Submitted:
11 December 2024
Posted:
11 December 2024
You are already at the latest version
Abstract
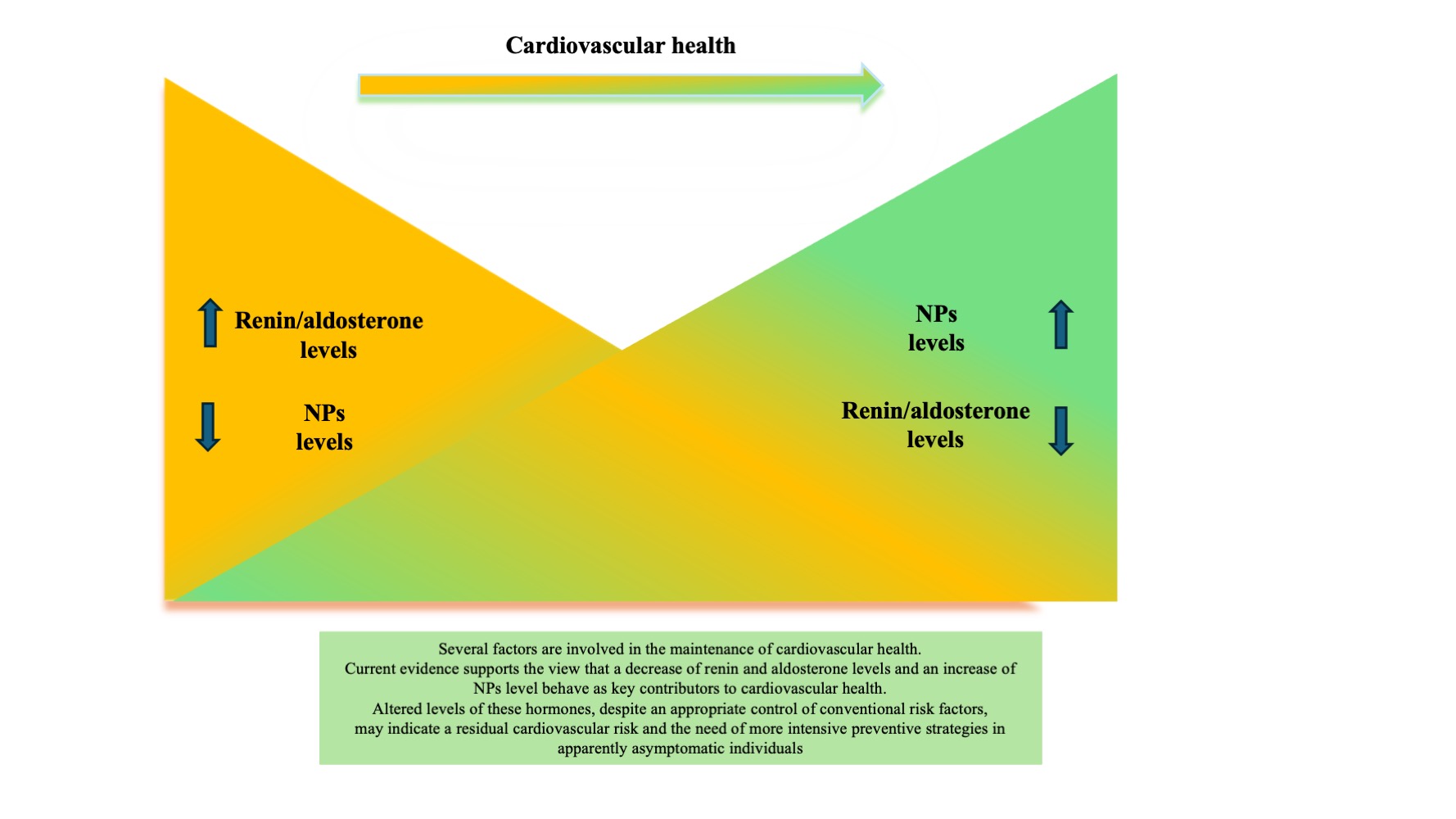
A healthy lifestyle plays a key role for maintaining the cardiovascular health (CVH) status and prevent cardiovascular disease occurrence. In fact, a healthy lifestyle was included in the AHA Cardiovascular Health score (Life’s Simple 7 [LS7]), subsequently updated to Life’s Simple 8 [LS8]. Apart from the importance of controlling conventional cardiovascular risk factors, increasing evidence supports the contributory role of cardiovascular hormones. Higher levels of natriuretic peptides (NPs) and lower levels of renin and aldosterone were significantly associated to CVH. NT-proBNP levels showed a direct relationship with CVH scores in large general Caucasian populations, being also a marker of CVH changes and a predictor of future adverse events. On the other hand, renin and aldosterone were inversely related to CVH scores. In contrast, the counter-regulatory angiotensins [Ang (1-7) acting through Mas receptor, Ang (1-9) acting through Angiotensin Type 2 receptor, and alamandine] strengthen the beneficial properties of NPs. This evidence can be explained by both the effects on systemic hemodynamic and possible pleiotropic local functions regulating different pathways involved in the maintenance of CVH. Based on the current evidence, circulating levels of NT-proBNP, renin and aldosterone may affect CVH in apparently asymptomatic individuals and represent additional markers of residual cardiovascular risk.
