Introduction:
Erectile dysfunction (ED), a condition that affects millions worldwide refers to the persistent problem of obtaining and sustaining a sufficient penile erection for engaging in successful sexual activity. According to
National Institute of Health (NIH) Consensus Development Conference Erectile dysfunction is the inability to achieve or maintain an erection sufficient for satisfactory sexual performance[
1]
. Some professionals propose that this condition should endure for at least six months, the incidence of ED rises alongside age and other health issues. Approximately, 40% of men aged 40-70 have ED [
2,
3], However, only 22% of people with sexual dysfunction seek medical help[
4].
A person's quality of life is negatively impacted by erectile dysfunction through damage to self-image confidence [
5]. ED in Chronic kidney disease and End-stage renal disease (ESRD) are multifactorial condition associated with diabetes, hypertension, dyslipidemia, hormonal imbalances, vascular dysfunction, neuropathy, and psychosocial factors[
5,
6,
7,
8,
9,
10].The classification of kidney diseases etiologies is based on patients' glomerular filtration rates (GFR).
ESRD is defined as kidney disease in its final stage, necessitating renal replacement therapy like hemodialysis and renal transplant[
11]. Whereas CKD is the deterioration of kidney structure and function caused by various conditions[
12]. Kidney transplantation has emerged as a potential therapeutic intervention that enhances life quality and longevity more than dialysis[
13]. Erectile dysfunction is highly prevalent among patients with chronic kidney disease in rates that reach even 70%, especially in those suffering from end stage renal disease.
Renal failure is a major risk for erectile dysfunction and about half of patients with chronic renal failure may be impotent which is multifactorial but primarily organic[
14]
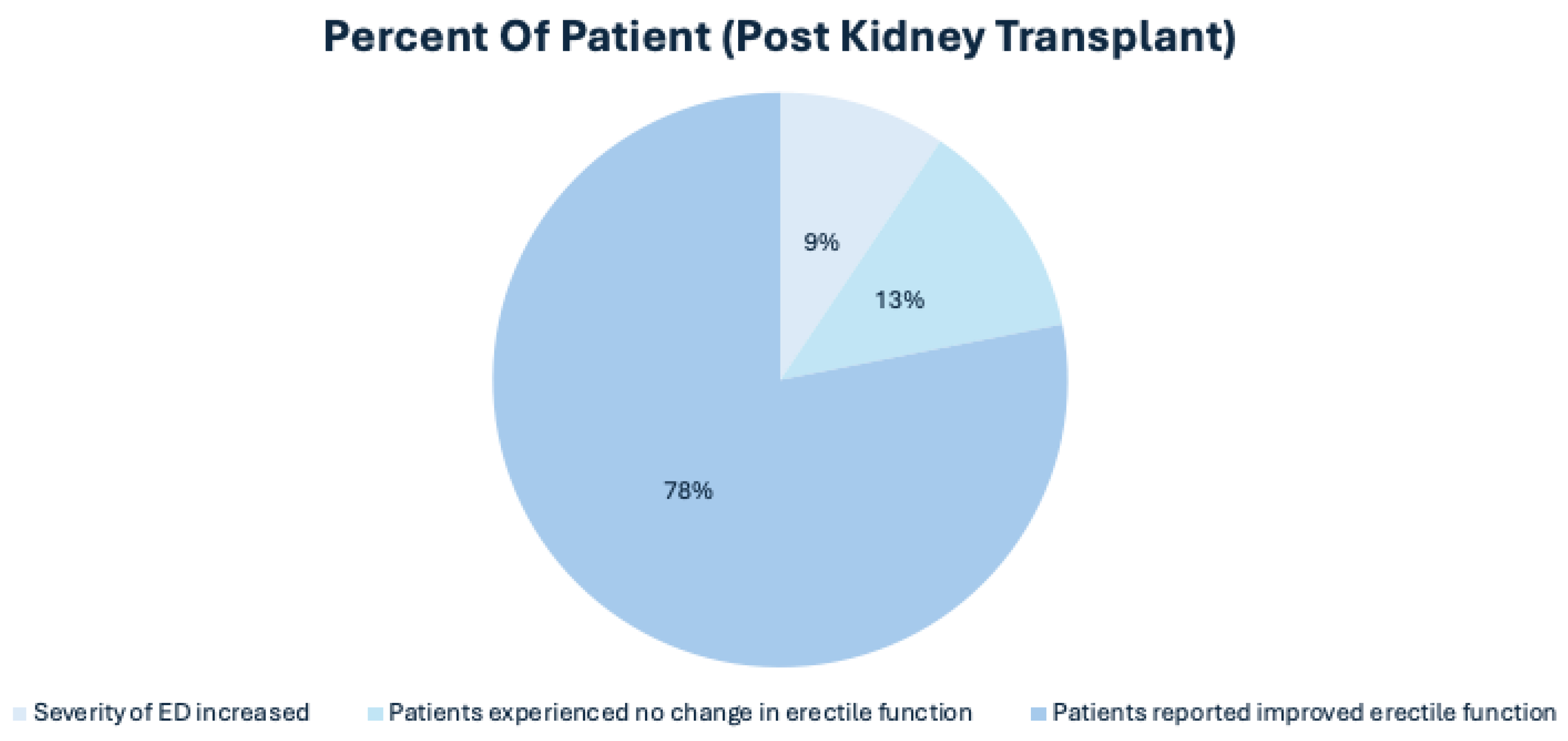
. Despite these promising findings, the relationship between kidney transplantation and ED remains inadequately explored. While kidney transplantation resolves the problem for some patients, erectile dysfunction continues to affect around 20–50% of transplant recipients[
15].The same study reports that most patients developed improvement in the erectile function after transplantation
