1. Background
Peripherally inserted central catheters (PICCs) are essential tools in modern healthcare, primarily used for administering chemotherapy or antibiotics. Known for their lower infection rates and longer indwelling times, PICCs are crucial in reducing healthcare-associated infections [
1,
2]. Different types of PICCs appeared to reduce catheter-related complications, and the costs were increasing relatively. The payers need to understand the cost-effectiveness of different PICCs, which is important for making the best healthcare decisions. According to industry data, over 2.7 million PICCs were used in the US in 2020; in China, almost 1 million PICCs were used in 2020, and the rate has kept increasing by over 20%.
Along with its wide usage, the common concerns of PICC are central line-associated bloodstream infection (CLABSI) and venous thromboembolism (VTE) [
3]. One study researched the relationship between the indwelling time of PICC and the CLABSI rate, and the results showed that the median indwelling time was 26 days (range 0 – 385), and the central line-associated bloodstream infection (CLABSI) incidence was 4.0 per 1000 catheter days [
4].
This study focuses on two types of PICCs—one standard (Standard PICC) and one with a Chlorhexidine coating (AGBA PICC)—to compare their efficacy in managing catheter-related complications. Conducted within the hematology department of a Class 3A hospital in China, this health economic model draws on data from a randomized controlled trial. Several studies of this hospital reported the average 4-year overall survival rates were all upper 75% [
5,
6,
7]. This means the patients need several PICC catheters during their treatment period, and some severe catheter-related events can impact survival, like central line-associated bloodstream infection (CLABSI). Common adverse events related to catheters include catheter occlusion, exit-site infection, venous thromboembolism (VTE), and central line-associated bloodstream infection (CLABSI) [
8]. While some adverse events, such as occlusion and suspected infections, may resolve with appropriate intervention, CLABSI is a significant concern as it requires laboratory-confirmed testing for diagnosis. However, in real-world settings, empiric therapies are often initiated, which involve removing the catheter and administering antibiotics [
9].
The standard catheter care protocol involves obtaining blood cultures to test for CLABSI and performing routine catheter maintenance. If catheter function cannot be restored, the catheter must be removed, and a new one is typically inserted after a few days. This process can contribute to increased costs and patient discomfort, highlighting the importance of reducing catheter-related complications [
10,
11].
As a result, more accurate and cost-effective methods are needed for evaluating PICC insertion and maintenance in long-term treatments, whether in hospital or home-based settings. Although PICCs are not the decisive factor in treatment outcomes, they are critical components that support the overall treatment process. However, there is a gap in economic evaluations related to these essential devices, leaving a lack of knowledge regarding their integration into the care pathway.
The primary aim of this research is to evaluate a health-economic model that compares a new, potentially superior PICC design with a standard option over a 90-day follow-up period. This analysis aims to fill existing knowledge gaps in economic evaluations and guide the integration of more effective PICC types into clinical practice, ultimately enhancing patient care and resource utilization.
