1. Introduction
Conventional cardiopulmonary resuscitation (CCPR) has been the foundational approach to resuscitating children and adults for decades, providing a lifeline through manual chest compressions and ventilatory support [
1]. Yet, its effectiveness is often limited by various factors, including the quality of compressions and the patient's underlying health conditions. The advent of Extracorporeal Membrane Oxygenation (ECMO) assisted CPR (ECPR) allows a potentially superior alternative, promising to redefine the boundaries of life-saving care [
2].
ECPR is a complex treatment modality, and instituting ECMO under CPR conditions can compromise the quality of conventional CPR efforts [
3]. Beyond the complexity of performing cannulation under CPR, ECMO itself is a high-risk treatment modality that is associated with significant morbidity and mortality [
4]. Finding the balance between lower complexity and lower treatment risk of conventional CPR against higher complexity and higher treatment risk, but potentially better outcomes of ECPR, remains challenging. Additionally, several studies have shown that the time from arrest to initiation of ECMO flows is negatively related to improved outcomes after ECPR [
5]. Committing a patient early during resuscitation to ECPR may be beneficial as this may shorten the time to ECMO flow. Equally, persisting with CCPR may be beneficial as ECMO is a high risk, resource intense treatment modality [
3].
To improve our understanding which patients may benefit from prompt conversion from CCPR to ECPR we performed the here presented analysis which aims to establish pre CPR-event variables that may predict the need for ECPR, or the success of CCPR. Additionally, we aim to compare outcomes between the two treatment modalities.
2. Materials and Methods
We performed a retrospective analysis of pediatric in-hospital events requiring CPR that occurred in a tertiary paediatric intensive care unit (PICU). First, we assessed whether any pre CPR-event variables were associated with the need to convert from CCPR to ECPR. Second, we analysed the survival outcomes for either event.
Patients were identified via an institutional database where all CPR-events in the PICU are recorded.
Inclusion criteria were: age less than 18 years, admission to PICU between 2016 and 2022, and occurrence of an event that required cardiopulmonary resuscitation (with cardiac compressions) in PICU. We used the definition of “event requiring CPR” or “CPR-event” rather than “cardiorespiratory arrest”, as the distinction between severe bradycardia versus asystolic arrest is not clearly defined, and more recent guidelines recommend commencing CPR when there are no signs of life rather than be guided by the specifics of a detected or diagnosed rhythm [
6]. Patients were excluded if their CPR-event occurred outside of the PICU, including out-of-hospital CPR-events. We recorded the duration of the CPR-event, from the commencement of CPR until the return of spontaneous circulation (ROSC). For ECPR cases we only recorded the time to ECMO flow, independent on whether they had ROSC prior to the commencement of ECMO flows.
At our institution, decision to provide ECPR is physician led, though in principle all children with CPR-events qualify for ECPR, unless they meet contraindications for ECMO support. Such contraindications include severe life limiting illnesses, pre-existing severe disease limiting cerebral functioning, severe coagulopathy, technical inability to provide ECMO (such as severe thromboses). Our analysis was deemed a quality assurance activity by the local Ethics and Human Research Committee (HREC) and was therefore exempt from requiring HREC approval or patient consent for use of the data.
Data Analysis
Data were cleaned and screened for outliers, missing values, and inconsistencies prior to analysis. Moderate proportions (28%) of missing observations were present for pre CPR-event clinical measurements, with no missing values for all other reported variables.
Descriptive statistics were calculated for the CCPR and ECPR groups to summarise the participants' baseline characteristics. Due to strongly skewed distributions, continuous variables were summarised using medians and interquartile ranges (IQRs), with frequencies and percentages reported for categorical variables.
Bivariate penalised logistic generalised estimating equation (GEE) models were constructed to assess the association between the patient characteristics, pre-CPR-event lab measurements, and conversion from CCPR to ECPR. Penalised logistic GEEs, as described by Geroldinger et al. [
8], were applied to account for quasi-complete separation in the multivariable setting and the occurrence of repeated cardiac arrests within PICU admissions. An exchangeable correlation structure was assumed between arrests, and cluster robust standard errors were calculated for effect estimates. All covariates evaluated in the bivariate setting, excluding admission weight, were included in a multivariable penalised logistic GEE model to assess their association with the outcome upon controlling for baseline characteristics and potential confounders. These covariates included age, sex, admission diagnosis, pre CPR plasma lactate, and pre CPR pH. Weight was excluded from the multivariable model due to substantial collinearity with age, and superior model fit with the inclusion of the latter.
