Submitted:
07 January 2025
Posted:
08 January 2025
You are already at the latest version
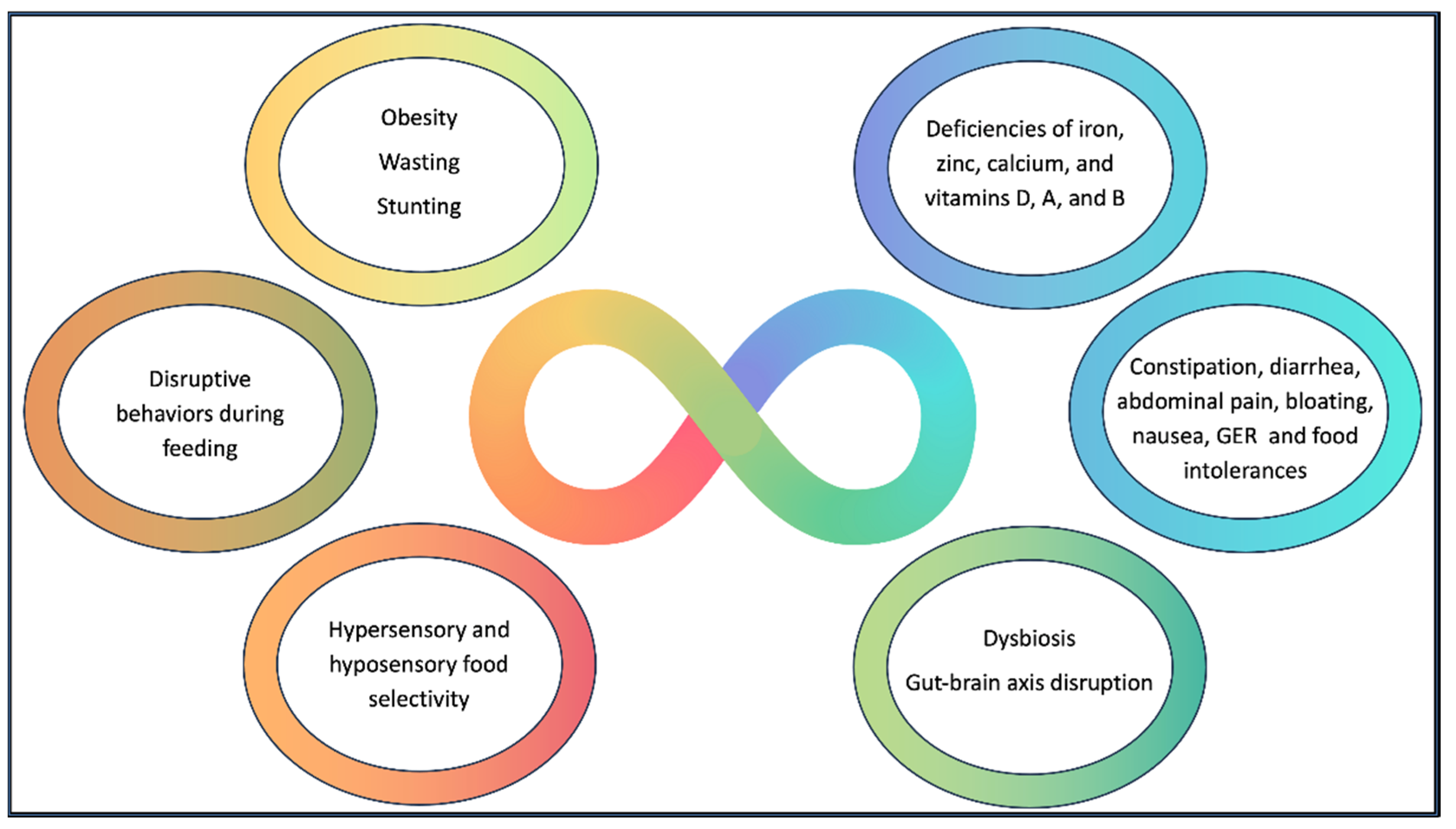
Abstract
Keywords:
1. Introduction
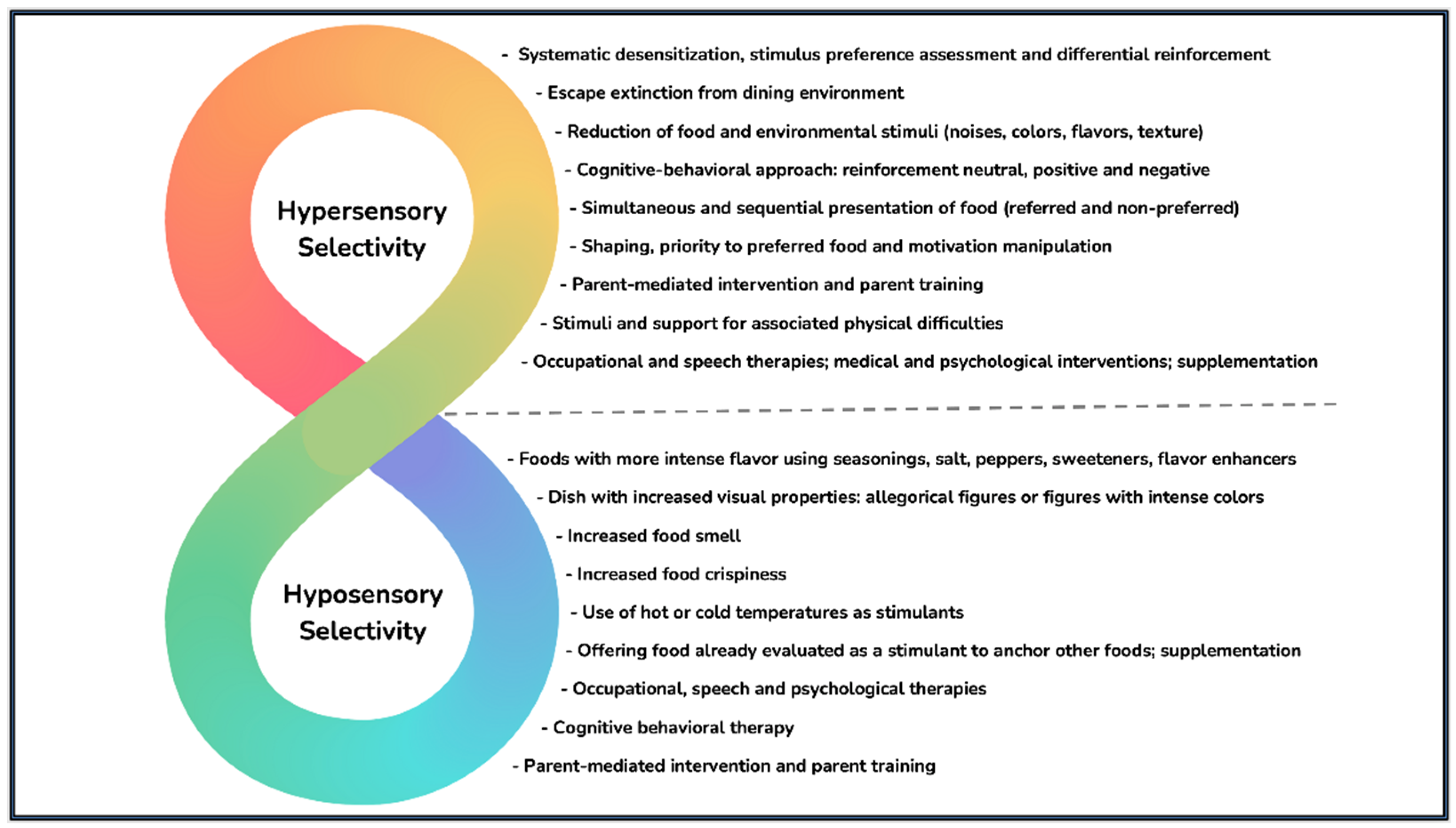
2. Eating Behavior
3. Macro and Micronutrients
4. Underweight and Obesity
5. Gastrointestinal Issues
6. Microbiota
7. Limitations
8. Conclusion
References
- APA. Diagnostic and Statistical Manual of Mental Disorders. 5th ed: American Psychiatric Publishing (2014).