Keywords:
1. Introduction
2. Experimental and Human Evidence Linking NPs to CVH
3. The Implications of Both Classical and Counter-Regulatory RAAS in CVH Maintenance
4. Perspectives
Authors contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of interest
References
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; Arnett, D.K.; Fonarow, G.C.; Ho, P.M.; Lauer, M.S.; Masoudi, F.A.; Robertson, R.M.; Roger, V.; Schwamm, L.H.; Sorlie, P.; Yancy, C.W.; Rosamond, W.D.; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Jones, D.M.; Allen, N.B.; Anderson, C.A.M.; Black, T.; Brewer, L.C.; Foraker, R.E.; Grandner, M.A.; Lavretsky, H.; Perak, A.M.; Sharma, G.; Rosamond, W.; American Heart Association. Life's Essential 8: Updating and Enhancing the American Heart Association's Construct of Cardiovascular Health: A Presidential Advisory from the American Heart Association. Circulation 2022, 146, e18–e43. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, Y.; Mao, Y.; Zhu, F.; Zhang, M.; Pan, M.; Yin, T.; Xu, J.; Chen, R.; Zheng, W. Association of life's essential 8 with mortality among the individuals with cardiovascular disease. Sci Rep 2024, 14, 18520. [Google Scholar] [CrossRef] [PubMed]
- Te Hoonte, F.; Spronk, M.; Sun, Q.; Wu, K.; Fan, S.; Wang, Z.; Bots, M.L.; Van der Schouw, Y.T.; Uijl, A.; Vernooij, R.W.M. Ideal cardiovascular health and cardiovascular-related events: a systematic review and meta-analysis. Eur J Prev Cardiol 2024, 31, 966–985. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Saavedra, J.M.; Lobelo, F.; Celis-Morales, C.A.; Pozo-Cruz, B.D.; García-Hermoso, A. Ideal cardiovascular health and incident cardiovascular disease among adults: a systematic review and meta-analysis. Mayo Clin Proc 2018, 93, 1589–1599. [Google Scholar] [CrossRef]
- Xanthakis, V.; Enserro, D.M.; Murabito, J.M.; Polak, J.F.; Wollert, K.C.; Januzzi, J.L.; Wang, T.J.; Tofler, G.; Vasan, R.S. Ideal cardiovascular health: associations with biomarkers and subclinical disease and impact on incidence of cardiovascular disease in the Framingham Offspring Study. Circulation 2014, 130, 1676–1683. [Google Scholar] [CrossRef]
- Osibogun, O.; Ogunmoroti, O.; Tibuakuu, M.; Benson, E.M.; Michos, E.D. Sex differences in the association between ideal cardiovascular health and biomarkers of cardiovascular disease among adults in the United States: a cross-sectional analysis from the multiethnic study of atherosclerosis. BMJ Open 2019, 9, e031414. [Google Scholar] [CrossRef]
- Yuan, Y.E.; Haas, A.V.; Williams, G.H.; Taylor, H.; Seely, E.W.; Adler, G.K. Association between Life's Simple 7 and biomarkers of cardiovascular disease: aldosterone, interleukin-6, C-Reactive Protein. J Am Heart Assoc 2023, 12, e028718. [Google Scholar] [CrossRef]
- Kluwe, B.; Pohlman, N.; Kesireddy, V.; Zhao, S.; Tan, Y.; Kline, D.; Brock, G.; Odei, J.B.; Effoe, V.S.; Tcheugui, J.B.E.; Kalyani, R.R.; Sims, M.; Taylor, H.A.; Mongraw-Chaffin, M.; Akhabue, E.; Joseph, J.J. The role of aldosterone and ideal cardiovascular health in incident cardiovascular disease: The Jackson heart study. Am J Prev Cardiol 2023, 14, 100494. [Google Scholar] [CrossRef]
- Kesireddy, V.; Tan, Y.; Kline, D.; Brock, G.; Odei, J.B.; Kluwe, B.; Effoe, V.S.; Echouffo Tcheugui, J.B.; Kalyani, R.R.; Sims, M.; Taylor, H.A.; Mongraw-Chaffin, M.; Akhabue, E.; Joseph, J.J. The Association of Life's Simple 7 with Aldosterone among African Americans in the Jackson Heart Study. Nutrients 2019, 11, 955. [Google Scholar] [CrossRef]
- Mirabito Colafella, K.M.; Bovée, D.M.; Danser, A.H.J. The renin-angiotensin-aldosterone system and its therapeutic targets. Exp Eye Res 2019, 186, 107680. [Google Scholar] [CrossRef] [PubMed]
- Volpe, M.; Gallo, G.; Rubattu, S. Endocrine functions of the heart: from bench to bedside. Eur Heart J 2023, 44, 643–655. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Qi, Y.; Lu, W. Endogenous Vasoactive Peptides and Vascular Aging-Related Diseases. Oxid Med Cell Longev 2022, 2022, 1534470. [Google Scholar] [CrossRef]