Complete case analyses were conducted using the bivariate and multivariable penalised logistic GEE models. Additionally, a sensitivity analysis was performed where missing pre CPR-event measurement observations were imputed prior to model construction using multiple imputation by chained equations [
9]. Linear mixed-effects regression was used for imputation, with all covariates in the multivariable model included as fixed effects, and PICU admission identifiers included as random intercepts. One hundred imputed datasets were generated, with bivariate and multivariable models fit to the imputed datasets and estimated odds ratios and confidence intervals combined using Rubin’s rules [
9].
Odds ratios (OR) and 95% confidence intervals (95% CIs) for both the complete case analysis and multiple imputation are reported for the bivariate and multivariable models. Kaplan-Meier analysis was conducted to assess differences in survival time following the respective CPR-event between the ECPR and CCPR groups. Survival time was censored at the time of commencement of a subsequent arrest, PICU discharge, or 90 days following arrest, with all-cause mortality as the event of interest.
As this is a convenience sample, the study is not powered for statistical comparisons and therefore p-values are not reported. Analyses were undertaken using the R programming language (version 4.4.0), the modified geefirthr package by Geroldinger et al. [
8], and the mice and survival packages [
10,
11].
3. Results
Demographics
A total of 201 CPR-events occurred between January 2016 and December 2022 in 164 children in the PICU, over a total of 160 hospital admissions. Of these 201 CPR-events, 45 (22.4%) led to ECMO support. The ECPR group versus the CCPR group consisted of a higher proportion of neonates (55.3% vs. 27.0%) and patients with cardiac surgical diseases, as compared with other diseases (55.3% vs. 32.5%;
Table 1).
CPR-Event Characteristics
CPR-events occurred primarily outside of daylight hours (62.2%) and were predominantly asystolic and/or bradycardic episodes (57.2%). The median time to ROSC was 2 minutes (IQR: 1, 5) for the CCPR group. For the ECPR group the median time to ECMO flow was 43 minutes (IQR: 30, 64). ROSC was achieved in 93.6% of CCPR-events. Patients with CCPR received a median of 1 dose (IQR: 0, 2) of epinephrine versus 7 doses (IQR: 4, 11) that were given in ECPR patients (
Table 2). Pre CPR-event laboratory values were similar for creatinine, pH and pCO2. The median serum lactate was 1.8 mmol/L (IQR: 1.0, 3.6) in the CCPR, and 4.5 mmol/L (IQR: 1.6, 7.4) in the ECPR group. The pre CPR-event mean arterial pressure and heart rate did not differ between the two groups (
Table 2).
Of the 156 CCPR-events, 22 (14.1%) lasted longer than 10 minutes. In contrast, 43 (95.6%) of the 45 ECPR-events lasted longer than 10 minutes. Six (4.8%) patients in the CCPR group received elective ECMO support during their PICU stay, however they did not receive ECPR and are represnted in the CCPR group, not the ECPR group. Three patients in the ECPR group had a CPR-event while on ECMO and re-establishing ECMO flow took less than 10 minutes.
Outcomes
The duration of mechanical ventilation was 6 days (median, IQR: 3, 16) in the CCPR versus 14 (IQR: 9, 30) days in the ECPR group. The median PICU length of stay was 13 (IQR: 6, 31) vs. 19 (IQR: 9, 34) days, and median hospital length of stay was 37 (IQR: 14, 94) vs. 39 (IQR: 19, 65) days in the CCPR and ECPR group, respectively. Eleven (7.1%) patients died within two hours of their CPR-event in the CCPR group versus none in the ECPR group. The PICU mortality was 27.8% in the CCPR, and 50% in the ECPR group, with the hospital mortality showing similar numbers. Four patients were transferred out of the PICU, resulting in a denominator of 160 patients for the hospital mortality.