2. Methods
2.1. Study Compliance and Design
This study adheres to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) to ensure thoroughness and accuracy in reporting [
12]. The observed objectives are the standard PICC and AGBA PICC.
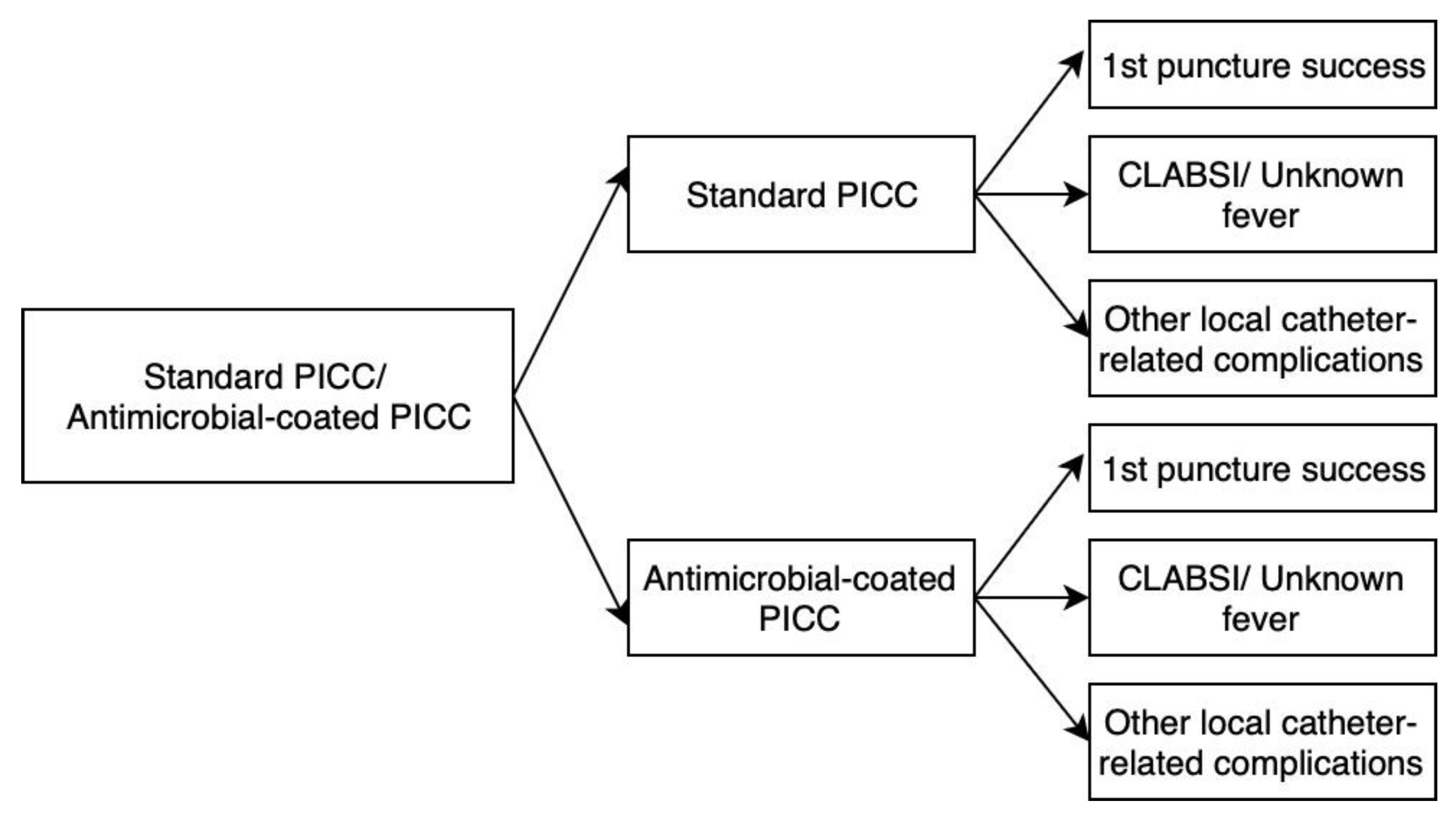
The methods section is structured as follows: first, a description of the model used, followed by a presentation of the model based on real-world evidence. Finally, a description of how the model was tested through sensitivity analysis. The population target comprises patients who are suspected of needing to take PICC catheters, and the considered time horizon is 5 years, which refers to the common survival time of oncology patients (
Figure 1).
2.2. Target Population and Economic Perspective
Cost analyses are conducted from the perspective of a social reimbursement payer, reflecting the structure of China's healthcare funding, where the government shoulders the majority of direct medical costs. This analysis is particularly pertinent given the rapid demographic shifts and escalating healthcare demands due to an aging population. The study specifically targets oncology patients likely to require long-term PICC placement.
Analyses of costs are conducted from a social reimbursement payer’s perspective, in line with an attempt to reduce the healthcare resources allocated to this treatment. In the health system, like China's reimbursement system, the government is the biggest payer for the direct costs, and the development of the aging population is rapid; thereby, the healthcare burden is enormous.
2.3. Conceptual Model: Decision Tree of Two PICCs Selection at > 30 Days Maintenance
Modeling is a tool for supporting decision-making that anticipates and predicts the impact of specific healthcare interventions on a group of patients or society [
13,
14,
15]. A decision tree is one type of decision-analysis model used for economic evaluation in this study. It will be used to depict potential complications when the patient needs to accept a PICC catheter insertion procedure. The decision tree is mainly valued for its simplicity and transparency in describing the options of interest, the costs, and health outcomes indicated on the specific path or branch.
In the case of two types of related complications, a hypothetical assumption is that all complications could be detected by the lab tests. In the model, there are two alternative outcomes after prescribing inserting a PICC catheter: two branches indicating first-time attempt insertion success or failure. When the patient accepted PICC insertion, the PICC catheter would indwell in the patient's body for almost 15 days to 3 months, and the catheter-related complication would show on the models as the branches. The possibilities of branches are fever, local complication, and complication-free.
The catheter-related complications have been discussed sufficiently since the end of the 1990s, along with the booming treatments. There are three alternative outcomes: the recovery from the complication without the catheter removal, the recovery from the complication with the catheter removal, and the situation turning worse [
16,
17,
18,
19]. If the catheter is removed, the new catheter needs to be inserted again; the symptom-related treatments have to be considered. The model examined in this study thus includes some additional sections, which these patients need to multiple lab tests to confirm diagnosis during follow-up period.
