett, K.J.; Freel, S.A.; Gbadegesin, R.A.; Kontos, C.D.; Hu, P.J.; Hartmann, K.E.; Williams, C.S.; Vyas, J.M. Addressing the Physician-Scientist Pipeline: Strategies to Integrate Research into Clinical Training Programs. J Clin Invest 2020, 130, 1058–1061. [Google Scholar] [CrossRef]
- Ganetzky, R.D. Becoming a Physician-Scientist: A View Looking Up From Base Camp. Acad Med 2017, 92, 1373–1374. [Google Scholar] [CrossRef]
- Dos Santos Rocha, A.; Combescure, C.; Negro, F. The MD-PhD Program in Geneva: A 10-Year Analysis of Graduate Demographics and Outcomes. BMC Med Educ 2020, 20, 425. [Google Scholar] [CrossRef]
- Anwer, L.A.; Anwer, A.N.; Mahmood, M.; Abu-Zaid, A.; Shareef, M.A. Meeting the Global Need for Physician-Scientists: A Middle Eastern Imperative. Med Educ Online 2014, 19, 26138. [Google Scholar] [CrossRef]
- Garrison, H.H.; Ley, T.J. Physician-Scientists in the United States at 2020: Trends and Concerns. FASEB J 2022, 36, e22253. [Google Scholar] [CrossRef]
- Brass, L.F.; Akabas, M.H. The National MD-PhD Program Outcomes Study: Relationships between Medical Specialty, Training Duration, Research Effort, and Career Paths. JCI Insight 2019, 4, e133009. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Rocha, A.; Scherlinger, M.; Ostermann, L.; Mehler, D.M.A.; Nadiradze, A.; Schulze, F.; Feldmeyer, L.; de Koning, M.; Berbecar, V.T.; Buijs, R.; et al. Characteristics and Opinions of MD-PhD Students and Graduates from Different European Countries: A Study from the European MD-PhD Association. Swiss Med Wkly 2020, 150, w20205. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.K.W.; Wollny, K.; Twilt, M.; Walsh, C.M.; Bright, K.; Dimitropoulos, G.; Pires, L.; Pritchard, L.; Samuel, S.; Tomfohr-Madsen, L. Curricula, Teaching Methods, and Success Metrics of Clinician-Scientist Training Programs: A Scoping Review. Acad Med 2022, 97, 1403–1412. [Google Scholar] [CrossRef]
- Ommering, B.W.C.; van Blankenstein, F.M.; Waaijer, C.J.F.; Dekker, F.W. Future Physician-Scientists: Could We Catch Them Young? Factors Influencing Intrinsic and Extrinsic Motivation for Research among First-Year Medical Students. Perspect Med Educ 2018, 7, 248–255. [Google Scholar] [CrossRef]
- Lefkowitz, R.J. Inspiring the next Generation of Physician-Scientists. J Clin Invest 2015, 125, 2905–2907. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.J.; Fresquez, A.M.; Christophers, B. Success and the next Generation of Physician-Scientists. J Clin Transl Sci 2020, 4, 477–479. [Google Scholar] [CrossRef]
- Thoma, B.; Karwowska, A.; Samson, L.; Labine, N.; Waters, H.; Giuliani, M.; Chan, T.M.; Atkinson, A.; Constantin, E.; Hall, A.K.; et al. Emerging Concepts in the CanMEDS Physician Competency Framework. Can Med Educ J 2023, 14, 4–12. [Google Scholar] [CrossRef]
- Solaja, O.; Skinner, T.A.A.; McGregor, T.B.; Siemens, D.R. CanMEDS Scholars: A National Survey on Urology Residents’ Attitudes towards Research during Training. CUAJ 2017, 12, E191-6. [Google Scholar] [CrossRef]
- Koo, J.; Bains, J.; Collins, M.B.; Dharamsi, S. Residency Research Requirements and the CanMEDS-FM Scholar Role: Perspectives of Residents and Recent Graduates. Can Fam Physician 2012, 58, e330–e336. [Google Scholar]
- Babenko, O.; Gruneir, A. Fostering Collaborative Research Culture Through Research Development Rounds. J Contin Educ Health Prof 2022, 42, 4–4. [Google Scholar] [CrossRef]
- Kohlert, S.; Zuccaro, L.; McLean, L.; Macdonald, K. Does Medical School Research Productivity Predict a Resident’s Research Productivity during Residency? J Otolaryngol Head Neck Surg 2017, 46, 34. [Google Scholar] [CrossRef] [PubMed]
- Husain, M. Why the next Generation of UK Clinician Scientists Is under Threat. Brain 2021, 144, 3277–3278. [Google Scholar] [CrossRef] [PubMed]
- Adefuye, A.O.; Adeola, H.A.; Bezuidenhout, J. The Physician-Scientists: Rare Species in Africa. Pan Afr Med J 2018, 29, 8. [Google Scholar] [CrossRef] [PubMed]
- Morel, P.A.; Ross, G. The Physician Scientist: Balancing Clinical and Research Duties. Nat Immunol 2014, 15, 1092–1094. [Google Scholar] [CrossRef]
- Abu-Zaid, A. The Endangered Clinician-Investigator Profession in Saudi Arabia: Curricular Attention Is Required. Ann Saudi Med 2018, 38, 69–70. [Google Scholar] [CrossRef]
- Abu-Zaid, A.; Altinawi, B. Perceived Barriers to Physician-Scientist Careers among Female Undergraduate Medical Students at the College of Medicine - Alfaisal University: A Saudi Arabian Perspective. Med Teach 2014, 36 Suppl 1, S3-7. [Google Scholar] [CrossRef]
- Wade, C. Physician-Scientists in the Era of COVID-19: Gone but Not Forgotten. Acad Med 2021, 96, e5–e6. [Google Scholar] [CrossRef]
- Mukesh, K. Jain, Tadataka Yamada and Robert Lefkowitz Opinion | We Need More Doctors Who Are Scientists (Published 2019). Available online: https://www.nytimes.com/2019/09/23/opinion/doctor-scientist-medical-research.html (accessed on 25 June 2023).