Fifty-four patients died. The admission diagnosis of “Cardiac Surgical” was associated with the highest mortality. Of 19 deaths in the ECPR group, 10 (52.6%) were admitted for cardiac surgical reasons. All ECPR-events occurred after their surgical repair.
Of 134 CCPR-events that lasted less than or equal to 10 minutes, 21 (15.7%) led to death. Of the 22 CCPR-events that lasted longer than 10 minutes, 15 (68.2%) resulted in death (
Table 3).
Timing and Reason for Demise
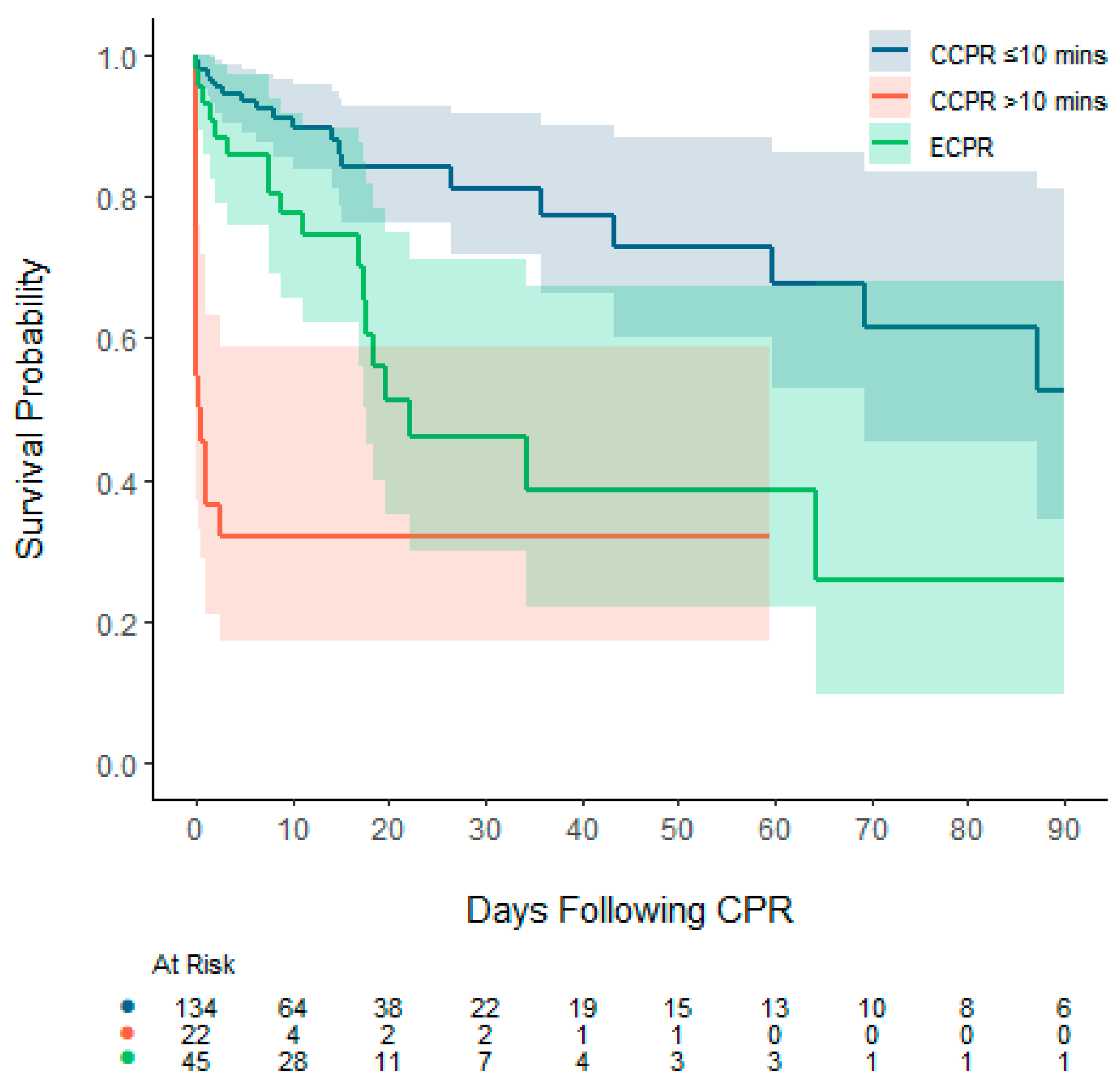
Deaths occurred at a median of 3 days (IQR: 0, 17) after the CPR-event. After ECPR, deaths occurred at a median of 10 days (IQR: 3, 18), versus a median of one day (IQR: 0, 15) for patients after CCPR. After ECPR, deaths occurred in an initial period of up to 64 days, whereas after CCPR, deaths continued to occur up to 87 days post-arrest (
Figure 1). Amongst CPR-events lasting longer than 10 minutes, deaths occurred at a median of 9 days (IQR: 2, 18) following ECPR and 0 days (IQR: 0, 0) following CCPR (
Table 3).