- Loutzenhiser, R.; Hayashi, K.; Epstein, M. Atrial natriuretic peptide reverses afferent arteriolar vasoconstriction and potentiates efferent arteriolar vasoconstriction in the isolated perfused rat kidney. J Pharmacol Exp Ther 1888, 246, 522–528. [Google Scholar]
- McGrath, M.F.; de Bold, M.L.; de Bold, A.J. The endocrine function of the heart. Trends Endocrinol Metab 2005, 16, 469–477. [Google Scholar] [CrossRef]
- Melo, L.G.; Steinhelper, M.E.; Pang, S.C.; Tse, Y.; Ackermann, U. ANP in regulation of arterial pressure and fluid-electrolyte balance: Lessons from genetic mouse models. Physiol Genomics 2000, 3, 45–58. [Google Scholar] [CrossRef]
- Atchison, D.J.; Ackermann, U. Influence of atrial natriuretic factor on autonomic control of heart rate. Am J Phys 1990, 258, R718–R723. [Google Scholar] [CrossRef]
- Butler, G.C.; Senn, B.L.; Floras, J.S. Influence of atrial natriuretic factor on heart rate variability in normal men. Am J Phys 1994, 267, H500–H505. [Google Scholar] [CrossRef]
- Struthers, A.D.; Anderson, J.V.; Payne, N.; Causon, R.C.; Slater, J.D.; Bloom, S.R. The effect of atrial natriuretic peptide on plasma renin activity, plasma aldosterone, and urinary dopamine in man. Eur J Clin Pharmacol 1986, 31, 223–226. [Google Scholar] [CrossRef]
- Brenner, B.M.; Ballermann, B.J.; Gunning, M.E.; Zeidel, M.L. Diverse biological actions of atrial natriuretic peptide. Physiol Rev 1990, 70, 665–699. [Google Scholar] [CrossRef]
- Franco-Saenz, R.; Atarashi, K.; Takagi, M.; Mulrow, P.J. Effect of atrial natriuretic factor on renin and aldosterone. J Cardiovasc Pharmacol 1989, 13 (Suppl 6), S31–S35. [Google Scholar] [CrossRef] [PubMed]
- Burger, A.J. A review of the renal and neurohormonal effects of B-type natriuretic peptide. Congest Heart Fail 2005, 11, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Dhingra, H.; Roongsritong, C.; Kurtzman, N.A. Brain natriuretic peptide: role in cardiovascular and volume homeostasis. Seminars in Nephrology 2002, 22, 423–437. [Google Scholar] [CrossRef] [PubMed]
- Mukoyama, M.; Nakao, K.; Hosoda, K.; Suga, S.; Saito, Y.; Ogawa, Y.; Shirakami, G.; Jougasaki, M.; Obata, K.; Yasue, H.; Kambayashi, Y.; Inoue, K.; Imura, H. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest 1991, 87, 1402–1412. [Google Scholar] [CrossRef]
- Vanderheyden, M.; Bartunek, J.; Goethals, M. Brain and other natriuretic peptides: molecular aspects. Eur J Heart Fail 2004, 6, 261–268. [Google Scholar] [CrossRef]
- Gómez-Virgilio, L.; Silva-Lucero, M.D.; Flores-Morelos, D.S.; Gallardo-Nieto, J.; Lopez-Toledo, G.; Abarca-Fernandez, A.M.; Zacapala-Gómez, A.E.; Luna-Muñoz, J.; Montiel-Sosa, F.; Soto-Rojas, L.O.; Pacheco-Herrero, M.; Cardenas-Aguayo, M.D. Autophagy: a key regulator of homeostasis and disease: an overview of molecular mechanisms and modulators. Cells 2022, 11, 2262. [Google Scholar] [CrossRef]
- Forte, M.; Marchitti, S.; Di Nonno, F.; Stanzione, R.; Schirone, L.; Cotugno, M.; Bianchi, F.; Schiavon, S.; Raffa, S.; Ranieri, D.; Fioriniello, S.; Della Ragione, F.; Torrisi, M.R.; Carnevale, R.; Valenti, V.; Versaci, F.; Frati, G.; Vecchione, C.; Volpe, M.; Rubattu, S.; Sciarretta, S. NPPA/atrial natriuretic peptide is an extracellular modulator of autophagy in the heart. Autophagy 2023, 19, 1087–1099. [Google Scholar] [CrossRef]
- Forte, M.; Marchitti, S.; di Nonno, F.; Pietrangelo, D.; Stanzione, R.; Cotugno, M.; D'Ambrosio, L.; D'Amico, A.; Cammisotto, V.; Sarto, G.; Rocco, E.; Simeone, B.; Schiavon, S.; Vecchio, D.; Carnevale, R.; Raffa, S.; Frati, G.; Volpe, M.; Sciarretta, S.; Rubattu, S. Atrial natriuretic peptide (ANP) modulates stress-induced autophagy in endothelial cells. BBA Mol Cell Res 2024, in press. [Google Scholar] [CrossRef]
- Furuya, M.; Yoshida, M.; Hayashi, Y.; Ohnuma, N.; Minamino, N.; Kangawa, K.; Matsuo, H. C-type natriuretic peptide is a growth inhibitor of rat vascular smooth muscle cells. Biochem Biophys Res Commun 1991, 177, 927–931. [Google Scholar] [CrossRef]