- CDC. Prevalence of Autism Spectrum Disorder among Children Aged 8 Years — United States, 2020. Centers for Disease Control and Prevention, (2020).
- Esposito M, Mirizzi P, Fadda R, Pirollo C, Ricciardi O, Mazza M, et al. Food Selectivity in Children with Autism: Guidelines for Assessment and Clinical Interventions. Int J Environ Res Public Health (2023) 20(6). Epub 20230314. [CrossRef]
- Iglesias-Vázquez L, Van Ginkel Riba G, Arija V, Canals J. Composition of Gut Microbiota in Children with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Nutrients (2020) 12(3). [CrossRef]
- Yap CX, Henders AK, Alvares GA, Wood DLA, Krause L, Tyson GW, et al. Autism-Related Dietary Preferences Mediate Autism-Gut Microbiome Associations. Cell (2021) 184(24):5916-31.e17. Epub 20211111. [CrossRef]
- Carneiro ACdS, Moreira ES, Lisboa CS. Eating Habits and Behaviors of Children with Autism Spectrum Disorder: An Integrative Review. Research, Society and Development (2022) 11(8):e37211830976. [CrossRef]
- da Silva RV, Gomes DL. Eating Behavior and Nutritional Profile of Children with Autism Spectrum Disorder in a Reference Center in the Amazon. Nutrients (2024) 16(3):452.
- Petitpierre G, Luisier A-C, Bensafi M. Eating Behavior in Autism: Senses as a Window Towards Food Acceptance. Current Opinion in Food Science (2021) 41:210-6. [CrossRef]
- Trinh NB, Phan NDT, Bui AT, Phan HT, Nguyen LTT, Nguyen LHT, et al. Nutritional Status and Eating Behavior of Children with Autism Spectrum Disorders in Vietnam: A Case-Control Study. Nutrition and Health (2023):02601060231152278. [CrossRef]
- Lázaro CP, Pondé MP. Narratives of Mothers of Children with Autism Spectrum Disorders: Focus on Eating Behavior. Trends in Psychiatry and Psychotherapy (2017) 39. [CrossRef]
- Plaza-Diaz J, Flores-Rojas K, Torre-Aguilar MJ, Gomez-Fernandez AR, Martin-Borreguero P, Perez-Navero JL, et al. Dietary Patterns, Eating Behavior, and Nutrient Intakes of Spanish Preschool Children with Autism Spectrum Disorders. Nutrients (2021) 13(10):3551. Epub 20211010. [CrossRef]
- Lemes MA, Garcia GP, Carmo BLd, Santiago BA, Teixeira DDB, Agostinho Junior F, et al. Comportamento Alimentar De Crianças Com Transtorno Do Espectro Autista. Jornal Brasileiro de Psiquiatria (2023) 72. [CrossRef]
- Nadeau MV, Richard E, Wallace GL. The Combination of Food Approach and Food Avoidant Behaviors in Children with Autism Spectrum Disorder: "Selective Overeating". Journal of Autism and Developmental Disorders (2022) 52:987+. [CrossRef]
- Nogueira-de-Almeida CA, Del Ciampo LA, Ued FdV, Ferraz IS, Contini AA, Epifanio M, et al. Feeding Difficulties among Brazilian Children: Prevalence and Associated Factors. Research, Society and Development (2022) 11(13). [CrossRef]
- Wenzell ML, Pulver SL, McMahon MXH, Rubio EK, Gillespie S, Berry RC, et al. Clinical Correlates and Prevalence of Food Selectivity in Children with Autism Spectrum Disorder. The Journal of Pediatrics (2024) 269:114004. [CrossRef]
- Kozak A, Czepczor-Bernat K, Modrzejewska J, Modrzejewska A, Matusik E, Matusik P. Avoidant/Restrictive Food Disorder (Arfid), Food Neophobia, Other Eating-Related Behaviours and Feeding Practices among Children with Autism Spectrum Disorder and in Non-Clinical Sample: A Preliminary Study. Int J Environ Res Public Health (2023) 20(10). Epub 20230514. [CrossRef]
- Rodrigues JVS, Poli MCF, Petrilli PH, Dornelles RCM, Turcio KH, Theodoro LH. Food Selectivity and Neophobia in Children with Autism Spectrum Disorder and Neurotypical Development: A Systematic Review. Nutr Rev (2023) 81(8):1034-50. [CrossRef]
- Hodges A, Davis T, Crandall M, Phipps L, Weston R. Using Shaping to Increase Foods Consumed by Children with Autism. J Autism Dev Disord (2017) 47(8):2471-9. [CrossRef]
- Alibrandi A, Zirilli A, Loschiavo F, Gangemi MC, Sindoni A, Tribulato G, et al. Food Selectivity in Children with Autism Spectrum Disorder: A Statistical Analysis in Southern Italy. Children (Basel) (2023) 10(9). Epub 20230914. [CrossRef]
- St John BM, Ausderau KK. The Characterization of Feeding Challenges in Autistic Children. Autism (2024) 28(9):2381-93. Epub 20240202. [CrossRef]
- Kinnaird E, Norton C, Pimblett C, Stewart C, Tchanturia K. Eating as an Autistic Adult: An Exploratory Qualitative Study. PLoS One (2019) 14(8):e0221937. Epub 20190829. [CrossRef]
- Silva ÁGS, Chaves SPL, Almeida LNA, Nascismento RLd, Macêdo MLM, Sarmento AQ. Aspectos Sensoriais E a Seletividade Alimentar Da Criança Com Transtorno Do Espectro Autista: Um Estudo De Revisão Integrativa. Research, Society and Development (2021) 10(10). [CrossRef]
- Sarnat H, Samuel E, Ashkenazi-Alfasi N, Peretz B. Oral Health Characteristics of Preschool Children with Autistic Syndrome Disorder. Journal of Clinical Pediatric Dentistry (2016) 40(1):21-5. [CrossRef]
- Byrska A, Błażejczyk I, Faruga A, Potaczek M, Wilczyński KM, Janas-Kozik M. Patterns of Food Selectivity among Children with Autism Spectrum Disorder. Journal of Clinical Medicine [Internet]. (2023; 12(17). Available from: https://mdpi-res.com/d_attachment/jcm/jcm-12-05469/article_deploy/jcm-12-05469-v2.pdf?version=1693203876.