2.4. Data Collection: Probabilities, Costs and QALYs
Populating the model includes the probabilities of PICC patients’ maintenance period of more than 30 days at each node in the tree and branch. In this model, most of the data were collected based on the China two types of PICC randomized clinical trial; the QALYs were collected based on the published literature, which was not observed through the China two types of PICC randomized clinical trial directly [
20,
21]. The cost-per-procedure data for the PICC insertion and maintenance were obtained from the official list of Beijing Municipal Medical Insurance Bureau from 2020 to 2023. All the costs in the trial were reported in RMB, and in this study, it is recalculated in US dollars (¥678.03 =
$100) [
22,
23]. The costs were categorized into different items: lab tests, in-hospital care expenses, follow-up, catheter and catheter maintenance expenses, catheter-related complications treatments, and other treatments. The end of each branch accounts for several cost categories, corresponding to all the steps conducted in the specific pathways. The lab tests include the blood test, the ultrasound test, and X-ray scan. The in-hospital care and follow-up expenses are based on clinical routines. According to the protocol, the catheter-related complications all need the lab test to confirm the clinical inference, the related treatment costs were from the real study data. Other treatment costs are based on the real records which are difficult to predict on the model assumption. For the catheter-related cost component, 95% bias-corrected confidence interval were calculated using Monte Carlo of 10,000 random samples with replacement. Monte Carlo is a method to model the different outcomes’ probabilities, which is difficult to predict because of the intervention of random variables and helps optimize the process parameters.
