Submitted:
27 December 2024
Posted:
27 December 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Objectives
1.2. Theoretical Framework
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sample
2.3. Intervention
2.4. Measures
2.5. Procedures
2.6. Data Analysis
3. Results
3.1. Child and Maternal Characteristics by Group
3.2. Risk of Child Developmental Delay and Maternal Scale Scores
4. Discussion
4.1. Maternal Psychosocial Distress and Child Development
4.2. Maternal Self-Efficacy and Child Development
4.3. Maternal Demographic Characteristics and Child Development
4.4. Limitations and Future Research
5. Conclusions
Acronyms and Abbreviations
| ASQ-3 | Ages and Stages Questionnaire version |
| ASQ:SE-2 | Ages and Stages Questionnaire version |
| BITSEA | Brief Infant and Toddler Social Emotional Assessment |
| CA | corrected age |
| CESD-R | Center for Epidemiological Studies Depression scale -Revised |
| FICare | family integrated care |
| GA | gestational age |
| GSE | General Self-Efficacy scale |
| MLPI | moderate and late preterm infant |
| NICU | neonatal intensive care unit |
| PSI-4-SF | Parenting Stress Index version – short form |
| STAI | State Trait Anxiety Scale |
References
- About AHS. Alberta Health Services, 2023. Available online: https://www.albertahealthservices.ca/about/about.aspx.
- Meléndez, L. Parental Beliefs and Practices Around Early Self-regulation: The Impact of Culture and Immigration. Infants & Young Children, 18, 136–146.
- Shaw, D.S.; Connell, A.; Dishion, T.J.; Wilson, M.N.; Gardner, F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology 2009, 21, 417–439. [Google Scholar] [CrossRef] [PubMed]
- Moe, A.M.; Kurilova, J.; Afzal, A.R.; Benzies, K.M. Effects of Alberta Family Integrated Care (FICare) on preterm infant development: Two studies at 2 months and between 6- and 24-months corrected age. Journal of Clinical Medicine 2022, 11, 1684. [Google Scholar] [CrossRef] [PubMed]