- Nakao, K.; Kuwahara, K.; Nishikimi, T.; Nakagawa, Y.; Kinoshita, H.; Minami, T.; Kuwabara, Y.; Yamada, C.; Yamada, Y.; Tokudome, T.; Nagai-Okatani, C.; Minamino, N.; Nakao, Y.M.; Yasuno, S.; Ueshima, K.; Sone, M.; Kimura, T.; Kangawa, K.; Nakao, K. Endothelium-derived C-type natriuretic peptide contributes to blood pressure regulation by maintaining endothelial integrity. Hypertension 2017, 69, 286–296. [Google Scholar] [CrossRef]
- Moyes, A.J.; Khambata, R.S.; Villar, I.; Bubb, K.J.; Baliga, R.S.; Lumsden, N.G.; Xiao, F.; Gane, P.J.; Rebstock, A.S.; Worthington, R.J.; Simone, M.I.; Mota, F.; Rivilla, F.; Vallejo, S.; Peiró, C.; Sánchez Ferrer, C.F.; Djordjevic, S.; Caulfield, M.J.; MacAllister, R.J.; Selwood, D.L.; Hobbs, A.J. Endothelial C-type natriuretic peptide maintains vascular homeostasis. J Clin Invest 2014, 124, 4039–4051. [Google Scholar] [CrossRef] [PubMed]
- Moyes, A.J.; Chu, S.M.; Aubdool, A.A.; Dukinfield, M.S.; Margulies, K.B.; Bedi, K.C.; Hodivala-Dilke, K.; Baliga, R.S.; Hobbs, A.J. C-type natriuretic peptide co-ordinates cardiac structure and function. Eur Heart J 2020, 41, 1006–1020. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Redfield, M.M.; Melenovsky, V.; Kane, G.C.; Karon, B.L.; Jacobsen, S.J.; Rodeheffer, R.J. Longitudinal changes in left ventricular stiffness: a community-based study. Circ Heart Fail 2013, 6, 944–952. [Google Scholar] [CrossRef]
- Echocardiographic Normal Ranges Meta-Analysis of the Left Heart Collaboration Ethnic-specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: the EchoNoRMAL Study. JACC Cardiovasc Imaging 2015, 8, 656–665. [CrossRef]
- Cannone, V.; Cabassi, A.; Volpi, R.; Burnett, J.C., Jr. Atrial natriuretic peptide: a molecular target of novel therapeutic approaches to cardio-metabolic disease. Int J Mol Sci 2019, 20, 3265. [Google Scholar] [CrossRef]
- Patel, N.; Russell, G.K.; Musunuru, K.; Gutierrez, O.M.; Halade, G.; Kain, V.; Lv, W.; Prabhu, S.D.; Margulies, K.B.; Cappola, T.P.; Arora, G.; Wang, T.J.; Arora, P. Race, natriuretic peptides, and high-carbohydrate challenge: a clinical trial. Circ Res 2019, 125, 957–968. [Google Scholar] [CrossRef]
- Rubattu, S.; Stanzione, R.; Cotugno, M.; Bianchi, F.; Marchitti, S.; Forte, M. Epigenetic control of natriuretic peptides: implications for health and disease. Cell Mol Life Sci 2020, 77, 5121–5130. [Google Scholar] [CrossRef]
- Cannone, V.; Scott, C.G.; Decker, P.A.; Larson, N.B.; Palmas, W.; Taylor, K.D.; Wang, T.J.; Gupta, D.K.; Bielinski, S.J.; Burnett, J.C., Jr. A favorable cardiometabolic profile is associated with the G allele of the genetic variant rs5068 in African Americans: The Multi-Ethnic Study of Atherosclerosis (MESA). PLoS One 2017, 12, e0189858. [Google Scholar] [CrossRef]
- Prickett, T.C.R.; Spittlehouse, J.K.; Miller, A.L.; Liau, Y.; Kennedy, M.A.; Cameron, V.A.; Pearson, J.F.; Boden, J.M.; Troughton, R.W.; Espiner, E.A. Contrasting signals of cardiovascular health among natriuretic peptides in subjects without heart disease. Sci Rep 2019, 9, 12108. [Google Scholar] [CrossRef]
- Prickett, T.C.R.; Darlow, B.A.; Troughton, R.W.; Cameron, V.A.; Elliott, J.M.; Martin, J.; Horwood, L.J.; Espiner, E.A. New insights into cardiac and vascular natriuretic peptides: findings from young adults born with very low birth weight. Clin Chem 2018, 64, 363–373. [Google Scholar] [CrossRef]
- Prickett, T.C.R.; Pearson, J.F.; Troughton, R.W.; Kennedy, M.A.; Espiner, E.A. The predictive value of A, B, and C-type natriuretic peptides in people at risk of heart disease: protocol for a longitudinal observational study. JMIR Res Protoc 2023, 12, e37011. [Google Scholar] [CrossRef] [PubMed]