A literature review was conducted to gather QALYs data for marrow transplant patients for pre-and post-transplant [
20,
22]. The database used for the engines are PubMed, Scopus and Cochrane. The timeframe set was 10 years, from 2014 to 2023. The search terms were: [(QALYs) OR (Health-Related Quality of Life)] AND (marrow transplant).
2.5. ICER and Threshold
An incremental cost-effectiveness ratio (ICER) are calculated to judge whether the Chlorhexidine-coated PICC is a cost-effective solution for hematology patients undergoing long-term intravenous infusion therapy. Because the PICC is a tool device, the ratios will reflect the different costs between the two models and correspond to the same QALYs. The calculated ICER will be compared with a threshold value that presents society’s willingness to pay for better health outcomes per year, i.e. one QALY. China Minister of Health has no official guidelines about the willingness to pay (WTP) referring the NICE guidelines, the related articles recommended that 1.76 times of gross domestic product (GDP) will be the considered threshold, which is for the not life-saving technology. In this study, the threshold of ≈ RMB 113,120 (USD 16,884) is used [
24,
25,
26,
27,
28].
2.6. Sensitivity Analyses
The sensitivity analyses are conducted based on the assumption that the standard and AGBA PICCs can be expected to influence the cost-effectiveness of the whole infusion treatment period [
29,
30]. A probabilistic sensitivity analyses are performed to estimate the distribution of ICER. A cost-effectiveness plane was built, and the Monte Carlo model ran 10,000 repetitions. The sensitivity analysis of Net Monetary Benefit (NMB) and willingness-to-pay (WTP) tested the assumptions relating to their respective levels in the catheter indwelling period using descriptive statistics for cost-per-patient data and varying other parameters based on theoretical grounds [