- Dotinga, B.M.; Winter, A.F.D.; Bocca-Tjeertes, I.F.; Kerstjens, J.M.; Reijneveld, S.A. Bos.; et al. Longitudinal growth and emotional and behavioral problems at age 7 in moderate and late preterms. PloS One 2019, 14, e0211427. [Google Scholar] [CrossRef] [PubMed]
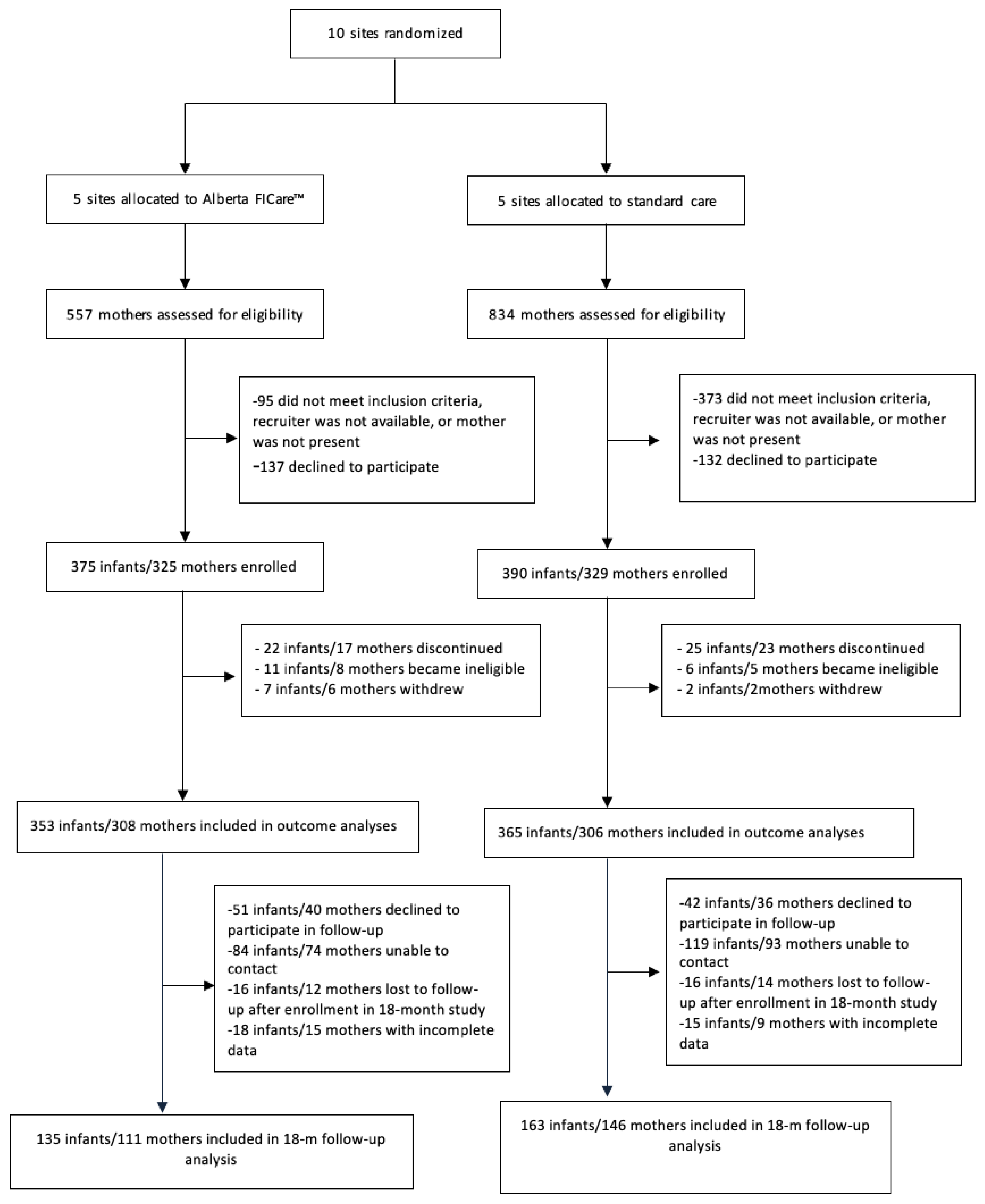
- Benzies, K.M.; Shah, V.; Aziz, K.; Isaranuwatchai, W.; Palacio-Derflingher, L.; Scotland, J.; Larocque, J.; Mrklas, K.; Suter, E. Family Integrated Care (FICare) in Level II Neonatal Intensive Care Units: Study protocol for a cluster randomized controlled trial. Trials, 2017; 47. [Google Scholar]
- Haward, M.F.; Lantos, J.; Janvier, A. Helping parents cope in the NICU. Pediatrics 2020, 145, e20193567. [Google Scholar] [CrossRef] [PubMed]
- Faleschini, S.; Matte-Gagné, C.; Côté, S.; Tremblay, R.E.; Boivin, M. Trajectories of behavioral problems among moderate-late preterm children from 4 to 10 years: A prospective population-based study. Early Human Development 2020, 143, 104964. [Google Scholar] [CrossRef] [PubMed]
- O’brien, K.; Robson, K.; Bracht, M.; Cruz, M.; Lui, K.; Alvaro, R.; Silva, O.D.; Monterrosa, L.; Narvey, M.; Ng, E. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomized controlled trial. The Lancet Child & Adolescent Health 2018, 2, 245–254. [Google Scholar]
- Larsen, M.L.; Wiingreen, R.; Jensen, A.; Rackauskaite, G.; Laursen, B.; Hansen, B.M.; Hoei-Hansen, C.E.; Greisen, G.; et al. The effect of gestational age on major neurodevelopmental disorders in preterm infants, 2022.
- Hartzell, G.; Shaw, R.J.; Givrad, S. Preterm infant mental health in the neonatal intensive care unit: A review of research on NICU parent-infant interactions and maternal sensitivity. Infant Mental Health Journal, 2023, 44, 837–856. [Google Scholar] [CrossRef]
- Wasylak, T.; Benzies, K.; Mcneil, D.; Zanoni, P.; Osiowy, K.; Mullie, T.; Chuck, A. Creating Value Through Learning Health Systems 2023.