- Huynh DT, Estorninos E, Capeding RZ, Oliver JS, Low YL, Rosales FJ. Longitudinal Growth and Health Outcomes in Nutritionally at-Risk Children Who Received Long-Term Nutritional Intervention. J Hum Nutr Diet (2015) 28(6):623-35. Epub 20150325. [CrossRef]
- Kerzner B, Milano K, MacLean WC, Berall G, Stuart S, Chatoor I. A Practical Approach to Classifying and Managing Feeding Difficulties. Pediatrics (2015) 135(2):344-53. [CrossRef]
- Milano K, Chatoor I, Kerzner B. A Functional Approach to Feeding Difficulties in Children. Current Gastroenterology Reports (2019) 21(10). [CrossRef]
- Nogueira-de-Almeida C, de Mello E, Filho D, Maximino P, Fisberg M. Consenso Da Associação Brasileira De Nutrologia Sobre O Uso De Suplementos Alimentares Para Crianças Com Dificuldades Alimentares. International Journal of Nutrology (2018) 11(S 01):S4-S15. [CrossRef]
- Nogueira-de-Almeida CA, Del Ciampo LA, Martinez EZ, Contini AA, Nogueira-de-Almeida ME, Ferraz IS, et al. Clinical Evolution of Preschool Picky Eater Children Receiving Oral Nutritional Supplementation during Six Months: A Prospective Controlled Clinical Trial. Children (2023) 10(3). [CrossRef]
- Susilowati E, Umayah A, Diniayuningrum A. Interventions for Managing Picky Eating in Preschool Children: Literature Review. Media Publikasi Promosi Kesehatan Indonesia (MPPKI) (2024) 7(11):2584-91. [CrossRef]
- Breda C, Santero S, Conti MV, Cena H. Programmes to Manage Food Selectivity in Individuals with Autism Spectrum Disorder. Nutr Res Rev (2024):1-14. Epub 20240222. [CrossRef]
- Ahearn WH. Using Simultaneous Presentation to Increase Vegetable Consumption in a Mildly Selective Child with Autism. J Appl Behav Anal (2003) 36(3):361-5. [CrossRef]
- Sarnat H, Samuel E, Ashkenazi-Alfasi N, Peretz B. Oral Health Characteristics of Preschool Children with Autistic Syndrome Disorder. J Clin Pediatr Dent (2016) 40(1):21-5. [CrossRef]
- Soares RCS, Candido FG, Filgueiras MS, Rosa COB, de Novaes JF, Araujo RMA. Problematic Behaviors at Mealtimes and the Nutritional Status of Brazilian Children with Autism Spectrum Disorder. Front Public Health (2024) 12:1392478. Epub 20241014. [CrossRef]
- Toomey KA, Ross ES. Sos Approach to Feeding. Perspectives on Swallowing and Swallowing Disorders (Dysphagia) (2011) 20(3):82-7. [CrossRef]
- Benson JD, Parke CS, Gannon C, Muñoz D. A Retrospective Analysis of the Sequential Oral Sensory Feeding Approach in Children with Feeding Difficulties. Journal of Occupational Therapy, Schools, & Early Intervention (2013) 6(4):289-300. [CrossRef]
- Maitin-Shepard M, O'Tierney-Ginn P, Kraneveld AD, Lyall K, Fallin D, Arora M, et al. Food, Nutrition, and Autism: From Soil to Fork. Am J Clin Nutr (2024) 120(1):240-56. Epub 20240425. [CrossRef]
- Keski-Rahkonen A, Ruusunen A. Avoidant-Restrictive Food Intake Disorder and Autism: Epidemiology, Etiology, Complications, Treatment, and Outcome. Curr Opin Psychiatry (2023) 36(6):438-42. Epub 20230829. [CrossRef]
- Nyholmer M, Wronski M-L, Hog L, Kuja-Halkola R, Lichtenstein P, Lundström S, et al. (2024). [CrossRef]
- Wronski M-L, Kuja-Halkola R, Hedlund E, Martini MI, Lichtenstein P, Lundström S, et al. (2024). [CrossRef]
- James RM, O’Shea J, Micali N, Russell SJ, Hudson LD. Physical Health Complications in Children and Young People with Avoidant Restrictive Food Intake Disorder (Arfid): A Systematic Review and Meta-Analysis. BMJ Paediatrics Open (2024) 8(1). [CrossRef]
- Thomas JJ, Lawson EA, Micali N, Misra M, Deckersbach T, Eddy KT. Avoidant/Restrictive Food Intake Disorder: A Three-Dimensional Model of Neurobiology with Implications for Etiology and Treatment. Current Psychiatry Reports (2017) 19(8). [CrossRef]
- Thomas JJ, Wons OB, Eddy KT. Cognitive–Behavioral Treatment of Avoidant/Restrictive Food Intake Disorder. Current Opinion in Psychiatry (2018) 31(6):425-30. [CrossRef]
- Hyman SL, Levy SE, Myers SM, Council On Children With Disabilities SOD, Behavioral P. Identification, Evaluation, and Management of Children with Autism Spectrum Disorder. Pediatrics (2020) 145(1). Epub 20191216. [CrossRef]
- Nadon G, Feldman DE, Dunn W, Gisel E. Association of Sensory Processing and Eating Problems in Children with Autism Spectrum Disorders. Autism Research and Treatment (2011) 2011:1-8. [CrossRef]
- Bahadir A, Reis PG, Erduran E. Oral Vitamin B12 Treatment Is Effective for Children with Nutritional Vitamin B12 Deficiency. Journal of Paediatrics and Child Health (2014) 50(9):721-5. [CrossRef]
- Bastos Maia S, Rolland Souza AS, Costa Caminha MdF, Lins da Silva S, Callou Cruz RdSBL, Carvalho dos Santos C, et al. Vitamin a and Pregnancy: A Narrative Review. Nutrients (2019) 11(3). [CrossRef]
- Chandra J, Dewan P, Kumar P, Mahajan A, Singh P, Dhingra B, et al. Diagnosis, Treatment and Prevention of Nutritional Anemia in Children: Recommendations of the Joint Committee of Pediatric Hematology-Oncology Chapter and Pediatric and Adolescent Nutrition Society of the Indian Academy of Pediatrics. Indian Pediatr (2022) 59(10):782-801.
- Devalia V, Hamilton MS, Molloy AM. Guidelines for the Diagnosis and Treatment of Cobalamin and Folate Disorders. British Journal of Haematology (2014) 166(4):496-513. [CrossRef]
- Hemamy M, Pahlavani N, Amanollahi A, Islam SMS, McVicar J, Askari G, et al. The Effect of Vitamin D and Magnesium Supplementation on the Mental Health Status of Attention-Deficit Hyperactive Children: A Randomized Controlled Trial. BMC Pediatrics (2021) 21(1). [CrossRef]
- Imdad A, Rogner J, Sherwani RN, Sidhu J, Regan A, Haykal MR, et al. Zinc Supplementation for Preventing Mortality, Morbidity, and Growth Failure in Children Aged 6 Months to 12 Years. Cochrane Database of Systematic Reviews (2023) 2023(3). [CrossRef]
- Kaczmarek KA, Dobrzyńska M, Drzymała-Czyż S. Iron, Magnesium, Zinc and Selenium - the Most Common Elemental Deficiencies in Children with Autism Spectrum Disorder. Research in Autism Spectrum Disorders (2024) 110. [CrossRef]
- Khan KM, Jialal I. Folic Acid Deficiency. Statpearls. Treasure Island (FL)(2024).
- McGuire S. Who Guideline: Vitamin a Supplementation in Pregnant Women. Geneva: Who, 2011; Who Guideline: Vitamin a Supplementation in Postpartum Women. Geneva: Who, 2011. Advances in Nutrition (2012) 3(2):215-6. [CrossRef]
- Mousain-Bosc M, Siatka C, Bali JP. Magnesium, Hyperactivity and Autism in Children. In: Vink R, Nechifor M, editors. Magnesium in the Central Nervous System. Adelaide (AU): University of Adelaide Press. © 2011 The Authors. (2011).
- Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, et al. Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. The Journal of Clinical Endocrinology & Metabolism (2016) 101(2):394-415. [CrossRef]
- Nogueira-de-Almeida CA, Fernandes SL, Soriano EdA, Lourenço DM, Zotarelli Filho IJ, Iucif Junior N, et al. Consensus of the Brazilian Association of Nutrology on Diagnosis, Prophylaxis, and Treatment of Vitamin B12 Deficiency. International Journal of Nutrology (2023) 16(1). [CrossRef]
- Rasmussen SA, Fernhoff PM, Scanlon KS. Vitamin B12 Deficiency in Children and Adolescents. The Journal of Pediatrics (2001) 138(1):10-7. [CrossRef]
- Ross DA. Recommendations for Vitamin a Supplementation. The Journal of Nutrition (2002) 132(9):2902S-6S. [CrossRef]
- Sezer RG, Bozaykut A, Akoğlu HA, Özdemir GN. The Efficacy of Oral Vitamin B12 Replacement for Nutritional Vitamin B12 Deficiency. Journal of Pediatric Hematology/Oncology (2018) 40(2):e69-e72. [CrossRef]
- Srinivasan S, O'Rourke J, Bersche Golas S, Neumeyer A, Misra M. Calcium and Vitamin D Supplement Prescribing Practices among Providers Caring for Children with Autism Spectrum Disorders: Are We Addressing Bone Health? Autism Res Treat (2016) 2016:6763205. Epub 2016/04/05. [CrossRef]
- Valavi E, Hakimzadeh M, Shamsizadeh A, Aminzadeh M, Alghasi A. The Efficacy of Zinc Supplementation on Outcome of Children with Severe Pneumonia. A Randomized Double-Blind Placebo-Controlled Clinical Trial. Indian J Pediatr (2011) 78(9):1079-84. Epub 2011/06/11. [CrossRef]
- Weinstein M, Babyn P, Zlotkin S. An Orange a Day Keeps the Doctor Away: Scurvy in the Year 2000. Pediatrics (2001) 108(3):e55-e. [CrossRef]
- Peretti S, Mariano M, Mazzocchetti C, Mazza M, Pino MC, Verrotti Di Pianella A, et al. Diet: The Keystone of Autism Spectrum Disorder? Nutritional Neuroscience (2018) 22(12):825-39. [CrossRef]
- Molina-López J, Leiva-García B, Planells E, Planells P. Food Selectivity, Nutritional Inadequacies, and Mealtime Behavioral Problems in Children with Autism Spectrum Disorder Compared to Neurotypical Children. International Journal of Eating Disorders (2021) 54(12):2155-66. [CrossRef]
- Omaña Covarrubias A, Hernández Fernández IG, Conde Vega J, Rodríguez Ávila J, Díaz Martínez G, Moya Escalera A, et al. Nutritional Status and Food Intake Frequency in Children with Autism Spectrum Disorder. Nutrición Hospitalaria (2023). [CrossRef]
- Trinh NB, Phan NDT, Bui AT, Phan HT, Nguyen LTT, Nguyen LHT, et al. Nutritional Status and Eating Behavior of Children with Autism Spectrum Disorders in Vietnam: A Case-Control Study. Nutr Health (2023):2601060231152278. Epub 20230127. [CrossRef]
- Narzisi A, Masi G, Grossi E. Nutrition and Autism Spectrum Disorder: Between False Myths and Real Research-Based Opportunities. Nutrients (2021) 13(6). [CrossRef]
- Sharp WG, Postorino V, McCracken CE, Berry RC, Criado KK, Burrell TL, et al. Dietary Intake, Nutrient Status, and Growth Parameters in Children with Autism Spectrum Disorder and Severe Food Selectivity: An electronic Medical Record Review. Journal of the Academy of Nutrition and Dietetics (2018) 118(10):1943-50. [CrossRef]
- Ali F, Mouzaki M. Nutritional Deficiencies in Children. Curr Opin Gastroenterol (2024) 40(2):106-11. Epub 20240102. [CrossRef]
- G. Santiago F, D. S. Lyra E, Da Silva Pantoja P. A Systematic Review: Nutritional Status and the Effect in Autism Spectrum Disorder. Brazilian Journal of Health and Biomedical Sciences (2024) 23(1). [CrossRef]
- Adams JB, Kirby J, Audhya T, Whiteley P, Bain J. Vitamin/Mineral/Micronutrient Supplement for Autism Spectrum Disorders: A Research Survey. BMC Pediatr (2022) 22(1):590. Epub 20221013. [CrossRef]
- Al-Beltagi M, Saeed NK, Bediwy AS, Elbeltagi R, Alhawamdeh R. Role of Gastrointestinal Health in Managing Children with Autism Spectrum Disorder. World J Clin Pediatr (2023) 12(4):171-96. Epub 20230909. [CrossRef]
- Arija V, Esteban-Figuerola P, Morales-Hidalgo P, Jardi C, Canals-Sans J. Nutrient Intake and Adequacy in Children with Autism Spectrum Disorder: Epined Epidemiological Study. Autism (2023) 27(2):371-88. Epub 20220620. [CrossRef]
- De Moraes LS, Bubolz VK, Marques AyC, Borges LR, Muniz LC, Bertacco RTA. Seletividade Alimentar Em Crianças E Adolescente Com Transtorno Do Espectro Autista. Revista da Associação Brasileira de Nutrição - RASBRAN (2021) 12(2):42-58. [CrossRef]
- Kittana M, Ahmadani A, Williams KE, Attlee A. Nutritional Status and Feeding Behavior of Children with Autism Spectrum Disorder in the Middle East and North Africa Region: A Systematic Review. Nutrients (2023) 15(3). Epub 20230130. [CrossRef]
- Li YJ, Xie XN, Lei X, Li YM, Lei X. Global Prevalence of Obesity, Overweight and Underweight in Children, Adolescents and Adults with Autism Spectrum Disorder, Attention-Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Obesity Reviews (2020) 21(12). [CrossRef]
- Sammels O, Karjalainen L, Dahlgren J, Wentz E. Autism Spectrum Disorder and Obesity in Children: A Systematic Review and Meta-Analysis. Obes Facts (2022) 15(3):305-20. Epub 20220309. [CrossRef]
- Esteban-Figuerola P, Canals J, Fernández-Cao JC, Arija Val V. Differences in Food Consumption and Nutritional Intake between Children with Autism Spectrum Disorders and Typically Developing Children: A Meta-Analysis. Autism (2018) 23(5):1079-95. [CrossRef]
- Neumeyer AM, Cano Sokoloff N, McDonnell EI, Macklin EA, McDougle CJ, Holmes TM, et al. Nutrition and Bone Density in Boys with Autism Spectrum Disorder. J Acad Nutr Diet (2018) 118(5):865-77. Epub 20180302. [CrossRef]
- Sharp WG, Berry RC, McCracken C, Nuhu NN, Marvel E, Saulnier CA, et al. Feeding Problems and Nutrient Intake in Children with Autism Spectrum Disorders: A Meta-Analysis and Comprehensive Review of the Literature. J Autism Dev Disord (2013) 43(9):2159-73. [CrossRef]
- Tomova A, Soltys K, Kemenyova P, Karhanek M, Babinska K. The Influence of Food Intake Specificity in Children with Autism on Gut Microbiota. Int J Mol Sci (2020) 21(8). Epub 20200417. [CrossRef]
- Yule S, Wanik J, Holm EM, Bruder MB, Shanley E, Sherman CQ, et al. Nutritional Deficiency Disease Secondary to Arfid Symptoms Associated with Autism and the Broad Autism Phenotype: A Qualitative Systematic Review of Case Reports and Case Series. Journal of the Academy of Nutrition and Dietetics (2021) 121(3):467-92. [CrossRef]