31,
32].
3. Results
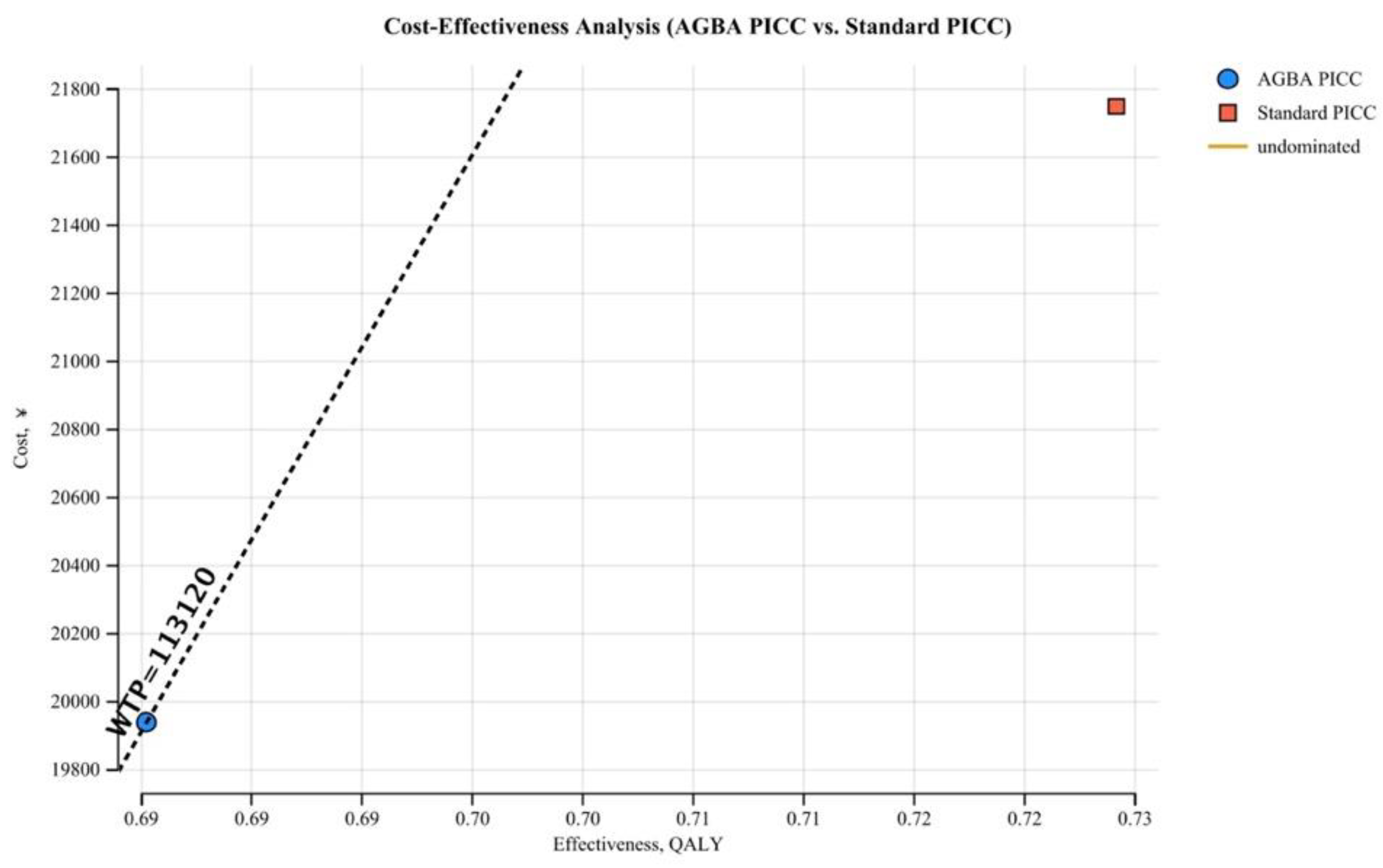
According to the study data, the mean healthcare cost per patient of the standard PICC is RMB 21,987.32 (USD 3,242.82, at an average exchange rate of ¥678.03 = $100), affecting 0.68 QALYs in 90 days, and AGBA PICC is RMB 19,696.23 (USD 2,904.92), affecting 0.73 QALYs in 90 days, thus resulting in incremental costs of RMB 2,291.10 (USD 428.44). Due to the catheter working as a channel, it does not impact QALYs, but after the model’s simulation, the standard PICC gains -0.05 QALYs. The Incremental Cost-Effectiveness Ratio (ICER) for AGBA PICCs compared to standard PICCs is consistently centered at RMB 4,271.31 (USD 629.96), with no variability across simulations.
3.1. Sensitivity Analysis
A willingness-to-pay (WTP) threshold of RMB 113,120 (USD 16,683.63) per QALY is used to assess the cost-effectiveness of the two interventions. This cost-effectiveness analysis (CEA) evaluates the economic and clinical value of AGBA PICCs compared to standard PICCs by examining cost and effectiveness, measured in quality-adjusted life years (QALY) (
Figure 2). The AGBA PICC lies below the willingness-to-pay (WTP) threshold line, indicating it is cost-effective. In contrast, the standard PICC is positioned above the WTP line, reflecting higher costs and lower cost-effectiveness. This suggests that AGBA PICCs offer a better balance of cost and health outcomes, reinforcing their economic advantage.
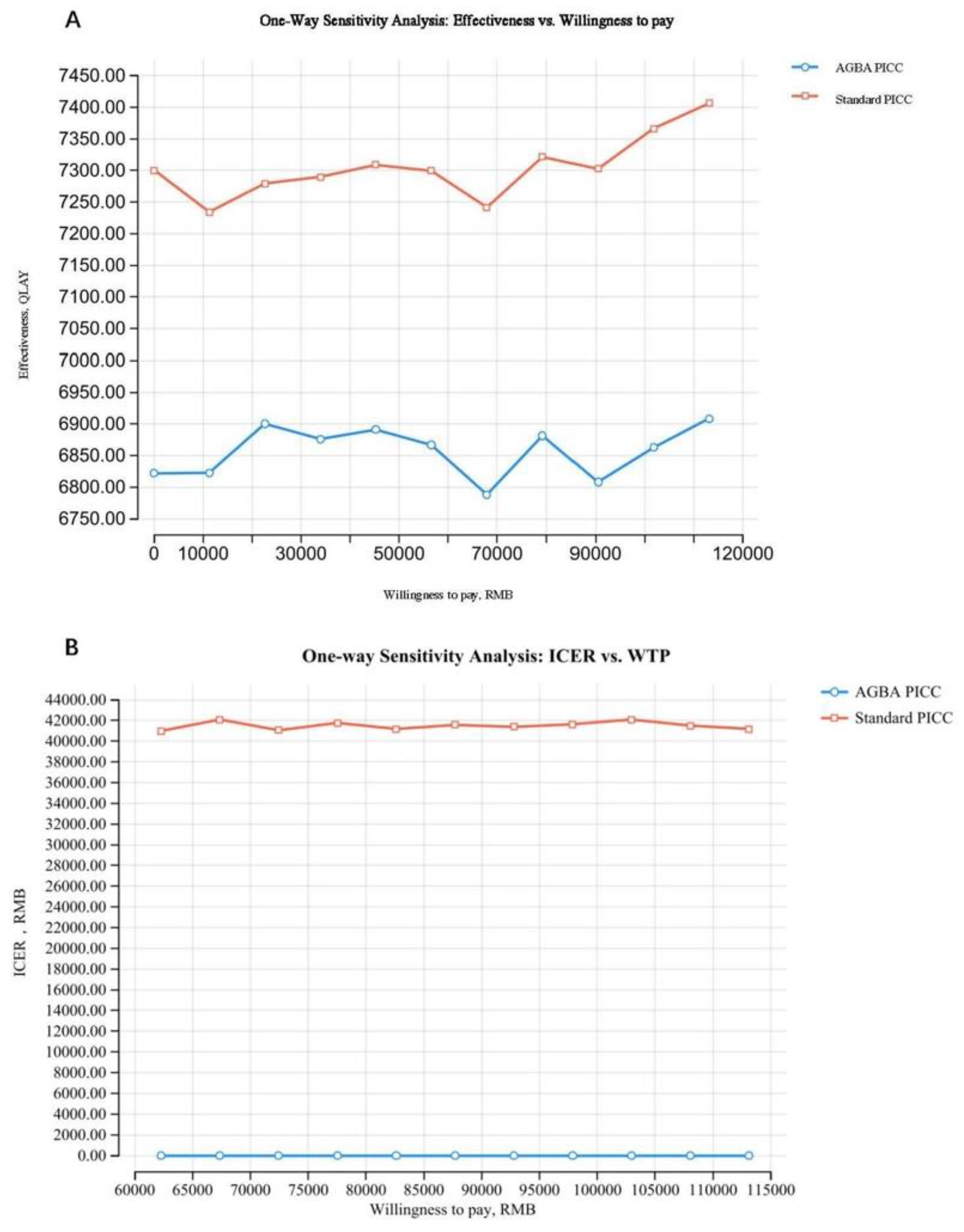
According to the one-way sensitivity analysis, the relationship between willingness to pay (WTP) and effectiveness (QALY) is observed, which is for AGBA PICCs and standard PICCs. The results indicate that standard PICCs consistently show higher QALYs than AGBA PICCs across varying WTP thresholds (