The majority of deaths (74.1%) occurred due to elective withdrawal of life-sustaining treatments due to the severity of overall illness. In the ECPR group, this amounted to 89.5% of deaths, whereas in the CCPR group, in 65.7% life sustaining therapies were ceased. (
Table 3).
In nine events (4.5%) ROSC could not be achieved. In over 50% of cases this was due to pulmonary hypertensive crises. None of these patients were ECPR supported.
In four patients death occurred due to illnesses or events that were unrelated to the initial condition that necessitated CPR. Cardiac conditions were the most common cause of death among both the ECPR (57.9%) and CCPR (28.6%) groups.
Bivariate and Multivariable Analysis
In both the complete case analysis and analysis following multiple imputation, serum lactate concentration was associated with a conversion of CCPR to ECPR in the bivariate and multivariable settings. An association was observed in the bivariate setting between admission diagnosis and conversion of CCPR to ECPR in both the complete case and multiple imputation analysis, however, was not present in the multivariable setting. No associations were observed between conversion of CCPR to ECPR and age, sex, or pH across all analyses and settings (
Table 4). Duration of CRP was highly predictive of conversion from CCPR to ECPR in both analyses, where duration of CPR was included.
4. Discussion
Predicting which patients require escalation from CCPR to ECPR during a CPR-event remains challenging, and data in the literature is lacking. Where CCPR-events are compared to ECPR ones, comparisons focus on outcome differences between the two when used for resuscitation, rather than factors that may predict a conversion from CCPR to ECPR [
12,
13,
14]. To deepen our understanding of resuscitation events and the need for ECPR we attempted to identify pre CPR-event factors associated with the need for ECPR, or with success of CCPR.
We found that cardiac surgical diagnosis and pre CPR-event serum lactate levels were positively associated with conversion to ECPR. This demonstrates that presence of these patient or laboratory findings should alert clinicians of the increased risk that a CCPR-event may need escalation to ECPR. On the other hand, CPR-events that were the result of respiratory arrest events rarely converted to ECPR, making this group unlikely to need ECPR. Duration of CPR was highly predictive of conversion from CCPR to ECPR, though this is not a suprising finding, given that ECPR is instituted after CCPR is unsuccessful for a finite period of time.
While the benefits of ECPR for out-of-hospital cardiac arrests continue to be debated, some data suggest that for in-hospital cardiac arrest (IHCA) there may be a benefit when offering ECPR [
12,
13,
15]. Most recently, Kobayashi demonstrated that ECPR improved survival when CPR continued for more than 10 min [
16]. All these analyses follow the clinical reality where ECPR is usually decided on after five minutes of CPR and implemented after 30 to 40 min, mainly due to the complexity of the ECMO cannulation process. Our study shows a similar finding, where mortality in CPR-events that lasted more than 10 minutes was very high should CCPR continue and ECPR not be employed. In fact, after 10 minutes of CPR, survival in the CCPR group was inferior to survival in the ECPR group – a finding that is similar to those of Kobayashi et al [
16]. The Kaplan Meier graph shows how survival can be divided into three groups: those with CPR-events shorter than 10 minutes, patients who received ECPR and those who had CPR-events longer than 10 minutes who didn’t receive ECPR. Our data suggest that using ECPR over CCPR after short CPR-events may not be associated with higher survival whereas for longer CPR-events, the converse may be true, where ECPR may be associated with higher survival compared to CCPR. These findings question the threshold benefit of ECPR versus CCPR, in a similar way as ECMO provision has demonstrated to lead to poorer survival in low-risk but higher survival in high-risk patients, albeit for sepsis and congenital diaphragmatic hernia patients, rather than undefined CPR-events [
17,
18].