. Conversely, many studies have focused on patients undergoing dialysis or those with end-stage renal disease (ESRD), leaving a gap in knowledge regarding the pre- and post-transplant experiences of patients with ED. After transplantation, age, comorbidities, drugs, vascular conditions, transplant surgical procedures, iterative transplantation, voluptuous habits, interpersonal problems, altered body image perception, and psychological factors (e.g., self-esteem, stress, and depression) may impact on ED. Furthermore, the psychosocial dimensions of sexual health, including the impact of depression, anxiety, and overall quality of life, are often overlooked in the context of renal transplantation and its effects on erectile function.
Understanding the hormonal changes, such as fluctuations in testosterone and thyroid levels, and the psychosocial stresses associated with the post-transplant period is crucial. This review synthesizes existing research to provide a comprehensive understanding of how kidney transplantation influences ED, focusing on hormonal alterations and psychosocial impacts in male patients. By assessing changes in erectile function, hormonal levels, and psychosocial factors before and after transplantation, we seek to provide a comprehensive understanding of how renal transplantation can influence sexual health outcomes. The findings from this research could inform clinical practices and enhance the quality of life for kidney transplant recipients, ultimately contributing to a more holistic approach to patient care in vulnerable population.
Pathophysiology of Erectile Dysfunction
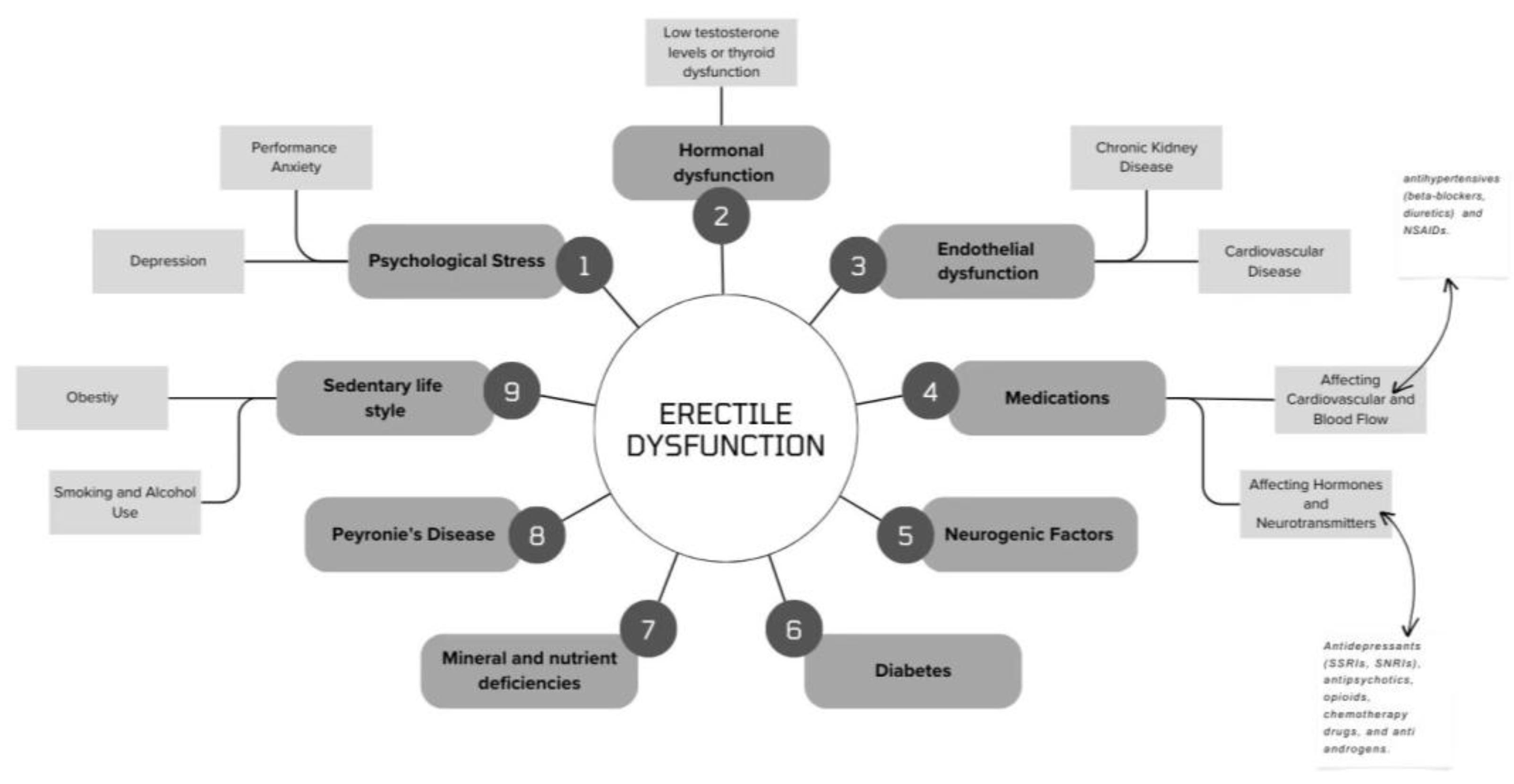
Erectile dysfunction (ED) represents a multifaceted condition that arises from a complex integration of neurovascular, hormonal, and psychological factors [
Figure 1]. Central to the erectile process is a neurovascular event triggered by sexual stimulation. Upon stimulation, nerve terminals within the cavernous tissue and endothelial cells release nitric oxide (NO), a vital vasodilator that facilitates increased blood flow into the penis. NO achieves this by activating soluble guanylate cyclase, leading to the production of cyclic guanosine monophosphate (cGMP), which ultimately results in relaxation of cavernosal smooth muscle and inflammation of the erectile tissue
Figure 1[
5,
16].
A critical aspect of achieving and maintaining a satisfactory erection is the hormonal environment, with testosterone playing a crucial role. Low testosterone levels have been correlated with increased prevalence of ED (shown in