- Noble, K.; Owens, J.; André, F.; Bakhoum, S.F.; Loi, S.; Reinhardt, H.C.; Tuveson, D.; Swanton, C. Securing the Future of the Clinician-Scientist. Nat Cancer 2020, 1, 139–141. [Google Scholar] [CrossRef]
- Ballios, B.G.; Rosenblum, N.D. Challenges Facing Physician Scientist Trainees: A Survey of Trainees in Canada’s Largest Undergraduate and Postgraduate Programs in a Single Centre. ClinInvestMed 2014, E268–E283. [Google Scholar] [CrossRef]
- NIHR Progressing UK Clinical Academic Training in 2020: Addressing the Challenges of COVID-19. Available online: https://www.nihr.ac.uk/documents/progressing-uk-clinical-academic-training-in-2020-addressing-the-challenges-of-covid-19/24958 (accessed on 25 June 2023).
- Williams, C.S.; Rathmell, W.K.; Carethers, J.M.; Harper, D.M.; Lo, Y.M.D.; Ratcliffe, P.J.; Zaidi, M. A Global View of the Aspiring Physician-Scientist. Elife 2022, 11, e79738. [Google Scholar] [CrossRef]
- Kliment, C.R.; Barbash, I.J.; Brenner, J.S.; Chandra, D.; Courtright, K.; Gauthier, M.C.; Robinson, K.M.; Scheunemann, L.P.; Shah, F.A.; Christie, J.D.; et al. COVID-19 and the Early-Career Physician-Scientist. Fostering Resilience beyond the Pandemic. ATS Sch 2020, 2, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Salata, R.A.; Geraci, M.W.; Rockey, D.C.; Blanchard, M.; Brown, N.J.; Cardinal, L.J.; Garcia, M.; Madaio, M.P.; Marsh, J.D.; Todd, R.F. U.S. Physician-Scientist Workforce in the 21st Century: Recommendations to Attract and Sustain the Pipeline. Acad Med 2018, 93, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Al-Worafi, Y.M. Medical and Health Sciences in Developing Countries: Importance of Research. In Handbook of Medical and Health Sciences in Developing Countries: Education, Practice, and Research; Al-Worafi, Y.M., Ed.; Springer International Publishing: Cham, Switzerland, 2023; pp. 1–30. ISBN 978-3-030-74786-2. [Google Scholar]
- Thomas, M.P. The Geographic and Topical Landscape of Medical Education Research. BMC Med Educ 2019, 19, 189. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; Ghoshal, U.C.; Ragunath, K.; Jenkins, G.; Rahman, M.; Edwards, C.; Hasan, M.; Taylor-Robinson, S.D. Biomedical Research in Developing Countries: Opportunities, Methods, and Challenges. Indian J Gastroenterol 2020, 39, 292–302. [Google Scholar] [CrossRef]
- Nemr, E.; Moussallem, M.; Nemr, R.; Kosremelli Asmar, M. Exodus of Lebanese Doctors in Times of Crisis: A Qualitative Study. Front Health Serv 2023, 3, 1240052. [Google Scholar] [CrossRef]
- Bou Sanayeh, E.; El Chamieh, C. The Fragile Healthcare System in Lebanon: Sounding the Alarm about Its Possible Collapse. Health Econ Rev 2023, 13, 21. [Google Scholar] [CrossRef]
- Fleifel, M.; Abi Farraj, K. The Lebanese Healthcare Crisis: An Infinite Calamity. Cureus 2022, 14, e25367. [Google Scholar] [CrossRef]
- Alemayehu, C.; Mitchell, G.; Nikles, J. Barriers for Conducting Clinical Trials in Developing Countries- a Systematic Review. Int J Equity Health 2018, 17, 37. [Google Scholar] [CrossRef]