Hospital survival was approximately 50% and 70% for patients that received ECPR and CCPR, respectively. The ECPR survival for this cohort was lower than our previously reported ECPR outcomes over a longer time period, likely due to variations in survival between years, and variations in illness severity of patients that were supported with ECMO [
19]. The majority of mortality in the ECPR group occurred due to elective withdrawal of support due to the severity of the underlying condition rather than complications of ECMO. This demonstrates the initial effectiveness of ECPR and the uncertainty for long-term survival at the time of ECPR institution.
Our hospital survival of 70% after CCPR-events compares favourably with the literature, where IHCA survival is quoted at around 50%, most recently by Frazier et al. [
20]. Our numbers may well be higher due to the fact that very short CPR-events were included in our cohort. We included a Kaplan Meier analysis in our report given that the trajectory of survival is a finding that – to our knowledge – has not been reported before in the literature. While the ECPR mortality seems to occur slightly later than after CCPR events, it plateaus after 64 days, whereas the CCPR mortality, while overall lower than that of the ECPR group, likely due to a lower disease severity pre-CPR-event, continues to occur longer after the CPR-event. As such, IHCA events may be seen as a risk factor for ongoing mortality, possibly well into the future of a patient’s journey.
Limitations
The retrospective nature of our analysis limits the comparability of the ECPR and CCPR group: some patients in the CCPR group, who received prolonged resuscitation may not have been offered ECPR due to factors clinicians considered at the time of resuscitation, thereby limiting their comparability. Our study is limited to patients within the PICU. Patients outside the PICU are not monitored as closely as those in the PICU, and had we included these patients in our study, there would have been a larger number of missing pre-CPR-event observations. This limitation to PICU patients, however, limits the generalisability of our findings. Lastly, our study is a single-centre study, with institutional practices that may vary compared to other centres.
5. Conclusions
Predicting the need for ECPR at the outset of a CCPR-event remains challenging. Pre-CPR-event serum lactate concentrations are associated with the need to convert from CCPR to ECPR and may, therefore, serve as markers for a higher likelihood of a need for ECMO support. Any CCPR-event should alert clinicians that, even if the patient recovers from the event, their mortality risk remains high, even at a time well after the CPR-event has resolved.
Author Contributions
Conceptualization, AM, KJ, SM; Methodology, ML, KJ, RL, ES, KG; Formal analysis, ES, KG; Data curation, ES, KG; Writing—original draft preparation, AM; writing—review and editing, AM, KJ, ES, KG, SM; Project administration, KJ; Funding acquisition, AM. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a “Study, Education and Research Trust Account (SERTA)” grant by the Queensland Children’s Hospital, Brisbane, Australia.
Institutional Review Board Statement
Our analysis was deemed a quality assurance activity by the local Ethics and Human Research Committee (HREC) and was therefore exempt from requiring HREC approval or patient consent for use of the data.
Informed Consent Statement
Patient consent was waived due to this study being a retrospective review of anonymized data.