Figure 2), as this hormone is integral for the maintenance of libido and erectile function [
17] . The disturbances in hormonal levels, particularly the presence of declined testosterone, are often observed in male patients with chronic kidney disease (CKD) and post-kidney transplantation. The etiology of ED can be broadly classified into three categories: psychogenic, organic, and mixed forms. Psychogenic ED encompasses issues tied to performance anxiety, depression, and other psychological factors, while organic ED can be linked to vascular, neurogenic, and endocrinological disorders [
18]. Additionally, the pathophysiology of ED is often compounded in populations with comorbid conditions like diabetes and hypertension, prevalent in CKD patients, who demonstrate a notable prevalence of ED [
19,
20]. In men with chronic renal disease, a combination of testicular failure and secondary disturbances in the pituitary-gonadal axis can be detected in the early stages of CKD and progressively worsen as the renal disease progresses[
21]. Exploring the multifactorial nature of ED among kidney transplant patients requires a thorough understanding of the intertwining physiological pathways and psychosocial implications. By simultaneously addressing these determinants through a multidisciplinary treatment approach, healthcare providers can optimize outcomes and improve sexual health for their patients navigating the post-transplant phase.
Some authors have reported that successful kidney transplantation may improve sexual function with reference to the previous situation of hemodialysis[
22]. NO is the primary neurotransmitter of penile erection. In chronic renal failure NO bioavailability is reduced. The expression of NO-synthase (NOS) has been shown to be altered thus leading to a disturbance in sexual function [
23]. Possible causes of NO deficiency are substrate limitation (L-arginine), because of disturbances in the renal biosynthesis of this amino acid and increased levels of circulating endogenous inhibitors of NOS especially asymmetric dimethylarginine (ADMA). Elevated levels of ADMA have emerged as an independent risk factor in end stage renal disease and reducing ADMA concentration might be a therapeutic goal[
24]. Hypogonadism (low testosterone) defined as total testosterone below 300 ng/mL is a prevalent condition in men with CKD especially in those undergoing dialysis and can contribute to decreased libido, ED, oligospermia infertility and anemia [
Table 1][
25] .