- Ding, X.; Zhu, L.; Zhang, R.; Wang, L.; Wang, T.T.; Latour, J.M. Effects of family-centred care interventions on preterm infants and parents in neonatal intensive care units: a systematic review and meta-analysis of randomized controlled trials. Australian Critical Care, 2019, 32, 63–75. [Google Scholar] [CrossRef]
- Roque, A.T.F.; Lasiuk, G.C.; Radünz, V.; Hegadoren, K. Scoping review of the mental health of parents of infants in the NICU. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 46, 576–587.
- Cheong, J.; Doyle, L.; Burnett, A.; Lee, K.; Walsh, J.; Potter, C.; Treyvaud, K.; Thompson, D.; Olsen, J.; Anderson, P. Association between moderate and late preterm birth and neurodevelopment and social-emotional development at age 2 years 2017.
- Treyvaud, K.; Spittle, A.; Anderson, P.J.; O’Brien, K. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Human Development 2019. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Chen, X.; Wang, Q.; Liu, L. Family-centered care interventions for preterm infants in the NICU: A systematic review and meta-analysis of randomized controlled trials. Journal of Clinical Nursing 2021, 30, 651–662. [Google Scholar]
- Labrie, N.H.; Veenendaal, N.R.V.; Ludolph, R.A.; Ket, J.C.; Schoor, S.R.V.D.; Kempen, A.A.V. Effects of parent-provider communication during infant hospitalization in the NICU on parents: A systematic review with meta-synthesis and narrative synthesis. Patient Education and Counseling 2021, 104, 1526–1552. [Google Scholar] [CrossRef]
- Øberg, G.K.; Sørvoll, M.; Labori, C.; Girolami, G.L.; Håkstad, R.B. A systematic synthesis of qualitative studies on parents’ experiences of participating in early intervention programs with their infant born preterm. Frontiers in Psychology 2023, 1172578. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.H.S. ; Shefaly. Effectiveness of psychosocial interventions on the psychological outcomes of parents with preterm infants: A systematic review and meta-analysis. Journal of Pediatric Nursing, 2024; 23–34. [Google Scholar]
- Squires, J.; Bricker, D. Ages & Stages Questionnaires - Third Edition (ASQ-3): A parent-completed child monitoring system. Brookes. 2009. [Google Scholar]
- Briggs-Gowan, M.; Carter, A. Brief Infant-Toddler Social and Emotional Assessment Examiner’s Manual. Pearson. 2006. [Google Scholar]
- Benzies, K.M.; Magill-Evans, J.E.; Hayden, K.A.; Ballantyne, M. Key components of early intervention programs for preterm infants and their parents: a systematic review and meta-analysis. BMC Pregnancy and Childbirth 2013, 13. [Google Scholar] [CrossRef]
- Squires, J.; Bricker, D.; Twombly, E. Ages & Stages Questionnaires®: Social-Emotional, Second Edition (ASQ:SE-2TM). Brookes. 2015. [Google Scholar]
- Franck, L.S.; Waddington, C.; O’Brien, K. Family integrated care for preterm infants. Critical Care Nursing Clinics of North America 2020, 32, 149–165. [Google Scholar] [CrossRef]
- Chawanpaiboon, S. ; Vogel,.P.; Moller, A.B.; Lumbiganon, P.; Petzold, M.; Hogan, D.; Landoulsi, S.; Jampathong, N. Global, Regional, and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis. 2019.