- da Silva RV, Gomes DL. Eating Behavior and Nutritional Profile of Children with Autism Spectrum Disorder in a Reference Center in the Amazon. Nutrients (2024) 16(3). [CrossRef]
- Magagnin T, Silva MAd, Nunes RZdS, Ferraz F, Soratto J. Aspectos Alimentares E Nutricionais De Crianças E Adolescentes Com Transtorno Do Espectro Autista. Physis: Revista de Saúde Coletiva (2021) 31(1). [CrossRef]
- Marinov D, Chamova R, Pancheva R. Micronutrient Deficiencies in Children with Autism Spectrum Disorders Compared to Typically Developing Children – a Scoping Review. Research in Autism Spectrum Disorders (2024) 114. [CrossRef]
- Meguid NA, Anwar M, Bjorklund G, Hashish A, Chirumbolo S, Hemimi M, et al. Dietary Adequacy of Egyptian Children with Autism Spectrum Disorder Compared to Healthy Developing Children. Metab Brain Dis (2017) 32(2):607-15. Epub 20170110. [CrossRef]
- Dosman CF, Brian JA, Drmic IE, Senthilselvan A, Harford MM, Smith RW, et al. Children with Autism: Effect of Iron Supplementation on Sleep and Ferritin. Pediatr Neurol (2007) 36(3):152-8. [CrossRef]
- Sidrak S, Yoong T, Woolfenden S. Iron Deficiency in Children with Global Developmental Delay and Autism Spectrum Disorder. J Paediatr Child Health (2014) 50(5):356-61. Epub 20131223. [CrossRef]
- Conti MV, Santero S, Luzzi A, Cena H. Exploring Potential Mechanisms for Zinc Deficiency to Impact in Autism Spectrum Disorder: A Narrative Review. Nutr Res Rev (2023):1-9. Epub 20230920. [CrossRef]
- Ross MM, Hernandez-Espinosa DR, Aizenman E. Neurodevelopmental Consequences of Dietary Zinc Deficiency: A Status Report. Biol Trace Elem Res (2023) 201(12):5616-39. Epub 20230325. [CrossRef]
- Siddiqi UR, Begum S, Shahjadi S, Afroz S, Mahruba SN, Parvin J, et al. Plasma Zinc, Copper and Serum Ceruloplasmin Levels of Autism Spectrum Disorder Children in Bangladesh. Heliyon (2023) 9(8):e18624. Epub 20230809. [CrossRef]
- Kambe T, Fukue K, Ishida R, Miyazaki S. Overview of Inherited Zinc Deficiency in Infants and Children. J Nutr Sci Vitaminol (Tokyo) (2015) 61 Suppl:S44-6. [CrossRef]
- Hartman JS, Silver AH. Nutritional Rickets Due to Severe Food Selectivity in Autism Spectrum Disorder. Journal of Developmental & Behavioral Pediatrics (2021) 42(1):66-72. [CrossRef]
- Jacob M, Censani M, Faridi MMA. 13-Year-Old Boy Presenting with Bilateral Femur Fractures in the Setting of Severe Vitamin D Deficiency. Case Reports in Pediatrics (2021) 2021:1-4. [CrossRef]
- Pia Riccio M, Catone G, Siracusano R, Occhiati L, Bernardo P, Sarnataro E, et al. Vitamin D Deficiency Is Not Related to Eating Habits in Children with Autistic Spectrum Disorder. AIMS Public Health (2020) 7(4):792-803. [CrossRef]
- Şengenç E, Kıykım E, Saltik S. Vitamin D Levels in Children and Adolescents with Autism. Journal of International Medical Research (2020) 48(7). [CrossRef]
- Wang T, Shan L, Du L, Feng J, Xu Z, Staal WG, et al. Serum Concentration of 25-Hydroxyvitamin D in Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. European Child & Adolescent Psychiatry (2015) 25(4):341-50. [CrossRef]
- Çıtar Dazıroğlu ME, Sağdıçoğlu Celep AG. Determination of Nutrient Intake and Dietary Antioxidant Capacity in Autism Spectrum Disorder: A Case–Control Study. Journal of Autism and Developmental Disorders (2023) 54(6):2322-32. [CrossRef]
- Shom S, Saha S, Chatterjee M, Sinha S, Mukhopadhyay K. Indian Asd Probands with 25(Oh)D and Vitamin D Binding Protein Deficiency Exhibited Higher Severity. Scientific Reports (2024) 14(1). [CrossRef]
- Bener A, Khattab A, Al-Dabbagh M. Is High Prevalence of Vitamin D Deficiency Evidence for Autism Disorder?: In a Highly Endogamous Population. Journal of Pediatric Neurosciences (2014) 9(3). [CrossRef]
- van der Lubbe A, Swaab H, Vermeiren R, van den Akker E, Ester W. Novel Insights into Obesity in Preschool Children with Autism Spectrum Disorder. Child Psychiatry & Human Development (2024). [CrossRef]
- Fiamenghi VI, Mello EDd. Vitamin D Deficiency in Children and Adolescents with Obesity: A Meta-Analysis. Jornal de Pediatria (2021) 97(3):273-9. [CrossRef]
- Feng J, Shan L, Du L, Wang B, Li H, Wang W, et al. Clinical Improvement Following Vitamin D3 Supplementation in Autism Spectrum Disorder. Nutritional Neuroscience (2016) 20(5):284-90. [CrossRef]
- Altun H, Kurutaş EB, Şahin N, Güngör O, Fındıklı E. The Levels of Vitamin D, Vitamin D Receptor, Homocysteine and Complex B Vitamin in Children with Autism Spectrum Disorders. Clinical Psychopharmacology and Neuroscience (2018) 16(4):383-90. [CrossRef]
- Qi X, Yang T, Chen J, Dai Y, Chen L, Wu L, et al. Vitamin D Status Is Primarily Associated with Core Symptoms in Children with Autism Spectrum Disorder: A Multicenter Study in China. Psychiatry Research (2022) 317. [CrossRef]
- Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial Activation and Neuroinflammation in the Brain of Patients with Autism. Annals of Neurology (2004) 57(1):67-81. [CrossRef]
- Noriega DB, Savelkoul HFJ. Immune Dysregulation in Autism Spectrum Disorder. European Journal of Pediatrics (2013) 173(1):33-43. [CrossRef]
- Esnafoglu E, Subaşı B. Association of Low 25-Oh-Vitamin D Levels and Peripheral Inflammatory Markers in Patients with Autism Spectrum Disorder. Psychiatry Research (2022) 316. [CrossRef]
- Sweetman DU, O'Donnell SM, Lalor A, Grant T, Greaney H. Zinc and Vitamin a Deficiency in a Cohort of Children with Autism Spectrum Disorder. Child: Care, Health and Development (2019) 45(3):380-6. [CrossRef]
- Yang T, Chen L, Dai Y, Jia F, Hao Y, Li L, et al. Vitamin a Status Is More Commonly Associated with Symptoms and Neurodevelopment in Boys with Autism Spectrum Disorders—a Multicenter Study in China. Frontiers in Nutrition (2022) 9. [CrossRef]
- Chiu M, Watson S. Xerophthalmia and Vitamin a Deficiency in an Autistic Child with a Restricted Diet. BMJ Case Rep (2015) 2015. Epub 20151005. [CrossRef]
- Moreno N, Lynch FC, Zalazar MA, Miranda CF, Vidal SH, Armeno ML. [Decreased Vision Due to Hypovitaminosis a in Children with Food Selectivity]. Medicina (B Aires) (2024) 84(5):860-7.