Histological changes in the testes revealed decreased spermatogenic activity especially in the later stages of spermatogenesis which are hormonally dependent [
23]. Testicular biopsy is often performed to demonstrate reduced spermatogenesis [
26]. Hypogonadism (low testosterone) defined as total testosterone below 300 ng/mL is a prevalent condition in men with CKD especially in those undergoing dialysis and can contribute to decreased libido, ED, oligospermia infertility and anemia [
25]. On the other hand, total plasma estrogen concentration is often elevated. The plasma concentration of the pituitary gonadotropin luteinizing hormone (LH) is elevated probably because of the decreased release of testosterone from the Leydig cells and the consequent loss of normal negative feedback. In addition, the metabolic clearance rate of LH is reduced, and it is not corrected by dialysis [
27]. Follicle-stimulating hormone (FSH) secretion is also elevated in men with CKD. A peptide erection and difficulty with ejaculation. Spironolactone can cause gynecomastia, decreased libido, and ED while drugs such as calcium antagonists, angiotensin converting enzyme (ACE) inhibitors and angiotensin II receptor blockers, are associated with lower incidence of these side effects. Other drugs commonly involved in the development of ED are cimetidine, tricyclic antidepressants, and metoclopramide[
28,
29,
30].
Prevalence of Erectile Dysfunction
Rosen et al [
31] have established the International Index of Erectile Dysfunction (IIEF) in 1997 which served as a pivotal tool for evaluating various aspects of male sexual function, including erectile function, orgasmic function, sexual desire, intercourse satisfaction, and overall satisfaction. This comprehensive questionnaire allows for an objective assessment of sexual function in male patients, which is critical in understanding the multifaceted nature of erectile dysfunction (ED). The prevalence of erectile dysfunction (ED) is significantly influenced by age, with a pronounced increase as individuals grow older. According to the Massachusetts Male Aging Study (MMAS), ED is reported in 8% of men in their 40s, escalating to 80% among those aged over 70 years [
32] . Furthermore, Messina et al [
33] found that men under 50 years with chronic kidney disease (CKD) exhibit a higher prevalence of ED compared to their counterparts over 50, mirroring the trends observed in the MMAS, where the incidents of impotence and ED prevalence are positively correlated with the age of subjects [
30]. In recent decades, there has been a significant global rise in the prevalence of end-stage renal disease (ESRD), attributed largely to advancements in renal replacement therapies. Individuals with ESRD often experience a diminished quality of life (QoL), a decline associated with various factors including age, complications from treatment, psychological issues, and the presence of co-existing health conditions [
34]. Mesquita et al [
35] reported that the overall prevalence of ED among patients with CKD was 76.5%, with rates of 72.3% in stage 3, 81.5% in stage 4, and 87.5% in stage 5 CKD. In terms of kidney transplant recipients, Espinoza et al [
36] observed an ED prevalence of 48.9% in their study involving men who had undergone kidney transplantation.. Rosas et al [
37] found that the prevalence of ED among all hemodialysis (HD) patients was 82% in a cross-sectional study of 302 subjects receiving treatment. Notably, among older HD patients (> 50 years), the prevalence of ED reached 90%, while it was observed at 63% in younger individuals (< 50 years) [
Table 2] [
37].
Comorbidities and Erectile dysfunction
Erectile dysfunction (ED) and kidney dysfunction are interlinked conditions, sharing several common risk factors associated with diseases that impair endothelial function, such as diabetes mellitus, hypertension, dyslipidemia, coronary artery disease, smoking, and obesity[
35]. Cigarette smoking is an established modifiable risk factor of arteriosclerosis. Notably, cigarette smoking is recognized as a modifiable risk factor for arteriosclerosis, with smokers exhibiting higher rates of ED compared to non-smokers. However, although there is a notable prevalence of smoking among men with severe or complete ED, these findings did not demonstrate statistical significance in multivariate analyses[
38]. Dyslipidemia is another condition correlated with an increased risk of ED, attributable to its detrimental effects on the endothelium and smooth muscle cells of the corpus cavernosum. The MMAS study did report a significant association between serum lipid levels and the prediction of ED[
32]. In contrast, findings from the Rancho Bernardo Study revealed that elevated serum cholesterol and triglyceride levels correlated with more severe ED, as men without ED consistently had lower cholesterol levels compared to those reporting moderate ED or no sexual activity. The relationship between hypertension and the onset of ED is well-established in numerous studies [
39,
40,
41], Nevertheless, uncertainty remains regarding whether hypertension is an independent risk factor for ED. In hypertensive patients, ED may arise either as a direct consequence of the condition itself or as an effect of the antihypertensive medications prescribed [
32,
42]. Given the evident association between ED and other vascular abnormalities, it is crucial for clinicians to evaluate CKD patients experiencing ED for cardiovascular disease (CVD) risks. Consequently, a thorough assessment of coexisting comorbidities and management of potential risk factors is essential in optimizing patient outcomes.