- He, F.B.; Axelin, A.; Ahlqvist-Bjorkroth, S.; Raiskola, S.; Loyttyniemi, E. Effectiveness of the Close Collaboration with Parents intervention on parent-infant closeness in the NICU. Translational Pediatrics 2020, 9, S3–S8. [Google Scholar] [CrossRef]
- Natarajan, G.; Shankaran, S. Short-and long-term outcomes of moderate and late preterm infants. American Journal of Perinatology 2016, 33, 305–317. [Google Scholar] [PubMed]
- Synnes, A.R.; Petrie, J.; Grunau, R.E.; Church, P.; Kelly, E.; Moddemann, D.; Ye, X.; Lee, S.K.; O’Brien, K. Family integrated care: very preterm neurodevelopmental outcomes at 18 months. Archives of Disease in Childhood: Fetal and Neonatal Edition, Advance online publication. 2021. [Google Scholar]
- Hei, M.; Gao, X.; Li, Y.; Gao, X.; Li, Z.; Xia, S.; Zhang, Q.; Han, S.; Gao, H.; Nong, S. Family integrated care for preterm infants in China: A cluster randomized controlled trial. The Journal of Pediatrics 2021, 36–43. [Google Scholar] [CrossRef]
- Mclean, M.A.; Scoten, O.C.; Yu, W.; Xiang, Y.; Ye, J.; Petrie, P.T.; Church, A.S.; Soraisham, L.S.M.; Weinberg, J.; Synnes, A.R. Lower maternal chronic physiological stress and better child behavior at 18 months: Follow-up of a cluster randomized trial of Neonatal Intensive Care Unit Family Integrated Care. The Journal of Pediatrics 2022, 107–115. [Google Scholar] [CrossRef]
- Dubner, S.E.; Morales, V.A.M.C.; Marchman, R.J.; Shaw, K.E.; Melissa, T.; Scala. Maternal mental health and engagement in developmental care activities with preterm infants in the NICU. Journal of Perinatology 2023, 871–3876. [Google Scholar] [CrossRef] [PubMed]
- The Alberta Strategic Clinical Network Experience. Nursing Administration Quarterly, 37, 20–30.
- Huff, K.; Rose, R.S.; Engle, W.A. Late preterm infants: morbidities, mortality, and management recommendations, 2019.
- Ward, V. C. , Lee, A. C., Hawken, S., Otieno, N. A., Mujuru, H. A., Chimhini, G., Darmstadt, G. L. (2024). Overview of the Global and US Burden of Preterm Birth. Clinics in Perinatology.
- Benzies, K.M.; Aziz, K.; Shah, V.; Faris, P.; Isaranuwatchai, W.; Scotland, J.; Larocque, J.; Mrklas, K.J.; Naugler, C.; Stelfox, H.T.; et al. Effectiveness of Alberta Family Integrated Care on infant length of stay in level II neonatal intensive care units: a cluster randomized controlled trial. BMC Pediatrics 2020, 535. [Google Scholar] [CrossRef]
- Spielberger, C. D. , Gorsuch, R. L., & Lushene, R. E. (1970). Test manual for the State-Trait Anxiety Inventory, Consulting Psychologists Press: Palo Alto, CA.
- Bronfenbrenner, U. The bioecological theory of human development. In U. Bronfenbrenner (Ed.), Making human beings human: biological perspectives on human development. Sage, 2005; 3–15. [Google Scholar]
- Schwarzer, R.; Jerusalem, M. Generalized Self-Efficacy scale. In J. Weinman, S. Wright, & M. Johnston (Eds.), Measures in health psychology: a user’s portfolio. Causal and control beliefs. NFER-NELSON, 1995, 35–37.
- Church, P.T.; Grunau, R.E.; Mirea, L.; Petrie, J.; Soraisham, A.S.; Synnes, A. Family Integrated Care (FICare): Positive impact on behavioural outcomes at 18 months. Early Human Development 2020, 15. [Google Scholar] [CrossRef]
- Spittle, A. Orton, J., Anderson, P. J., Boyd, R., & Doyle, L. W. (2015). Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database of Systematic Reviews, 11, CD005495.
- Jin, J. H. Yoon, S. W., Song, J., Kim, S. W., & Chung, H. J. (2020). Long-term cognitive, executive, and behavioral outcomes of moderate and late preterm at school age. Clinical and Experimental Pediatrics, 63, 219-225.
- Abidin, R. R. (2012). Parenting Stress Index, Fourth Edition Short Form. Lutz, FL: Psychological Assessment Resource.
- de Gamarra-Oca, L.F.; Ojeda, N.; Gómez-Gastiasoro, A.; Peña, J.; Ibarretxe-Bilbao, N.; García-Guerrero, M.A.; Loureiro, B. Long-term neurodevelopmental outcomes after moderate and late preterm birth: a systematic review. The Journal of Pediatrics, 168–176.