- Yegros-Yegros, A.; van de Klippe, W.; Abad-Garcia, M.F.; Rafols, I. Exploring Why Global Health Needs Are Unmet by Research Efforts: The Potential Influences of Geography, Industry and Publication Incentives. Health Res Policy Syst 2020, 18, 47. [Google Scholar] [CrossRef]
- Walsh, K.; Maloney, S.; Ilic, D.; Reeves, S.; Rivers, G. Medical Education Research: The Realm of the Rich. Med Teach 2017, 39, 225–226. [Google Scholar] [CrossRef]
- Franzen, S.R.P.; Chandler, C.; Lang, T. Health Research Capacity Development in Low and Middle Income Countries: Reality or Rhetoric? A Systematic Meta-Narrative Review of the Qualitative Literature. BMJ Open 2017, 7, e012332. [Google Scholar] [CrossRef] [PubMed]
- Dodani, S.; LaPorte, R.E. Ways to Strengthen Research Capacity in Developing Countries: Effectiveness of a Research Training Workshop in Pakistan. Public Health 2008, 122, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Cassell, H.M.; Rose, E.S.; Moon, T.D.; Bello-Manga, H.; Aliyu, M.H.; Mutale, W. Strengthening Research Capacity through an Intensive Training Program for Biomedical Investigators from Low- and Middle-Income Countries: The Vanderbilt Institute for Research Development and Ethics (VIRDE). BMC Med Educ 2022, 22, 97. [Google Scholar] [CrossRef] [PubMed]
- Ogdie, A.; Shah, A.A.; Makris, U.E.; Jiang, Y.; Nelson, A.E.; Kim, A.H.J.; Angeles-Han, S.T.; Castelino, F.V.; Golding, A.; Muscal, E.; et al. Barriers to and Facilitators of a Career as a Physician-Scientist Among Rheumatologists in the US. Arthritis Care Res (Hoboken) 2015, 67, 1191–1201. [Google Scholar] [CrossRef]
- Pepin, M.E.; Kamal, Y.; Reisman, B.J.; Rockman, M.E.; Waller, J.P. Making the Match and Breaking It: Values, Perceptions, and Obstacles of Trainees Applying into Physician-Scientist Training Programs. BMC Med Educ 2023, 23, 763. [Google Scholar] [CrossRef]
- Galderisi, A.; Bressan, S.; Da Dalt, L.; Perilongo, G.; Baraldi, E. Nurturing the next Generation of Pediatric Physician Scientists: The Padova Physician Scientist Research Training for Pediatric Residents. Eur J Pediatr 2024, 183, 1567–1570. [Google Scholar] [CrossRef]
- Kitching, A.R.; Ebeling, P.R. Challenges for Trainee Physician-Scientists during Their PhD Candidature: A Cross-Sectional Study. Intern Med J 2024, 54, 1190–1196. [Google Scholar] [CrossRef]
- Nassar, M.; Abdallah, W.; Najib, B.; Khalil, K.; Atallah, D. Weakening of the Lebanese Health Sector. East Mediterr Health J. 2023, 29, 168–169. [Google Scholar] [CrossRef]
- WHO Joint Statement by Dr Tedros Adhanom Ghebreyesus, WHO Director General, and Dr Ahmed Al Mandhari, Regional Director for the Eastern Mediterranean, on Lebanon . Available online: http://www.emro.who.int/media/news/joint-statement-by-dr-tedros-adhanom-ghebreyesus-who-director-general-and-dr-ahmed-al-mandhari-regional-director-for-the-eastern-mediterranean-on-lebanon.html (accessed on 25 December 2023).
- World Bank World Bank Open Data. Physicians (per 1,000 People) - Lebanon World Health Organization’s Global Health Workforce Statistics, OECD, Supplemented by Country Data. Available online: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=LB (accessed on 25 December 2023).