Erectile Dysfunction in Post-Transplant Patients
Kidney transplantation is regarded as the most effective therapeutic intervention for individuals suffering from chronic kidney disease (CKD) (
Figure 2). Many of these procedures are performed on middle-aged patients, a demographic for whom sexual function and fertility are of significant concern[
43]. Research indicates that erectile dysfunction (ED) remains notably prevalent among this population, with rates approaching 50% following kidney transplantation [
36,
44]. Post-operative sexual function may be compromised by a variety of factors, including graft malfunction and pre-existing comorbidities such as diabetes mellitus, hypertension, dyslipidemia, and smoking. Additional considerations include the duration of dialysis prior to transplantation and the effects of immunosuppressive or antihypertensive therapies, all of which can be linked to the initial cause of kidney insufficiency[
22,
45]. The duration of hemodialysis prior to transplantation, as reported by Rebollo et al [
10] may contribute to prolonged vascular damage and hormonal changes in dialysis patients, thereby influencing ED outcomes. Concerning immunosuppressive therapy, Malavaud et al [
44] found no statistically significant association between the use of cyclosporine and the incidence of ED, while Rebollo et al [
22] reported no connections between ED and tacrolimus usage. Interestingly, the combination of cyclosporine and prednisone may yield more favorable effects on gonadal function post-transplant compared to azathioprine [
46]. Normally, renal transplantation leads to the normalization of hormonal profiles in recipients, characterized by reduced levels of prolactin and luteinizing hormone (LH) alongside increased plasma testosterone [
46,
47,
48,
49] . However, it is essential to note that the recovery of sexual function is not uniformly observed; various factors can continue to affect erectile function, resulting in persistent high prevalence rates of ED among patients with renal insufficiency even after receiving a kidney transplant.
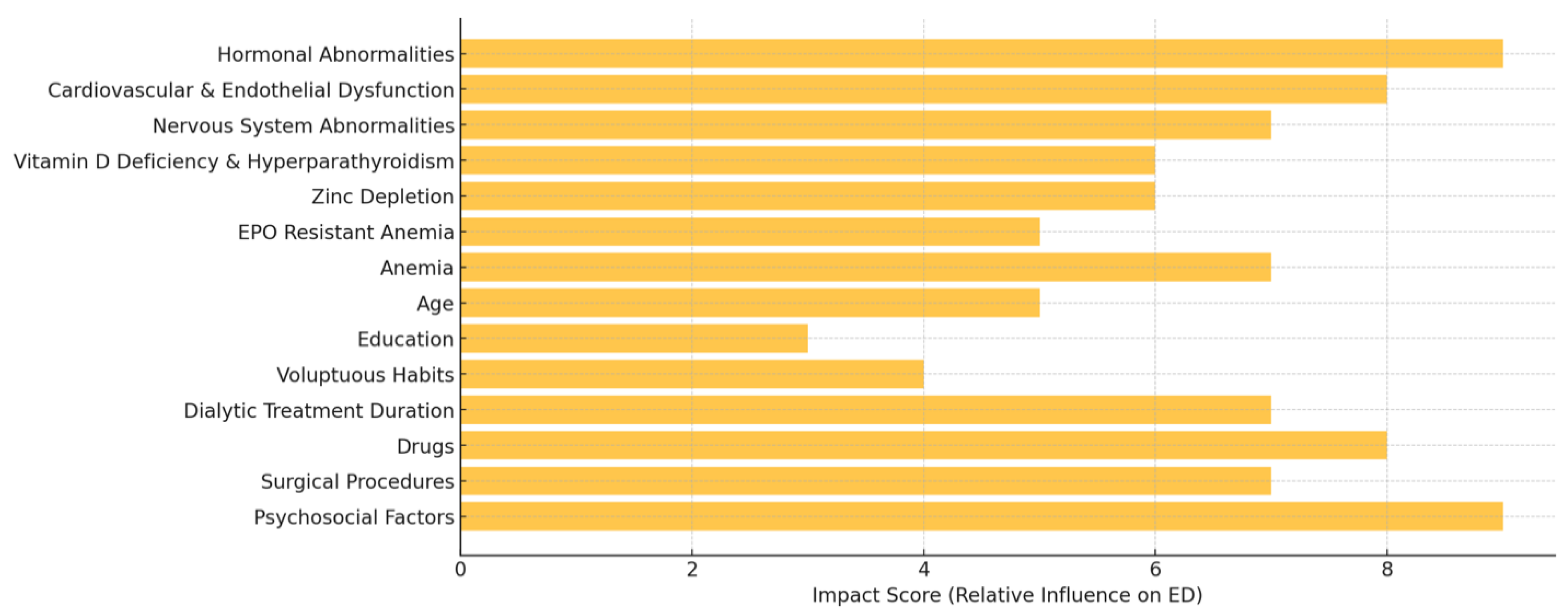
Erectile dysfunction (ED) in male patients with chronic kidney disease (CKD) and those who have undergone kidney transplantation involves an intricate interplay of hormonal, psychological, and physiological factors. Hormonal dysfunction is particularly significant (
Figure 3), as many CKD patients exhibit imbalances that can result in hypogonadism. This condition, marked by reduced testosterone levels, impacts both libido and erectile function, thereby contributing to the elevated prevalence of ED within this demographic [
50].