- Stuart, A.C.; Egmose, M.; Guedeney, I.; Væver, A.S.M. Associations between symptoms of maternal postpartum depression, gestational age and infant social withdrawal: A longitudinal study in a community cohort. British Journal of Developmental Psychology 2022. [Google Scholar] [CrossRef]
- Soleimani, F.; Azari, N.; Ghiasvand, H.; Shahrokhi, A.; Rahmani, N. Do NICU developmental care improve cognitive and motor outcomes for preterm infants? A systematic review and meta-analysis. BMC Pediatrics, 2020; 67. [Google Scholar]
- Karnati, S.; Kollikonda, S.; Abu-Shaweesh, J.; et al. Late preterm infants-changing trends and continuing challenges. International Journal of Pediatrics and Adolescent Medicine 2020, 7, 38–46. [Google Scholar] [CrossRef]
- Crump, C. An overview of adult health outcomes after preterm birth. Early Human Development 2020, 105187–105187. [Google Scholar] [CrossRef] [PubMed]
- Yui, V. , Gordon, D., Woods, S., & Pougnet, J. (2015). The patient first strategy. Alberta Canada: Alberta Health Services.
- Quitadamo, P.A.; Zambianco, F.; Palumbo, G.; Wagner, X.; Gentile, M.A. Monitoring the Use of Human Milk, the Ideal Food for Very Low-Birth-Weight Infants—A Narrative Review. Foods 2024, 13, 649. [Google Scholar] [CrossRef]
- Zhang, X. Kurtz, M., Lee, S.-Y., & Liu, H. (2021). Early intervention for preterm infants and their mothers: a systematic review. The Journal of Perinatal & Neonatal Nursing, 35, E69-E82.
- Chung, H.; Chou, E.; Brown, J. A. K. Neurodevelopmental outcomes of preterm infants: a recent literature review. Translational Pediatrics 2020, 9, S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Synnes, A.; Hicks, M. Neurodevelopmental Outcomes of Preterm Children at School Age and Beyond. Clinics in Perinatology.
- Eaton, W. Muntaner, C., Smith, C., A, T., & Ybarra, M. (2004). Center for Epidemiologic Studies Depression Scale: review and revision (CESD and CESD-R). In M. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment. Volume 3: instruments for adults (3rd ed., 363-377). Mahwah, NJ: Lawrence Erlbau.
- Givrad, S. , Hartzell, G., & Scala, M. (2021). Promoting infant mental health in the neonatal intensive care unit (NICU): A review of nurturing factors and interventions for NICU infant-parent relationships. Early Human Development, 154, 105281.
- Lodha, A.; Lakhani, J.; Ediger, K.; Tang, S.; Lodha, A.; Gandhi, V.; Creighton, D. Do preterm infants with a birth weight 1250g born to single-parent families have poorer neurodevelopmental outcomes at age 3 than those born to two-parent families? Journal of Perinatology 2018, 900–907. [Google Scholar] [CrossRef] [PubMed]
| Measure | Description |
|---|---|
| Ages and Stages Questionnaires, 3rd Edition (ASQ- 3) [21] | Widely used developmental screening instrument consisting of 21 age-appropriate questionnaires for use with infants and children 2 to 60 months of age. Each questionnaire has 30 items that assess risk of developmental delay across five domains: communication, gross motor, fine motor, problem solving, and personal-social. For each domain, age-specific cut-off scores have been empirically derived for appropriate development, monitoring zone (1 and > standard deviations below the mean) or referral required (1 standard deviation below the mean). Sensitivity (0.86) and specificity (0.85) are high. For this study we use referral in any domain to denote risk. |