- Godfrey D, Stone RT, Lee M, Chitnis T, Santoro JD. Triad of Hypovitaminosis a, Hyperostosis, and Optic Neuropathy in Males with Autism Spectrum Disorders. Nutritional Neuroscience (2021) 25(8):1697-703. [CrossRef]
- Togari A, Kondo M, Arai M, Matsumoto S. Effects of Retinoic Acid on Bone Formation and Resorption in Cultured Mouse Calvaria. General Pharmacology: The Vascular System (1991) 22(2):287-92. [CrossRef]
- Sharp WG, Berry RC, Burrell L, Scahill L, McElhanon BO. Scurvy as a Sequela of Avoidant-Restrictive Food Intake Disorder in Autism: A Systematic Review. Journal of Developmental & Behavioral Pediatrics (2020) 41(5):397-405. [CrossRef]
- Kinlin LM, Weinstein M. Scurvy: Old Disease, New Lessons. Paediatrics and International Child Health (2023) 43(4):83-94. [CrossRef]
- Al-Farsi YM, Waly MI, Deth RC, Al-Sharbati MM, Al-Shafaee M, Al-Farsi O, et al. Low Folate and Vitamin B12 Nourishment Is Common in Omani Children with Newly Diagnosed Autism. Nutrition (2013) 29(3):537-41. Epub 20130101. [CrossRef]
- Tsujiguchi H, Miyagi S, Nguyen TTT, Hara A, Ono Y, Kambayashi Y, et al. Relationship between Autistic Traits and Nutrient Intake among Japanese Children and Adolescents. Nutrients (2020) 12(8). [CrossRef]
- Yektaş Ç, Alpay M, Tufan AE. <P>Comparison of Serum B12, Folate and Homocysteine Concentrations in Children with Autism Spectrum Disorder or Attention Deficit Hyperactivity Disorder and Healthy Controls</P>. Neuropsychiatric Disease and Treatment (2019) Volume 15:2213-9. [CrossRef]
- Erden S, Akbaş İleri B, Sadıç Çelikkol Ç, Nalbant K, Kılınç İ, Yazar A. Serum B12, Homocysteine, and Anti-Parietal Cell Antibody Levels in Children with Autism. International Journal of Psychiatry in Clinical Practice (2021) 26(1):8-13. [CrossRef]
- Zou M, Zhang Y, Li D, Li S, Hu J, Gao Y, et al. Correlation of Co-Morbidities with Symptom Severity of Children with Autism Spectrum Disorder: A Cross-Sectional Survey. Nutrients (2024) 16(17). [CrossRef]
- Baird JS, Ravindranath TM. Vitamin B Deficiencies in a Critically Ill Autistic Child with a Restricted Diet. Nutrition in Clinical Practice (2014) 30(1):100-3. [CrossRef]
- Ângelo KHdA, Silva Filho PFd, Araújo NDd, Guedes TAL, Almeida LHAd. Suplementação Nutricional Como Abordagem Terapêutica No Transtorno Do Espectro Autista: Uma Revisão De Literatura. Research, Society and Development (2021) 10(9). [CrossRef]
- Monteiro MA, Santos AAAd, Gomes LMM, Rito RVVF. Autism Spectrum Disorder: A Systematic Review About Nutritional Interventions. Revista Paulista de Pediatria (2020) 38. [CrossRef]
- Jayashree R, Gayathri G, Udayakumar N. Nutritional Supplements in Autism Spectrum Disorder: A Scoping Review. International Journal of Nutrition, Pharmacology, Neurological Diseases (2024) 14(2):153-6. [CrossRef]
- Leonario Rodríguez M, Díaz Vargas D. Effectiveness of Nutritional Interventions on Behavioral Symptomatology of Autism Spectrum Disorder: A Systematic Review. Nutrición Hospitalaria (2022). [CrossRef]
- Meguid NA, Bjørklund G, Gebril OH, Doşa MD, Anwar M, Elsaeid A, et al. The Role of Zinc Supplementation on the Metallothionein System in Children with Autism Spectrum Disorder. Acta Neurologica Belgica (2019) 119(4):577-83. [CrossRef]
- Maximino P, Fisberg M. A Alimentação Da Criança Com Transtorno Do Espectro Autista. São Paulo: Centro de Excelência em Nutrição e Dificuldades Alimentares (CENDA) do Instituto PENSI (2024). Available from: https://autismoerealidade.org.br/convivendo-com-o-tea/cartilhas/cartilha-a-alimentacao-da-crianca-com-tea/.
- Kahathuduwa CN, Dhanasekara CS, Wakefield S, Moustaid-Moussa N, Mastergeorge A. Autism Spectrum Disorder Is Associated with an Increased Risk of Development of Underweight in Children and Adolescents: A Systematic Review and Meta-Analysis. Research in Autism Spectrum Disorders (2022) 94:101969. [CrossRef]
- Malhi P, Saini S, Bharti B, Attri S, Sankhyan N. Sensory Processing Dysfunction and Mealtime Behavior Problems in Children with Autism. Indian Pediatr (2021) 58(9):842-5. Epub 20210520.
- Ward JH, Weir E, Allison C, Baron-Cohen S. Increased Rates of Chronic Physical Health Conditions across All Organ Systems in Autistic Adolescents and Adults. Molecular Autism (2023) 14(1):35. [CrossRef]
- Nuyttens L, De Vlieger L, Diels M, Schrijvers R, Bullens DMA. The Clinical and Immunological Basis of Early Food Introduction in Food Allergy Prevention. Frontiers in Allergy (2023) 4. [CrossRef]
- Bölte S, Özkara N, Poustka F. Autism Spectrum Disorders and Low Body Weight: Is There Really a Systematic Association? International Journal of Eating Disorders (2002) 31(3):349-51. [CrossRef]
- Talmi Z, Mankuta D, Raz R. Birth Weight and Autism Spectrum Disorder: A Population-Based Nested Case–Control Study. Autism Research (2020) 13(4):655-65. [CrossRef]
- Wei L, Zhong S, Nie S, Gong G. Aberrant Development of the Asymmetry between Hemispheric Brain White Matter Networks in Autism Spectrum Disorder. Eur Neuropsychopharmacol (2018) 28(1):48-62. Epub 20171207. [CrossRef]
- Adams JB, Audhya T, Geis E, Gehn E, Fimbres V, Pollard EL, et al. Comprehensive Nutritional and Dietary Intervention for Autism Spectrum Disorder-a Randomized, Controlled 12-Month Trial. Nutrients (2018) 10(3). Epub 20180317. [CrossRef]
- Lordan R, Storni C, De Benedictis CA. Autism Spectrum Disorders: Diagnosis and Treatment. In: Grabrucker AM, editor. Autism Spectrum Disorders. Brisbane (AU): Exon Publications. Copyright: The Authors. (2021).