- Garrison, H.H.; Deschamps, A.M. NIH Research Funding and Early Career Physician Scientists: Continuing Challenges in the 21st Century. FASEB j. 2014, 28, 1049–1058. [Google Scholar] [CrossRef]
- Hu, Y.; Huang, Y.; Ding, J.; Liu, Y.; Fan, D.; Li, T.; Shou, C.; Fan, J.; Wang, W.; Dong, Z.; et al. Status of Clinical Research in China. Lancet 2011, 377, 124–125. [Google Scholar] [CrossRef]
- Heinig, S.J.; Krakower, J.Y.; Dickler, H.B.; Korn, D. Sustaining the Engine of U. S. Biomedical Discovery. N Engl J Med 2007, 357, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Brambila, C.N.; Reyes-Gonzalez, L.; Veloso, F.; Perez-Angón, M.A. The Scientific Impact of Developing Nations. PLoS ONE 2016, 11, e0151328. [Google Scholar] [CrossRef] [PubMed]
- Obuku, E.A.; Lavis, J.N.; Kinengyere, A.; Ssenono, R.; Ocan, M.; Mafigiri, D.K.; Ssengooba, F.; Karamagi, C.; Sewankambo, N.K. A Systematic Review on Academic Research Productivity of Postgraduate Students in Low- and Middle-Income Countries. Health Res Policy Syst 2018, 16, 86. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Gao, Y.; Ming, L.; Yang, K.; Sun, Y.; Chen, J.; Shi, S.; Geng, J.; Li, L.; Wu, J.; et al. A Bibliometric Analysis of Global Research Output on Network Meta-Analysis. BMC Med Inform Decis Mak 2021, 21, 144. [Google Scholar] [CrossRef]
- Cox, T.M.; Brimicombe, J.; Wood, D.F.; Peters, D.K. The Cambridge Bachelor of Medicine (MB)/Doctor of Philosophy (PhD): Graduate Outcomes of the First MB/PhD Programme in the UK. Clin Med (Lond) 2012, 12, 530–534. [Google Scholar] [CrossRef]
- Rimmer, A. Clinical Academic Workforce Continues to Shrink. BMJ 2017, 358, j3352. [Google Scholar] [CrossRef] [PubMed]
- Lalloo, D.; Demou, E.; Pahl, N.; Macdonald, E.B. Research and Teaching Activity in UK Occupational Physicians. Occup Med (Lond) 2020, 70, 64–67. [Google Scholar] [CrossRef]
- Hussain, A.B.; Healy, E.; Reynolds, N.J. Training and Retaining Physician-Scientists in Dermatology: A United Kingdom Perspective. JID Innov 2022, 2, 100091. [Google Scholar] [CrossRef]
- Ashour, L.; Schoumann-Alkhatib, A.; Alshawabkeh, A.; Alsouri, M.; Sawalmeh, M.; Hatamleh, H.; Sawahreh, H. Highlighting the Need for MD-PhD Programs in Developing Countries. Avicenna J Med 2023, 13, 65–67. [Google Scholar] [CrossRef]
- Khan, M.S.; Fatima, K.; Butler, J. Creation of next Generation of Diverse Cardiovascular Physician-Scientists from Developing Countries: Insights from Research Council of Pakistan. Eur Heart J 2023, ehad493. [Google Scholar] [CrossRef]
- Tankwanchi, A.B.S.; Ozden, C.; Vermund, S.H. Physician Emigration from Sub-Saharan Africa to the United States: Analysis of the 2011 AMA Physician Masterfile. PLoS Med 2013, 10, e1001513. [Google Scholar] [CrossRef]
- Uthman, O.A.; Wiysonge, C.S.; Ota, M.O.; Nicol, M.; Hussey, G.D.; Ndumbe, P.M.; Mayosi, B.M. Increasing the Value of Health Research in the WHO African Region beyond 2015--Reflecting on the Past, Celebrating the Present and Building the Future: A Bibliometric Analysis. BMJ Open 2015, 5, e006340. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.L. Balancing Research, Teaching, Clinical Care, and Family: Can Physician-Scientists Have It All? J Infect Dis 2018, 218, S32–S35. [Google Scholar] [CrossRef] [PubMed]
- Estrada, L.; Williams, M.A.; Williams, C.S. A Competency-Guided Approach to Optimizing a Physician-Scientist Curriculum. Med Sci Educ 2022, 32, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Yeravdekar, R.C.; Singh, A. Physician-Scientists: Fixing the Leaking Pipeline - A Scoping Review. Med Sci Educ 2022, 32, 1413–1424. [Google Scholar] [CrossRef]
- Beran, D.; Pesantes, M.A.; Berghusen, M.C.; Hennig, B.J.; Jacobi, J.; Lazo-Porras, M.; Llanque, A.; Placella, E.; Robledo-Abad, C.; Bayona, M.T.; et al. Rethinking Research Processes to Strengthen Co-Production in Low and Middle Income Countries. BMJ 2021, 372, m4785. [Google Scholar] [CrossRef]
- Hamer, D.H.; Hansoti, B.; Prabhakaran, D.; Huffman, M.D.; Nxumalo, N.; Fox, M.P.; Gopal, S.; Oberhelman, R.; Mwananyanda, L.; Vwalika, B.; et al. Global Health Research Mentoring Competencies for Individuals and Institutions in Low- and Middle-Income Countries. Am J Trop Med Hyg 2019, 100, 15–19. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).