| Ages and Stages Questionnaires: Social-Emotional, 2nd Edition (ASQ:SE-2) [24] | Widely used screening instrument for social and emotional difficulties in infants and children 2 to 60 months of age. Consists of 9 age-appropriate questionnaires, with about 30 items per questionnaire. Total scores are compared to empirically derived age-specific cut-offs for appropriate social-emotional development, monitoring zone (≥1 and <2 standard deviations below the mean), or referral required (≥2 standard deviations below the mean). Sensitivity (0.81), specificity (0.84), test-retest reliability (0.89), and internal consistency reliability (0.84) are all high. For this study, we collapsed monitoring and referral categories to denote risk. |
| Brief Infant Toddler Social Emotional Assessment (BITSEA) [22] | Valid and reliable screening instrument designed to identify emerging social-emotional and behavioral problems in children between the ages of 12 and 36 months. Consists of 42 items and provides total scores on two subscales: Problem Behavior and Competence. Age and gender specific cut-off scores have been empirically derived for each subscale to identify children at risk of delay in social-emotional development. For this study, we collapsed risk on problem and competence subscales to denote risk. |
| Center for Epidemiologic Studies Depression Scale – Revised (CESD-R) [54] | Self-report measure of depressive symptoms for the general population. Consists of 20 items rated on a 4-point Likert scale. Items are summed to calculate a total score; higher scores indicate greater depressive symptoms. Theoretical scores range from 0 to 60. Internal consistency reliabilities (0.85 to 0.90) are high and test-retest reliabilities (0.45 to 0.70) are moderate. |
| State-Trait Anxiety Inventory (STAI) [37] | Self-report measure of current (state) and dispositional (trait) anxiety. Consists of 40 items, 20 per subscale, rated on a 4-point Likert scale. Items are summed to calculate a total score for each subscale; higher scores indicate greater anxiety. Internal consistency (0.86 to 0.95) and test-retest reliabilities (0.73 to 0.86) are high. Only state anxiety was measured in this study. |
| Parenting Stress Index, 4th Edition Short Form (PSI-4-SF) [43] | Self-report measure of parenting stress across three domains: parental distress, parent-child dysfunctional interaction, and difficult child. Consists of 36 items rated on a 5-point Likert scale. Items are summed to calculate domain scores and a Total Stress score. Theoretical scores range from 12 to 60 for each domain and 36 to 180 for Total Stress; higher scores indicate greater parenting stress. Internal consistency reliability coefficients (0.95 for Total Stress and 0.88 to 0.90 for subscales) are high. Test-retest studies were not conducted for this version of the instrument. |
| General Self- Efficacy (GSE) [39] | Self-report measure of self-efficacy consisting of 10 items measured on a 4-point Likert scale. Theoretical scores range between 10 and 40. Items are summed to calculate a total score; higher scores indicate greater self-efficacy. Internal consistency reliability is high (0.76 to 0.90 across samples). |
| Alberta FICare | Standard Care | P(χ2) | |||
|---|---|---|---|---|---|
| No. | Frequency (%) | No. | Frequency (%) | ||
| Child Characteristics | |||||
| Singleton (% yes) | 163 | 129 (79.1) | 135 | 87 (64.4) | .005 |
| Gestational age at birth (% yes) | 163 | 135 | .463 | ||
| 32 weeks | 41 (25.2) | 29 (21.5) | |||
| 33 weeks | 48 (29.5) | 35 (25.9) | |||
| 34 weeks | 74 (45.4) | 71 (52.6) | |||
| Male (% yes) | 163 | 86 (52.8) | 135 | 77 (57.0) | .460 |
| Caesarean delivery (% yes) | 163 | 76 (46.6) | 135 | 69 (51.1) | .441 |