Figure 3). However, the difference in effectiveness is relatively stable, suggesting that while standard PICCs may provide slightly better health outcomes, the cost-effectiveness ratio may favor AGBA PICCs depending on cost considerations.
Another one-way sensitivity analysis of the relationship between incremental cost-effectiveness ratio (ICER) and willingness to pay (WTP) for AGBA PICCs compares to standard PICCs, plotted against varying willingness-to-pay (WTP) thresholds (
Figure 3). The ICER values fluctuate between RMB 41,000 (USD 6,046.93) and RMB 42,000 (USD 6,194.42) across different WTP levels, reflecting the variability in cost-effectiveness under different economic assumptions. The dashed vertical line at RMB 113,120 (USD 16,683.63) represents the threshold at which an intervention is considered cost-effective based on the predetermined WTP limit.
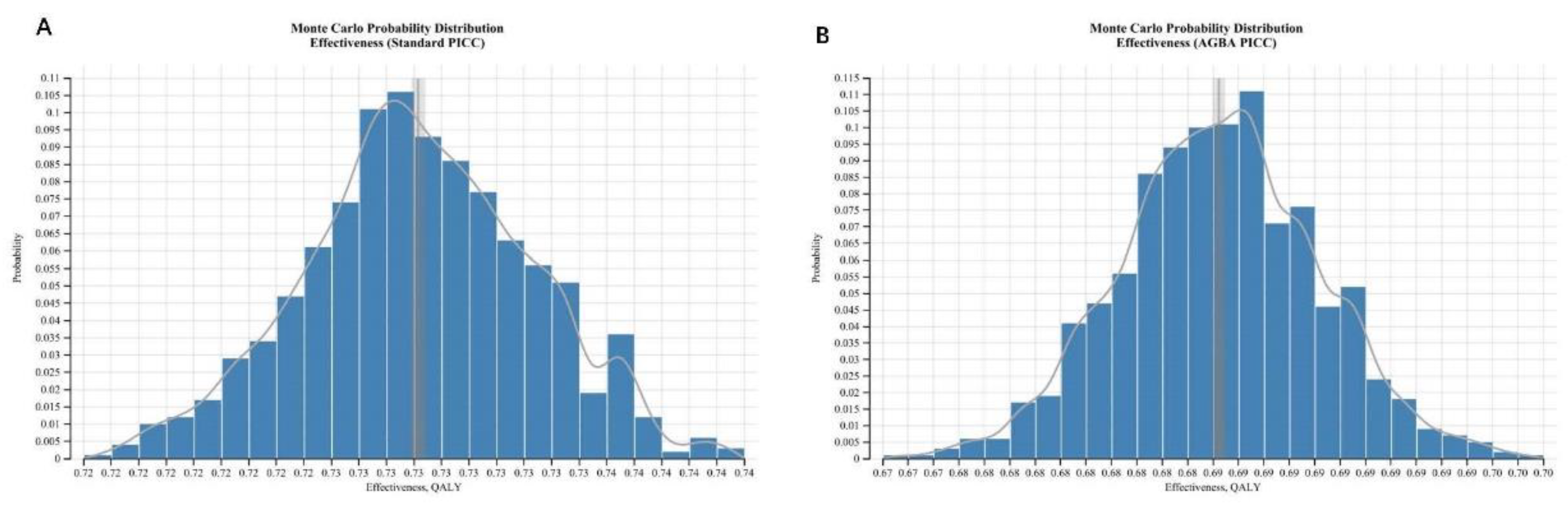
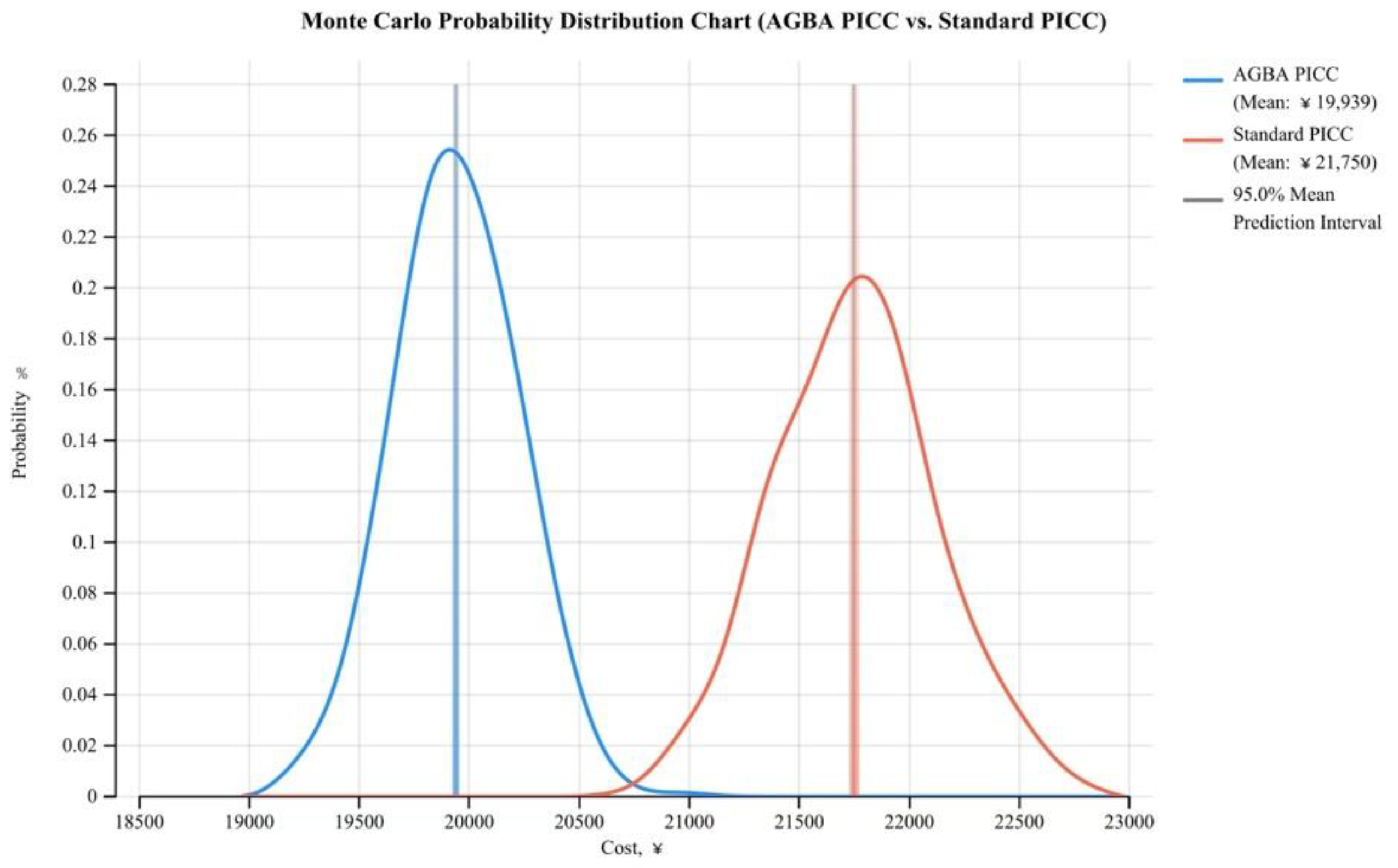
3.2. Monte Carlo Probabilistic Analysis
The Monte Carlo probability distribution simulation for AGBA PICCs and Standard PICCs is conducted to predict the distribution of QALYs. The results show that the values of AGBA PICCs clustered around 0.69 QALYs the most (
Figure 4). The standard PICCs demonstrate a higher mean QALY (~0.73) compared to AGBA PICCs. The distribution reflects the probabilistic nature of effectiveness, highlighting the variability in patient outcomes. The narrow 95% prediction interval around the AGBA PICC cost further reflects lower variability and greater cost predictability. In contrast, the standard PICC distribution exhibits a higher mean cost with slightly wider variability. The curve of AGBA PICC’s relatively narrow spread indicates consistent effectiveness and cost; the distribution of standard PICC is broader, indicating more variability and high risk of patient outcomes (
Figure 5).