Data Availability Statement
The data presented in this study are available on request from the corresponding author after data sharing agreements have been established.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CPR |
Cardiopulmonary resuscitation |
| CCPR |
Conventional cardiopulmonary resuscitation |
| ECMO |
Extracorporeal membrane oxygenation |
| ECPR |
ECMO assisted CPR |
| HREC |
Human Research and Ethics Committee |
| IQR |
Interquartile Range |
| OT |
Operating theatre |
| PICU |
Paediatric Intensive Care Unit |
| ROSC |
Return of Spontaneous Circulation |
| VA |
Veno-arterial |
| VV |
Veno-venous |
References
- Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet. 2010;375:1347-54. [CrossRef]
- Bimerew M, Wondmieneh A, Gedefaw G, Gebremeskel T, Demis A, Getie A. Survival of pediatric patients after cardiopulmonary resuscitation for in-hospital cardiac arrest: a systematic review and meta-analysis. Ital J Pediatr. 2021;47:118. [CrossRef]
- Taeb M, Levin AB, Spaeder MC, Schwartz JM. Comparison of Pediatric Cardiopulmonary Resuscitation Quality in Classic Cardiopulmonary Resuscitation and Extracorporeal Cardiopulmonary Resuscitation Events Using Video Review. Pediatr Crit Care Med. 2018;19:831-8. [CrossRef]
- Jin Y, Gao P, Zhang P, Bai L, Li Y, Wang W, et al. Mortality prediction in pediatric postcardiotomy veno-arterial extracorporeal membrane oxygenation: A comparison of scoring systems. Front Med (Lausanne). 2022;9:967872. [CrossRef]
- Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D, et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care. 2017;21:157. [CrossRef]
- Wyckoff MH, Greif R, Morley PT, Ng KC, Olasveengen TM, Singletary EM, et al. 2022 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation. 2022;146:e483-e557. [CrossRef]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [CrossRef]
- Geroldinger A, Blagus R, Ogden H, Heinze G. An investigation of penalization and data augmentation to improve convergence of generalized estimating equations for clustered binary outcomes. BMC Med Res Methodol. 2022;22:168. [CrossRef]
- Rubin, DB. Multiple imputation for nonresponse in surveys. New York ;: Wiley; 1987.
- Therneau, TM. A Package for Survival Analysis in R. 2024.
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software. 2011;45:1 - 67. [CrossRef]
- Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015;86:88-94. [CrossRef]
- Dennis M, Buscher H, Gattas D, Burns B, Habig K, Bannon P, et al. Prospective observational study of mechanical cardiopulmonary resuscitation, extracorporeal membrane oxygenation and early reperfusion for refractory cardiac arrest in Sydney: the 2CHEER study. Crit Care Resusc. 2020;22:26-34. [CrossRef]
- Ahn C, Kim W, Cho Y, Choi KS, Jang BH, Lim TH. Efficacy of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation for adult cardiac arrest patients: a systematic review and meta-analysis. Sci Rep. 2016;6:34208. [CrossRef]
- Kim SJ, Kim HJ, Lee HY, Ahn HS, Lee SW. Comparing extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: A meta-analysis. Resuscitation. 2016;103:106-16. [CrossRef]
- Kobayashi RL, Gauvreau K, Alexander PMA, Teele SA, Fynn-Thompson F, Lasa JJ, et al. Higher Survival With the Use of Extracorporeal Cardiopulmonary Resuscitation Compared With Conventional Cardiopulmonary Resuscitation in Children Following Cardiac Surgery: Results of an Analysis of the Get With The Guidelines-Resuscitation Registry. Crit Care Med. 2024;52:563-73. [CrossRef]
- Schlapbach LJ, Chiletti R, Straney L, Festa M, Alexander D, Butt W, et al. Defining benefit threshold for extracorporeal membrane oxygenation in children with sepsis-a binational multicenter cohort study. Crit Care. 2019;23:429. [CrossRef]
- Does extracorporeal membrane oxygenation improve survival in neonates with congenital diaphragmatic hernia? The Congenital Diaphragmatic Hernia Study Group. J Pediatr Surg. 1999;34:720-4; discussion 4-5. [CrossRef]
- Mattke AC, Stocker CF, Schibler A, Alphonso N, Johnson K, Karl TR. A newly established extracorporeal life support assisted cardiopulmonary resuscitation (ECPR) program can achieve intact neurological outcome in 60% of children. Intensive Care Med. 2015;41:2227-8. [CrossRef]
- Frazier ME, Brown SR, O'Halloran A, Raymond T, Hanna R, Niles DE, et al. Risk factors and outcomes for recurrent paediatric in-hospital cardiac arrest: Retrospective multicenter cohort study. Resuscitation. 2021;169:60-6. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).