- Natriuretic Peptides Studies Collaboration Willeit, P.; Kaptoge, S.; Welsh, P.; Butterworth, A.S.; Chowdhury, R.; Spackman, S.A.; Pennells, L.; Gao, P.; Burgess, S.; Freitag, D.F.; Sweeting, M.; Wood, A.M.; Cook, N.R.; Judd, S.; Trompet, S.; Nambi, V.; Olsen, M.H.; Everett, B.M.; Kee, F.; Ärnlöv, J.; Salomaa, V.; Levy, D.; Kauhanen, J.; Laukkanen, J.A.; Kavousi, M.; Ninomiya, T.; Casas, J.P.; Daniels, L.B.; Lind, L.; Kistorp, C.N.; Rosenberg, J.; Mueller, T.; Rubattu, S.; Panagiotakos, D.B.; Franco, O.H.; de Lemos, J.A.; Luchner, A.; Kizer, J.R.; Kiechl, S.; Salonen, J.T.; Goya Wannamethee, S.; de Boer, R.A.; Nordestgaard, B.G.; Andersson, J.; Jørgensen, T.; Melander, O.; Ballantyne, C.h.M.; DeFilippi Ch Ridker, P.M.; Cushman, M.; Rosamond, W.D.; Thompson, S.G.; Gudnason, V.; Sattar, N.; Danesh, J.; Di Angelantonio, E. Natriuretic peptides and integrated risk assessment for cardiovascular disease: an individual-participant-data meta-analysis. Lancet Diabetes Endocrinol 2016, 4, 840–849. [Google Scholar]
- Neumann, J.T.; Twerenbold, R.; Weimann, J.; Ballantyne, C.M.; Benjamin, E.J.; Costanzo, S.; de Lemos, J.A.; deFilippi, C.R.; Di Castelnuovo, A.; Donfrancesco, C.; Dörr, M.; Eggers, K.M.; Engström, G.; Felix, S.B.; Ferrario, M.M.; Gansevoort, R.T.; Giampaoli, S.; Giedraitis, V.; Hedberg, P.; Iacoviello, L.; Jørgensen, T.; Kee, F.; Koenig, W.; Kuulasmaa, K.; Lewis, J.R.; Lorenz, T.; Lyngbakken, M.N.; Magnussen, C.; Melander, O.; Nauck, M.; Niiranen, T.J.; Nilsson, P.M.; Olsen, M.H.; Omland, T.; Oskarsson, V.; Palmieri, L.; Peters, A.; Prince, R.L.; Qaderi, V.; Vasan, R.S.; Salomaa, V.; Sans, S.; Smith, J.G.; Söderberg, S.; Thorand, B.; Tonkin, A.M.; Tunstall-Pedoe, H.; Veronesi, G.; Watanabe, T.; Watanabe, M.; Zeiher, A.M.; Zeller, T.; Blankenberg, S.; Ojeda, F. Prognostic value of cardiovascular biomarkers in the population. JAMA 2024, 331, 1898–1909. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, S.; Lampa, E.; Jensevik Eriksson, K.; Butterworth, A.S.; Elmståhl, S.; Engström, G.; Hveem, K.; Johansson, M.; Langhammer, A.; Lind, L.; Läll, K.; Masala, G.; Metspalu, A.; Moreno-Iribas, C.; Nilsson, P.M.; Perola, M.; Simell, B.; Sipsma, H.; Åsvold, B.O.; Ingelsson, E.; Hammar, U.; Ganna, A.; Svennblad, B.; Fall, T.; Sundström, J. Markers of imminent myocardial infarction. Nat Cardiovasc Res 2024, 3, 130–139. [Google Scholar] [CrossRef]
- Zhou, H.; Yang, C.; Li, J.; Sun, L. Association of N-terminal pro-B natriuretic peptide with all-cause mortality and cardiovascular mortality in obese and non-obese populations and the development of a machine learning prediction model: National Health and Nutrition Examination Survey (NHANES) 1999-2004. Diabetes Obes Metab 2024. [Google Scholar]
- Segar, M.W.; Khan, M.S.; Patel, K.V.; Vaduganathan, M.; Kannan, V.; Willett, D.; Peterson, E.; Tang, W.H.W.; Butler, J.; Everett, B.M.; Fonarow, G.C.; Wang, T.J.; McGuire, D.K.; Pandey, A. Incorporation of natriuretic peptides with clinical risk scores to predict heart failure among individuals with dysglycaemia. Eur J Heart Fail 2022, 24, 169–180. [Google Scholar] [CrossRef]
- Jehn, S.; Mahabadi, A.A.; Pfohl, C.; Vogel, L.; Al-Rashid, F.; Luedike, P.; Totzeck, M.; Rassaf, T.; Dykun, I. BNP and NT-proBNP thresholds for the assessment of prognosis in patients without heart failure. JACC Adv 2023, 2, 100688. [Google Scholar] [CrossRef]
- Volpe, M.; Gallo, G.; Rubattu, S. BNP/NT-proBNP levels are sensitive markers of impaired prognosis in patients without heart failure. JACC Adv 2023, 2, 100691. [Google Scholar] [CrossRef]
- Oh, H.S.; Rutledge, J.; Nachun, D.; Pálovics, R.; Abiose, O.; Moran-Losada, P.; Channappa, D.; Urey, D.Y.; Kim, K.; Sung, Y.J.; Wang, L.; Timsina, J.; Western, D.; Liu, M.; Kohlfeld, P.; Budde, J.; Wilson, E.N.; Guen, Y.; Maurer, T.M.; Haney, M.; Yang, A.C.; He, Z.; Greicius, M.D.; Andreasson, K.I.; Sathyan, S.; Weiss, E.F.; Milman, S.; Barzilai, N.; Cruchaga, C.; Wagner, A.D.; Mormino, E.; Lehallier, B.; Henderson, V.W.; Longo, F.M.; Montgomery, S.B.; Wyss-Coray, T. Organ aging signatures in the plasma proteome track health and disease. Nature 2023, 624, 164–172. [Google Scholar] [CrossRef]
- Kuh, D.; Cooper, R.; Sattar, N.; Welsh, P.; Hardy, R.; Ben-Shlomo, Y. Systemic inflammation and cardio-renal organ damage biomarkers in middle age are associated with physical capability up to 9 years later. Circulation 2019, 139, 1988–1999. [Google Scholar] [CrossRef]