Testosterone is essential for regulating male sexual arousal and affects both central and peripheral mechanisms related to erectile function [
51]. Another significant endocrine disorder linked to erectile dysfunction is thyroid dysfunction. Additionally, hyperparathyroidism has been associated with the development of erectile dysfunction, potentially due to elevated prolactin levels. Clinical findings have highlighted a noteworthy connection between penile calcification in hemodialysis patients and the occurrence of erectile dysfunction [
52,
53]. Moreover, men with hypothyroidism frequently experience reduced erectile function and lower semen quality, contributing to the complex causes of erectile dysfunction (ED)[
54] . Additionally, endothelial dysfunction plays a critical role in erectile health among patients with chronic kidney disease (CKD). The endothelium produces nitric oxide (NO), which is crucial for vasodilation and ensuring sufficient blood flow to the penis. Damage to the endothelium, often resulting from conditions such as hypertension and diabetes, initiates a series of events that lead to vasoconstriction and heightened cardiovascular risks, both of which can worsen erectile dysfunction [
55]. Moreover, psychological factors are essential for comprehending the complete impact of erectile dysfunction in individuals with chronic kidney disease (CKD). The emotional burden of managing a chronic illness like kidney disease can lead to depression, decreased self-esteem, and increased relationship stress. These psychological challenges can be intensified by physical changes associated with kidney disease and its treatments, including surgical scars from transplantation and fluctuations in weight due to medications. Changes in body image often detrimentally influence sexual confidence and intimacy in relationships, establishing a feedback loop that can further impair erectile function [
51]. Chronic kidney disease (CKD) presents numerous risk factors for erectile dysfunction (ED), largely stemming from the stress of managing a serious health condition, which can lead to relational and interpersonal challenges. Research indicates that individuals undergoing dialysis frequently experience a higher prevalence of ED, attributed to a combination of factors such as diabetes, cardiovascular disease, and suboptimal dialysis treatments [
56]. The link between ED and cardiovascular disease is significant; erectile dysfunction can serve as an early warning indicator of vascular issues akin to those associated with chronic renal disease. The increased risk of cardiovascular mortality in this patient group highlights the importance of closely monitoring erectile function as a critical component of comprehensive care for CKD patients [
57]. Addressing erectile dysfunction in male kidney transplant recipients and patients with chronic kidney disease (CKD) requires a multidisciplinary approach that combines hormonal evaluations, psychological support, and the management of endothelial health. A comprehensive understanding of the relationship between these physical and psychological factors is crucial for optimizing patient outcomes and improving the quality of life for those impacted. By acknowledging the multifaceted nature of ED, healthcare providers can develop strategies that effectively address these complexities and enhance the overall well-being of patients.
Medications and Nutritional Deficiencies Impacting Erectile Dysfunction in Post-Kidney Transplant Patients: Hormonal, Cardiovascular, and Neurogenic Factors
Erectile dysfunction (ED) is a common and multifaceted challenge faced by male patients after kidney transplantation, largely influenced by medications and nutritional deficiencies. Immunosuppressants, particularly calcineurin inhibitors like cyclosporine and tacrolimus, are essential for preventing graft rejection. However, these medications can lead to vasoconstriction, which contributes to hypertension and restricts penile blood flow, thereby impairing erectile function [
21]. Additionally, many post-transplant patients need antihypertensive drugs to manage their blood pressure, with beta-blockers potentially worsening ED by reducing blood flow and lowering libido. Psychological factors are also significant, as kidney transplant recipients often deal with anxiety and depression. This can result in the prescription of SSRIs and other antidepressants, which can adversely impact sexual desire, delay orgasm, and create difficulties in achieving an erection by altering serotonin levels crucial for normal erectile function [
58]. Nutritional deficiencies, particularly in essential nutrients like Vitamin D and zinc, add another layer of complexity. Vitamin D is vital for regulating testosterone levels and maintaining overall male reproductive health. Low levels of this vitamin are commonly linked to hypogonadism in chronic kidney disease (CKD) and may persist even after transplantation, further exacerbating ED due to reduced testosterone production. Also, Vitamin D deficiency has been associated with endothelial dysfunction[
59], which can impair the production of nitric oxide necessary for adequate penile blood flow. Zinc deficiency, often seen in CKD patients due to dietary restrictions, adversely impacts testosterone levels and can contribute to issues with libido [
60]. Zinc is integral for testosterone synthesis and supports reproductive health by protecting tissues from oxidative stress[
61]. Zinc is crucial for testosterone synthesis and plays a protective role against oxidative stress in reproductive health. A deficiency not only disrupts testosterone production but also increases the risk of cellular damage, compounding erectile dysfunction. Medications, hormonal changes, and nutritional deficiencies creates a complex environment affecting erectile function in male kidney transplant recipients. A comprehensive understanding of these factors is vital for developing effective treatment strategies that address both the physiological and psychological aspects of ED in this vulnerable population.