- Siafis S, Çıray O, Wu H, Schneider-Thoma J, Bighelli I, Krause M, et al. Pharmacological and Dietary-Supplement Treatments for Autism Spectrum Disorder: A Systematic Review and Network Meta-Analysis. Mol Autism (2022) 13(1):10. Epub 20220304. [CrossRef]
- SBP. Obesidade Na Infância E Adolescência – Manual De Orientação. 3 ed. Weffort VRS, editor. São Paulo: Departamento de Nutrologia da Sociedade Brasileira de Pediatria (2019).
- Micai M, Fatta LM, Gila L, Caruso A, Salvitti T, Fulceri F, et al. Prevalence of Co-Occurring Conditions in Children and Adults with Autism Spectrum Disorder: A Systematic Review and Meta-Analysis. Neurosci Biobehav Rev (2023) 155:105436. Epub 20231031. [CrossRef]
- Nogueira-de-Almeida CA, Weffort VRS, Ued FdV, Ferraz IS, Contini AA, Martinez EZ, et al. What Causes Obesity in Children and Adolescents? Jornal de Pediatria (2024) 100:S48-S56. [CrossRef]
- Kahathuduwa CN, West BD, Blume J, Dharavath N, Moustaid-Moussa N, Mastergeorge A. The Risk of Overweight and Obesity in Children with Autism Spectrum Disorders: A Systematic Review and Meta-Analysis. Obes Rev (2019) 20(12):1667-79. Epub 20191008. [CrossRef]
- Dhaliwal KK, Orsso CE, Richard C, Haqq AM, Zwaigenbaum L. Risk Factors for Unhealthy Weight Gain and Obesity among Children with Autism Spectrum Disorder. Int J Mol Sci (2019) 20(13). Epub 20190704. [CrossRef]
- Ortega-García JA, Kloosterman N, Alvarez L, Tobarra-Sánchez E, Cárceles-Álvarez A, Pastor-Valero R, et al. Full Breastfeeding and Obesity in Children: A Prospective Study from Birth to 6 Years. Childhood Obesity (2018) 14(5):327-37. [CrossRef]
- Tseng PT, Chen YW, Stubbs B, Carvalho AF, Whiteley P, Tang CH, et al. Maternal Breastfeeding and Autism Spectrum Disorder in Children: A Systematic Review and Meta-Analysis. Nutr Neurosci (2019) 22(5):354-62. Epub 20171018. [CrossRef]
- Evans EW, Must A, Anderson SE, Curtin C, Scampini R, Maslin M, et al. Dietary Patterns and Body Mass Index in Children with Autism and Typically Developing Children. Res Autism Spectr Disord (2012) 6(1):399-405. [CrossRef]
- Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, et al. Food Selectivity in Children with Autism Spectrum Disorders and Typically Developing Children. J Pediatr (2010) 157(2):259-64. Epub 20100401. [CrossRef]
- Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK. Cardiometabolic Risk of Second-Generation Antipsychotic Medications during First-Time Use in Children and Adolescents. JAMA (2009) 302(16):1765-73. [CrossRef]
- Lai M-C, Lombardo MV, Baron-Cohen S. Autism. The Lancet (2014) 383(9920):896-910. [CrossRef]
- Jones RA, Downing K, Rinehart NJ, Barnett LM, May T, McGillivray JA, et al. Physical Activity, Sedentary Behavior and Their Correlates in Children with Autism Spectrum Disorder: A Systematic Review. PLoS One (2017) 12(2):e0172482. Epub 20170228. [CrossRef]
- Bishop SL, Havdahl KA, Huerta M, Lord C. Subdimensions of Social-Communication Impairment in Autism Spectrum Disorder. J Child Psychol Psychiatry (2016) 57(8):909-16. Epub 20160108. [CrossRef]
- McPhillips M, Finlay J, Bejerot S, Hanley M. Motor Deficits in Children with Autism Spectrum Disorder: A Cross-Syndrome Study. Autism Research (2014) 7(6):664-76. [CrossRef]
- Healy S, Haegele JA, Grenier M, Garcia JM. Physical Activity, Screen-Time Behavior, and Obesity among 13-Year Olds in Ireland with and without Autism Spectrum Disorder. J Autism Dev Disord (2017) 47(1):49-57. [CrossRef]
- Mazurek MO, Wenstrup C. Television, Video Game and Social Media Use among Children with Asd and Typically Developing Siblings. J Autism Dev Disord (2013) 43(6):1258-71. [CrossRef]
- Maxwell-Horn A, Malow BA. Sleep in Autism. Semin Neurol (2017) 37(4):413-8. Epub 20170824. [CrossRef]
- Zuckerman KE, Hill AP, Guion K, Voltolina L, Fombonne E. Overweight and Obesity: Prevalence and Correlates in a Large Clinical Sample of Children with Autism Spectrum Disorder. J Autism Dev Disord (2014) 44(7):1708-19. [CrossRef]
- Bachmann-Gagescu R, Mefford HC, Cowan C, Glew GM, Hing AV, Wallace S, et al. Recurrent 200-Kb Deletions of 16p11.2 That Include the Sh2b1 Gene Are Associated with Developmental Delay and Obesity. Genet Med (2010) 12(10):641-7. [CrossRef]
- Walters RG, Jacquemont S, Valsesia A, de Smith AJ, Martinet D, Andersson J, et al. A New Highly Penetrant Form of Obesity Due to Deletions on Chromosome 16p11.2. Nature (2010) 463(7281):671-5. [CrossRef]
- Bennett EA, Kolko RP, Chia L, Elliott JP, Kalarchian MA. Treatment of Obesity among Youth with Intellectual and Developmental Disabilities: An Emerging Role for Telenursing. West J Nurs Res (2017) 39(8):1008-27. Epub 20170328. [CrossRef]
- Leekam SR, Nieto C, Libby SJ, Wing L, Gould J. Describing the Sensory Abnormalities of Children and Adults with Autism. Journal of Autism and Developmental Disorders (2006) 37(5):894-910. [CrossRef]
- Hinckson EA, Dickinson A, Water T, Sands M, Penman L. Physical Activity, Dietary Habits and Overall Health in Overweight and Obese Children and Youth with Intellectual Disability or Autism. Res Dev Disabil (2013) 34(4):1170-8. Epub 20130209. [CrossRef]
- Helsel BC, Foster RNS, Sherman J, Steele R, Ptomey LT, Montgomery R, et al. The Family Nutrition and Physical Activity Survey: Comparisons with Obesity and Physical Activity in Adolescents with Autism Spectrum Disorder. J Autism Dev Disord (2023) 53(1):89-95. Epub 20220104. [CrossRef]
- Draudviliene L, Draudvila J, Stankeviciute S, Daniuseviciute-Brazaite L. Two Physiotherapy Methods to Improve the Physical Condition of Children with Autism Spectrum Disorder. Children (Basel) (2024) 11(7). Epub 20240628. [CrossRef]
- Mano-Sousa BJ, Pedrosa AM, Alves BC, Galduróz JCF, Belo VS, Chaves VE, et al. Effects of Risperidone in Autistic Children and Young Adults: A Systematic Review and Meta-Analysis. Current Neuropharmacology (2021) 19(4):538-52. [CrossRef]
- Järvinen A, Laine MK, Tikkanen R, Castrén ML. Beneficial Effects of Glp-1 Agonist in a Male with Compulsive Food-Related Behavior Associated with Autism. Frontiers in Psychiatry (2019) 10. [CrossRef]
- Hung LY, Margolis KG. Autism Spectrum Disorders and the Gastrointestinal Tract: Insights into Mechanisms and Clinical Relevance. Nature Reviews Gastroenterology & Hepatology (2023) 21(3):142-63. [CrossRef]