- van Peet, P.G.; de Craen, A.J.; Gussekloo, J.; de Ruijter, W. Plasma NT-proBNP as predictor of change in functional status, cardiovascular morbidity and mortality in the oldest old: the Leiden 85-plus study. Age (Dordr) 2014, 36, 9660. [Google Scholar] [CrossRef] [PubMed]
- Hozawa, A.; Sugawara, Y.; Tomata, Y.; Kakizaki, M.; Ohmori-Matsuda, K.; Nakaya, N.; Kuriyama, S.; Fukao, A.; Tsuji, I. Relationships between N-terminal pro B-type natriuretic peptide and incident disability and mortality in older community-dwelling adults: the Tsurugaya study. J Am Geriatr Soc 2010, 58, 2439–2441. [Google Scholar] [CrossRef] [PubMed]
- Gallo, G.; Bianchi, F.; Cotugno, M.; Volpe, M.; Rubattu, S. Natriuretic peptides, cognitive impairment and dementia: an intriguing pathogenic link with implications in hypertension. J Clin Med 2020, 9, 2265. [Google Scholar] [CrossRef]
- Ostovaneh, M.R.; Moazzami, K.; Yoneyama, K.; Venkatesh, B.A.; Heckbert, S.R.; Wu, C.O.; Shea, S.; Post, W.S.; Fitzpatrick, A.L.; Burke, G.L.; Bahrami, H.; Sanchez, O.A.; Daniels, L.B.; Michos, E.D.; Bluemke, D.A.; Lima, J.A.C. Change in NT-proBNP (N-Terminal pro-B-type natriuretic peptide) level and risk of dementia in multi-ethnic study of atherosclerosis (MESA). Hypertension 2020, 75, 316–323. [Google Scholar] [CrossRef]
- 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Failure Society of America. J Card Fail 2016, 22, 659–669.
- Raffa, S.; Forte, M.; Gallo, G.; Ranieri, D.; Marchitti, S.; Magrì, D.; Testa, M.; Stanzione, R.; Bianchi, F.; Cotugno, M.; Fiori, E.; Visco, V.; Sciarretta, S.; Volpe, M.; Rubattu, S. Atrial natriuretic peptide stimulates autophagy/mitophagy and improves mitochondrial function in chronic heart failure. Cell Mol Life Sci 2023, 80, 134. [Google Scholar] [CrossRef]
- Rubattu, S.; Cotugno, M.; Forte, M.; Stanzione, R.; Bianchi, F.; Madonna, M.; Marchitti, S.; Volpe, M. Effects of dual angiotensin type 1 receptor/neprilysin inhibition vs. angiotensin type 1 receptor inhibition on target organ injury in the stroke-prone spontaneously hypertensive rat. J Hypertens 2018, 36, 1902–1914. [Google Scholar] [CrossRef]
- Xiao, Y.; Zhou, Z.Y.; Sun, J.C.; Xing, W.; Yan, J.; Xu, W.J.; Lu, Y.S.; Liu, T.; Jin, Y. Protective effect of novel angiotensin receptor neprilysin inhibitor S086 on target organ injury in spontaneously hypertensive rats. Biomed Pharmacother 2024, 170, 115968. [Google Scholar] [CrossRef]
- Chen, H.H.; Wan, S.H.; Iyer, S.R.; Cannone, V.; Sangaralingham, S.J.; Nuetel, J.; Burnett, J.C., Jr. First-in-human study of MANP: a novel ANP (Atrial Natriuretic Peptide) analog in human hypertension. Hypertension 2021, 78, 1859–1867. [Google Scholar] [CrossRef]
- Ma, X.; McKie, P.M.; Iyer, S.R.; Scott, C.; Bailey, K.; Johnson, B.K.; Benike, S.L.; Chen, H.; Miller, W.L.; Cabassi, A.; Burnett, J.C., Jr.; Cannone, V. MANP in hypertension with metabolic syndrome: proof-of-concept study of natriuretic peptide-based therapy for cardiometabolic disease. JACC Basic Transl Sci 2023, 9, 18–29. [Google Scholar] [CrossRef]
- Ferrario, C.M. The renin-angiotensin system: Importance in physiology and pathology. J Cardiovasc Pharmacol 1990, 15 (Suppl. 3), S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Li, X.C.; Campbell, D.J.; Ohishi, M.; Yuan, S.; Zhuo, J.L. AT1 receptor-activated signaling mediates angiotensin IV-induced renal cortical vasoconstriction in rats. Am J Physiol Renal Physiol 2006, 290, F1024–1033. [Google Scholar] [CrossRef] [PubMed]
- Volpe, M.; Rubattu, S.; Gigante, B.; Ganten, D.; Porcellini, A.; Russo, R.; Romano, M.; Enea, I.; Lee, M.A.; Trimarco, B. Regulation of aldosterone biosynthesis by adrenal renin is mediated through AT1 receptors in renin transgenic rats. Circ Res 1995, 77, 73–79. [Google Scholar] [CrossRef]
- Carey, R.M. Update on angiotensin AT2 receptors. Curr Opin Nephrol Hypertens 2017, 26, 91–96. [Google Scholar] [CrossRef]