4. Discussion
According to this health-economic model, the chlorhexidine-coated PICC is a more cost-effective tool; but the standard PICCs show slightly higher QALYs than chlorhexidine-coated PICCs, and the difference is marginal. In this case, the Incremental Cost-Effectiveness Ratio (ICER) for chlorhexidine-coated PICCs compared to standard PICCs is RMB 4,271.31 per QALY, which is far lower than the RMB 113,120 used as an informal WTP threshold in China. Since the ICER values consistently remain below this threshold, chlorhexidine-coated PICCs are deemed cost-effective across the entire range of WTP values. This result reinforces the economic viability of chlorhexidine-coated PICCs, demonstrating that even under the most conservative estimates, the intervention remains within acceptable cost-effectiveness limits.
In the sensitivity analysis, the chlorhexidine-coated PICC proved to be the cost-effective option, but there are some uncertainties in WTP and cost variations. This finding further supports the adoption of chlorhexidine-coated PICCs in clinical practice, especially in resource-constrained environments where cost containment is a priority.
While standard PICCs may yield marginally and uncertainty better health outcomes, the associated cost exceeds the WTP threshold, limiting their economic feasibility. The cost savings and lower risk associated with chlorhexidine-coated PICCs provide a compelling case for their adoption in long-term treatment plans.
The findings suggest that integrating chlorhexidine-coated PICCs into routine practice can optimize healthcare resource allocation without jeopardizing patient outcomes. This analysis serves as a valuable tool for policymakers and healthcare administrators seeking to enhance cost-efficiency while maintaining high standards of care. This model supports decision-makers in optimizing resource allocation, emphasizing the importance of balancing economic constraints with clinical effectiveness.
5. Conclusion
In conclusion, chlorhexidine-coated PICCs represent a cost-effective alternative that aligns with value-based care principles, providing a sustainable option for long-term treatment strategies.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
The study was conceptualized and executed by JX, who designed the model, collected necessary data, and conducted the analysis. RC, HZ and HCC served as clinical and economic expert panel members. HF took the lead in drafting the manuscript, and the final version received input, approval, and contributions from all team members. All authors have collectively agreed to investigate and resolve any such questions and document the resolution in the literature.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is provided within the manuscript or supplementary information files.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CLABSI |
Central line-associated bloodstream infection |
| PICC |
Peripherally inserted central catheter |
| QALY |
Quality-adjusted life years |
| ICER |
Incremental cost-effectiveness ratio |
| WTP |
Willingness to pay |
| GDP |
Gross domestic product |
| VTE |
Venous thromboembolism |
References
- Marschall J, Mermel LA, Scm DO, et al. Strategies to Prevent Central Line-Associated Bloodstream Infections in Acute Care Hospitals: 2014 Update. Hospital Epidemiology. 2014;35(7):753-771. [CrossRef]
- Böll B, Schalk E, Buchheidt D, et al. Central venous catheter–related infections in hematology and oncology: 2020 updated guidelines on diagnosis, management, and prevention by the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Hematol. 2021;100(1):239-259. [CrossRef]
- Baskin KM, Hunnicutt C, Beck ME, Cohen ED, Crowley JJ, Fitz CR. Long-term central venous access in pediatric patients at high risk: Conventional versus antibiotic-impregnated catheters. Journal of Vascular and Interventional Radiology. 2014;25(3):411-418. [CrossRef]
- Caris MG, De Jonge NA, Punt HJ, et al. Indwelling time of peripherally inserted central catheters and incidence of bloodstream infections in haematology patients: a cohort study. Published online 2020. [CrossRef]
- Chang YJ, Wang Y, Liu YR, et al. Haploidentical allograft is superior to matched sibling donor allograft in eradicating pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: A retrospective and prospective analysis. J Hematol Oncol. 2017;10(1):1-13. [CrossRef]
- Li SQ, Fan QZ, Xu LP, et al. Different Effects of Pre-transplantation Measurable Residual Disease on Outcomes According to Transplant Modality in Patients With Philadelphia Chromosome Positive ALL. Front Oncol. 2020;10. [CrossRef]
- Li SQ, Fan QZ, Xu LP, et al. Different Effects of Pre-transplantation Measurable Residual Disease on Outcomes According to Transplant Modality in Patients With Philadelphia Chromosome Positive ALL. Front Oncol. 2020;10. [CrossRef]
- 2021 Infusion Therapy Standards of Practice Updates. J Infus Nurs. 2021;44(4):190. [CrossRef]
- Buetti N, Marschall J, Drees M, et al. Strategies to prevent central line-associated bloodstream infections in acute-care hospitals: 2022 Update. [CrossRef]
- Bradford NK, Edwards RM, Chan RJ. Normal saline (0.9% sodium chloride) versus heparin intermittent flushing for the prevention of occlusion in long-term central venous catheters in infants and children. Cochrane Database of Systematic Reviews. 2020;2020(4). [CrossRef]
- Kitamura H, Kubota Y, Komukai S, et al. Venue of catheter insertion does not significantly impact the event of central line-associated bloodstream infection in patients with haematological diseases Infection Prevention in Practice. Infection Prevention in Practice. 2020;2:100050. [CrossRef]
- Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ. 2013;346. [CrossRef]
- Earl DJ, Deem MW. Monte Carlo simulations. Methods Mol Biol. 2008;443:25-36. [CrossRef]
- Briggs AH. Statistical Issues in Economic Evaluations. Encyclopedia of Health Economics. Published online January 1, 2014:352-361. [CrossRef]
- Kuntz K, Sainfort F, Butler M, et al. Overview of Decision Models Used in Research. Published online 2013. Accessed June 18, 2023. https://www.ncbi.nlm.nih.gov/books/NBK127474/.