- Madra M, Ringel R, Margolis KG. Gastrointestinal Issues and Autism Spectrum Disorder. Psychiatric Clinics of North America (2021) 44(1):69-81. [CrossRef]
- Holingue C, Pfeiffer D, Ludwig NN, Reetzke R, Hong JS, Kalb LG, et al. Prevalence of Gastrointestinal Symptoms among Autistic Individuals, with and without Co-Occurring Intellectual Disability. Autism Research (2023) 16(8):1609-18. [CrossRef]
- Holingue C, Poku O, Pfeiffer D, Murray S, Fallin MD. Gastrointestinal Concerns in Children with Autism Spectrum Disorder: A Qualitative Study of Family Experiences. Autism (2021) 26(7):1698-711. [CrossRef]
- McElhanon BO, McCracken C, Karpen S, Sharp WG. Gastrointestinal Symptoms in Autism Spectrum Disorder: A Meta-Analysis. Pediatrics (2014) 133(5):872-83. [CrossRef]
- Al-Beltagi M. Nutritional Management and Autism Spectrum Disorder: A Systematic Review. World Journal of Clinical Pediatrics (2024) 13(4). [CrossRef]
- Wang X, Tang R, Wei Z, Zhan Y, Lu J, Li Z. The Enteric Nervous System Deficits in Autism Spectrum Disorder. Frontiers in Neuroscience (2023) 17. [CrossRef]
- Xu G, Snetselaar LG, Jing J, Liu B, Strathearn L, Bao W. Association of Food Allergy and Other Allergic Conditions with Autism Spectrum Disorder in Children. JAMA Network Open (2018) 1(2). [CrossRef]
- Yu Y, Zhao F. Microbiota-Gut-Brain Axis in Autism Spectrum Disorder. Journal of Genetics and Genomics (2021) 48(9):755-62. [CrossRef]
- Ferguson BJ, Dovgan K, Takahashi N, Beversdorf DQ. The Relationship among Gastrointestinal Symptoms, Problem Behaviors, and Internalizing Symptoms in Children and Adolescents with Autism Spectrum Disorder. Frontiers in Psychiatry (2019) 10. [CrossRef]
- Nogay NH, Nahikian-Nelms M. Effects of Nutritional Interventions in Children and Adolescents with Autism Spectrum Disorder: An Overview Based on a Literature Review. International Journal of Developmental Disabilities (2022) 69(6):811-24. [CrossRef]
- Buie T, Campbell DB, Fuchs GJ, Furuta GT, Levy J, VandeWater J, et al. Evaluation, Diagnosis, and Treatment of Gastrointestinal Disorders in Individuals with Asds: A Consensus Report. Pediatrics (2010) 125(Supplement_1):S1-S18. [CrossRef]
- Whitney DG, Shapiro DN. National Prevalence of Pain among Children and Adolescents with Autism Spectrum Disorders. JAMA Pediatrics (2019) 173(12). [CrossRef]
- Yu R, Hafeez R, Ibrahim M, Alonazi WB, Li B. The Complex Interplay between Autism Spectrum Disorder and Gut Microbiota in Children: A Comprehensive Review. Behavioural Brain Research (2024) 473:115177. [CrossRef]
- Lagod PP, Naser SA. The Role of Short-Chain Fatty Acids and Altered Microbiota Composition in Autism Spectrum Disorder: A Comprehensive Literature Review. Int J Mol Sci (2023) 24(24). Epub 20231213. [CrossRef]
- Lewandowska-Pietruszka Z, Figlerowicz M, Mazur-Melewska K. Microbiota in Autism Spectrum Disorder: A Systematic Review. Int J Mol Sci (2023) 24(23):16660. Epub 20231123. [CrossRef]
- Niehus R, Lord C. Early Medical History of Children with Autism Spectrum Disorders. J Dev Behav Pediatr (2006) 27(2 Suppl):S120-7. [CrossRef]
- Wang H, Liu S, Xie L, Wang J. Gut Microbiota Signature in Children with Autism Spectrum Disorder Who Suffered from Chronic Gastrointestinal Symptoms. BMC Pediatr (2023) 23(1):476. Epub 20230920. [CrossRef]
- Mhanna A, Martini N, Hmaydoosh G, Hamwi G, Jarjanazi M, Zaifah G, et al. The Correlation between Gut Microbiota and Both Neurotransmitters and Mental Disorders: A Narrative Review. Medicine (Baltimore) (2024) 103(5):e37114. [CrossRef]
| Micronutrient | Therapeutic scheme |
|---|---|
| Iron | Oral dose of 2 mg/kg/day of elemental iron, for a period sufficient to recovery of ferritin and hemoglobin |
| Magnesium | Oral dose of 6 mg/kg/day when serum values are below 1.7 mg/dL or when the dietary survey shows evident deficiency in consumption |
| Zinc | Oral dose of 2 mg/kg/day of elemental zinc, respecting the maximum dose of 20 g/day, until serum zinc concentration reaches 70 mg/dL |
| Calcium | Oral dose of 100 mg per day of elemental calcium while the nutritional risk situation persists |
| Vitamin D | Oral dose for 90 days: - Under 1 year of age: 2,000 IU/day - Between 1 and 12 years of age: 3,000 and 6,000 IU/day - Over 12 years of age: 6,000 IU/day |
| Vitamin A | Oral dose of retinol palmitate: - Under 6 months of age: 50,000 IU/day - Between 6 months and 1 year: 100,000 IU/day - Over 1 year (male): 200,000 IU/day - Between 1 and 12 years (female): 200,000 IU/day - Over 12 years (female): 10,000 IU/day or 25,000 IU/week for three months in cases of night blindness and/or Bitot's spots - Note 1: Treatment should only be administered to individuals with clinical manifestations of VAD (xerophthalmia) or severe malnutrition (regardless of the presence of vitamin deficiency) - Note 2: Treatment will be in a single dose for cases of severe malnutrition and in three doses (D1, D2 and D14) in cases of xerophthalmia and/or active lesions (ulcers) in the cornea - Note 3: In cases of pregnant adolescents or those suspected of being pregnant, the initiation of treatment for active corneal lesions (considered an emergency due to the risk of vision loss within 24 to 48 hours) should be carefully weighed against the risk of maternal blindness and the potential undesirable effects of vitamin A on the fetus. Administration of vitamin A to women of childbearing age should be done with extreme caution due to the risk of teratogenicity to the fetus |
| Vitamin C | Oral dose of 100-300 mg/day of vitamin C for infants and children for one month or until full recovery occur |
| Vitamin B12 | - Initial dose: 0.2 μg/kg, subcutaneously for two days (attention to the possible hypokalemia during this phase in children with severe anemia) - After the initial dose: 1,000 μg/day, subcutaneously for 2 to 7 days; subsequently, a dose of 100 μg/week, subcutaneously, for one month |
| Folate | Oral dose of 1 to 5 mg/day of folic acid for up to four months; in infants, doses of 50 µg/day may be sufficient |
| Vitamin B6 | Except for cases of children with pyridoxine-dependent syndromes who present with seizures, the doses for vitamin B6 supplementation in the pediatric population in cases of nutritional deficiency are not well defined |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