- Albiston, A.L.; McDowall, S.G.; Matsacos, D.; Sim, P.; Clune, E.; Mustafa, T.; Lee, J.; Mendelsohn, F.A.; Simpson, R.J.; Connolly, L.M.; Chai, S.Y. Evidence that the angiotensin IV (AT (4)) receptor is the enzyme insulin-regulated aminopeptidase. J Biol Chem 2001, 276, 48623–48626. [Google Scholar] [CrossRef]
- Matavelli, L.C.; Siragy, H.M. AT2 receptor activities and pathophysiological implications. J Cardiovasc Pharmacol 2015, 65, 226–232. [Google Scholar] [CrossRef]
- Kemp, B.A.; Howell, N.L.; Gildea, J.J.; Keller, S.R.; Padia, S.H.; Carey, R.M. AT2 receptor activation induces natriuresis and lowers blood pressure. Circ Res 2014, 115, 388–399. [Google Scholar] [CrossRef]
- Gigante, B.; Rubattu, S.; Russo, R.; Porcellini, A.; Enea, I.; De Paolis, P.; Savoia, C.; Natale, A.; Piras, O.; Volpe, M. Opposite feedback control of renin and aldosterone biosynthesis in the adrenal cortex by angiotensin II AT1-subtype receptors. Hypertension 1997, 30, 563–568. [Google Scholar] [CrossRef]
- De Paolis, P.; Porcellini, A.; Gigante, B.; Giliberti, R.; Lombardi, A.; Savoia, C.; Rubattu, S.; Volpe, M. Modulation of the AT2 subtype receptor gene activation and expression by the AT1 receptor in endothelial cells. J Hypertens 1999, 17, (Pt 2), 1873–1877. [Google Scholar] [CrossRef]
- Bauer, J.H. Age-related changes in the renin-aldosterone system. Physiological effects and clinical implications. Drugs Aging. 1993, 3, 238–245. [Google Scholar] [CrossRef]
- Zhuo, J.L.; Ferrao, F.M.; Zheng, Y.; Li, X.C. New frontiers in the intrarenal Renin-Angiotensin system: a critical review of classical and new paradigms. Frontiers in Endocrinology 2013, 4, 166. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Gul, R.; Yuan, K.; Gao, S.; Oh, Y.B.; Kim, U.H.; Kim, S.H. Angiotensin-(1-7) stimulates high atrial pacing-induced ANP secretion via Mas/PI3-kinase/Akt axis and Na+/H+ exchanger. Am J Physiol Heart Circ Physiol 2010, 298, H1365–H1374. [Google Scholar] [CrossRef] [PubMed]
- Foote, K.; Reinhold, J.; Yu, E.P.K.; Figg, N.L.; Finigan, A.; Murphy, M.P.; Bennett, M.R. Restoring mitochondrial DNA copy number preserves mitochondrial function and delays vascular aging in mice. Aging Cell 2018, 17, e12773. [Google Scholar] [CrossRef]
- Guo, L.; Yin, A.; Zhang, Q.; Zhong, T.; O'Rourke, S.T.; Sun, C. Angiotensin-(1-7) attenuates angiotensin II-induced cardiac hypertrophy via a Sirt3-dependent mechanism. Am J Physiol Heart Circ Physiol 2017, 312, H980–H991. [Google Scholar] [CrossRef]
- Pinheiro, S.V.; Ferreira, A.J.; Kitten, G.T.; da Silveira, K.D.; da Silva, D.A.; Santos, S.H. , et al., Genetic deletion of the angiotensin-(1–7) receptor Mas leads to glomerular hyperfiltration and microalbuminuria. Kidney Intern 2009, 75, 1184–1193. [Google Scholar] [CrossRef]
- Li, Y.; Wu, J.; He, Q.; Shou, Z.; Zhang, P.; Pen, W. , et al., Angiotensin (1–7) prevents heart dysfunction and left ventricular remodeling caused by renal dysfunction in 5/6 nephrectomy mice. Hypertens Res 2009, 32, 369–374. [Google Scholar] [CrossRef]
- Oliveira Andrade, J.M.; de Farias Lelis, D.; Mafra, V.; Cota, J. The Angiotensin Converting Enzyme 2 (ACE2), Gut microbiota, and cardiovascular health. Protein Pept Lett. 2017, 24, 827–832. [Google Scholar] [CrossRef]
- Gamino-Gutierrez, J.A.; Teran-Hernandez, I.M.; Castellar-Lopez, J.; Villamizar-Villamizar, W.; Osorio-Llanes, E.; Palacios-Cruz, M.; Rosales, W.; Chang, A.Y.; Diaz-Ariza, L.A.; Ospino, M.C.; Mendoza-Torres, E. Novel insights into the cardioprotective effects of the peptides of the counter-regulatory renin–angiotensin system. Biomedicines 2024, 12, 255. [Google Scholar] [CrossRef]
- Cha, S.A.; Park, B.M.; Gao, S.; Kim, S.H. Stimulation of ANP by angiotensin-(1-9) via the angiotensin type 2 receptor. Life Sci 2013, 93, 934–940. [Google Scholar] [CrossRef]
- Park, B.M.; Phuong, H.T.A.; Yu, L.; Kim, S.H. Alamandine protects the heart against reperfusion injury via the MrgD receptor. Circ J 2018, 82, 2584–2593. [Google Scholar] [CrossRef]
- Campbell, D.J. Critical review of prorenin and (pro)renin receptor research. Hypertension 2008, 51, 1259–1264. [Google Scholar] [CrossRef] [PubMed]