Current Therapeutic Approaches for Erectile Dysfunction in Post-Kidney Transplant Patients
Testosterone Replacement Therapy (TRT) has emerged as a cornerstone in the management of erectile dysfunction (ED) among male kidney transplant recipients suffering from low testosterone levels. Testosterone is crucial for maintaining libido, energy levels, and overall sexual health. In the context of kidney transplant patients, testosterone deficiency often stems from multiple sources like the effects of chronic kidney disease (CKD), the side effects of immunosuppressive therapy, and the psychological stress associated with recovery from surgery[
14]. Research has consistently shown that nearly up to 50% of male kidney transplant recipients exhibit clinically low testosterone levels post-operation[
62] . The primary goal of TRT is to restore testosterone levels to normal ranges, potentially leading to significant improvements in sexual health and reduction of ED symptoms. Testosterone plays a vital role in the modulation of nitric oxide (NO) pathways, which are essential for vasodilation and, consequently, proper erectile function. By enhancing testosterone levels through TRT, blood flow to the penile tissues is improved, thereby facilitating erections. Furthermore, TRT can positively affect sexual drive, energy levels, and overall mood, addressing several interconnected issues that arise in the wake of kidney transplantation-induced ED. While TRT shows promise, it is not free from risk, especially in a population that is often on complex medication regimens. Significant concerns revolve around cardiovascular health; testosterone can potentially worsen hypertension and increase the risk of thromboembolic events. For instance, elevated testosterone levels may lead to erythrocytosis, raising hematocrit levels, which can subsequently heighten cardiovascular risks [
63]. Additionally, the interaction between TRT and immunosuppressive agents, such as corticosteroids and calcineurin inhibitors, demands close scrutiny, as TRT might modify the metabolism and effectiveness of these essential medications. In scenarios where TRT is deemed inappropriate or contraindicated, alternatives such as clomiphene citrate, an estrogen receptor modulator, may be considered. Clomiphene functions by stimulating the body’s intrinsic testosterone production without supplementing it directly, thereby mitigating some of the associated risks linked with direct testosterone therapy. Evidence indicates that clomiphene can enhance testosterone levels without significantly increasing the likelihood of complications like polycythemia or cardiovascular issues often attributed to TRT [
64,
65]. Given the potential adverse effects associated with TRT, a comprehensive evaluation is paramount before treatment commencement. Baseline assessments of cardiovascular health, along with the regular monitoring of hematocrit, lipid profiles, and prostate health, should be standard practice to ensure the therapeutic regimen’s safety. In conclusion, while TRT presents significant potential for improving ED and the overall quality of life in post-transplant patients, careful individualized assessment and ongoing monitoring are critical for balancing its benefits against inherent risks.
The psychosocial aspects of ED in post-kidney transplant patients are equally critical, as psychological stressors can significantly impact sexual health independently. Interventions such as cognitive-behavioral therapy (CBT), counseling, and other psychosocial approaches have demonstrated efficacy in managing ED, particularly when linked to underlying anxieties, depression, and performance-related stress. These therapies not only assist patients but also their partners in addressing the emotional and relational dynamics that may arise following surgery, thereby enhancing both quality of life and sexual health. Among the various therapeutic modalities, CBT stands out as one of the most extensively supported interventions for ED linked to psychological factors[
66]. In CBT, therapists guide patients to identify and modify negative thought patterns, beliefs, and behaviors that may contribute to their ED. For example, post-transplant patients often grapple with performance anxiety related to health concerns, organ rejection, or potential medication side effects. CBT helps patients reframe these fears and develop healthier coping strategies, thus reducing psychological barriers to sexual function. Empirical studies substantiate the effectiveness of CBT in improving ED symptoms and enhancing sexual satisfaction. Research conducted showed that individuals undergoing CBT reported marked improvements in sexual confidence and reduced performance anxiety, both of which are pivotal in restoring erectile function[
67]. Additionally, CBT can address broader post-transplant concerns[
68], such as self-esteem and body image, which are common challenges faced by patients post-surgery. Furthermore, psychosocial support should extend beyond individual therapy to encompass relationship counseling. For many transplant patients, ED can place a strain on intimate relationships, often leading partners to misinterpret the patient’s reluctance to engage sexually as a lack of interest or desire. Relationship therapy serves as a platform to facilitate open communication, enhance empathy, and develop shared strategies for intimacy and support. Such therapeutic relationships not only bolster sexual function but also contribute to greater marital satisfaction, reflecting the significance of treating ED as a relational issue, rather than merely a physiological one. A comprehensive approach to managing erectile dysfunction in post-kidney transplant patients necessitates addressing both hormonal and psychosocial dimensions. By combining effective hormonal therapies with robust psychosocial interventions, healthcare providers can enhance patient outcomes and improve the overall quality of life for this vulnerable population.