| Maternal Characteristic | |||||
| Relationship status (% yes) | 147 | 116 | .597 | ||
| Single | 7 (4.8) | 4 (3.4) | |||
| Partnered | 140 (95.2) | 112 (96.6) | |||
| Employment (% yes) | 148 | 116 | .231 | ||
| Employed full- or part-time | 108 (73.0) | 86 (74.1) | |||
| Homemaker/not in the labor force | 26 (17.6) | 24 (20.7) | |||
| Unemployed and looking for work | 8 (5.4) | 1 (0.9) | |||
| Other a | 6. (4.1) | 5 (4.3) | |||
| Education (% yes) | 160 | 134 | .846 | ||
| High school diploma or less | 28 (17.5) | 22 (16.4) | |||
| Postsecondary certificate/diploma | 43 (26.9) | 33 (24.6) | |||
| College/university degree | 89 (55.6) | 79 (59.0) | |||
| Annual family Income (CAD) (% yes) | 159 | 132 | .782 | ||
| < $40,000 | 7 (4.4) | 8 (6.1) | |||
| $40,000 to $79,999 | 22 (13.8) | 20 (15.2) | |||
| ≥ $80,000 | 108 (67.9) | 90 (68.2) | |||
| Prefer not to answer/don’t know | 22 (13.8) | 14 (10.6) | |||
| Born in Canada (% yes) | 160 | 131 (81.9) | 134 | 103 (76.9) | .289 |
| Ethnicity (% Caucasian) | 161 | 132 (81.0) | 134 | 93 (69.4) | .011 |
| Child Assessments | No. | Alberta FICare | No. | Standard Care |
|---|---|---|---|---|
| Frequency (%) | Frequency (%) | |||
| ASQ-3 Domains | ||||
| Communication | 154 | 129 | ||
| Referral | 4 (2.6) | 1 (0.8) | ||
| Gross Motor | 154 | 129 | ||
| Referral | 11 (7.1) | 5 (3.9) | ||
| Fine Motor | 154 | 129 | ||
| Referral | 8 (5.2) | 3 (2.3) | ||
| Problem Solving | 152 | 127 | ||
| Referral | 14 (9.2) | 6 (4.7) | ||
| Personal-Social | 154 | 129 | ||
| Referral | 3 (1.9) | 2 (1.6) | ||
| Any Domain | 152 | 128 | ||
| Referral | 23 (15.1) | 16 (12.5) | ||
| ASQ:SE-2 | 157 | 122 | ||
| Referral | 10 (6.4) | 7 (5.7) | ||
| BITSEA | ||||
| Problem Behavior | 155 | 124 | ||
| Risk | 27 (17.4) | 22 (17.7) | ||
| Competence | 155 | 124 | ||
| Risk | 11 (7.1) | 15 (12.1) | ||
| Any Subscale | 155 | 124 | ||
| Risk | 33 (21.3) | 30 (24.2) |
| No. | FICare Mean (SD) |
No. | Standard Care Mean (SD) |
|
|---|---|---|---|---|
| Maternal scales | ||||
| CESD-R | 151 | 7.40 (8.62) | 118 | 6.47 (8.86) |
| STAI State Anxiety | 151 | 32.70 (10.18) | 117 | 32.86 (10.84) |
| PSI-4-SF | ||||
| Total Stress | 152 | 61.53 (17.13) | 113 | 64.89 (19.85) |
| Parental Distress subscale | 152 | 23.74 (8.02) | 113 | 24.84 (9.32) |
| Parent-Child Dysfunctional Interaction subscale | 152 | 17.52 (5.55) | 113 | 18.72 (5.78) |
| Difficult Child subscale | 152 | 20.28 (5.95) | 113 | 21.34 (6.93) |
| GSE | 151 | 33.06 (4.53) | 117 | 33.23 (4.39) |
| Variable | ASQ-3 | ASQ:SE-2 | BITSEA |
|---|---|---|---|
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Constant | .110 | 17.053 | 12.578 |
| Socio-demographics | |||
| Marital status | .255 (.64, 1.009) * | .118(.021, .662) ** | .896 (.211, 3.800) |
| Maternal age | 1.043 (.968, 1.124) | .958 (.847, 1.083) | .953 (.893, 1.018) |
| Maternal Education | .895 (.522, 1.535) | .641 (.275, 1.496) | .379 (.474, 1.151) |
| Born in Canada | .836 (.328, 2.130) | .192 (.055, .675) ** | .373 (.174, .802) ** |
| Maternal psychosocial distress | |||
| CESD-R | .981 (.928, 1.037) | .993 (.928, 1.061) | 1.012 (.961, 1.066) |
| STAI | 1.000 (.949, 1.054) | .977 (.908, 1.052) | .976 (.931, 1.023) |
| PSI (total) | 1.046 . (1.017, 1.075) ** | 1.061 (1.017,1.107) ** | 1.033 (1.009, 1.057) ** |
| Maternal self-efficacy | |||
| GSE | .993 (.893, 1.103) | .979 (.837, 1.144) | .937 (.863, 1.017) |
| Group | .692 (.309, 1.548) | .601 (.166, 2.175) | 1.049 (.542, 2.029) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