- Neves, M.F.; Cunha, A.R.; Cunha, M.R.; Gismondi, R.A.; Oigman, W. The role of renin-angiotensin-aldosterone system and its new components in arterial stiffness and vascular aging. High Blood Press Cardiovasc Prev 2018, 25, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Feldman, J.M.; Frishman, W.H.; Aronow, W.S. Emerging therapies for treatment-resistant hypertension: A review of lorundrostat and related selective aldosterone synthase inhibitors. Cardiol Rev. 2024, in press. [CrossRef]
- Roth, L.; Dogan, S.; Tuna, B.G.; Aranyi, T.; Benitez, S.; Borrell-Pages, M.; Bozaykut, P.; De Meyer, G.R.Y.; Duca, L.; Durmus, N.; Fonseca, D.; Fraenkel, E.; Gillery, P.; Giudici, A.; Jaisson, S.; Johansson, M.; Julve, J.; Lucas-Herald, A.K.; Martinet, W.; Maurice, P.; McDonnell, B.J.; Ozbek, E.N.; Pucci, G.; Pugh, C.J.A.; Rochfort, K.D.; Roks, A.J.M.; Rotllan, N.; Shadiow, J.; Sohrabi, Y.; Spronck, B.; Szeri, F.; Terentes-Printzios, D.; Tunc Aydin, E.; Tura-Ceide, O.; Ucar, E.; Yetik-Anacak, G. Pharmacological modulation of vascular ageing: A review from VascAgeNet. Ageing Res Rev 2023, 92, 102122. [Google Scholar] [CrossRef]
- de Cavanagh, E.M.; Inserra, F.; Ferder, L. Angiotensin II blockade: how its molecular targets may signal to mitochondria and slow aging. Coincidences with calorie restriction and mTOR inhibition. Am J Physiol Heart Circ Physiol 2015, 309, H15–H44. [Google Scholar] [CrossRef]
- de Cavanagh, E.M.V.; Inserra, F.; Ferder, L. Renin-angiotensin system inhibitors positively impact on multiple aging regulatory pathways: could they be used to protect against human aging? Physiol Rep 2024, 12, e16094. [Google Scholar] [CrossRef]
- Zheng, L.; Wang, J.; Zhang, R.; Zhang, Y.; Geng, J.; Cao, L.; Zhao, X.; Geng, J.; Du, X.; Hu, Y.; Cong, H. Angiotensin II mediates cardiomyocyte hypertrophy in atrial cardiomyopathy via epigenetic transcriptional regulation. Comput Math Methods Med 2022, 2022, 6312100. [Google Scholar] [CrossRef]
- Bryniarski, P.; Nazimek, K.; Marcinkiewicz, J. Immunomodulatory activity of the most commonly used antihypertensive drugs-angiotensin converting enzyme inhibitors and angiotensin II receptor blockers. Int J Mol Sci 2022, 23, 1772. [Google Scholar] [CrossRef]
- Fatima, N.; Patel, S.N.; Hussain, T. Angiotensin II Type 2 Receptor: a target for protection against hypertension, metabolic dysfunction, and organ remodeling. Hypertension 2021, 77, 1845–1856. [Google Scholar] [CrossRef]
- Gwathmey, T.M.; Shaltout, H.A.; Pendergrass, K.D.; Pirro, N.T.; Figueroa, J.P.; Rose, J.C.; Diz, D.I.; Chappell, M.C. Nuclear angiotensin II type 2 (AT2) receptors are functionally linked to nitric oxide production. Am J Physiol Renal Physiol 2009, 296, F1484–F1493. [Google Scholar] [CrossRef]
- Savoia, C.; Arrabito, E.; Parente, R.; Nicoletti, C.; Madaro, L.; Battistoni, A.; Filippini, A.; Steckelings, U.M.; Touyz, R.M.; Volpe, M. Mas receptor activation contributes to the improvement of nitric oxide bioavailability and vascular remodeling during chronic AT1R (Angiotensin Type-1 Receptor) blockade in experimental hypertension. Hypertension 2020, 76, 1753–1761. [Google Scholar] [CrossRef] [PubMed]
- Welsh, P.; Campbell, R.T.; Mooney, L.; Kimenai, D.M.; Hayward, C.; Campbell, A.; Porteous, D.; Mills, N.L.; Lang, N.N.; Petrie, M.C.; Januzzi, J.L.; McMurray, J.J.V.; Sattar, N. Reference ranges for NT-proBNP (N-Terminal Pro-B-Type Natriuretic Peptide) and risk factors for higher NT-proBNP concentrations in a large general population cohort. Circ Heart Fail 2022, 15, e009427. [Google Scholar] [CrossRef] [PubMed]
- Shetty, N.S.; Patel, N.; Gaonkar, M.; Li, P.; Arora, G.; Arora, P. Natriuretic peptide normative levels and deficiency: The National Health and Nutrition Examination Survey. JACC Heart Fail. 2024, 12, 50–63. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.E.; Januzzi, J.L., Jr. NT-proBNP concentrations in the community: elevation, deficiency, and everything in between. JACC Heart Fail. 2024, 12, 64–66. [Google Scholar] [CrossRef]
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