Figure 4.
The diverse molecular and psychological factors influencing ED across multiple levels.
Figure 4.
The diverse molecular and psychological factors influencing ED across multiple levels.
Challenges and Future Directions
While there have been significant strides in understanding and managing erectile dysfunction (ED) in male kidney transplant recipients, several challenges persist that necessitate urgent attention from the medical community. One of the foremost obstacles is the limited understanding of the long-term effects of hormonal therapies on the overall transplant outcomes for patients. Given that testosterone plays a vital role in sexual health and is often deficient post-transplant, there's a pressing need to conduct longitudinal studies that evaluate how long-term testosterone replacement therapy (TRT) impacts not only sexual function but also other critical aspects such as transplant rejection rates, metabolic health, and cardiovascular risks. The relationship between improved sexual health from TRT and potential adverse outcomes such as increased rate of organ rejection due to immunologic changes remains inadequately studied. Understanding these dynamics is paramount for developing comprehensive care protocols that prioritize both sexual health and the long-term viability of the transplanted organ. Further complicating matters is the multifactorial nature of ED itself. While hormonal imbalances are a significant contributor, psychosocial factors including anxiety, depression, and body image concerns equally impact patient outcomes. Thus, rigorous clinical trials are essential to identify the most effective psychosocial interventions tailored specifically for this population. Such interventions should not only focus on individual therapy but also encompass couple-based approaches that foster healthy communication and intimacy post-transplant. Current research on psychosocial treatments often lacks specificity to the unique challenges faced by kidney transplant recipients, hindering the development of optimal therapeutic strategies. Moreover, the intricacies of TRT in the context of concurrent medications pose another challenge.
Table 3.
Challenges and Research Gaps in ED Management Post-Transplant.
Table 3.
Challenges and Research Gaps in ED Management Post-Transplant.
| Challenge |
Key Issues |
Research Gaps |
| Hormonal Therapy |
Limited data on long-term TRT outcomes |
Impact on rejection, metabolic health, CV risks |
| Psychosocial Factors |
Anxiety, depression, body image concerns |
Lack of transplant-specific interventions |
| Drug Interactions |
TRT and immunosuppressants |
Need for safety evaluations in transplant patients |
| Interdisciplinary Collaboration |
Lack of coordinated care |
Developing comprehensive care protocols |
The interaction between TRT and immunosuppressive agents (such as calcineurin inhibitors and corticosteroids) necessitates further exploration to ensure that testosterone supplementation does not compromise immunosuppressive efficacy. Specific attention should be paid to evaluating the safety profiles of various hormone therapies, especially given the heightened cardiovascular risk associated with altered testosterone levels in this already vulnerable population. More systematic reviews and randomized controlled trials are warranted to establish clear guidelines and best practices concerning the initiation of hormonal therapies in kidney transplant recipients. Lastly, fostering interdisciplinary collaboration among nephrologists, urologists, endocrinologists, and mental health professionals will be critical to surmounting these challenges. By integrating insights from various specialties, healthcare providers can create holistic, patient-centered care plans capable of addressing the complex interplay between physical and psychological factors in ED management post-transplant.
Conclusion
Erectile dysfunction remains a prevalent and multifactorial health issue among male kidney transplant recipients, stemming from a complex interplay of hormonal changes, psychosocial stress, and the consequences of chronic illness. The impact of ED transcends mere sexual function, influencing self-esteem, relationship dynamics, and overall quality of life for patients navigating the post-transplant landscape. To effectively tackle these challenges, a comprehensive multidisciplinary approach is essential. This approach must contemplate both medical interventions—particularly the optimization of hormonal therapies—and robust psychosocial support interventions tailored to the unique circumstances of post-transplant patients. Integrating psychological counseling, sexual health education, and relationship therapy alongside pharmacological strategies may create a more supportive environment for patients as they reintegrate into their intimate lives. Future research avenues should prioritize refining and standardizing hormonal treatments, exploring the long-term implications of therapy on health outcomes, and identifying psychosocial interventions that resonate with the experiences of this patient population. By doing so, healthcare professionals can significantly enhance patient outcomes, alleviate the burden of ED, and ultimately improve the quality of life for kidney transplant recipients, ensuring they experience a more fulfilling post-transplant journey.