- CDC, Ncezid, DHQP. Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-central Line Associated Bloodstream Infection).
- Novikov A, Lam MY, Mermel LA, Casey AL, Elliott TS, Nightingale P. Impact of catheter antimicrobial coating on species-specific risk of catheter colonization: a meta-analysis. Antimicrob Resist Infect Control. 2012;1:40. [CrossRef]
- Hanna H, Benjamin R, Chatzinikolaou I, et al. Long-Term Silicone Central Venous Catheters Impregnated With Minocycline and Rifampin Decrease Rates of Catheter-Related Bloodstream Infection in Cancer Patients: A Prospective Randomized Clinical Trial. 2016;22(15):3163-3171. [CrossRef]
- Yamaguchi RS, Noritomi DT, Degaspare NV, et al. Peripherally inserted central catheters are associated with lower risk of bloodstream infection than central venous catheters in pediatric intensive care patients: a propensity-adjusted analysis. Intensive Care Med. 2017;43(8):1097-1104. [CrossRef]
- Liang Y, Wang H, Niu M, Zhu X, Cai J, Wang X. Health-related quality of life before and after hematopoietic stem cell transplant: evidence from a survey in Suzhou, China. Hematology. 2018;23(9):626-632. [CrossRef]
- Xie F, Zhou T, Humphries B, Neumann PJ. Do Quality-Adjusted Life-Years Discriminate Against the Elderly? An Empirical Analysis of Published Cost-Effectiveness Analyses. Value in Health. Published online March 26, 2024. [CrossRef]
- Leech AA, Kim DD, Cohen JT, Neumann PJ. Are low and middle-income countries prioritizing high-value healthcare interventions? BMJ Glob Health. 2020;5:1850. [CrossRef]
- Containing medical expenditure: lessons from reform of Beijing public hospitals. [CrossRef]
- Butt T, Liu GG, Kim DD, Neumann PJ, Gordon D, Liu G. Taking stock of cost-effectiveness analysis of healthcare in China What do the new findings imply? BMJ Glob Health. 2019;4:1418. [CrossRef]
- Wu JT, Jit M, Zheng Y, et al. Routine Pediatric Enterovirus 71 Vaccination in China: a Cost-Effectiveness Analysis. Published online 2016. [CrossRef]
- Lan T, Guan L, Pang X, Li X, Yu Q. Impact of the National Centralized Drug Procurement Policy (4 + 7 policy) on the drug expenditures of patients treated in outpatient and emergency departments in a large tertiary level-A hospital in China: A single centre, interrupted time series. J Clin Pharm Ther. 2022;47(1):104-111. [CrossRef]
- Pan L, Xiao K, Zhu H, Luo L. The impacts of public hospital comprehensive reform policies on hospital medicine cost, revenues and healthcare expenditures 2014-2019: An analysis of 103 tertiary public hospitals in China. Frontiers in health services. 2023;3. [CrossRef]
- Ye Z, Abduhilil R, Huang J, Sun · Lihua. Willingness to Pay for One Additional Quality Adjusted Life Year: A Population Based Survey from China Key Points for Decision Makers. 2022;20:893-904. [CrossRef]
- Choong SHC, Poon M, Soh TG, et al. Use of Peripherally Inserted Central Catheter (PICC) for the Infusion of Peripheral Blood Stem Cell Products Is Safe and Effective. Blood. 2020;136(Supplement 1):41-42. [CrossRef]
- Comas M, Domingo L, Jansana A, et al. Cost-effectiveness Analysis of Peripherally Inserted Central Catheters Versus Central Venous Catheters for in-Hospital Parenteral Nutrition. J Patient Saf. 2022;18(7):E1109-E1115. [CrossRef]
- Huang Y, Yan S, Xie H, et al. Health Related Quality of Life of Rosacea Patients in China Assessed by Dermatology Life Quality Index and Willingness to Pay. Published online 2022. [CrossRef]
- Health economic evaluation: Important principles and methodology. Accessed January 8, 2023. https://onlinelibrary.wiley.com/doi/epdf/10.1002/lary.23943?saml_referrer.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).